OVERVIEW OF A CIT PROGRAM Virginia Annual CIT








- Slides: 38
OVERVIEW OF A CIT PROGRAM Virginia Annual CIT Summit 2018 Conference Crisis System Solutions-“Public Health is Public Safety” TM
How Real Collaboration Can Transform A Community Virginia Annual CIT Summit 2018 Conference Crisis System Solutions-“Public Health is Public Safety” TM

INTRODUCTIONS § Law-Enforcement o Regions o Urban/Rural o Perspective of Program Status §Family/Consumer/Advocate §Behavioral Health o Regions o Urban/Rural o Crisis or Outpatient üFacility üMobile üPhones §Funders Crisis System Solutions-“Public Health is Public Safety” TM
Background q The Crisis Intervention Team (CIT) Program is a model community initiative that emerged in Memphis, Tennessee (1988) that seeks to bridge the gap between police officers and the mental health system. The model is designed to create partnerships between: 1. Law enforcement 2. Behavioral health professionals 3. Service recipients and their families. q CIT helps to provide a forum for effective community problem solving and communication q Diversion Opportunities: CIT relies on a strong community partnership and a vibrant crisis system that understands the role and needs of law enforcement and encourages officers to access crisis facilities. Crisis System Solutions-“Public Health is Public Safety” TM
Mission q CIT Programs – Promote and support collaborative efforts to create and sustain more effective interactions among law enforcement, mental health care providers, individuals with mental illness, their families and communities ü Diversion away from Criminal Justice System and into Behavioral Health System ü Improved safety for officers and consumers ü Reduce the stigma of mental illness. ü Increase public and stakeholder awareness ü CIT can facilitate linkages to long term treatment and service which affects sustainable change in the community. ü Improving Public Health and Public Safety Crisis System Solutions-“Public Health is Public Safety” TM
