Pacing in Bardyarrhythmia Indications for Pacing Main Reference
Pacing in Bardyarrhythmia
Indications for Pacing � Main Reference ◦ ACC/AHA/HRS 2008 Guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the ACC/AHA/NASPE 2002 Guideline Update for Implantation of Cardiac Pacemakers and Antiarrhythmia Devices): developed in collaboration with the American Association for Thoracic Surgery and Society of Thoracic Surgeons. �Circulation. 2008 May 27; 117(21): e 350 -408.
Indications for Permanent pacing in Aquired Atrioventricular Block � Complete (3 rd degree AV block) ◦ Complete A V dissociation, regular R waves, Atrium>Ventricle � Second degree AV block ◦ Mobitz I (Wenckebach) �Progressive increase in PR interval before block �Shortening of RR intervals P-P equal (*ventricular phasic dysrhythmia) ◦ Mobitz II �Fixed PR interval before and after block, can be high grade (≥ 2 non-conducted P waves) or 2: 1. � First degree AV block ◦ PR interval >200 ms
Permanent pacing is Indicated in Aquired Atrioventricular Block � Third degree or second degree block: ◦ Class 1 indication for pacing if: �Bradycardia associated with symptoms �Need for drug therapy resulting in symptomatic bradycardia �Asymptomatic with pause >3. 0 s or escape <40 bpm or broad complex escape (below level of AV node) �Asymptomatic with AF and pause >5. 0 secs �Asymptomatic but associated neuromuscular disease �Block occurring during exercise regardless of presence of ischaemia.
Permanent pacing is Reasonable in Aquired Atrioventricular Block � Class IIa recommendations ◦ Asymptomatic adults, resting rate >40 bpm and without structural heart disease. ◦ Asymptomatic adults with level of block discovered below the AV node at electrophysiological study ◦ Symptoms of pacemaker syndrome ◦ Asymptomatic type II AV block with narrow QRS (note wide QRS makes this class I indication)
Permanent pacing is Not Indicated in Aquired Atrioventricular Block � Pacing is not indicated or is harmful for the following: ◦ Asymptomatic 1 st degree heart block ◦ Asymptomatic Mobitz type 1 Wenckebach ◦ Transient or unlikely to recur, during episodes of hypoxia in the sleep apnoea syndromes.
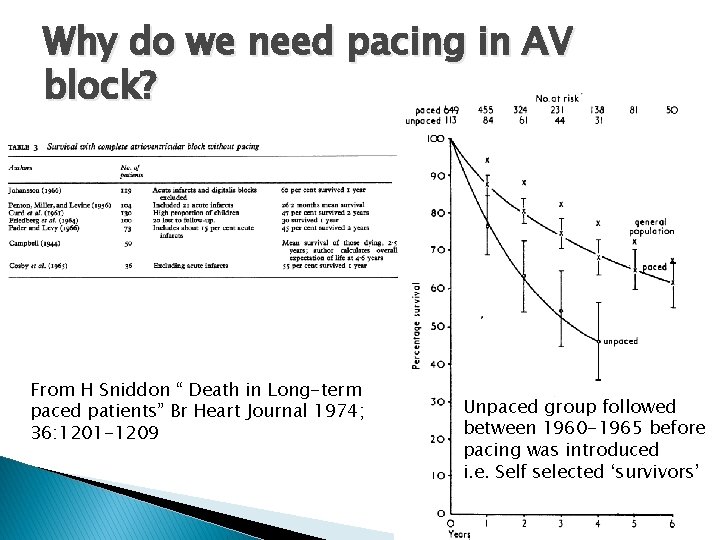
Why do we need pacing in AV block? From H Sniddon “ Death in Long-term paced patients” Br Heart Journal 1974; 36: 1201 -1209 Unpaced group followed between 1960 -1965 before pacing was introduced i. e. Self selected ‘survivors’
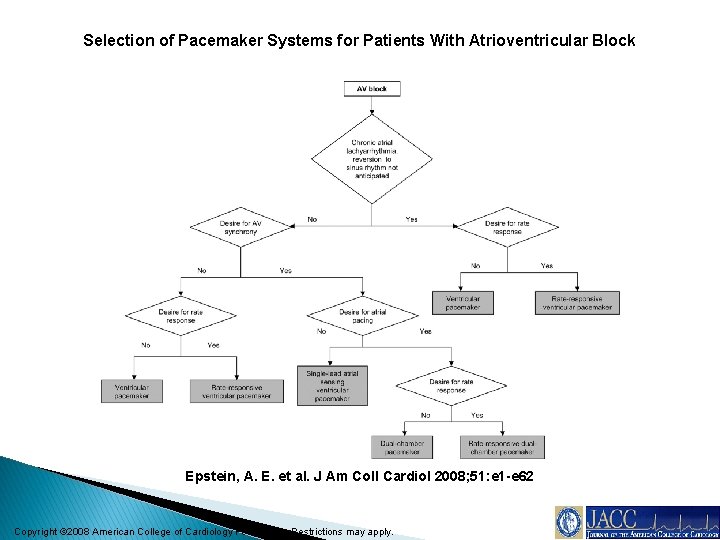
Selection of Pacemaker Systems for Patients With Atrioventricular Block Epstein, A. E. et al. J Am Coll Cardiol 2008; 51: e 1 -e 62 Copyright © 2008 American College of Cardiology Foundation. Restrictions may apply.
