Overview and Key Elements of Population Health Management





- Slides: 40

Overview and Key Elements of Population Health Management Building Leaders – Transforming Hospitals – Improving Care © HTS 3 2016 | Page 1
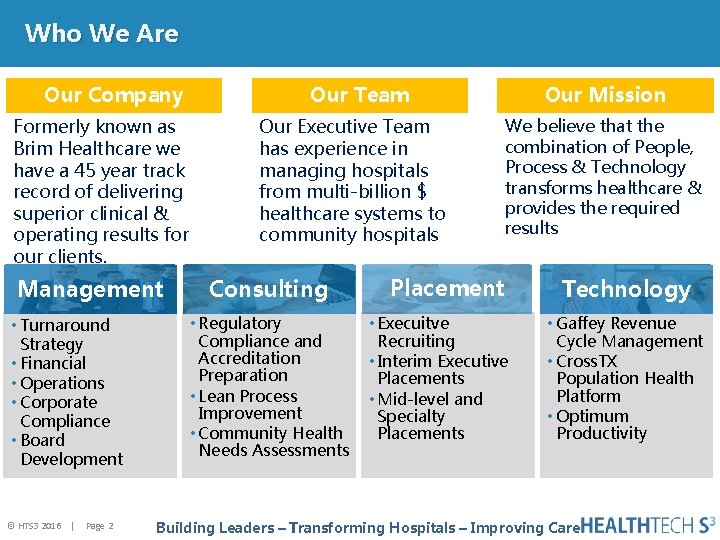
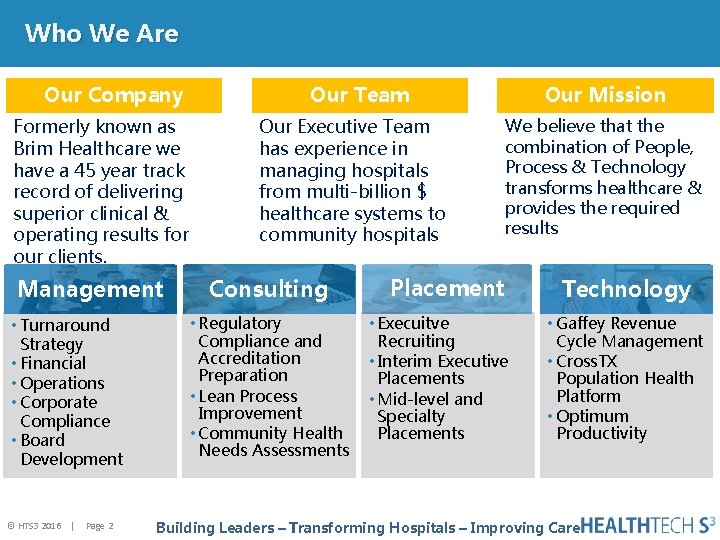
Who We Are Our Company Formerly known as Brim Healthcare we have a 45 year track record of delivering superior clinical & operating results for our clients. Management • Turnaround Strategy • Financial • Operations • Corporate Compliance • Board Development © HTS 3 2016 | Page 2 Our Team Our Mission Our Executive Team has experience in managing hospitals from multi-billion $ healthcare systems to community hospitals We believe that the combination of People, Process & Technology transforms healthcare & provides the required results Consulting • Regulatory Compliance and Accreditation Preparation • Lean Process Improvement • Community Health Needs Assessments Placement • Execuitve Recruiting • Interim Executive Placements • Mid-level and Specialty Placements Technology • Gaffey Revenue Cycle Management • Cross. TX Population Health Platform • Optimum Productivity Building Leaders – Transforming Hospitals – Improving Care
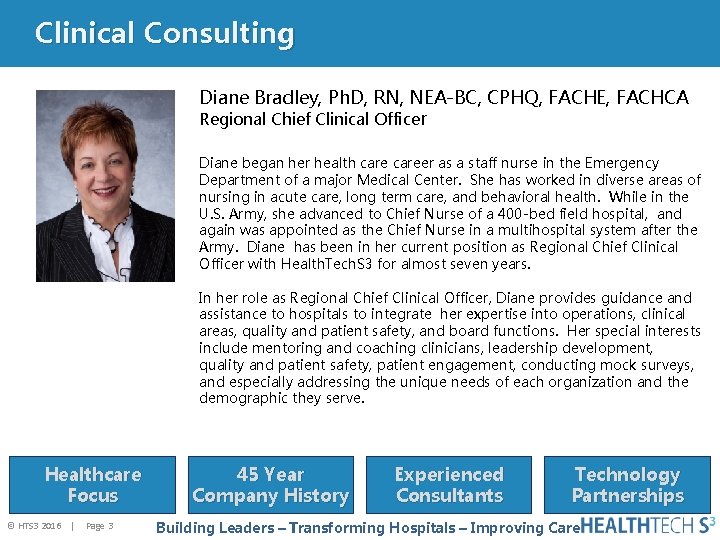
Clinical Consulting Diane Bradley, Ph. D, RN, NEA-BC, CPHQ, FACHE, FACHCA Regional Chief Clinical Officer Diane began her health career as a staff nurse in the Emergency Department of a major Medical Center. She has worked in diverse areas of nursing in acute care, long term care, and behavioral health. While in the U. S. Army, she advanced to Chief Nurse of a 400 -bed field hospital, and again was appointed as the Chief Nurse in a multihospital system after the Army. Diane has been in her current position as Regional Chief Clinical Officer with Health. Tech. S 3 for almost seven years. In her role as Regional Chief Clinical Officer, Diane provides guidance and assistance to hospitals to integrate her expertise into operations, clinical areas, quality and patient safety, and board functions. Her special interests include mentoring and coaching clinicians, leadership development, quality and patient safety, patient engagement, conducting mock surveys, and especially addressing the unique needs of each organization and the demographic they serve. Healthcare Focus © HTS 3 2016 | Page 3 45 Year Company History Experienced Consultants Technology Partnerships Building Leaders – Transforming Hospitals – Improving Care

