Outline v Common Conditions of the Elbow Wrist
Outline v Common Conditions of the Elbow, Wrist and Hand v For each topic: v v What is it? Brief Overview How do patients present? How is the condition diagnosed? Treatment options Question and answer session

Tennis Elbow
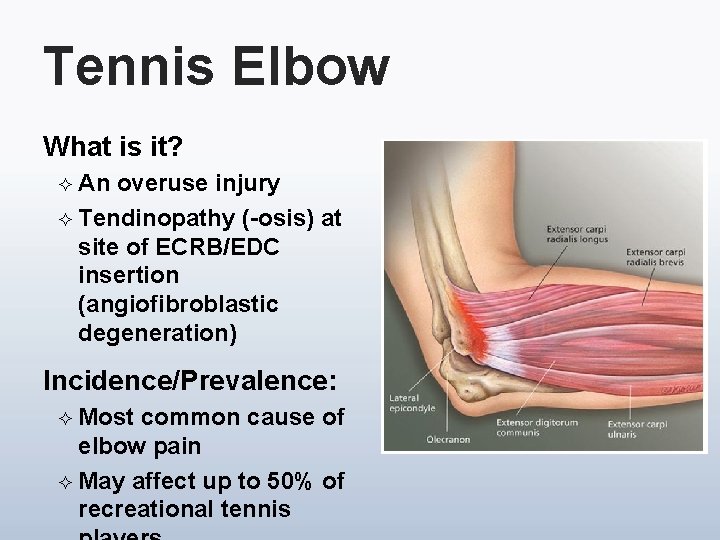
Tennis Elbow What is it? ² An overuse injury ² Tendinopathy (-osis) at site of ECRB/EDC insertion (angiofibroblastic degeneration) Incidence/Prevalence: ² Most common cause of elbow pain ² May affect up to 50% of recreational tennis
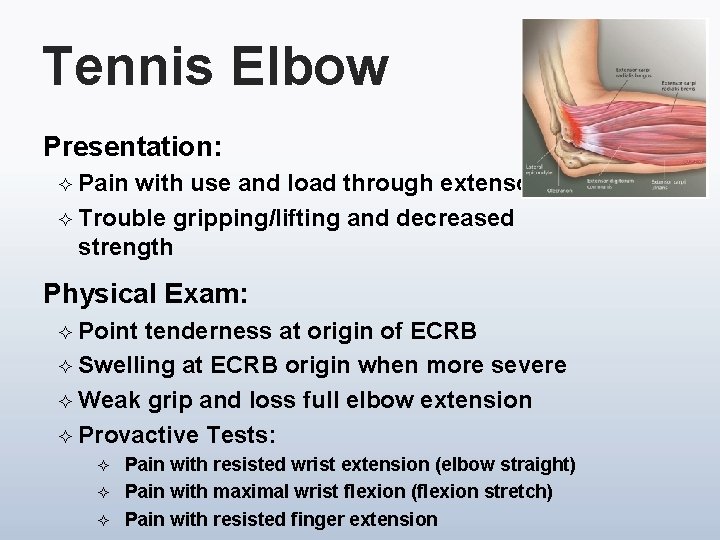
Tennis Elbow Presentation: ² Pain with use and load through extensors ² Trouble gripping/lifting and decreased strength Physical Exam: ² Point tenderness at origin of ECRB ² Swelling at ECRB origin when more severe ² Weak grip and loss full elbow extension ² Provactive Tests: ² ² ² Pain with resisted wrist extension (elbow straight) Pain with maximal wrist flexion (flexion stretch) Pain with resisted finger extension
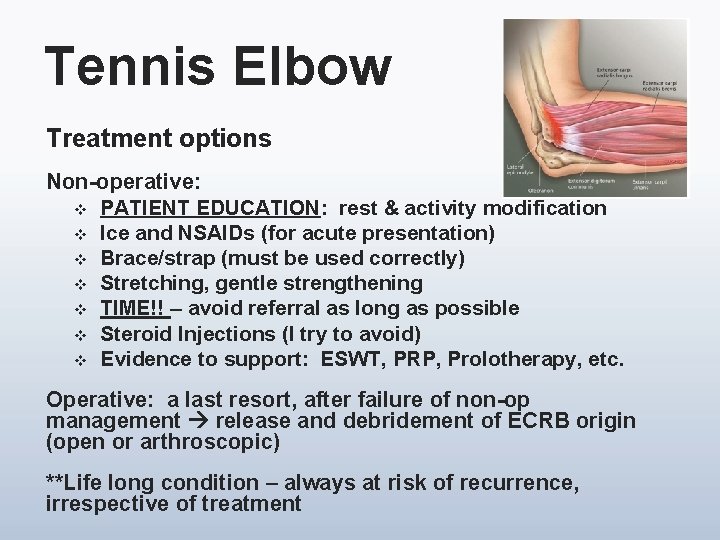
Tennis Elbow Treatment options Non-operative: v PATIENT EDUCATION: rest & activity modification v Ice and NSAIDs (for acute presentation) v Brace/strap (must be used correctly) v Stretching, gentle strengthening v TIME!! – avoid referral as long as possible v Steroid Injections (I try to avoid) v Evidence to support: ESWT, PRP, Prolotherapy, etc. Operative: a last resort, after failure of non-op management release and debridement of ECRB origin (open or arthroscopic) **Life long condition – always at risk of recurrence, irrespective of treatment

Golfer’s Elbow
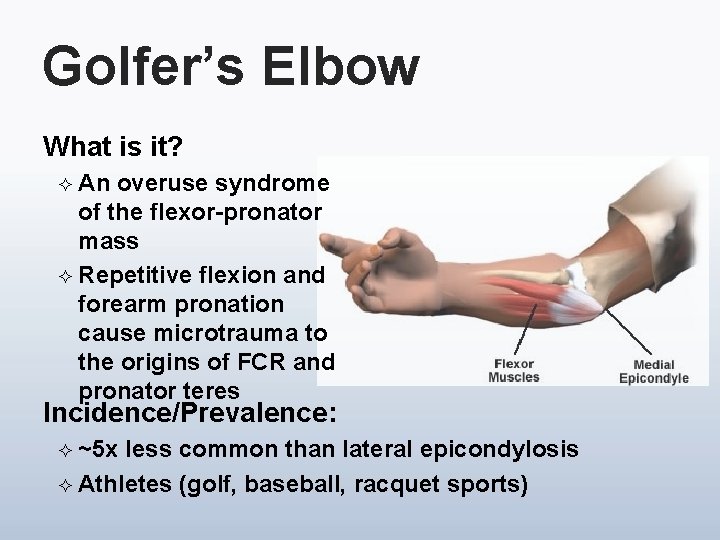
Golfer’s Elbow What is it? ² An overuse syndrome of the flexor-pronator mass ² Repetitive flexion and forearm pronation cause microtrauma to the origins of FCR and pronator teres Incidence/Prevalence: ² ~5 x less common than lateral epicondylosis ² Athletes (golf, baseball, racquet sports)
