OUTCOMES AMONG NSTEMI PATIENTS PRESENTING TO HOSPITALS WITH
- Slides: 17
OUTCOMES AMONG NSTEMI PATIENTS PRESENTING TO HOSPITALS WITH AND WITHOUT BACKUP CARDIAC SURGERY From the National Registry of Myocardial Infarction Presented by Yuri B. Pride, MD
Background � Among patients with NSTEMI, early angiography and, if warranted, PCI have been associated with improved outcomes � Because of this, there has been a proliferation of cardiac catheterization laboratories with PCI capability � Many such laboratories have been established at hospitals without backup cardiac surgery (No-OHS hospitals)
Background � Elective PCI at No-OHS hospitals is currently not recommended in the most recent ACC/AHA guidelines � This is based largely on a Medicare study reporting higher mortality among patients undergoing non-primary/rescue PCI at No-OHS hospitals Anderson et al. , Circulation 116 e 148 Wennberg et al. , JAMA 292 1961
Hypothesis � Improved outcomes at hospitals with backup cardiac surgery (OHS hospitals) may be the result of its use after PCI complications or may simply be a marker of improved quality of care
Objective � The goals of the current analyses were two-fold 1) To determine the outcomes NSTEMI patients presenting to hospitals with and without backup cardiac surgery 2) To specifically evaluate the outcomes among such patients who underwent PCI � In order to evaluate these objectives, we used Phase 5 of the National Registry of Myocardial Infarction, which enrolled patients from 2004 -2006
Methods � Three analyses were performed 1) Unadjusted 2) Propensity-matched for baseline characteristics, including transfer-in status, in the entire cohort, and then further adjusted for differences in treatment within 24 hours 3) Propensity-matched in the groups undergoing primary and elective PCI
Results � There were 100, 071 NSTEMI patients, of whom 9, 189 presented to 52 No-OHS hospitals and 90, 872 presented to 214 OHS hospitals � Owing to the large number of patients, there were many differences in baseline characteristics in the unadjusted populations � In the propensity-matched analysis, baseline characteristics were well-matched Pride et al. JACC Cardiovasc Interv 2: 944
Results � Patients presenting to No-OHS hospitals were significantly less likely to receive aspirin, beta-blockers or statins within 24 hours of arrival, both in the unadjusted and propensity-matched analyses � Patients presenting to No-OHS hospitals were also less likely to undergo angiography and PCI both in unadjusted and propensity-matched analyses Pride et al. JACC Cardiovasc Interv 2: 944
