OUTCOMES OF ACUTE INFLAMMATION Dr Ramadas Nayak Professor


- Slides: 27
OUTCOMES OF ACUTE INFLAMMATION Dr Ramadas Nayak Professor & HOD Pathology Yenepoya Medical College Mangaluru
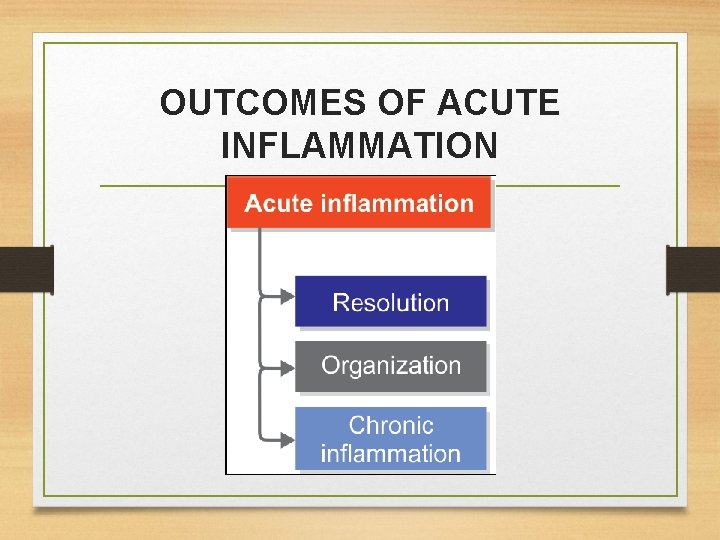
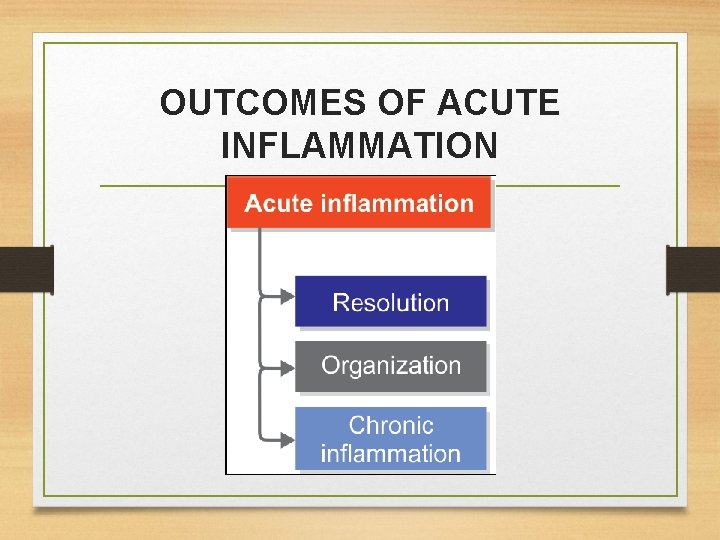
OUTCOMES OF ACUTE INFLAMMATION
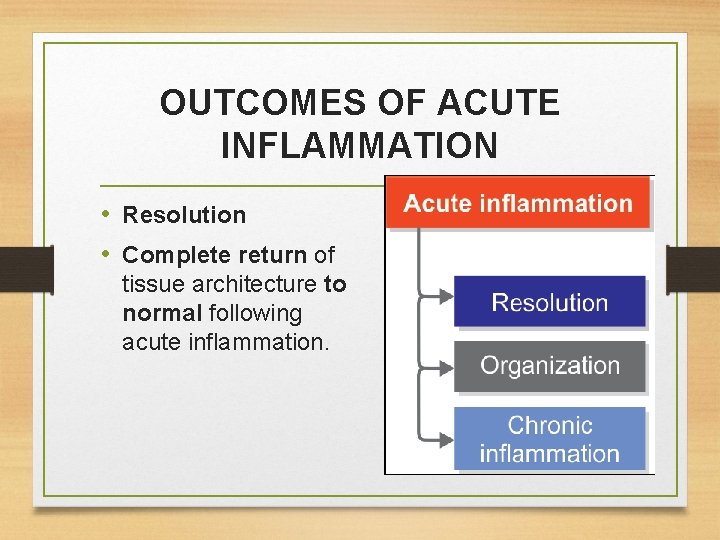
OUTCOMES OF ACUTE INFLAMMATION • Resolution • Complete return of tissue architecture to normal following acute inflammation.