CIT – A Program or a Training? ? ? üLARGE MISUNDERSTANDING THAT CIT IS TRAINING FOR POLICE • It’s Training but so much more üBased on Memphis Model-10 Core Elements üUse my Stool as Allegory for Collaboration ü Picture a 5 -Legged Stool • Nothing with only 1 or 2, can stand with 3, but 4/5 how sturdy & enduring. Crisis System Solutions-“Public Health is Public Safety” TM
#1 – Police Training q Police Training ü ü ü Smallest Part of My Job (even though 1000+ cops trained) Based on Memphis Model 40 hours Advanced officer training Voluntary Students Goal typically around 20 -25% Patrol q Improve understanding when LE is called to a BH Situation. Hope & Goal is officer will be better able to: ü ü Recognize Hopefully resolve peacefully if possible If appropriate Divert from CJ to BH System How to “Navigate” confusing world of BH Services, etc. q This is the part that most think of, but is just ONE of the Legs q Consider Mental Health Awareness i. e. MHFA-LE for AOT, Academy, In-service etc. Crisis System Solutions-“Public Health is Public Safety” TM
#2 Community Collaboration q Police, Advocacy, Providers, Community, etc. ü Core of CIT ü Not only Builds Support but also • • • Understanding Relationships Instructors Resources Helps with Sustainability q Community Dynamic – Needs a Community Solution: ü Not “owned” by just one entity & not the “responsibility” of just one entity to “solve” the problem. Crisis System Solutions-“Public Health is Public Safety” TM
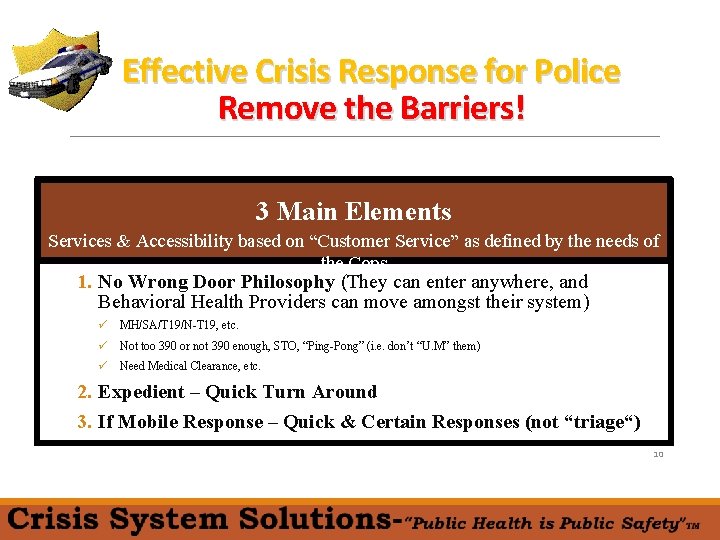
#3 Vibrant – Accessible Crisis System q One of my Biggest Passions… q Frequently Forgotten q Not Just that a Community Has Crisis Services, but more HOW Easy & ACCESSIBLE they are, determines what cops will do ü If harder to divert than jail… Crisis System Solutions-“Public Health is Public Safety” TM
Effective Crisis Response for Police Remove the Barriers! 3 Main Elements Services & Accessibility based on “Customer Service” as defined by the needs of the Cops 1. No Wrong Door Philosophy (They can enter anywhere, and Behavioral Health Providers can move amongst their system) ü MH/SA/T 19/N-T 19, etc. ü Not too 390 or not 390 enough, STO, “Ping-Pong” (i. e. don’t “U. M” them) ü Need Medical Clearance, etc. 2. Expedient – Quick Turn Around 3. If Mobile Response – Quick & Certain Responses (not “triage“) 10
