OVERVIEW OF MECHANICAL VENTILATORY SUPPORT AND MANAGEMENT OF






































- Slides: 98
OVERVIEW OF MECHANICAL VENTILATORY SUPPORT AND MANAGEMENT OF PATIENT- AND VENTILATOR-RELATED RESPONSES PREPARED BY: Dr. Altayeb Abdulazeem Idress Ph. D , RN , CNS altayebabdo 9@gmail. com
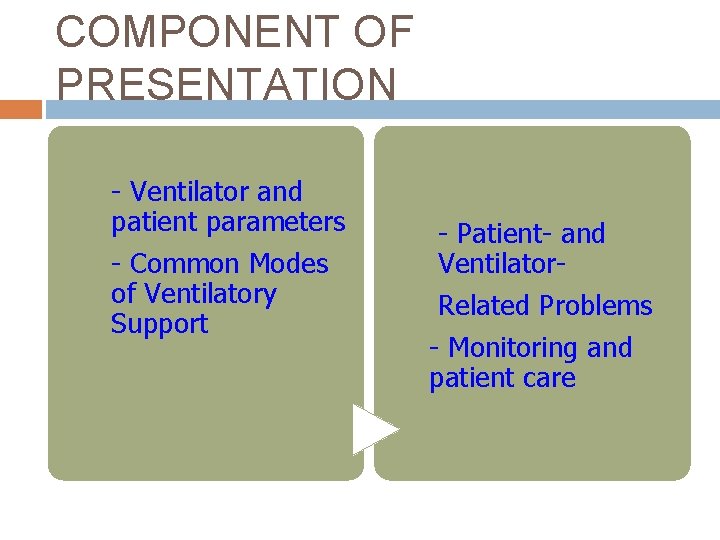
COMPONENT OF PRESENTATION - Ventilator and patient parameters - Common Modes of Ventilatory Support - Patient- and Ventilator. Related Problems - Monitoring and patient care

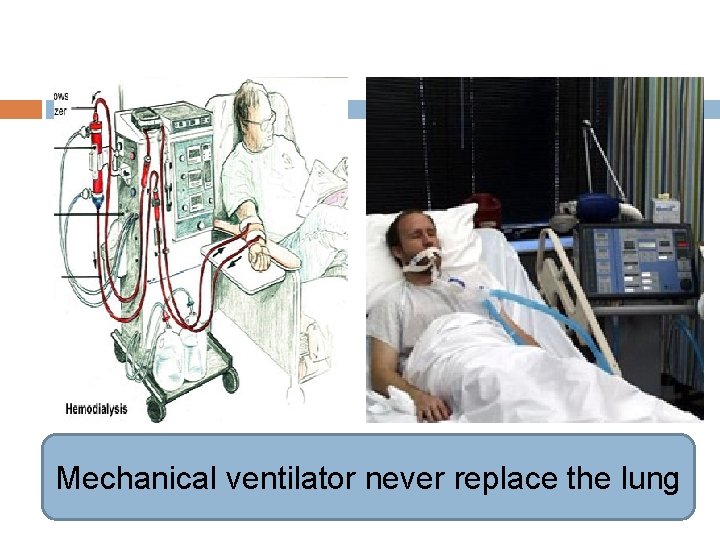
What is the different between two machine

Hemodialysis completely replace the kidney
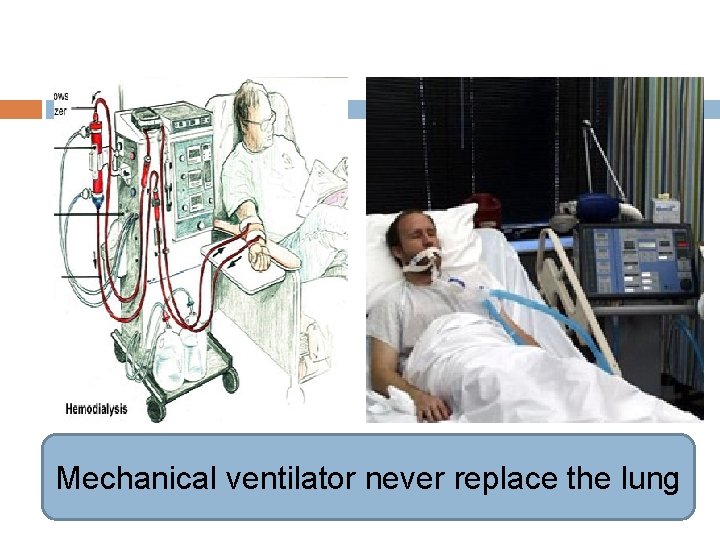
Mechanical ventilator never replace the lung

Nurses must be knowledgeable about the function and limitations of ventilator modes, causes of respiratory distress and dyssynchrony with the ventilator, and appropriate management in order to provide high-quality patient-centered care.

Prompt recognition of problems and action by the nurse may resolve acute respiratory distress, dyspnea, and increased work of breathing and prevent adverse events. This article presents an overview of mechanical ventilation modes and the assessment and management of dyspnea and patient-ventilator dyssynchrony.
mechanical ventilatory support is routinely needed for critically ill adults in intensive care units and is also a common therapy in subacute and longterm care settings.
The primary goals of mechanical ventilatory support are to normalize arterial blood gas levels and acid-base imbalance by providing adequate ventilation and oxygenation.
Mechanical ventilation can decrease the patient’s work of breathing by unloading respiratory muscles in a synchronous manner. Mechanical ventilation can also maintain long term respiratory support of patients with chronic ventilatory problems.
Responsibilities related to ventilator management may vary among acute care settings, but the nurse is usually the “first-line manager” challenged with patient- and ventilator-related problems.
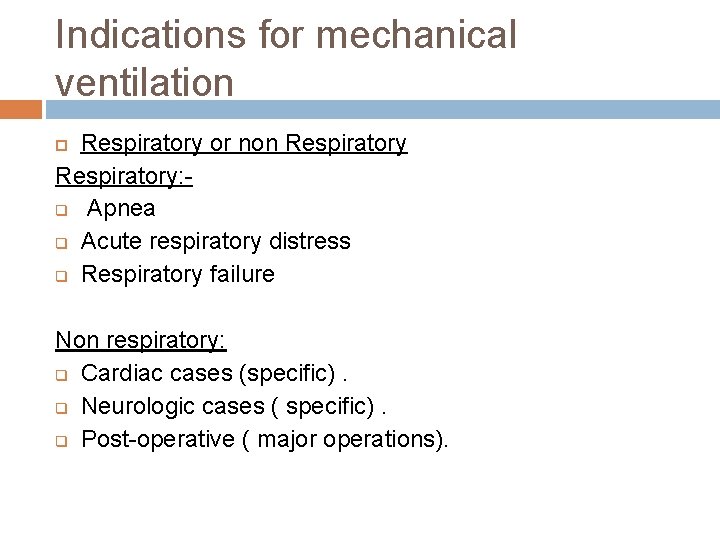
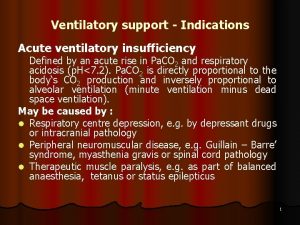
Indications for mechanical ventilation Respiratory or non Respiratory: q Apnea q Acute respiratory distress q Respiratory failure Non respiratory: q Cardiac cases (specific). q Neurologic cases ( specific). q Post-operative ( major operations).
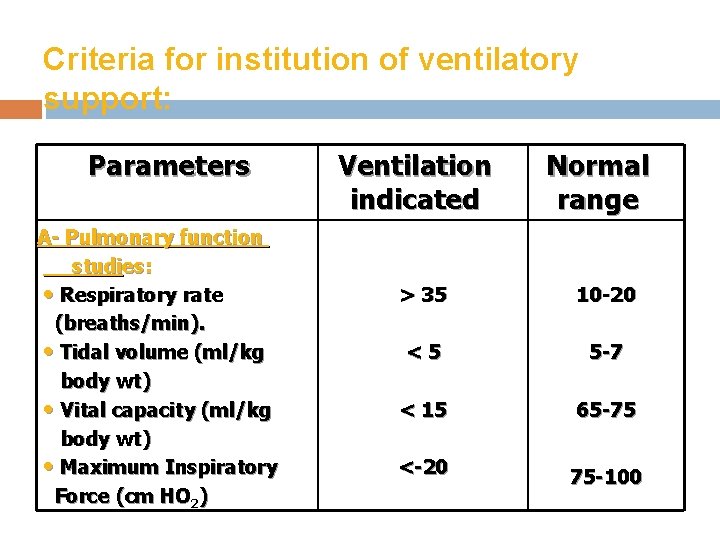
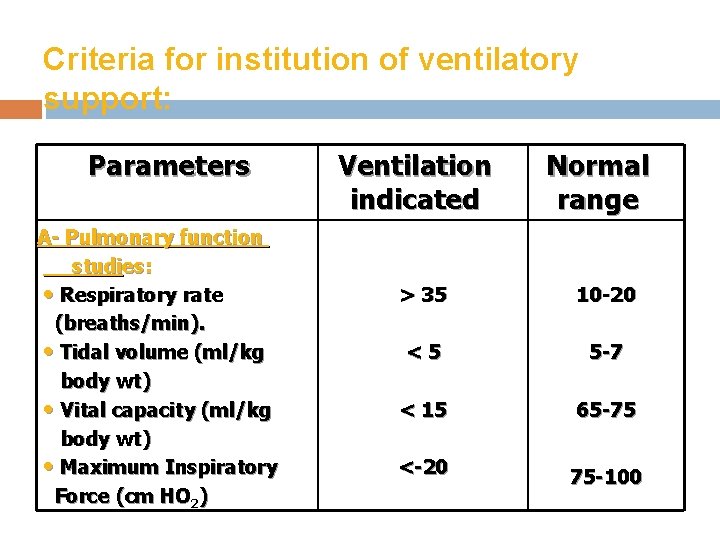
Criteria for institution of ventilatory support: Parameters A- Pulmonary function studies: • Respiratory rate (breaths/min). • Tidal volume (ml/kg body wt) • Vital capacity (ml/kg body wt) • Maximum Inspiratory Force (cm HO 2) Ventilation indicated Normal range > 35 10 -20 <5 5 -7 < 15 65 -75 <-20 75 -100

