Outcome evaluation of immunization WeiChu Chie outcome research
- Slides: 53
Outcome evaluation of immunization Wei-Chu Chie outcome research 1
Immunization • Primary prevention – specific protection • baseline (basic) immunization • booster immunization – active vs. passive – special groups • infants and children, elderly • adults, high risk groups outcome research 2
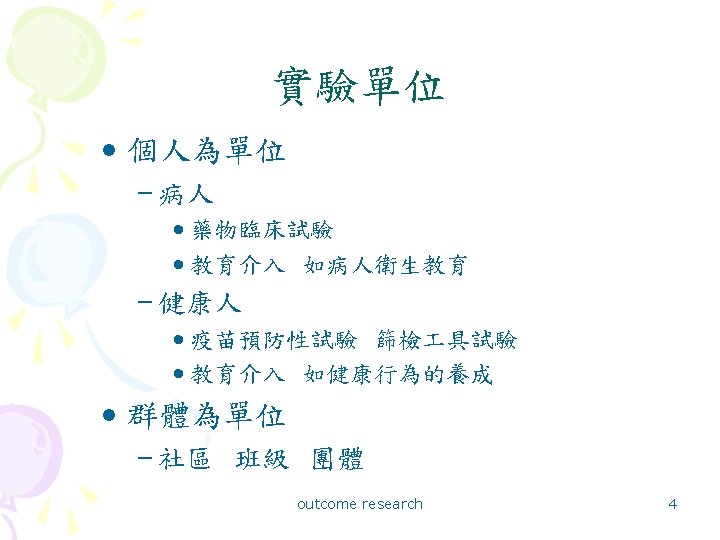
實驗性方法的三要素 • 實驗單位 (experimental unit) • 處置 (treatment) • 評估 (evaluation) outcome research 3
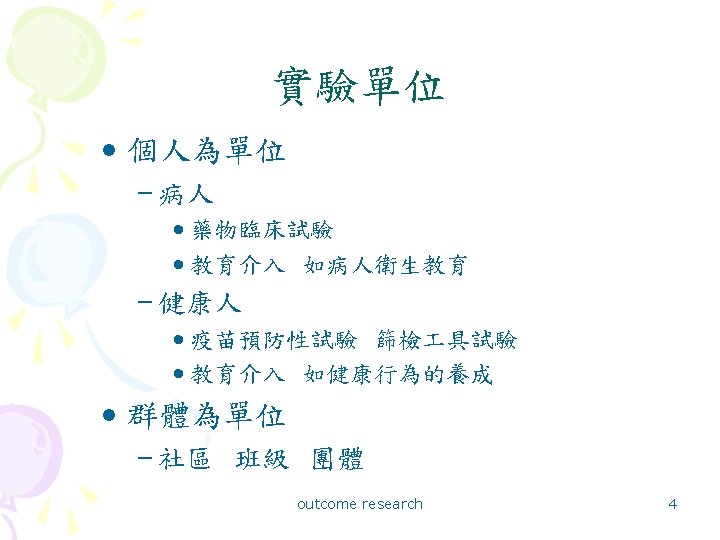
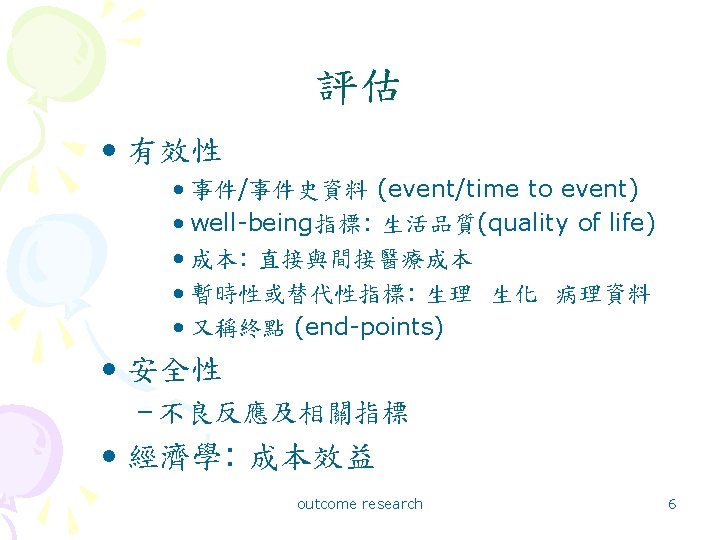
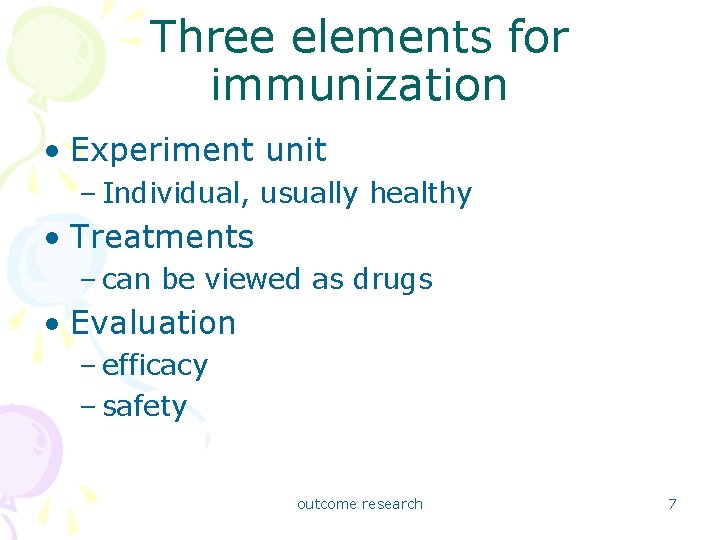
Three elements for immunization • Experiment unit – Individual, usually healthy • Treatments – can be viewed as drugs • Evaluation – efficacy – safety outcome research 7
Basic characteristics • Easy to follow the rule of randomized controlled double-blinded trials – placebo control with blindness: easy to make, usually difficult to guess – individual randomization possible • requires a large sample size – low incidence of the disease to prevent – low incidence of adverse effects outcome research 8
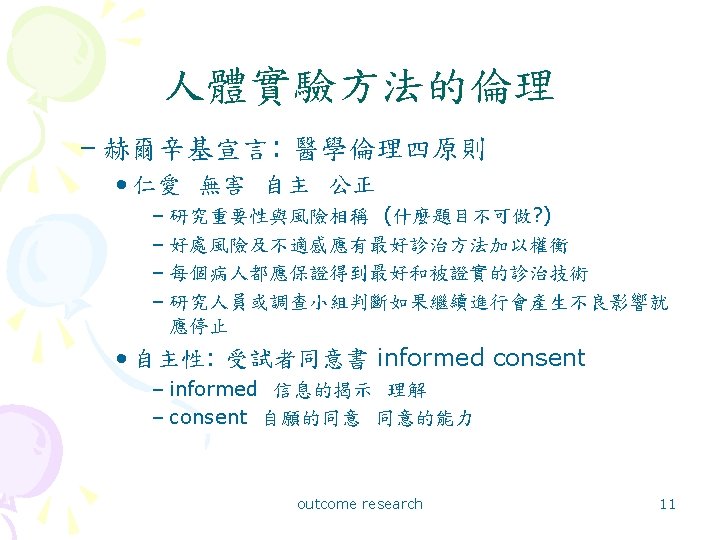
ethical concerns • administered on healthy people – autonomy emphasized: informed consent – safety emphasized: lower tolerance to adverse effects • active drug or placebo controls – placebo controls: standard design, required by FDA – active drug: ethical reason-the best available outcome research 9
人體實驗方法的倫理 • 以藥物臨床試驗發展最完備 – 赫爾辛基宣言 – ICH: International Conference on Harmonisation – GCP: Good Clinical Practice – IRB: Institutional Review Board – 人體試驗委員會 outcome research 10
Cost and effectiveness/utility • Usually proved to be cost-effective • Old schedule and contents of immunization has been established • New vaccines: suffers high cost for R&D • diminishing of marginal return • very difficult to find new, largesampled, disease outcome research 12
Examples • Salmonella typhi Vi conjugate vaccine for children • HPV vaccine for young women – double-blind randomized controlled trials – efficacy: the diseases to prevent • Registry-driven outreach: – randomized controlled trial – administrative study outcome research 13
