Outline Dementia and delirium facts and figures Patients










- Slides: 36
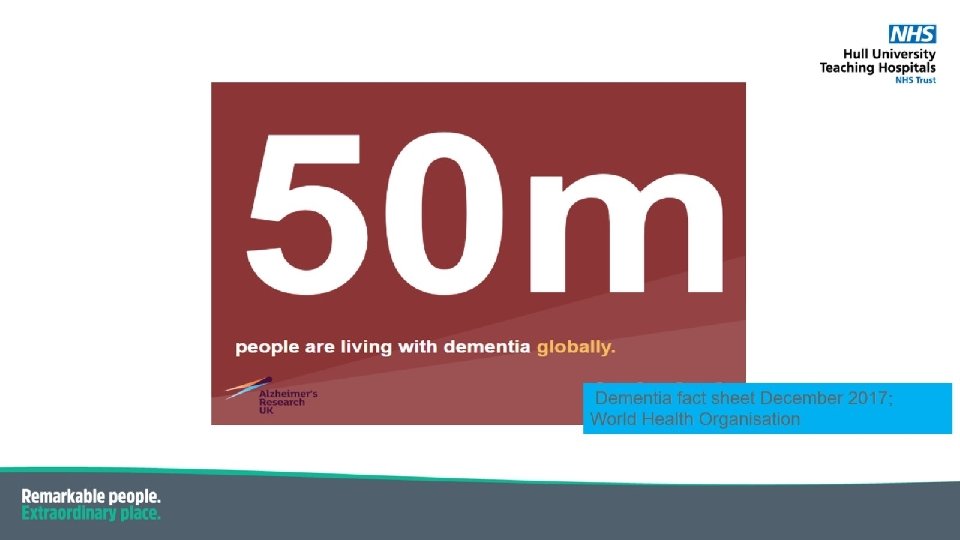
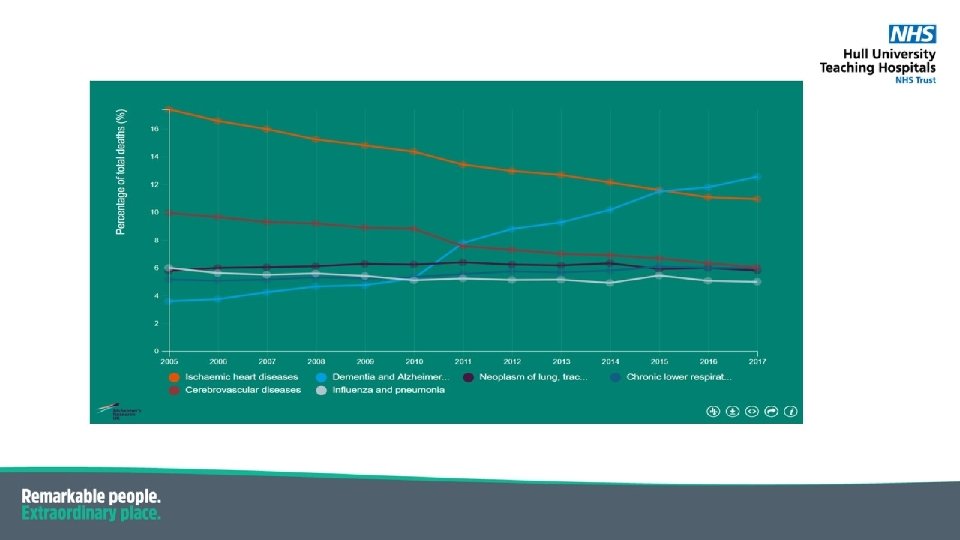
Outline • Dementia and delirium – facts and figures




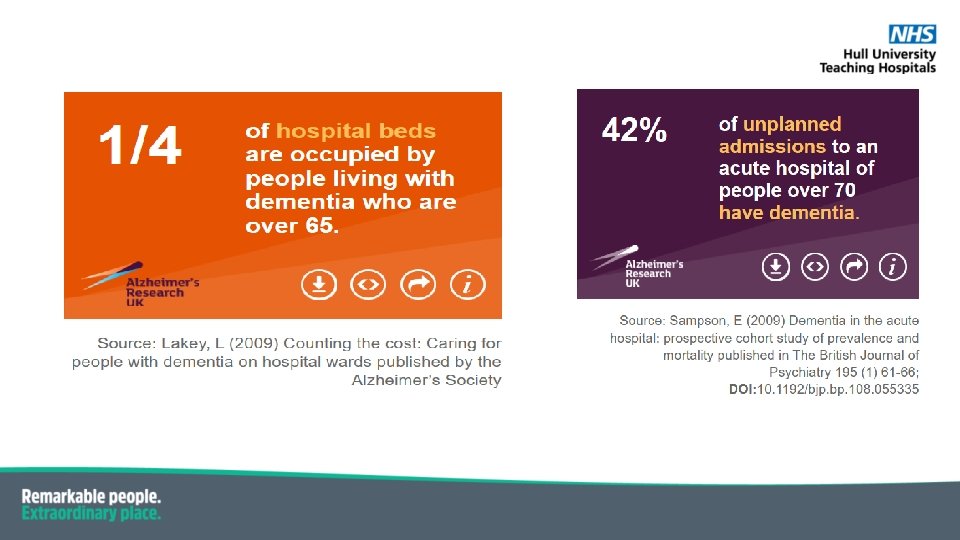

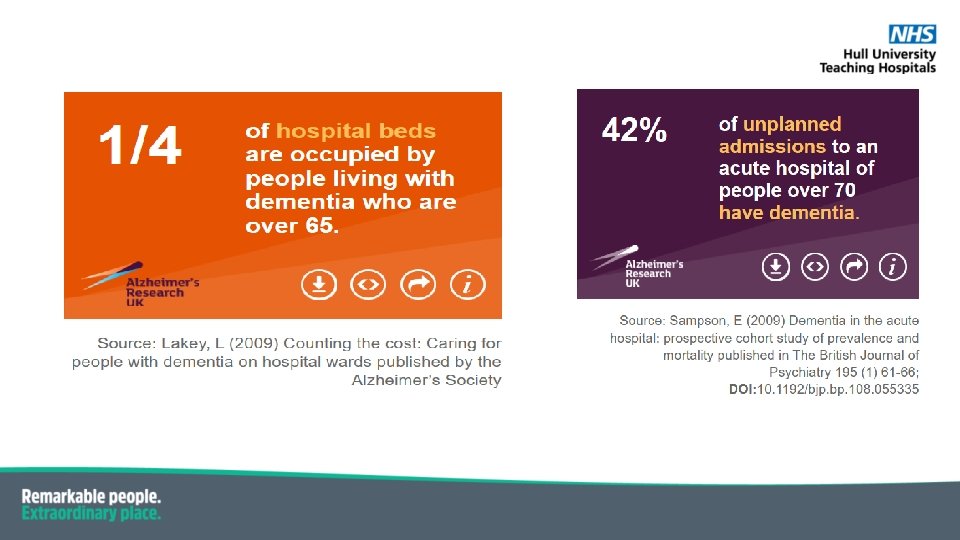