Criteria for institution of ventilatory support: Parameters Ventilation indicated Normal range B- Arterial blood Gases • PH • Pa. O 2 (mm. Hg) • Pa. CO 2 (mm. Hg) < 7. 25 < 60 > 50 7. 35 -7. 45 75 -100 35 -45
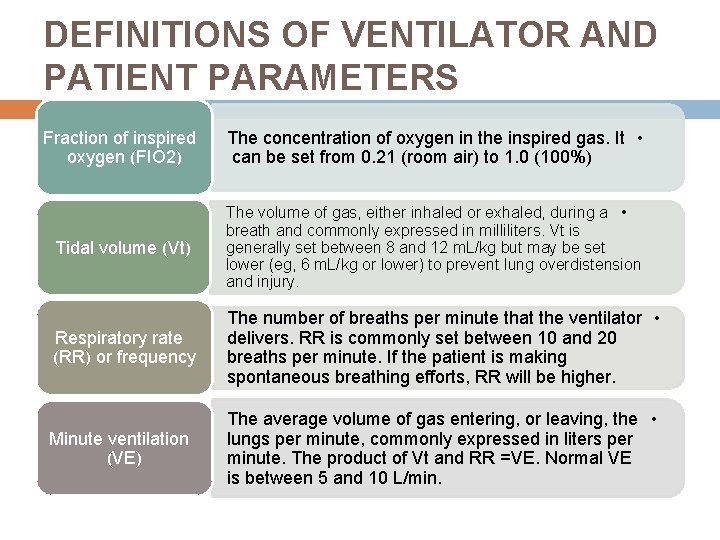
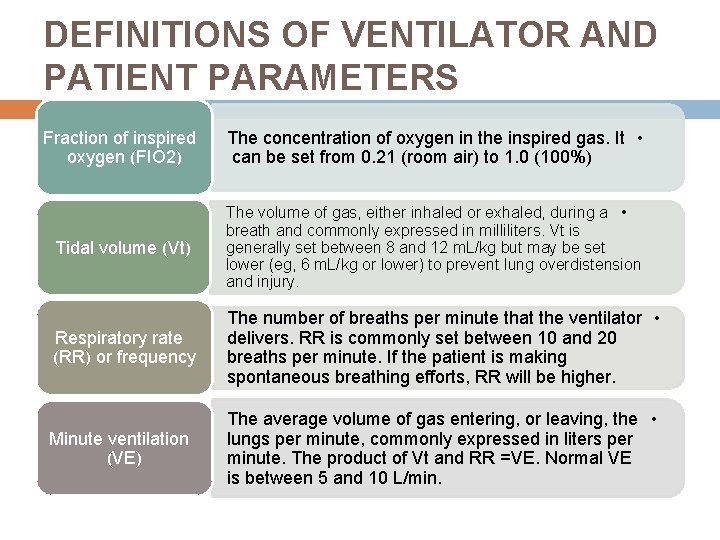
DEFINITIONS OF VENTILATOR AND PATIENT PARAMETERS Fraction of inspired oxygen (FIO 2) The concentration of oxygen in the inspired gas. It • can be set from 0. 21 (room air) to 1. 0 (100%) Tidal volume (Vt) The volume of gas, either inhaled or exhaled, during a • breath and commonly expressed in milliliters. Vt is generally set between 8 and 12 m. L/kg but may be set lower (eg, 6 m. L/kg or lower) to prevent lung overdistension and injury. Respiratory rate (RR) or frequency The number of breaths per minute that the ventilator • delivers. RR is commonly set between 10 and 20 breaths per minute. If the patient is making spontaneous breathing efforts, RR will be higher. Minute ventilation (VE) The average volume of gas entering, or leaving, the • lungs per minute, commonly expressed in liters per minute. The product of Vt and RR =VE. Normal VE is between 5 and 10 L/min.
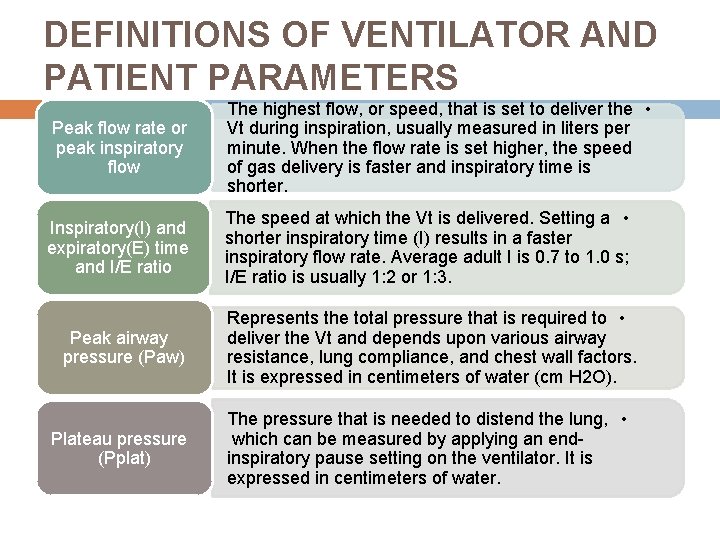
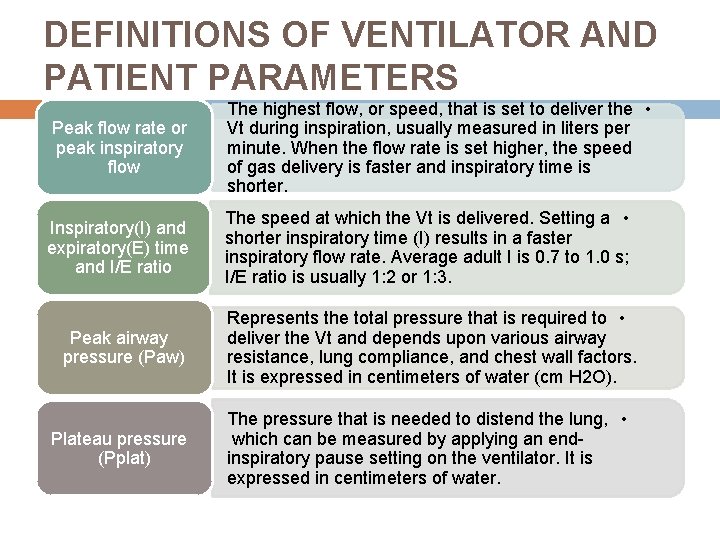
DEFINITIONS OF VENTILATOR AND PATIENT PARAMETERS Peak flow rate or peak inspiratory flow The highest flow, or speed, that is set to deliver the • Vt during inspiration, usually measured in liters per minute. When the flow rate is set higher, the speed of gas delivery is faster and inspiratory time is shorter. Inspiratory(I) and expiratory(E) time and I/E ratio The speed at which the Vt is delivered. Setting a • shorter inspiratory time (I) results in a faster inspiratory flow rate. Average adult I is 0. 7 to 1. 0 s; I/E ratio is usually 1: 2 or 1: 3. Peak airway pressure (Paw) Represents the total pressure that is required to • deliver the Vt and depends upon various airway resistance, lung compliance, and chest wall factors. It is expressed in centimeters of water (cm H 2 O). Plateau pressure (Pplat) The pressure that is needed to distend the lung, • which can be measured by applying an endinspiratory pause setting on the ventilator. It is expressed in centimeters of water.
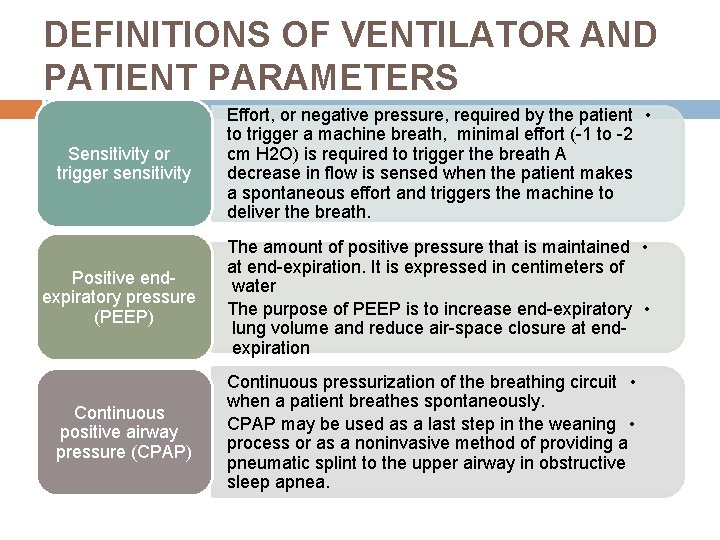
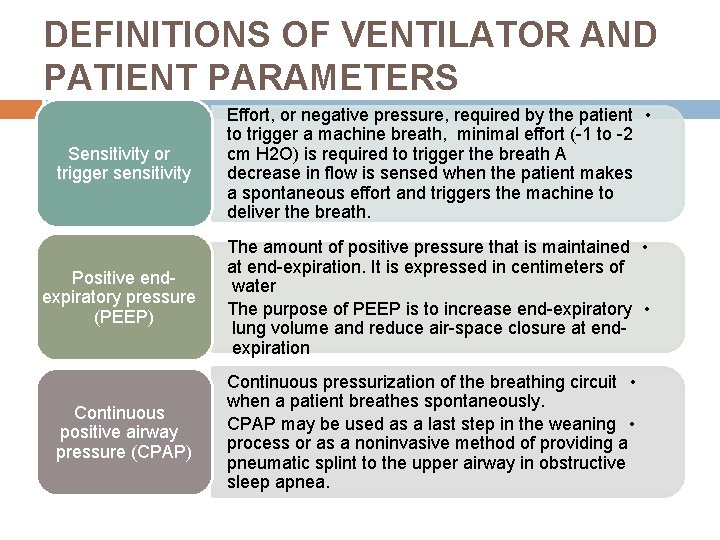