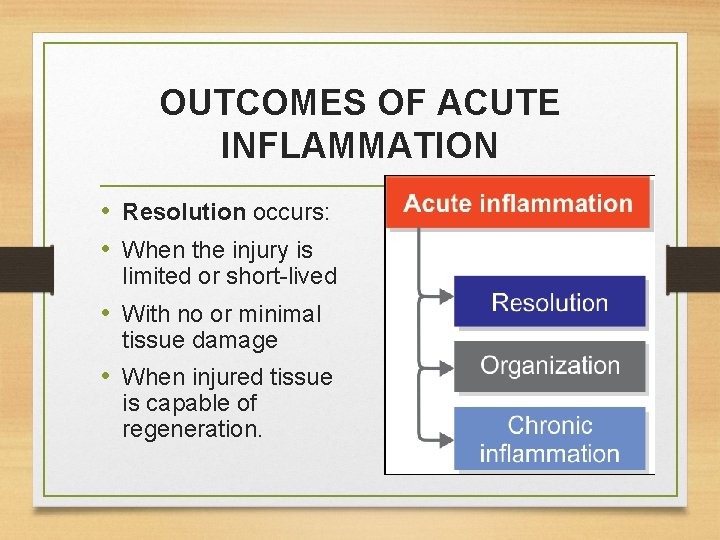
OUTCOMES OF ACUTE INFLAMMATION • Resolution occurs: • When the injury is limited or short-lived • With no or minimal tissue damage • When injured tissue is capable of regeneration.
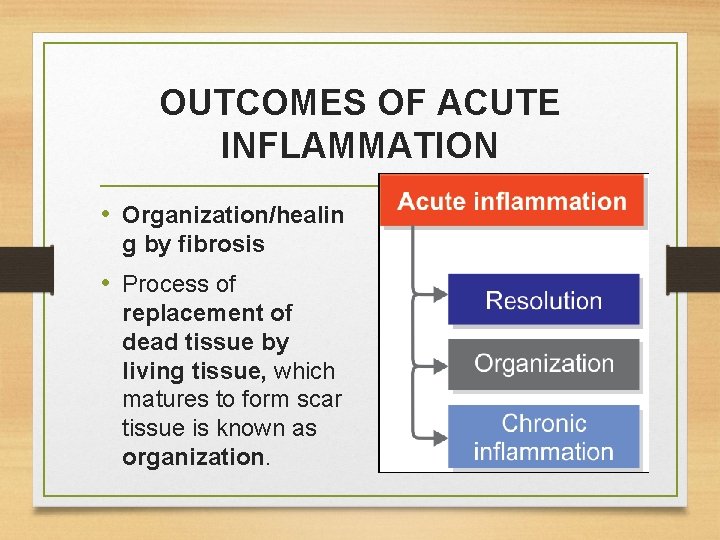
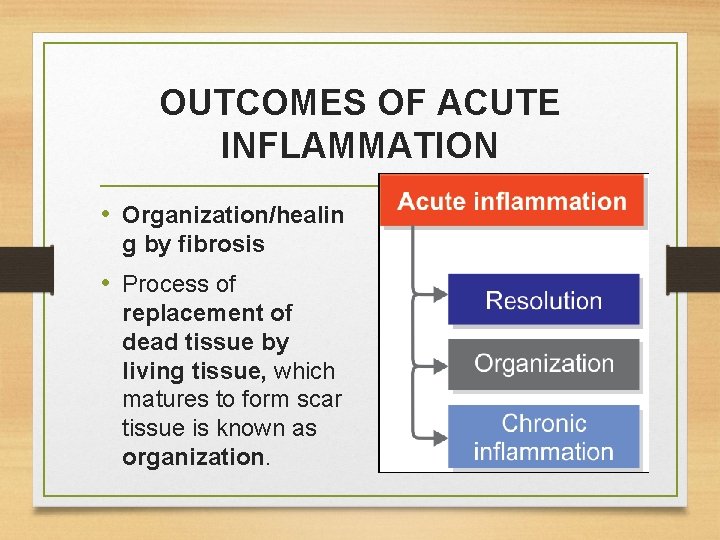
OUTCOMES OF ACUTE INFLAMMATION • Organization/healin g by fibrosis • Process of replacement of dead tissue by living tissue, which matures to form scar tissue is known as organization.