Patients with dementia : • Longer length of stay • Risk of hospital acquired harm higher • Mortality higher • Discharge process more complex • Readmission rates higher

Person centred care
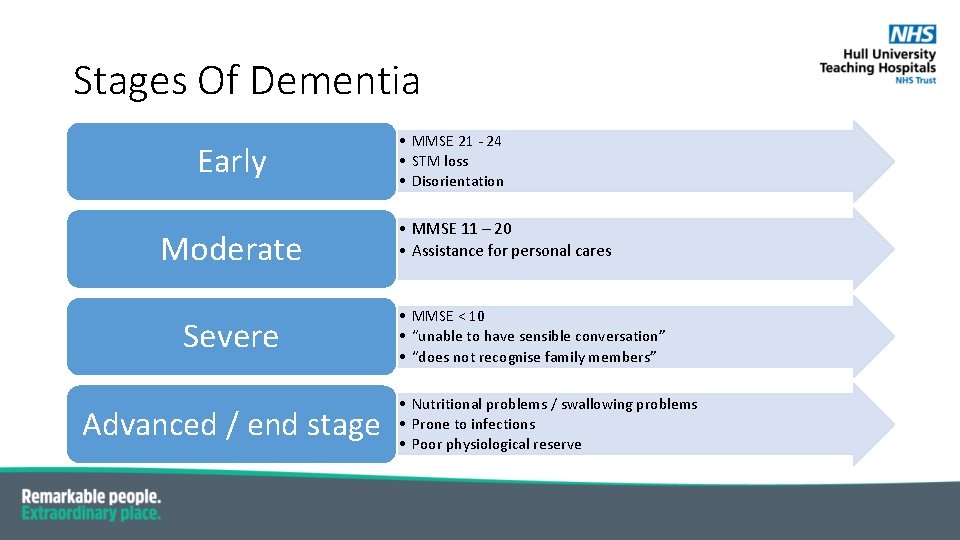
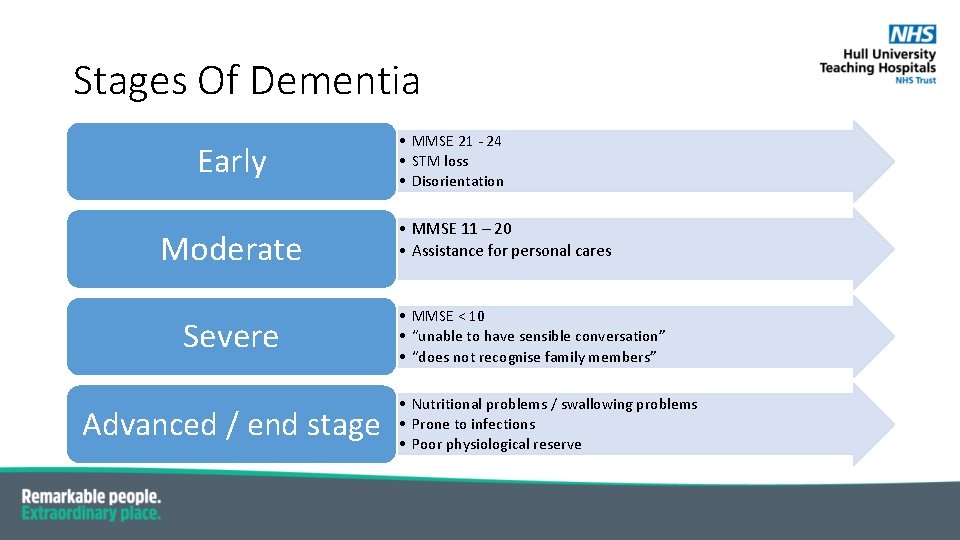
Stages Of Dementia Early Moderate Severe Advanced / end stage • MMSE 21 - 24 • STM loss • Disorientation • MMSE 11 – 