DEFINITIONS OF VENTILATOR AND PATIENT PARAMETERS Sensitivity or trigger sensitivity Effort, or negative pressure, required by the patient • to trigger a machine breath, minimal effort (-1 to -2 cm H 2 O) is required to trigger the breath A decrease in flow is sensed when the patient makes a spontaneous effort and triggers the machine to deliver the breath. Positive endexpiratory pressure (PEEP) The amount of positive pressure that is maintained • at end-expiration. It is expressed in centimeters of water The purpose of PEEP is to increase end-expiratory • lung volume and reduce air-space closure at endexpiration Continuous positive airway pressure (CPAP) Continuous pressurization of the breathing circuit • when a patient breathes spontaneously. CPAP may be used as a last step in the weaning • process or as a noninvasive method of providing a pneumatic splint to the upper airway in obstructive sleep apnea.
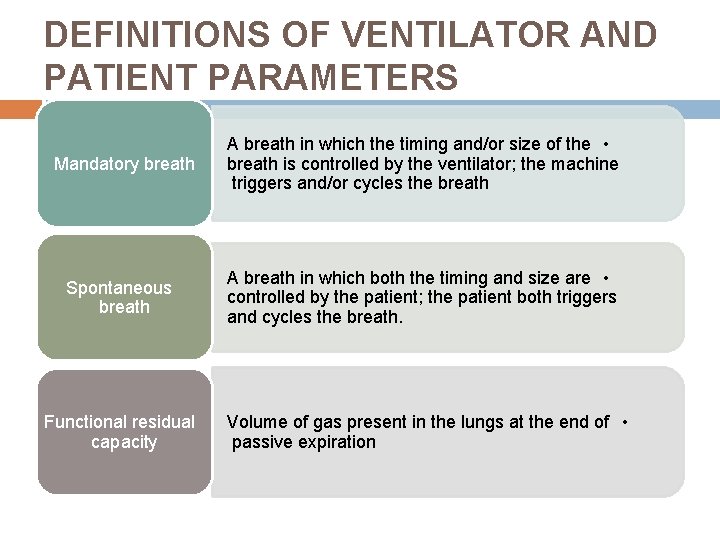
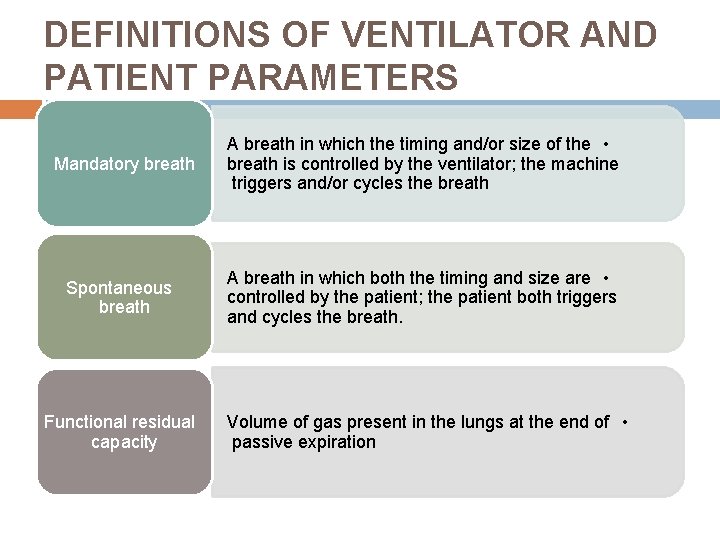
DEFINITIONS OF VENTILATOR AND PATIENT PARAMETERS Mandatory breath A breath in which the timing and/or size of the • breath is controlled by the ventilator; the machine triggers and/or cycles the breath Spontaneous breath A breath in which both the timing and size are • controlled by the patient; the patient both triggers and cycles the breath. Functional residual capacity Volume of gas present in the lungs at the end of • passive expiration
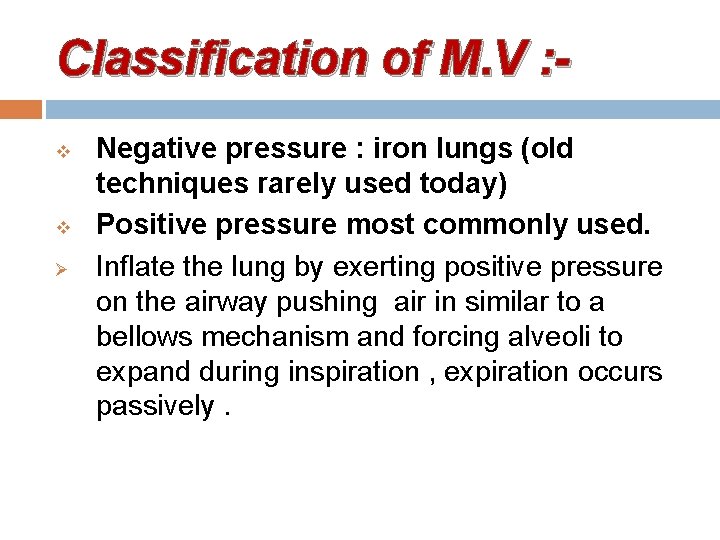
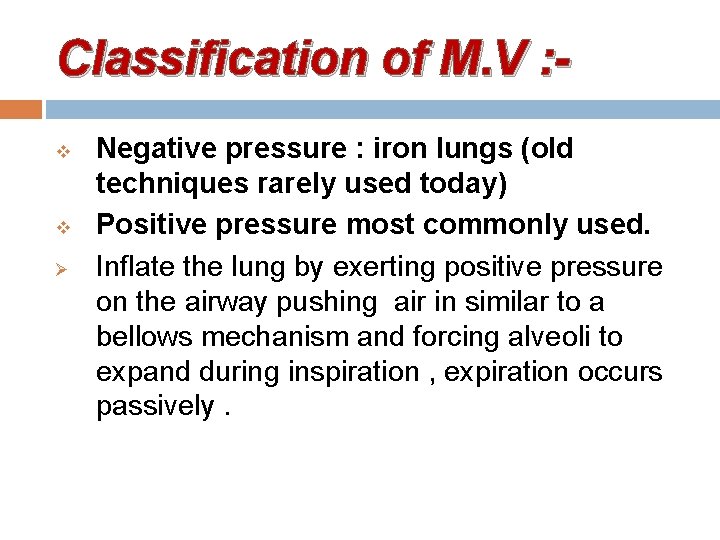
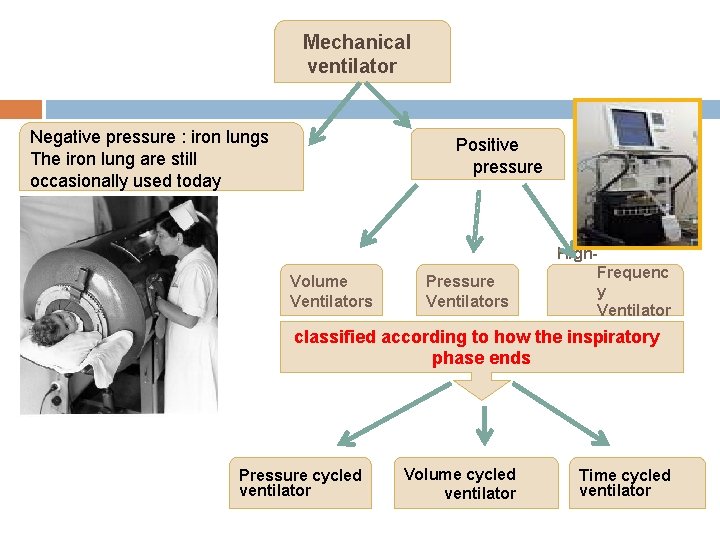
Classification of M. V : v v Ø Negative pressure : iron lungs (old techniques rarely used today) Positive pressure most commonly used. Inflate the lung by exerting positive pressure on the airway pushing air in similar to a bellows mechanism and forcing alveoli to expand during inspiration , expiration occurs passively.
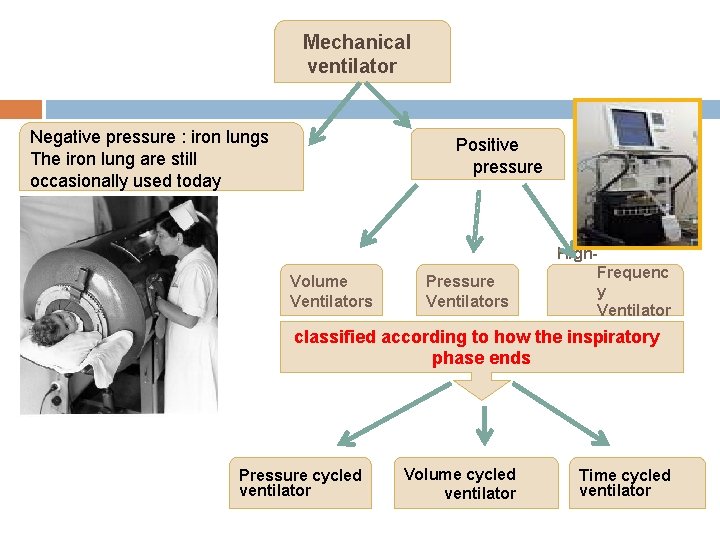
Mechanical ventilator Negative pressure : iron lungs The iron lung are still occasionally used today Positive pressure High. Frequenc Volume Pressure y Ventilators Ventilator s classified according to how the inspiratory phase ends Pressure cycled ventilator Volume cycled ventilator Time cycled ventilator
Types of Positive-Pressure Ventilators 1 - Volume Ventilators. 2 - Pressure Ventilators 3 - High-Frequency Ventilators
1 - Volume Ventilators The volume ventilator is commonly used in critical care settings. The basic principle of this ventilator is that a designated volume of air is delivered with each breath. The amount of pressure required to deliver the set volume depends on : - Patient’s lung compliance - Patient–ventilator resistance factors.

