Pacemaker follow up and troubleshooting When the patient

Pacemaker follow up and troubleshooting
When the patient leaves the cath. lab with a permanent pacemaker what should I do?
Should I? A- Educate the patient. B- Document. C- Start follow up. D- Non of the above. E- All of the above.
• The arm. Phones: on the same side the • Cellular You may useas a cellular should nothold be lifted above phone; however, not cellular • The pacemaker sitedo should bethe kept clean and dry. phone on level the same as your pacemaker for side four weeks. • The shoulder patient may take a tub bath when you go or place it in your shirt pocket over the should beacareful not to but hit or rub the home • He after getting pacemaker, keep pacemaker. the insertion site. Avoid incision dry for. Magnets: at least two weeks. • Strong strong magnets. • dressing Instruct the patient not tofor "fiddle" or Examples are magnets used an MRI and • The should be changed every day using • Emphasize on the importance of follow up activity Wound care play with the pacemaker hand-held security wands. under your sterile gauze. • Strong Fields: and Avoid strong skin. • • Give him the. Electrical exact place time He must not use ointment on the incision site electrical fields. Examples are radio • avoid activities likesoheavy lifting, instructed to do by the • unless Provide him with a phone number transmitting towers, ham radios, doctor. and arc running, or contact sports. Do not liftdressing • Carefully inspect the incision with each welders. Also, avoid leaning over the open Follow up Concerns more than 5 kilograms for two weeks. hood of a running car because its electrical change tocan note any or Iffield you have anyredness, specific questions interfere with your pacemaker. • Microwave Ovens: ask You your may cook with a regarding activity, doctor. discharge. Educate The patient swelling microwave oven. Microwave ovens in good • It is best to take it easy for working order are safe to use. four weeks at home to avoid damaging the pacemaker.