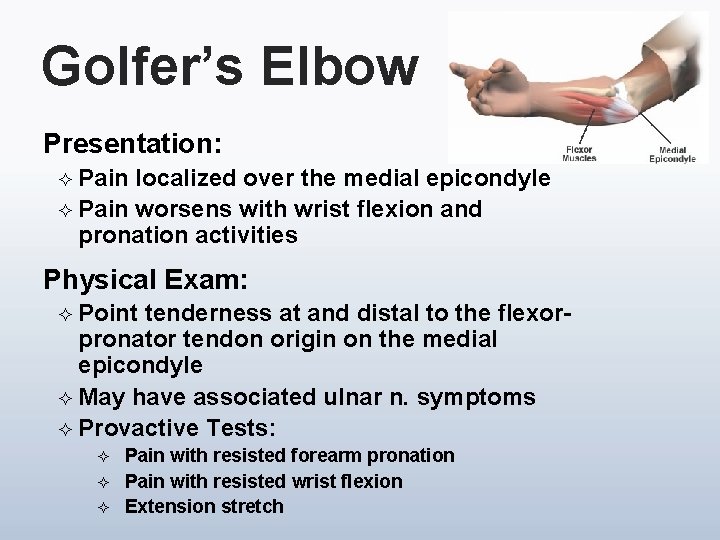
Golfer’s Elbow Presentation: ² Pain localized over the medial epicondyle ² Pain worsens with wrist flexion and pronation activities Physical Exam: ² Point tenderness at and distal to the flexorpronator tendon origin on the medial epicondyle ² May have associated ulnar n. symptoms ² Provactive Tests: ² ² ² Pain with resisted forearm pronation Pain with resisted wrist flexion Extension stretch
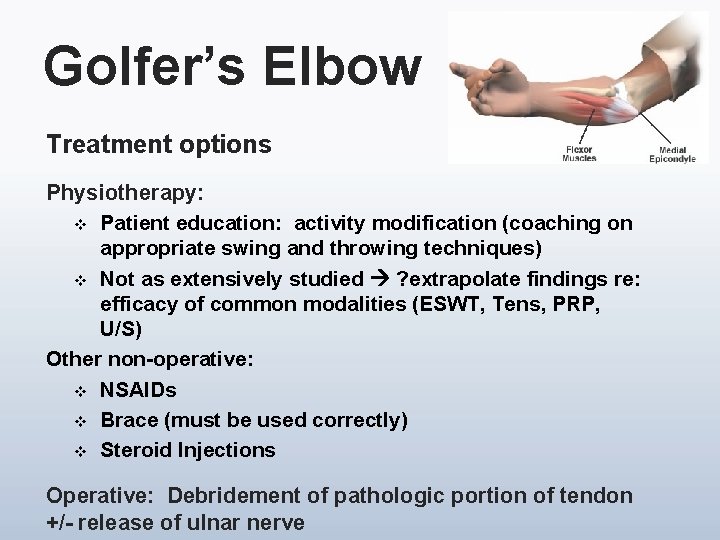
Golfer’s Elbow Treatment options Physiotherapy: v Patient education: activity modification (coaching on appropriate swing and throwing techniques) v Not as extensively studied ? extrapolate findings re: efficacy of common modalities (ESWT, Tens, PRP, U/S) Other non-operative: v NSAIDs v Brace (must be used correctly) v Steroid Injections Operative: Debridement of pathologic portion of tendon +/- release of ulnar nerve
Radial Tunnel Syndrome
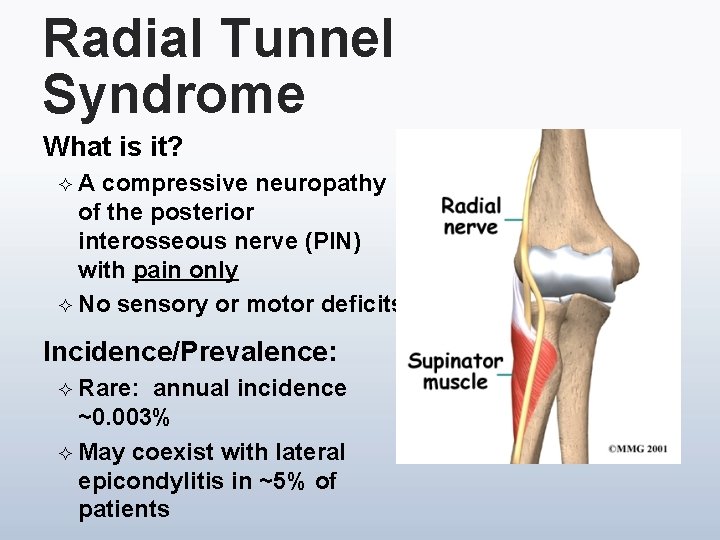
Radial Tunnel Syndrome What is it? ²A compressive neuropathy of the posterior interosseous nerve (PIN) with pain only ² No sensory or motor deficits Incidence/Prevalence: ² Rare: annual incidence ~0. 003% ² May coexist with lateral epicondylitis in ~5% of patients
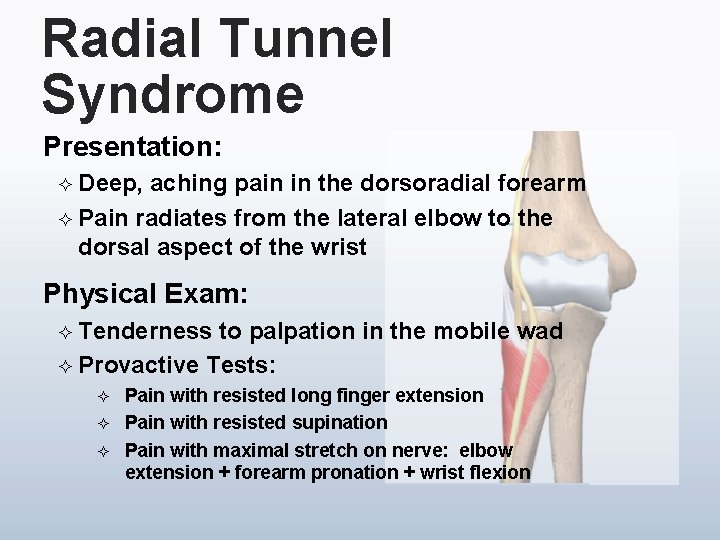
Radial Tunnel Syndrome Presentation: ² Deep, aching pain in the dorsoradial forearm ² Pain radiates from the lateral elbow to the dorsal aspect of the wrist Physical Exam: ² Tenderness to palpation in the mobile wad ² Provactive Tests: ² ² ² Pain with resisted long finger extension Pain with resisted supination Pain with maximal stretch on nerve: elbow extension + forearm pronation + wrist flexion