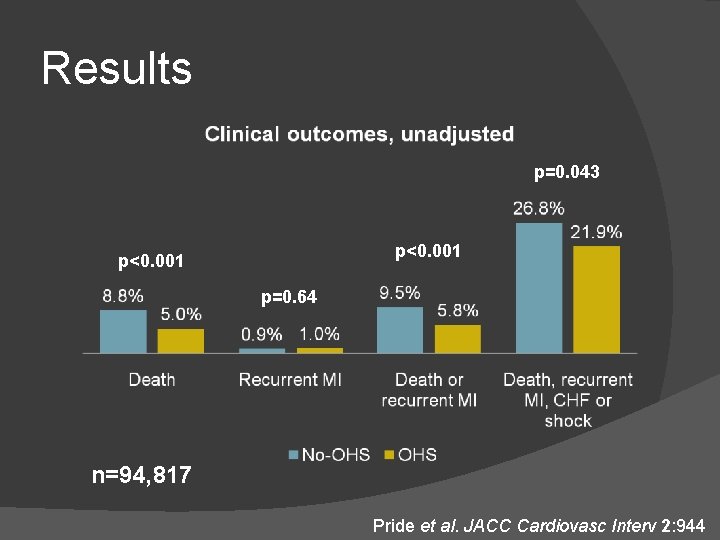
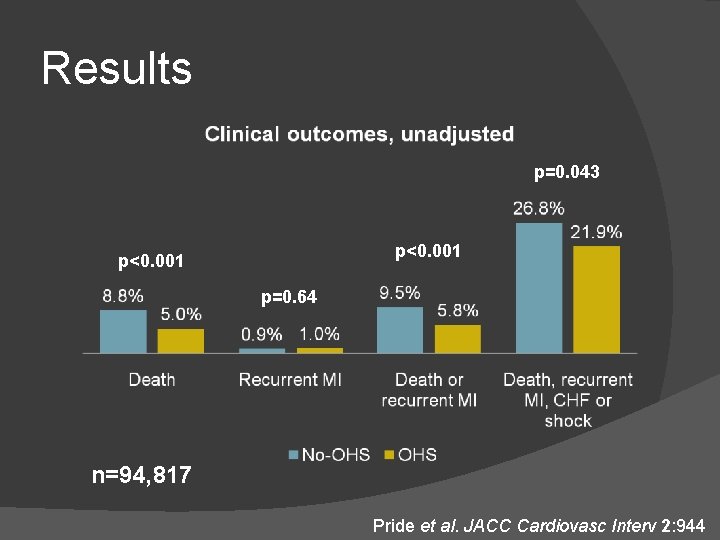
Results p=0. 043 p<0. 001 p=0. 64 n=94, 817 Pride et al. JACC Cardiovasc Interv 2: 944
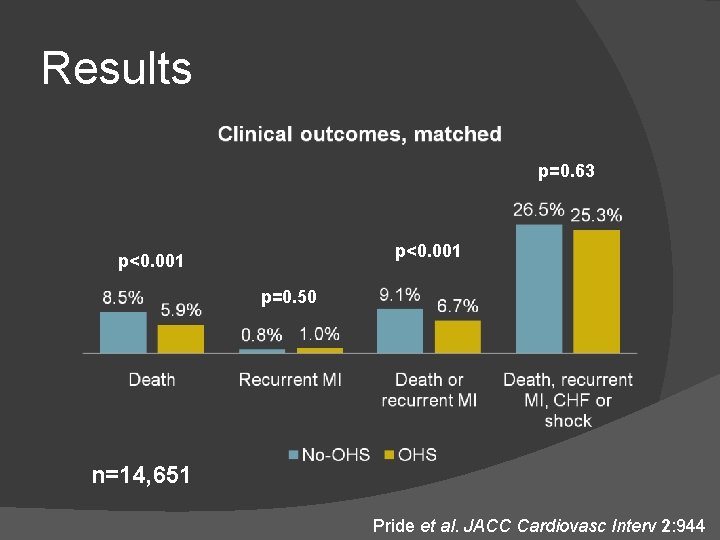
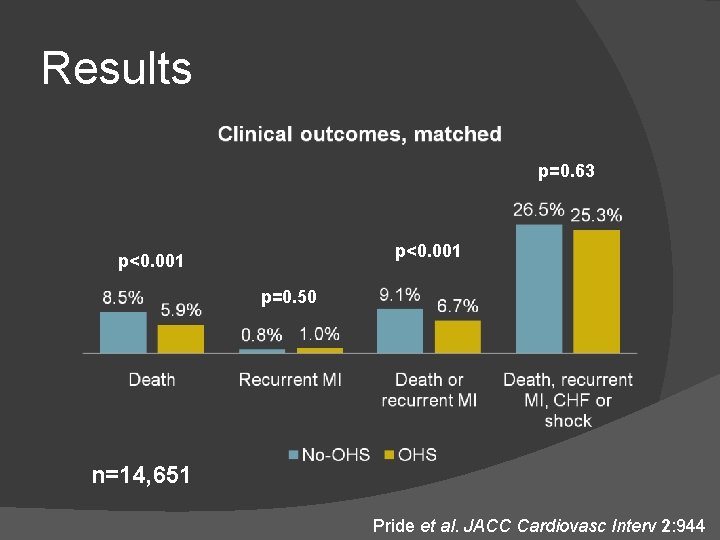
Results p=0. 63 p<0. 001 p=0. 50 n=14, 651 Pride et al. JACC Cardiovasc Interv 2: 944
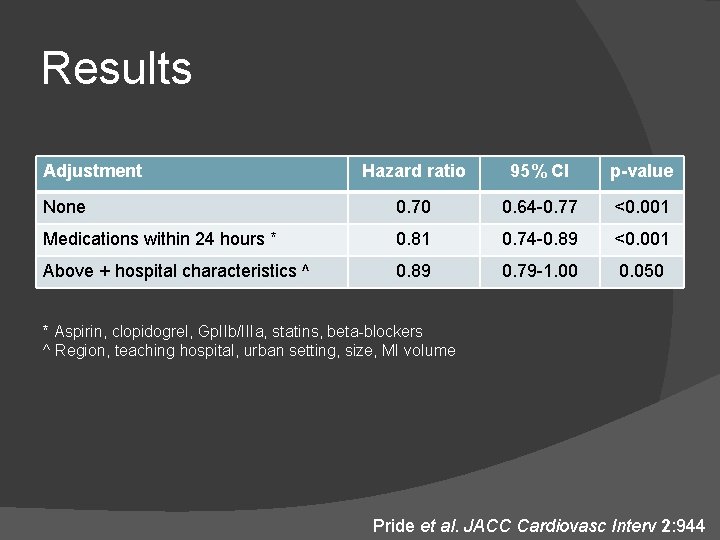
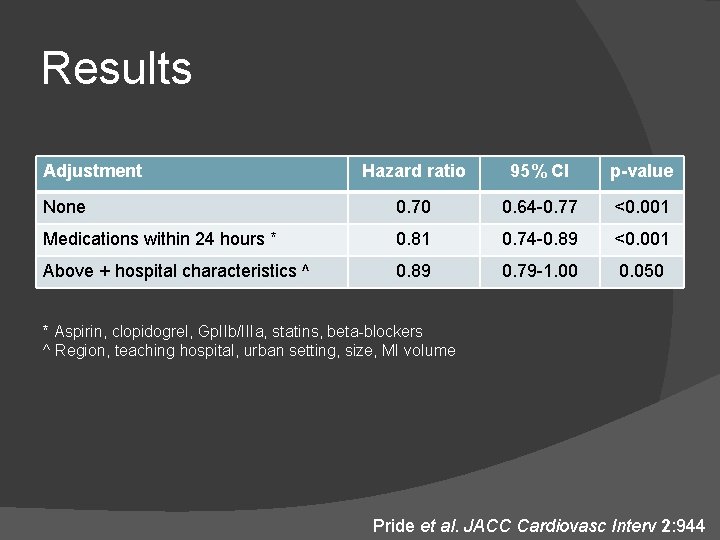
Results Adjustment Hazard ratio 95% CI p-value None 0. 70 0. 64 -0. 77 <0. 001 Medications within 24 hours * 0. 81 0. 74 -0. 89 <0. 001 Above + hospital characteristics ^ 0. 89 0. 79 -1. 00 0. 050 * Aspirin, clopidogrel, Gp. IIb/IIIa, statins, beta-blockers ^ Region, teaching hospital, urban setting, size, MI volume Pride et al. JACC Cardiovasc Interv 2: 944
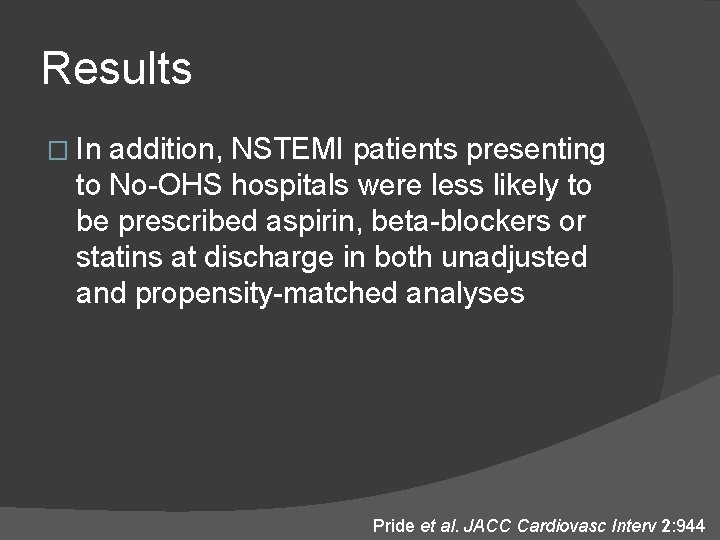
Results � In addition, NSTEMI patients presenting to No-OHS hospitals were less likely to be prescribed aspirin, beta-blockers or statins at discharge in both unadjusted and propensity-matched analyses Pride et al. JACC Cardiovasc Interv 2: 944
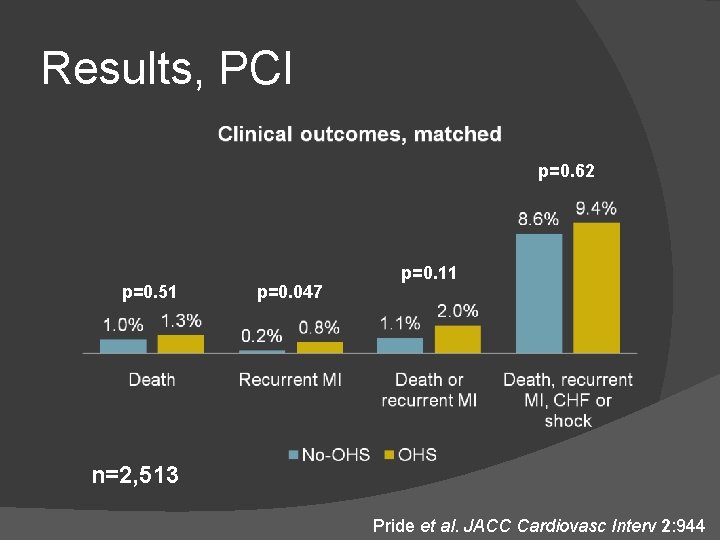
