OVERVIEW OF BIO MOLECULAR FUNCTIONS OF LIVER 1
OVERVIEW OF BIO MOLECULAR FUNCTIONS OF LIVER 1
LEARNING OBJECTIVES By end of this lecture, the student should be able to list: • Biomolecular functions of liver • Common liver disorders • Clinical manifestations of liver disorders 2
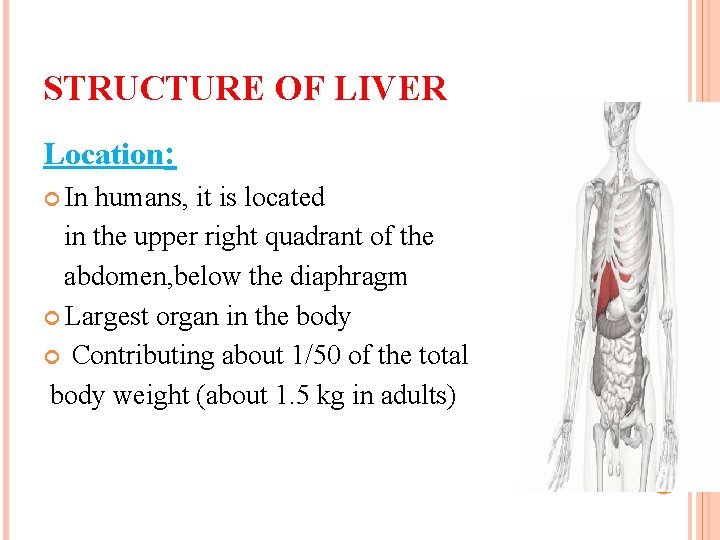
STRUCTURE OF LIVER Location: In humans, it is located in the upper right quadrant of the abdomen, below the diaphragm Largest organ in the body Contributing about 1/50 of the total body weight (about 1. 5 kg in adults) 3
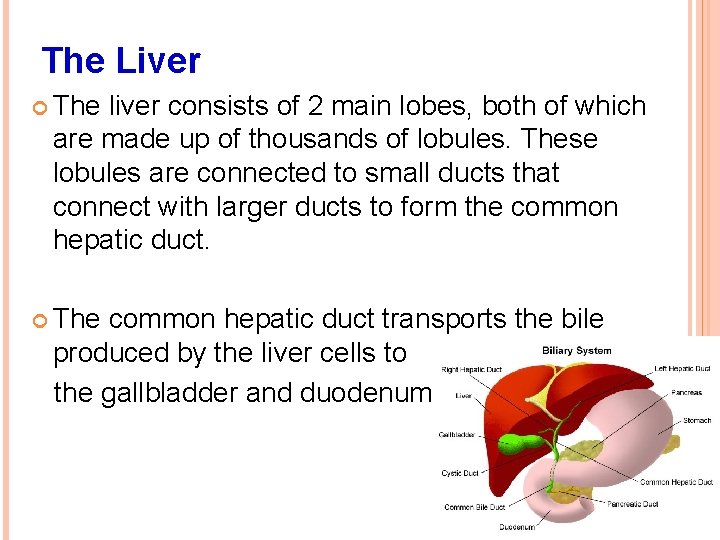
The Liver The liver consists of 2 main lobes, both of which are made up of thousands of lobules. These lobules are connected to small ducts that connect with larger ducts to form the common hepatic duct. The common hepatic duct transports the bile produced by the liver cells to the gallbladder and duodenum. 4
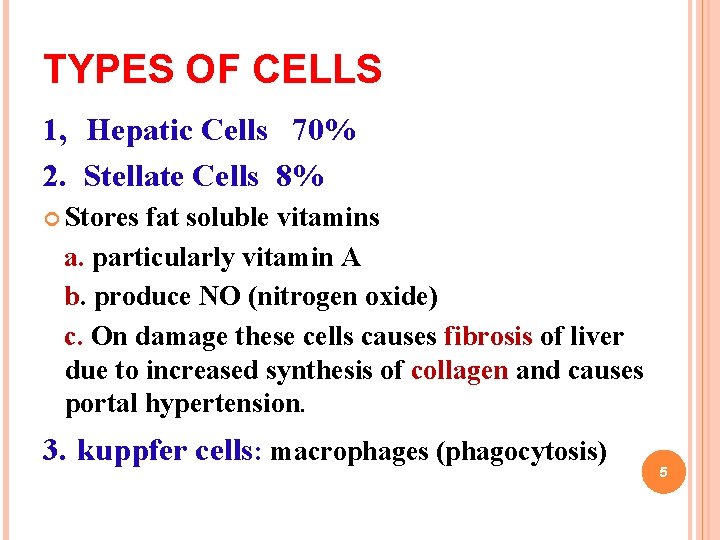
TYPES OF CELLS 1, Hepatic Cells 70% 2. Stellate Cells 8% Stores fat soluble vitamins a. particularly vitamin A b. produce NO (nitrogen oxide) c. On damage these cells causes fibrosis of liver due to increased synthesis of collagen and causes portal hypertension. 3. kuppfer cells: macrophages (phagocytosis) 5
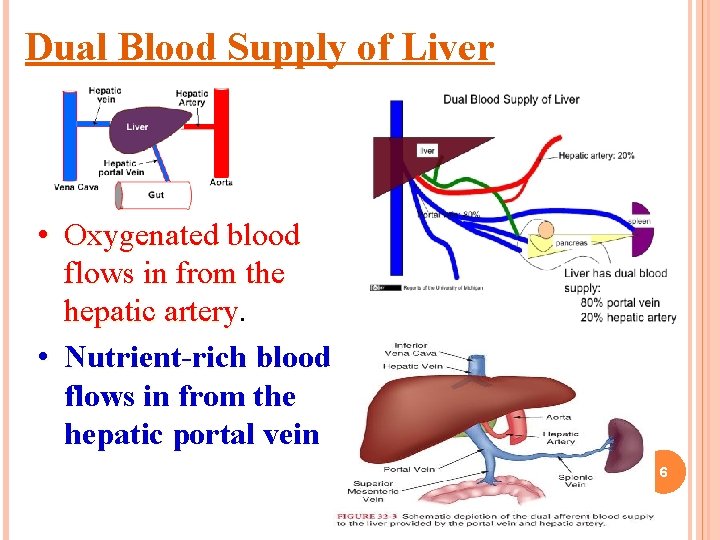
Dual Blood Supply of Liver • Oxygenated blood flows in from the hepatic artery • Nutrient-rich blood flows in from the hepatic portal vein 6
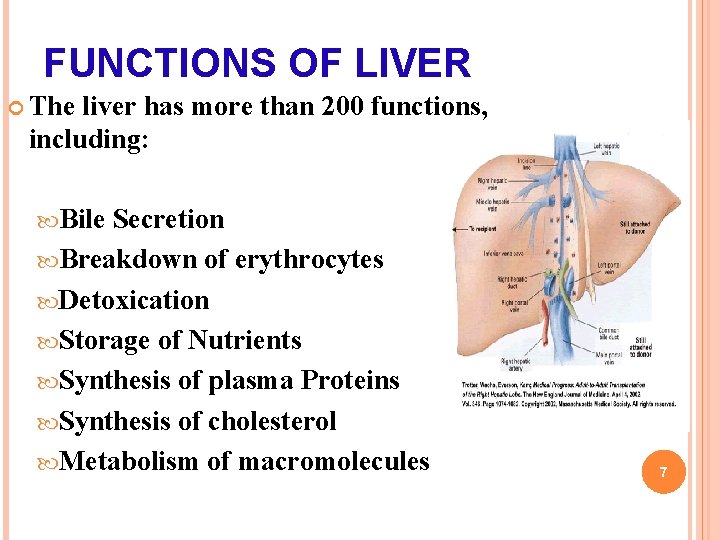
FUNCTIONS OF LIVER The liver has more than 200 functions, including: Bile Secretion Breakdown of erythrocytes Detoxication Storage of Nutrients Synthesis of plasma Proteins Synthesis of cholesterol Metabolism of macromolecules 7