UPCOMING EVENTS Community Health Needs Assessment: Setting Priorities Date: Friday – October 7, 2016 12: 00 – 1: 00 p. m. CDT Host: Carolyn St. Charles, RN, BSN, MBA, Regional Chief Clinical Officer Pokemon Finds MACRA Date: Thursday – October 13, 2016 12: 00 – 1: 00 p. m. CDT Hosted By: Michael Lieb, Regional Vice President Data Analytics: The Key To Making Decisions Date: Monday – October 24, 2016 12: 00 – 1: 00 p. m. CDT Host: Diane Bradley, Ph. D, RN, NEA-BC, CPHQ, FACHE, FACHCA, Regional Chief Clinical Officer A Deep Dive: Continuous Survey Readiness – Myth Or Reality? Date: Friday – November 4, 2016 12: 00 – 1: 00 p. m. CDT Host: Carolyn St. Charles, RN, BSN, MBA, Regional Chief Clinical Officer © HTS 3 2016 | Page 4 Building Leaders – Transforming Hospitals – Improving Care
Instructions for Today’s Webinar • You may type a question in the text box if you have a question during the presentation • We will try to cover all of your questions – but if we don’t get to them during the webinar we will follow-up with you by e-mail • You may also send questions after the webinar to Diane Bradley (contact information is included at the end of the presentation) • The webinar will be recorded and the recording will be available on the Health. Tech. S 3 web site www. healthtechs 3. com Health. Tech. S 3 hopes that the information contained herein will be informative and helpful on industry topics. However, please note that this information is not intended to be definitive. Health. Tech. S 3 and its affiliates expressly disclaim any and all liability, whatsoever, for any such information and for any use made thereof. Health. Tech. S 3 does not and shall not have any authority to develop substantive billing or coding policies for any hospital, clinic or their respective personnel, and any such final responsibility remains exclusively with the hospital, clinic or their respective personnel. Health. Tech. S 3 recommends that hospitals, clinics, their respective personnel, and all other third party recipients of this information consult original source materials and qualified healthcare regulatory counsel for specific guidance in healthcare reimbursement and regulatory matters. © HTS 3 2016 | Page 5
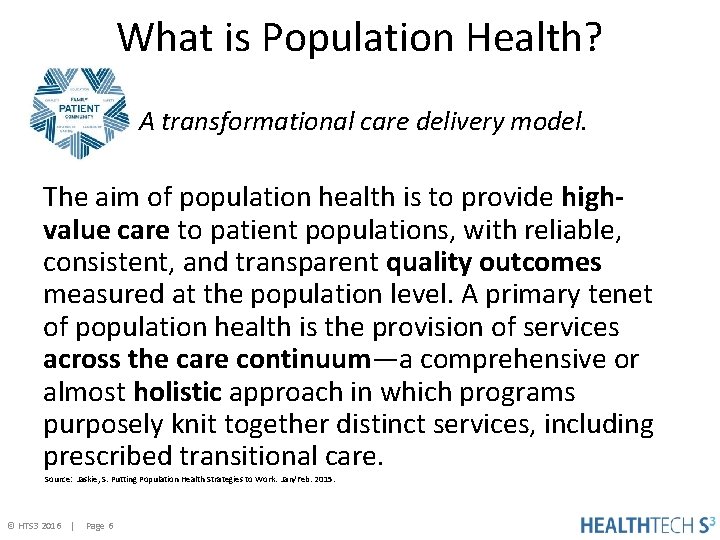
What is Population Health? A transformational care delivery model. The aim of population health is to provide highvalue care to patient populations, with reliable, consistent, and transparent quality outcomes measured at the population level. A primary tenet of population health is the provision of services across the care continuum—a comprehensive or almost holistic approach in which programs purposely knit together distinct services, including prescribed transitional care. Source: Jaskie, S. Putting Population Health Strategies to Work. Jan/Feb. 2015. © HTS 3 2016 | Page 6