Therefore, peak inspiratory pressure (PIP ) must be monitored in volume modes because it varies from breath to breath. With this mode of ventilation, a respiratory rate, inspiratory time, and tidal volume are selected for the mechanical breaths.

2 - Pressure Ventilators The use of pressure ventilators is increasing in critical care units. A typical pressure mode delivers a selected gas pressure to the patient early in inspiration, and sustains the pressure throughout the inspiratory phase. By meeting the patient’s inspiratory flow demand throughout inspiration, patient effort is reduced and comfort increased.

Although pressure is consistent with these modes, volume is not. Volume will change with changes in resistance or compliance, Therefore, exhaled tidal volume is the variable to monitor closely. With pressure modes, the pressure level to be delivered is selected, and with some mode options (i. e. , pressure controlled [PC], described later), rate and inspiratory time are preset as well.
3 - High-Frequency Ventilators High-frequency ventilators use small tidal volumes (1 to 3 m. L/kg) at frequencies greater than 100 breaths/minute. The high-frequency ventilator accomplishes oxygenation by the diffusion of oxygen and carbon dioxide from high to low gradients of concentration.

This diffusion movement is increased if the kinetic energy of the gas molecules is increased. A high-frequency ventilator would be used to achieve lower peak ventilator pressures, thereby lowering the risk of barotrauma.
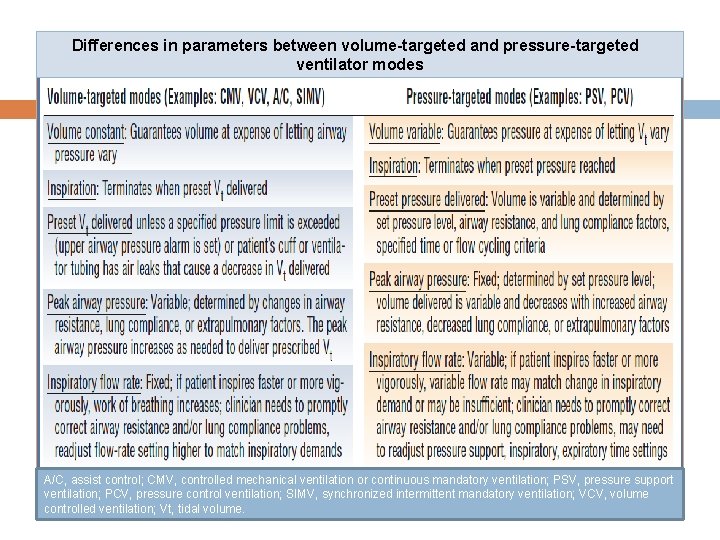
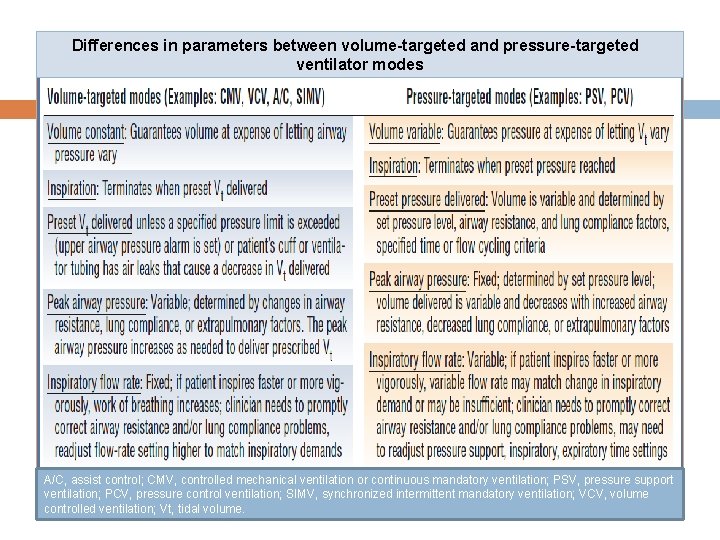
Differences in parameters between volume-targeted and pressure-targeted ventilator modes A/C, assist control; CMV, controlled mechanical ventilation or continuous mandatory ventilation; PSV, pressure support ventilation; PCV, pressure control ventilation; SIMV, synchronized intermittent mandatory ventilation; VCV, volume controlled ventilation; Vt, tidal volume.
Dual-Controlled Modes Newer ventilators offer hybrid modes that combine features of volume-targeted and pressure targeted ventilation in an attempt to avoid both the high peak airway pressures of volume ventilation and the varying tidal volumes that may occur with pressure ventilation.
Classification of positive-pressure ventilators: Ventilators are classified according to how the inspiratory phase ends. The factor which terminates the inspiratory cycle reflects the machine type. They are classified as: 1 - Pressure cycled ventilator 2 - Volume cycled ventilator 3 - Time cycled ventilator
1 - Volume-cycled ventilator Inspiration is terminated after a preset tidal volume has been delivered by the ventilator. The ventilator delivers a preset tidal volume (VT), and inspiration stops when the preset tidal volume is achieved.
2 - Pressure-cycled ventilator In which inspiration is terminated when a specific airway pressure has been reached. The ventilator delivers a preset pressure; once this pressure is achieved, end inspiration occurs.
3 - Time-cycled ventilator In which inspiration is terminated when a preset inspiratory time, has elapsed. Time cycled machines are not used in adult critical care settings. They are used in pediatric intensive care areas.
Common Modes of Ventilatory Support
What is the mode? Mode of ventilation refers to the method of inspiratory support provided by the mechanical ventilator. It is the specific combination of breathing pattern and control

variables to deliver inspiration and selection of mode is based on the clinician’s familiarity and experience
Ventilator mode The way the machine ventilates the patient How much the patient will participate in his own ventilatory pattern. Each mode is different in determining how much work of breathing the patient has to do.

Point of Reference: Spontaneous Ventilation
Controlled Mechanical Ventilation (CMV) Assist controlled ventilation (ACV) Synchronized Intermittent Mandatory Ventilation (SIMV) Continuous Positive Airway Pressure (CPAP) Positive End-Expiratory Pressure (PEEP)
Controlled Mechanical Ventilation (CMV) Assist controlled ventilation (ACV) Synchronized Intermittent Mandatory Ventilation (SIMV) Continuous Positive Airway Pressure (CPAP) Positive End-Expiratory Pressure (PEEP)
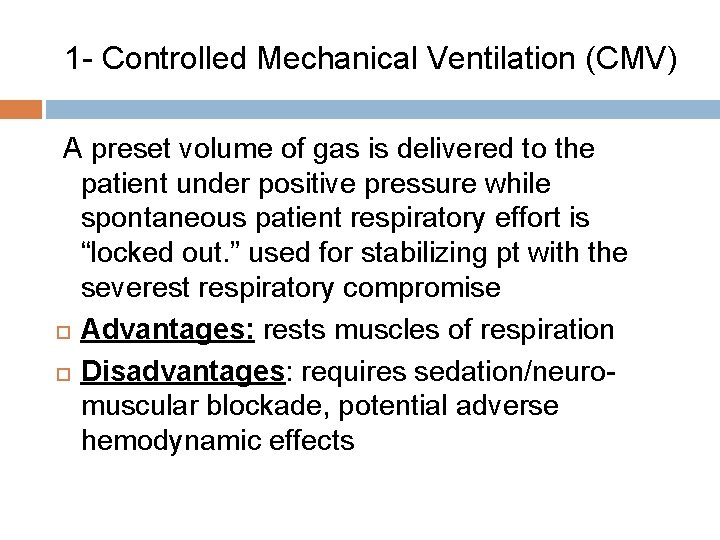
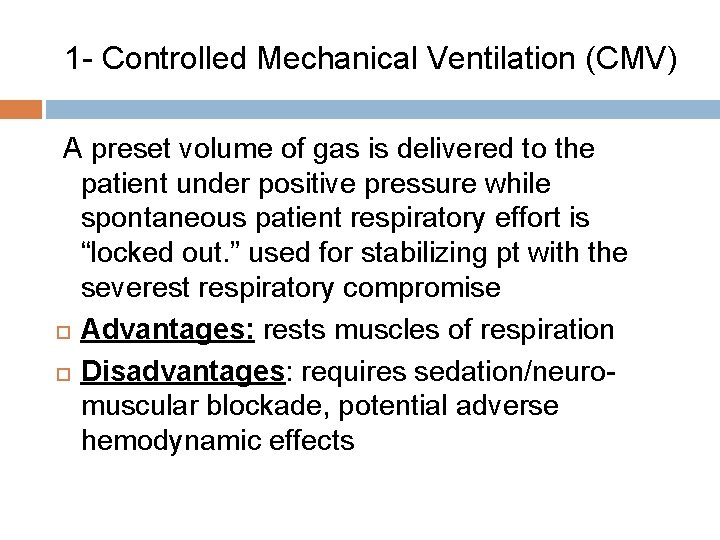
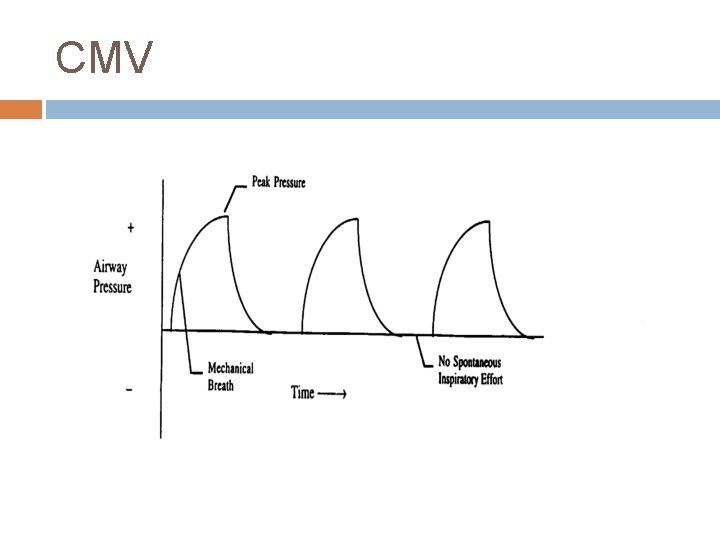
1 - Controlled Mechanical Ventilation (CMV) A preset volume of gas is delivered to the patient under positive pressure while spontaneous patient respiratory effort is “locked out. ” used for stabilizing pt with the severest respiratory compromise Advantages: rests muscles of respiration Disadvantages: requires sedation/neuromuscular blockade, potential adverse hemodynamic effects
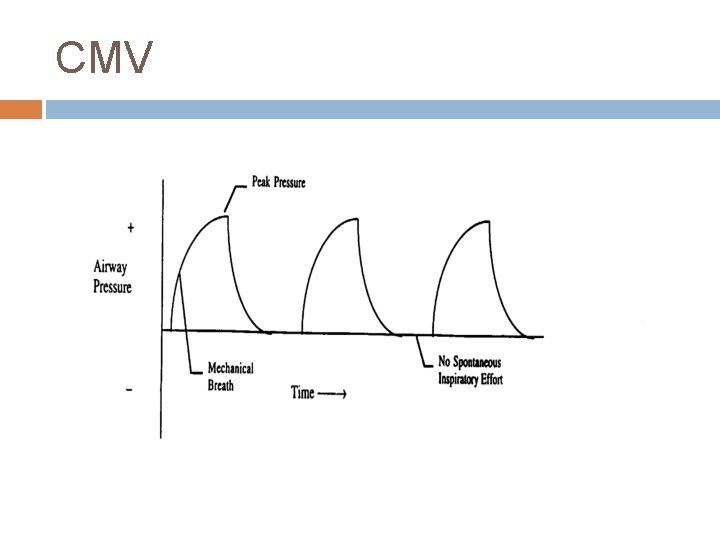
CMV

Mechanical/Positive pressure breath
CMV The duration of CMV is vary from hours to days to weeks, or even to months, depending of the nature of the lung injury.
Controlled Mechanical Ventilation (CMV) Assist controlled ventilation (ACV) Synchronized Intermittent Mandatory Ventilation (SIMV) Continuous Positive Airway Pressure (CPAP) Positive End-Expiratory Pressure (PEEP)
Controlled Mechanical Ventilation (CMV) Assist controlled ventilation (ACV) Synchronized Intermittent Mandatory Ventilation (SIMV) Continuous Positive Airway Pressure (CPAP) Positive End-Expiratory Pressure (PEEP)