Salmonella typhi Vi • Lin FYC at el. The efficacy of a Salmonella typhi Vi conjugate vaccine in two-to-five-year-old children – NEJM 2001; 344: 1263 -9. – Vi-r. EPA: Vi 22. 5 ug+r. EPA (Psudomonas aeroginosa exotoxin A) 22 ug in 0. 5 ml of phosphate-buffered saline + 0. 01% thimerosal – enhance immunogenicity 14 outcome research
Vi-r. EPA: background/goal/hypothesis • Background: – typhoid fever of children under 5 years in developing countries – the need for vaccination/ previous studies • Goal/hypothesis: – to determine whether. . . /the vaccine is safe and can prevent typhoid fever in 2 -5 -year-old children outcome research 15
Vi-r. EPA: study design • Randomized controlled double-blinded trial – vaccine vs. saline placebo control – five-dose vials, indistinguishable 0. 5 ml. X 5 (2. 8 ml/vial) – randomized by individual random number 09 • randomization code: kept by the Department of Pharmacy of the NIH Clinical Center and by the chairman of the safety monitoring committee • broken on June 23, 2000 outcome research 16
Vi-r. EPA: study design • Randomization – by individual – for subjects: seven-digit ID – for injection vials: 0 -9 on a random basis – subject vs. vial • the same last digit outcome research 17
Vi-r. EPA: study design • Injection protocol • two rounds – 2/21 -3/8/1998… 4/4 -4/20/1998, 64 teams – separate 6 weeks – 0. 5 ml with identical last digit • examination before and observations after injection outcome research 18
Vi-r. EPA: subjects • Cao Lanh District of Dong Thap Province in the Mekong Delta of Vietnam • 13776 children (96. 4% of 14285) enrolled – exclusion: with illness requiring ongoing medical care • informed consents – parents or guardians outcome research 19
Vi-r. EPA: subjects • At least one injection: 12008 (5991: 6017) • Two injections from correctly labeled vials: 11091 (5525: 5566) outcome research 20
Vi-r. EPA: exposure/intervention • 0. 5 ml Vi-r. EPA X 2 six weeks apart – only one experiment group – control: saline placebo outcome research 21
