Overview of GIT Hepatobiliary Diseases Objectives List GIT
Overview of GIT & Hepatobiliary Diseases
Objectives • List GIT and Hepatobiliary diseases of Public Health importance • Knowledge of the environmental factors influencing the occurrence of infectious diseases GIT • Discuss the prospects of prevention and improved control of infectious diseases of GIT and Hepatobiliary tract. • Discuss the indicators of GI disease presence and activity • Describe the causes, transmission, and symptoms of viral hepatitis infections. 2
List Of GIT And Hepatobiliary Diseases Of Public Health Importance • Intestinal Infections i. Cholera • Neoplasms ii. Typhoid fever Priority diseases i. Ca stomach iii. Salmonellosis in Pakistan iii. Ca esophagus iv. Diarrhea v. Dysentery ii. Colorectal Ca iv. Hepatocellular Ca vi. Food poisoning • Viral Hepatitis (Hepatitis A, B, C, E) (priority diseases) 3
Environmental factors influencing the spread of GIT diseases 1. Water: Lack of safe drinking water 2. Living conditions: Poor and crowded, inadequate excreta disposal facilities, poor hygiene 3. Food: prepared or stored in unhygienic conditions 4. Climate: Local climate can affect distribution and number of disease vectors. Flooding after heavy rains can result in sewage overflow and widespread water contamination. Also pathogens can be spread from one region to another along air streams or by wind. 4
• Common Gastrointestinal infections kill around 2. 2 million people globally each year, mostly children in developing countries. • Causative agent may be bacterial, viral and parasitic organisms most of which can be spread by contaminated water. • Water may be contaminated with human faeces e. g. from municipal sewage, septic tanks and latrines. • Animal faeces also contain microorganisms that can cause GI infections. • Infections can also spread from person to person, aggravated by poor personal hygiene. • Fish and seafood from polluted water may also contribute to the disease. 5
Seasonality • In the developing world cholera outbreaks generally occur during times of heavy rainfall and flooding. • Intestinal parasitic infections tend to be more common in the cooler, wetter months, situations which tend to favors the survival of cysts. • Rotavirus infections dramatically increase during the winter months and markedly fall during the warm, dry summer months. • Enteric adenoviruses cases are common throughout the year. 6
Transmission • Route: Fecal-oral route; the organism itself/cyst or oocyst is excreted in feces which can then be transmitted to other humans by – Direct person-to-person contact or – Food and/or water • Reservoirs: Humans are the major reservoirs for many intestinal infections like amoebiasis and shigellosis. • Zoonosis: Salmonella, Campylobacter jejuni and certain parasitic infections like cryptosporidiosis and giardiasis have large animal reservoirs, and thus fulfil the criterial for zoonotic diseases. 7
Prospects of Prevention And Control Primary Prevention • Achieved by interruption of the fecal-oral transmission route • Safe drinking water/bottled/boiled • Adequate sanitation to ensure safe disposal of feces • Personal hygiene to minimize person-to-person transmission • Prevention and control of GI infection epidemics during natural disasters or wars needs vigilant application of the above measures 8
• Guidelines and legislation are required to ensure the highest standards in: 1. Animal husbandry 2. Food production 3. Subsequent food handling with regular surveillance procedures to ensure that these standards are maintained. 9
Chemoprophylaxis • Recommended in high-risk individuals. • Broad-spectrum antibiotics, taken at approximately half therapeutic dose, can prevent certain bacterial infections like: • Travelers’ diarrhea/cholera and enteric fever • Non-antibiotic approaches such as bismuth subsalicylate have also been used to prevent travelers’ diarrhea. Its less effective than antibiotics but is free of the potential adverse effects and doesn’t increase the emergence of antibiotic resistant. 10
Probiotics & Immuno - prophylaxis • Probiotics help to restore the bacteria in the body. Probiotics are live bacteria. They’re added to some foods, drugs, dietary supplements, and other products. Probiotic bacteria when administered in enough amounts give several health benefits like: • Reducing the number of harmful organisms in the intestine • Producing antimicrobial substances • Stimulating the body’s immune response 11
Hepatitis A, E, B, C & D
Viral hepatitis • Hepatitis is an inflammation of the liver. • The condition can be self-limiting or can progress to fibrosis, cirrhosis or liver cancer. • Most common cause of hepatitis is viral, but toxic substances (e. g. alcohol/drugs), and autoimmune diseases can also cause hepatitis. • 5 main hepatitis viruses types A, B, C, D and E. • Types B and C lead to chronic disease in hundreds of millions of people are the most common cause of liver cirrhosis and cancer.