#4 BH System Training q. Just like training the Cops… ü Increase Awareness re: working with PD ü Not just Leadership getting the culture/need, but equally important that GROUND LEVEL Staff get trained and understand, etc. ü Ride-Alongs &/Or “Cop Culture 101” • Approximately 500 over past few years on how to improve interactions w/ LE Crisis System Solutions-“Public Health is Public Safety” TM
#5 Educate Family/Recipient/Advocates 1. Increase understanding of Realistic Outcomes of LE Interactions ◦ Increase understanding of what “CIT”/LE is and its role 2. Education on Preparing for incidents before in “crisis” 3. Appropriate Support. . . how to productively support & advocate for LE & Protect Crisis Services Crisis System Solutions-“Public Health is Public Safety” TM
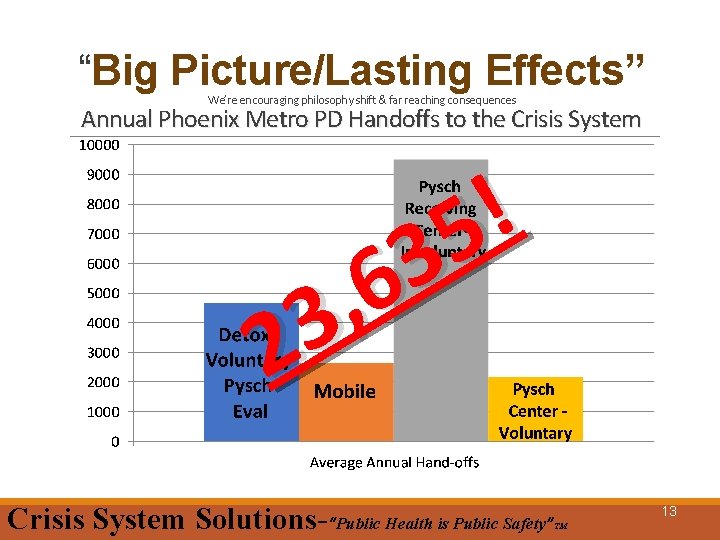
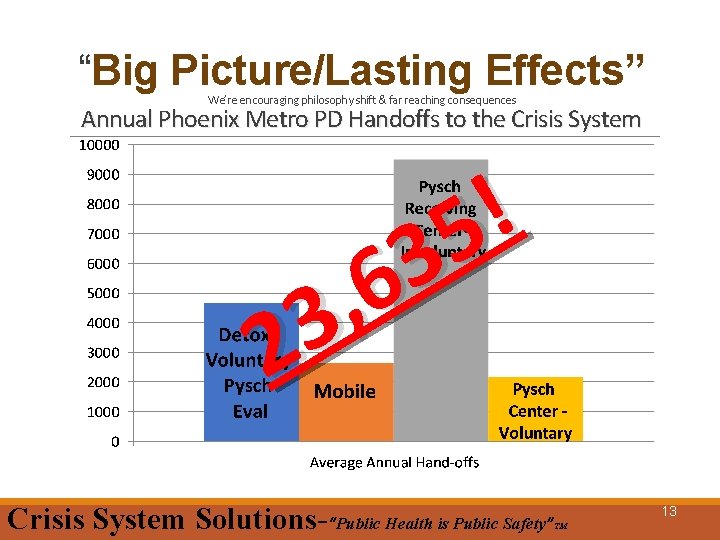
“Big Picture/Lasting Effects” We’re encouraging philosophy shift & far reaching consequences Annual Phoenix Metro PD Handoffs to the Crisis System ! 5 3 6 , 3 2 Crisis System Solutions-“Public Health is Public Safety” 13 TM

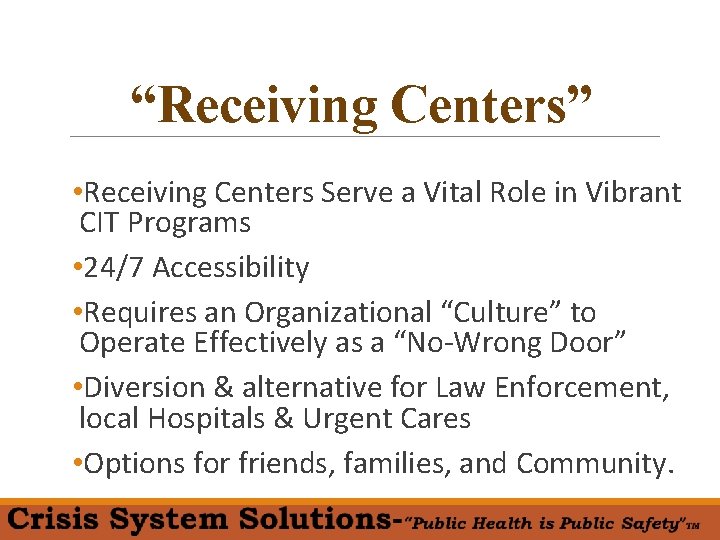
“Receiving Centers”
“Receiving Centers” • Receiving Centers Serve a Vital Role in Vibrant CIT Programs • 24/7 Accessibility • Requires an Organizational “Culture” to Operate Effectively as a “No-Wrong Door” • Diversion & alternative for Law Enforcement, local Hospitals & Urgent Cares • Options for friends, families, and Community.
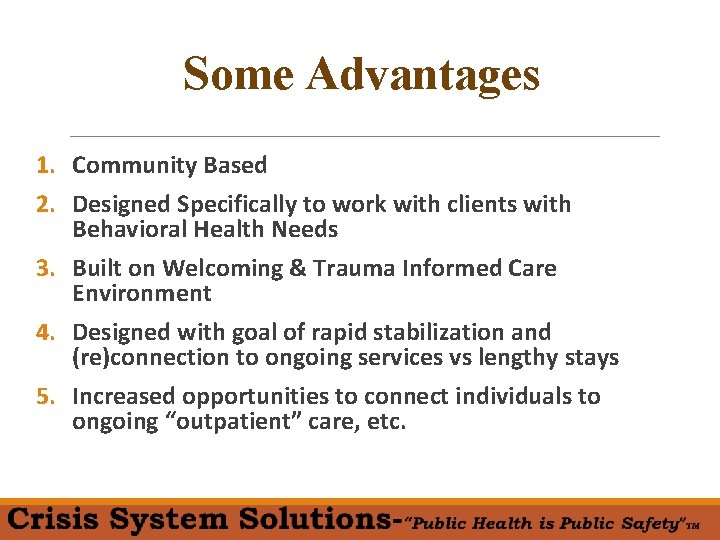
Some Advantages 1. Community Based 2. Designed Specifically to work with clients with Behavioral Health Needs 3. Built on Welcoming & Trauma Informed Care Environment 4. Designed with goal of rapid stabilization and (re)connection to ongoing services vs lengthy stays 5. Increased opportunities to connect individuals to ongoing “outpatient” care, etc.

