Overview of obstructive uropathy DR I O LAWAL
Overview of obstructive uropathy DR I. O. LAWAL MBCh. B, FWACS(Urol), FMAS, FACS Snr Consultant Urological Surgeon National Hospital, Abuja. © NITMED TUTORIALS
Lecture outline § Introduction – definitions. - epidemiology § Aetiology § Pathophysiology § Clinical features § Investigations § Treatment –resuscitation - definitive

Definitions § Obstructive uropathy: change in the outflow tract suggestive of an obstructing process being present § Obstructing uropathy: confirms the presence of an obstructing process § Obstructive nephropathy: effect of the obstructing process on the kidney

Aetiology § Congenital ► urethral valves (anterior & posterior), urethral polyps, urethral stricture, phimosis , paraphimosis

Aetiology § Acquired ►Structural - BPH, Ca. P, bladder neck stenosis, urethral stricture, calculi (urethral, bladder, bil ureteral/renal), external compression (faecal impaction, pelvic tumour), ► functional (bladder neck dyssynergia, detrusor-sphincter dyssynergia)
Pathophysiology § Effects of unrecognised or untreated obstruction lead to structural and functional changes on the urinary tract § Early and late changes are recognised
Pathophysiology § Mechanical obstruction and neuromuscular dysfunction have the same effect of stasis in the urinary tract. The effects are manifested in the tract proximal to the obstruction: - the lower tract – urethra - the mid tract – the bladder - the upper tract – ureter and kidney
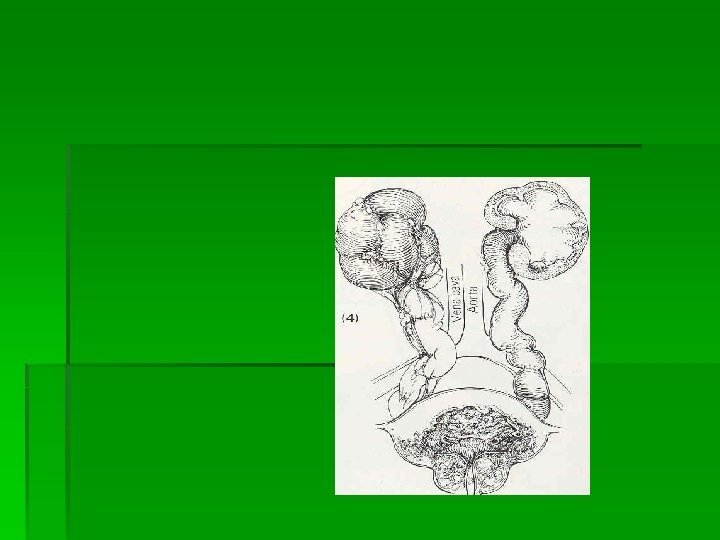
OBSTRUCTION THE LOWER TRACT - URETHRA Straining to void Proximal dilatation Periurethral abscess multiple urethrocutaneous fistulae watering-can scrotum/perineum. THE URINARY BLADDER Obstructions in the bladder neck or urethra produce similar effects in the urinary bladder and Upper tract – in two phases (1) compensation and (2) decompensation. Stage of compensation Hypertrophy, Trabeculation and Diverticula
. STAGE OF DECOMPENSATION - Bladder dilates, residual urine increases - Power of contraction diminishes - Inability to void UPPER TRACT - Back pressure effect – Ureter compensation by - Hypertrophy, hyperperistalsis - Elongation and tortuosity - Reflux may occur late - hydroureter
