Overview of Health Issues for Children with PWS






- Slides: 34
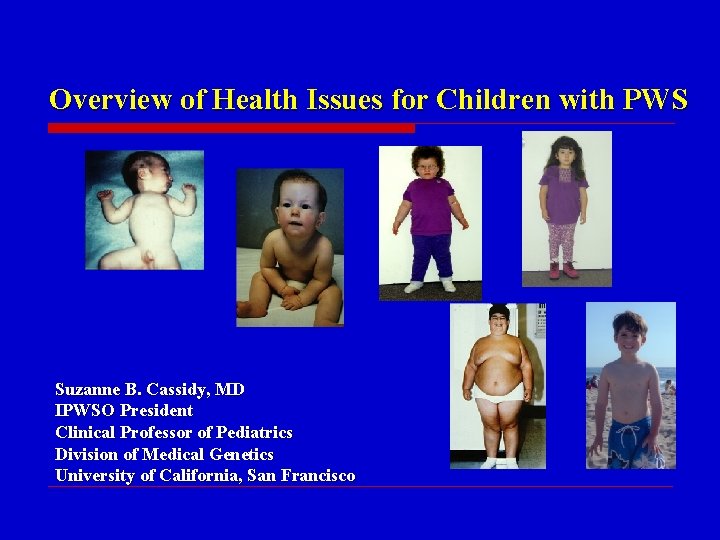
Overview of Health Issues for Children with PWS Suzanne B. Cassidy, MD IPWSO President Clinical Professor of Pediatrics Division of Medical Genetics University of California, San Francisco
Discussion of Problems • Many positive aspects to people with PWS • This presentation relates to difficulties • Few well-controlled studies • • Different doctors may approach problems differently My information based on >30 years directing PWS clinics and conducting clinical research, the medical literature, and discussions with other experts
PWS is Highly Variable • Syndrome = a collection of features that are found together more often than by chance alone • • • Not every affected individual has every finding The severity of each finding in PWS is quite variable The severity of one finding does not determine the severity of other findings Other family characteristics and life experience can influence appearance, abilities and behavior People with PWS can have problems or features unrelated to PWS

The Course in PWS Has Changed • • • Diagnosis occurs at much younger ages Many issues recognized earlier and treatment started Growth hormone has made a big difference in some aspects Much more knowledge of health issues and how to address them Much more educational materials for families and health care providers And it will be different in the future • Cannot judge the future by the present
Age-Focused Approach • • Newborn (<1 mo) Infancy (1 mo. – 1 year) Early childhood (1 – 5 years) Late childhood (5 -13 years) • Most issues span more than one period
Health Issues in Newborns (< 1 month) • • • Hypotonia and its consequences Lethargy Sometimes issues related to delivery problems • Prematurity/postmaturity
Hypotonia of PWS • Hypotonia = low muscle tone, low resistance to gravity • • Present in ~100%; Most consistent feature of PWS Abnormal brain signals to muscle, not a muscle abnormality Evident prenatally • • • Manifests as decreased movement and weak suck Decreased fetal movement Abnormal delivery position and timing Frequent need for assisted delivery (Cesarean common) Severe hypotonia lasts weeks to months Gradually improves, but doesn’t resolve completely