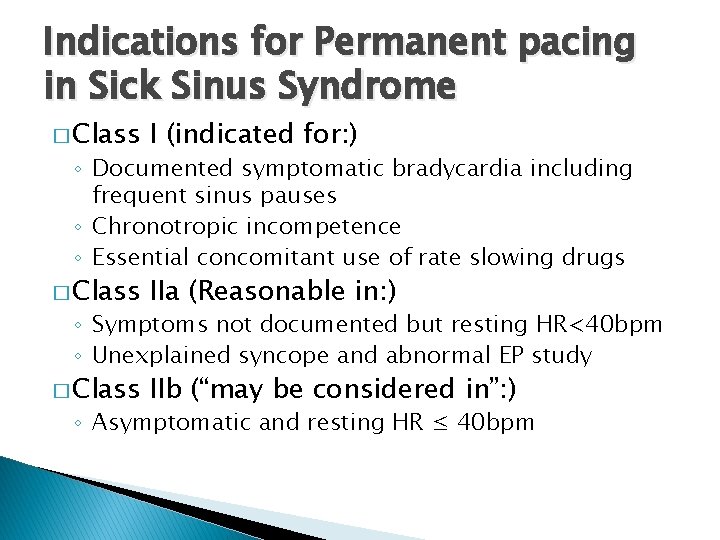
Indications for Permanent pacing in Sick Sinus Syndrome � Class I (indicated for: ) � Class IIa (Reasonable in: ) � Class IIb (“may be considered in”: ) ◦ Documented symptomatic bradycardia including frequent sinus pauses ◦ Chronotropic incompetence ◦ Essential concomitant use of rate slowing drugs ◦ Symptoms not documented but resting HR<40 bpm ◦ Unexplained syncope and abnormal EP study ◦ Asymptomatic and resting HR ≤ 40 bpm
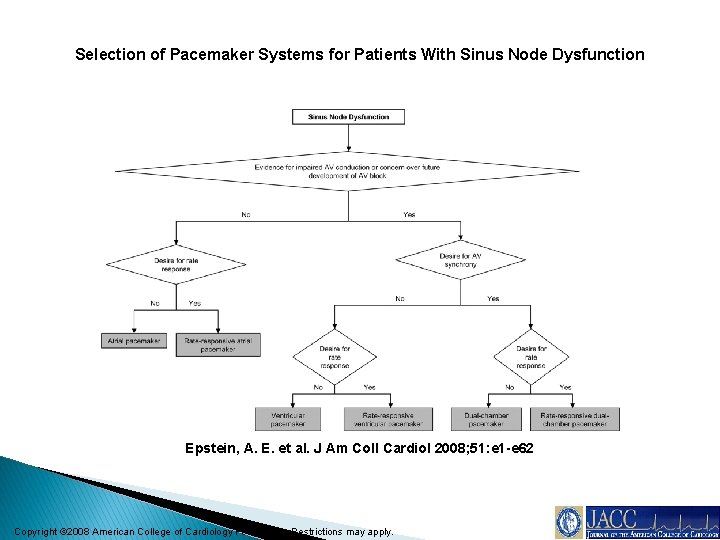
Selection of Pacemaker Systems for Patients With Sinus Node Dysfunction Epstein, A. E. et al. J Am Coll Cardiol 2008; 51: e 1 -e 62 Copyright © 2008 American College of Cardiology Foundation. Restrictions may apply.