Vi-r. EPA: endpoints • Primary – efficacy: typhoid fever attack rate – safety: rates of adverse effects • Secondary – paired serum Ig. G antibody titer (ELISA) – antibody persistence • Follow-up – visit weekly to 5/31/2000 (2 years) 22 outcome research
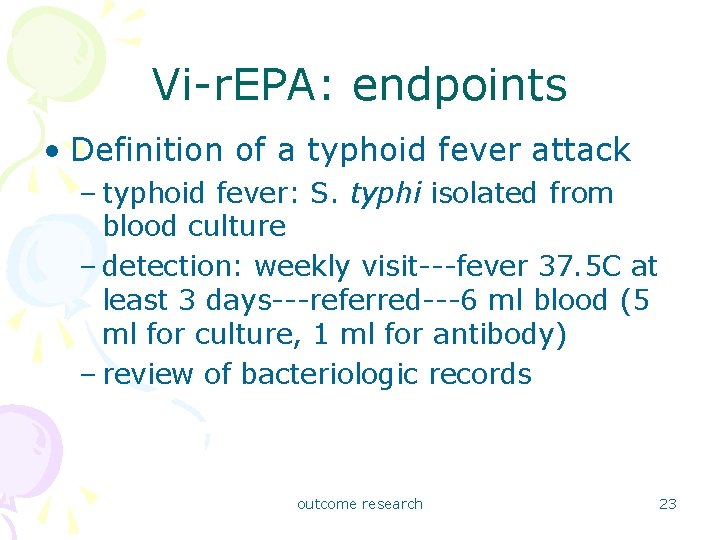
Vi-r. EPA: endpoints • Definition of a typhoid fever attack – typhoid fever: S. typhi isolated from blood culture – detection: weekly visit---fever 37. 5 C at least 3 days---referred---6 ml blood (5 ml for culture, 1 ml for antibody) – review of bacteriologic records outcome research 23
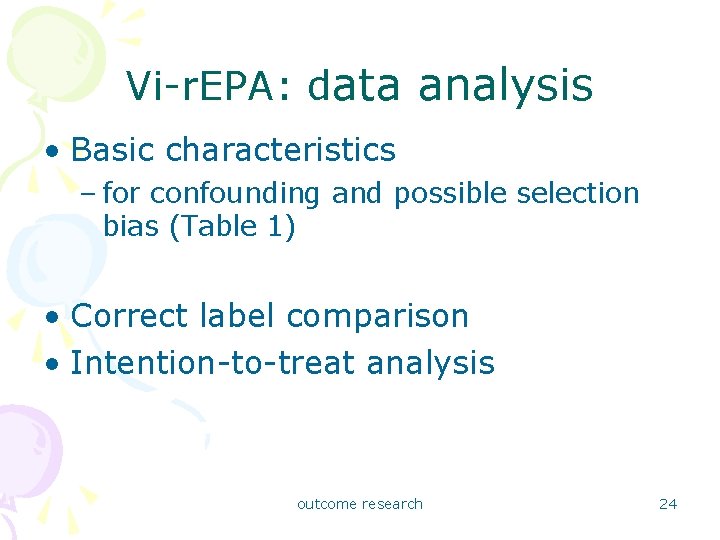
Vi-r. EPA: data analysis • Basic characteristics – for confounding and possible selection bias (Table 1) • Correct label comparison • Intention-to-treat analysis outcome research 24
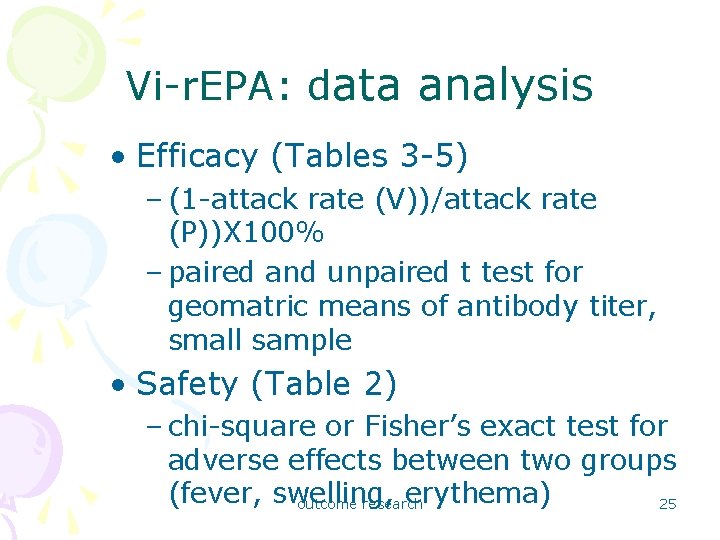
Vi-r. EPA: data analysis • Efficacy (Tables 3 -5) – (1 -attack rate (V))/attack rate (P))X 100% – paired and unpaired t test for geomatric means of antibody titer, small sample • Safety (Table 2) – chi-square or Fisher’s exact test for adverse effects between two groups (fever, swelling, erythema) 25 outcome research
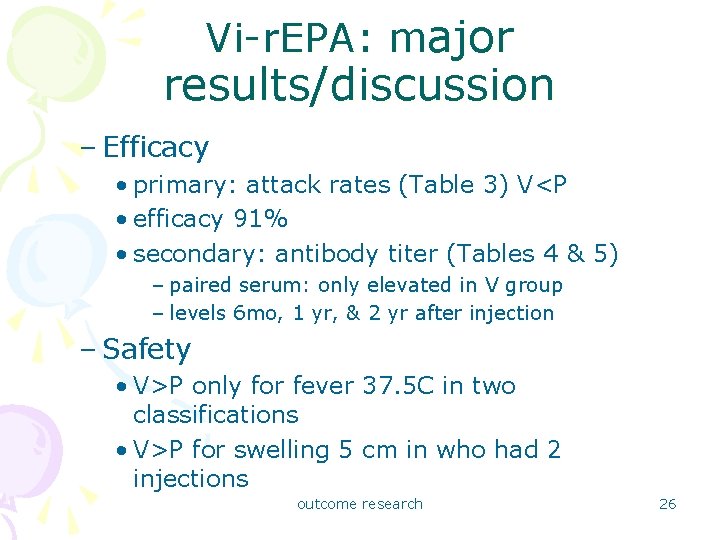
Vi-r. EPA: major results/discussion – Efficacy • primary: attack rates (Table 3) V<P • efficacy 91% • secondary: antibody titer (Tables 4 & 5) – paired serum: only elevated in V group – levels 6 mo, 1 yr, & 2 yr after injection – Safety • V>P only for fever 37. 5 C in two classifications • V>P for swelling 5 cm in who had 2 injections outcome research 26
Vi-r. EPA: major results/discussion • Discussion – Confounding, selection bias: randomization – Information bias: blindness – Definition – Sample size and power of test • Conclusion: – safe and 90% efficacy for 2 -5 years outcome research 27
HPV • Koutsky LA, et al. A controlled trial of a human papillomavirus type 16 vaccine – NEJM 2002; 347: 1645 -51. – HPV-16 L 1 virus-like particle vaccine – purified L 1 polypeptide (yeast) outcome research 28