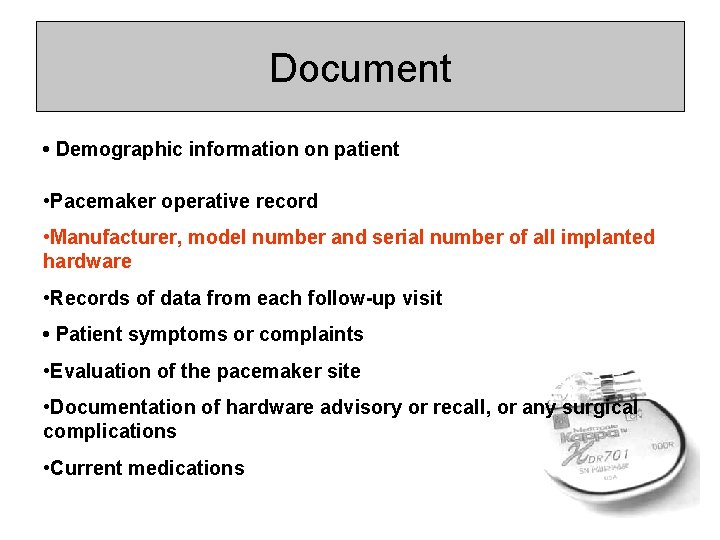
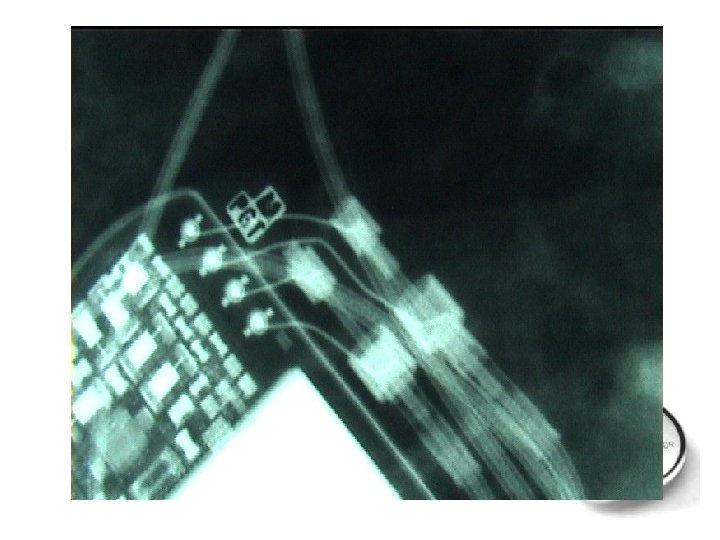
Document • Demographic information on patient • Pacemaker operative record • Manufacturer, model number and serial number of all implanted hardware • Records of data from each follow-up visit • Patient symptoms or complaints • Evaluation of the pacemaker site • Documentation of hardware advisory or recall, or any surgical complications • Current medications
What is the aim of the follow up visits? 1 - patient and family education. 2 - Collect and maintain patient records and institutional databases. 3 - Optimize pacing system function including maximizing power source utilization. 4 - detect and correct pacemaker system abnormalities. 5 - Act as a resource centre for cardiac pacing (RESERCH AND TRAINING)
Frequency Of Pacemaker Follow Up Postimplantation Two weeks 12 weeks Six months Maintenance period Intensified follow up period
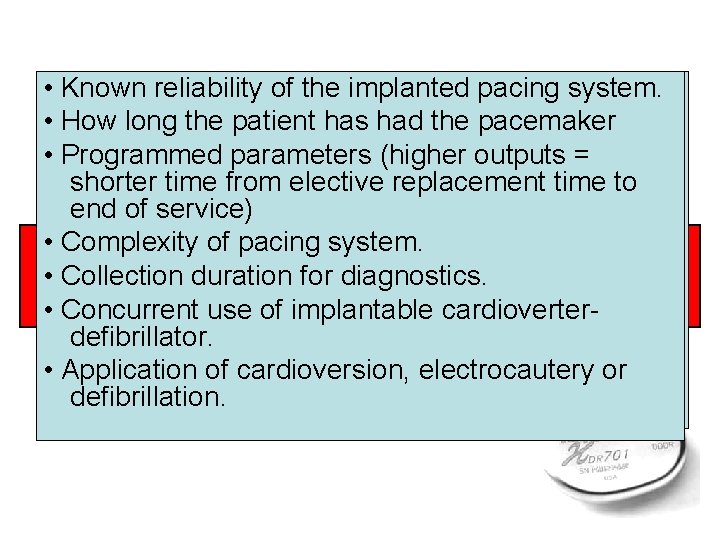
• • Known reliability of the implanted pacing system. Patient dependency on pacing. Considerations in determining a • How long the patient has had the pacemaker Stability of rhythm and(higher cardiovascular pacemaker follow-up schedule • • Programmed parameters outputs = symptoms. shorter time from elective replacement time to end of service) • High or unstable thresholds or low and • Complexity of pacing system. Patient-related Pacer system-related stable thresholds. • Collection duration for diagnostics. considerations • • Concurrent use of to implantable cardioverter. Patient’s ability report symptoms defibrillator. accurately. • Application of cardioversion, electrocautery or • Patient distance from follow-up clinic. defibrillation.
Troubleshooting
What troubles to shoot? Patient related problems 1 - pocket related problems. 2 - pacemaker syndrome. 3 - accessory muscle stimulation.