THE KIDNEY - Pelvis first progressively dilate - Hydrocalycosis and hydronephrosis - Stone formation and infection - recurrent pyelonephritis - Urine formation decreases but never ceases Small contracted kidney, hydronephrotic atrophy - Renal hypertension - Renal counter balance - Renal failure or non-function
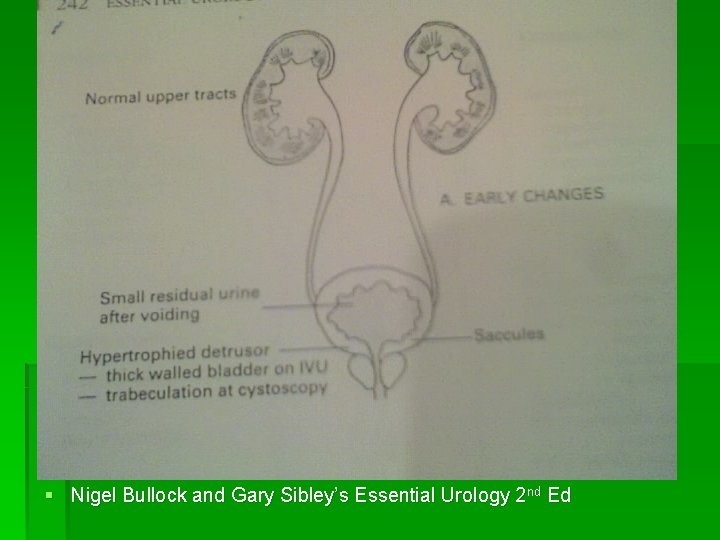
Early changes § Nigel Bullock and Gary Sibley’s Essential Urology 2 nd Ed
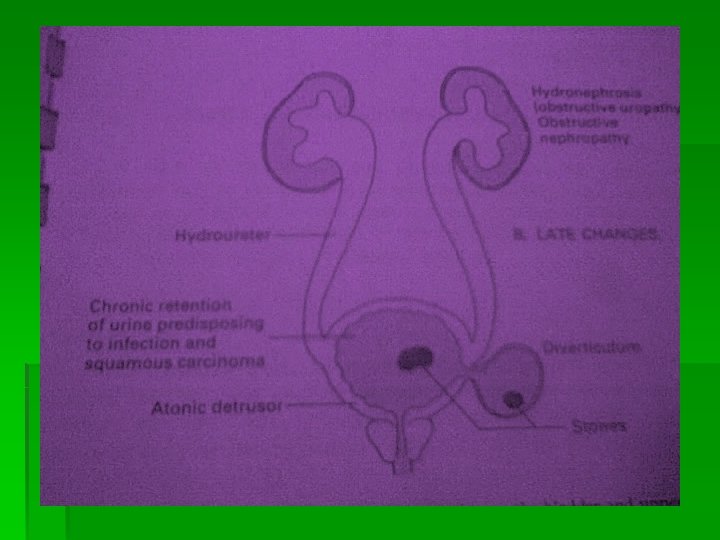
Late changes
![Clinical features [Modes of presentations] ►Irritative (storage) symptoms - freq, urgency, nocturia ►Obstructive (voiding) Clinical features [Modes of presentations] ►Irritative (storage) symptoms - freq, urgency, nocturia ►Obstructive (voiding)](http://slidetodoc.com/presentation_image_h2/5622f132c00ce78c976fbaa200090e97/image-14.jpg)
Clinical features [Modes of presentations] ►Irritative (storage) symptoms - freq, urgency, nocturia ►Obstructive (voiding) symptoms – hesitancy, poor stream, terminal dribbling, use of abd. muscles ►Urinary retention ►Complications of obstruction – UTI, bladder calculi, heamaturia ►Renal impairment ►Others – neurological Sxs
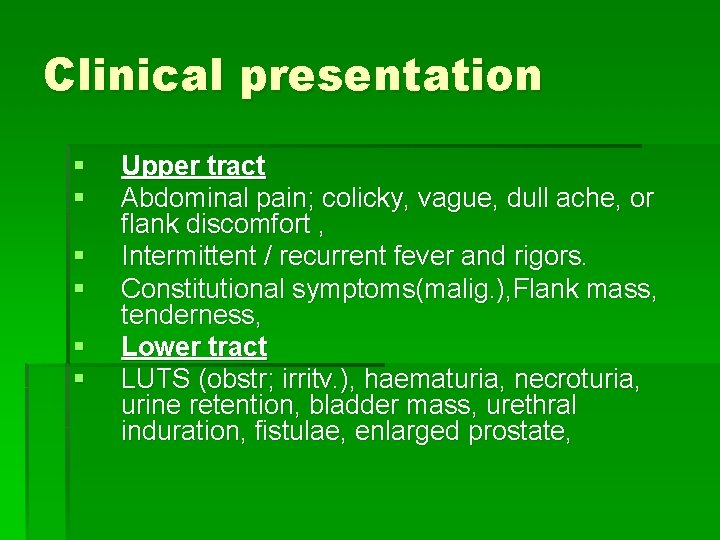
Clinical presentation § § § Upper tract Abdominal pain; colicky, vague, dull ache, or flank discomfort , Intermittent / recurrent fever and rigors. Constitutional symptoms(malig. ), Flank mass, tenderness, Lower tract LUTS (obstr; irritv. ), haematuria, necroturia, urine retention, bladder mass, urethral induration, fistulae, enlarged prostate,

Clinical features of uraemia § Symptoms are common when the serum urea con § centration exceeds 40 mmol/L, but many patients develop uraemic symptoms at lower levels of serum urea. § Symptoms include: - malaise, -nausea, vomiting -paraesthesiae and tetany due to hypocalcaemia -symptoms due to anaemia
clinical features cntd. § In more advanced uraemia (serum urea > 50 -60 mmol/L), § these symptoms become more severe, and CNS symptoms are common: clouding of consciousness, and seizures, encephalopathy,