HFMA Definition Population health management has been identified as a critical strategy for improving value in an era of reform. It is a model of care management designed to enhance coordination of care and services for specific patient populations, such as Medicare patients or patients with chronic disease, and more actively engage consumers in improving and maintaining their health. This model has the potential to significantly reduce costs for healthcare purchasers and consumers. © HTS 3 2016 | Page 7
Transforming Health—How? Population health (part of the ACA) is defined as the health outcomes of a group of individuals, including the distribution of such outcomes within the group. Source: Kindig & Stoddard. Population Health Definition. 2003 CLINICAL FINANCIAL © HTS 3 2016 | Page 8
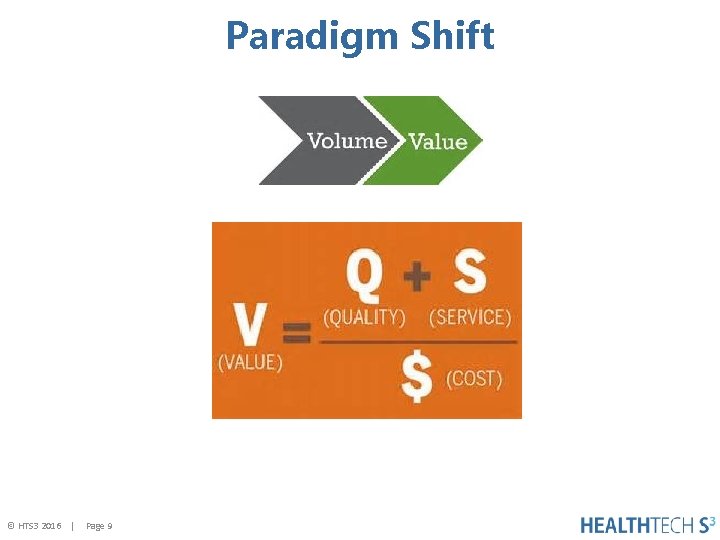
Paradigm Shift © HTS 3 2016 | Page 9
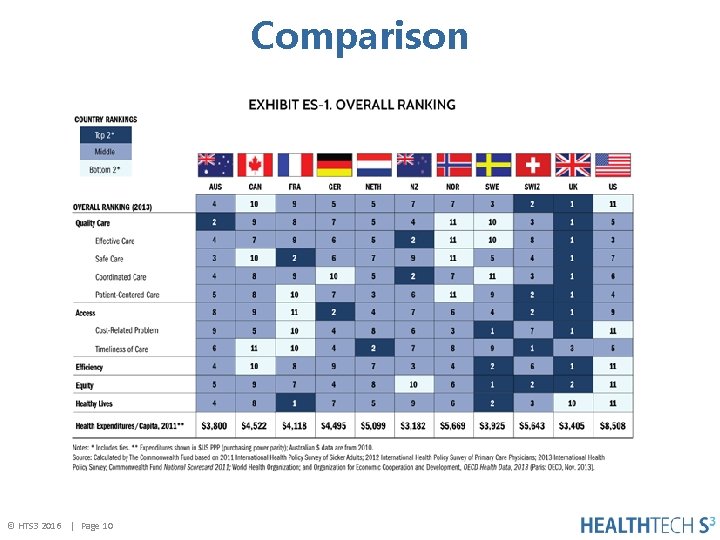
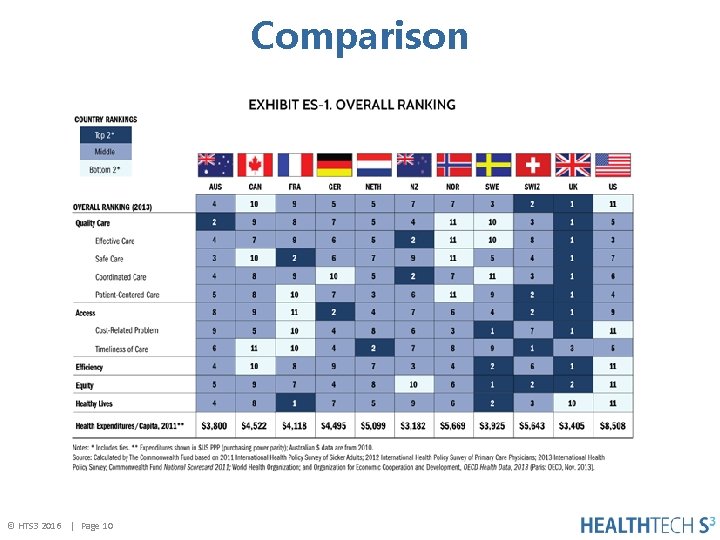
Comparison © HTS 3 2016 | Page 10
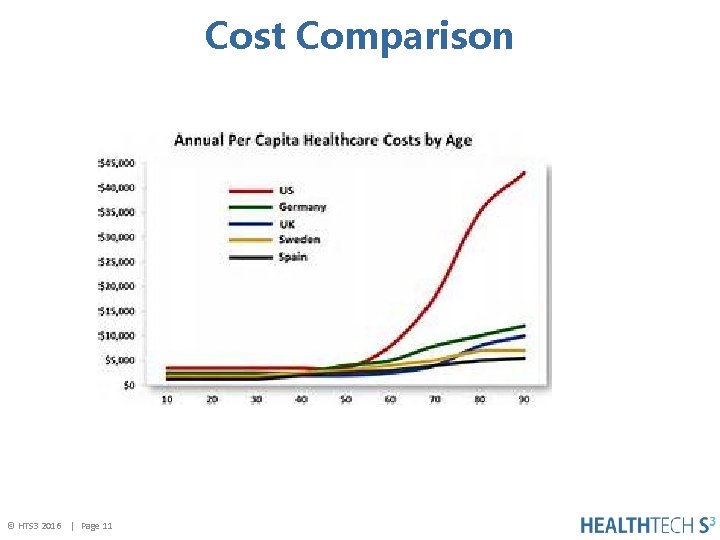
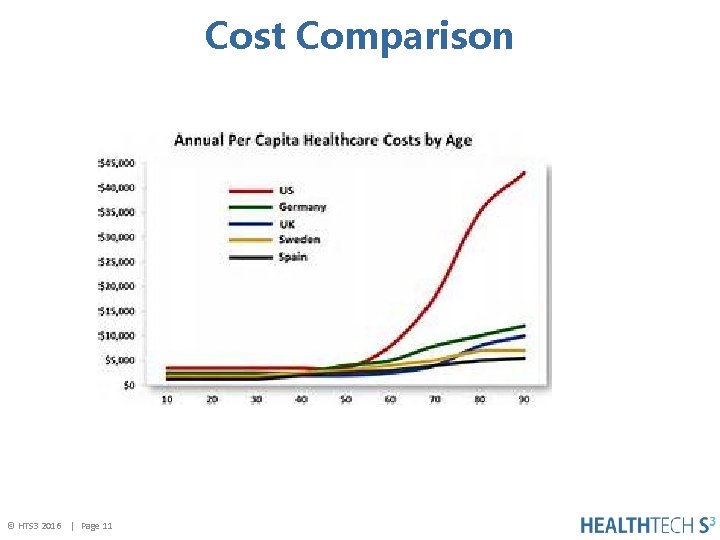
Cost Comparison © HTS 3 2016 | Page 11
Why? © HTS 3 2016 | Page 12
Who makes up PHM groups? These groups are often geographic populations such as nations or communities, but can also be other groups such as employees, ethnic groups, disabled persons, prisoners, or any other defined group. © HTS 3 2016 | Page 13
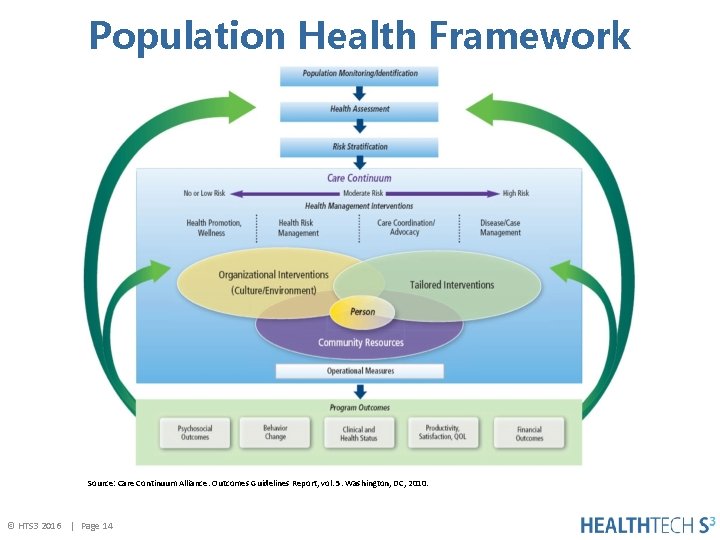
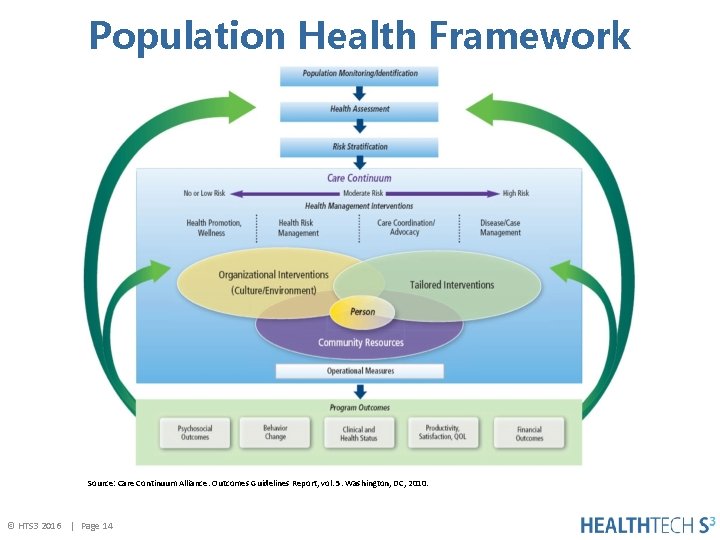
Population Health Framework Source: Care Continuum Alliance. Outcomes Guidelines Report, vol. 5. Washington, DC, 2010. © HTS 3 2016 | Page 14
Starting Point Questions to answer: 1. What factors affect a person’s health? 2. How should we assure care coordination across the continuum? 3. How do we engage individual’s in their health and subsequently their care? 4. What types of staff and technologies do we need? 5. Are there community agencies that we need to partner with, and how do we begin those conversations? 6. Is creating an infrastructure important? © HTS 3 2016 | Page 15
Risk Stratification Basic model: Ø Aggregate utilization data based on claims Ø Stratify individuals into risk categories based on utilization and calculating a risk score Advanced model: Ø Collect data from EMR Ø Determine whethere is any non-clinical data available such as socioeconomic factors Ø Know your market Ø Identify specific outcomes desired; for example, readmissions for chronic illnesses © HTS 3 2016 | Page 16
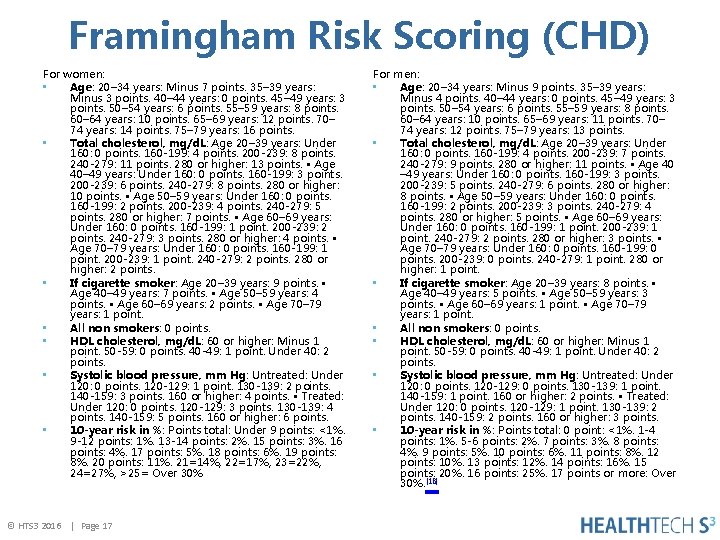
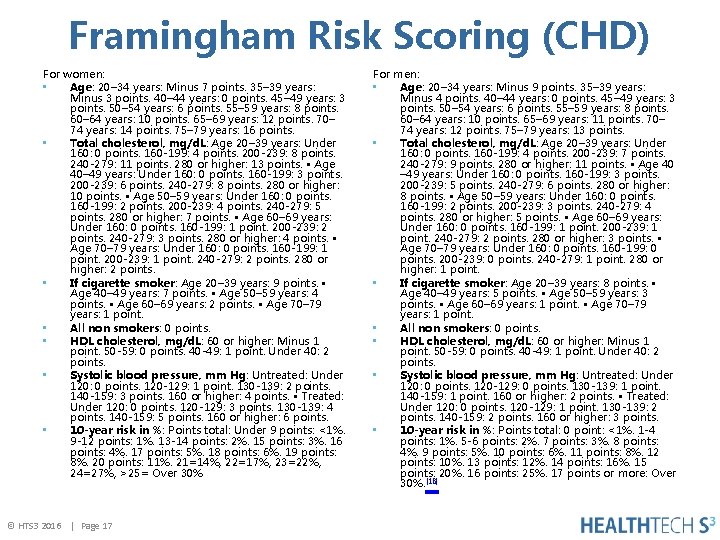