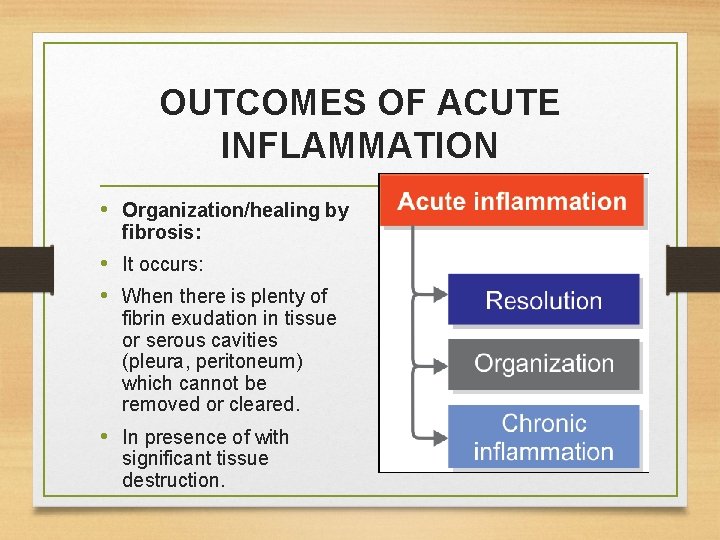
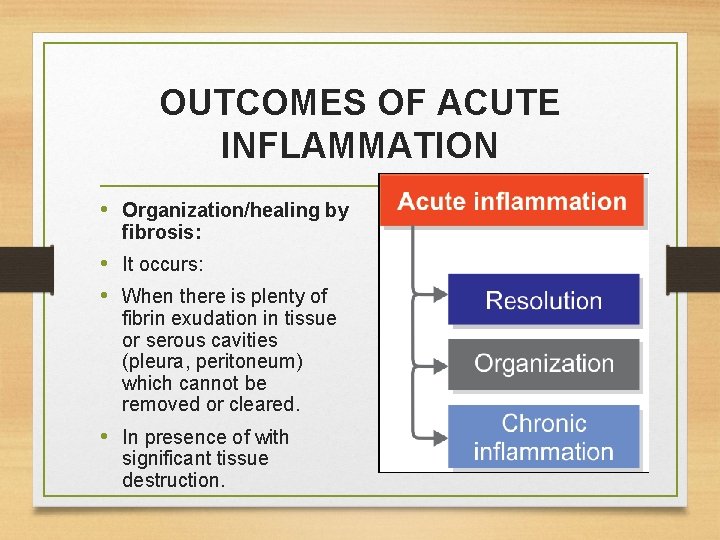
OUTCOMES OF ACUTE INFLAMMATION • Organization/healing by fibrosis: • It occurs: • When there is plenty of fibrin exudation in tissue or serous cavities (pleura, peritoneum) which cannot be removed or cleared. • In presence of with significant tissue destruction.