FUNCTIONS OF THE LIVER Formation and secretion of bile Bile is produce and secreted by the liver cells (hepatocytes) stored in the gallbladder and discharge through the common bile duct into the duodenum. 600 ml to 1 liter of bile produced in a day 8
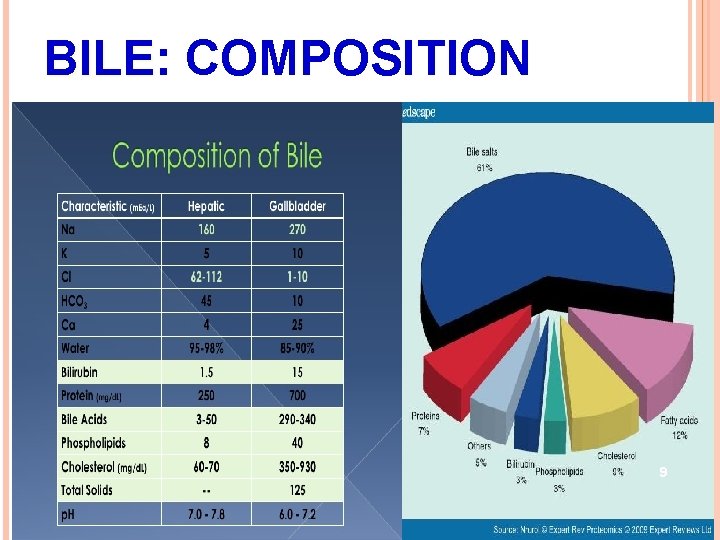
BILE: BILE COMPOSITION 9
TWO IMPORTANT FUNCTIONS OF BILE Bile acids assists with digestion and absorption of fat and fat soluble vitamin in the intestine. Excrete waste products from the blood (bilirubin from hemoglobin break down), carries excess cholesterol out of the body 10
BILE ACIDS ARE DERIVATIVES OF CHOLESTEROL SYNTHESIZED IN HEPATOCYTES Cholesterol, ingested as part of the diet or derived from hepatic synthesis is converted into the bile acids. Ø cholic and chenodeoxycholic acids which are then conjugated to an amino acid (glycine or taurine) to yield the conjugated form that is actively secreted into canaliculi 11
EMULSIFICATION FUNCTIONS OF BILE SALTS Emulsification of lipids to facilitate the digestion and absorption. lipids are hydrophobic molecules and have to be hydrolyzed and emulsified to very small droplets (micelles) before they can be absorbed 12
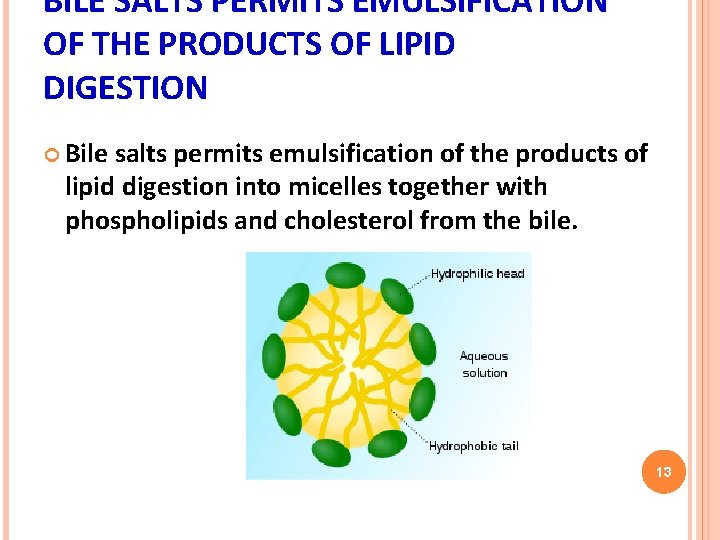
BILE SALTS PERMITS EMULSIFICATION OF THE PRODUCTS OF LIPID DIGESTION Bile salts permits emulsification of the products of lipid digestion into micelles together with phospholipids and cholesterol from the bile. 13
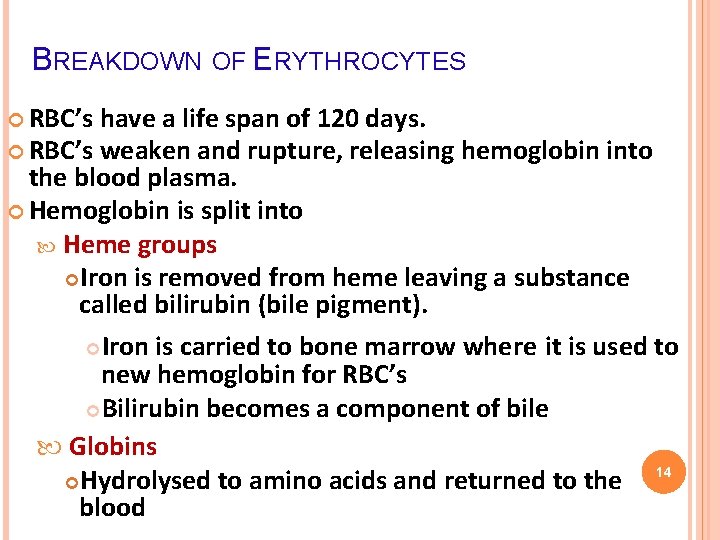
BREAKDOWN OF ERYTHROCYTES RBC’s have a life span of 120 days. RBC’s weaken and rupture, releasing hemoglobin into the blood plasma. Hemoglobin is split into Heme groups Iron is removed from heme leaving a substance called bilirubin (bile pigment). Iron is carried to bone marrow where it is used to new hemoglobin for RBC’s Bilirubin becomes a component of bile Globins 14 Hydrolysed to amino acids and returned to the blood