HPV: background/goal/hypothesis • Background: – HPV as a STD/ HVP-16 and cervical cancer – HPV-16 L 1 virus-like particle • Goal/hypothesis: – to determine whether. . . /the vaccine can prevent HPV-16 infection in women (reduce the incidence of persistent HPV infection) outcome research 29
HPV: study design • Randomized controlled doubleblinded trial – vaccine vs. placebo control – double-blind: indistinguishable – intramuscular injection – randomized by individual – permuted-block design 1: 1 outcome research 30
HPV: subjects – 10/1998 -11/1999, 2392 women from 16 centers in the US / advertisement: 1194 vs. 1198 – inclusion criteria: • 16 -23 years, not pregnant, reported no prior abnormal Pap smears, no more than 5 male sex partners, virgins seeking contraception – exclusion (Table 1) • positive infection before intervention completed and other reasons – informed consents, IRB, compensation per visit outcome research 31
HPV: subjects • Sample size – fixed-number-of-events design – at least 31 cases required to show a statistically significant reduction in the primary endpoint – 75% efficacy, 90% power, 2% dropout per yr – 2350 enrolled – 31 cases on 8/31/2001… primary analysis 32 outcome research
HPV: exposure/intervention • Vaccine – 40 ug HPV-16 L 1 virus-like particles + 225 ug of aluminum adjuvant = 0. 5 ml – only one experiment group – control: placebo 225 ug of aluminum adjuvant in 0. 5 ml – im injection at day 0, month 2, and month 6 outcome research 33
HPV: endpoints • Primary – efficacy: persistent HPV infection (surrogate!) – safety: adverse effects • Secondary – HPV antibody titer 5. 9 m. MU/ml • Follow-up – one month, 6 months after 3 rd vaccination, every six months outcome research 34
HPV: definition and detection of HPV infection – method: • cervical samples: Pap smear, swabs, lavage for HPV-16 DNA testing • abnormal Pap smear: colposcopic exam biopsy – case of ‘persistent’ HPV-16 infection: • (-) at day 0 & month 7… (+) subsequently in 2 or more consecutive visits 4 or more months apart • … biopsy: CIN or cancer and HPV-16 DNA • … HPV-16 DNA detected in the last visit • transient infection: once (+) outcome research 35