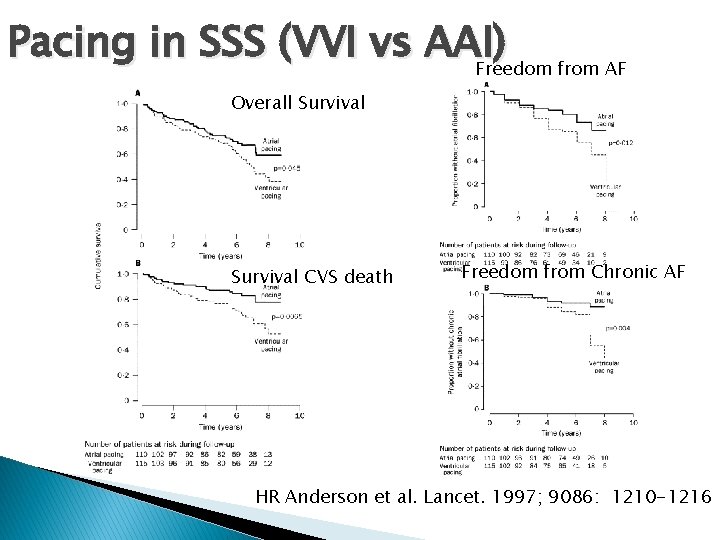
Pacing in SSS (VVI vs AAI) Freedom from AF Overall Survival CVS death Freedom from Chronic AF HR Anderson et al. Lancet. 1997; 9086: 1210 -1216
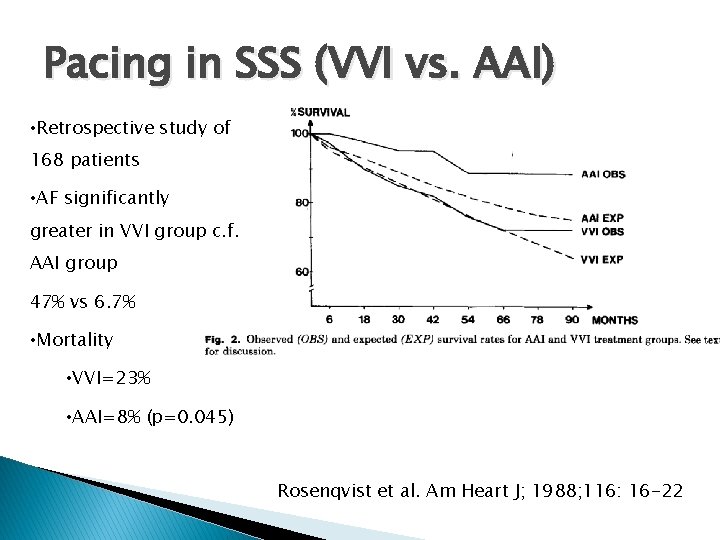
Pacing in SSS (VVI vs. AAI) • Retrospective study of 168 patients • AF significantly greater in VVI group c. f. AAI group 47% vs 6. 7% • Mortality • VVI=23% • AAI=8% (p=0. 045) Rosenqvist et al. Am Heart J; 1988; 116: 16 -22

Pacing in SSS (DDD vs. VVI) RCT of 2010 pts with SSS 1014 DDD 996 VVI AF developed in: VVI 27. 1% DDD 21. 4% (p=0. 004) Note still high rate of AF with V pacing in either arm Lamas et al. NEJM 2002; 346: 1854

Pacing in SSS (MVP vs. DDD) Comparison of minimal ventricular pacing (MVP) and conventional DDD. RCT of 1065 patients MVP 530 DDD 535 Primary endpoint time to Afib (trial stopped early as endpoint met) AF MVP: 7. 9% DDD: 12. 7% (p=0. 004) HR 0. 6 (0. 41 -0. 88) Sweeny et al. NEJM. 2007; 357: 1000 -8
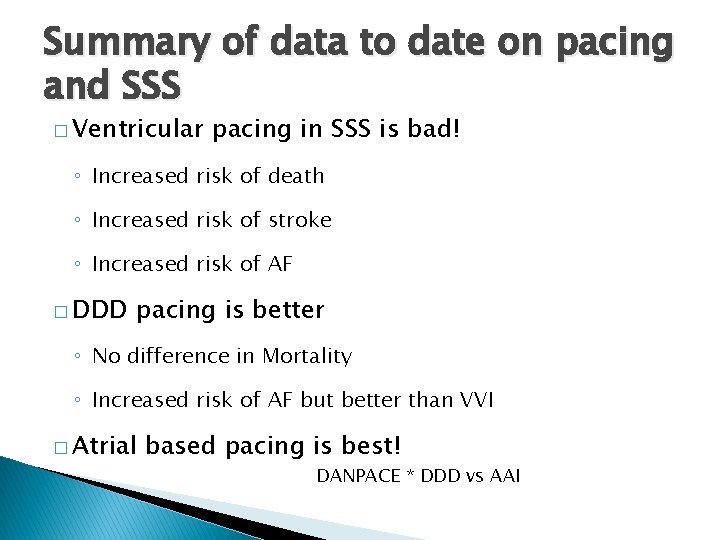