20 • Assistance for personal cares • MMSE < 10 • “unable to have sensible conversation” • “does not recognise family members” • Nutritional problems / swallowing problems • Prone to infections • Poor physiological reserve
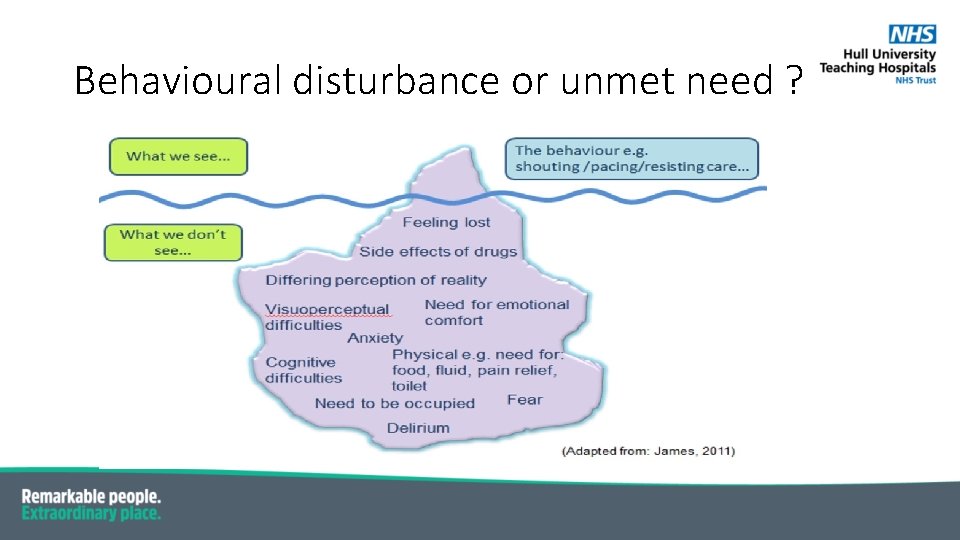
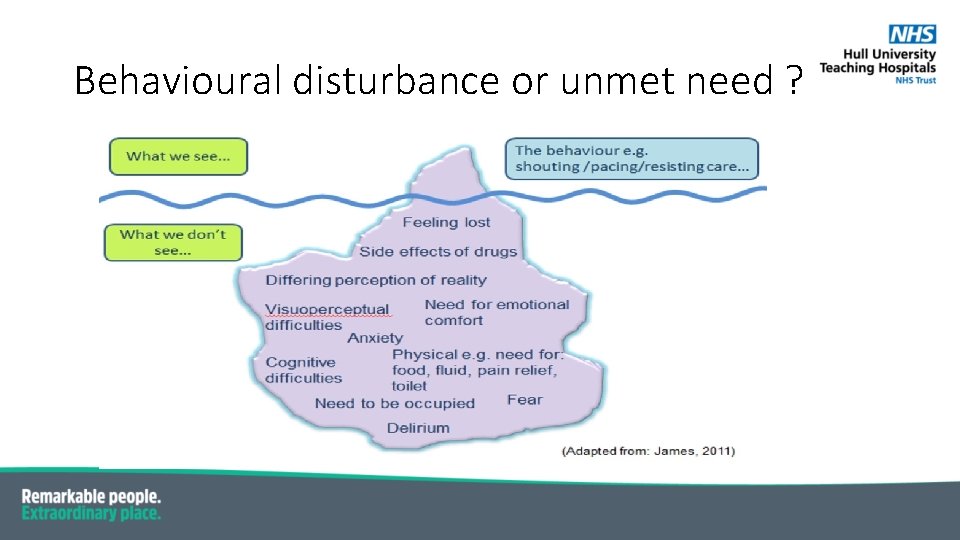
Behavioural disturbance or unmet need ?