What troubles to shoot? Patient related problems Under passing or no pacing
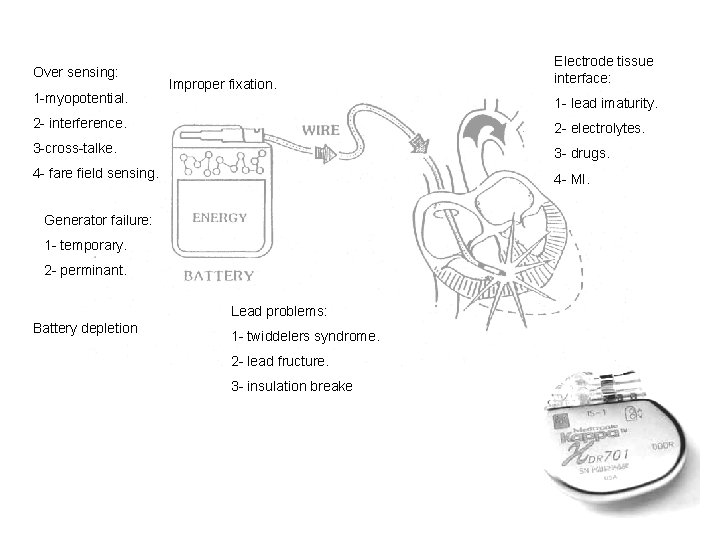
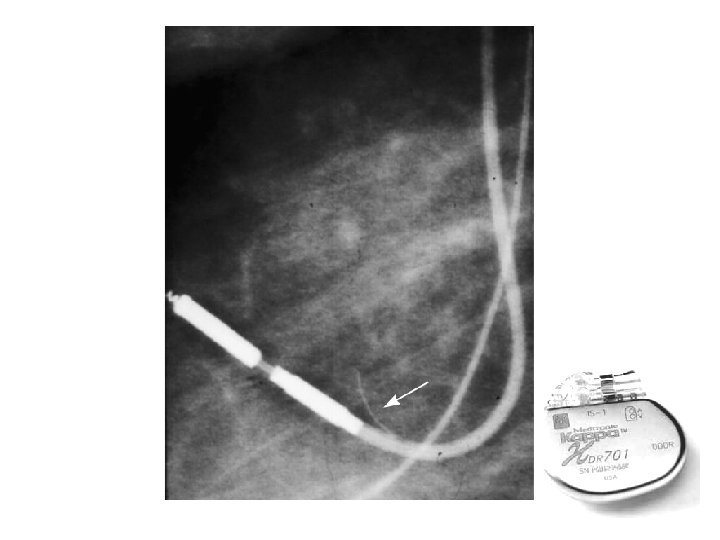
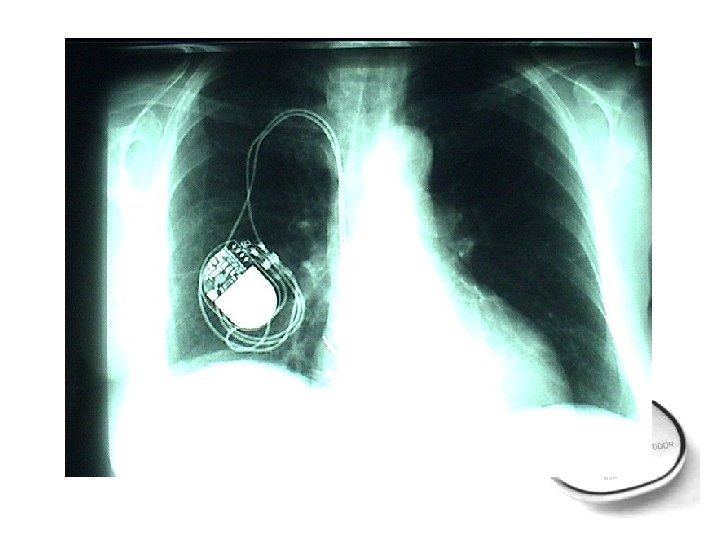
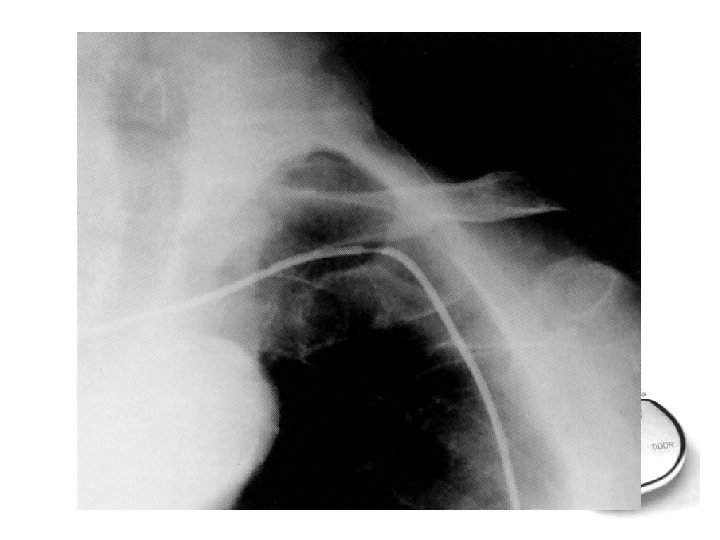
Over sensing: 1 -myopotential. Improper fixation. Electrode tissue interface: 1 - lead imaturity. 2 - interference. 2 - electrolytes. 3 -cross-talke. 3 - drugs. 4 - fare field sensing. 4 - MI. Generator failure: 1 - temporary. 2 - perminant. Lead problems: Battery depletion 1 - twiddelers syndrome. 2 - lead fructure. 3 - insulation breake