Radial Tunnel Syndrome Treatment options Physiotherapy: ² Patient education: activity modification – avoidance of prolonged periods of elbow extension and forearm pronation and wrist flexion ² Stretching ² Primarily anecdotal ‘evidence’ only ² Encourage conservative and avoid referral Other non-operative treatments: ² NSAIDs ² Splinting ² Steroid Injections Operative: Radial tunnel release
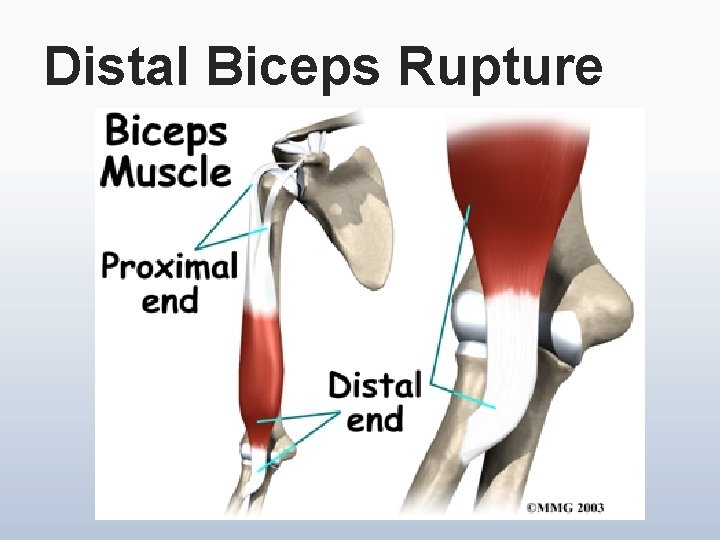
Distal Biceps Rupture
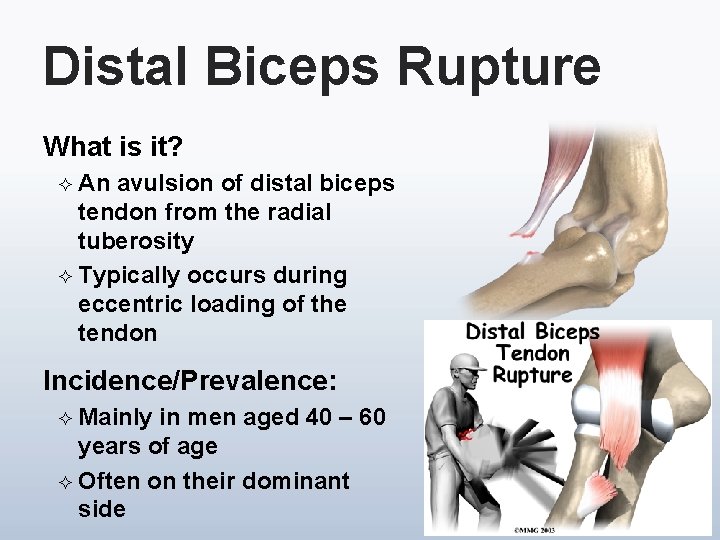
Distal Biceps Rupture What is it? ² An avulsion of distal biceps tendon from the radial tuberosity ² Typically occurs during eccentric loading of the tendon Incidence/Prevalence: ² Mainly in men aged 40 – 60 years of age ² Often on their dominant side
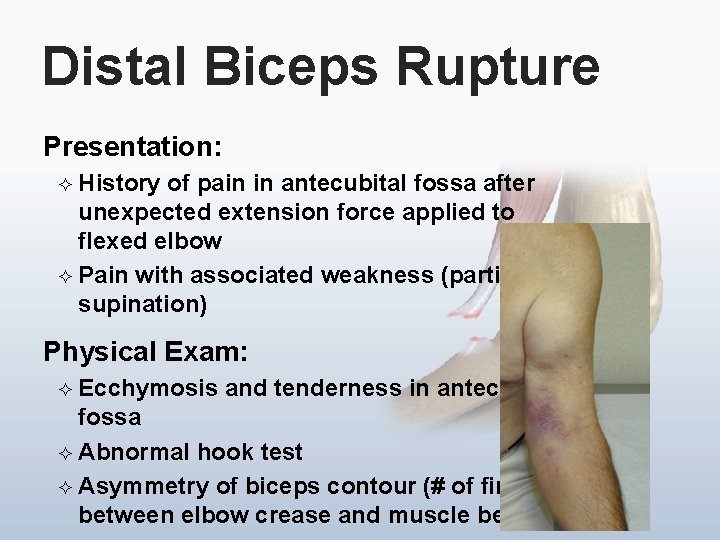
Distal Biceps Rupture Presentation: ² History of pain in antecubital fossa after unexpected extension force applied to flexed elbow ² Pain with associated weakness (particularly supination) Physical Exam: ² Ecchymosis and tenderness in antecubital fossa ² Abnormal hook test ² Asymmetry of biceps contour (# of fingers between elbow crease and muscle belly)
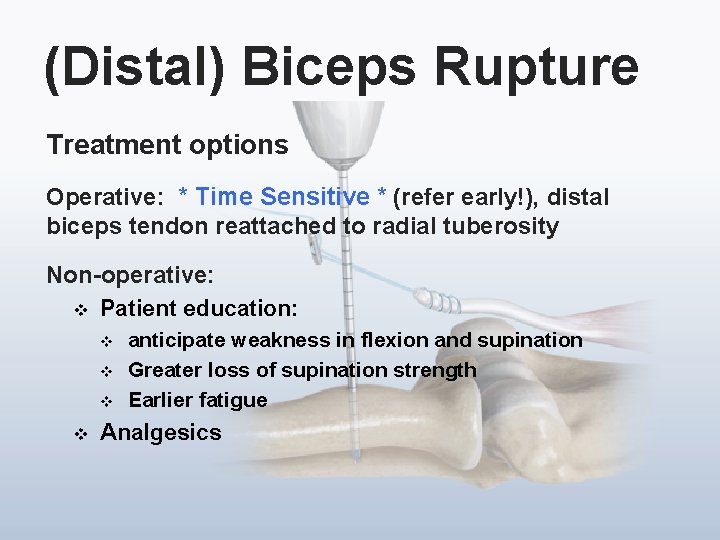
(Distal) Biceps Rupture Treatment options Operative: * Time Sensitive * (refer early!), distal biceps tendon reattached to radial tuberosity Non-operative: v Patient education: v v anticipate weakness in flexion and supination Greater loss of supination strength Earlier fatigue Analgesics
Thrower’s Elbow
Thrower’s Elbow
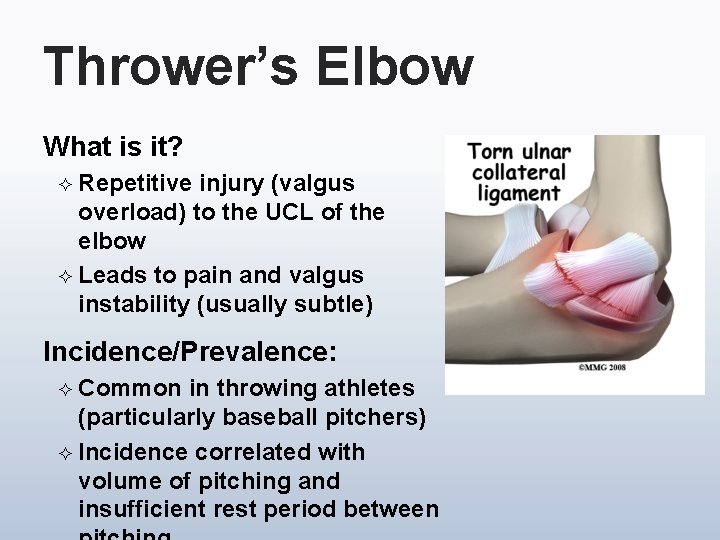
Thrower’s Elbow What is it? ² Repetitive injury (valgus overload) to the UCL of the elbow ² Leads to pain and valgus instability (usually subtle) Incidence/Prevalence: ² Common in throwing athletes (particularly baseball pitchers) ² Incidence correlated with volume of pitching and insufficient rest period between
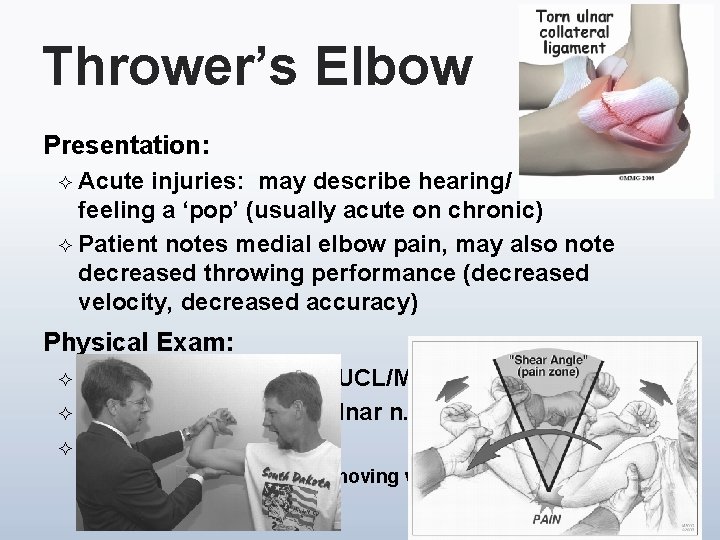