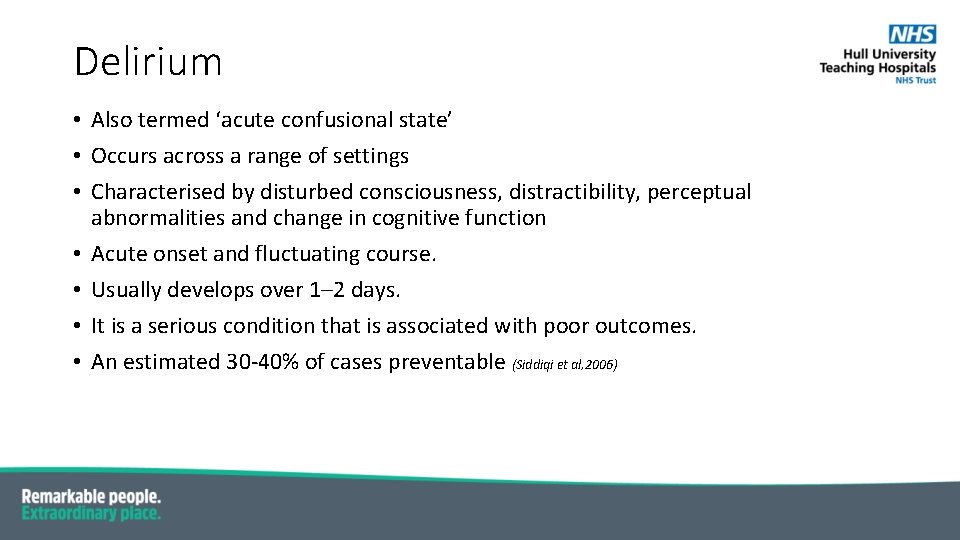
Delirium • Also termed ‘acute confusional state’ • Occurs across a range of settings • Characterised by disturbed consciousness, distractibility, perceptual abnormalities and change in cognitive function • Acute onset and fluctuating course. • Usually develops over 1– 2 days. • It is a serious condition that is associated with poor outcomes. • An estimated 30 -40% of cases preventable (Siddiqi et al, 2006)
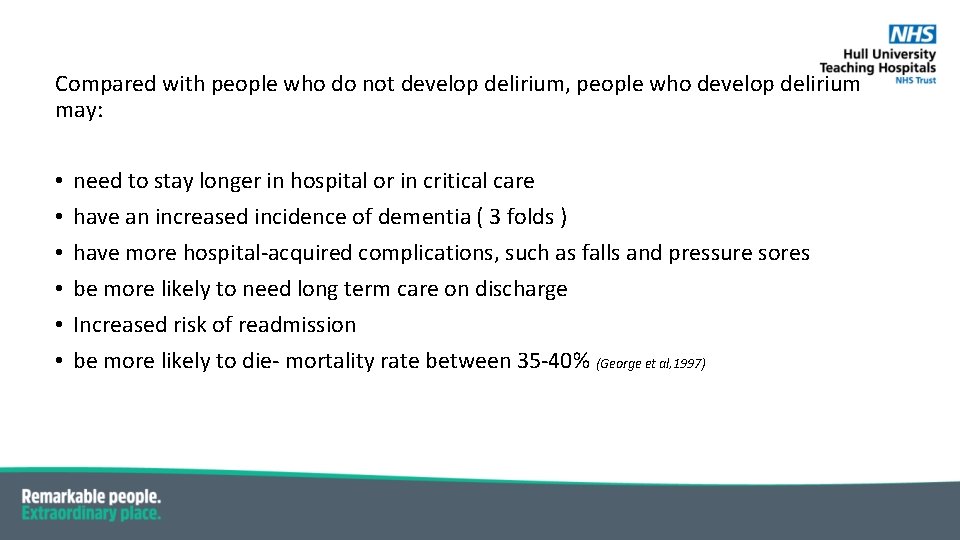
Compared with people who do not develop delirium, people who develop delirium may: • • • need to stay longer in hospital or in critical care have an increased incidence of dementia ( 3 folds ) have more hospital-acquired complications, such as falls and pressure sores be more likely to need long term care on discharge Increased risk of readmission be more likely to die- mortality rate between 35 -40% (George et al, 1997)
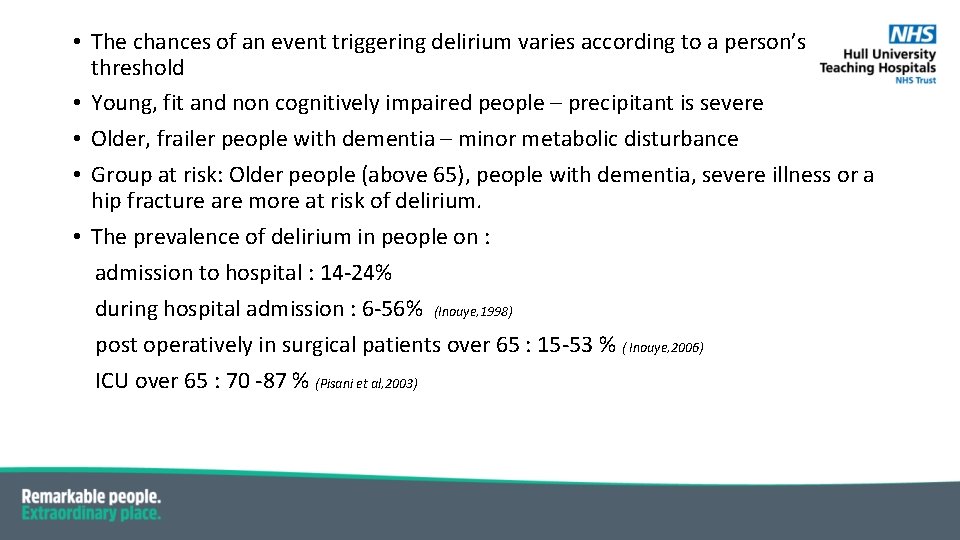
• The chances of an event triggering delirium varies according to a person’s threshold • Young, fit and non cognitively impaired people – precipitant is severe • Older, frailer people with dementia – minor metabolic disturbance • Group at risk: Older people (above 65), people with dementia, severe illness or a hip fracture are more at risk of delirium. • The prevalence of delirium in people on : admission to hospital : 14 -24% during hospital admission : 6 -56% (Inouye, 1998) post operatively in surgical patients over 65 : 15 -53 % ( Inouye, 2006) ICU over 65 : 70 -87 % (Pisani et al, 2003)