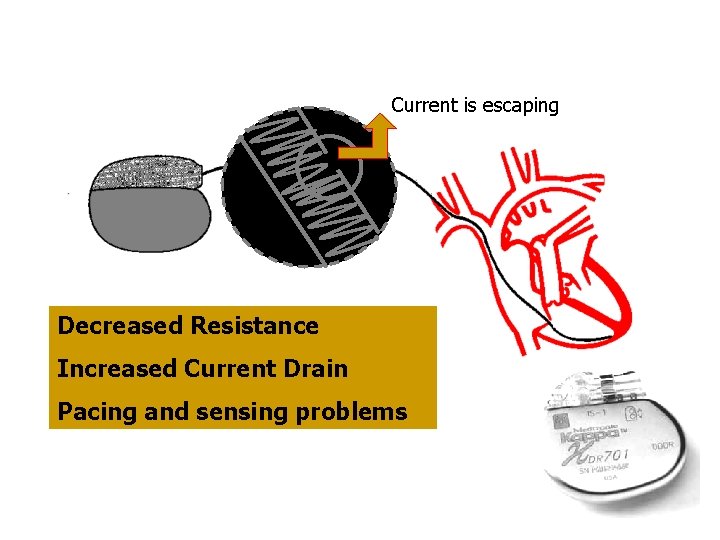
Current is escaping Decreased Resistance Increased Current Drain Pacing and sensing problems
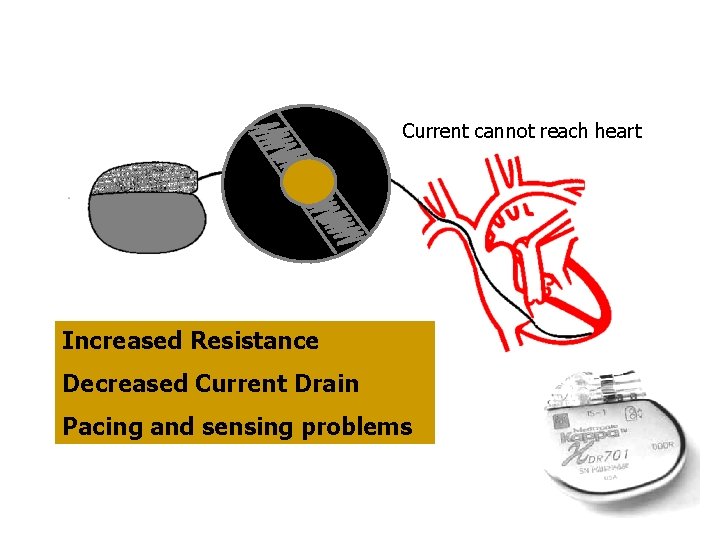
Current cannot reach heart Increased Resistance Decreased Current Drain Pacing and sensing problems
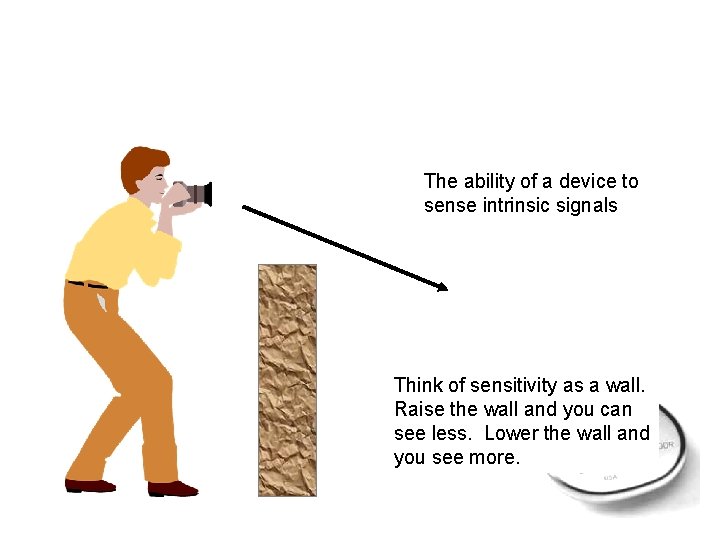
The ability of a device to sense intrinsic signals Think of sensitivity as a wall. Raise the wall and you can see less. Lower the wall and you see more.