Results, PCI � The propensity-matched analysis was then restricted to patients who underwent PCI, who were generally of lower risk than the overall population � There was no significant difference in the administration of aspirin, betablockers or statins, but patients presenting to No-OHS hospitals were more likely to receive clopidogrel in the first 24 hours. Pride et al. JACC Cardiovasc Interv 2: 944
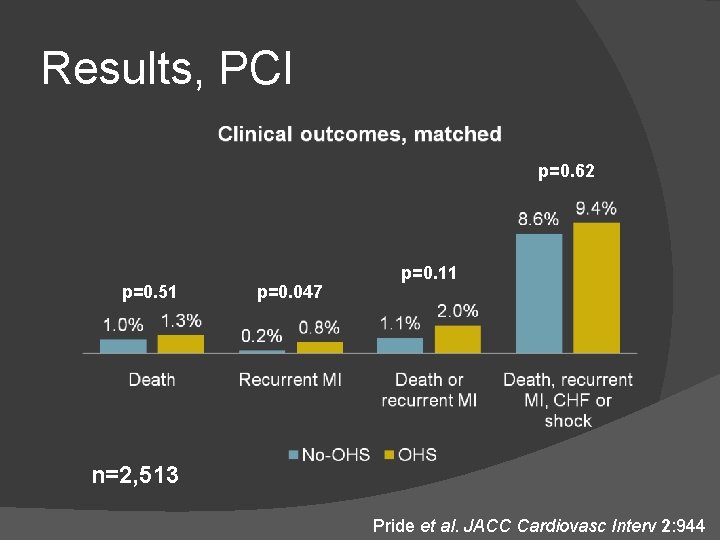
Results, PCI p=0. 62 p=0. 51 p=0. 047 p=0. 11 n=2, 513 Pride et al. JACC Cardiovasc Interv 2: 944
Limitations � NRMI enrolled far more patients at OHS hospitals � The outcomes of patients who were transferred are unknown � Long-term outcomes are unknown
Conclusions � STEMI and NSTEMI patients presenting to No-OHS hospitals have significantly worse in-hospital outcomes, even after adjusting for differences in baseline characteristics � After further adjusting for differences in hospital characteristics and adherence to guideline recommendations, the difference in outcomes was attenuated
Conclusions � Furthermore, among patients undergoing PCI, there were actually differences favoring No-OHS hospitals in the administration of some medications as well as some clinical outcomes � These results suggest that efforts to increase adherence to guideline recommendations are warranted