Consequences of Neonatal Hypotonia • Poor suckling • Unable to breast feed, weak suck on bottle • Frequent need for nasogastric tube (gavage) feeding for weeks to months • Slow feeding thereafter • Failure-to-thrive • Decreased movement • Increases likelihood of altered head shape • Weak cough, increased pneumonia risk • Increased congenital hip abnormalities (10 -20%)
Other Findings in Newborns • Lethargy; poor arousal • Weak cry • Sometimes hypothermia

Management of Hypotonia in the Newborn • • No medication shown to treat hypotonia directly Compensate for poor suck • • • Gavage feeding, special nipples; gastrostomy tube usually not needed Assure adequate caloric intake by following growth closely Frequent feeding of small quantities if taking orally • • • Support cheeks Awaken to feed, if needed Avoid nipple feeding longer than 20 minutes Doctor should check for hip dislocation, treat if present Refer to services for physical and occupational therapy, if available Parents should interact and stimulate baby despite sleepiness and quietness
Health Issues in Infants (1 month-1 year) • Hypotonia slowly improving • • • Squint is common Undescended testicles in males (80%-90%) Scoliosis is common (40% – 80%) • • • Feeding issues often still present, may last months Motor delays become evident Can occur any time throughout childhood Gastroesophageal reflux may be present Growth deficiency may become apparent Sleep apnea in some Hypothermia or fever of unknown origin occasionally
Management of Health Issues in Infants • Hypotonia and feeding difficulties • Growth and weight-to-height should be monitored frequently (monthly) by doctor, nurse or dietician • • • Calorie intake adjusted accordingly, volume and/or calorie density Gavage feeding until nippling well, taking feedings under 20 minutes Or move directly to cup and spoon Continue physical therapy and developmental stimulation Lots of interaction with parents, siblings Check thyroid function if hypotonia not improving significantly with time