Other findings in Uraemic pt § Skin: uremic frost. Hyperpigmented , as uremia worsens (melanosis), scratch marks. § Cardiovascular system: Uremic pericarditis (pericardial effusion). fluid retention→ pulmonary edema, peripheral edema, and severe hypertension. § Lungs: pulmonary edema , crackles § GI system: Uremic fetor §. Neurologic system: Uremic encephalopathy , seizures,
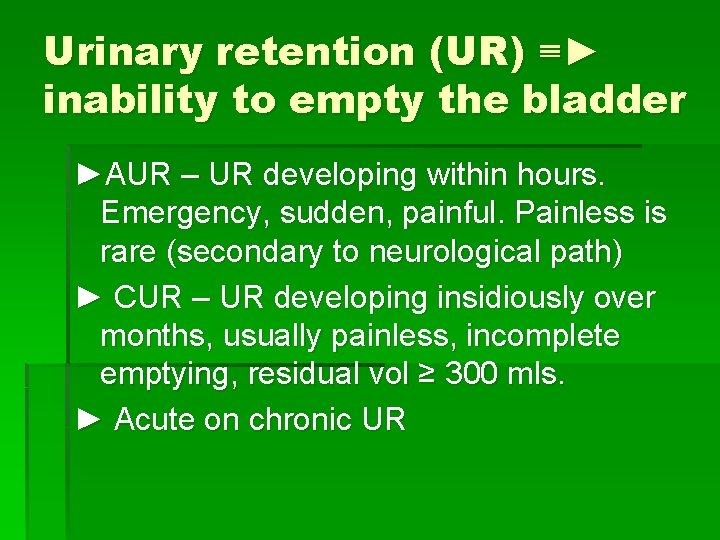
Urinary retention (UR) ≡► inability to empty the bladder ►AUR – UR developing within hours. Emergency, sudden, painful. Painless is rare (secondary to neurological path) ► CUR – UR developing insidiously over months, usually painless, incomplete emptying, residual vol ≥ 300 mls. ► Acute on chronic UR

Investigations § § § Haematology Blood chemistry Microbiology Radiology Others - cystoscopy -surgery
investigations § § § Serum E/U/Cr, Urine m/c/s, Urinalysis, Specific gravity 24 cr clearance. FBC,
Imaging: Ultrasound § Useful in Post renal ARF. § Early obstruction may not show significant hydronephrosis. § External obstruction encasing the whole urinary system may not show hydronephrosis, for e. g. , retroperitoneal fibrosis.
Imagings cntd. - KUB IVU Antegrade pyelography Cystoscopy , retrograde pyelography
CT scan § Useful for detecting stones, location of the obstruction, Tumours etc. , Isotope renography § To evaluate the function significance of obstruction. § Done with lasix and Mag 3 isotope for evaluating obstruction.
Principles of management § Aim ►Removing obstruction ► Correcting or preventing damage to kidneys
Preliminary treatment § § § Urinary tract infection Urinary retention Anaemia

UTI § § Specimen → microscopy and culture Antibiotics Urinary diversion Surgery
Anaemia § § § Complete blood count Clotting profile Haemoglobin genotype Grouping and cross matching Haematinics, nutrition Blood transfusion

Urinary retention § Painful UR ►catheterize→ residual vol <300 ml or Sxs persist →consider alternative Dx ► Retention confirmed → ↑creatinine→ watch for POD →consider def Rx of BOO ► Normal Cr → Rx or resolution of ppting factors →TWOC → succeeds → keep under surveillance
Painless UR § No neurological Sxs/signs ►↑Cr →HPCUR →cath monitor (hydration, Hrly urine) ►N Cr → LPCUR → Inv & Mx electively ► Hrly urine >200 mls/hr for 12 hrs → IVF
Urinary retention § Failed catheterization ►Urinary diversion -Suprapubic cystostomy
RELIEVE OF OBSTRUCTION



Post Obstructive Diuresis § Physiological § 90% retained Na, Water, Urea § Pathological § ADH Insensitivity § Salt loss § ALOGRITHM § § § Catheterize / note RV/ CSU Bloods BUN / Na Admit if UO >200 mls/hr If >200 mls/hr on 2 consecutive hrs send urine for osmolality If iso-osmolar UO usually returns to normal within 24 hrs If hypo-osmolar (ADH insensitivity) replace 1/2 of UO with dext. sal & oral fluids. Daily weight § If hyper-osmolar (Na loss) replace equal with Na. Cl. Postural BP, Serum & urine Na QDS. High mortality
Definitive treatment § Treat the underlying cause § Surgery-Open Surgery-depends on cause. - Minimal access-TURP, Laparascopic/ Robotic Non surgical – drugs - radiotherapy - others
THANK YOU ALL
Questions
- Slides: 39