Framingham Risk Scoring (CHD) For women: • Age: 20– 34 years: Minus 7 points. 35– 39 years: Minus 3 points. 40– 44 years: 0 points. 45– 49 years: 3 points. 50– 54 years: 6 points. 55– 59 years: 8 points. 60– 64 years: 10 points. 65– 69 years: 12 points. 70– 74 years: 14 points. 75– 79 years: 16 points. • Total cholesterol, mg/d. L: Age 20– 39 years: Under 160: 0 points. 160 -199: 4 points. 200 -239: 8 points. 240 -279: 11 points. 280 or higher: 13 points. • Age 40– 49 years: Under 160: 0 points. 160 -199: 3 points. 200 -239: 6 points. 240 -279: 8 points. 280 or higher: 10 points. • Age 50– 59 years: Under 160: 0 points. 160 -199: 2 points. 200 -239: 4 points. 240 -279: 5 points. 280 or higher: 7 points. • Age 60– 69 years: Under 160: 0 points. 160 -199: 1 point. 200 -239: 2 points. 240 -279: 3 points. 280 or higher: 4 points. • Age 70– 79 years: Under 160: 0 points. 160 -199: 1 point. 200 -239: 1 point. 240 -279: 2 points. 280 or higher: 2 points. • If cigarette smoker: Age 20– 39 years: 9 points. • Age 40– 49 years: 7 points. • Age 50– 59 years: 4 points. • Age 60– 69 years: 2 points. • Age 70– 79 years: 1 point. • All non smokers: 0 points. • HDL cholesterol, mg/d. L: 60 or higher: Minus 1 point. 50 -59: 0 points. 40 -49: 1 point. Under 40: 2 points. • Systolic blood pressure, mm Hg: Untreated: Under 120: 0 points. 120 -129: 1 point. 130 -139: 2 points. 140 -159: 3 points. 160 or higher: 4 points. • Treated: Under 120: 0 points. 120 -129: 3 points. 130 -139: 4 points. 140 -159: 5 points. 160 or higher: 6 points. • 10 -year risk in %: Points total: Under 9 points: <1%. 9 -12 points: 1%. 13 -14 points: 2%. 15 points: 3%. 16 points: 4%. 17 points: 5%. 18 points: 6%. 19 points: 8%. 20 points: 11%. 21=14%, 22=17%, 23=22%, 24=27%, >25= Over 30% © HTS 3 2016 | Page 17 For men: • Age: 20– 34 years: Minus 9 points. 35– 39 years: Minus 4 points. 40– 44 years: 0 points. 45– 49 years: 3 points. 50– 54 years: 6 points. 55– 59 years: 8 points. 60– 64 years: 10 points. 65– 69 years: 11 points. 70– 74 years: 12 points. 75– 79 years: 13 points. • Total cholesterol, mg/d. L: Age 20– 39 years: Under 160: 0 points. 160 -199: 4 points. 200 -239: 7 points. 240 -279: 9 points. 280 or higher: 11 points. • Age 40 – 49 years: Under 160: 0 points. 160 -199: 3 points. 200 -239: 5 points. 240 -279: 6 points. 280 or higher: 8 points. • Age 50– 59 years: Under 160: 0 points. 160 -199: 2 points. 200 -239: 3 points. 240 -279: 4 points. 280 or higher: 5 points. • Age 60– 69 years: Under 160: 0 points. 160 -199: 1 point. 200 -239: 1 point. 240 -279: 2 points. 280 or higher: 3 points. • Age 70– 79 years: Under 160: 0 points. 160 -199: 0 points. 200 -239: 0 points. 240 -279: 1 point. 280 or higher: 1 point. • If cigarette smoker: Age 20– 39 years: 8 points. • Age 40– 49 years: 5 points. • Age 50– 59 years: 3 points. • Age 60– 69 years: 1 point. • Age 70– 79 years: 1 point. • All non smokers: 0 points. • HDL cholesterol, mg/d. L: 60 or higher: Minus 1 point. 