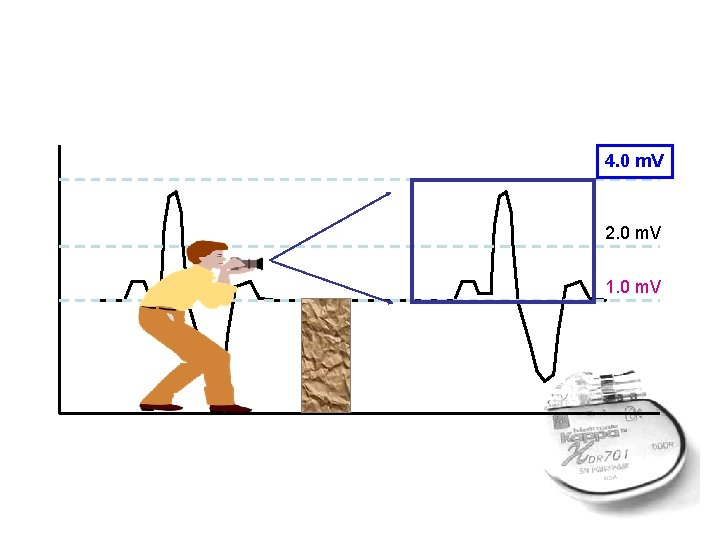
4. 0 m. V 2. 0 m. V 1. 0 m. V
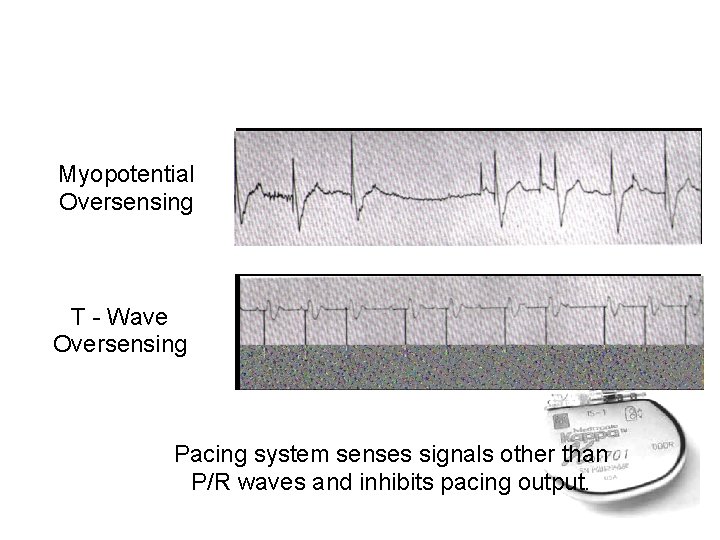
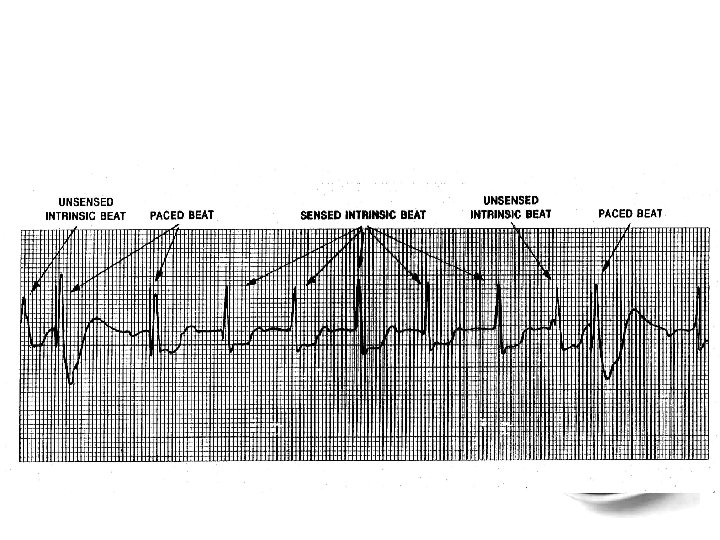
Myopotential Oversensing T - Wave Oversensing Pacing system senses signals other than P/R waves and inhibits pacing output.
