PAD Rehabilitation Toolkit A Guide for Healthcare Professionals
PAD Rehabilitation Toolkit A Guide for Healthcare Professionals Healthy Steps for Peripheral Artery Disease (PAD) Developed by AACVPR and the Vascular Disease Foundation
What is PAD? Peripheral artery disease (PAD) results from systemic atherosclerosis and involves blood vessels throughout the body however, PAD is most commonly used in reference to lower extremity disease.

About PAD • PAD symptoms result from limited arterial blood flow, which causes debilitating, activity-induced, ischemic pain (intermittent claudication) • PAD is associated with major limitations in mobility and physical functioning, and decreased quality of life • Not all persons with PAD have symptoms • Subsequent risk for other manifestations of CVD (heart attack and stroke) is high
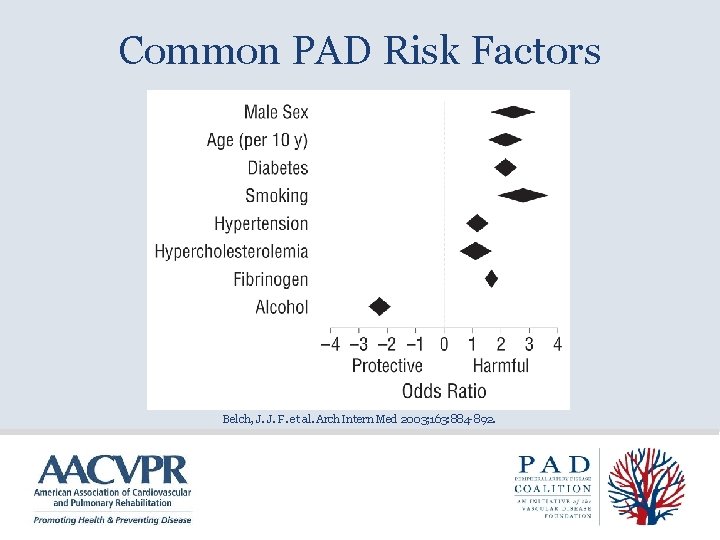
Common PAD Risk Factors Belch, J. J. F. et al. Arch Intern Med 2003; 163: 884 -892.
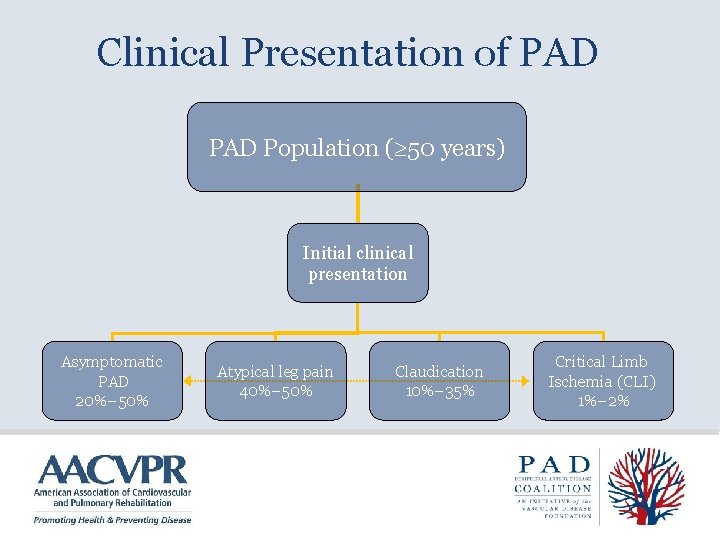
Clinical Presentation of PAD Population ( 50 years) Initial clinical presentation Asymptomatic PAD 20%– 50% Atypical leg pain 40%– 50% Claudication 10%– 35% Hirsch AT et al. J Am Coll Cardiol. 2006; 47: 1239 -1312. Critical Limb Ischemia (CLI) 1%– 2%
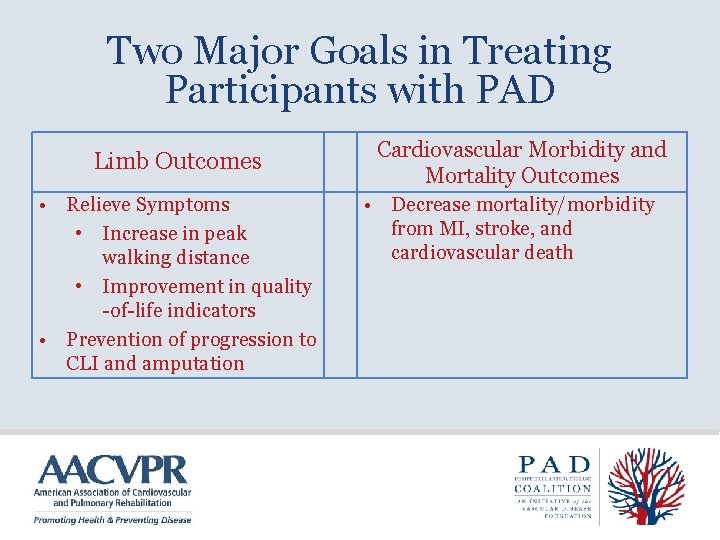
Two Major Goals in Treating Participants with PAD Limb Outcomes • Relieve Symptoms • Increase in peak walking distance • Improvement in quality -of-life indicators • Prevention of progression to CLI and amputation Cardiovascular Morbidity and Mortality Outcomes • Decrease mortality/morbidity from MI, stroke, and cardiovascular death
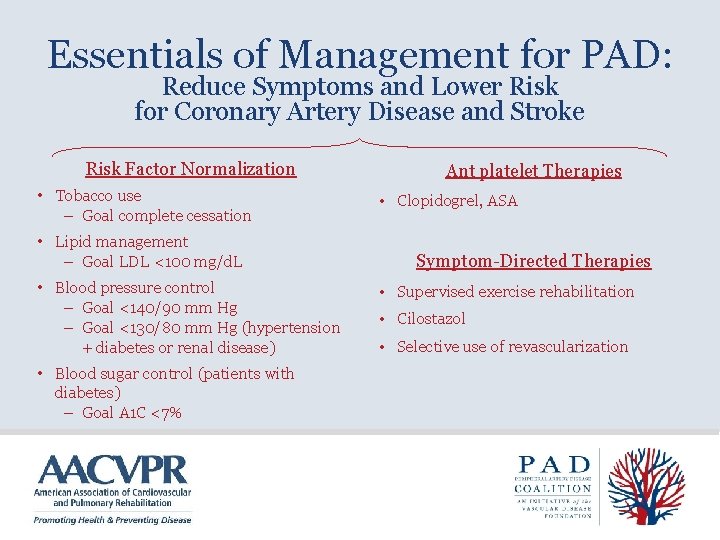
Essentials of Management for PAD: Reduce Symptoms and Lower Risk for Coronary Artery Disease and Stroke Risk Factor Normalization • Tobacco use – Goal complete cessation • Lipid management – Goal LDL <100 mg/d. L • Blood pressure control – Goal <140/90 mm Hg – Goal <130/80 mm Hg (hypertension + diabetes or renal disease) • Blood sugar control (patients with diabetes) – Goal A 1 C <7% Ant platelet Therapies • Clopidogrel, ASA Symptom-Directed Therapies • Supervised exercise rehabilitation • Cilostazol • Selective use of revascularization
Intermittent Claudication (IC) • “Claudicatio” (Latin: “to limp”) Claudius was known to limp • A symptom of PAD characterized by pain, aching, or fatigue in exercising leg muscles • It can be thought of as ANGINA of the legs

