Ovarian stimulation Overview Dr Mridula A Benjamin Dept
Ovarian stimulation Overview Dr. Mridula A. Benjamin Dept of Obs and Gyn RIPAS Hospital, Brunei
Objective n To highlight the rationale, principles and different protocols of ovarian stimulation in cases of intrauterine insemination (IUI)
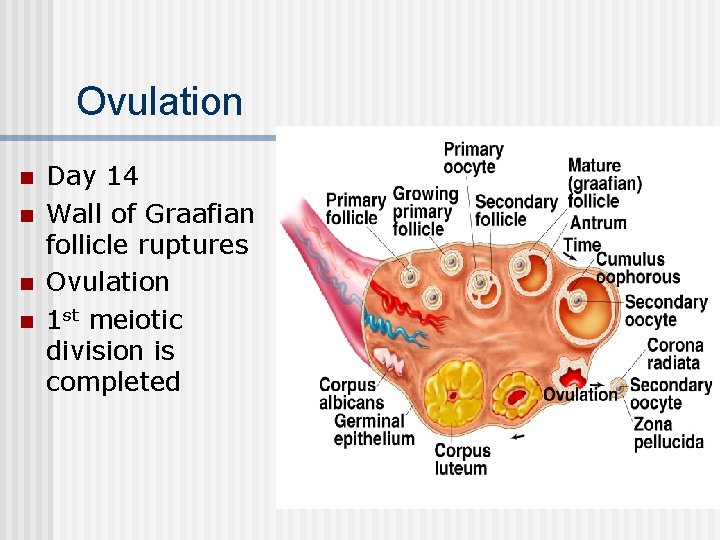
Ovulation n n Day 14 Wall of Graafian follicle ruptures Ovulation 1 st meiotic division is completed
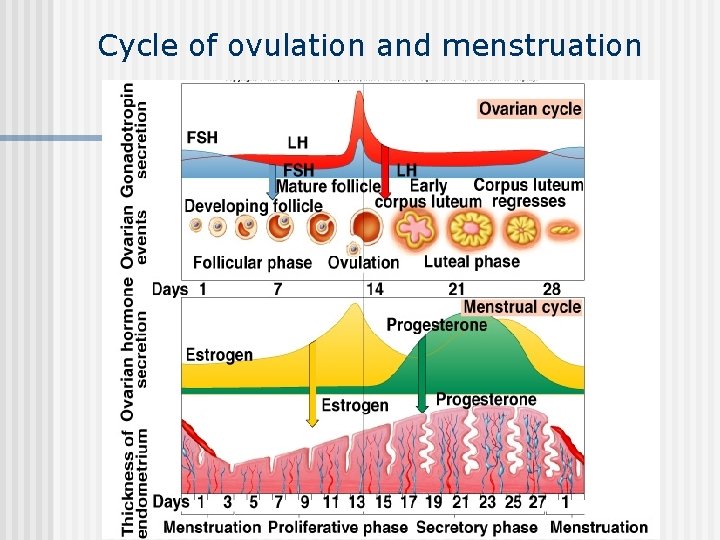
Cycle of ovulation and menstruation Insert fig. 20. 35
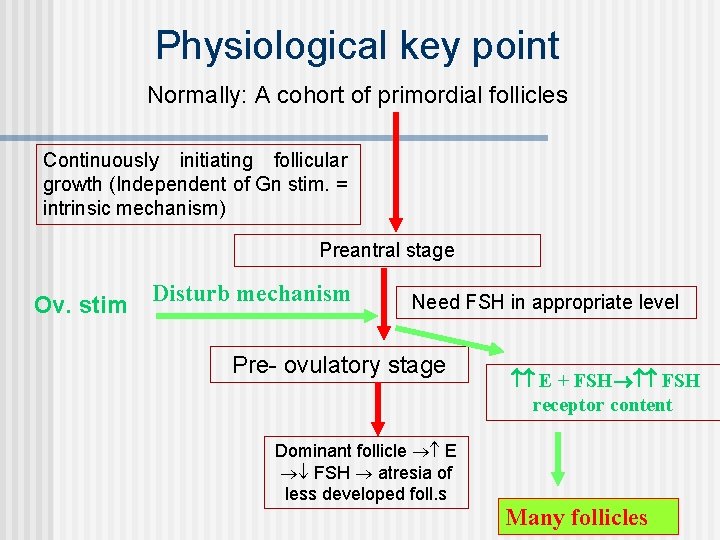
Physiological key point Normally: A cohort of primordial follicles Continuously initiating follicular growth (Independent of Gn stim. = intrinsic mechanism) Preantral stage Ov. stim Disturb mechanism Need FSH in appropriate level Pre- ovulatory stage Dominant follicle E FSH atresia of less developed foll. s E + FSH receptor content Many follicles
Aim of COH Regulated superovulation by turning off the patient’s own HPO system (down regulation) followed by stimulation. 1. 2. 3. 4. 5. Recruiting multiple follicles Control timing of ovulation (eggs can be surgically retrieved before they are ovulated) Prevention of premature LH surge To time the insemination Increase the pregnancy rate
Monitoring n n n To time HCG injection Decreases OHSS Decreases multiple pregnancy Follicular monitoring from D 9 S. estradiol levels did not give any additional information in various studies