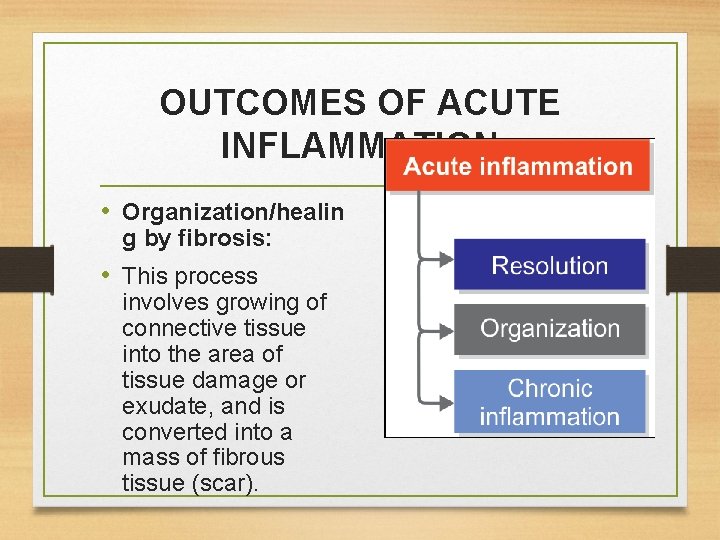
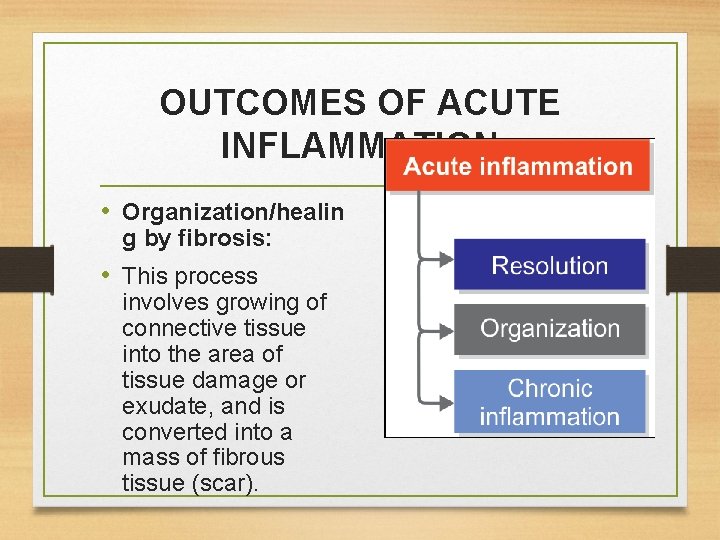
OUTCOMES OF ACUTE INFLAMMATION • Organization/healin g by fibrosis: • This process involves growing of connective tissue into the area of tissue damage or exudate, and is converted into a mass of fibrous tissue (scar).
OUTCOMES OF ACUTE INFLAMMATION • Abscess • Localized collection of pus is called abscess.
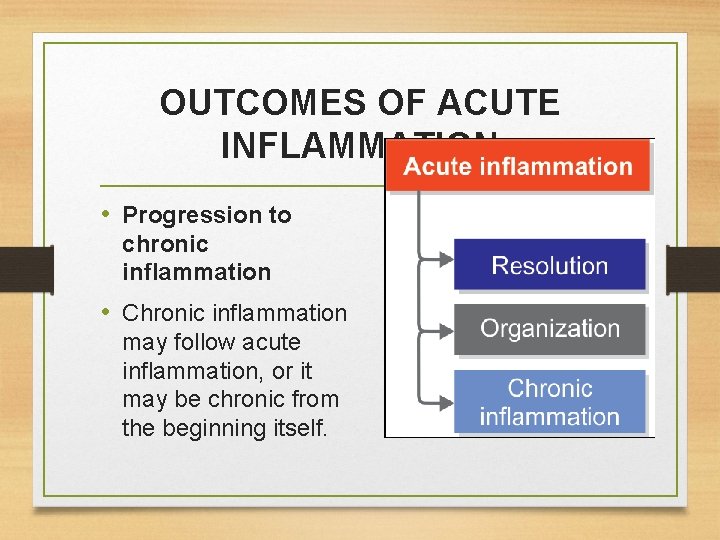
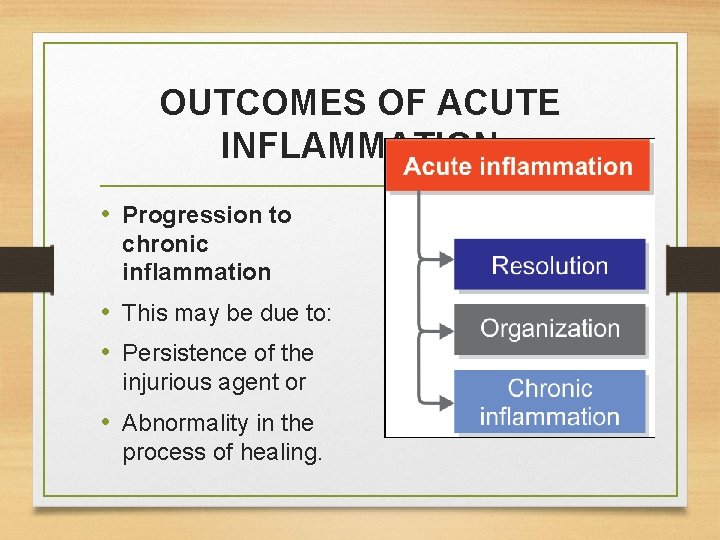
OUTCOMES OF ACUTE INFLAMMATION • Progression to chronic inflammation • Chronic inflammation may follow acute inflammation, or it may be chronic from the beginning itself.