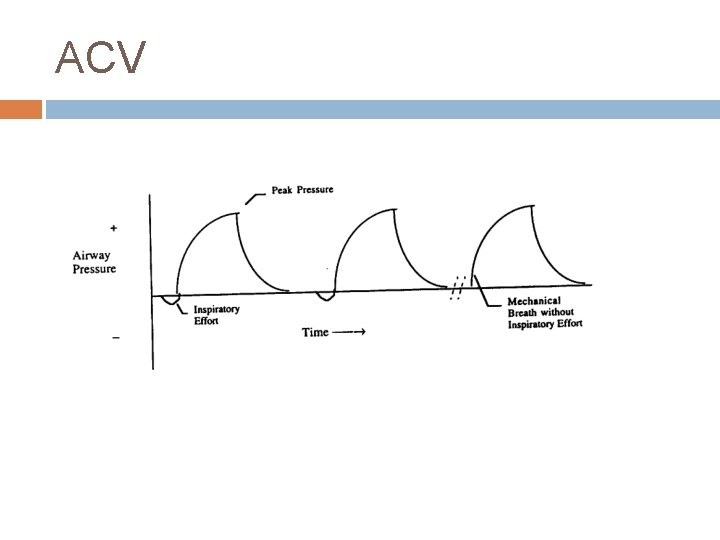
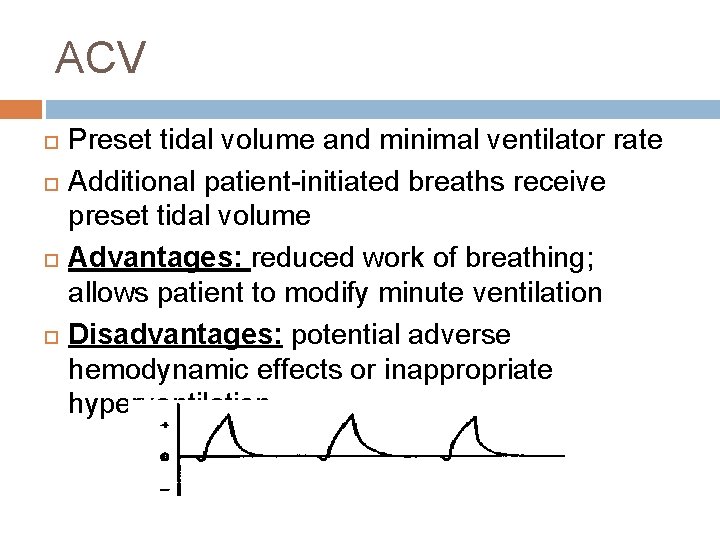
ACV In this mode, a preset volume of gas is delivered to the patient at a preset rate, but the patient may trigger a ventilator breath with negative inspiratory effort.
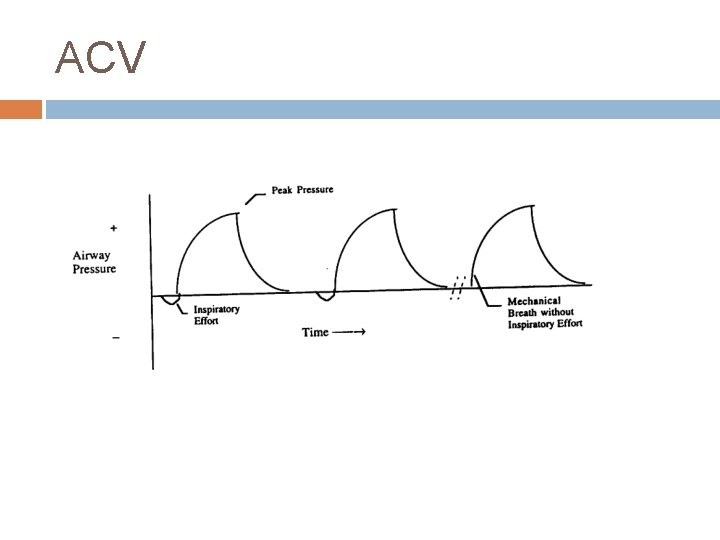
ACV
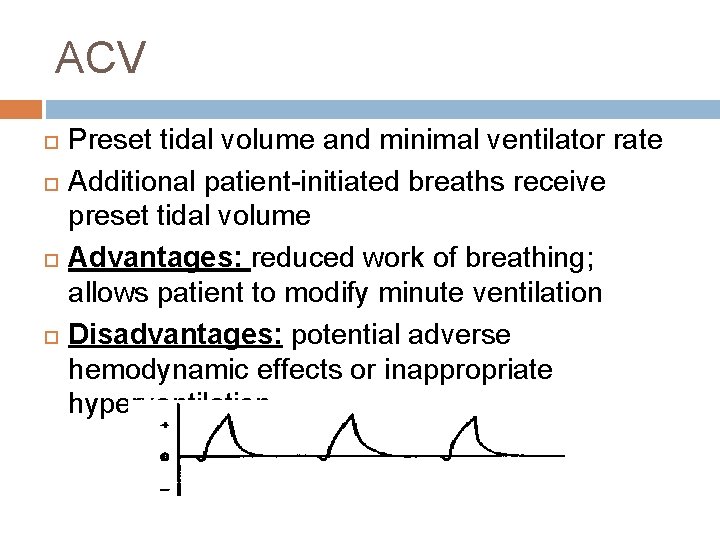
ACV Preset tidal volume and minimal ventilator rate Additional patient-initiated breaths receive preset tidal volume Advantages: reduced work of breathing; allows patient to modify minute ventilation Disadvantages: potential adverse hemodynamic effects or inappropriate hyperventilation
Controlled Mechanical Ventilation (CMV) Assist controlled ventilation (ACV) Synchronized Intermittent Mandatory Ventilation (SIMV) Continuous Positive Airway Pressure (CPAP) Positive End-Expiratory Pressure (PEEP)
Controlled Mechanical Ventilation (CMV) Assist controlled ventilation (ACV) Synchronized Intermittent Mandatory Ventilation (SIMV) Continuous Positive Airway Pressure (CPAP) Positive End-Expiratory Pressure (PEEP)

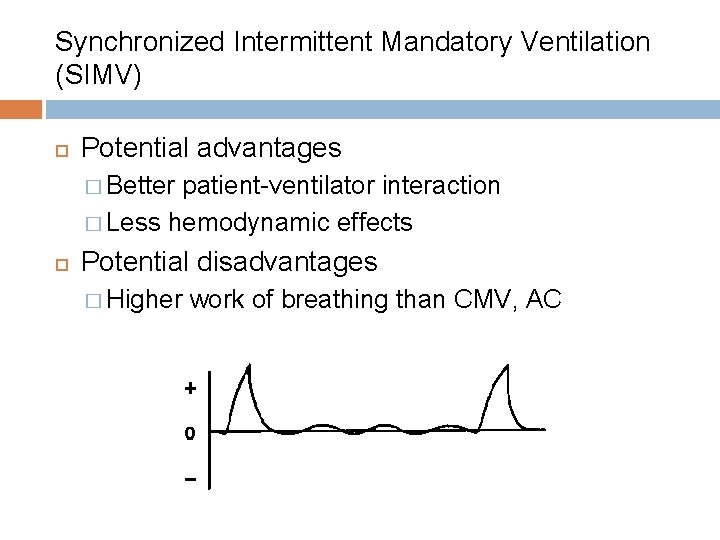
Synchronized Intermittent Mandatory Ventilation (SIMV) Preset tidal volume at a preset rate Additional spontaneous breaths at tidal volume and rate determined by patient Often used with pressure support
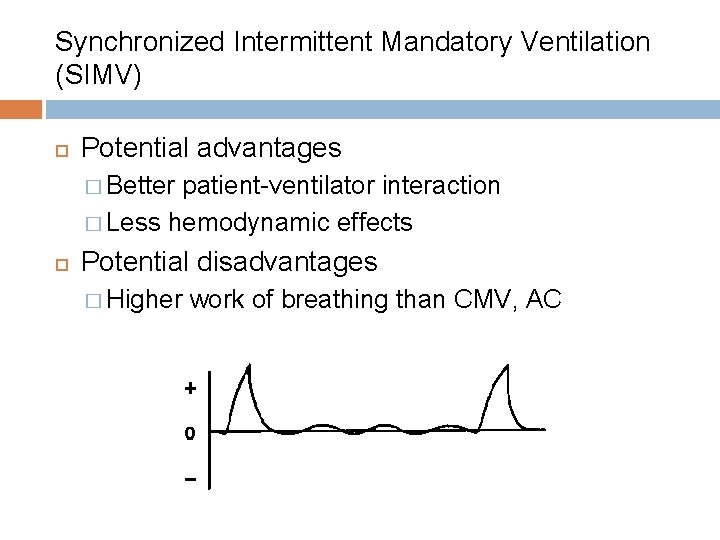
Synchronized Intermittent Mandatory Ventilation (SIMV) Potential advantages � Better patient-ventilator interaction � Less hemodynamic effects Potential disadvantages � Higher work of breathing than CMV, AC