50 -59: 0 points. 40 -49: 1 point. Under 40: 2 points. • Systolic blood pressure, mm Hg: Untreated: Under 120: 0 points. 120 -129: 0 points. 130 -139: 1 point. 140 -159: 1 point. 160 or higher: 2 points. • Treated: Under 120: 0 points. 120 -129: 1 point. 130 -139: 2 points. 140 -159: 2 points. 160 or higher: 3 points. • 10 -year risk in %: Points total: 0 point: <1%. 1 -4 points: 1%. 5 -6 points: 2%. 7 points: 3%. 8 points: 4%. 9 points: 5%. 10 points: 6%. 11 points: 8%. 12 points: 10%. 13 points: 12%. 14 points: 16%. 15 points: 20%. 16 points: 25%. 17 points or more: Over 30%. [18]
Negotiating Risk When negotiating with third party payors, some leverage that will help: 1. Results of quality initiatives that benchmarks 2. Present how efficient and cost-effective processes are – show value 3. Suggest and identify alternate payment models (APM), e. g. bundled payments 4. Determine the potential for renegotiating rates after conducting a retrospective review of service(s) volumes, for example, ED, outpatient. More volume should hopefully yield greater efficiencies. © HTS 3 2016 | Page 18
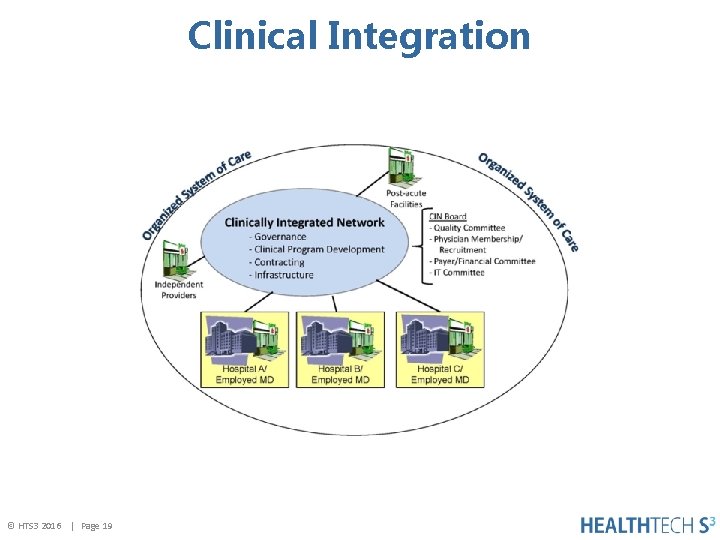
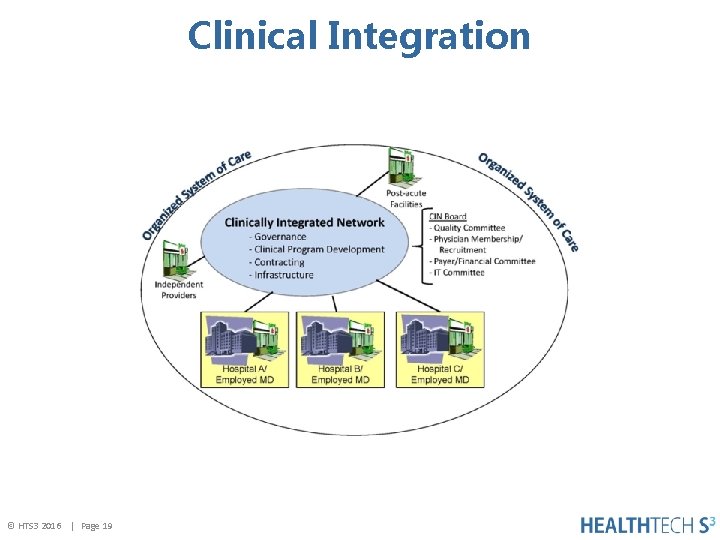
Clinical Integration © HTS 3 2016 | Page 19
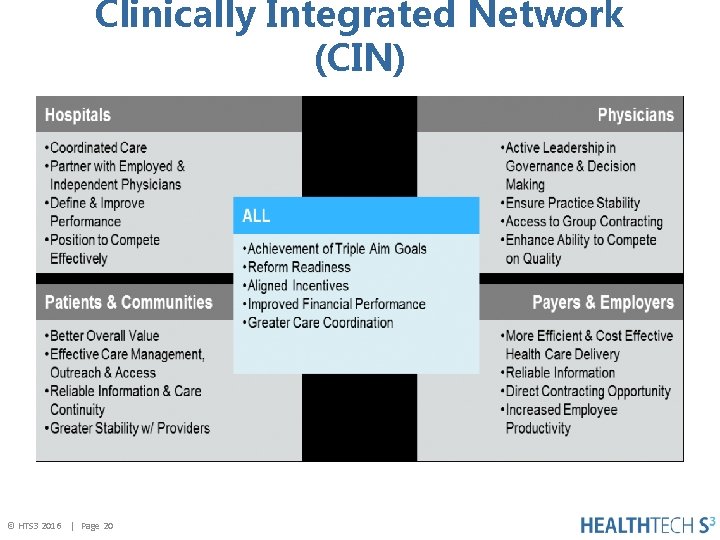
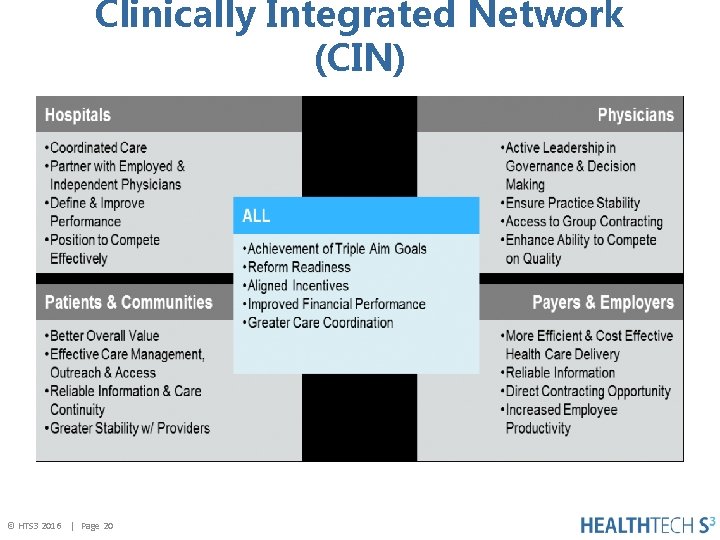
Clinically Integrated Network (CIN) © HTS 3 2016 | Page 20

Leadership CEO © HTS 3 2016 | Page 21
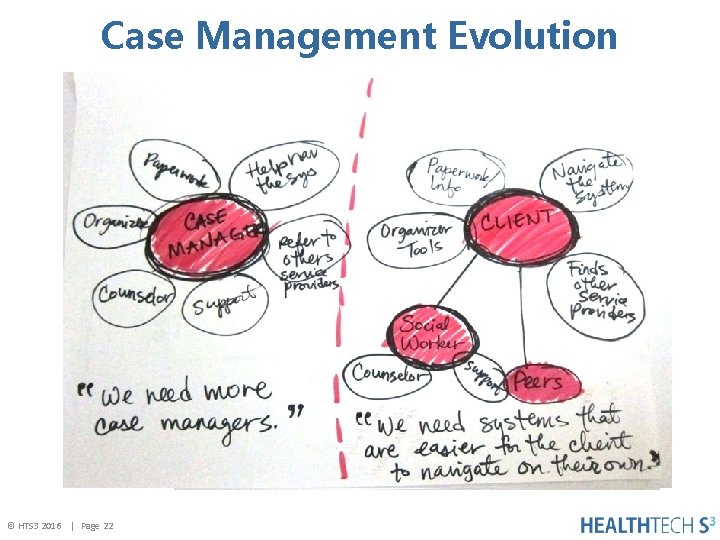
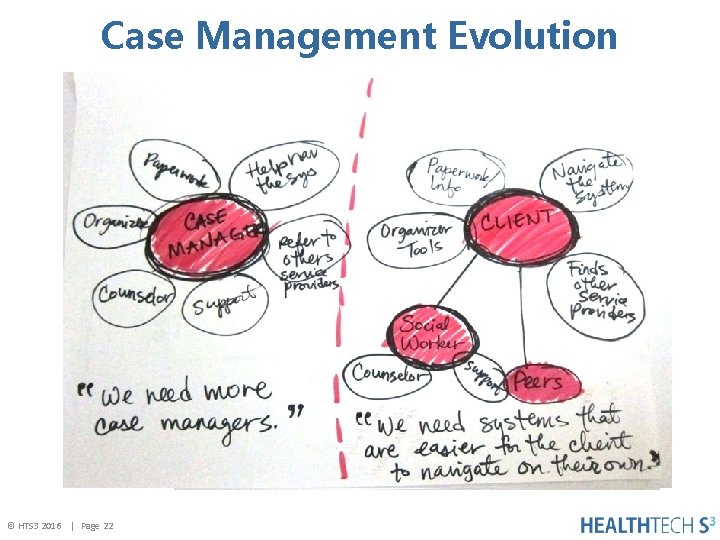
Case Management Evolution © HTS 3 2016 | Page 22
Next. Gen of Case Management Coordinating care and managing transitions – success means utilizing evidence-based, patientcentered approaches to: • Improve patient outcomes • Enhance access to quality care • Decrease hospital readmissions • Decrease health care costs • Help patients navigate the health care maze • Ensure continuity and seamless transitions among levels and settings of care • Be more efficient, reduce redundancies • Improve the individual patient’s experience of care © HTS 3 2016 | Page 23
Care Management Care management has emerged as a primary means of managing the health of a defined population. Unlike case management which tends to be diseasecentric. CM is organized around the precept that appropriate interventions for individuals within a given population will reduce health risks and decrease the cost of care. Source: Taylor EF, Machta RM, Meyers DS, Genevro J, Peikes DN. Enhancing the primary care team to provide redesigned care: the roles of practice facilitators and care managers. Ann Fam Med 2013; 11(1): 80 -3. © HTS 3 2016 | Page 24