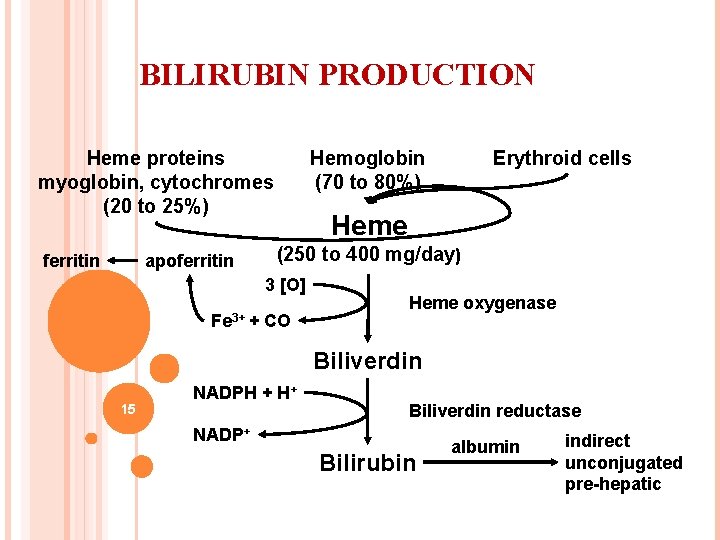
BILIRUBIN PRODUCTION Heme proteins myoglobin, cytochromes (20 to 25%) ferritin apoferritin Hemoglobin (70 to 80%) Heme (250 to 400 mg/day) 3 [O] Fe 3+ + Erythroid cells CO Heme oxygenase Biliverdin 15 NADPH + H+ Biliverdin reductase NADP+ Bilirubin albumin indirect unconjugated pre-hepatic
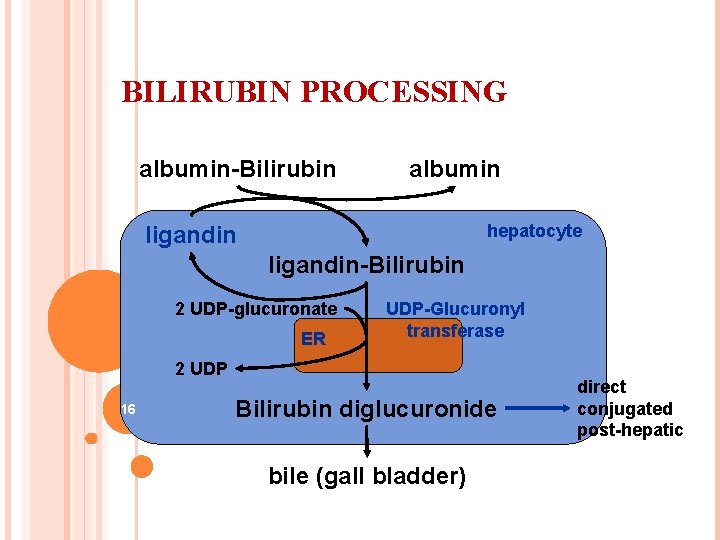
BILIRUBIN PROCESSING albumin-Bilirubin albumin hepatocyte ligandin-Bilirubin 2 UDP-glucuronate ER UDP-Glucuronyl transferase 2 UDP 16 Bilirubin diglucuronide bile (gall bladder) direct conjugated post-hepatic
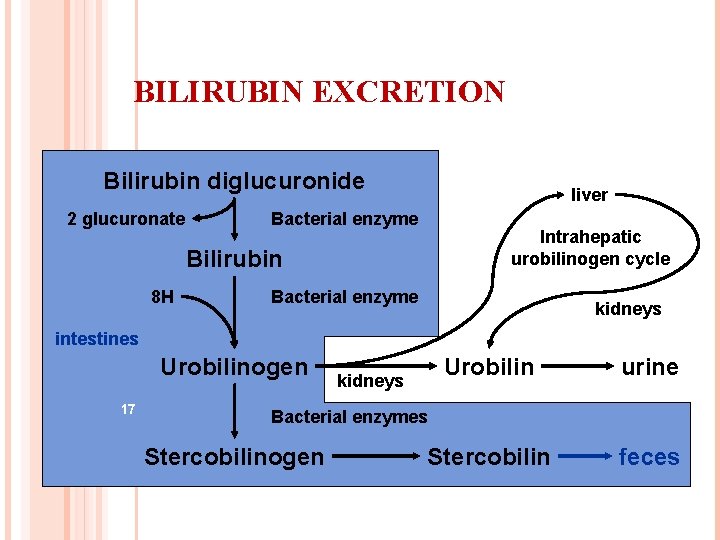
BILIRUBIN EXCRETION Bilirubin diglucuronide 2 glucuronate liver Bacterial enzyme Intrahepatic urobilinogen cycle Bilirubin 8 H Bacterial enzyme kidneys intestines Urobilinogen 17 Urobilin urine Stercobilin feces kidneys Bacterial enzymes Stercobilinogen
Relation to blood formation • storage of vitamin B 12 • metabolism of iron and its storage as ferritin (hepatic cell contains apoferritin and when excess of iron in the blood it forms ferritin) = blood iron buffer • participation on production of erythropoietin 18
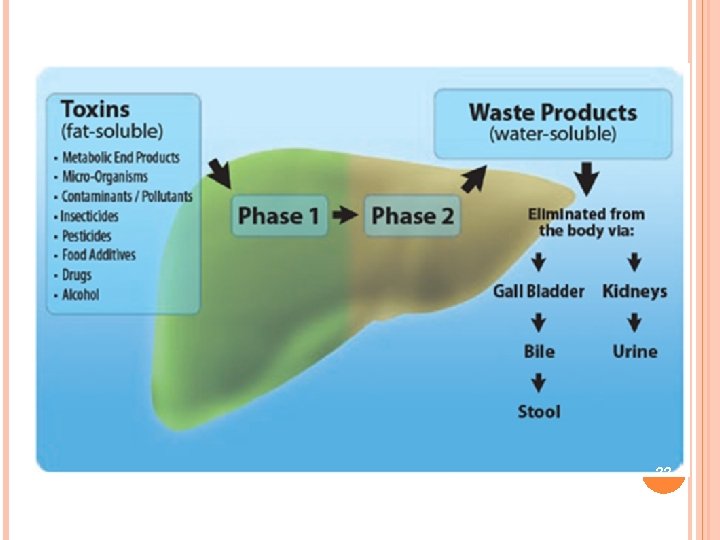
DETOXICATION OF VARIOUS SUBSTANCES Metabolic products of intestine microbes Exogenous toxins (medicaments, alcohol, poisons) Hormones (thyroxine, estrogen, cortisol, aldosterone) 19
DETOXIFICATION OF TOXIC SUBSTANCES IN LIVER Phase I and phase II. Phase I: Ø oxidation. Ø reduction, Ø hydrolysis These reactions introduce functional group (—OH, — NH 2, —SH, or —COOH) and usually result in a little increase of hydrophylic properties 20
Phase II includes (conjugation reaction) Ø glucuronation, ØGlutathione Ø glutamin Øglycin Øsulfation, Ø acetylation, Ø methylation, Phase II results in the marked increase of hydrophylic properties of xenobiotic. 21