Differential Diagnosis of Leg Pain (Other Potential Causes) • Spinal canal stenosis • Peripheral neuropathy • Peripheral nerve pain – Herniated disc impinging on sciatic nerve • Osteoarthritis of the hip or knee • Venous claudication • Symptomatic Baker’s cyst • Chronic compartment syndrome • Muscle spasms or cramps • Restless leg syndrome Also see Table 3 of Hirsch AT, et al. J Am Coll Cardiol. 2006; 47: e 1 -e 192.
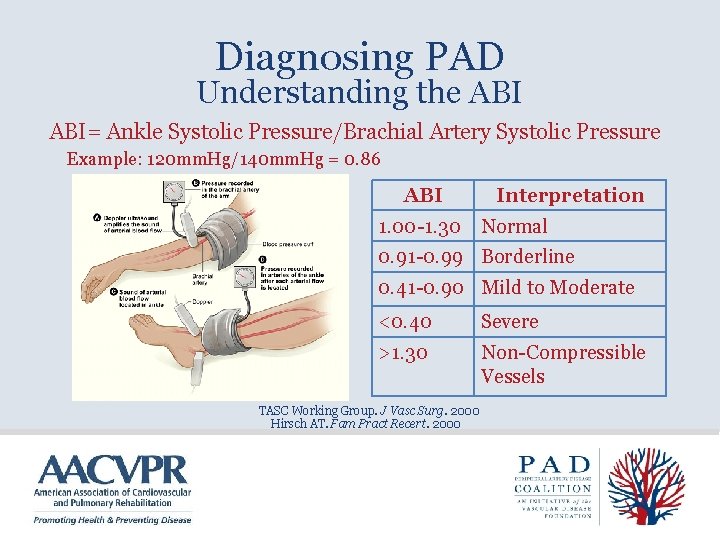
Diagnosing PAD Understanding the ABI= Ankle Systolic Pressure/Brachial Artery Systolic Pressure Example: 120 mm. Hg/140 mm. Hg = 0. 86 ABI Interpretation 1. 00 -1. 30 Normal 0. 91 -0. 99 Borderline 0. 41 -0. 90 Mild to Moderate <0. 40 Severe >1. 30 Non-Compressible Vessels TASC Working Group. J Vasc Surg. 2000 Hirsch AT. Fam Pract Recert. 2000