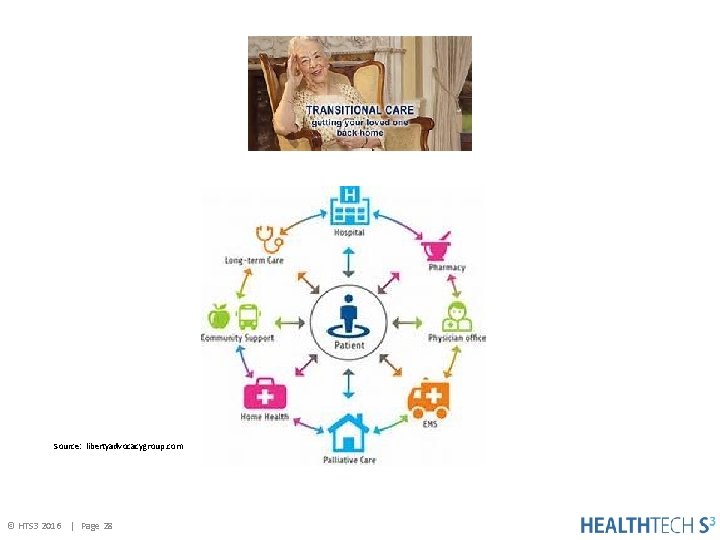
Transitional Care Management Transitional care: Care involved when a patient/client leaves one care setting (i. e. hospital, nursing home, assisted living facility, SNF, primary care physician, home health, or specialist) and moves to another. Specifically, they can occur: 1. Within settings; e. g. , primary care to specialty care, or intensive care unit (ICU) to step-down. 2. Between settings; e. g. , hospital to sub-acute care (LTACH), or ambulatory clinic. 3. Across health states; e. g. , curative care to palliative care or hospice, or personal residence to assisted living. 4. Between providers; e. g. , primary care to a specialist practitioner, or acute care provider to a palliative care specialist. Source: nacns, org © HTS 3 2016 | Page 25
Transitions of Care Transitions of care a set of actions designed to ensure coordination and continuity. They should be based on a comprehensive care plan and the availability of well-trained practitioners who have current information about the patient’s treatment goals, preferences, and health or clinical status. They include logistical arrangements and education of patient and family, as well as coordination among the health professionals involved in the transition. Source: (www. ntocc. org) © HTS 3 2016 | Page 26
Transitional Care A broad range of time-limited services designed to ensure health care continuity, avoid preventable poor outcomes among at-risk populations, and promote the safe and timely transfer of patients from one level of care to another or from one type of setting to another. Transitional care is complementary to but not the same as primary care, care coordination, discharge planning, disease management or case management. The hallmarks of transitional care the focus on highly vulnerable, chronically ill patients throughout critical transitions in health and health care, the time -limited nature of services, and the emphasis on educating patients and family caregivers to address root causes of poor outcomes and avoid preventable re-hospitalizations. Source: Naylor, M. D. , Aiken, L. H. , Kurtzman, E. T. , Olds, D. M. & Hirschman, K. B. The importance of transitional care in achieving Health Reform. Health Affairs 2011; 30(4): 746754. © HTS 3 2016 | Page 27
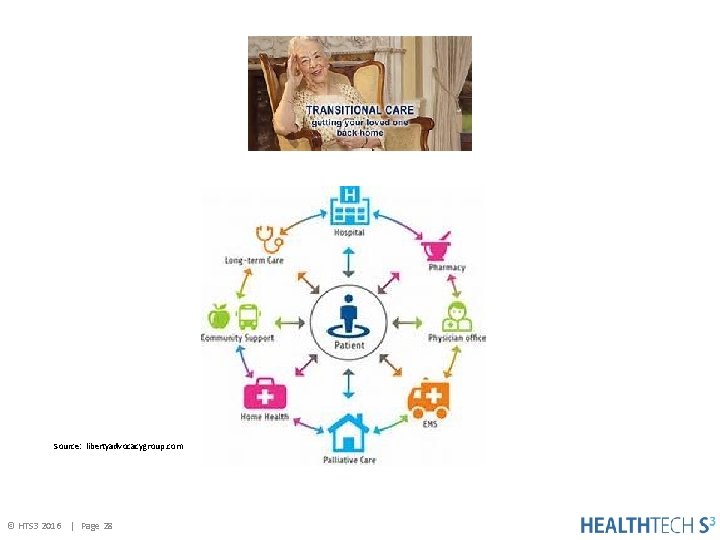
Source: libertyadvocacygroup. com © HTS 3 2016 | Page 28
© HTS 3 2016 | Page 29

Innovation • Fee-for-Service to Value Based payments • Quality outcomes • New ecosystems for care management • Payers, providers and pay-viders are organizing themselves for improved outcomes at lower costs • Technology exploding • Patient engagement strategies © HTS 3 2016 | Page 30