Summary of data to date on pacing and SSS � Ventricular pacing in SSS is bad! ◦ Increased risk of death ◦ Increased risk of stroke ◦ Increased risk of AF � DDD pacing is better ◦ No difference in Mortality ◦ Increased risk of AF but better than VVI � Atrial based pacing is best! DANPACE * DDD vs AAI

Pacing in Hypersentive Carotid Syndrome and Neurocardiogenic Syncope � Class IIa � Class IIb � Class III (Not-indicated) ◦ Syncope with clear carotid events and CSM producing pause >3 secs ◦ Syncope with CSM >3 secs ◦ ‘Significantly’ symptomatic neurocardiogenic syncope associated with documented bradycardia spontaneously or at Tilt table ◦ Positive CSM in absence of symptoms Situational vasovagal syncope
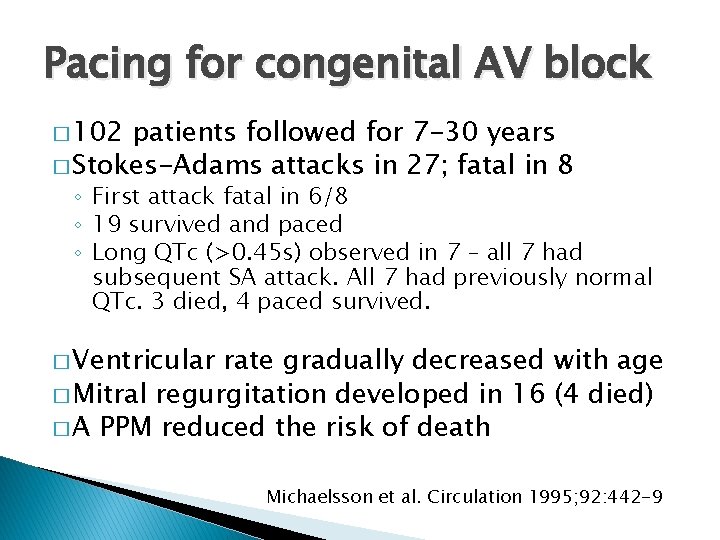
Pacing for congenital AV block � 102 patients followed for 7 -30 years � Stokes-Adams attacks in 27; fatal in 8 ◦ First attack fatal in 6/8 ◦ 19 survived and paced ◦ Long QTc (>0. 