A Word on Supplements • Some families have given supplements to their child with PWS • • Co. Q 10, Carnitine, and Fish Oil Involved in energy metabolism • Some see improvement in hypotonia, motor development, and/or energy; Others don’t • • No evidence of deficiency of these in PWS No well-controlled studies showing benefit or harm • Some specialists recommend them, others don’t • • Discuss with doctor Assess benefit
Management in Infants • Ophthalmologist evaluation for squint • • • Doctor to assess testicular position • • Squint treated with patching or surgery Regular (annual) ophthalmology visits thereafter Refer within the first year for hormonal and/or surgical treatment if undescended Doctor to clinically evaluate for scoliosis • Refer to orthopedist if present
Management in Infants (cont. ) • Assessment for GE reflux • • Spitting up/vomiting with discomfort or crying, breathing problems of any kind (gagging, choking, coughing, wheezing, or pneumonia due to aspiration) If present, doctor to evaluate and treat • • Treated with adjustments to feedings, medication and/or surgery Discussion of growth hormone in PWS with doctor or specialist • • Appropriate to start treatment in the first few months of life Sleep study before starting
Sleep and PWS (all ages) • Increase in sleep apnea (pauses in breathing) and other sleep alterations • • Risk for sleep apnea increased by • • • Central sleep apnea vs. obstructive sleep apnea Young age Severe hypotonia Prior respiratory problems Severe obesity Recommend formal sleep study in all • Strongly recommended before GH treatment • • GH treatment may increase tonsil & adenoid size before throat size Can be treated, as in general population • Tonsillectomy, Continous Positive Airway Pressure (CPAP), or other