22
SYNTHESIS OF PLASMA PROTEINS Produced by RER of Hepatocytes • Acute-phase proteins • Albumin • globulin • fibrinogen 23
COAGULATION • (synthesis of most of the coagulating factors). • Vitamin K is required for the formation of: • Factors II (prothrombin), • VII (proconvertin), • IX (Christmas factor), • X (Stuart factor) 24
. Immunity • (Kupffer cells = macrophages) . Storage • metabolism and storage of vitamins A, D, E and B 12 Iron as ferritin 25
CARBOHYDRATE METABOLISM Glycogenesis (Storage of glycogen 1 -4 %) Glycogenolysis Gluconeogenesis Conversion of galactose and fructose to glucose HMP shunt is source of the NADPH (required for cholesterol and fatty acids synthesis) Formation of many chemical compounds from intermediate products of carbohydrate metabolism 26
CARBOHYDRATE METABOLISM DISORDER IN HEPATIC DISEASES Hypoglycemia in alcohol abusers • Alcohol suppresses citrate cycle and thereby impairs gluconeogenesis from amino acids • After depletion of glycogen storages comes hypoglycemia that threatens the patient’s life. 27
Hyperglycemia in patients with cirrhosis after carbohydrate rich meal (50% has glucose tolerance, 10% has hepatic diabetes mellitus) • Combination of pathological glucose tolerance test, hyperinsulinemia, and increased insulin tolerance. • liver insufficiency decrease of glucose utilization hyperglycemia hyperinsulinemia down-regulation of insulin receptors insulin resistence. 28
FAT METABOLISM Fatty acids synthesis Triglycerides synthesis Oxidation of fatty acids to supply energy for other body function Cholesterol Synthesis Ketone bodies synethsis VLDL & HDL synthesis • Synthesis of fat from proteins and carbohydrates 29