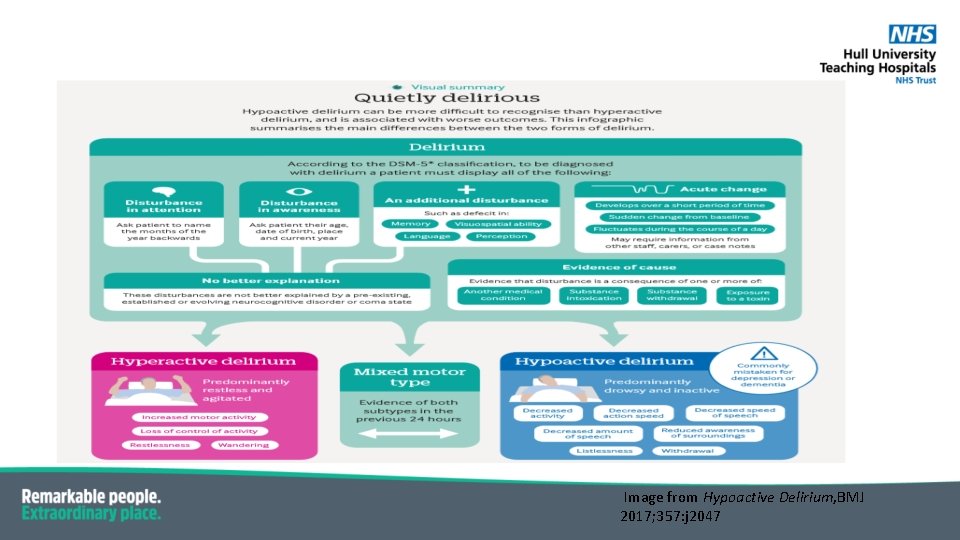
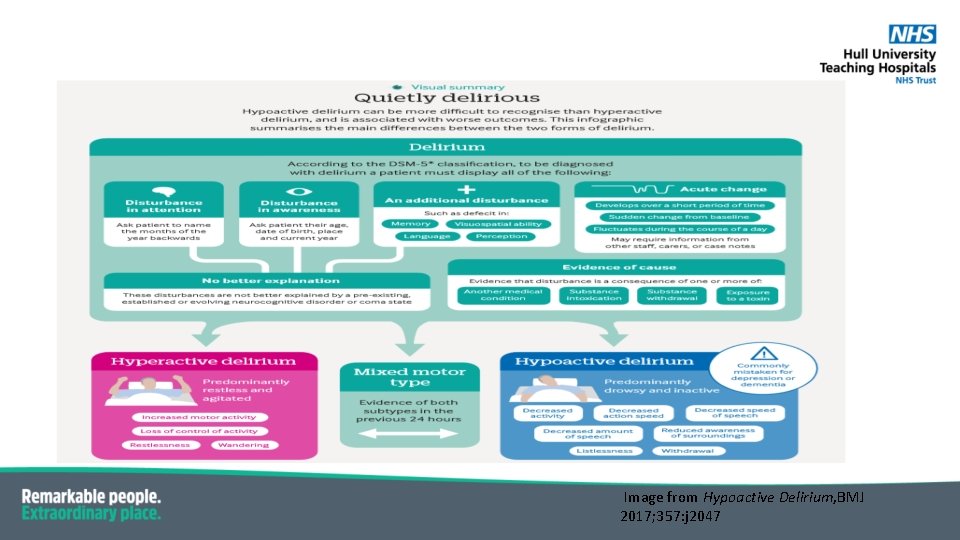
Image from Hypoactive Delirium, BMJ 2017; 357: j 2047
Hypoactive delirium • Associated with poorer outcome compared to hyperactive or mixed delirium • Increased mortality and admission to longer care facility • May not come to the attention of the care provider
Why hypoactive delirium can be missed? • The nature of the condition -patient too withdrawn to alert healthcare provider -condition fluctuates and period of near normality may coincide with clinician’s assessment -establishing the diagnosis requires a degree of longitudinal overview • The nature of healthcare systems -lack of continuity of care, poor access to records, sensory impairment -delayed assessment- patient not triaged as urgent Hypoactive delirium. BMJ 2017
• Misunderstandings within the workforce -it is normal for older patients to be forgetful or disorientated -hyperactive symptoms must be present for a diagnosis to be made -patients are offended by having their cognition tested -hypoactive delirium is irreversible • Factors inherent within the population at risk -elderly patients may be socially isolated - Age UK- more than 2 million live alone -More than 1 million go for a month without speaking to family, friends or neighbours Hypoactive delirium. BMJ 2017
Delirium assessment • SQi. D • 4 AT • CAM
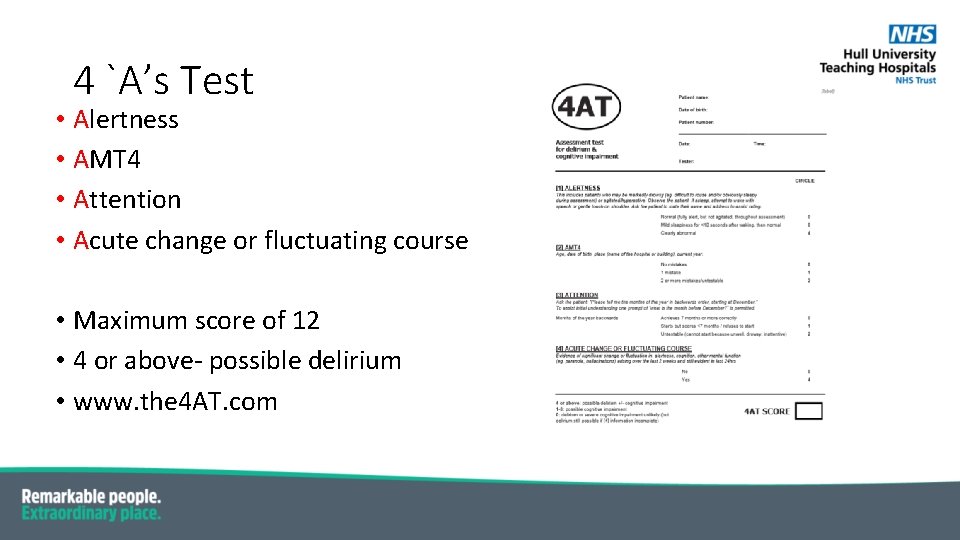
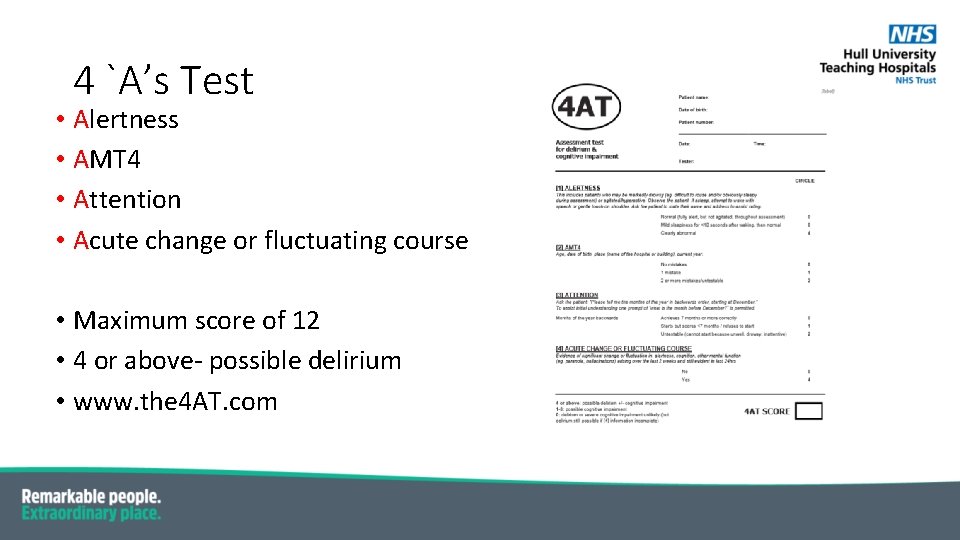
4 `A’s Test • Alertness • AMT 4 • Attention • Acute change or fluctuating course • Maximum score of 12 • 4 or above- possible delirium • www. the 4 AT. com