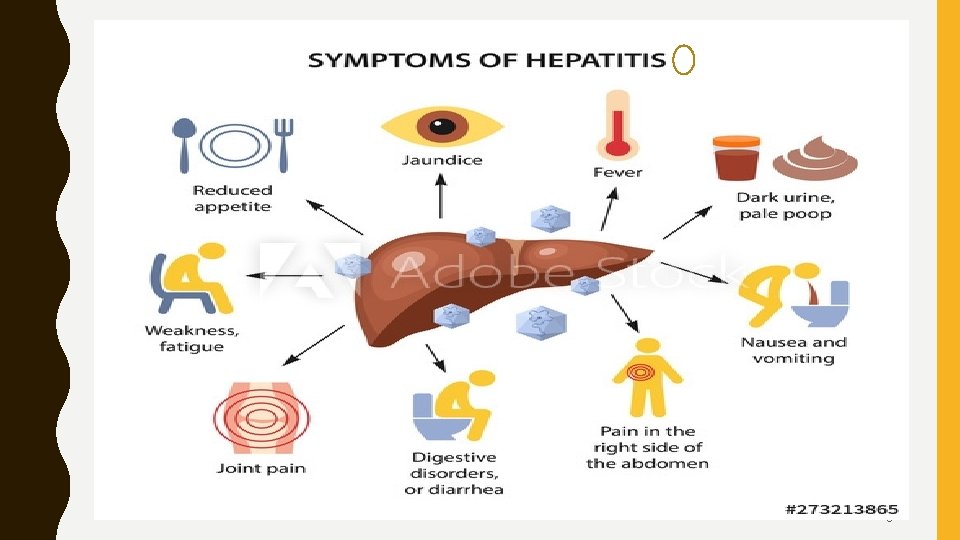
• Acute infection may occur with limited or no symptoms, or may include symptoms such as jaundice (yellowing of the skin and eyes), dark urine, extreme fatigue, nausea, vomiting and abdominal pain. 14
Hepatitis A virus (HAV) • The hepatitis A virus is present in the faeces of infected persons and is most often transmitted through consumption of contaminated water or food. • Infections are in many cases mild, with most people making a full recovery and remaining immune from further HAV infections. • Rarely HAV infections can also be severe and life threatening. • Most people in areas of the world with poor sanitation have been infected with this virus. 15
High risk people for Hepatitis A • People who are in direct contact with persons who have hepatitis A • Have travelled to a country that is known to have a high incidence of HAV infection • Homosexual males • Drug users • Have a clotting factor disorder • You work with primates 16
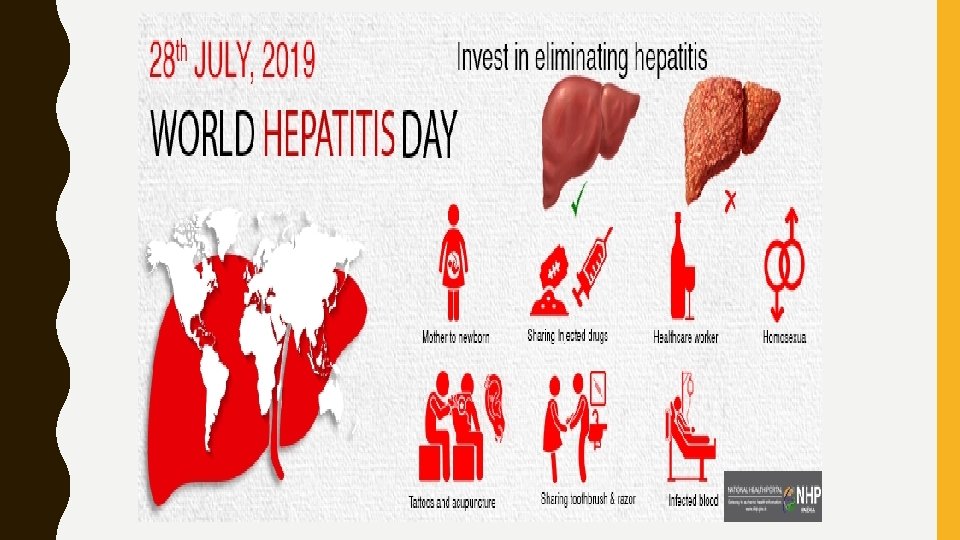
Hepatitis B virus (HBV) • Hepatitis B virus is transmitted through exposure to infective blood, semen, and other body fluids. • HBV can be transmitted from infected mothers to infants at the time of birth or from family member to infant in early childhood. • Transmission may also occur through HBV-contaminated blood and blood products, contaminated injections during medical procedures, and through injection drug use. • HBV also poses a risk to healthcare workers who sustain accidental needle stick injuries while caring for infected-HBV patients. 17
Hepatitis C virus (HCV) • Hepatitis C virus is mostly transmitted through exposure to infective blood. This may happen through transfusions of HCV-contaminated blood and blood products, contaminated injections during medical procedures, and through injection drug use. • Sexual transmission is also possible, but is much less common. 18
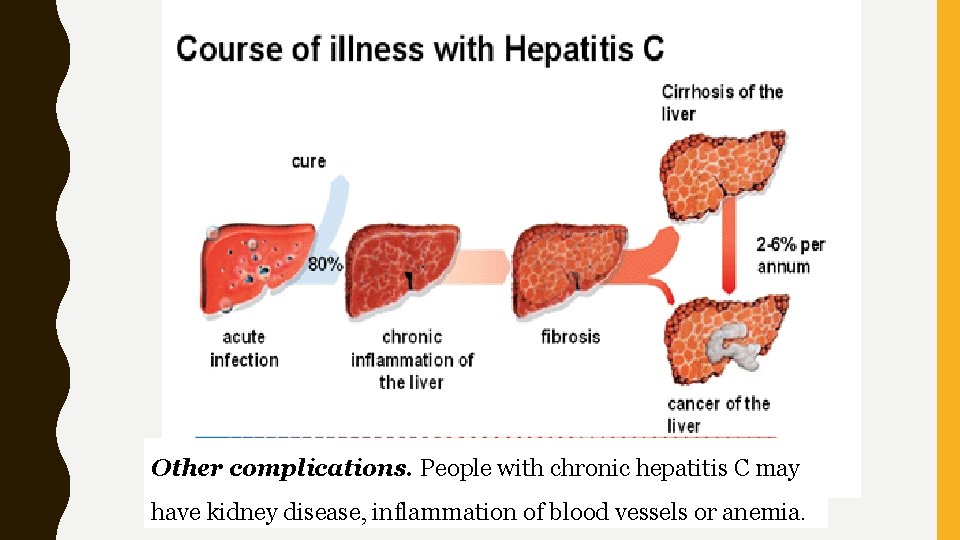
Other complications. People with chronic hepatitis C may have kidney disease, inflammation of blood vessels or anemia.