Thrower’s Elbow Presentation: ² Acute injuries: may describe hearing/ feeling a ‘pop’ (usually acute on chronic) ² Patient notes medial elbow pain, may also note decreased throwing performance (decreased velocity, decreased accuracy) Physical Exam: ² Point tenderness near UCL/MCL origin ² May have associated ulnar n. findings ² Provactive Tests: ² ² Valgus stress test and moving valgus stress test Milking maneuver
Thrower’s Elbow Treatment options Physiotherapy: v Flexor-pronator strengthening (after period of rest) v Patient education: improved throwing mechanics v Stretching Other non-operative treatments: v NSAIDs Operative: Medial Collateral Ligament Reconstruction (Tommy John Procedure)

Carpal Tunnel Syndrome
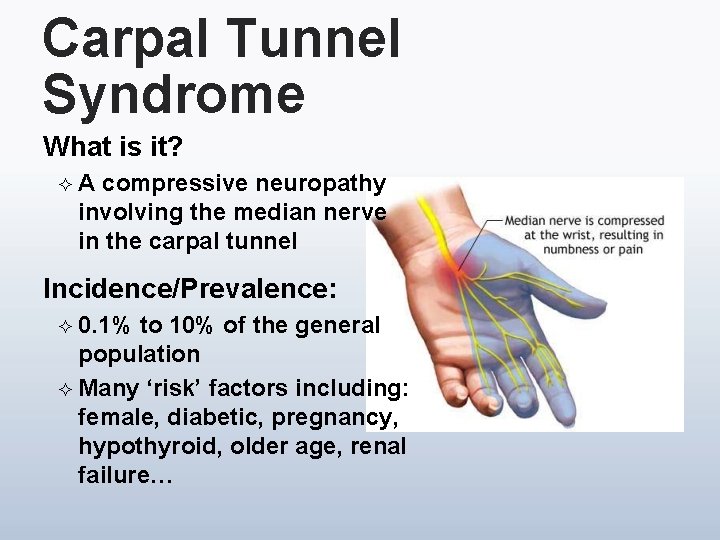
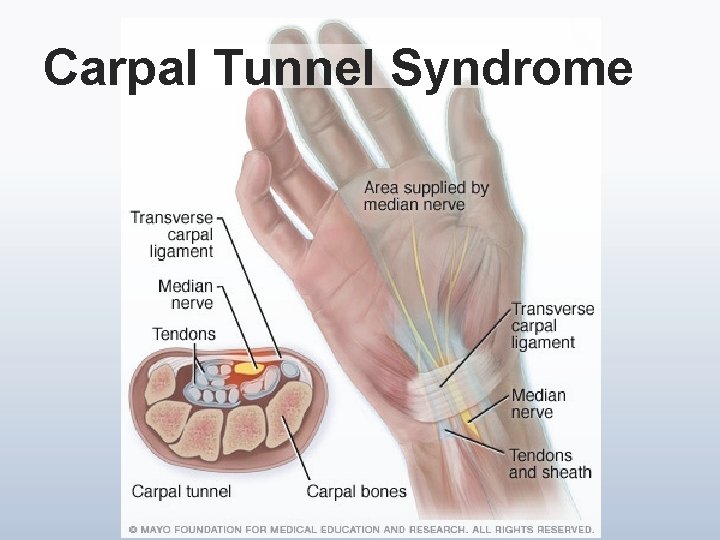
Carpal Tunnel Syndrome What is it? ²A compressive neuropathy involving the median nerve in the carpal tunnel Incidence/Prevalence: ² 0. 1% to 10% of the general population ² Many ‘risk’ factors including: female, diabetic, pregnancy, hypothyroid, older age, renal failure…
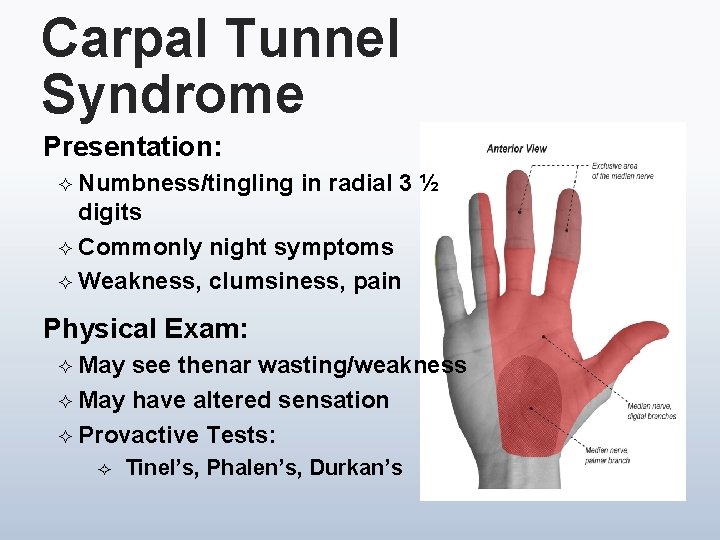
Carpal Tunnel Syndrome Presentation: ² Numbness/tingling in radial 3 ½ digits ² Commonly night symptoms ² Weakness, clumsiness, pain Physical Exam: ² May see thenar wasting/weakness ² May have altered sensation ² Provactive Tests: ² Tinel’s, Phalen’s, Durkan’s
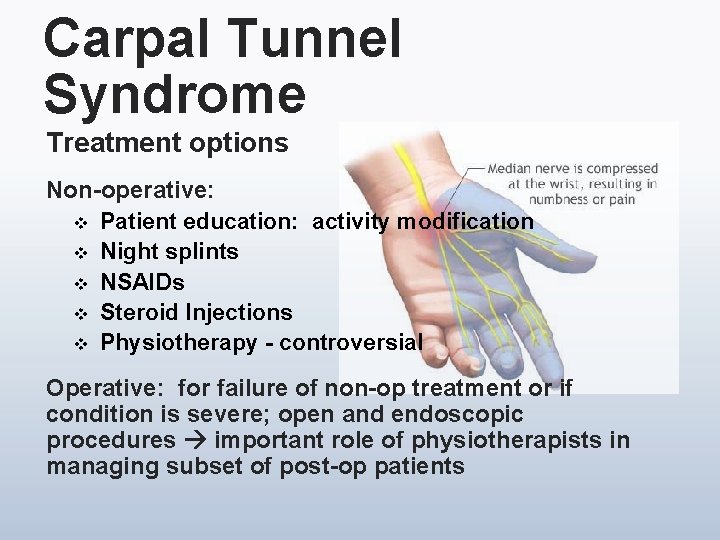
Carpal Tunnel Syndrome Treatment options Non-operative: v Patient education: activity modification v Night splints v NSAIDs v Steroid Injections v Physiotherapy - controversial Operative: for failure of non-op treatment or if condition is severe; open and endoscopic procedures important role of physiotherapists in managing subset of post-op patients
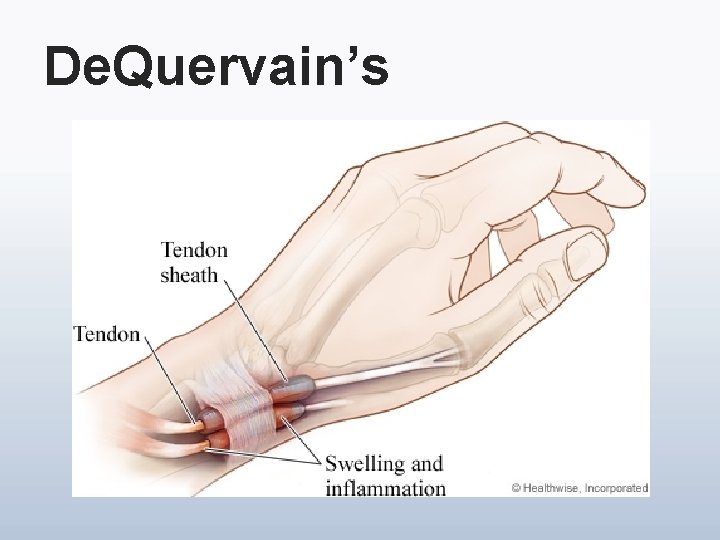
De. Quervain’s
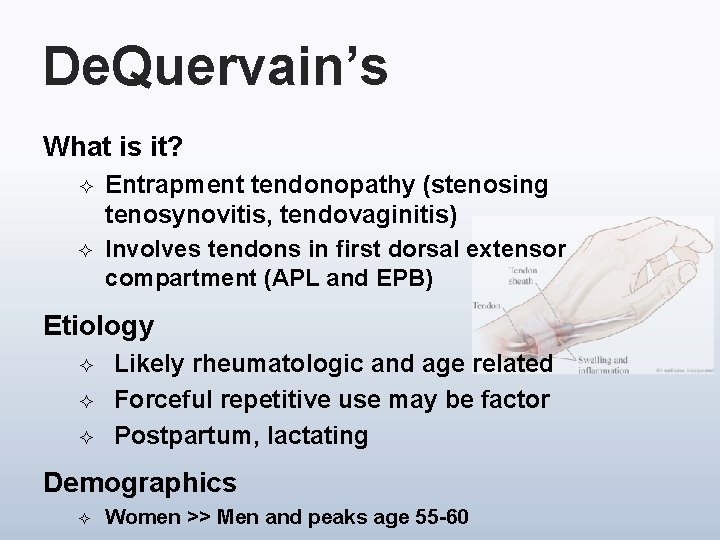