The Cycle of Disability in Intermittent Claudication peripheral artery disease Reduced oxygen Endothelial dysfunction Ischemic Reperfusion Systematic inflammation Free radical generation Muscle fiber denervation Muscle fiber atrophy Altered myosin heavy chain expression Deconditioning and worsening: Obesity, Hypertension Hyperlipidemia Hyperglycemia Thrombotic risk Altered muscle metabolism Acylcarnitine accumulation Altered electron transport Impaired walking ability Decreased quality of life Poor aerobic capacity Reduced muscle strength and endurance
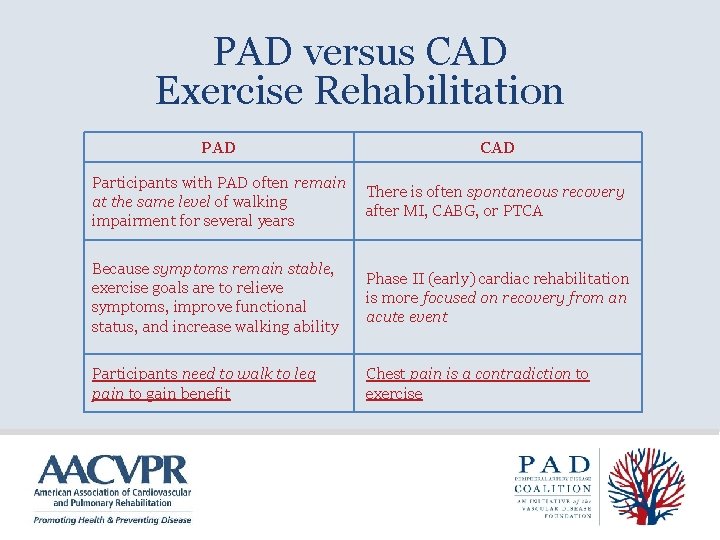
PAD versus CAD Exercise Rehabilitation PAD CAD Participants with PAD often remain at the same level of walking impairment for several years There is often spontaneous recovery after MI, CABG, or PTCA Because symptoms remain stable, exercise goals are to relieve symptoms, improve functional status, and increase walking ability Phase II (early) cardiac rehabilitation is more focused on recovery from an acute event Participants need to walk to leg pain to gain benefit Chest pain is a contradiction to exercise
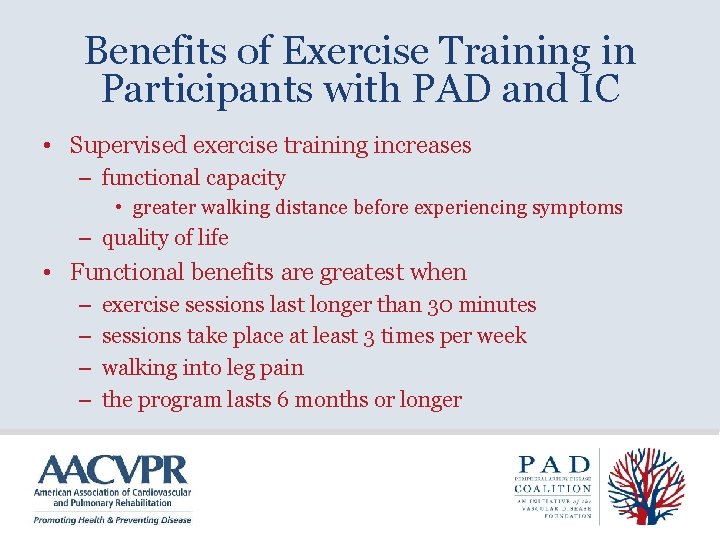
Benefits of Exercise Training in Participants with PAD and IC • Supervised exercise training increases – functional capacity • greater walking distance before experiencing symptoms – quality of life • Functional benefits are greatest when – – exercise sessions last longer than 30 minutes sessions take place at least 3 times per week walking into leg pain the program lasts 6 months or longer
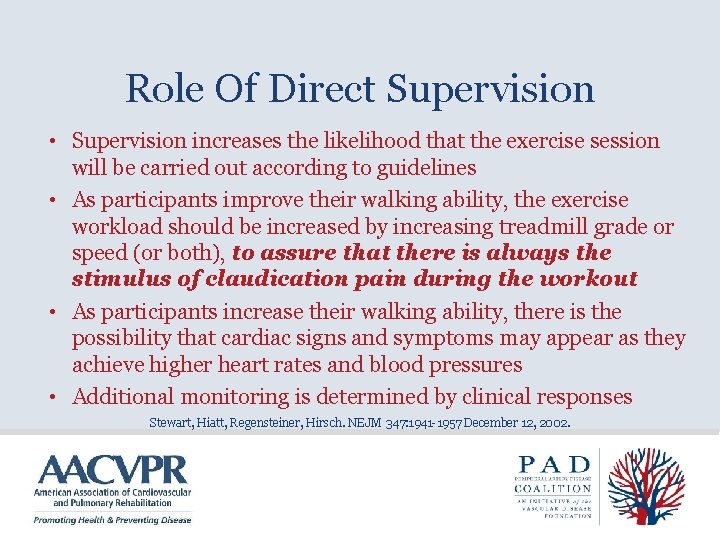
Role Of Direct Supervision • Supervision increases the likelihood that the exercise session will be carried out according to guidelines • As participants improve their walking ability, the exercise workload should be increased by increasing treadmill grade or speed (or both), to assure that there is always the stimulus of claudication pain during the workout • As participants increase their walking ability, there is the possibility that cardiac signs and symptoms may appear as they achieve higher heart rates and blood pressures • Additional monitoring is determined by clinical responses Stewart, Hiatt, Regensteiner, Hirsch. NEJM 347: 1941 -1957 December 12, 2002.