45 s) observed in 7 – all 7 had subsequent SA attack. All 7 had previously normal QTc. 3 died, 4 paced survived. � Ventricular rate gradually decreased with age � Mitral regurgitation developed in 16 (4 died) � A PPM reduced the risk of death Michaelsson et al. Circulation 1995; 92: 442 -9
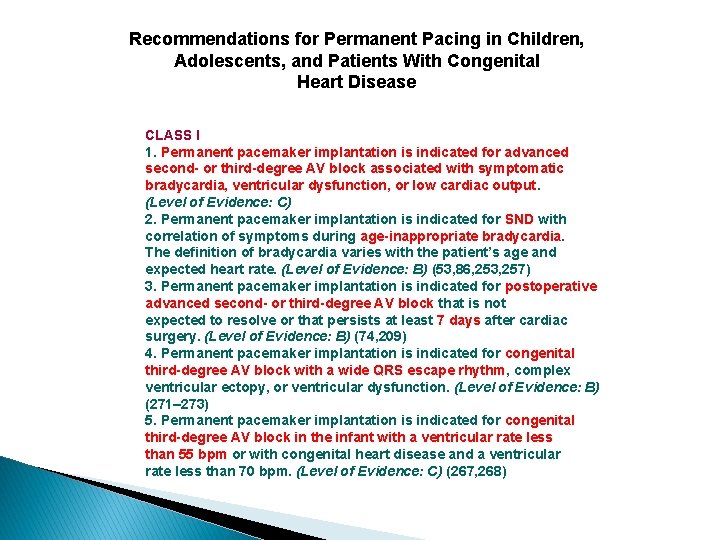
Recommendations for Permanent Pacing in Children, Adolescents, and Patients With Congenital Heart Disease CLASS I 1. Permanent pacemaker implantation is indicated for advanced second- or third-degree AV block associated with symptomatic bradycardia, ventricular dysfunction, or low cardiac output. (Level of Evidence: C) 2. Permanent pacemaker implantation is indicated for SND with correlation of symptoms during age-inappropriate bradycardia. The definition of bradycardia varies with the patient’s age and expected heart rate. (Level of Evidence: B) (53, 86, 253, 257) 3. Permanent pacemaker implantation is indicated for postoperative advanced second- or third-degree AV block that is not expected to resolve or that persists at least 7 days after