Controlled Mechanical Ventilation (CMV) Assist controlled ventilation (ACV) Synchronized Intermittent Mandatory Ventilation (SIMV) Continuous Positive Airway Pressure (CPAP) Positive End-Expiratory Pressure (PEEP)
Controlled Mechanical Ventilation (CMV) Assist controlled ventilation (ACV) Synchronized Intermittent Mandatory Ventilation (SIMV) Continuous Positive Airway Pressure (CPAP) Positive End-Expiratory Pressure (PEEP)
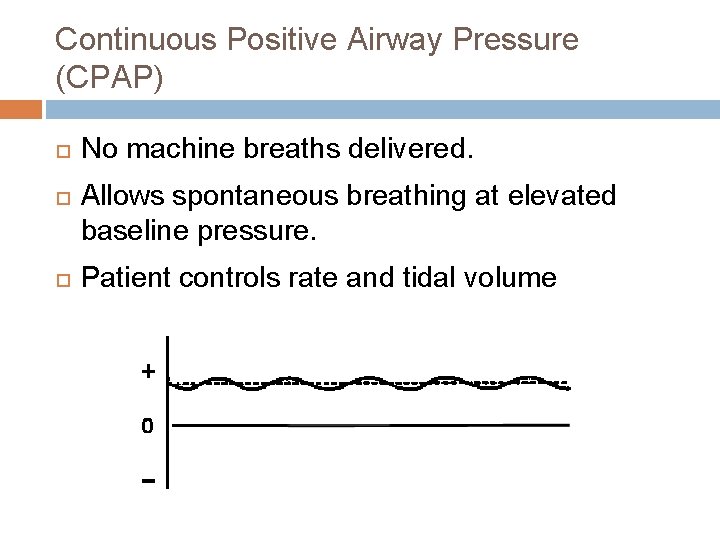
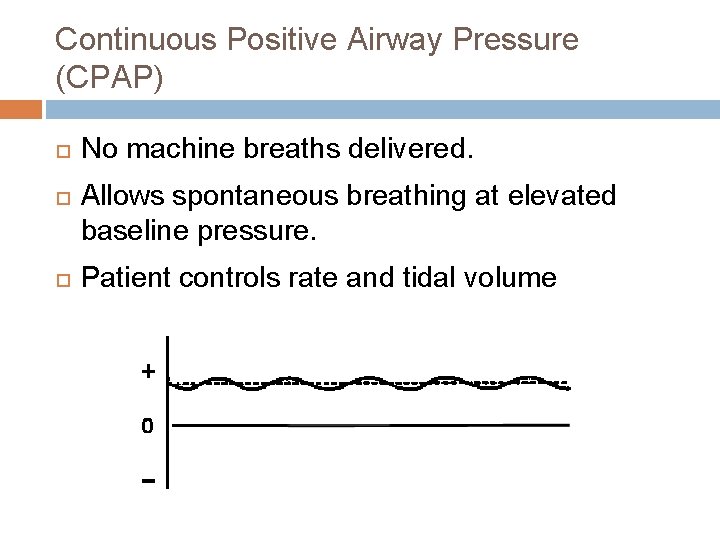
Continuous Positive Airway Pressure (CPAP) No machine breaths delivered. Allows spontaneous breathing at elevated baseline pressure. Patient controls rate and tidal volume
Controlled Mechanical Ventilation (CMV) Assist controlled ventilation (ACV) Synchronized Intermittent Mandatory Ventilation (SIMV) Continuous Positive Airway Pressure (CPAP) Positive End-Expiratory Pressure (PEEP)
Controlled Mechanical Ventilation (CMV) Assist controlled ventilation (ACV) Synchronized Intermittent Mandatory Ventilation (SIMV) Continuous Positive Airway Pressure (CPAP) Positive End-Expiratory Pressure (PEEP)

Positive End-Expiratory Pressure (PEEP). PEEP ventilation provides a pressure above atmospheric at end expiration, preventing alveolar collapse, atelectasis, and increases functional residual capacity (FRC).
Positive End-Expiratory Pressure (PEEP) What is PEEP? What is the goal of PEEP? � Improve � Diminish oxygenation the work of breathing
Positive End-Expiratory Pressure (PEEP) What are the secondary effects of PEEP? � Barotrauma � Diminish cardiac output � Regional hypoperfusion � Na. Cl retention � Hypoxemia
Patient- and Ventilator. Related Problems General Considerations and Troubleshooting Interventions
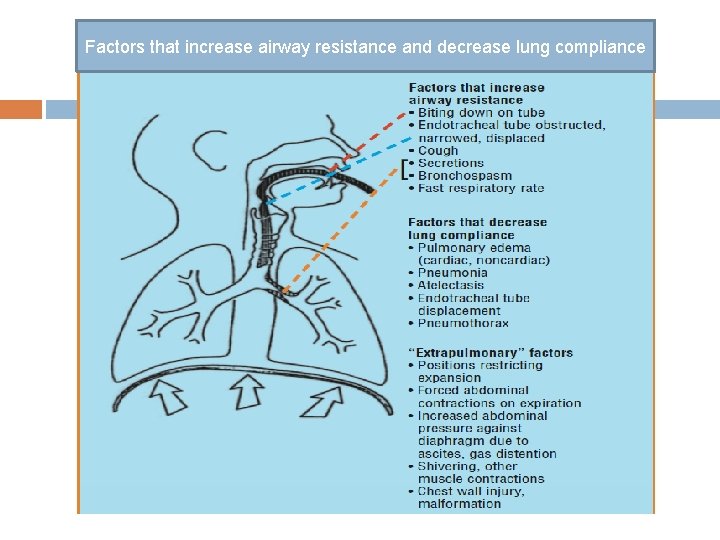
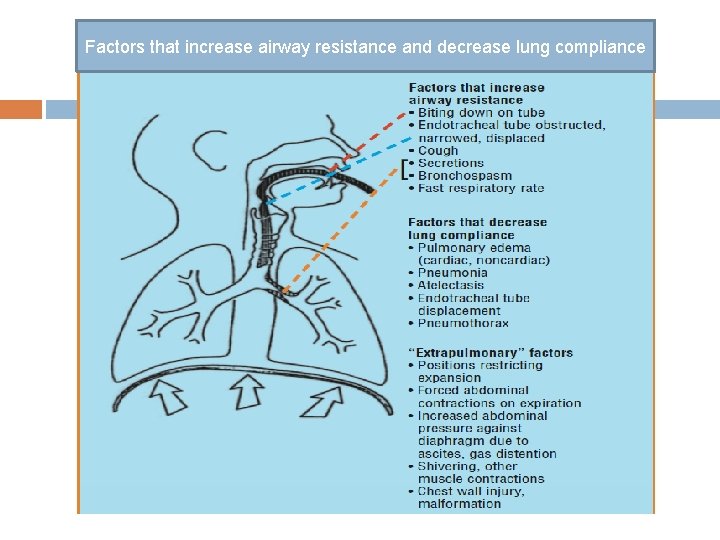
Factors that increase airway resistance and decrease lung compliance
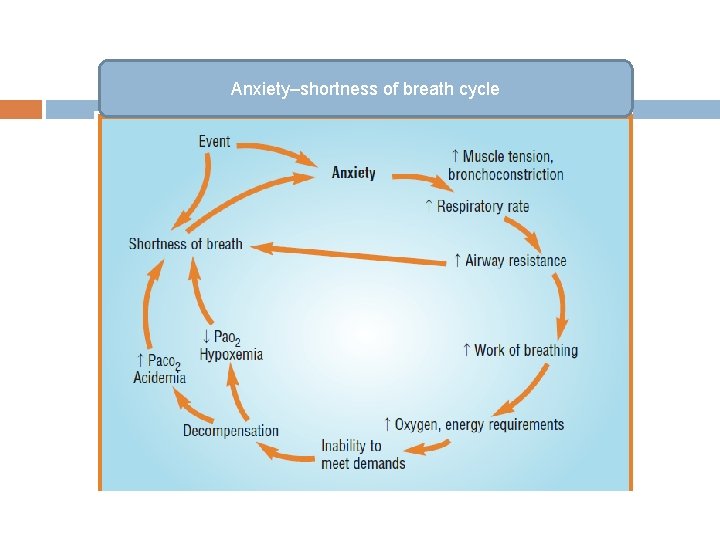
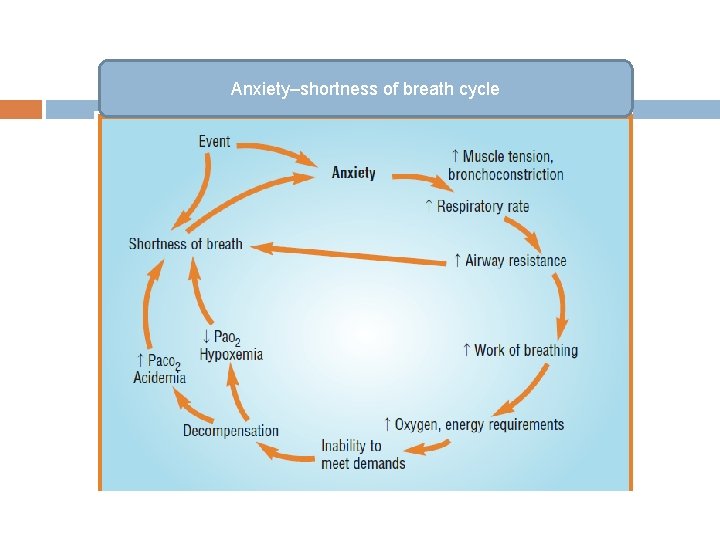
Anxiety–shortness of breath cycle
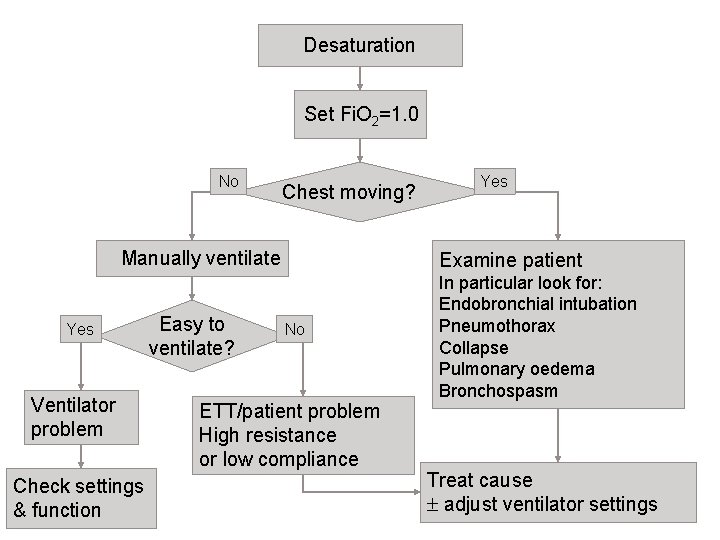
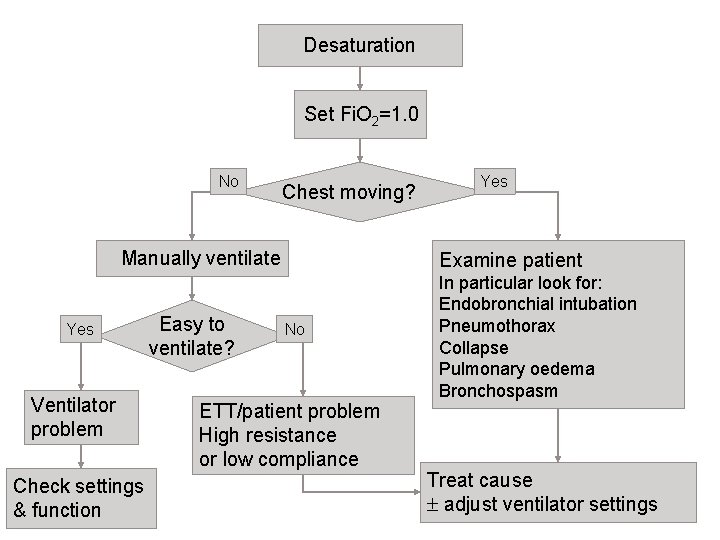
Desaturation Set Fi. O 2=1. 0 No Chest moving? Manually ventilate Yes Ventilator problem Check settings & function Easy to ventilate? Yes Examine patient No ETT/patient problem High resistance or low compliance In particular look for: Endobronchial intubation Pneumothorax Collapse Pulmonary oedema Bronchospasm Treat cause adjust ventilator settings