Potential Mechanisms for Exercise-Induced Improvements • Improved oxygen extraction and utilization by exercising muscle • Improved endothelial function • Improved blood rheology • Improved gait and walking economy • Increased tolerance to pain • Possibly increased blood supply
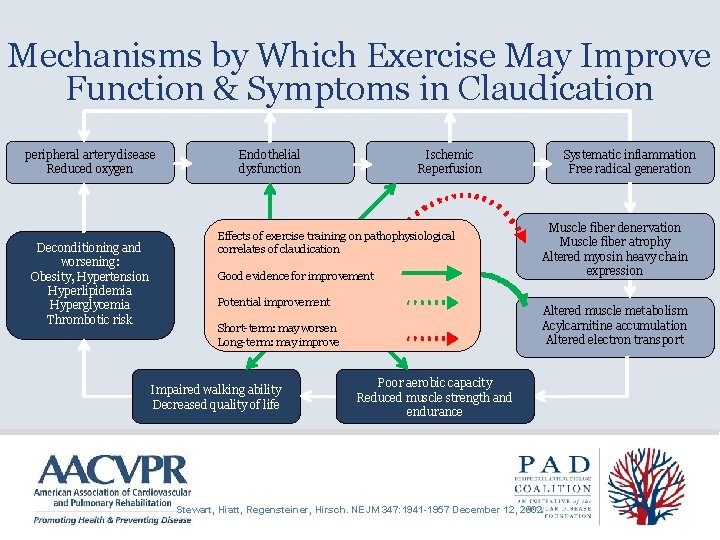
Mechanisms by Which Exercise May Improve Function & Symptoms in Claudication peripheral artery disease Reduced oxygen Deconditioning and worsening: Obesity, Hypertension Hyperlipidemia Hyperglycemia Thrombotic risk Endothelial dysfunction Ischemic Reperfusion Effects of exercise training on pathophysiological correlates of claudication Good evidence for improvement Potential improvement Muscle fiber denervation Muscle fiber atrophy Altered myosin heavy chain expression Altered muscle metabolism Acylcarnitine accumulation Altered electron transport Short-term: may worsen Long-term: may improve Impaired walking ability Decreased quality of life Systematic inflammation Free radical generation Poor aerobic capacity Reduced muscle strength and endurance Stewart, Hiatt, Regensteiner, Hirsch. NEJM 347: 1941 -1957 December 12, 2002.