cardiac surgery. (Level of Evidence: B) (74, 209) 4. Permanent pacemaker implantation is indicated for congenital third-degree AV block with a wide QRS escape rhythm, complex ventricular ectopy, or ventricular dysfunction. (Level of Evidence: B) (271– 273) 5. Permanent pacemaker implantation is indicated for congenital third-degree AV block in the infant with a ventricular rate less than 55 bpm or with congenital heart disease and a ventricular rate less than 70 bpm. (Level of Evidence: C) (267, 268)
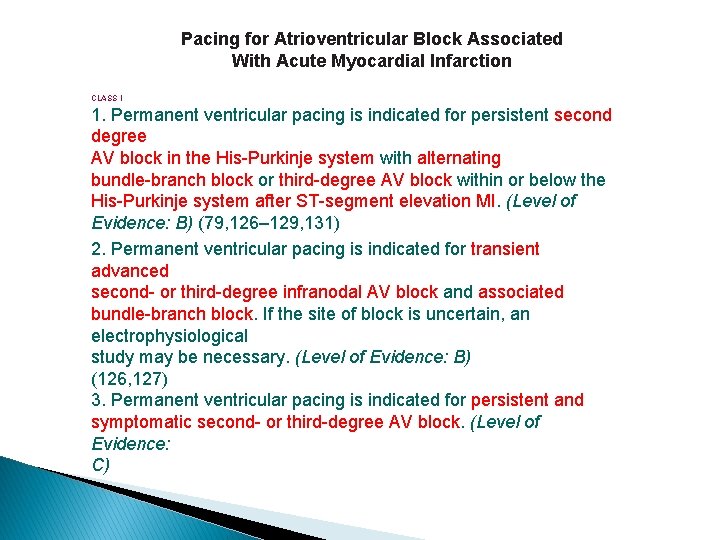
Pacing for Atrioventricular Block Associated With Acute Myocardial Infarction CLASS I 1. Permanent ventricular pacing is indicated for persistent second degree AV block in the His-Purkinje system with alternating bundle-branch block or third-degree AV block within or below the His-Purkinje system after ST-segment elevation MI. (Level of Evidence: B) (79, 126– 129, 131) 2. Permanent ventricular pacing is indicated for transient advanced second- or third-degree