Thank you

MONITORING & CARE OF PATIENT ON MECHANICAL VENTILATOR
Monitoring & Care of patient on Mechanical Ventilator Nursing care of patients who are being mechanically ventilated requires some special considerations. Ø Some special considerations relate specifically to the type of tube via which the patient is being ventilated (i. e. endotracheal or tracheostomy) and others related to the patient, and the ventilator itself. Ø
Monitoring & Care of patient on Mechanical Ventilator Wash your hands at the beginning of shift, before & after any patient Contact to prevent infection. Inspect Patient Head of Bed Position ( 30º – 45º). Assess the patient Physically & psychologically & Environmental comfort. Communicate with patient while you are providing

Monitoring & Care of patient on Mechanical Ventilator Divide the points of monitoring & Care into five Units: Patient Unit. Ventilator Unit. Hemodynamic or Monitoring systems Unit. Nursing Documentation Unit. Environmental and surrounding Unit.
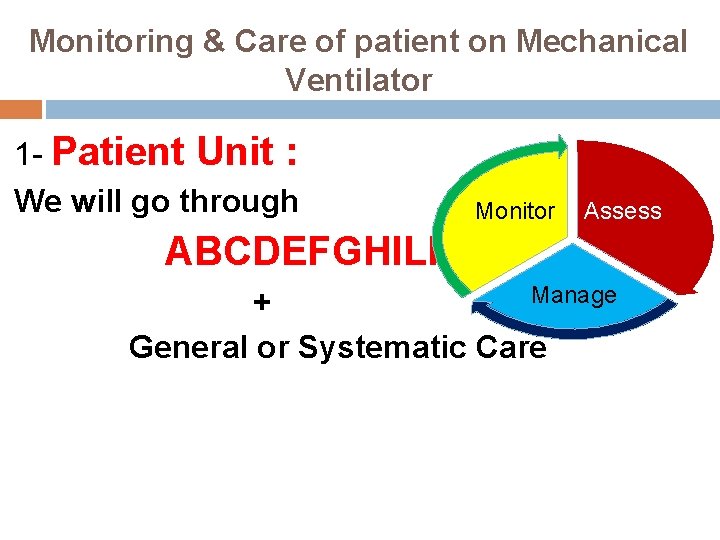
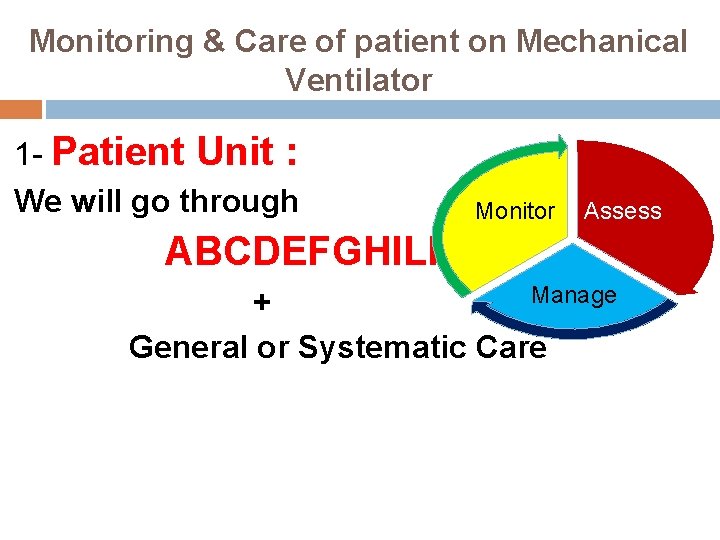
Monitoring & Care of patient on Mechanical Ventilator 1 - Patient Unit : We will go through Monitor Assess ABCDEFGHILPT Manage + General or Systematic Care

ABCDEFGHILPT Approach Monitor Assess A: Airway Manage B: Breathing C: Circulation D: Disablity + Drugs E: Exposure + Electrolytes F: Foley catheter, Fluids , Fluid Balance. G: GIT H: Hematology I: Infection, Infection Control , Infusion L: Lines P: Physiotherapy, Psychotherapy, Peptic Ulcer Prophylaxis, Personal Hygiene T: Thromboembolism
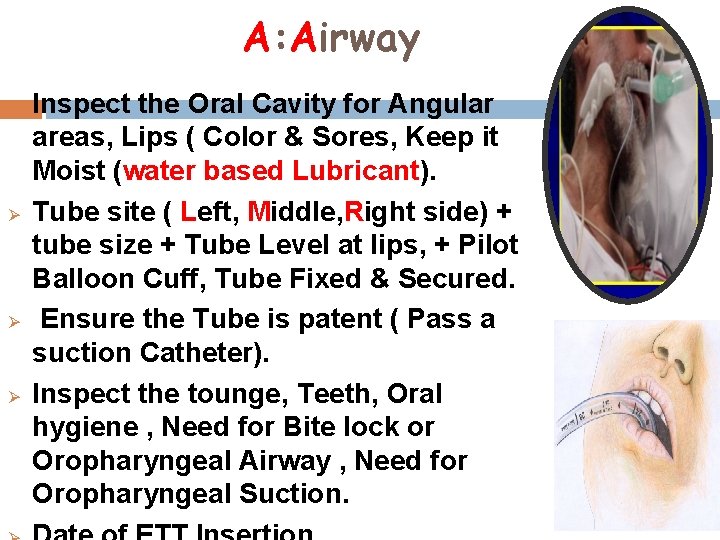
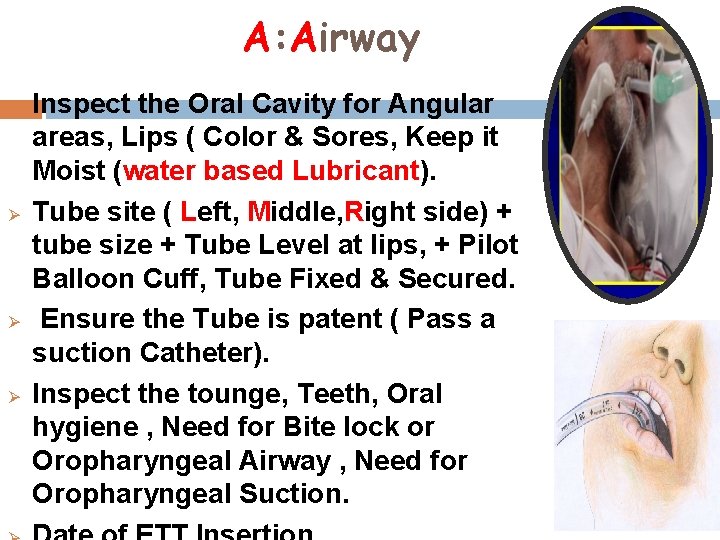
A: Airway Ø Ø Inspect the Oral Cavity for Angular areas, Lips ( Color & Sores, Keep it Moist (water based Lubricant). Tube site ( Left, Middle, Right side) + tube size + Tube Level at lips, + Pilot Balloon Cuff, Tube Fixed & Secured. Ensure the Tube is patent ( Pass a suction Catheter). Inspect the tounge, Teeth, Oral hygiene , Need for Bite lock or Oropharyngeal Airway , Need for Oropharyngeal Suction.
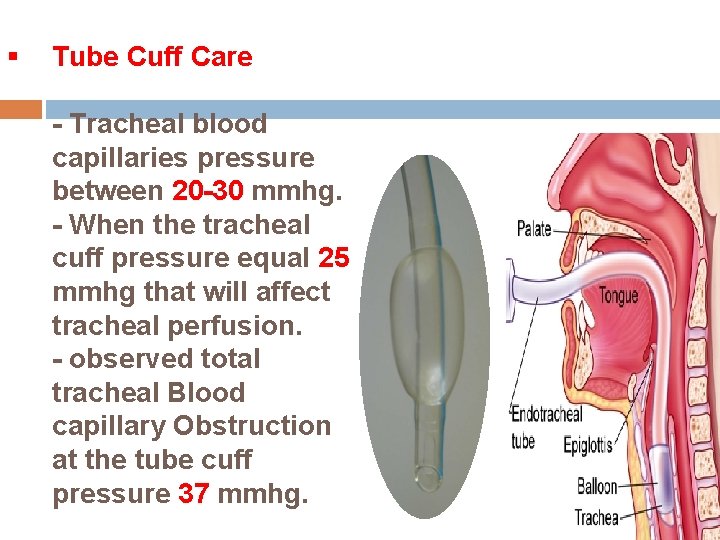
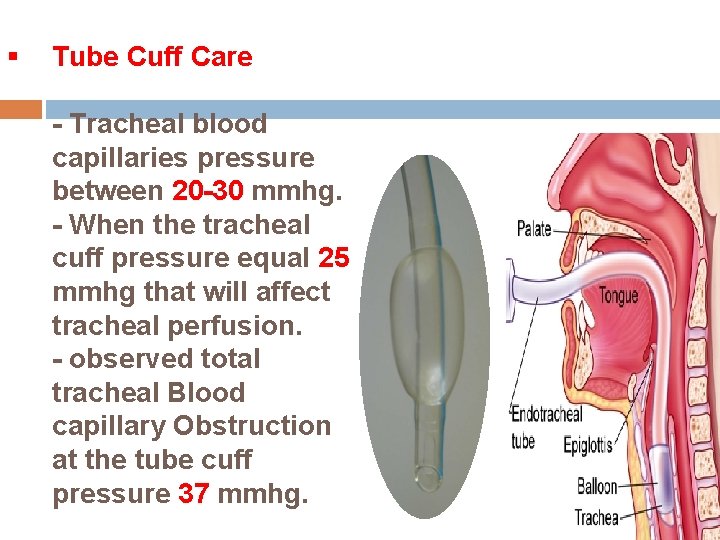
§ Tube Cuff Care - Tracheal blood capillaries pressure between 20 -30 mmhg. - When the tracheal cuff pressure equal 25 mmhg that will affect tracheal perfusion. - observed total tracheal Blood capillary Obstruction at the tube cuff pressure 37 mmhg.

So. . The Cuff balloon pressure should not exceed 25 mmhg , keep it between 20 -25 mmhg. If high pressure Tracheal stenosis Cuff pressure: If insufficient- Leak Displacement of the tube Aspiration

Oral Care Oral care should be done every 2 hours or when indicated. Solution for oral care Hydrogen peroxide 1. 5%. You can also use a brush tooth with Hydrogen peroxide 1. 5%. if possible. Decrease the risk of VAP.