Health Issues in Early Childhood (1 -5 years) • • Weight and onset of hyperphagia (excess eating) Growth Visual acuity (eyesight) Scoliosis Sleep problems Decreased saliva and dental problems Constipation Hypothyroidism
Weight Problems in PWS • 3 major causes of tendancy toward excess weight in people with PWS: 1. Altered brain perception of having eaten enough (satiety) 2. Decreased requirement for calories • Probably related to hypotonia, decreased activity and short stature 3. High threshold for vomiting and decreased pain perception, leading to eating large quantities without discomfort
Hyperphagia • Onset of excessive appetite (hyperphagia) between 1 and 6 years of age, often later • • • Nearly constant food seeking, variable intensity Present regardless of weight Physiological mechanism causing hyperphagia still unclear • • Currently no proven effective direct treatment Subject of much research and drug development efforts
Obesity in PWS • • • If uncontrolled externally, drive to eat excessively leads to obesity Obesity is the major cause of medical problems and death in people with PWS Impact of obesity in early childhood: • • Slows motor development Respiratory problems, if severe Sleep apnea Choking due to eating too fast (esp. hot dogs/sausages!) • • Is a cause of death in PWS at any age Social problems

Treatment of Obesity in PWS • No currently available safe drug known to decrease urge to eat • Surgery • • High rate of complications and low rate of long term weight loss • No long-term studies on newer techniques Prevention and Management of obesity • • • Low calorie diet (work with dietician, adjust to level of activity) Lots of physical activity Food security (environmental control) • • • Lock kitchen; constant supervision, no high calorie foods in the home, compensate for “indiscretion” Consistent limits, consistently enforced Important role for growth hormone