HPV: definition and detection of adverse effects • Any sign or symptom of illness or abnormal lab test … – asked 14 d (dairy, primary), 2, 6, and 7 months – that occurred during the protocol-specified follow-up period, that was not present at enrollment, or if present, had worsened • body temperature recorded five days after – 37. 7 C outcome research 36
HPV: data analysis • Exclusion and reasons (Table 1) • Basic characteristics – for confounding and possible selection bias (Table 2) • Fixed-number-of events design • including and excluding violation cases outcome research 37
HPV: data analysis • Efficacy – primary endpoint: efficacy by infection rate person-time • primary analysis: negative before the end of intervention and no violation • second analysis: negative … + general violation • for transient infection/CIN – secondary endpoint: difference of antibody titer at month 7 • geometric means of antibody titer outcome research 38
HPV: data analysis • Safety – adverse events during the 14 days after any of the 3 vaccinations – all subjects included – number of cases (almost equal size) • pain at the injection site • systemic • discontinued due to AE outcome research 39
HPV: major results/discussion – Efficacy – primary on persistent infection rate (Table 3) • primary analysis: 100%! • secondary analysis: 100%! • primary but including transient infection: 91. 2% • for neoplasia: P. 1649 – secondary on antibody titer (immunogenicity) – Safety (Table 4) outcome research 40
HPV: major results/discussion • Discussion – Confounding, selection bias: randomization • exclusion after randomization and intervention! – Information bias: blindness – Definition of cases: persistent, transient? – Sample size and power of test • loss of subjects because of (+) infection in the beginning outcome research 41
HPV: major results/discussion – Follow up time – relation to CIN and CC • Conclusion: – for infection high short-term efficacy – for related neoplasia outcome research 42