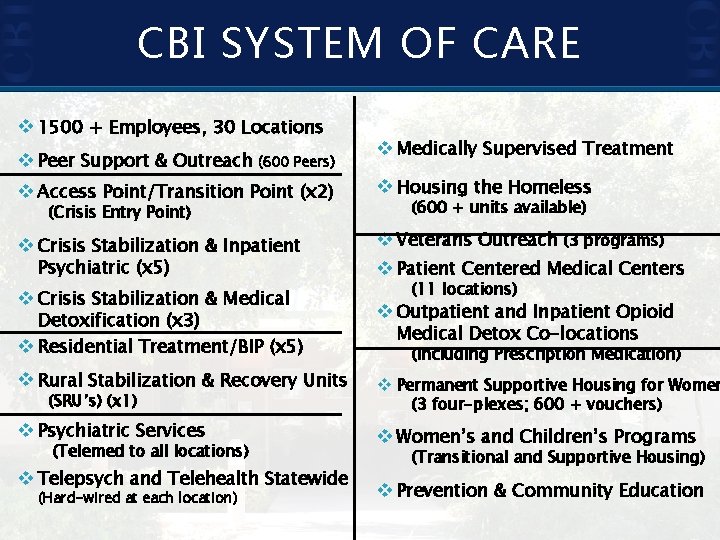
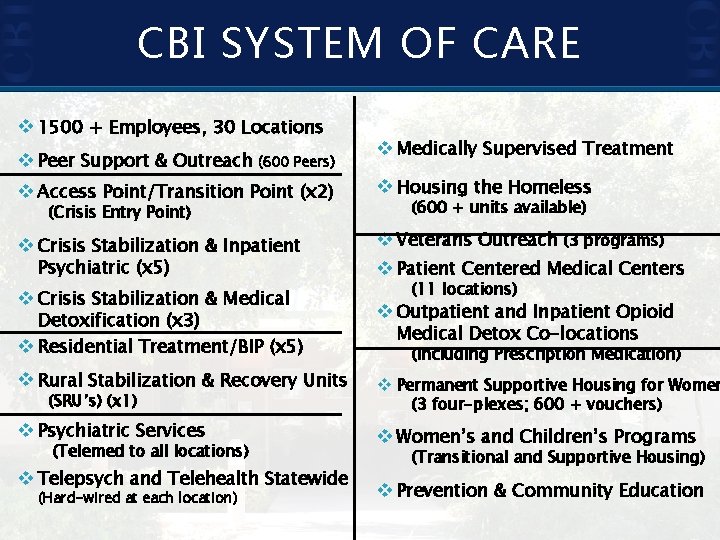
CBI SYSTEM OF CARE v 1500 + Employees, 30 Locations v Peer Support & Outreach (600 Peers) v Medically Supervised Treatment v Access Point/Transition Point (x 2) v Housing the Homeless v Crisis Stabilization & Inpatient v Veterans Outreach (3 programs) v Patient Centered Medical Centers (Crisis Entry Point) Psychiatric (x 5) v Crisis Stabilization & Medical (600 + units available) (11 locations) Detoxification (x 3) v Residential Treatment/BIP (x 5) v Outpatient and Inpatient Opioid v Rural Stabilization & Recovery Units v Permanent Supportive Housing for Women v Psychiatric Services v Women’s and Children’s Programs (SRU’s) (x 1) (Telemed to all locations) v Telepsych and Telehealth Statewide (Hard-wired at each location) Medical Detox Co-locations (including Prescription Medication) (3 four-plexes; 600 + vouchers) (Transitional and Supportive Housing) v Prevention & Community Education

CBI Programs FY 18/19 �Crisis Observation (5) �Inpatient Facilities (9) �Residential/TP (9) �PCMH (9) ◦ MAT/OTP (6) ◦ ACT Teams (2) ◦ FACT Teams (4) �Housing Units (600+) Crisis Beds/Chairs – 155 Inpatient Beds – 142 Residential/TP Beds - 164
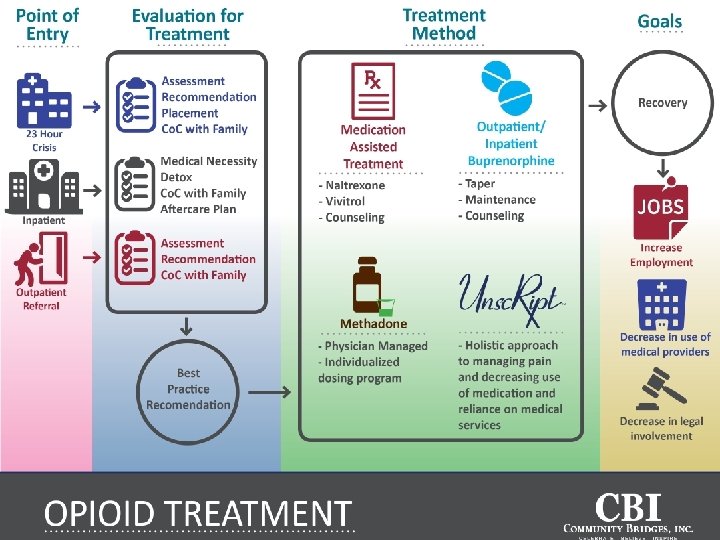
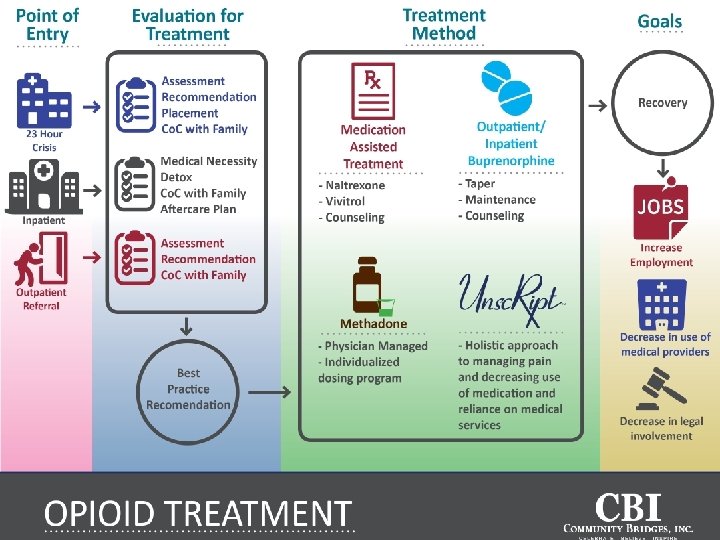