Management of Other Issues in Infancy • • Decreased saliva may increase risk for dental problems, predispose to choking on food, and contribute to speech problems • • Encourage liquids Arrange visit to dentist no later than age 3 years, preferably earlier • • At least twice yearly thereafter In later years, special toothpaste, gel, or mouthwash to increase saliva flow Constipation • • Very common problem, probably related to intestinal hypotonia Should be treated aggressively throughout life • • Dietary changes, softening agents, increased fiber intake, liquids Medications in later years
Management of Other Issues in Infancy • Hypothyroidism (low thyroid hormone production) • • • Present in 10%-20% of people with PWS Can occur at any age Can lead to prolonged hypotonia Screen annually If present, treat with standard dose (a small thyroid hormone pill)
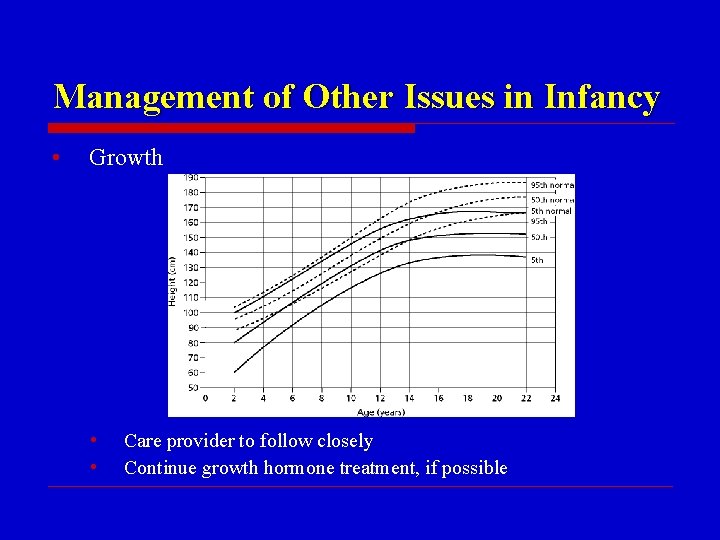
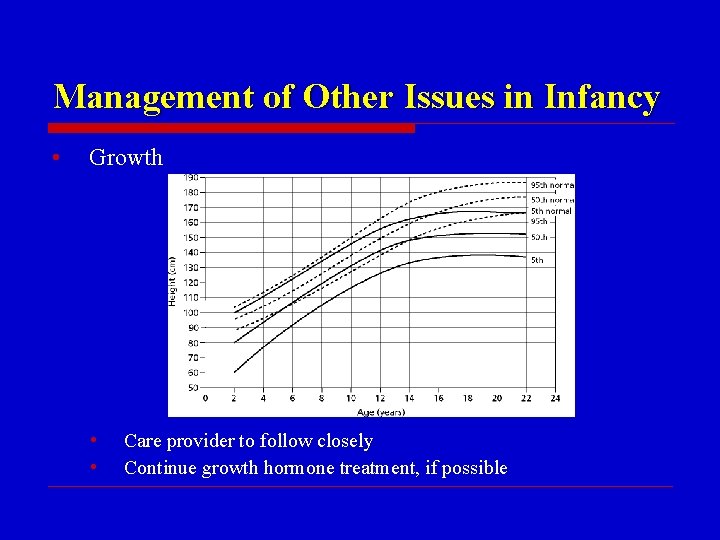
Management of Other Issues in Infancy • Growth • • Care provider to follow closely Continue growth hormone treatment, if possible
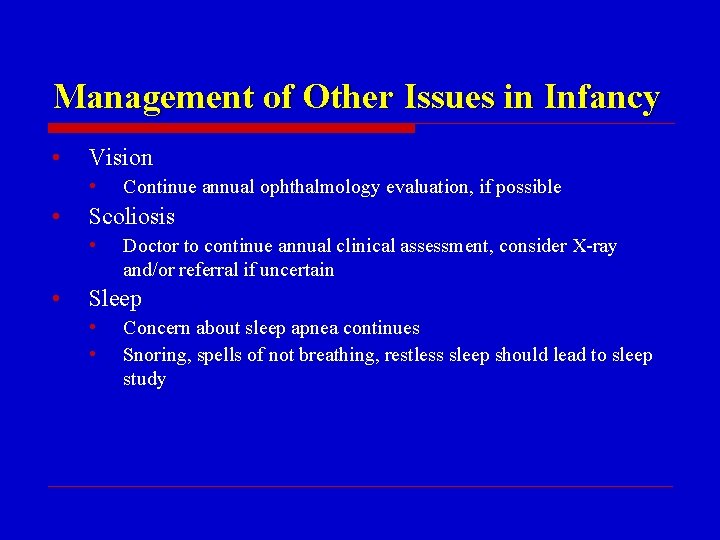
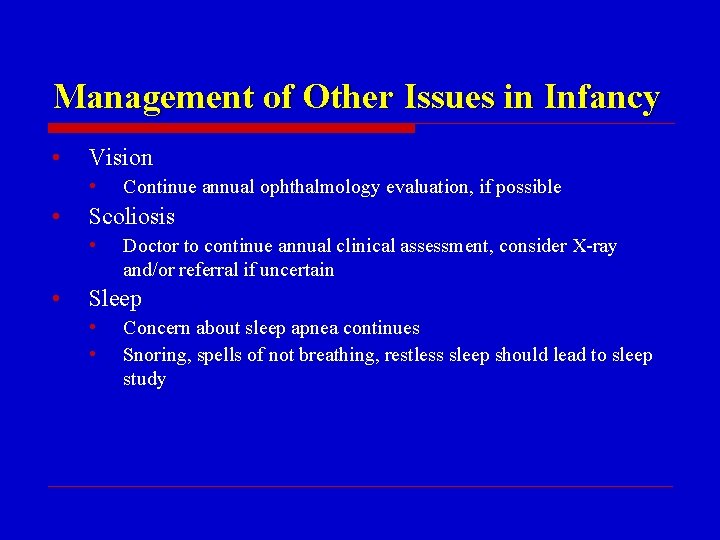
Management of Other Issues in Infancy • Vision • • Scoliosis • • Continue annual ophthalmology evaluation, if possible Doctor to continue annual clinical assessment, consider X-ray and/or referral if uncertain Sleep • • Concern about sleep apnea continues Snoring, spells of not breathing, restless sleep should lead to sleep study
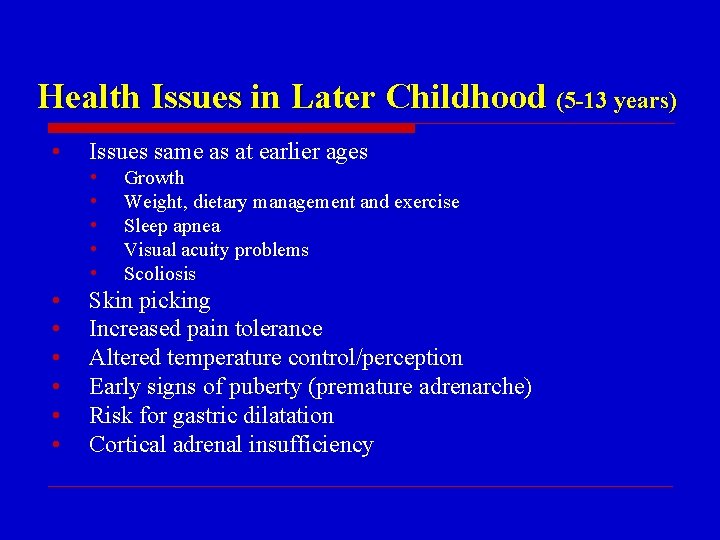
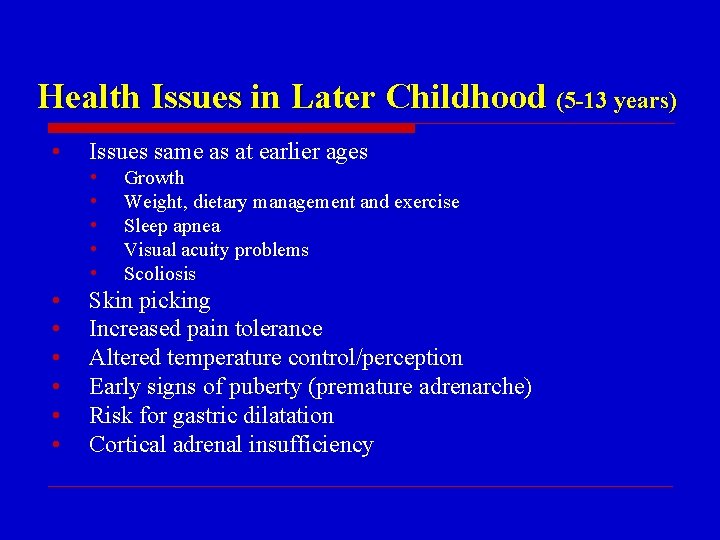
Health Issues in Later Childhood (5 -13 years) • Issues same as at earlier ages • • • Growth Weight, dietary management and exercise Sleep apnea Visual acuity problems Scoliosis Skin picking Increased pain tolerance Altered temperature control/perception Early signs of puberty (premature adrenarche) Risk for gastric dilatation Cortical adrenal insufficiency
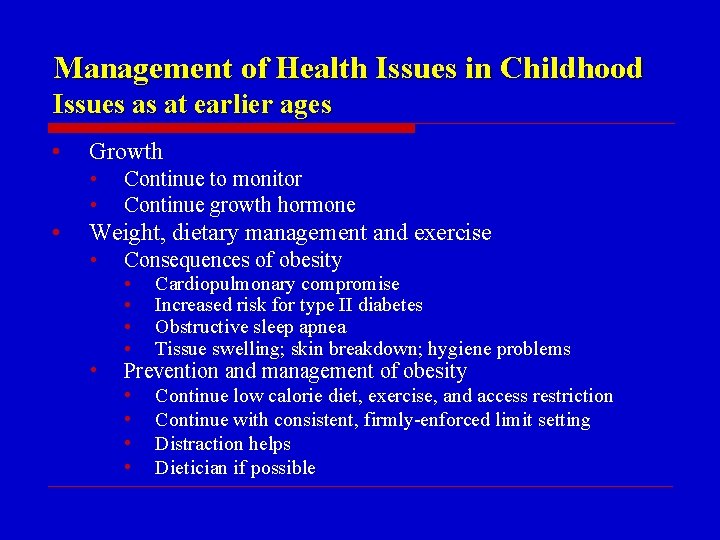
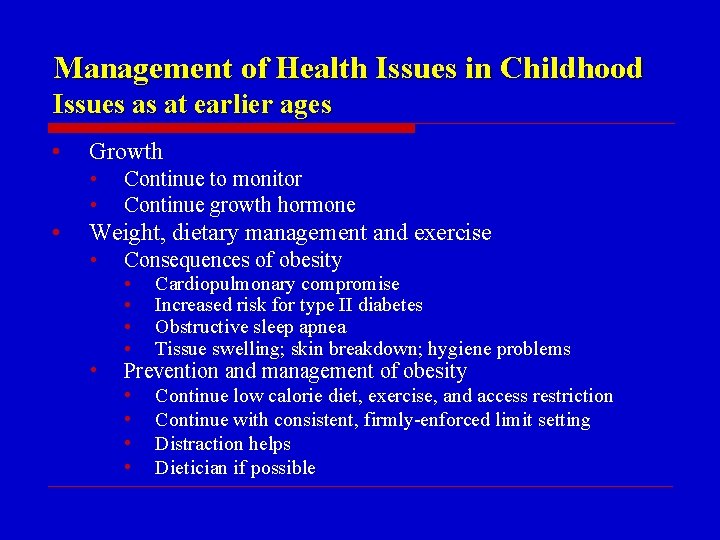
Management of Health Issues in Childhood Issues as at earlier ages • Growth • • • Continue to monitor Continue growth hormone Weight, dietary management and exercise • Consequences of obesity • Prevention and management of obesity • • Cardiopulmonary compromise Increased risk for type II diabetes Obstructive sleep apnea Tissue swelling; skin breakdown; hygiene problems • • Continue low calorie diet, exercise, and access restriction Continue with consistent, firmly-enforced limit setting Distraction helps Dietician if possible