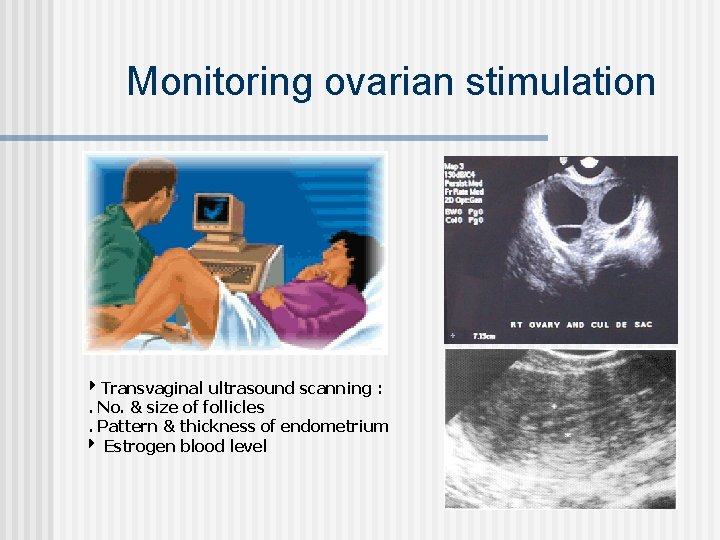
Monitoring ovarian stimulation Transvaginal ultrasound scanning : . No. & size of follicles. Pattern & thickness of endometrium Estrogen blood level
Optimum ovarian stimulation for IUI 2 – 3 follicles with Ø 18 – 19 mm. n Endometrium 9 mm thick & trilaminar. n IUI between Cycle D 13 and D 16, 36 -40 hrs. from HCG inj. Cancellation : 6 follicles 15 mm irrespective of E 2 level n
Classification n n WHO I - Hypothalamic pituitary failure (Hypogonadotrophic hypogonadism) Kallman’s, Sheehan’s, anorexia II - Hypothalamic pituitary dysfunction (PCOS) III – Ovulatory Failure – Hypergonadotrophic hypogonadism, Turner’s, autoimmune, mumps, RT, CT
Drugs for ov. stim. n n n n Anti oestrogens: Clomiphene Citrate, Tamoxifen Gonadotrophins: • HMG • highly purified ur FSH • Rec. FSH Gn. RH (pulsatile) Gn. RHa (intranasal-S. C- I. M) Gn. RH ant (involved in final steps of oocyte maturation) HCG Bromocriptine, Metformin, Letrozole
Which drug to choose for IUI? Drug Cost, Drug availability and Patient acceptability n CC is effective for young women with good prognosis n Remaining cases h. MG or FSH would be the preferable drug n r. FSH Vs Urinary preparations: no difference in clinical pregnancy rate n No advantage in routinely using Gn. Rh-a in conjunction with gonadotrophins for ovulation stimulation At the moment one should use the least expensive medication.