� INSERT Inforgraphic
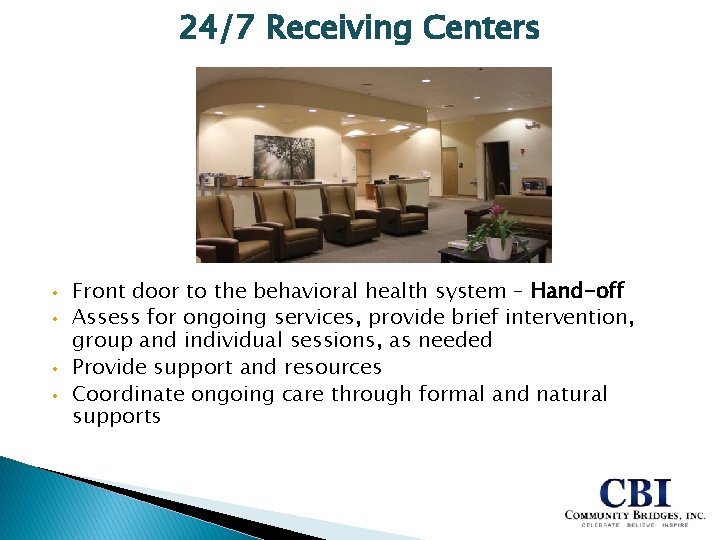
24/7 Receiving Centers • • Front door to the behavioral health system – Hand-off Assess for ongoing services, provide brief intervention, group and individual sessions, as needed Provide support and resources Coordinate ongoing care through formal and natural supports

Receiving Center Numbers Site FY 12/13 FY 13/14 FY 14/15 FY 15/16 FY 16/17 FY 17/18 CCARC 17, 049 17, 128 18, 561 19, 370 18, 772 18, 668 EVAP/ CPEC 8, 158 8, 535 7, 823 8, 068 9, 925 9, 590 EVARC 7, 542 6, 921 7, 539 7, 667 8, 382 8, 122 WVAP 7, 795 9, 316 10, 310 10, 123 9, 803 10, 564 Toole (TAP) N/A N/A 6, 828 10, 548 TOTAL 40, 544 41, 900 44, 233 45, 228 53, 710 57, 492 **110, 000 patient admissions/interactions across all CBI programs in FY 17/18** 8, 450 PD Drop Offs (23. 15 per day) 4, 338 Hospital Transfers (11. 88 per day) 22
Receiving Centers Ø What ◦ ◦ Voluntary? Involuntary? Co-Occurring? Co-Morbid Physical Health Care? Ø Goals ◦ ◦ is your Program Mission? Person Police/First Responders Community Payers
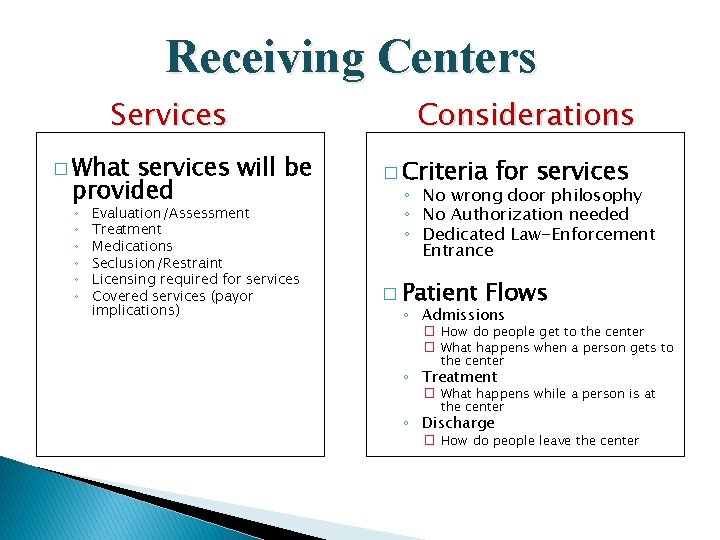
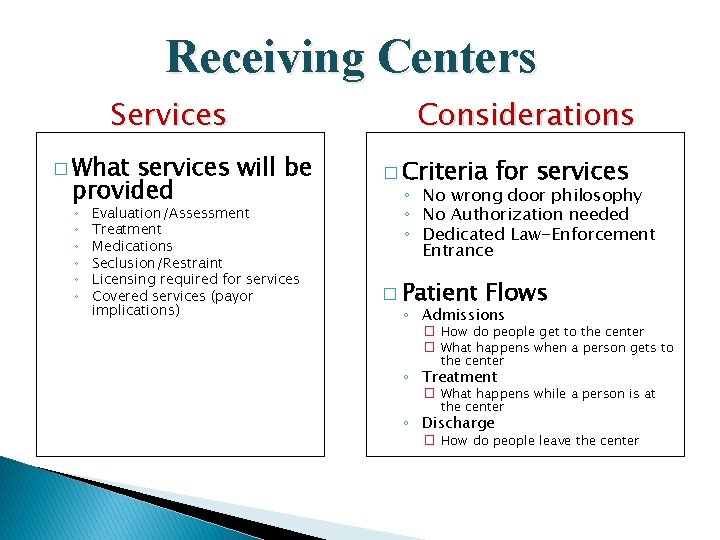