Hepatitis D virus (HDV) • Hepatitis D virus infections occur only in those who are infected with HBV. • The dual infection of HDV and HBV can result in a more serious disease and worse outcome. • Hepatitis B vaccines provide protection from HDV infection. 20
Hepatitis E virus (HEV) • Hepatitis E virus is mostly transmitted through consumption of contaminated water or food. • HEV is a common cause of hepatitis outbreaks in developing parts of the world and is increasingly recognized as an important cause of disease in developed countries. • Safe and effective vaccines to prevent HEV infection have been developed but are not widely available. 21
Causes of non infective hepatitis • Alcohol and other toxins: Excessive alcohol consumption cause liver damage and inflammation. • Alcohol directly injures the cells of liver and over time, it can cause permanent liver damage and lead to liver failure and cirrhosis. • Other toxic causes of hepatitis include overuse or overdose of medications and exposure to poisons. • Autoimmune system response: Sometime immune system mistakes the liver as a harmful object and begins to attack it. It causes ongoing inflammation that can range from mild to severe, often hindering liver function. 3 times more common in women than in men. 22
High risk people for Hepatitis B & C • The following groups of people should be screened for hepatitis B virus: 1. Men who have sex with men 2. Injecting drug users 3. Anyone with chronic kidney disease and is on dialysis 4. People with HIV 5. Pregnant women 6. Babies born to mothers who have HBV or HCV 23
7. Family members, sex partners of HBV/ HCV infected people 8. People on medicines that will weaken their immune system. [steroid therapy] 9. People with abnormal liver function blood tests 10. Have received blood transfusion or organ transplant 11. Health care workers who suffer needle-stick injury. 12. People who have shared toothbrushes, razors and other personal items with a family member that is HCV-infected 13. Have body piercing or tattooing 24