De. Quervain’s What is it? ² ² Entrapment tendonopathy (stenosing tenosynovitis, tendovaginitis) Involves tendons in first dorsal extensor compartment (APL and EPB) Etiology ² ² ² Likely rheumatologic and age related Forceful repetitive use may be factor Postpartum, lactating Demographics ² Women >> Men and peaks age 55 -60
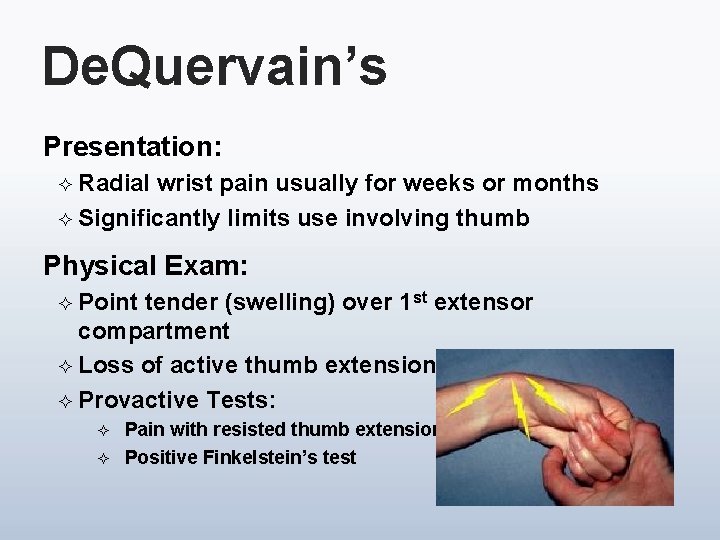
De. Quervain’s Presentation: ² Radial wrist pain usually for weeks or months ² Significantly limits use involving thumb Physical Exam: ² Point tender (swelling) over 1 st extensor compartment ² Loss of active thumb extension ² Provactive Tests: ² ² Pain with resisted thumb extension Positive Finkelstein’s test
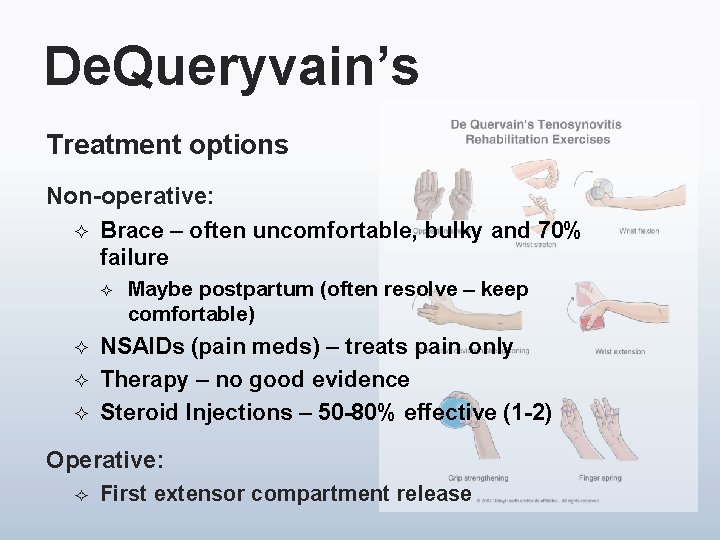
De. Queryvain’s Treatment options Non-operative: ² Brace – often uncomfortable, bulky and 70% failure ² ² Maybe postpartum (often resolve – keep comfortable) NSAIDs (pain meds) – treats pain only Therapy – no good evidence Steroid Injections – 50 -80% effective (1 -2) Operative: ² First extensor compartment release
Wrist Ganglion
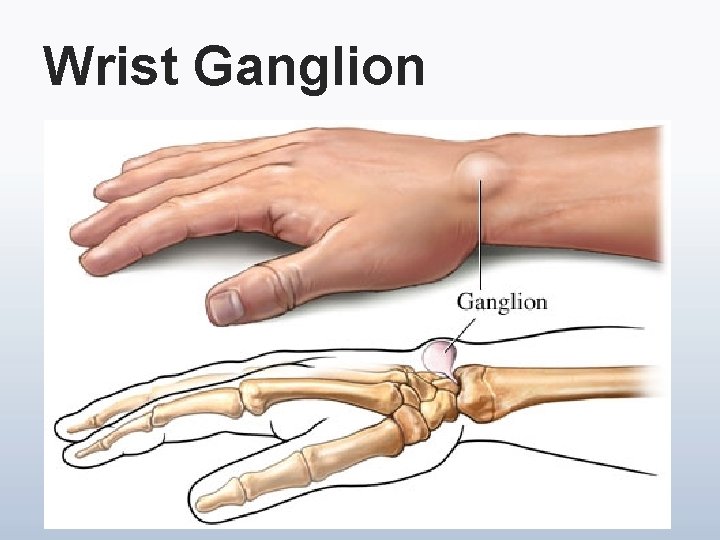
Wrist Ganglion What is it? ² Mucin filled cyst attached to underlying joint capsule Incidence/Prevalence: ² Relatively common ² More prevalent in women ² 70% in 2 nd to 4 th decades ² 10% may have traumatic etiology
Wrist Ganglion Presentation: ² Dorsal wrist mass, usually over scapholunate interval (can be anywhere over dorsal wrist – long stalk) ² Usually cosmetic; may have associated pain ² Size and symptoms fluctuate. May disappear. Physical Exam: ² Fixed dorsal fluctuant mass, may be tender ² May have pain with forced wrist extension ² Transillumination
Wrist Ganglion Diagnosis: ² Transillumination and aspiration are diagnostic ² Must rule out other masses and tumors ² MRI for occult ganglion (dorsal pain NYD) Treatment: ² Educate patient; encourage observational treatment ² May resolve on own ² Aspiration/injection steroid 20 -30% effective (I have had little success and have all but abandoned) ² Bible Surgery – open or arthroscopic excision