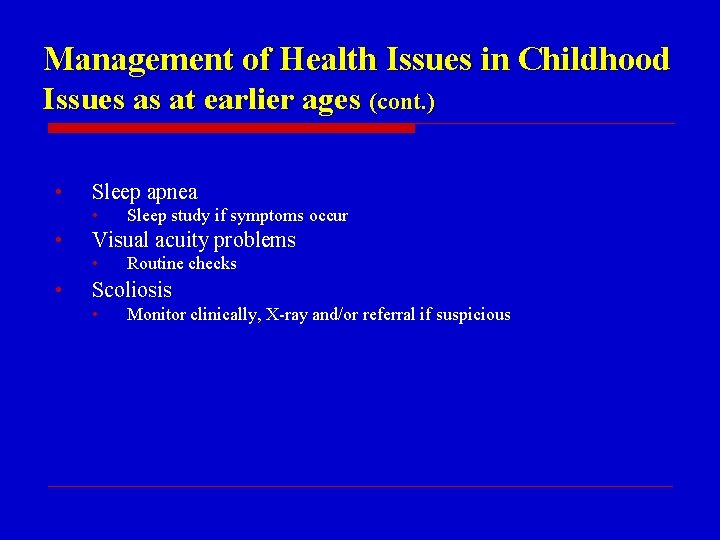
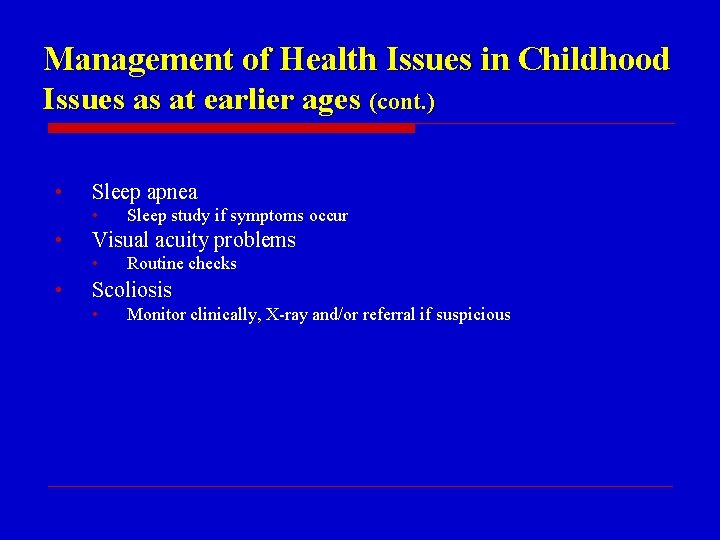
Management of Health Issues in Childhood Issues as at earlier ages (cont. ) • Sleep apnea • • Visual acuity problems • • Sleep study if symptoms occur Routine checks Scoliosis • Monitor clinically, X-ray and/or referral if suspicious
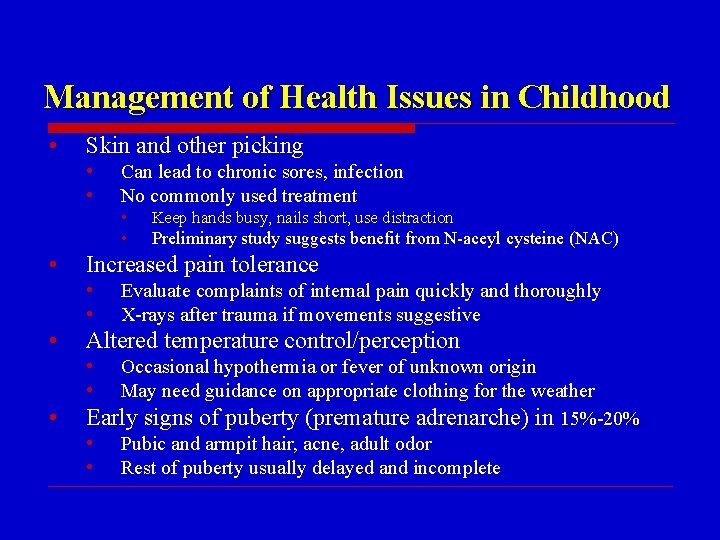
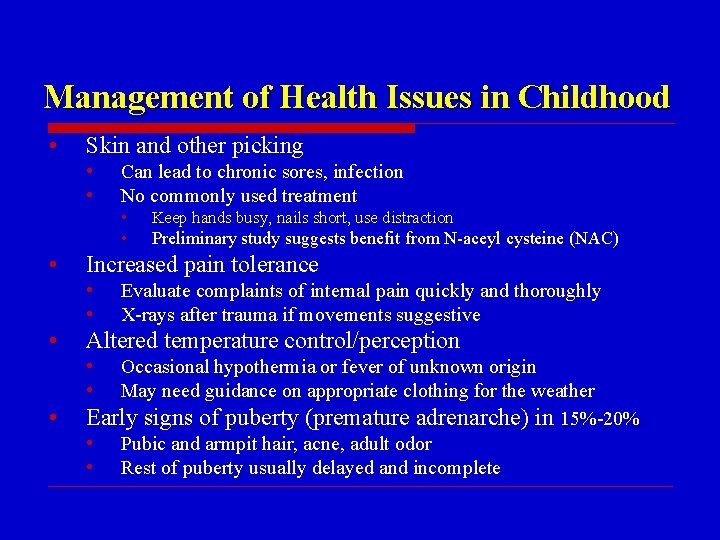
Management of Health Issues in Childhood • Skin and other picking • • • Keep hands busy, nails short, use distraction • Preliminary study suggests benefit from N-aceyl cysteine (NAC) Evaluate complaints of internal pain quickly and thoroughly X-rays after trauma if movements suggestive Altered temperature control/perception • • Increased pain tolerance • • • Can lead to chronic sores, infection No commonly used treatment Occasional hypothermia or fever of unknown origin May need guidance on appropriate clothing for the weather Early signs of puberty (premature adrenarche) in 15%-20% • Pubic and armpit hair, acne, adult odor • Rest of puberty usually delayed and incomplete
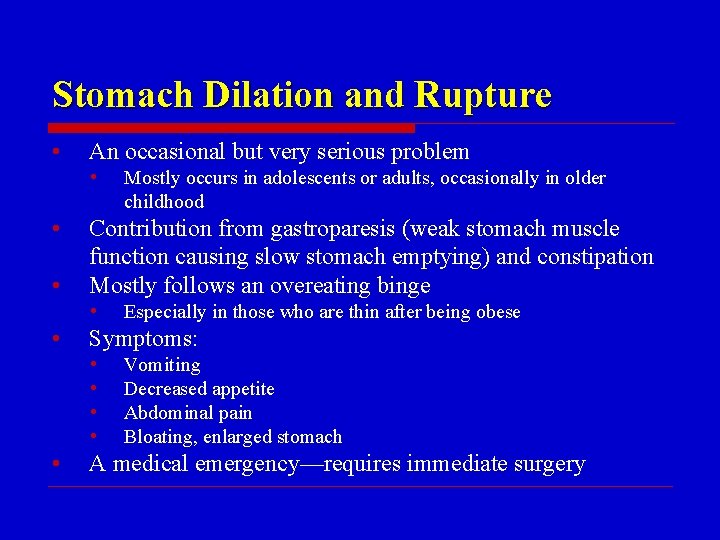
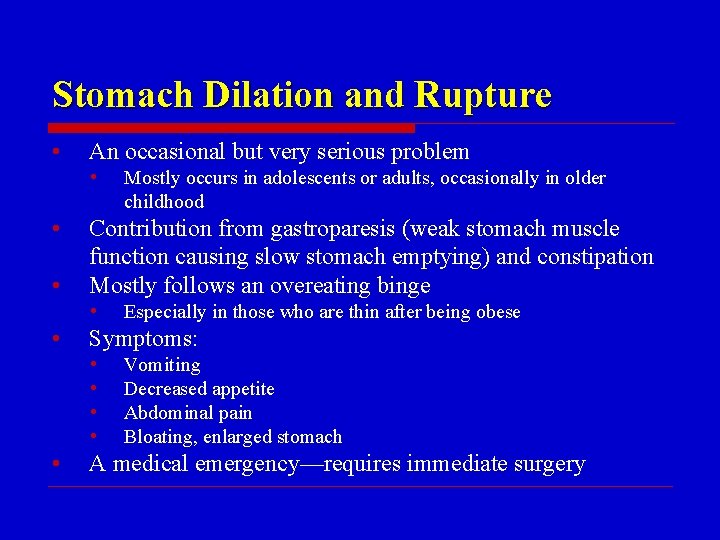
Stomach Dilation and Rupture • An occasional but very serious problem • • • Contribution from gastroparesis (weak stomach muscle function causing slow stomach emptying) and constipation Mostly follows an overeating binge • • Especially in those who are thin after being obese Symptoms: • • • Mostly occurs in adolescents or adults, occasionally in older childhood Vomiting Decreased appetite Abdominal pain Bloating, enlarged stomach A medical emergency—requires immediate surgery
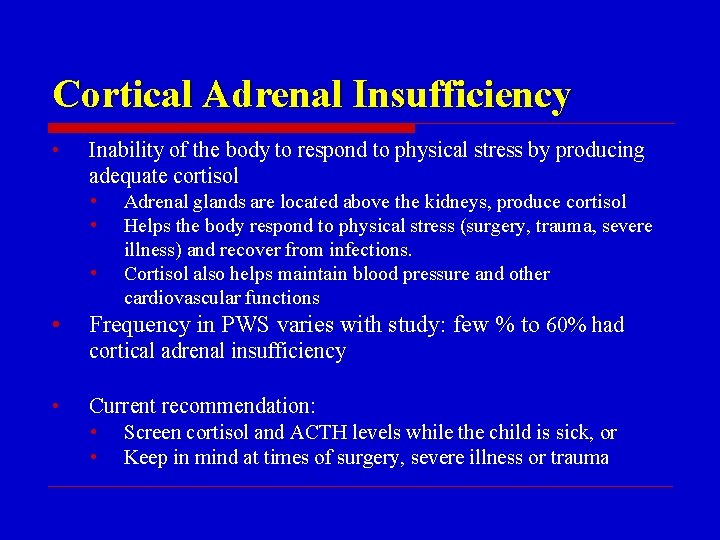
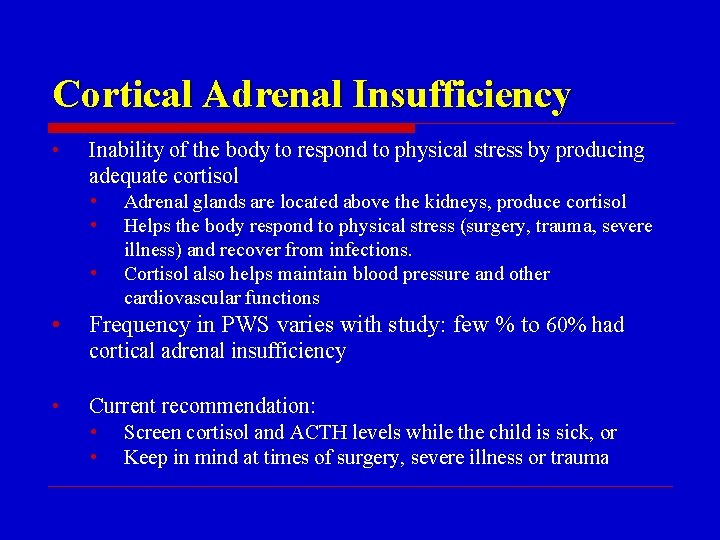