Anti Estrogens n n § § n n Clomiphene Most widely, 35 yrs. 1962 Ease of adm. , minimal side effects Clomiphene is a triphenylethylene derivative distantly related to diethylstilbestrol The commercially available form is dihydrogen citrate salt (clomiphene citrate) Contains two stereoisomers: zu-clomiphene (38 %) and en-clomiphene (62 %)
Pharmacology n n n Selective estrogen receptor modulator (similar to tamoxifen and raloxifene) Competitive inhibitors of estrogen binding to estrogen receptors Mixed agonist and antagonist activity depending upon the target tissue
Mech of action n n Pituitary action: Increases the gonadotropin response to Gn. RH Ovarian actions: Secondary to effects of elevated FSH and LH on ovarian follicular development Uterus, cervix, and vagina: antiestrogen Cervical mucous: decrease in the quality and quantity of cervical mucous with doses 100 mg/day

Indication n n n WHO class 2 Subfertility secondary to oligoovulation Anovulation in normogonadotropic Normoprolactinemic Euthyroid women Polycystic ovary syndrome
Dosage n n n n Usually first line drug Normal estrogenized females 50 mg D 2 - D 6 Max dose 200 mg Same dose at ovulation for 6 cycles Ovulation- 60 -85%, preg- 30 -40% No increase in abortion / cong. malformation
Problems with CC n n n Long lasting (till 14 -22 day of cycle) subclinical pregnancy loss compared to normal population LH sec > FSH miscarriage Anti E (cx &endometrium) Side effect : -Minor (nausea, vomiting, flush, hair loss, disturbed vision, bloatedness), OHSS, multiple pregnancy- 5%, ovarian ca
Tamoxifen n 20 -40 mg D 2 - D 6 Not licensed As effective as Clomiphene
Gonadotropins Unlike CC – Gn acts directly on the ovaries • HMG • Highly purified ur FSH (Metrodin – HP) • Rec. FSH (Gonal – F, Puregon)
Protocols 1. 2. 3. 4. 5. CC CC ± FSH or ± HMG Gn. Standard step-up protocol Gn. Low dose step-up, step-down protocol (Sequential)
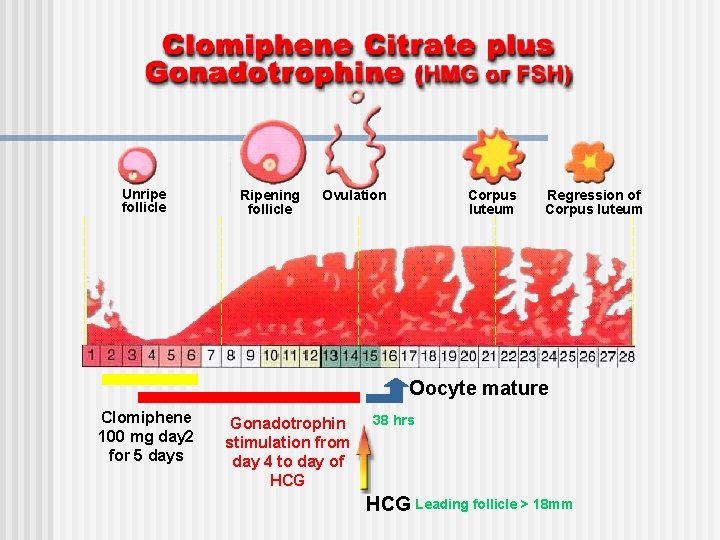
Unripe follicle Ripening follicle Ovulation Corpus luteum Regression of Corpus luteum Oocyte mature Clomiphene 100 mg day 2 for 5 days Gonadotrophin stimulation from day 4 to day of HCG 38 hrs HCG Leading follicle > 18 mm
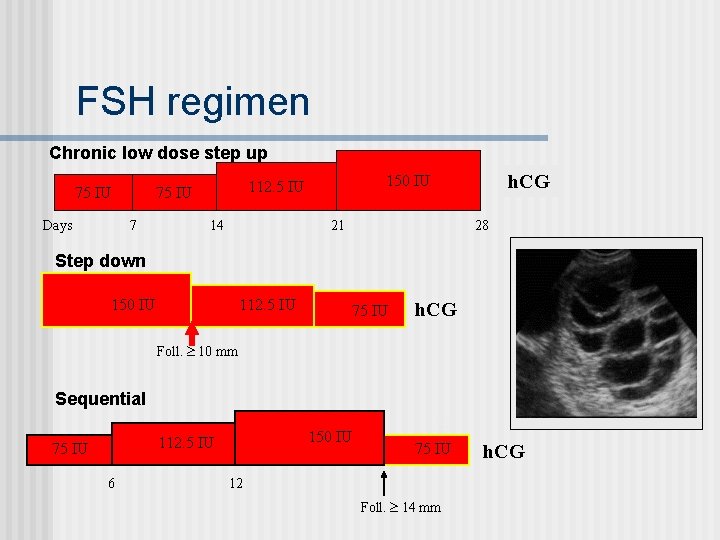
