OVERVIEW OF PATIENT CONTROLLED ANALGESIA Louise Reid and
- Slides: 15
OVERVIEW OF PATIENT CONTROLLED ANALGESIA Louise Reid and Claire Wright Bleep 6056
LEARNING OUTCOMES ► PRINCIPLES OF PATIENT CONTROLLED ANALGESIA SYSTEMS ► HOW TO PROMOTE EFFECTIVENESS ► DRUGS USED IN PCA’s
PCA (PATIENT CONTROLLED ANALGESIA) Works by ► Demand bolus ► Lockout interval ► Maximum dose limit
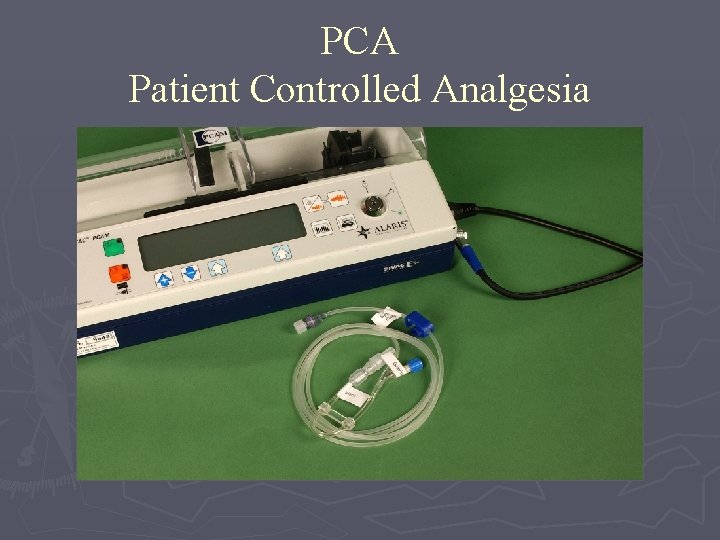
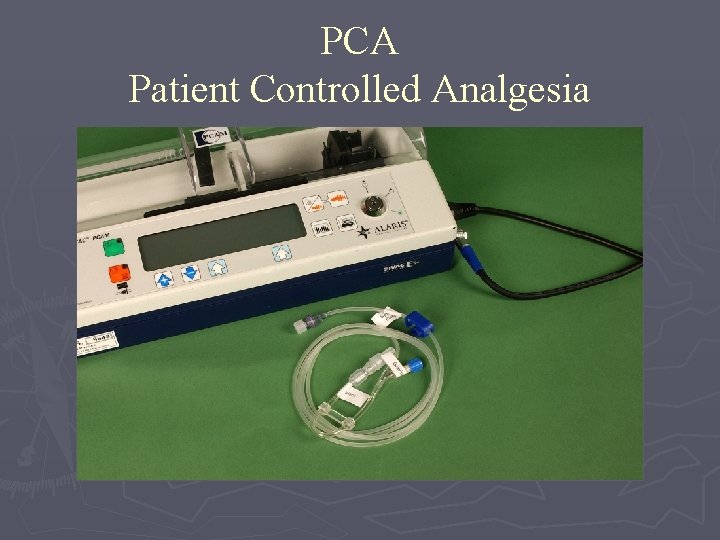
PCA Patient Controlled Analgesia
PCA (PATIENT CONTROLLED ANALGESIA) Exclusion/caution criteria ► Renal Impairment ► Previous side effects/allergy to drug ► Physically unable to use handset/Mentally unable to comprehend use ► Previous history of opioid abuse
PCA (PATIENT CONTROLLED ANALGESIA) Benefits to patient ► Provides rapid pain relief ► Decreased side-effects due to smaller bolus size ► Overcomes reluctance to request pain relief ► Standard protocol can be altered to meet the patient’s needs
PCA (PATIENT CONTROLLED ANALGESIA) Disadvantages ► Patients sleep! ► User error ► Untreated side-effects = ineffective analgesia
Drugs commonly used: ► Morphine – an opioid analgesic which acts on the central nervous system ► Common side-effects: - constipation, feeling nauseous/vomiting, feeling sleepy, tired or dizzy ► Less common side-effects: - reduced respiratory drive, confusion and hallucinations ► Metabolised in the liver ► Excreted renally, does have active metabolites
Oxycodone ► Oxycodone – an opioid analgesic which acts on the central nervous system, slightly more potent than morphine ► Common side-effects: - constipation, feeling nauseous/vomiting, feeling sleepy, tired or dizzy ► Less common side-effects: - reduced respiratory drive, and confusion ► Metabolised in the liver ► Excreted renally, does not have active metabolites
PCA prescriptions ► Standard lockout PCA’s – 1 mg bolus dose, 5 minute ► Special prescription – calculated to meet the needs of the patient, could be an increase in bolus dose and/or a background infusion ► Could be reduced dosing, but not regularly done here
When do we stop the PCA? ► Usually when the patient has an established oral route (able to eat and drink) ► For those with an oral route already – when the pain is starting to settle (e. g patient with fractured ribs)
What analgesia should be prescribed after a PCA? ► It all depends. . . ► How much has the patient used over the last 24 hours? ► Previous ► Too history, taking a pain history, much to discuss here!