OUTCOMES OF ACUTE INFLAMMATION • Progression to chronic inflammation • This may be due to: • Persistence of the injurious agent or • Abnormality in the process of healing.
MORPHOLOGICAL TYPES/PATTERNS OF ACUTE INFLAMMATION • Gross and microscopic appearances can often • • provide clues about the cause. Serous Inflammation Characterized by marked outpouring of a thin serous fluid. Serous exudate or effusion is yellow, straw-like in color and microscopically shows either few or no cells. Example: Pleural effusion as a complication of lobar pneumonia.
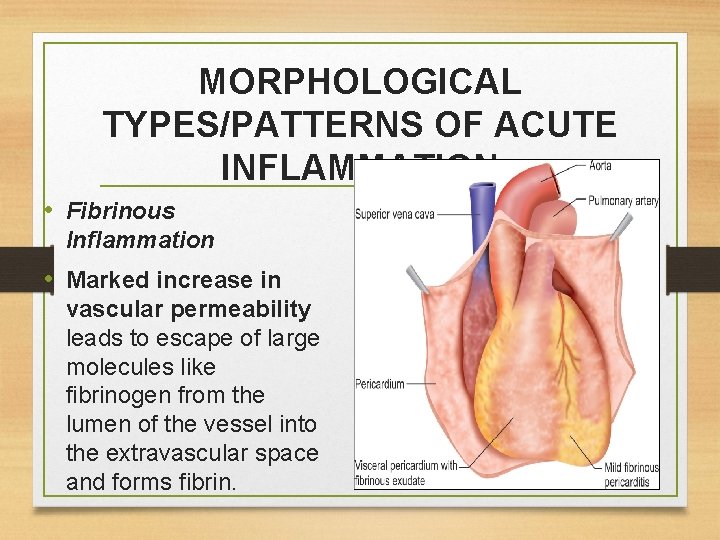
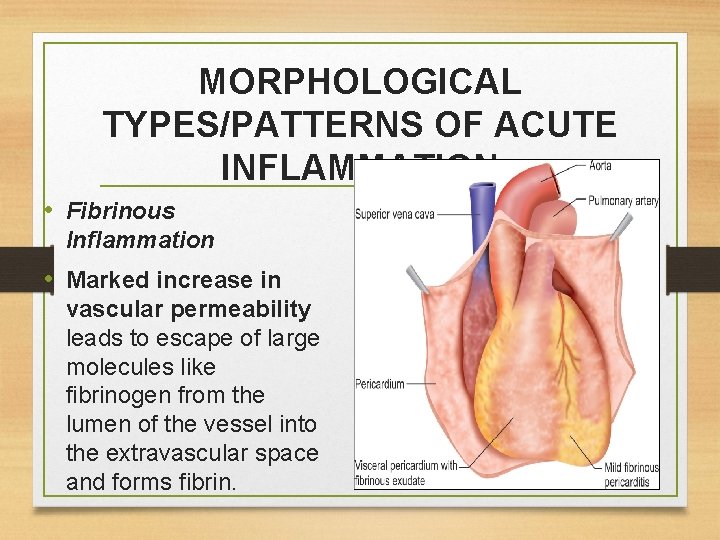
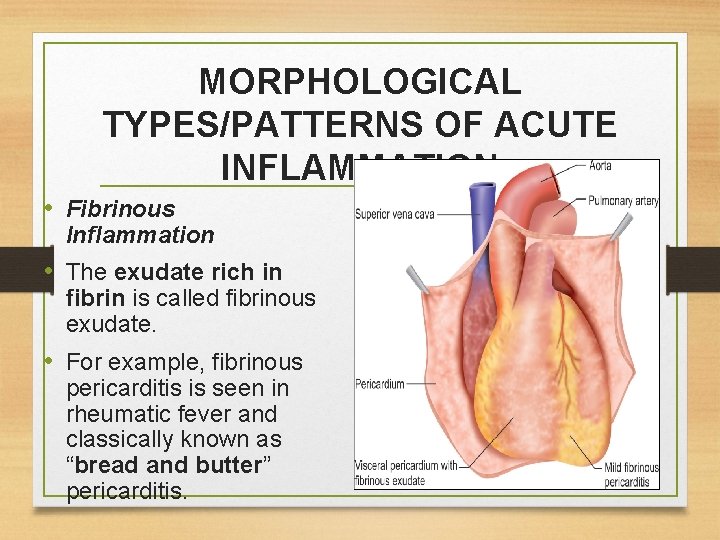