Goals of Medical Evaluation Before Exercise Rehabilitation • To confirm diagnosis of PAD and IC • To confirm absence of – – – Critical limb ischemia Unstable angina Decompensated heart failure Uncontrolled cardiac arrhythmias Severe or symptomatic valvular disease Other conditions that could be aggravated by exercise including, but not limited to, severe joint disease, uncontrolled diabetes, or uncontrolled hypertension • To screen for exercise-induced myocardial ischemia & arrhythmias – Exercise stress testing is preferred – Careful questioning for symptoms is an alternative
Pre-Exercise Functional Evaluation • May be either – Formal treadmill testing protocols – Observation during initial treadmill exercise session • Goal is to determine – Claudication threshold – Cardiovascular response to exercise – Establish parameters for the exercise prescription

Use of a Pain Scale in PAD Exercise Rehabilitation 1 No Pain 2 Onset of Pain 3 Mild Pain 4 Moderate 5 Severe

PAD Exercise Guidelines • Warm-up and cool-down: 5 minutes each • Mode: Treadmill walking • Intensity: Walk to claudication pain (3 -4 of 5 on the scale), maintain for 8 -10 min. Increase speed or grade when pain becomes less than moderate. • Duration: Initially, accumulate 35 min of walking in bouts of 8 -10 min each. Rest between bouts until pain subsides. Progress to 50 min, including 5 minutes warm up and cool down. • Frequency: 3 -5 times/week • Total Time: At least 3 months Source; Regensteiner and Hiatt: ACSM Resource Manual 2001.

Specifics About Exercise Prescription • The initial training intensity is defined as the % inclination that brings on the onset of claudication pain (level 2 of 5 on the claudication scale), with the initial speed set at 2. 0 mph • During the initial exercise session – Participants walk to a mild to moderate pain level (3 -4 of 5 on the claudication scale) at the initial training intensity above, then – Stop and rest until the claudication pain has completely abated and then – Resume walking at the initial training intensity again
Goals of the Initial Training Sessions • For the participant to understand the claudication scale, foot care, and purpose of exercise training • To teach warm up and cool down principles • To accumulate 15 minutes or more of total exercise treadmill time, excluding warm up and cool down

Goal of Subsequent Exercise Sessions • Cumulative exercise session of 50 minutes (including rest periods) • Advance speed and inclination over time to maintain a claudication stimulus to exercise training • Warm-up and cool-down periods of 5 minutes each • Total of 60 minutes per session
Progression of the Exercise Training Intensity • Should occur during the session after the participant can exercise for – at least 8 minutes without stopping for 3 -4/5 claudication pain – cumulative exercise duration of 50 minutes including rest periods • Increase inclination by 1 -2% maintain the same speed (2. 0 mph)
General Guidelines for Progression of Exercise Training Intensity During Rehabilitation • Continue to increase inclination as tolerated in subsequent sessions until reach 10% at 2. 0 mph • Then increase speed by 0. 1 to 0. 2 mph at 10% with goal to achieve more than 8 minutes before rest is needed for claudication pain (3 -4/5) • When reach 3. 0 mph/10% inclination, then increase inclination by 1 -2%, up to 15% • Final step is to increase speed by 0. 1 to 0. 2 mph increments as tolerated
Case Study: History & Clinical Profile • • 70 year old white female Wt: 180 lbs. Ht: 62” BMI = 32. 9 Current smoker: 1/2 pack per day Hyperlipidemia, hypertension Cardiac History: CABG January, 2004, and NSTEMI June, 2006
Case Study: History & Clinical Profile • Pertinent medical hx: Bilateral PAD • Current meds: cilostazol, lisinopril, furosemide, simvastatin, clopidogrel, aspirin • Resting BP: 128/46; RHR: 64 • Resting ECG: Non-specific ST-T wave ‘s

Case Study: History & Clinical Profile Exercise Test Results • Onset of leg pain @ 2. 0 mph / 7% grade • Maximal pain @ 2. 0 mph / 10. 5% grade • Normal BP & HR response • No complaints of angina • Stress ECG: No changes