Confusion Assessment Method (CAM) • The diagnosis of delirium by CAM requires the presence of features A and B and either C or D A acute change and fluctuating course B inattention C disorganised thinking D altered consciousness

Disturbance of perception in delirium • Hallucinations, illusions and delusions up to 40% of cases • Hallucinations usually visual • Ranges from terrifying images to surreal visions
Vision and dementia • Reduced visual acuity and colour vision in patients with Alzheimer’s disease (Colour vision deficiencies in Alzheimer’s disease; Age and Ageing 2003; ) • Posterior cortical atrophy – difficulty recognising faces and objects
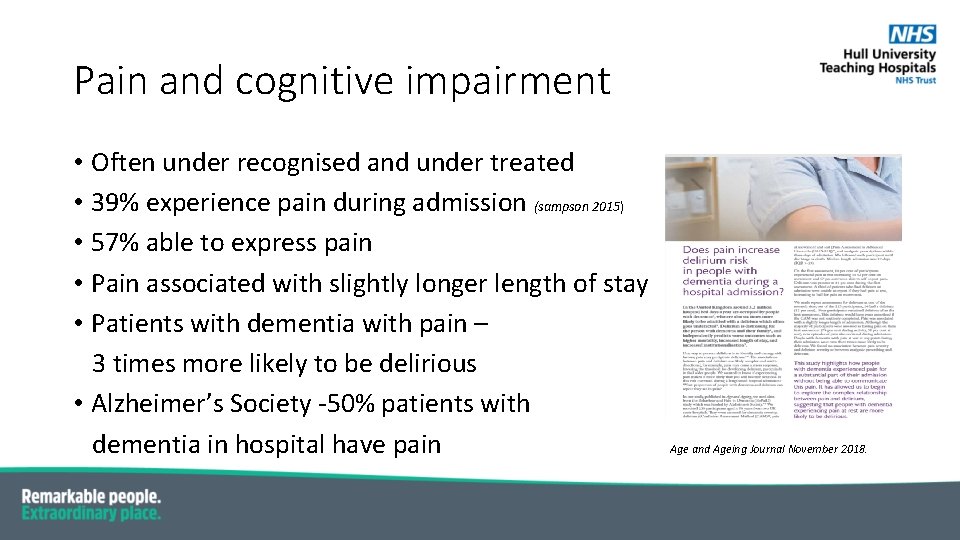
Pain and cognitive impairment • Often under recognised and under treated • 39% experience pain during admission (sampson 2015) • 57% able to express pain • Pain associated with slightly longer length of stay • Patients with dementia with pain – 3 times more likely to be delirious • Alzheimer’s Society -50% patients with dementia in hospital have pain Age and Ageing Journal November 2018.
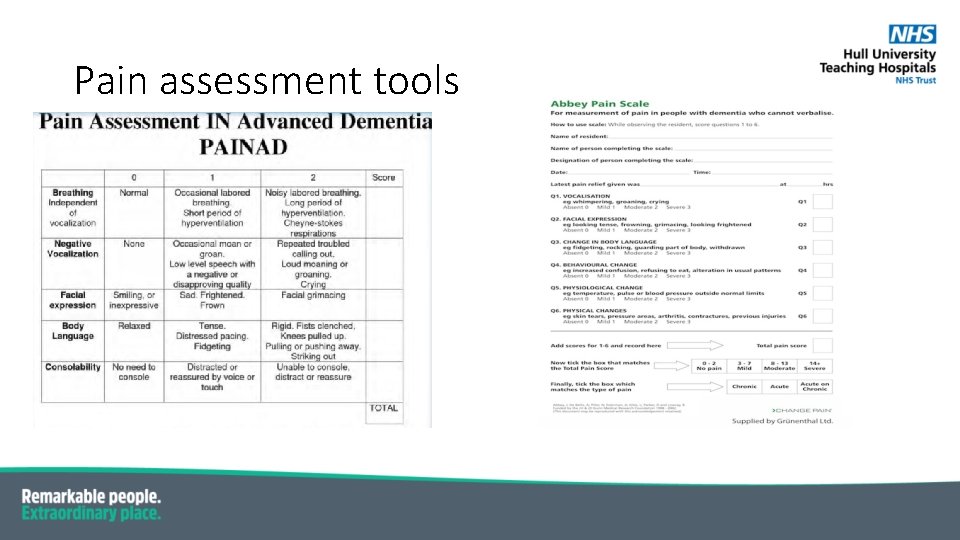
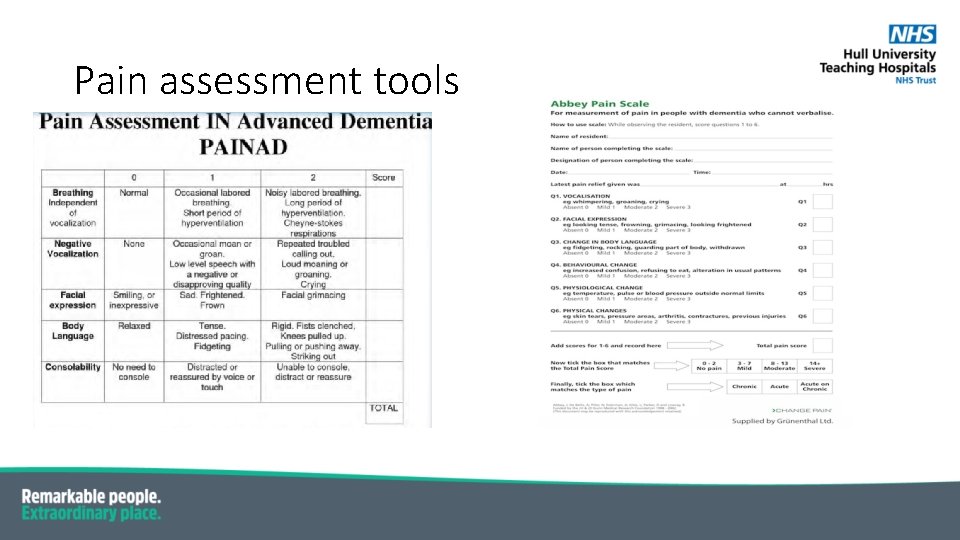
Pain assessment tools
Delirium management • Apart from treating the underlying cause… 1. Patient orientation • Clocks • Calendars • Familiar objects from home • Verbal orientation on every intervention • Avoid room/ward moves • Clear signage • Good lighting
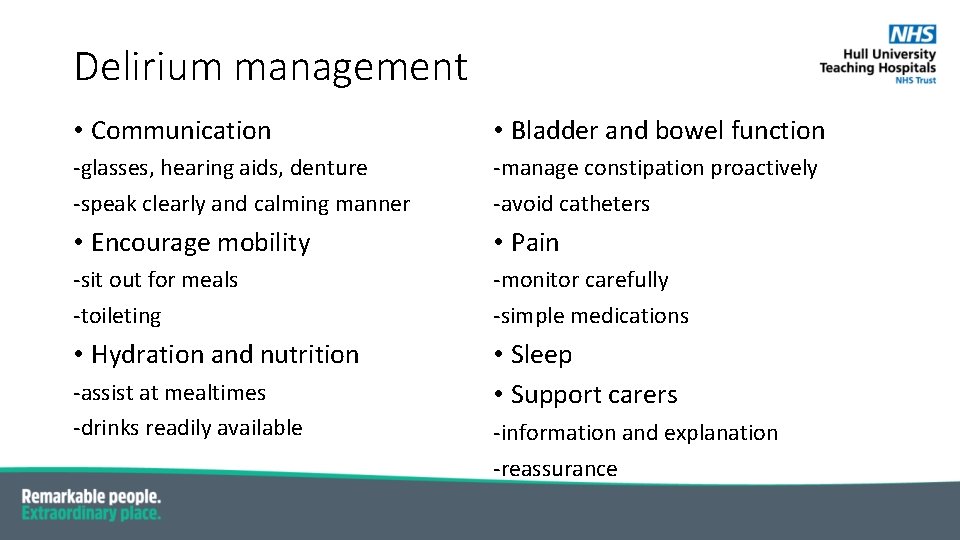