MORPHOLOGICAL TYPES/PATTERNS OF ACUTE INFLAMMATION • Fibrinous Inflammation • Marked increase in vascular permeability leads to escape of large molecules like fibrinogen from the lumen of the vessel into the extravascular space and forms fibrin.
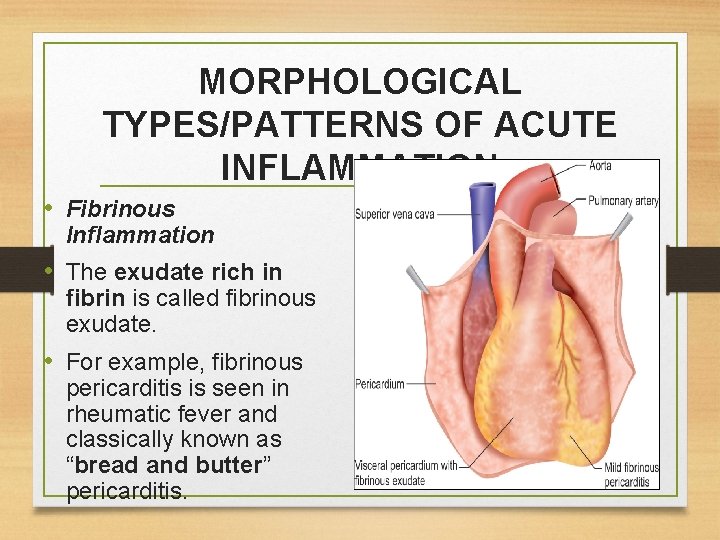
MORPHOLOGICAL TYPES/PATTERNS OF ACUTE INFLAMMATION • Fibrinous Inflammation • The exudate rich in fibrin is called fibrinous exudate. • For example, fibrinous pericarditis is seen in rheumatic fever and classically known as “bread and butter” pericarditis.
MORPHOLOGICAL TYPES/PATTERNS OF ACUTE INFLAMMATION • Suppurative or Purulent Inflammation: Abscess • It is characterized by the production of large amounts of pus or purulent exudate. • Microscopically, shows neutrophils, liquefactive necrosis, and edema fluid.