Cortical Adrenal Insufficiency • Inability of the body to respond to physical stress by producing adequate cortisol • • Adrenal glands are located above the kidneys, produce cortisol Helps the body respond to physical stress (surgery, trauma, severe illness) and recover from infections. Cortisol also helps maintain blood pressure and other cardiovascular functions Frequency in PWS varies with study: few % to 60% had cortical adrenal insufficiency • Current recommendation: • Screen cortisol and ACTH levels while the child is sick, or • Keep in mind at times of surgery, severe illness or trauma
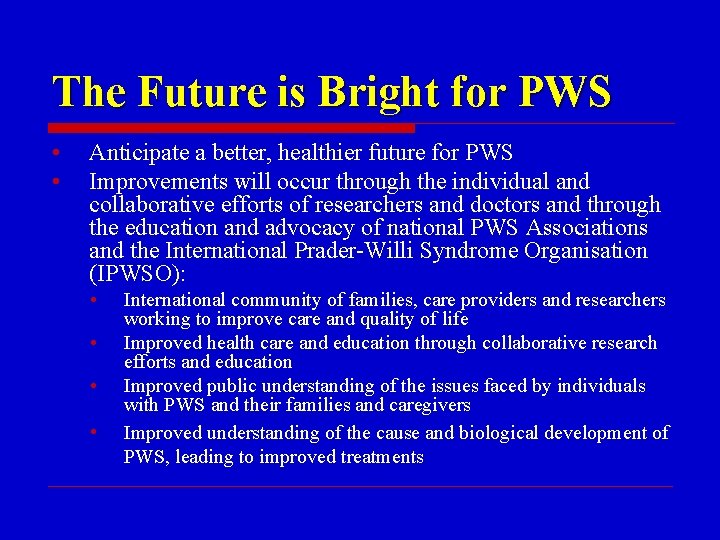
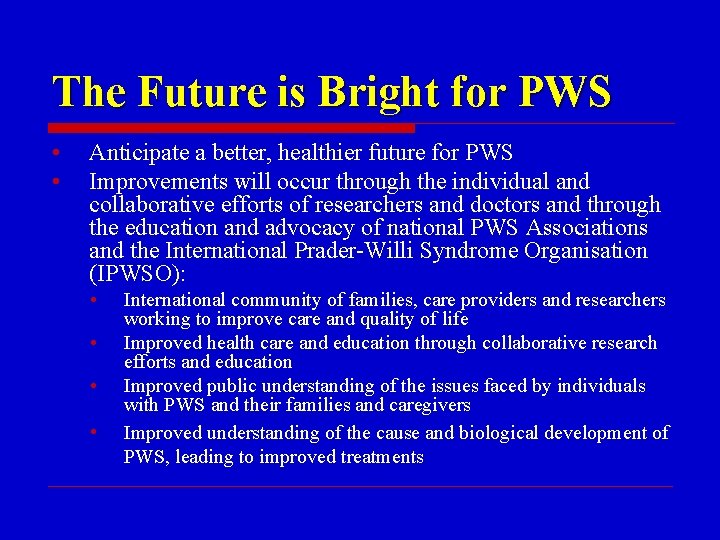
The Future is Bright for PWS • • Anticipate a better, healthier future for PWS Improvements will occur through the individual and collaborative efforts of researchers and doctors and through the education and advocacy of national PWS Associations and the International Prader-Willi Syndrome Organisation (IPWSO): • • International community of families, care providers and researchers working to improve care and quality of life Improved health care and education through collaborative research efforts and education Improved public understanding of the issues faced by individuals with PWS and their families and caregivers Improved understanding of the cause and biological development of PWS, leading to improved treatments
How You Can Help • • • Keep updated through your country organization (PWSAI) and through IPWSO Participate in research when asked, to move knowledge forward Please, do not forget those less fortunate who live in countries where knowledge, services, even diagnosis is not available • Support IPWSO, whose mission is to improve the quality of life for people with PWS throughout the world

Resources for PWS • • National support organizations and International PWS Organisation websites Recent medical review articles: • • American Academy of Pediatrics management guidelines: • • Cassidy SB & Driscoll DJ, Prader-Willi syndrome, Eur J Hum Genet, 2009; 17(1): 3– 13 Cassidy SB et al. , Prader-Willi syndrome, Genet Med, 2012; 14(1): 10 -26 www. genetests. org: Gene. Review on PWS Mc. Candless SE. Clinical report—health supervision for children with Prader-Willi syndrome. Pediatrics. 2011 Jan; 127(1): 195 -204 Growth hormone consensus statement: • Deal CL et al. , J Clin Endocrinol Metab. 2013 Jun; 98(6); E 1072 -87