PROTEIN METABOLISM Transamination of amino acids Deamination of amino acids Formation of urea for removal of ammonia from the body fluids Formation of plasma proteins (90% of all plasma proteins, up to 50 g of plasma proteins daily) – (cirrhosis = very low albumins = ascites and edema) 30
PROTEIN METABOLISM Protein metabolism disorder in hepatic diseases • Ammonia detoxication disorder and failure of urea formation • ammonia comes from bacterial degradation of nitrogen substances in intestines, • from intestine mucosa during glutamin degradation, • from degradation of amino acids in kidneys and muscles 31
HYPERAMMONEMIA increase of ammonia blood concentration (>50 μmol/l) Hepatic encephalopathy • toxic effect of ammonia in the brain ( Binding of ammonia to glutamate = glutamine) • Mental changes (capriciousness, disorientation, sleeping disorders, personality changes) • Motoric changes (increased in muscle 32 reactivity, hyperreflexion, tremor)
PRACTICE QUESTIONS 33
1) The compound that carries cholesterol out of the body a) Hemoglobin b) Bile c) Hemosiderin d) Urobilinogen KEY = B 34
KEY = B a) b) c) d) is the protein molecule in red blood cells that carries oxygen from the lungs to the body's tissues and returns carbon dioxide from the tissues back to the lungs is a dark green to yellowish brown fluid, produced by the liver that helps in excretion of cholesterol from body is an iron-storage complex. It is only found within cells is a colorless by-product of bilirubin reduction 35
Q 2. Urobilinogen is oxidized to form a colored product that give characteristic color to urine and feces. In which type of jaundice, the stool color is clay-colored because of lack of urobilins. a) Hemolytic jaundice. b) Obstructive jaundice c) Viral hepatitis. d) Alcoholic cirrhosis Key (B) 36