Endotracheal or Tracheostomy Tube Suctioning Closed Suctioning: Open Suctioning Disconnection from the ventilator v Not recommended when PEEP >10 v Facilitate continuous mechanical ventilation and oxygenation during the suctioning. v Indicated when PEEP level above v

A: Airway § § § In patient with tracheostomy Look for: Date of Tracheostomy Insertion Stoma Site (Dilation, Infection) tube Patency pilot balloon Cuff pressure Tube Fixed & Secured Tracheal secretions & Need for Suctioning or tracheal secretion specimen Need for Tube Or Tie Dressing Pt Not distressed Ensure the ETT or Trach tube was Connected properly to the Ventilator. Optimum Oxygenation &

B: Breathing Perform a simple chest Examination ( Look – Listen – Feel ). Document any abnormal Sounds ( Wheeze, Crackles, Gurgling. . Etc. Treat the underlying Problem. Call for Help. Monitor the Oxygenation & Ventilation Status. ( SPO 2 , ABG, Caponography).

Confirmation of the Tube & Adequate Air Entry Bilaterally 3 -4 cm

Conditions Affecting Accuracy Patient conditions Carboxyhemoglobin Erroneously high reading may present Anemia Values as low as 5 g/dl may result in 100% Sp. O 2 Hypovolemia/Hypotension: May not have adequate perfusion to be detected by oximetry Hypothermia: peripheral vasoconstriction may prevent oximetry detection

Patient Environments may Affect Accuracy Ambient Light � Any external light exposure to capillary bed where sampling is occurring may result in an erroneous reading � Excessive Motion � Always compare the palpable pulse rate with the pulse rate indicated on the pulse oximetry �

Fingernail polish and pressed on nails � Most commonly use nails and fingernail polish will not affect pulse oximetry accuracy � Some shades of blue, black and green may affect accuracy (remove with acetone pad) � Skin pigmentation � Apply sensor to the fingertips of darkly pigmented patients �

Different Pulse Oximetry

C = CIRCULATION HR + 12 lead Baseline ECG BP … MAP , CVP Extremities (Temp). Capillary refill IV Access Central + Peripheral Fluids, Inotropes? UOP LOC
E = ELECTROLYTES, Exposure Na K Ca Mg PO 4

F = Foley Catheter FLUIDS, Fluid Balance

G = GIT Feeding? NGT / PEG? Bowel sounds ? Absorption? Adequate calories? Laxatives? Bowel motions? + IV fluids? RBS
H = HAEMATOLOGY Hb : > 8 g/dl … > 10 g/dl with CVS problem PCV Plt count INR

I = INFECTION Infection Control Infusion Temp. TWBCs CRP … Source Control


L = LINES How long? Infection? Complication s?

P: PHYSIOTHERAPY

P: Peptic Ulcer Prophylaxis P: Patient Personal Hygiene
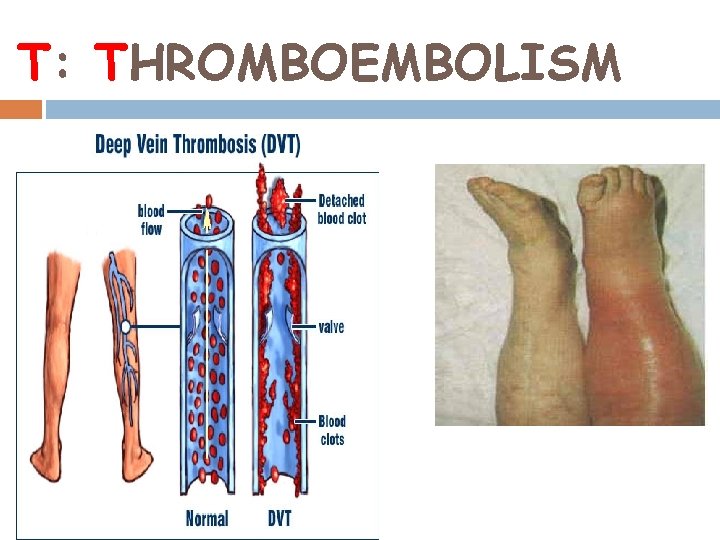
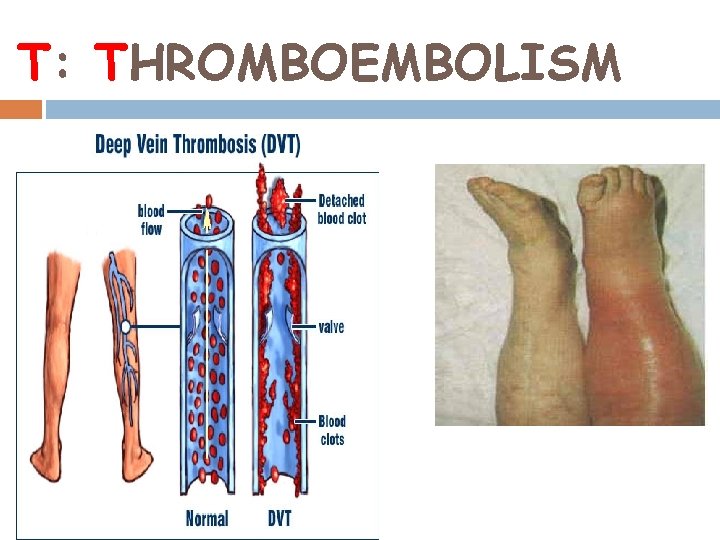
T: THROMBOEMBOLISM
P: PSYCHOTHERAPY
References 1. Huang YT, Singh, J. Basic modes of mechanical Ventilation 2. Pierson DJ. A primer on mechanical ventilation. 2008. http: //courses. washington. edu/med 610/mechanica lventilation/mv_primer 3. Burns SM. Mechanical ventilation and weaning. 4. Chatburn RJ. Classification of ventilator Modes 5. Mac. Intyre NR, Branson, RD. Mechanical Ventilation. 2 nd ed. Philadelphia 6. Mac. Intyre NR. Controversies in mechanical ventilation.
 Fungsi dexcom
Fungsi dexcom Actual mechanical advantage vs ideal mechanical advantage
Actual mechanical advantage vs ideal mechanical advantage Major details
Major details Seal support system
Seal support system Introduction to content management
Introduction to content management Intro to hrm
Intro to hrm Project management overview
Project management overview Gym management dashboard
Gym management dashboard Forrester wave real time interaction management
Forrester wave real time interaction management Gambaran
Gambaran Peta konsep manajemen ekonomi
Peta konsep manajemen ekonomi Overview of financial management
Overview of financial management Multinational financial management meaning
Multinational financial management meaning Chapter 1 an overview of financial management
Chapter 1 an overview of financial management Overview of financial management
Overview of financial management 7 habits diabetes self-management and support
7 habits diabetes self-management and support Overview of transcription and translation
Overview of transcription and translation Data cleaning problems and current approaches
Data cleaning problems and current approaches Chapter 17 elements and their properties answer key
Chapter 17 elements and their properties answer key Chicago time
Chicago time Multicullar
Multicullar An overview of data warehousing and olap technology
An overview of data warehousing and olap technology Data quality and data cleaning an overview
Data quality and data cleaning an overview Data quality and data cleaning an overview
Data quality and data cleaning an overview Overview of storage and indexing
Overview of storage and indexing Elements and their properties section 1 metals
Elements and their properties section 1 metals Scientific management
Scientific management Management pyramid
Management pyramid Top management middle management first line management
Top management middle management first line management Dr ocker
Dr ocker Management support definition
Management support definition Knowledge management decision support
Knowledge management decision support Cease meaning
Cease meaning Compare and contrast mechanical and chemical weathering
Compare and contrast mechanical and chemical weathering Mechanical and chemical weathering venn diagram
Mechanical and chemical weathering venn diagram Www stands for world wide web
Www stands for world wide web Maximo overview
Maximo overview Universal modeling language
Universal modeling language In uml is a connection among things
In uml is a connection among things Vertical retail
Vertical retail Figure 12-1 provides an overview of the lymphatic vessels
Figure 12-1 provides an overview of the lymphatic vessels Systemic circulation flow chart
Systemic circulation flow chart Texas public school finance overview
Texas public school finance overview Walmart company overview
Walmart company overview Stylistic overview of architecture
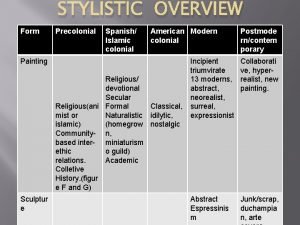
Stylistic overview of architecture Sa sd
Sa sd Spring framework overview
Spring framework overview Nagios tactical overview
Nagios tactical overview Market overview managed file transfer solutions
Market overview managed file transfer solutions Sdn nfv overview
Sdn nfv overview Sbic program
Sbic program Goods receipt note
Goods receipt note Sap ariba overview
Sap ariba overview Safe overview
Safe overview Rfid technology overview
Rfid technology overview Review paper introduction
Review paper introduction Example of a project title
Example of a project title Major systemic arteries labeled
Major systemic arteries labeled Is abstract a summary
Is abstract a summary Solvency ii pillar iii
Solvency ii pillar iii Physical storage devices
Physical storage devices Overview of education in health care
Overview of education in health care Overview funding programmes
Overview funding programmes Ospf overview
Ospf overview Onap architecture
Onap architecture Oedipus rex family tree
Oedipus rex family tree Cisco show top talkers
Cisco show top talkers Overview on the national tuberculosis elimination programme
Overview on the national tuberculosis elimination programme Mpls header format
Mpls header format Azure overview
Azure overview Master data services overview
Master data services overview Overview of cellular respiration
Overview of cellular respiration Overview of aerobic respiration
Overview of aerobic respiration Cellular respiration
Cellular respiration Total atp produced in cellular respiration
Total atp produced in cellular respiration Transformer overview
Transformer overview Kaizen prioritization
Kaizen prioritization Itil brief overview
Itil brief overview Iptv technology
Iptv technology Overview of mobile computing
Overview of mobile computing Microprocessor topics for presentation
Microprocessor topics for presentation Weakness of kfc
Weakness of kfc Sap
Sap Huawei company overview
Huawei company overview Eylf meaning
Eylf meaning Sap erp system overview
Sap erp system overview Sql server master data services example
Sql server master data services example Cuda overview
Cuda overview Counterfeit electronic components an overview
Counterfeit electronic components an overview Conclusion of accounting software
Conclusion of accounting software Generations overview
Generations overview Collections overview in java
Collections overview in java Dr korson
Dr korson Section 8-2 photosynthesis an overview
Section 8-2 photosynthesis an overview Chapter 24 trauma overview
Chapter 24 trauma overview Arteries of abdomen
Arteries of abdomen Chapter 14 medical overview
Chapter 14 medical overview Overview of the major systemic arteries
Overview of the major systemic arteries Badminton serving rules
Badminton serving rules