MORPHOLOGICAL TYPES/PATTERNS OF ACUTE INFLAMMATION • Suppurative or Purulent Inflammation: Abscess • Bacteria (e. g. staphylococci) which produce localized suppuration and are called as pyogenic (pus-producing) bacteria. • For example, acute appendicitis. • Abscesses: It is the localized collections of purulent inflammatory exudates in a tissue, an organ, or a confined space.
MORPHOLOGICAL TYPES/PATTERNS OF ACUTE INFLAMMATION • Hemorrhagic Inflammation • When inflammation is associated with severe vascular injury or deficiency of coagulation factors, it causes hemorrhagic inflammation, • e. g. acute pancreatitis due to proteolytic destruction of vascular walls.
MORPHOLOGICAL TYPES/PATTERNS OF ACUTE INFLAMMATION • Catarrhal Inflammation • Acute inflammation of a mucous membrane is accompanied by excessive secretion of mucus and the appearance is described as catarrhal • e. g. common cold.
MORPHOLOGICAL TYPES/PATTERNS OF ACUTE INFLAMMATION • Membranous Inflammation • In this type, epithelium is covered by membrane consisting of fibrin, desquamated epithelial cells and inflammatory cells • e. g. pharyngitis or laryngitis due to Corynebacterium diphtheria.
MORPHOLOGICAL TYPES/PATTERNS OF ACUTE INFLAMMATION • Necrotizing (Gangrenous) Inflammation • The combination of necrosis and bacterial putrefaction is gangrene • e. g. gangrenous appendicitis.
SYSTEMIC EFFECTS OF INFLAMMATION • Systemic changes in acute inflammation are collectively known as acute-phase response, or the systemic inflammatory response syndrome (SIRS). • Causes: Due to cytokines produced by leukocytes, in response to infections or immune reactions. Most important cytokines are TNF, IL-1, and IL-6.

SYSTEMIC EFFECTS OF INFLAMMATION • The clinical and pathologic changes of acute-phase response are: • 1. Fever: • Pyrogens: These are molecules that cause fever. It may be exogenous (bacterial products, like LPS), which stimulate leukocytes to release endogenous pyrogens (cytokines such as IL-1 and TNF). • The cytokines increase the enzymes cyclooxygenases resulting in conversion of AA into prostaglandins.
SYSTEMIC EFFECTS OF INFLAMMATION • 2. Raised plasma levels of acute-phase proteins: • These are plasma proteins synthesized in the liver and may be markedly raised in response to inflammatory stimuli. • • Types of acute-phase proteins: (1) C-reactive protein (CRP) (2) fibrinogen (3) serum amyloid A (SAA) protein.
SYSTEMIC EFFECTS OF INFLAMMATION • 3. Changes in the leukocytes: • A. Leukocytosis • Total leukocyte count more than 11, 000/μL are termed as leukocytosis. • Common in inflammatory reactions, especially those caused by bacterial infections.
SYSTEMIC EFFECTS OF INFLAMMATION • 3. Changes in the leukocytes: • B. Lymphocytosis: It is seen in viral infections (e. g. Infectious mononucleosis, mumps, and German measles).
SYSTEMIC EFFECTS OF INFLAMMATION • 3. Changes in the leukocytes: • C. Eosinophilia: It is seen in bronchial asthma, allergy, and parasitic infestations. • D. Leukopenia: Decreased number of circulating white cells is associated with few infections like typhoid fever and some viruses, rickettsia, and certain protozoa.
SYSTEMIC EFFECTS OF INFLAMMATION • 4. Other features of the acute-phase response: It includes: • Increased pulse and blood pressure. • Anorexia and malaise, probably due to cytokines acting on brain cells. • In severe bacterial infections (sepsis) cytokines (mainly TNF and IL-1) may be produced in large quantities and can result in disseminated intravascular coagulation and cardiovascular failure.

Thank you