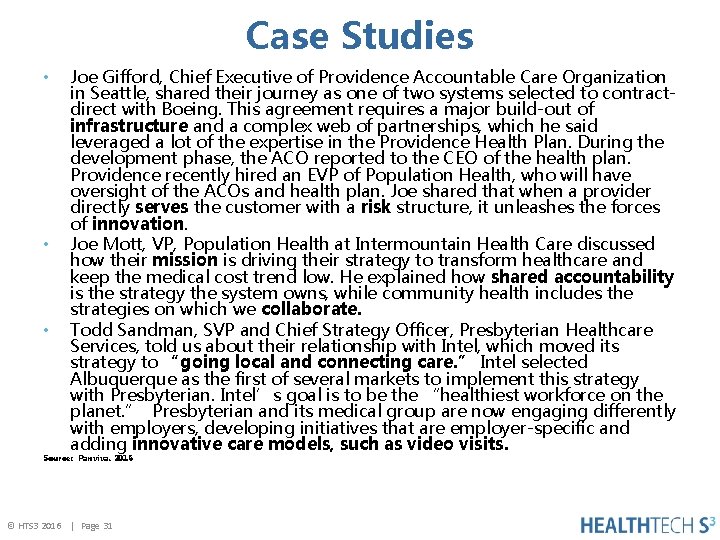
Case Studies • • • Joe Gifford, Chief Executive of Providence Accountable Care Organization in Seattle, shared their journey as one of two systems selected to contractdirect with Boeing. This agreement requires a major build-out of infrastructure and a complex web of partnerships, which he said leveraged a lot of the expertise in the Providence Health Plan. During the development phase, the ACO reported to the CEO of the health plan. Providence recently hired an EVP of Population Health, who will have oversight of the ACOs and health plan. Joe shared that when a provider directly serves the customer with a risk structure, it unleashes the forces of innovation. Joe Mott, VP, Population Health at Intermountain Health Care discussed how their mission is driving their strategy to transform healthcare and keep the medical cost trend low. He explained how shared accountability is the strategy the system owns, while community health includes the strategies on which we collaborate. Todd Sandman, SVP and Chief Strategy Officer, Presbyterian Healthcare Services, told us about their relationship with Intel, which moved its strategy to “going local and connecting care. ” Intel selected Albuquerque as the first of several markets to implement this strategy with Presbyterian. Intel’s goal is to be the “healthiest workforce on the planet. ” Presbyterian and its medical group are now engaging differently with employers, developing initiatives that are employer-specific and adding innovative care models, such as video visits. Source: Panviva. 2016 © HTS 3 2016 | Page 31
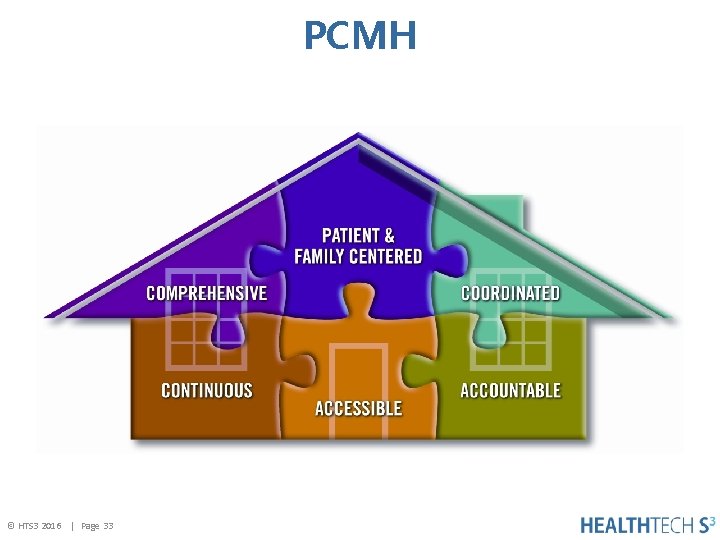
Patient Centered Medical Home (PCMH) Definition: The medical home is best described as a model or philosophy of primary care that is patientcentered, comprehensive, team-based, coordinated, accessible, and focused on quality and safety. It is a philosophy of health care delivery that encourages providers and care teams to meet patients where they are, from the most simple to the most complex conditions. It is a place where patients are treated with respect, dignity, and compassion, and enable strong and trusting relationships with providers and staff. Above all, the medical home is not a final destination instead, it is a model for achieving primary care excellence so that care is received in the right place, at the right time, and in the manner that best suits a patient's needs. Source: Patient-Centered Primary Care Collaborative © HTS 3 2016 | Page 32
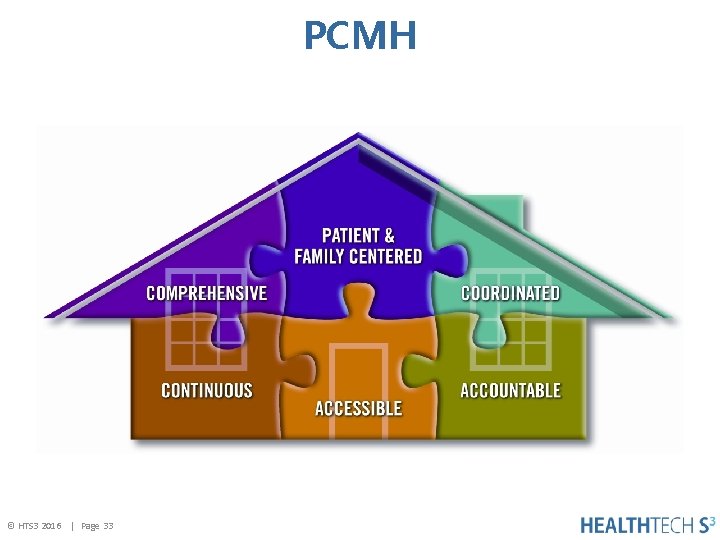
PCMH © HTS 3 2016 | Page 33