infranodal AV block and associated bundle-branch block. If the site of block is uncertain, an electrophysiological study may be necessary. (Level of Evidence: B) (126, 127) 3. Permanent ventricular pacing is indicated for persistent and symptomatic second- or third-degree AV block. (Level of Evidence: C)
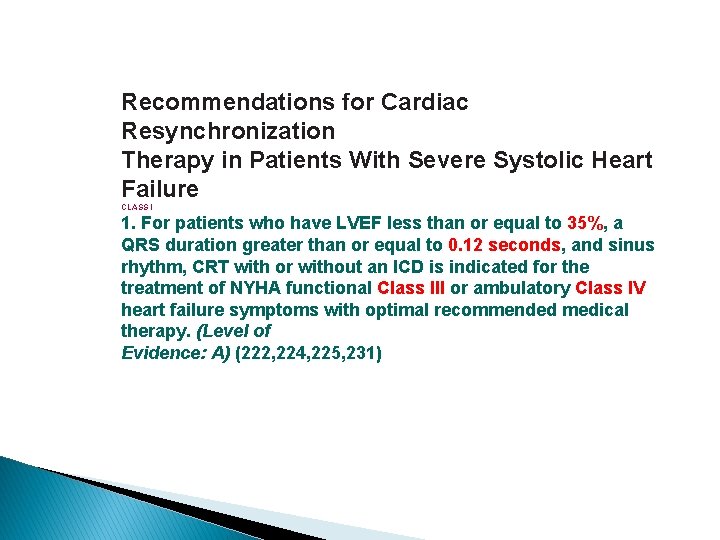
Recommendations for Cardiac Resynchronization Therapy in Patients With Severe Systolic Heart Failure CLASS I 1. For patients who have LVEF less than or equal to 35%, a QRS duration greater than or equal to 0. 12 seconds, and sinus rhythm, CRT with or without an ICD is indicated for the treatment of NYHA functional Class III or ambulatory Class IV heart failure symptoms with optimal recommended medical therapy. (Level of Evidence: A) (222, 224, 225, 231)
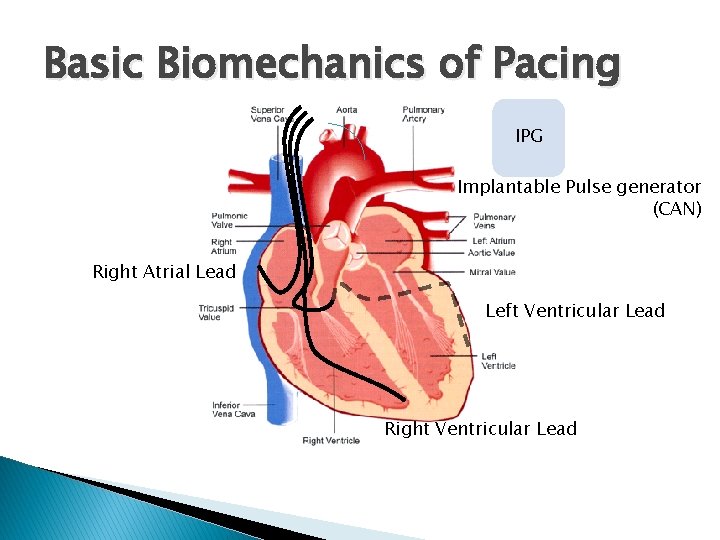
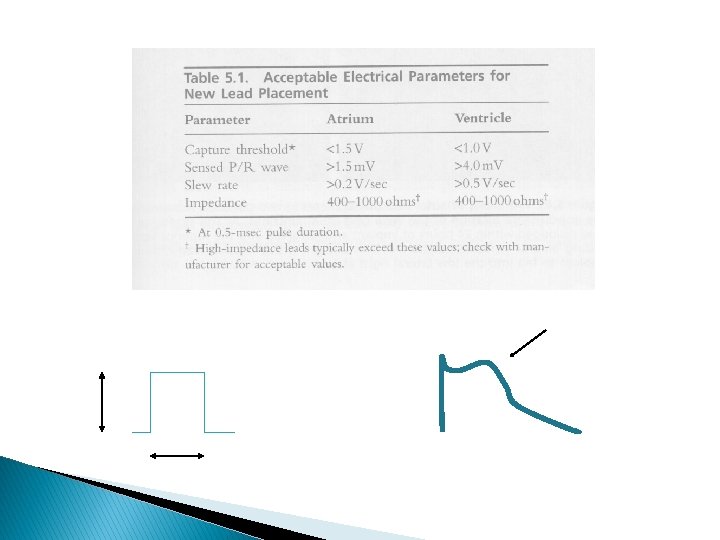
Basic Biomechanics of Pacing IPG Implantable Pulse generator (CAN) Right Atrial Lead Left Ventricular Lead Right Ventricular Lead