FSH regimen Chronic low dose step up 75 IU Days 7 14 h. CG 150 IU 112. 5 IU 75 IU 21 28 Step down 150 IU 112. 5 IU 75 IU h. CG Foll. 10 mm Sequential 150 IU 112. 5 IU 75 IU 6 ½ 75 IU 12 Foll. 14 mm h. CG
Complications § Multifetal pregnancy n (36%) OHSS (14%)- Life threatening More common in Young/ lean/ low BMI/ PCOS HCG triggering Prev. OHSS Pregnancy
Insulin sensitizing drugs n n n Metformin Oral, 1500 -2000 mg Hyperinsulinaemia, hyperandrogenaemia RCT- clomiphene resistant pts. , use of metformin & CC produced significant improvement Recent study- Letrozole & metformin also showed promising results Metaanalysis of metformin co-adm during gonadotrophin induction in PCOS has been inconclusive
Aromatase inhibitors n n n Letrozole- 3 rd generation 2. 5 mg OD/BD on D 3 -7 Breast cancer in postmenopausal for several years Lacks unfavourable effects on endometrium seen with CC Initial evidence is encouraging, but larger trials are required
Hyperprolactinaemia n n n Dopamine agonists- bromocriptine, cabergoline No MP, no monitoring Cabergoline more effective Micro- 80% / 85% Macro- 65% / 50% N, V, vertigo, hypotension, headache, drowsiness
Gn. RH analogues n n Gn. RHa - high levels of LH Metaanalysis - no clear advantage of routine use in conjunction with gonadotrophins in pts. with clomiphene resistant cases Increases cost, OHSS, multiple pregnancy Some say lessens overall cost by reducing gonadotrophin requirement by 50%
Dexamethasone or OCP n n n ? ? Improves pregnancy rates in anovulatory women in WHO group 2 with DHEA-S levels greater than 2. 0 mcg/ml OCP to regularise the cycles before stimulation Meprate withdrawal
Surgical Laparoscopic ovarian drilling n Armer’s criteria n Ovulation- 90% n Pregnancy- 70% n One step treatment n Within one year n Reduced MP & OHSS n
Ovulation trigger n n n Natural cycle- raised Oestradiol leads to LH surge Ov. stimulation- unpredictable HCG( pregnyl, Profasi) Recombinant form available(Ovitrelle) 5000 - 10, 000 IU S/C Causes higher luteal phase conc. of progesterone.
Conclusion n n n Ovarian stimulation is the fundamental tool of subfertility treatment Different options pose challenges Choice depends on doctors expertise and patients condition, choice Increases the pregnancy rate Time the IUI Judicious monitoring to avoid complications
Thank you
- Slides: 33