25
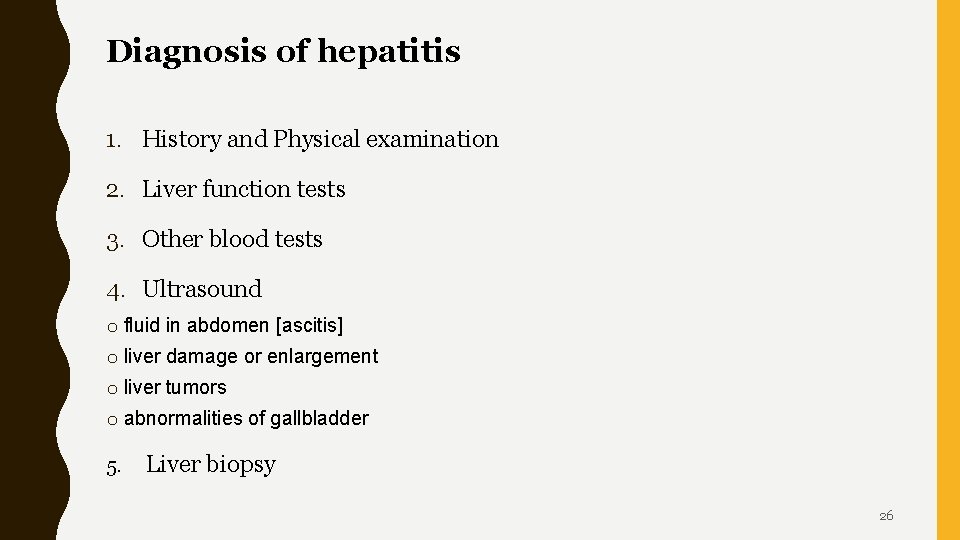
Diagnosis of hepatitis 1. History and Physical examination 2. Liver function tests 3. Other blood tests 4. Ultrasound o fluid in abdomen [ascitis] o liver damage or enlargement o liver tumors o abnormalities of gallbladder 5. Liver biopsy 26
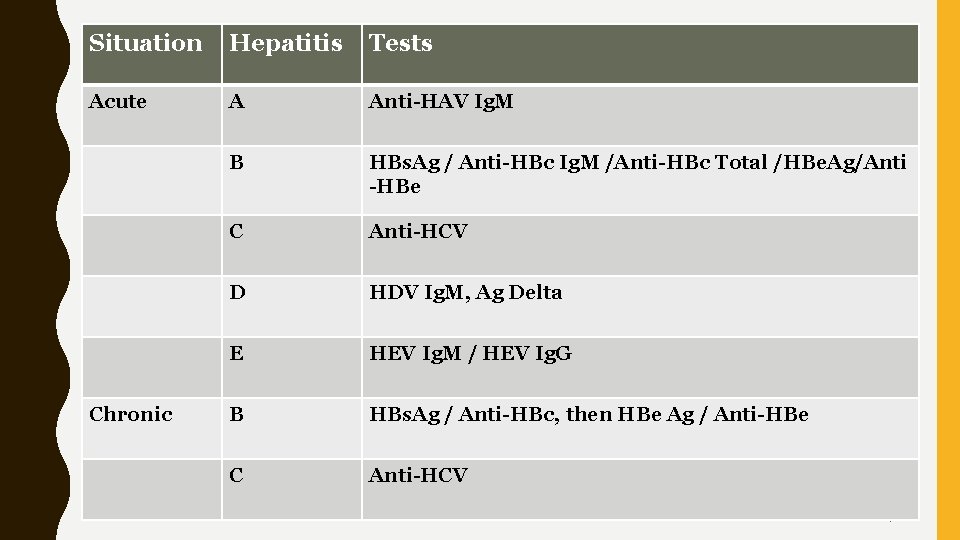
Situation Hepatitis Tests Acute Chronic A Anti-HAV Ig. M B HBs. Ag / Anti-HBc Ig. M /Anti-HBc Total /HBe. Ag/Anti -HBe C Anti-HCV D HDV Ig. M, Ag Delta E HEV Ig. M / HEV Ig. G B HBs. Ag / Anti-HBc, then HBe Ag / Anti-HBe C Anti-HCV 27
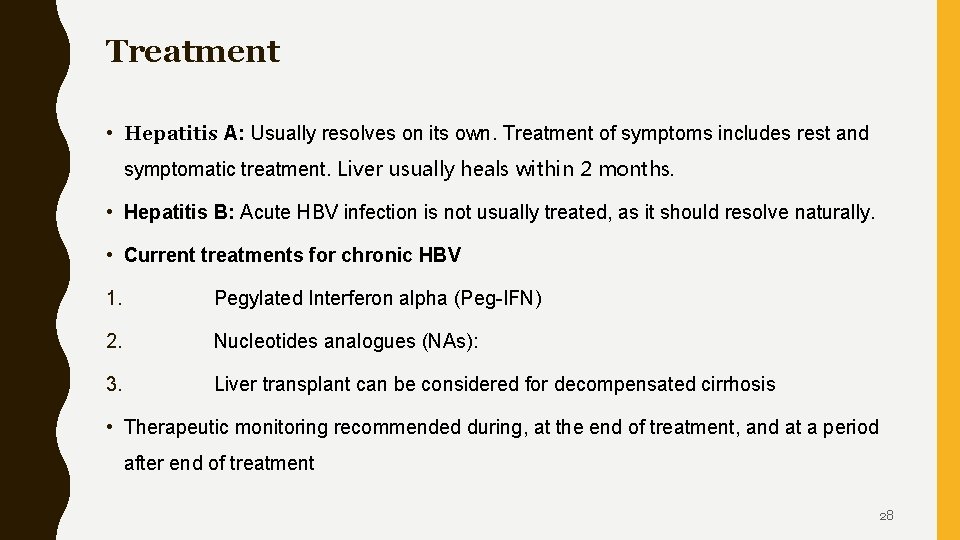
Treatment • Hepatitis A: Usually resolves on its own. Treatment of symptoms includes rest and symptomatic treatment. Liver usually heals within 2 months. • Hepatitis B: Acute HBV infection is not usually treated, as it should resolve naturally. • Current treatments for chronic HBV 1. Pegylated Interferon alpha (Peg-IFN) 2. Nucleotides analogues (NAs): 3. Liver transplant can be considered for decompensated cirrhosis • Therapeutic monitoring recommended during, at the end of treatment, and at a period after end of treatment 28
• Hepatitis C: No specific treatment for acute HCV, up to 1 out of 4 people who contract the hepatitis C virus will eventually be cured from the condition without treatment • Acute hepatitis C will develop into a chronic condition that does require treatment. Since the virus often doesn’t produce symptoms until after liver damage occurs, it’s important to get tested for it • Chronic hepatitis C leads to liver cancer or liver failure, and needs a liver transplant. 29
Prevention • The incidence of viral hepatitis is not distributed equally around the world mainly due to lack of access to prevention measures in low-resource populations and countries. • For this reason, the WHO global policy for the prevention and control of viral hepatitis aims to tailor responses to the specific national or regional context. • For hepatitis, the most important prevention strategies are: i. Universal access to childhood vaccination for hepatitis A & B ii. Improved hygiene and practices in and out of the healthcare setting iii. Screening of high risk 30