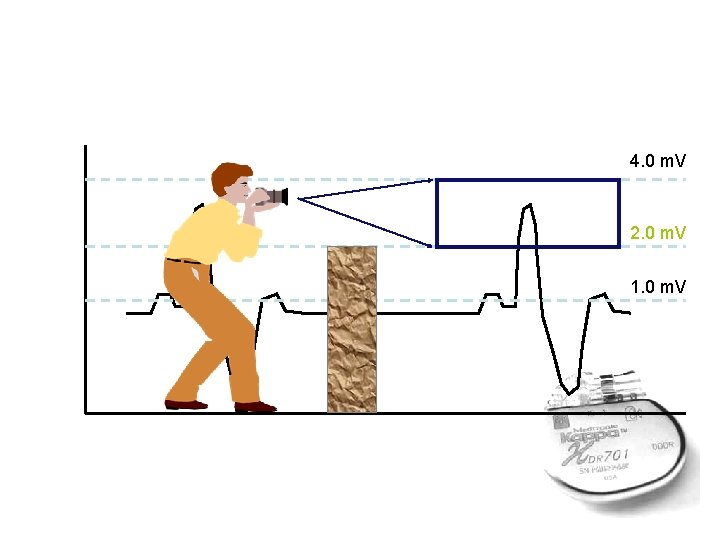
4. 0 m. V 2. 0 m. V 1. 0 m. V
What troubles to shoot? Patient related problems Over passing Under passing or no pacing
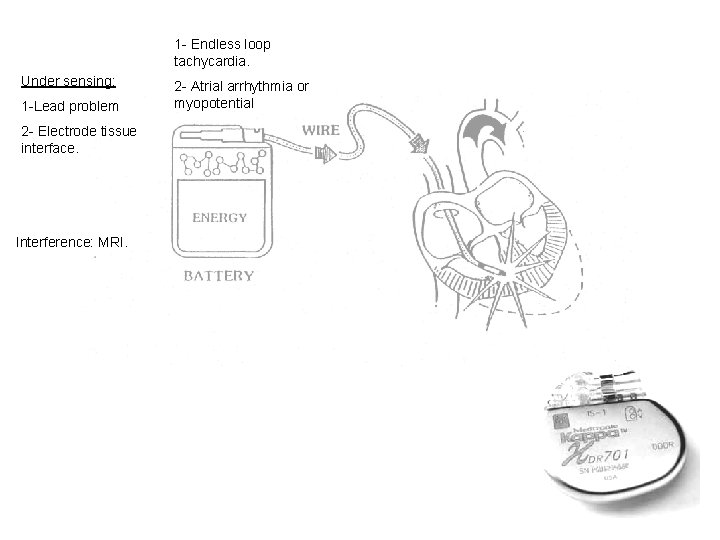
1 - Endless loop tachycardia. Under sensing: 1 -Lead problem 2 - Electrode tissue interface. Interference: MRI. 2 - Atrial arrhythmia or myopotential
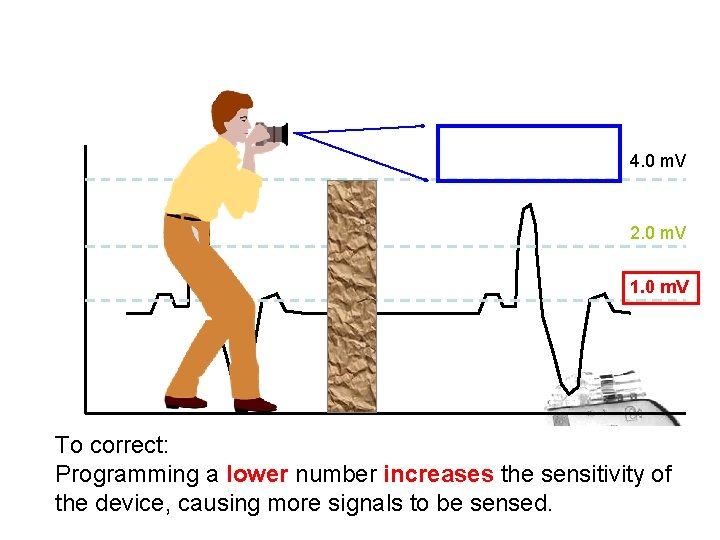
4. 0 m. V 2. 0 m. V 1. 0 m. V To correct: Programming a lower number increases the sensitivity of the device, causing more signals to be sensed.