KEY = B a) occurs as a result of hemolysis, or an accelerated breakdown of red blood cells, leading to an increase in production of bilirubin. b) occurs as a result of an obstruction in the bile duct c) is liver inflammation due to a viral infection. d) is the most advanced form of liver disease that's related to drinking alcohol. 37
4) Regarding the bile: a) Bile is synthesized in the gall bladder. b) Bile salts are hydrophobic molecules. c) Most bile salts are absorbed in the terminal ileum. d) Bile salts are the breakdown products of haemoglobin. KEY = C 38
KEY = C a) Bile is synthesized in the liver and stored in gall blader. b) The bile salts are amphipathic molecules which are synthesized from cholesterol. c) Most bile salts are absorbed in the terminal ileum. d) They are not breakbown product of hemoglobin 39
4. Sulfation is an important method of detoxification of foreign compounds. Which of the following acts as a source of sulfates? a. Sulphuric acid b. Hydrogen sulphide c. Phospho adenosine Phospho sulphate. d. Methionine. Key (C) 40
KEY = C a) b) c) d) is a mineral acid with molecular formula H 2 SO 4. It is a colorless odorless liquid that is soluble in water, in a reaction that is highly exothermic. is a colorless, flammable, extremely hazardous gas with a “rotten egg” smell. Is a derivative of adenosine monophosphate that is a common coenzyme in sulfotransferase reactions. is an essential amino acid in humans. 41
5. Which of the following is not the function of liver? a) Secretion of bile b) Storage of vitamin A c) Storage of vitamin C d) Storage of glycogen Key (C) 42
KEY = C All are functions of liver except (C) because vitamin C is a water soluble vitamin and cannot be stored in body. 43
- Slides: 43