 Performance work statement example
Performance work statement example Titelblad pws
Titelblad pws Evms pws sow
Evms pws sow Deelvragen voorbeeld
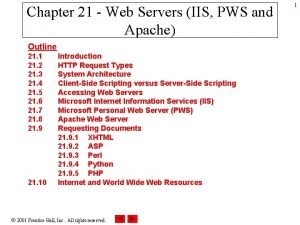
Deelvragen voorbeeld Pws web server
Pws web server Illbruck pr010
Illbruck pr010 Voorblad pws
Voorblad pws Pws onderwerpen
Pws onderwerpen Paul brocklehurst
Paul brocklehurst Oranje kruis boekje 27e druk download
Oranje kruis boekje 27e druk download Lms npru
Lms npru Pws npru
Pws npru Overview of education in health care
Overview of education in health care Child rights act 2005 images
Child rights act 2005 images National programs related to child health and welfare
National programs related to child health and welfare Children's mental health
Children's mental health National children's digital health collaborative
National children's digital health collaborative Green paper children's mental health
Green paper children's mental health Fspos vägledning för kontinuitetshantering
Fspos vägledning för kontinuitetshantering Novell typiska drag
Novell typiska drag Tack för att ni lyssnade bild
Tack för att ni lyssnade bild Returpilarna
Returpilarna Shingelfrisyren
Shingelfrisyren En lathund för arbete med kontinuitetshantering
En lathund för arbete med kontinuitetshantering Underlag för särskild löneskatt på pensionskostnader
Underlag för särskild löneskatt på pensionskostnader Personlig tidbok
Personlig tidbok Anatomi organ reproduksi
Anatomi organ reproduksi Förklara densitet för barn
Förklara densitet för barn Datorkunskap för nybörjare
Datorkunskap för nybörjare Stig kerman
Stig kerman Debattinlägg mall
Debattinlägg mall Delegerande ledarstil
Delegerande ledarstil Nyckelkompetenser för livslångt lärande
Nyckelkompetenser för livslångt lärande Påbyggnader för flakfordon
Påbyggnader för flakfordon Lufttryck formel
Lufttryck formel