What troubles to shoot? Patient related problems Under passing or no pacing Over passing Psudo-malfunction 1 - hysteresis. , 2 - rate smoothing. 3 - mood swithc. 4 - fusion and psudo-fusion.
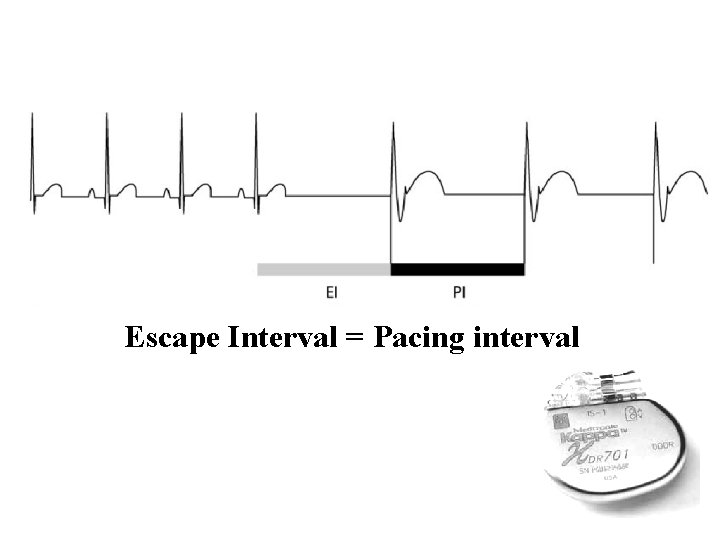
Escape Interval = Pacing interval
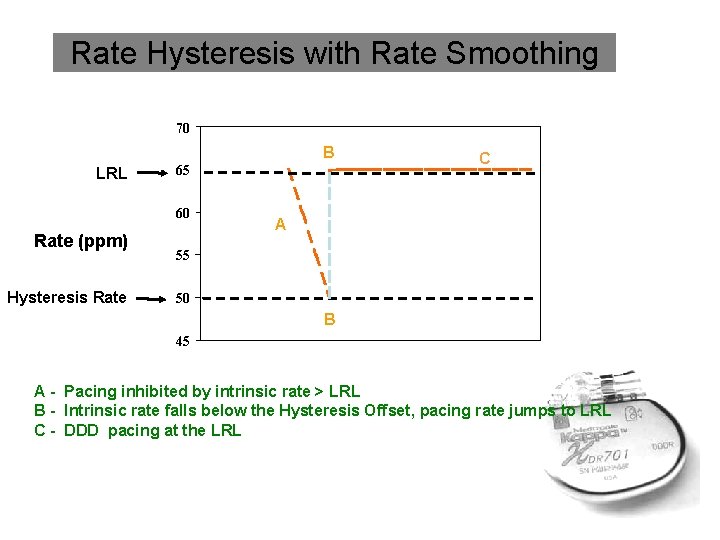
Rate Hysteresis with Rate Smoothing 70 B LRL 65 60 Rate (ppm) Hysteresis Rate C A 55 50 B 45 A - Pacing inhibited by intrinsic rate > LRL B - Intrinsic rate falls below the Hysteresis Offset, pacing rate jumps to LRL C - DDD pacing at the LRL
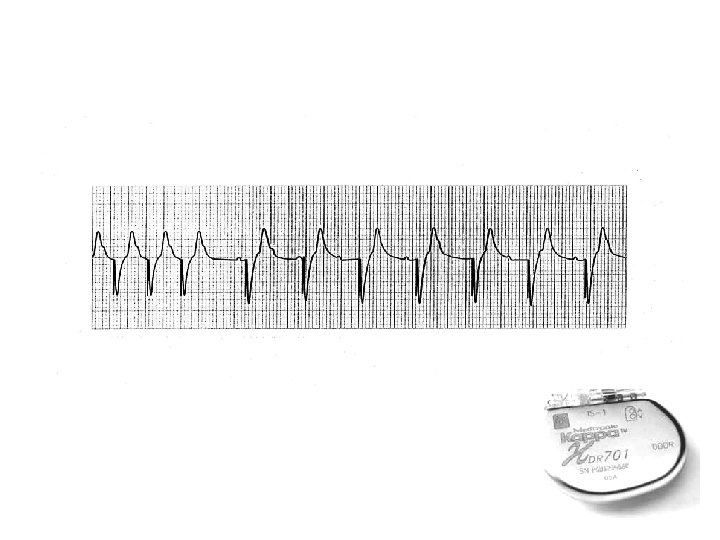
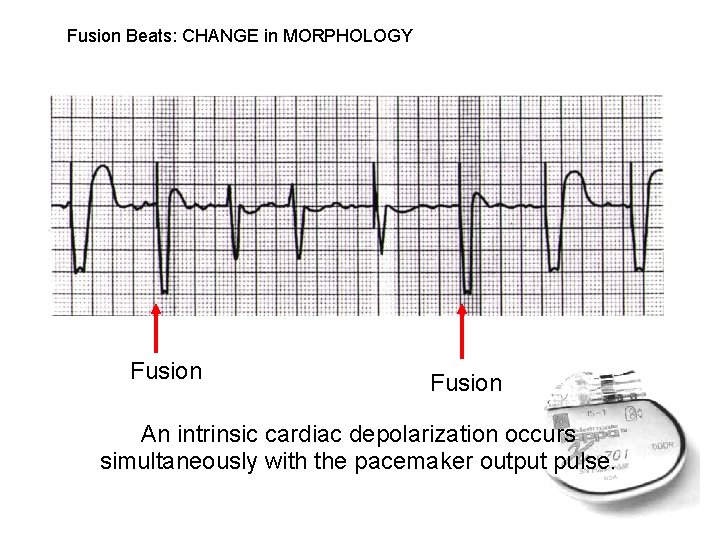
Fusion Beats: CHANGE in MORPHOLOGY Fusion An intrinsic cardiac depolarization occurs simultaneously with the pacemaker output pulse.
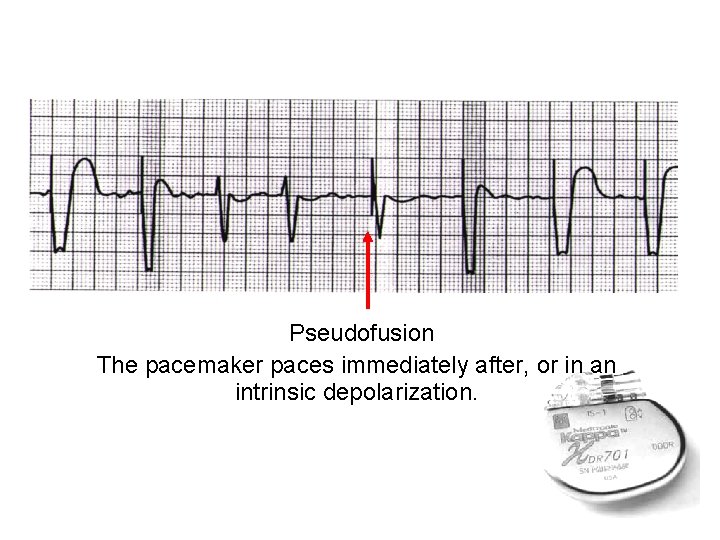
Pseudofusion The pacemaker paces immediately after, or in an intrinsic depolarization.
- Slides: 40