Delirium management • Communication • Bladder and bowel function -glasses, hearing aids, denture -speak clearly and calming manner -manage constipation proactively -avoid catheters • Encourage mobility • Pain -sit out for meals -toileting -monitor carefully -simple medications • Hydration and nutrition • Sleep • Support carers -assist at mealtimes -drinks readily available -information and explanation -reassurance

Pharmacological options • Usually prescribed in response to agitation/ aggression -rapid tranquilisation or treatment of delirium? • Start with lowest dose, shortest period of time • Should ideally discuss with patient/ family about potential side effects • Monitor closely and stop as soon as not needed • Haloperidol drug of choice but can try olanzapine or quetiapine • Benzodiazepines can prolong delirium
Discharge planning. . • Transfer if information from secondary care to primary care • Delirium clinic follow up

 Difference between dementia and delirium
Difference between dementia and delirium Difference between delirium and dementia ppt
Difference between delirium and dementia ppt Amnesia
Amnesia Wendylett sheets 1 carer
Wendylett sheets 1 carer Rocking chair therapy for dementia patients
Rocking chair therapy for dementia patients Pinch me delirium
Pinch me delirium Sindrom delirium akut
Sindrom delirium akut Nash delirium
Nash delirium Terminalt delirium
Terminalt delirium Escala de cam icu
Escala de cam icu Delirium care pathways
Delirium care pathways Acute confusion related to
Acute confusion related to Delirium definition