Outreach • Wilcox SA, et al. Registry-driven, community-ased immunization outreach: a randomized controlled trial. AJPH 2001; 91: 1507 -11. outcome research 43
Outreach: background/goal/hypothesis • Background: – provider-based vs. community-based registry-driven outreach • Goal/hypothesis: – whether community-based registry-driven outreach can improve immunization rate – whether predictors of under immunization can be used to target at-risk children outcome research 44
Outreach: study design • Randomized controlled trial – three groups • outreach (two samples) • mailed reminder letter • control: no intervention – no double-blindness • both subjects and raters were not blind. – randomized by individual outcome research 45
Outreach: subjects – KIDS immunization database/tracking system – Philadelphia, 1997 – 1696 6 -10 months children/2 random samples – a second random sample: 160 all assigned to the outreach group – no informed consents – IRB review (Albert Einstein Medical Center) outcome research 46
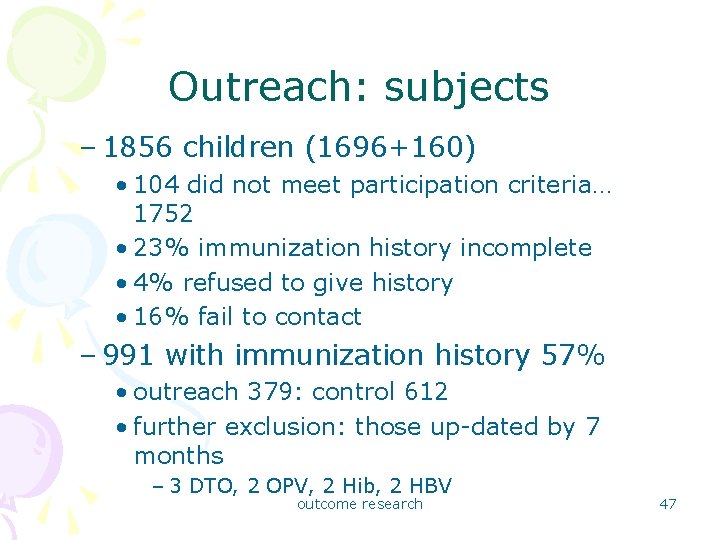
Outreach: subjects – 1856 children (1696+160) • 104 did not meet participation criteria… 1752 • 23% immunization history incomplete • 4% refused to give history • 16% fail to contact – 991 with immunization history 57% • outreach 379: control 612 • further exclusion: those up-dated by 7 months – 3 DTO, 2 OPV, 2 Hib, 2 HBV outcome research 47
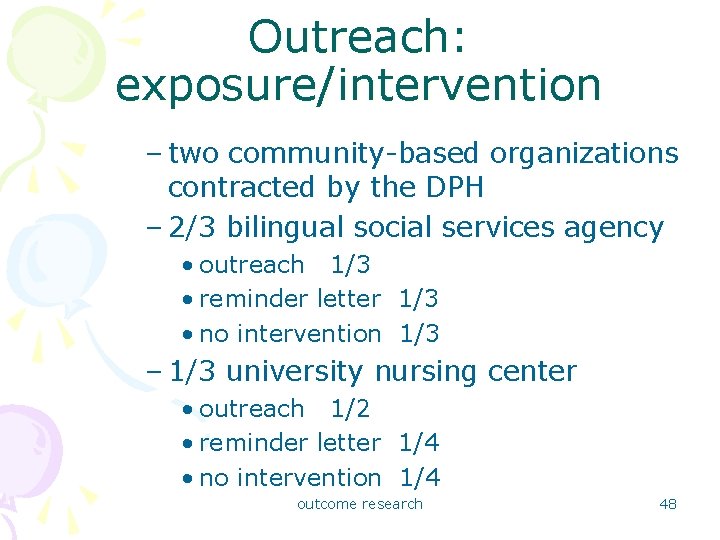
Outreach: exposure/intervention – two community-based organizations contracted by the DPH – 2/3 bilingual social services agency • outreach 1/3 • reminder letter 1/3 • no intervention 1/3 – 1/3 university nursing center • outreach 1/2 • reminder letter 1/4 • no intervention 1/4 outcome research 48
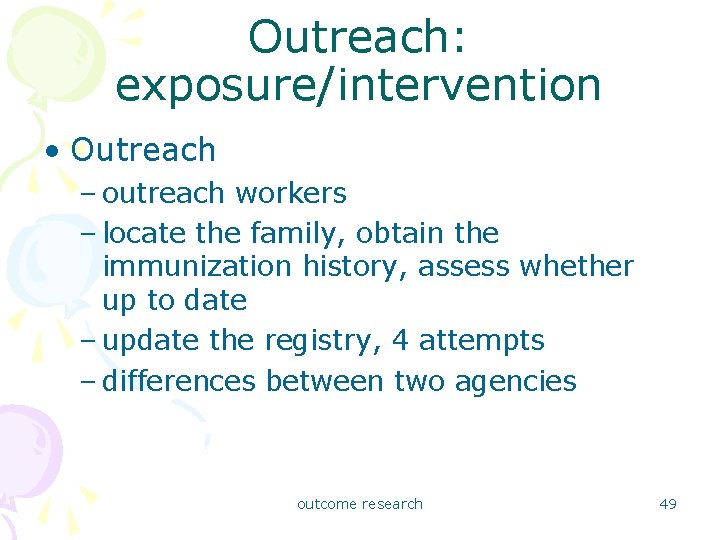
Outreach: exposure/intervention • Outreach – outreach workers – locate the family, obtain the immunization history, assess whether up to date – update the registry, 4 attempts – differences between two agencies outcome research 49
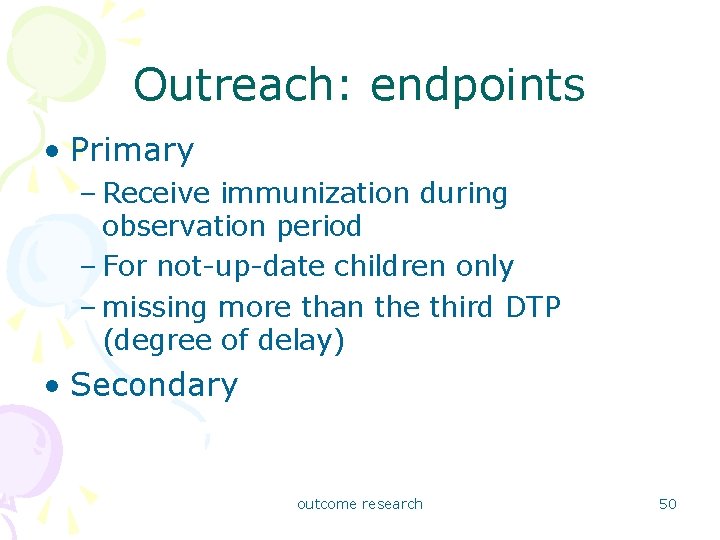