Multimodal analgesia ► Regular ►? paracetamol NSAIDs ► Use of local anaesthetic ► Doesn’t include more than one opioid!
Any Questions
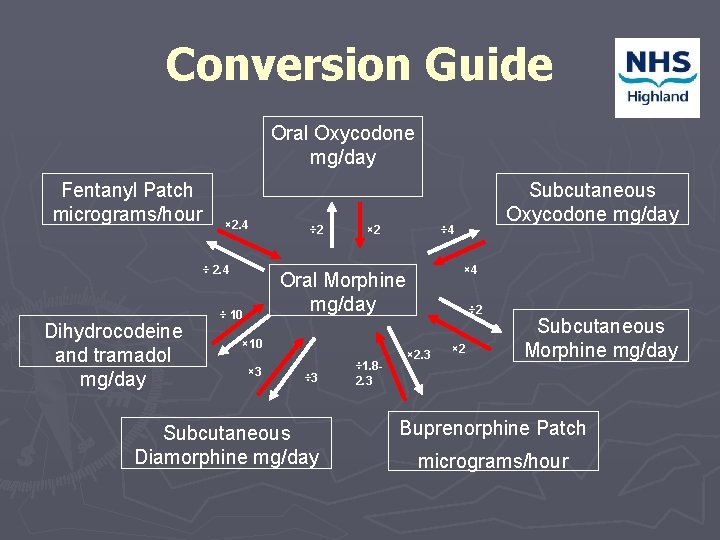
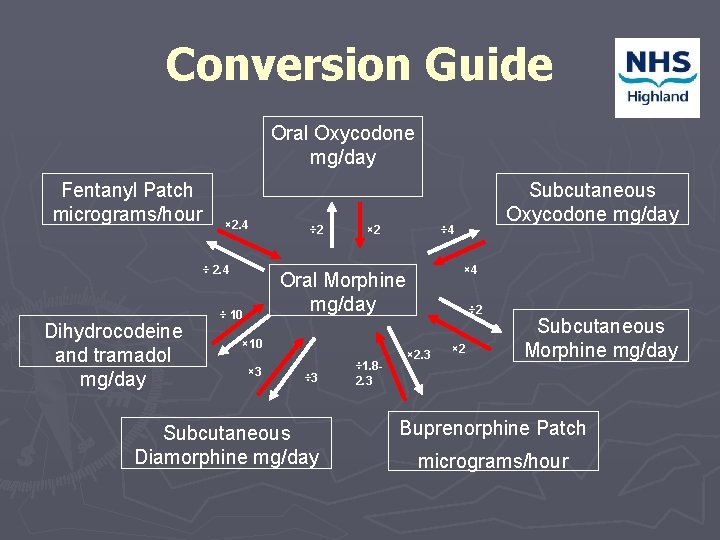
Conversion Guide Oral Oxycodone mg/day Fentanyl Patch micrograms/hour × 2. 4 ÷ 2. 4 Dihydrocodeine and tramadol mg/day ÷ 2 × 2 ÷ 4 × 4 Oral Morphine mg/day ÷ 10 × 3 ÷ 3 Subcutaneous Diamorphine mg/day ÷ 1. 82. 3 Subcutaneous Oxycodone mg/day ÷ 2 × 2. 3 × 2 Subcutaneous Morphine mg/day Buprenorphine Patch micrograms/hour