Potential Barriers to PHM 1. The current regulatory and legal environment does not support many of the collaborative approaches. 2. Malpractice insurance and tort reform are major hurdles in the pursuit of team clinical strategies. 3. Leaders who do not have the vision and engagement to know that change is necessary and that the change will result in a better system. © HTS 3 2016 | Page 34
Opportunities/Strategies 1. Re-envision quality performance—quality will be transparent to patients; quality becomes an “everybody” responsibility. 2. Engage physicians in a contemporary view of what quality management looks like. 3. Solve current financial problems. For example, are some patients staying after procedures who should not be staying? © HTS 3 2016 | Page 35
Opportunities/Strategies 4. Traditional metrics for market share less important – the goal is to keep people out of hospitals. 5. Convenience supersedes structure – appointments will become obsolete. Retail health care is surging. 6. Provider’s competition are apps – technology will replace “personableness”, and care will be delivered at home, e. g. wearables. 7. Care will be provided by multidisciplinary teams – led by physicians along with greater use of nurse practitioners to augment the projected physician shortage. 8. Non-traditional partnerships will be formed – community agencies, for-profit, governmental agencies, IT providers, analytics will partner with different sized hospitals. © HTS 3 2016 | Page 36
Opportunities/Strategies 9. PHM requires consistent adherence to care standards supported by electronic medical records and frugal utilization of resources. 10. The practice of medicine has changed from an individual sport to a team sport which is an enormous shift in the health care delivery paradigm. 11. PHM requires a fundamental change in the mindset of physicians and reorganization of day-to-day operations. 12. Enhancing care transitions using new models. 13. Clinical integration of providers who coordinate and collaborate in the provision of care based on consistent guidelines, pathways, protocols, and desired outcomes. © HTS 3 2016 | Page 37

Opportunities/Strategies © HTS 3 2016 | Page 38
Contact Information If you would like to schedule a consultation or have questions, please contact: Diane Bradley Regional Chief Clinical Officer Email: Phone: © HTS 3 2016 | Page 39 diane. bradley@healthtech. S 3. com 585 -671 -2212
THANK YOU and Hope to See You For the Next Webinar on October 24, 2016: Data Analytics: The Key to Making Decisions Diane Bradley, Ph. D, RN, NEA-BC, CPHQ, FACHE, FACHCA Health. Tech. S 3 Diane. Bradley@healthtechs 3. com © HTS 3 2016 | Page 40 Building Leaders – Transforming Hospitals – Improving Care