Outreach: endpoints • Primary – Receive immunization during observation period – For not-up-date children only – missing more than the third DTP (degree of delay) • Secondary outcome research 50
Outreach: data analysis • Exclusion and reasons (Table 1) • Basic characteristics – for confounding and possible selection bias (Table 1) outcome research 51
Outreach: data analysis • Efficacy – Only for not-on-time – Adjusting for confounders and assess the effects of predictors (Table 2) – Improve immunization rate (Table 3) • comparable? outcome research 52
Outreach: major results/discussion – Comparability: not comparable? ! – Efficacy • must adjust confounders • only for not-updated … why not exclude first? • information bias: no blindness – Conclusion • Identify high risk children and bring them to care outcome research 53
 Which reaction does akira most fear from chie?
Which reaction does akira most fear from chie? Counseling outcome research and evaluation
Counseling outcome research and evaluation Outcome evaluation
Outcome evaluation Outcome based evaluation definition
Outcome based evaluation definition Research project outcome example
Research project outcome example Louisiana immunization network for kids
Louisiana immunization network for kids Cir vfc
Cir vfc Importance of immunization slideshare
Importance of immunization slideshare Kentucky immunization records
Kentucky immunization records Ohio immunization summary for school attendance
Ohio immunization summary for school attendance Alam awatif
Alam awatif Grits immunization
Grits immunization What is nysiis
What is nysiis Vitamin a dose in immunization schedule
Vitamin a dose in immunization schedule Dr adeiga
Dr adeiga Immunization
Immunization Duration of portfolio
Duration of portfolio Portfolio immunization example
Portfolio immunization example What is polio disease
What is polio disease Kyir registry
Kyir registry Active immunization definition
Active immunization definition Immunization fhir
Immunization fhir Hazards of immunization