Wrist Sprain

Wrist Sprain What is it? ² Traumatic injury usually FOOSH, possible torsion ² A ligament injury (minor strain to rupture) Incidence/Prevalence: ² Common in sports & other outdoor activities ² Middle aged doctors who take up mountain biking
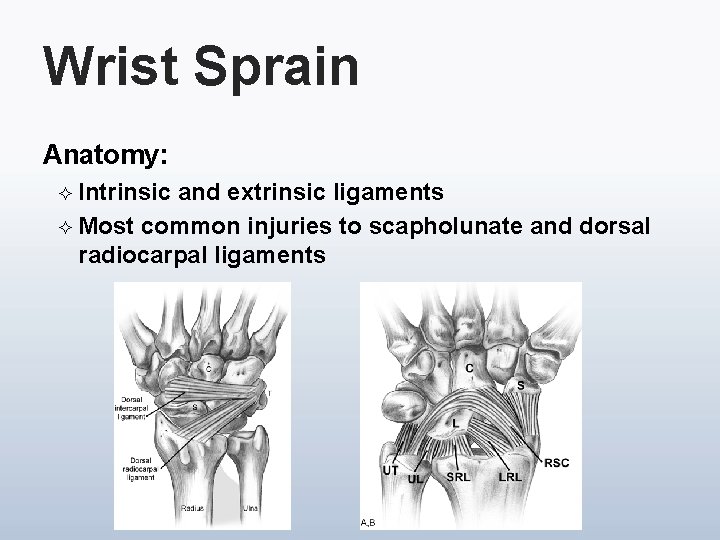
Wrist Sprain Anatomy: ² Intrinsic and extrinsic ligaments ² Most common injuries to scapholunate and dorsal radiocarpal ligaments
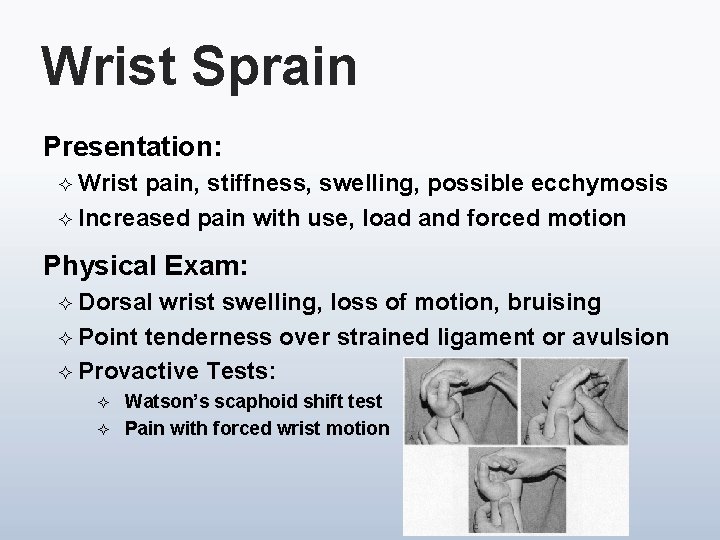
Wrist Sprain Presentation: ² Wrist pain, stiffness, swelling, possible ecchymosis ² Increased pain with use, load and forced motion Physical Exam: ² Dorsal wrist swelling, loss of motion, bruising ² Point tenderness over strained ligament or avulsion ² Provactive Tests: ² ² Watson’s scaphoid shift test Pain with forced wrist motion
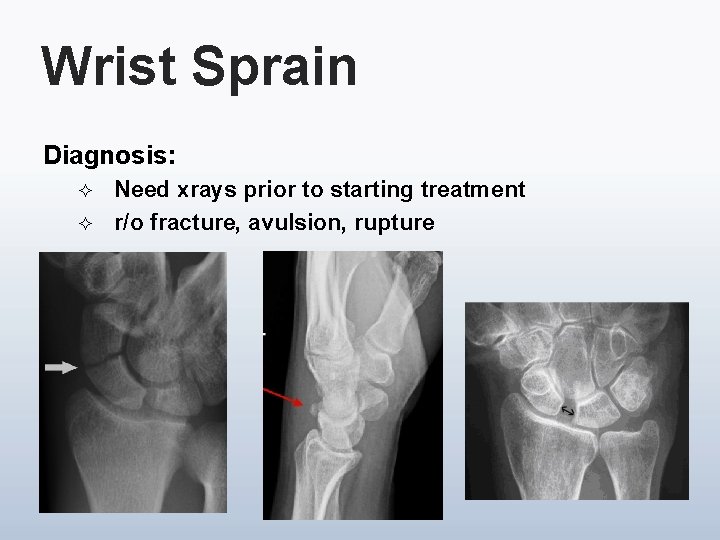
Wrist Sprain Diagnosis: ² ² Need xrays prior to starting treatment r/o fracture, avulsion, rupture

Wrist Sprain Treatment options Non-operative: ² RICE for acute injury ² ² ² Pain meds Wrap, tape, brace Time!!! Cortisone Therapy – as for all sprains ROM, proprioception, strengthening, modalities Operative: ² ² ² Acute ligament repair for rupture Scope for failed non surgical treatment

First CMC Joint OA
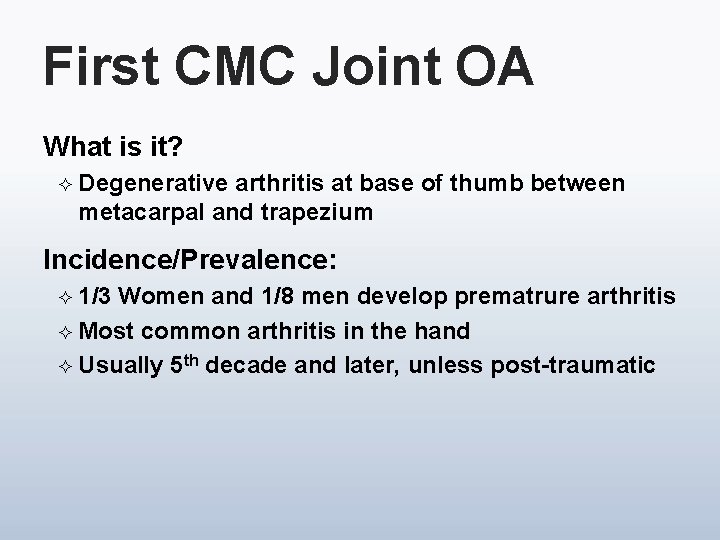
First CMC Joint OA What is it? ² Degenerative arthritis at base of thumb between metacarpal and trapezium Incidence/Prevalence: ² 1/3 Women and 1/8 men develop prematrure arthritis ² Most common arthritis in the hand ² Usually 5 th decade and later, unless post-traumatic
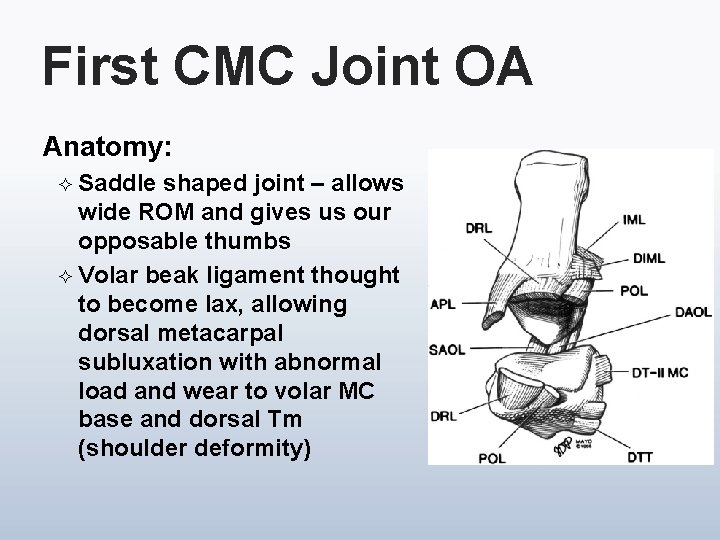