Delirium definition Excited delirium перевод
Excited delirium перевод R
R Delirium case presentation
Delirium case presentation Flocculation delirium
Flocculation delirium Gcs 456
Gcs 456 Driver diagram palliative care
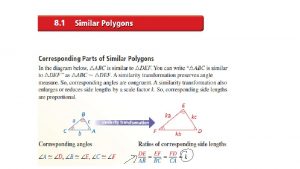
Driver diagram palliative care Are all congruent figures similar
Are all congruent figures similar Plane figures
Plane figures Solid and plane figures
Solid and plane figures Data raw facts and figures
Data raw facts and figures Facts and figures linda lee
Facts and figures linda lee Facts and figures linda lee
Facts and figures linda lee Fair trade coffee facts and figures
Fair trade coffee facts and figures Facts and figures
Facts and figures Facts and figures slide
Facts and figures slide Paragraph sandwich example
Paragraph sandwich example Similar figures worksheet
Similar figures worksheet 3 zones of space and awareness dementia
3 zones of space and awareness dementia Chapter 19 confusion dementia and alzheimer's disease
Chapter 19 confusion dementia and alzheimer's disease Chapter 49 confusion and dementia
Chapter 49 confusion and dementia Chapter 19 confusion dementia and alzheimer's disease
Chapter 19 confusion dementia and alzheimer's disease Confusion dementia and alzheimer's disease
Confusion dementia and alzheimer's disease If a resident with ad shows violent behavior the na should
If a resident with ad shows violent behavior the na should Dementia treatments and interventions near patterson
Dementia treatments and interventions near patterson