Hazards of immunization Conclusion of immunization slideshare
Conclusion of immunization slideshare Immunization schedule
Immunization schedule Global alliance for vaccines and immunization
Global alliance for vaccines and immunization Epi schedule pakistan 2020
Epi schedule pakistan 2020 Defination of immunization
Defination of immunization Cmu immunization
Cmu immunization Bond portfolio immunization techniques
Bond portfolio immunization techniques Adverse events following immunization (aefi) course answers
Adverse events following immunization (aefi) course answers Active vs passive immunization
Active vs passive immunization The major disadvantage of passive immunization is that it
The major disadvantage of passive immunization is that it Purposes of research
Purposes of research Research action communication evaluation
Research action communication evaluation Center for drug evaluation and research
Center for drug evaluation and research Cars checklist for research source evaluation
Cars checklist for research source evaluation Types of evaluation design
Types of evaluation design Research methods in monitoring and evaluation
Research methods in monitoring and evaluation Types of evaluation research
Types of evaluation research Research report vs research proposal
Research report vs research proposal Methods versus methodology
Methods versus methodology Appendix example
Appendix example Example of conclusive research
Example of conclusive research Scope research definition
Scope research definition Example of contribution in research paper
Example of contribution in research paper Contrast applied research and basic research
Contrast applied research and basic research Rephrasing research problem
Rephrasing research problem Research instrument in experimental research
Research instrument in experimental research 40 days baby in womb
40 days baby in womb Correlational and comparative research
Correlational and comparative research Chapter 3 research example
Chapter 3 research example Example of applied research
Example of applied research Bryman bell
Bryman bell