First CMC Joint OA Anatomy: ² Saddle shaped joint – allows wide ROM and gives us our opposable thumbs ² Volar beak ligament thought to become lax, allowing dorsal metacarpal subluxation with abnormal load and wear to volar MC base and dorsal Tm (shoulder deformity)
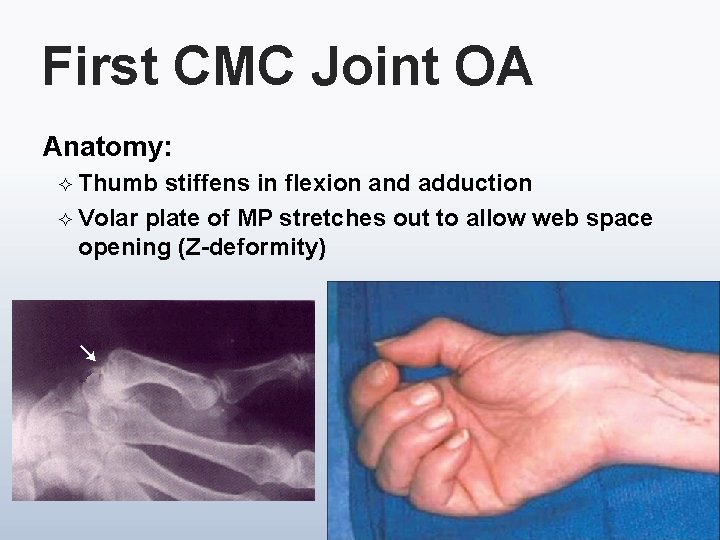
First CMC Joint OA Anatomy: ² Thumb stiffens in flexion and adduction ² Volar plate of MP stretches out to allow web space opening (Z-deformity)
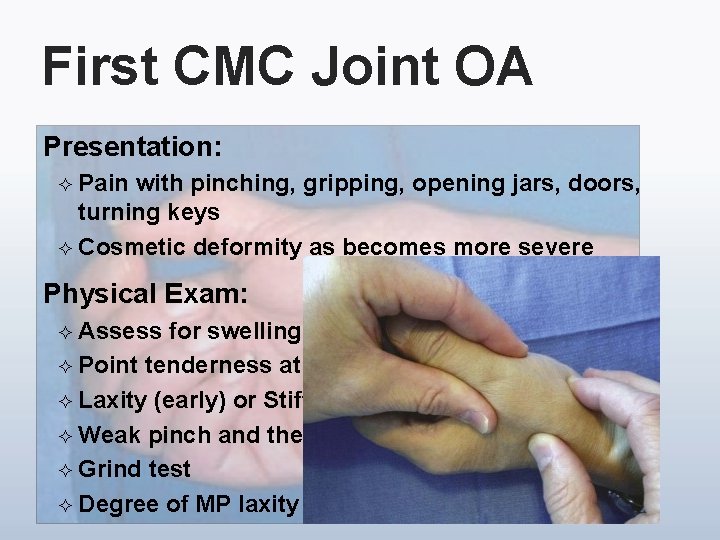
First CMC Joint OA Presentation: ² Pain with pinching, gripping, opening jars, doors, turning keys ² Cosmetic deformity as becomes more severe Physical Exam: ² Assess for swelling, shoulder and Z-deformity ² Point tenderness at joint, especially volarly ² Laxity (early) or Stiffness (late) ² Weak pinch and thenar wasting ² Grind test ² Degree of MP laxity

First CMC Joint OA Treatment options v Need to get radiographs to assess stage Non-operative: v v v Most patients respond well/adequately Patient education and activity modification NSAIDs Bracing (soft or rigid) – up to 6 weeks if acute Steroid and HA injections Exercises and therapy/OT
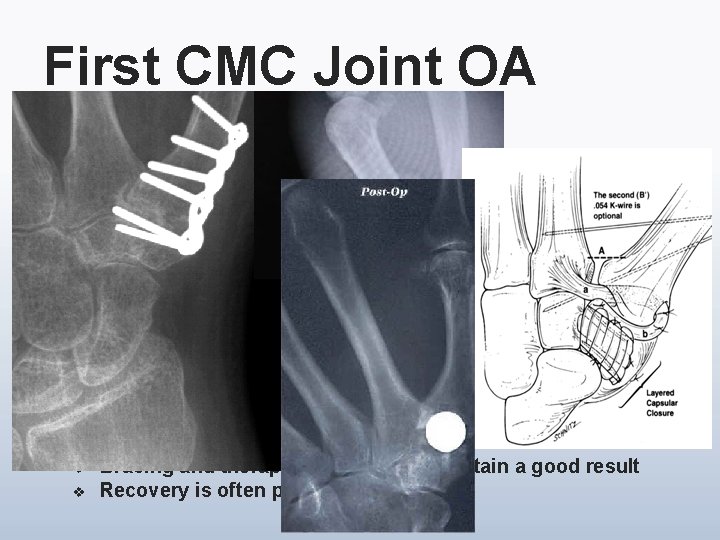
First CMC Joint OA Operative: Failure of conservative measures v Early v v v Ligament reconstruction Metacarpal extension osteotomy Arthroscopy Late v v v Ligament reconstruction tendon interposition (LRTI) Hematoma arthroplasty Joint replacement Fusion MP joint (possible fusion or volar capsulodesis) Post Surgical: v v Bracing and therapy are essential to obtain a good result Recovery is often prolonged
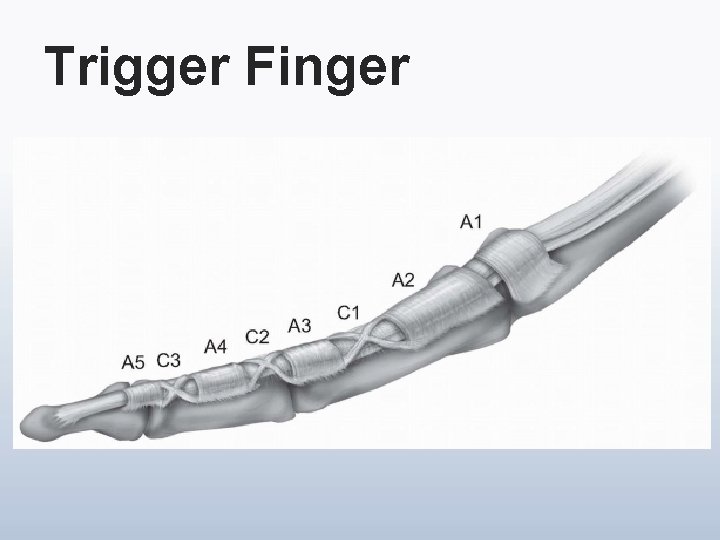
Trigger Finger
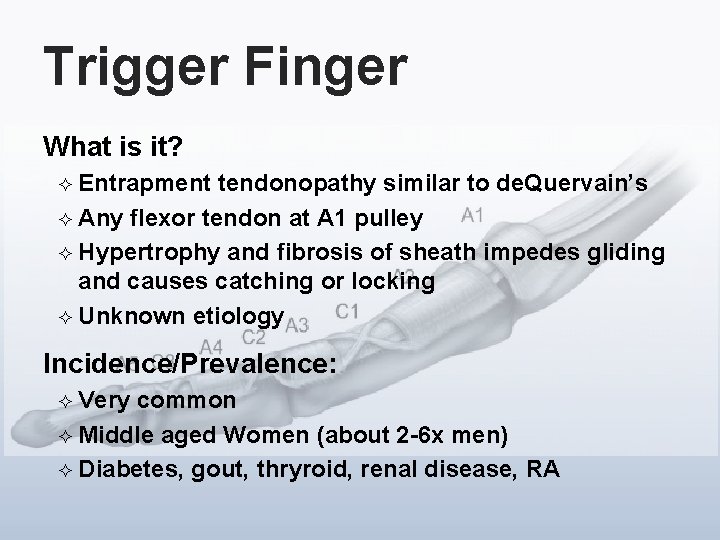
Trigger Finger What is it? ² Entrapment tendonopathy similar to de. Quervain’s ² Any flexor tendon at A 1 pulley ² Hypertrophy and fibrosis of sheath impedes gliding and causes catching or locking ² Unknown etiology Incidence/Prevalence: ² Very common ² Middle aged Women (about 2 -6 x men) ² Diabetes, gout, thryroid, renal disease, RA