Receiving Centers Services � What services will be provided ◦ ◦ ◦ Evaluation/Assessment Treatment Medications Seclusion/Restraint Licensing required for services Covered services (payor implications) Considerations � Criteria for services ◦ No wrong door philosophy ◦ No Authorization needed ◦ Dedicated Law-Enforcement Entrance � Patient Flows ◦ Admissions � How do people get to the center � What happens when a person gets to the center ◦ Treatment � What happens while a person is at the center ◦ Discharge � How do people leave the center
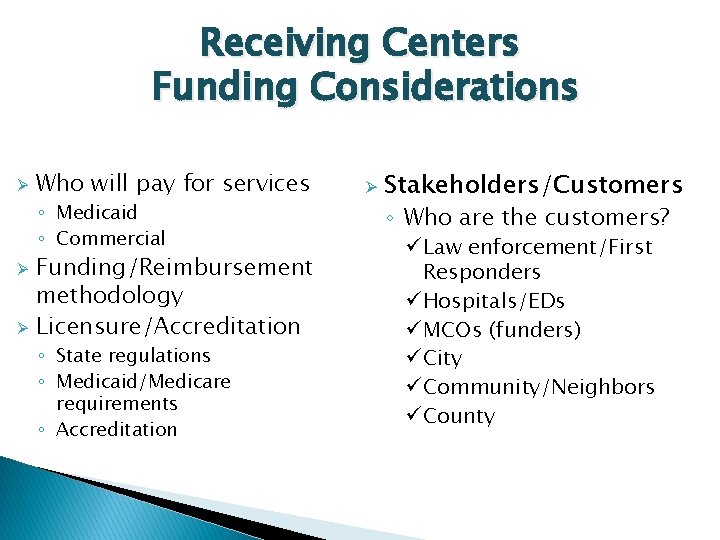
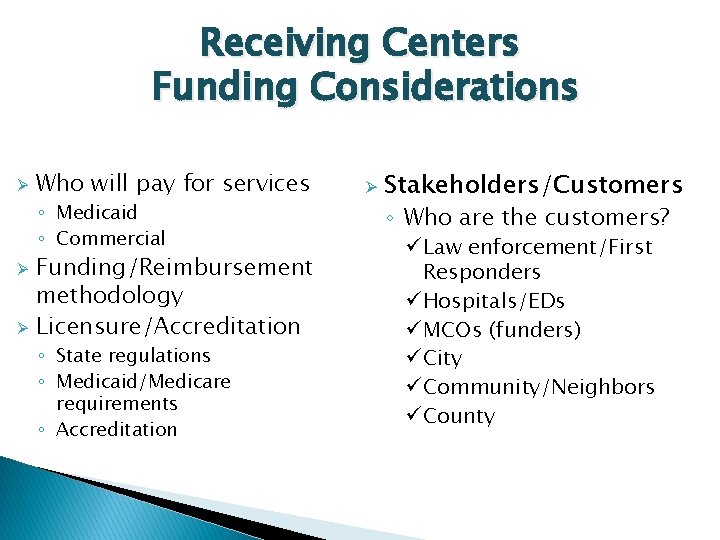
Receiving Centers Funding Considerations Ø Who will pay for services ◦ Medicaid ◦ Commercial Ø Ø Funding/Reimbursement methodology Licensure/Accreditation ◦ State regulations ◦ Medicaid/Medicare requirements ◦ Accreditation Ø Stakeholders/Customers ◦ Who are the customers? ü Law enforcement/First Responders ü Hospitals/EDs ü MCOs (funders) ü City ü Community/Neighbors ü County
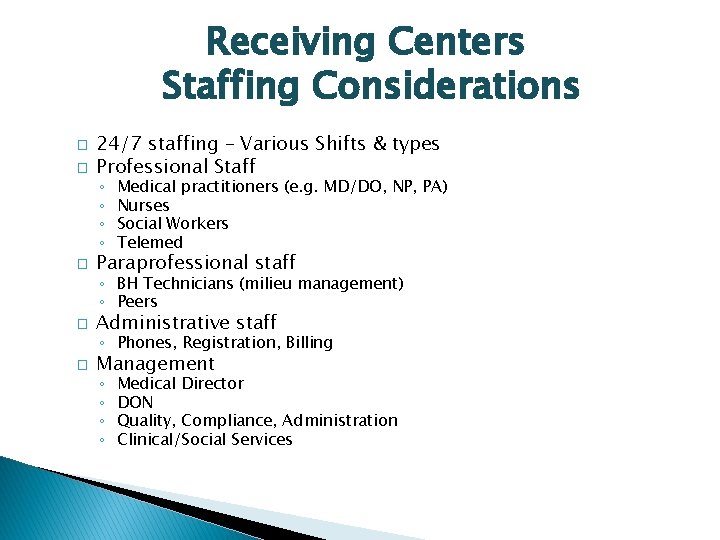
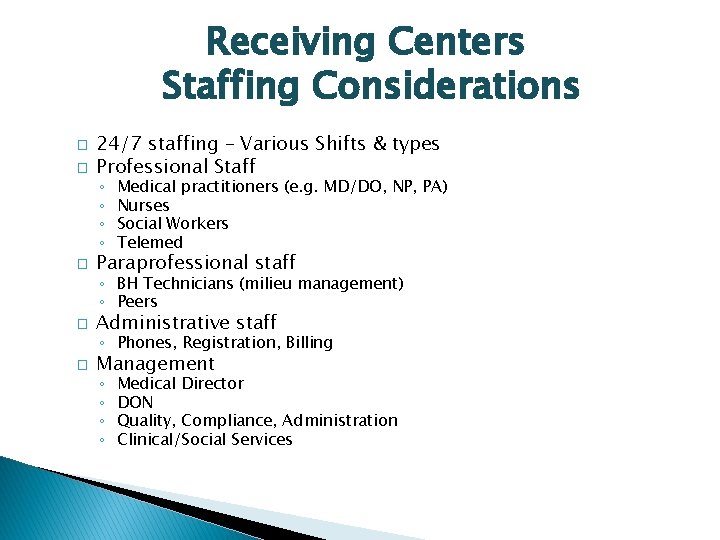
Receiving Centers Staffing Considerations � � 24/7 staffing – Various Shifts & types Professional Staff ◦ ◦ � Medical practitioners (e. g. MD/DO, NP, PA) Nurses Social Workers Telemed Paraprofessional staff ◦ BH Technicians (milieu management) ◦ Peers � Administrative staff ◦ Phones, Registration, Billing � Management ◦ ◦ Medical Director DON Quality, Compliance, Administration Clinical/Social Services