Vaccination: • Effective vaccines are available for hepatitis A and B. • The vaccine for HBV also protects against HDV, since HDV only affects populations already infected with HBV. • Universal vaccination in childhood is showing very good results in containing the number of HBV infections. • Vaccination is helping to reduce mother-to-child transmissions • Awareness and vaccination programs are also part of reducing the spread among adults, in particular at-risk groups. • Vaccination is compulsory for some at-risk groups in Pakistan 31
Hygiene: • Proper hygiene is an important prevention method for all types of viral hepatitis. This includes: • Clean drinking water and hygienic food handling • Proper hand washing • Safer sex • Injection drug users: not sharing needles and needle exchange programs • Health-care settings: fundamental infection control measures; aseptic techniques; no reuse of needles and syringes; safe injection practices 32
Screening: • Screening of people in at-risk populations and of blood products is helping to reduce the spread of hepatitis 33
Indicators of GI disease presence and activity • Morbidity rates: Morbidity rate is the percentage of people who have complications from a medical condition or after a procedure or treatment. • Mortality rates: Mortality rate is the percentage of deaths associated with a disease or medical treatment. • Hospital admission rates: Number (and mean) of hospital admissions person per year. Requires complete and reliable recording and reporting of the number of hospital admissions visits by public and private facilities. 34
References • https: //www. who. int/news-room/fact-sheets/detail/hepatitis-c • https: //www. who. int/hepatitis/publications/guidelines • https: //www. hepcoalition. org/se-documenter/article/updated-who-guidelines-for-the -screening-care-and-treatment-of-persons-with
- Slides: 36