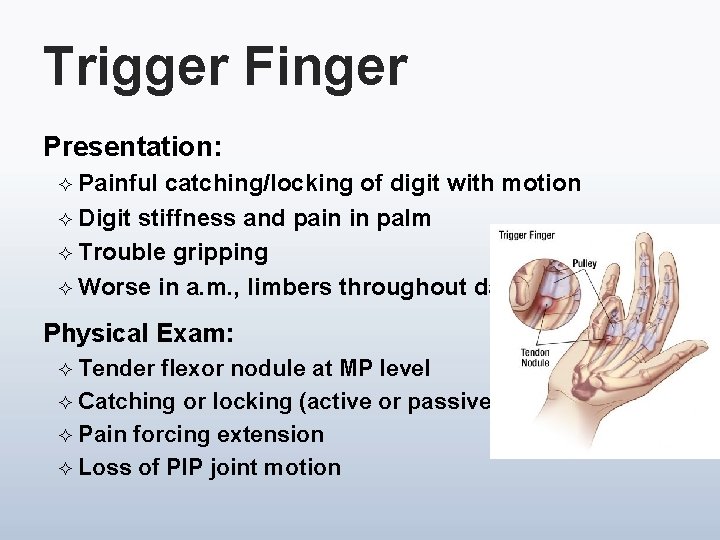
Trigger Finger Presentation: ² Painful catching/locking of digit with motion ² Digit stiffness and pain in palm ² Trouble gripping ² Worse in a. m. , limbers throughout day Physical Exam: Tender flexor nodule at MP level ² Catching or locking (active or passive) ² Pain forcing extension ² Loss of PIP joint motion ²

Trigger Finger Treatment options Non-operative: ² Injection steroid – about 80% cure with 2 injections ² Splinting – especially at night to prevent locking Operative: ² ² If fail 2 injections Open A 1 pulley release Percutaneous release (U/S? ) Therapy – for wound or stiffness problems
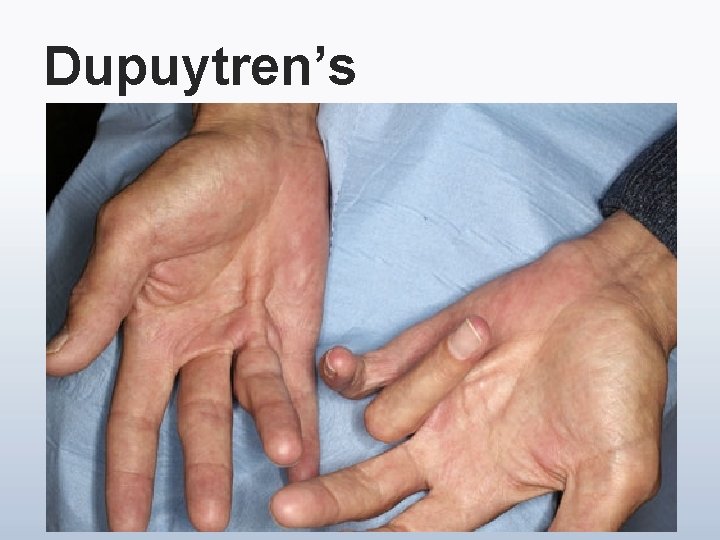
Dupuytren’s
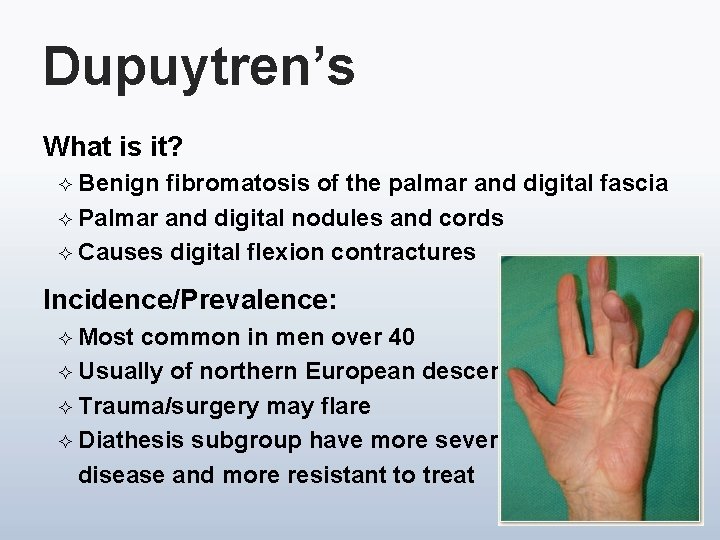
Dupuytren’s What is it? ² Benign fibromatosis of the palmar and digital fascia ² Palmar and digital nodules and cords ² Causes digital flexion contractures Incidence/Prevalence: ² Most common in men over 40 ² Usually of northern European descent ² Trauma/surgery may flare ² Diathesis subgroup have more severe disease and more resistant to treat
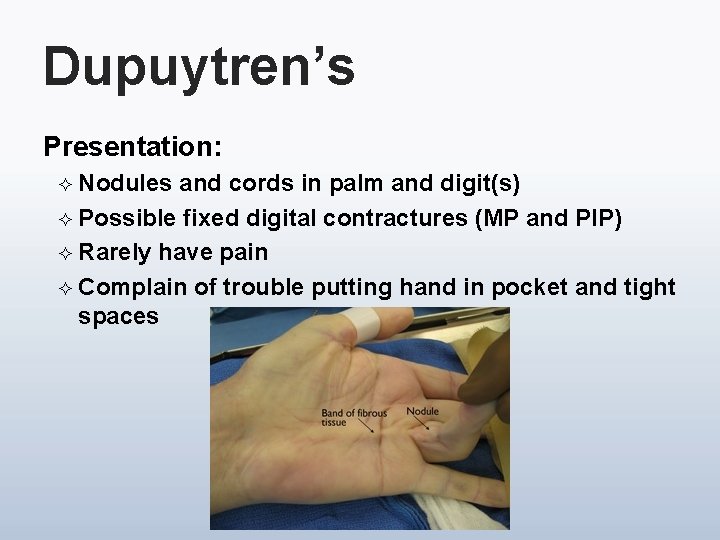
Dupuytren’s Presentation: ² Nodules and cords in palm and digit(s) ² Possible fixed digital contractures (MP and PIP) ² Rarely have pain ² Complain of trouble putting hand in pocket and tight spaces
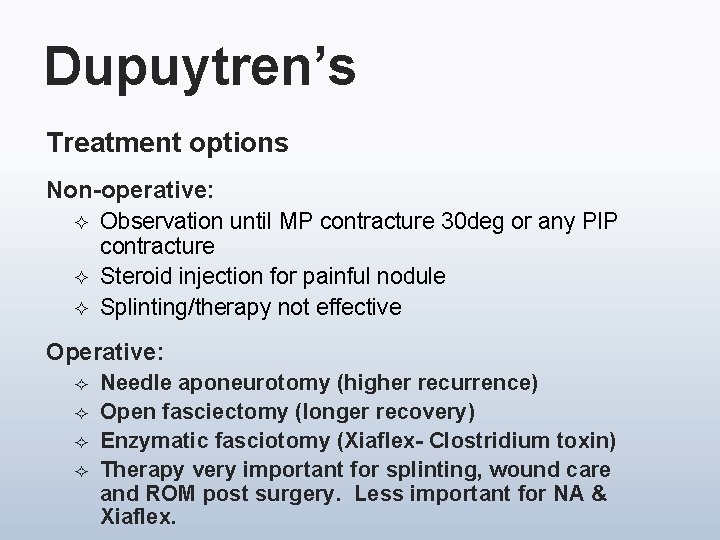
Dupuytren’s Treatment options Non-operative: ² Observation until MP contracture 30 deg or any PIP contracture ² Steroid injection for painful nodule ² Splinting/therapy not effective Operative: ² ² Needle aponeurotomy (higher recurrence) Open fasciectomy (longer recovery) Enzymatic fasciotomy (Xiaflex- Clostridium toxin) Therapy very important for splinting, wound care and ROM post surgery. Less important for NA & Xiaflex.

Dupuytren’s

Questions?
- Slides: 61