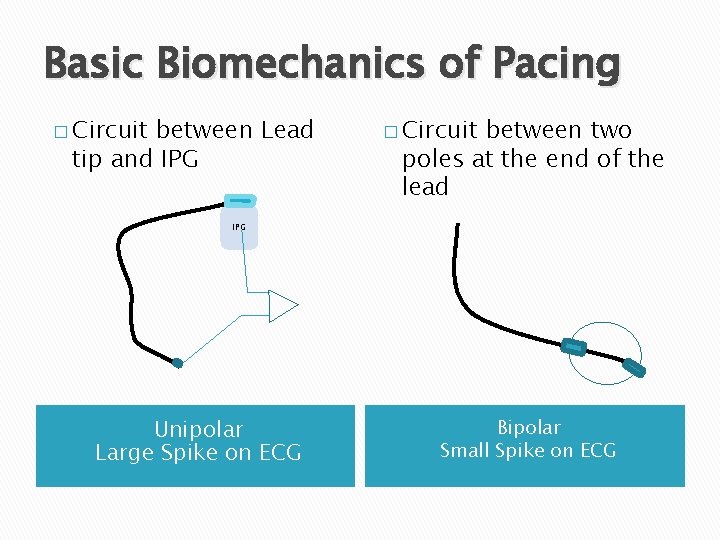
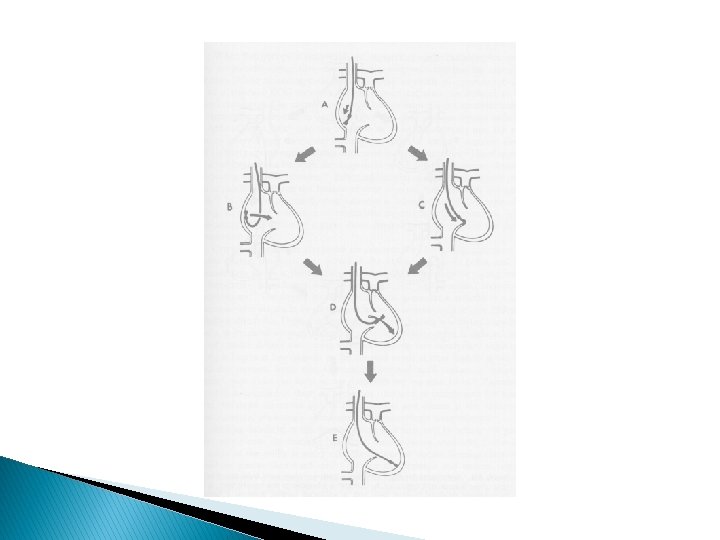
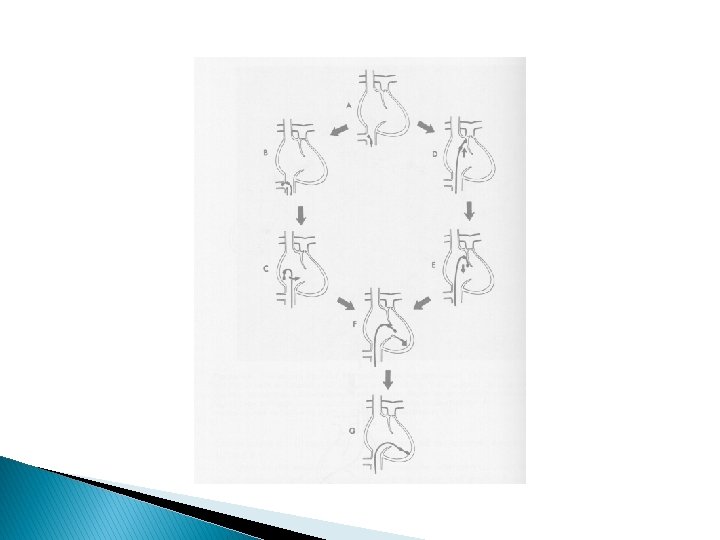
Basic Biomechanics of Pacing � Circuit between Lead tip and IPG � Circuit between two poles at the end of the lead IPG Unipolar Large Spike on ECG Bipolar Small Spike on ECG
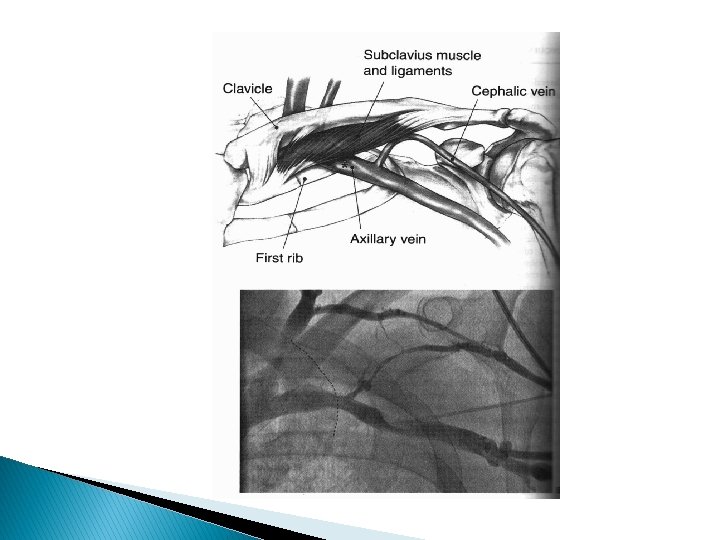
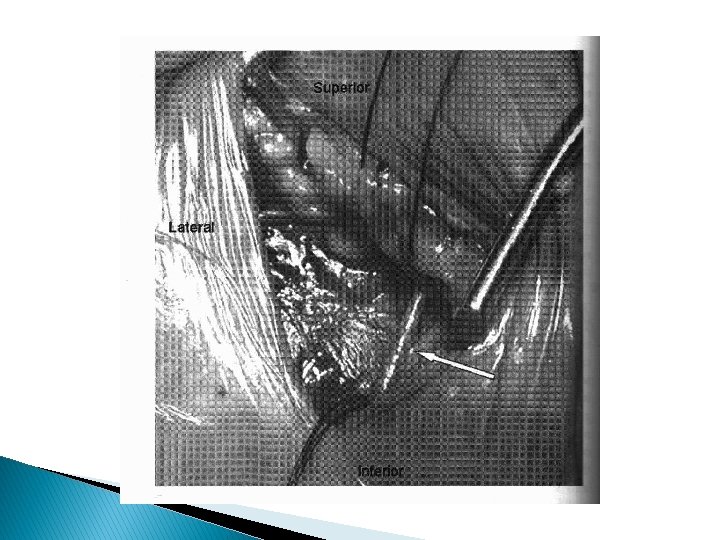
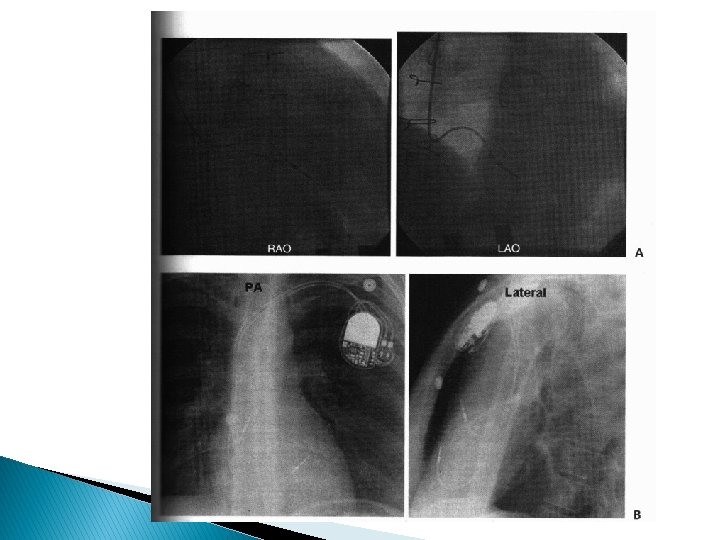
RV Lead Placement Septal and Apical
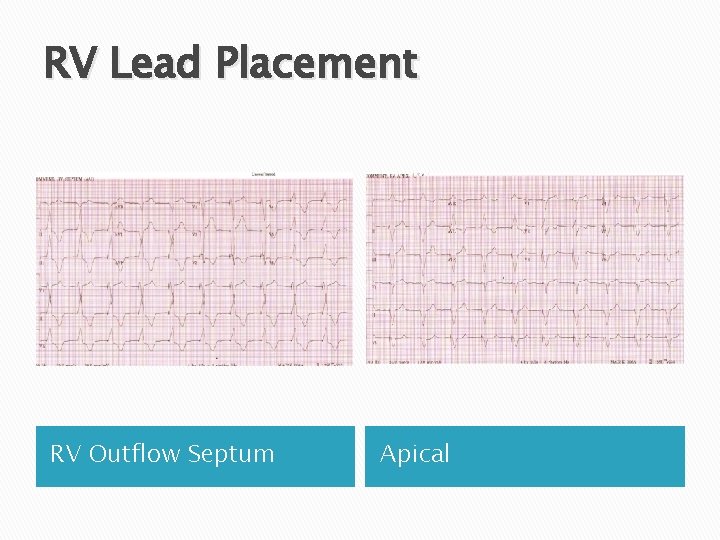
RV Lead Placement RV Outflow Septum Apical

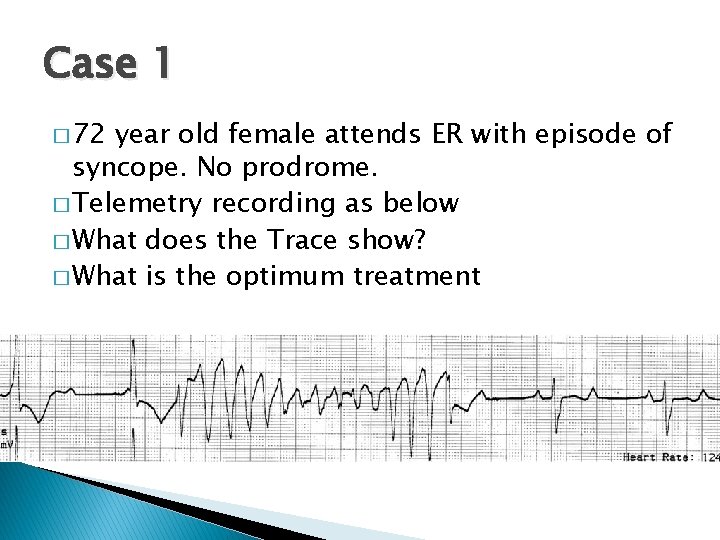
Case 1 � 72 year old female attends ER with episode of syncope. No prodrome. � Telemetry recording as below � What does the Trace show? � What is the optimum treatment
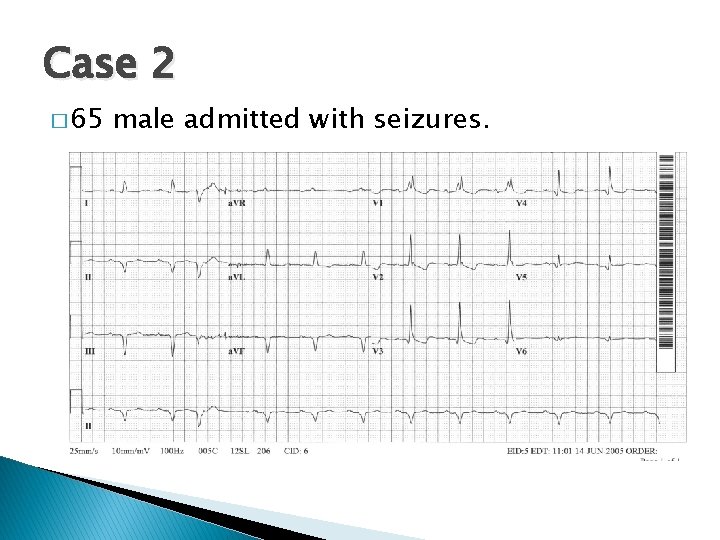
Case 2 � 65 male admitted with seizures.
Case 2
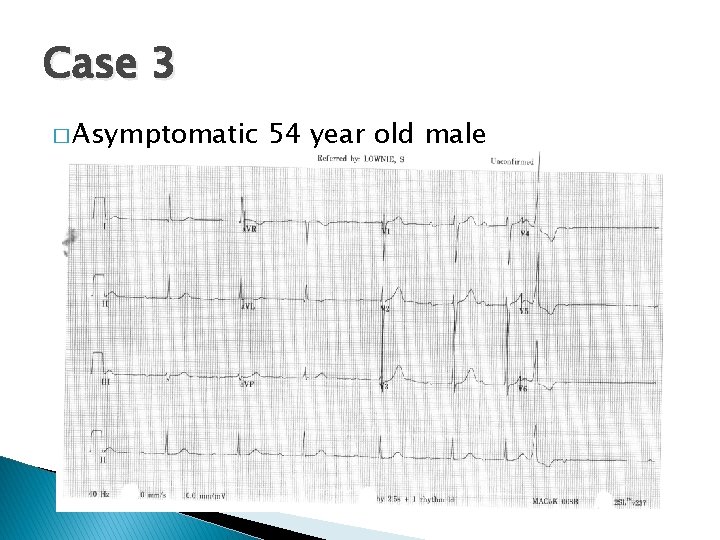
Case 3 � Asymptomatic 54 year old male
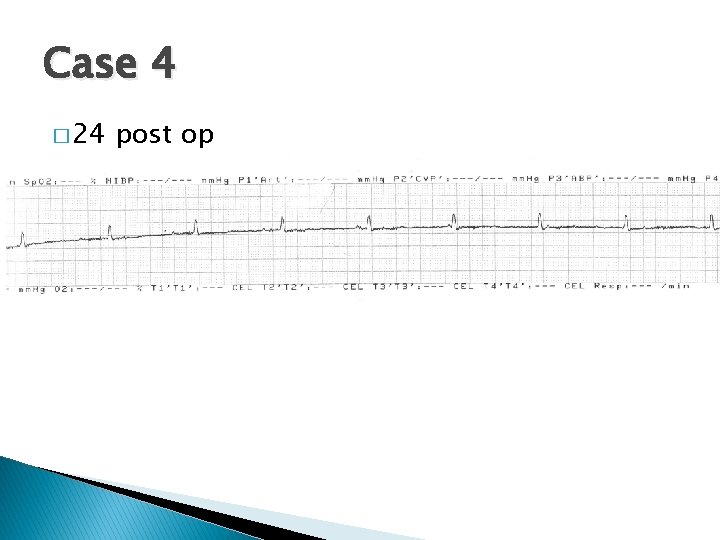
Case 4 � 24 post op
- Slides: 37