Case Study: Exercise Training Scenarios • What is the beginning exercise prescription?
Case Study: Exercise Training Scenarios • What is the beginning exercise prescription? • Treadmill walking at 2 mph / 7% grade • Walk to moderate pain (3 or 4 on scale)
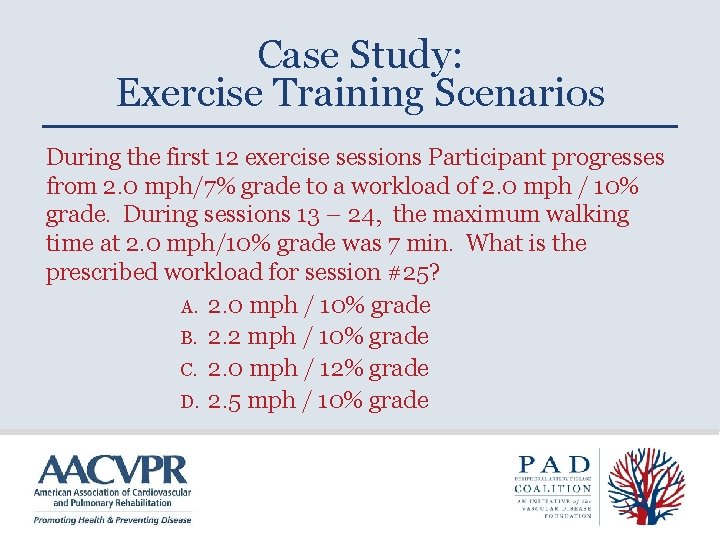
Case Study: Exercise Training Scenarios During the first 12 exercise sessions Participant progresses from 2. 0 mph/7% grade to a workload of 2. 0 mph / 10% grade. During sessions 13 – 24, the maximum walking time at 2. 0 mph/10% grade was 7 min. What is the prescribed workload for session #25? A. 2. 0 mph / 10% grade B. 2. 2 mph / 10% grade C. 2. 0 mph / 12% grade D. 2. 5 mph / 10% grade
Case Study: Exercise Training Scenarios During the first 12 exercise sessions Participant progresses from 2. 0 mph/7% grade to a workload of 2. 0 mph / 10% grade. During sessions 13 – 24, the maximum walking time at 2. 0 mph/10% grade was 7 min. What is the prescribed workload for session #25? A. 2. 0 mph / 10% grade B. 2. 2 mph / 10% grade C. 2. 0 mph / 12% grade D. 2. 5 mph / 10% grade
Other Program Considerations • Treadmill or other walking exercise is the cornerstone. – If possible it should be used during each exercise session • Other forms of exercise can also be added for cardiovascular health but have not been shown to improve claudication symptoms • Invite participants to join your facility’s CV risk factor education sessions

Interventional Treatment • Surgical or percutaneous intervention is recommended to treat: – ischemic rest pain – tissue loss – vocational limiting claudication • Further information is available at – http: //www. padcoalition. org/resources/slides. php – http: //www. acc. org/qualityandscience/clinical/pdfs/05%20 Treatment %20 -20 Revascularization%20 for%20 Individual%20 with%20 PAD%20%20 the%20 Symptomatic%20 Leg. PPT

Post Interventional Considerations • Avoid compression garments if ABI<0. 8 • If stents, avoid extended squatting or exercises that may compress the stent • Avoid walking if plantar foot wound • Observe for recurrent symptoms and notify health care provider if these occur • Stress importance of excellent foot care

Assessing Participant Outcomes and Program Effectiveness • • • Treadmill Testing Six Minute Walk Test Shuttle Walk Test Four Meter Walking Velocity Repeated Chair Rise Standing Balance Quality of Life Questionnaire Program Demographics Attendance
Marketing Considerations • Surgeons are generally aware of the benefits of exercise training for IC but do not think about or know how to refer participants to programs • Medical physicians are not always aware of benefits of exercise for these patients • Clinical practice guidelines stress discussion of supervised exercise training with patients with IC • Capture this marketing opportunity!

Keys to Successful Programs • Efficient use of staff and equipment • Build on successful existing programs • Feasible business plan with enthusiastic support by administration • Effective communication with referring physicians • Awareness that successful marketing depends on every team member
PAD Coalition www. vasculardisease. org/PADcoalition/ AACVPR www. aacvpr. org/
- Slides: 39