How to Operationalize 1. Get leadership to believe it 2. Change operations to meet it 3. Train people

Integrated Services � Psychiatric Services-NP, Psychiatrists, RN � Substance Use Treatment-Medical detoxification, Counseling, MAT Services � Medical-Physical PCP services. health treatment and

Discharge Planning � Considerations �ASAM Criteria �Natural Support Involvement �Outpatient / WRAP services �Medical Needs �Bridge Scripts �Transportation �Housing – Recovery Homes, Family, Independent Living, Residential, etc. �“Impact” on surrounding Community

Importance of Collaboration � Regular meetings and collaboration i. e. �Police �Funders �Stakeholders �Partner Agencies �Etc.
Rural Considerations � Community Needs ◦ Distance ◦ Population Density � Access to Services ◦ Medical ◦ Behavioral Health � Transportation � Cultural
Rural Considerations Stabilization and Recovery Unit Overview Front Door for Rural Communities
Stabilization and Recovery Unit (SRU) Services Ø Ø Ø Ø Staffed 24/7 with an EMT and a Peer Support Specialist Withdrawal Monitoring and supported by 24/7 Triage RNs– Reviews medical and withdrawal symptoms for each admission Follow-up for behavioral and physical health with a qualified Medical Practitioner Outpatient Treatment Center co-located for behavioral health support and ongoing care Tribal supports in place for specific programming Peer Support Services - Utilizes Living in Balance curriculum to address substance abuse, physical health and wellness, vocational, and recovery skills Access to inpatient behavioral health services for medical detoxification and other services in geographic area, when needed. Transportation and ongoing outreach
Telemedicine Capability v 24/7: �Medical Screenings - Immediate Treatment �Urgent Psych Assessments �Ambulatory Detoxification �Bridge Scripts �Routine Treatment �Addiction Medicine III
The Power of Peers in Crisis Services � � CBI Peers help to navigate the “Recovery Journey” Crisis Peers transform despair into hope…
Peer Support • • Peer Support are Integral to every stage Serve as a guide during intervention Critical role reducing anxiety and building “therapeutic alliance” Filling critical community gap Advocacy Discharge Planning & Coordination of Care Integrating Peers throughout Programs Integrating Peers throughout our Community
Questions?
§ Gabriella Guerra, Chief of Programs • Community Bridges, Inc. • Gguerra@cbridges. com § John Hogeboom, Deputy CEO • Community Bridges, Inc. • JHogeboom@cbridges. com § Nick Margiotta, President • Crisis System Solutions • Margiotta. nick@gmail. com