Otitis Media with Effusion Tuberculous otitis media Tympanosclerosis
Otitis Media with Effusion, Tuberculous otitis media, Tympanosclerosis, Adhehesive Otitis Media Dr. Nayana V G Senior Resident Dept of ENT
OME - DEFINITION � Otitis Media - Inflammatory condition of the M E � Middle ear effusion(MEE) is the fluid in ME � An effusion may be either • Serous • Mucoid • Purulent
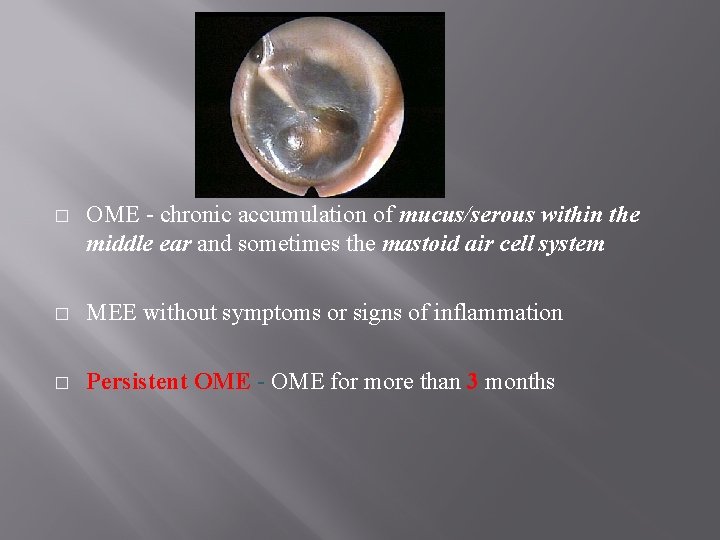
� OME - chronic accumulation of mucus/serous within the middle ear and sometimes the mastoid air cell system � MEE without symptoms or signs of inflammation � Persistent OME - OME for more than 3 months
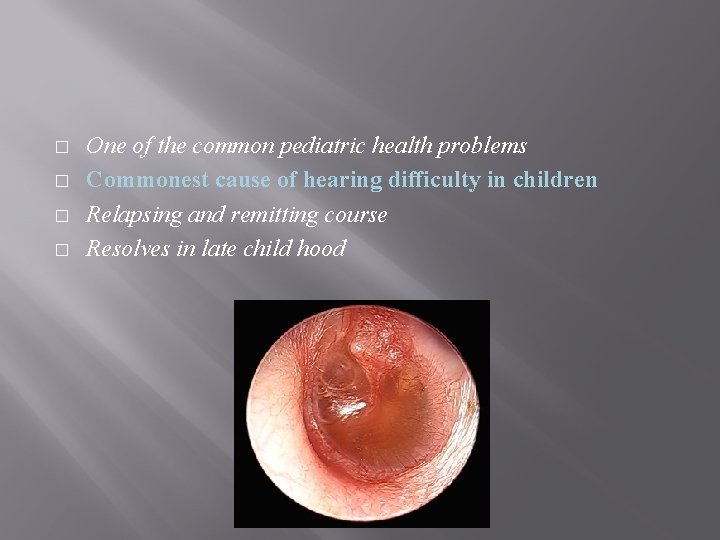
� � One of the common pediatric health problems Commonest cause of hearing difficulty in children Relapsing and remitting course Resolves in late child hood
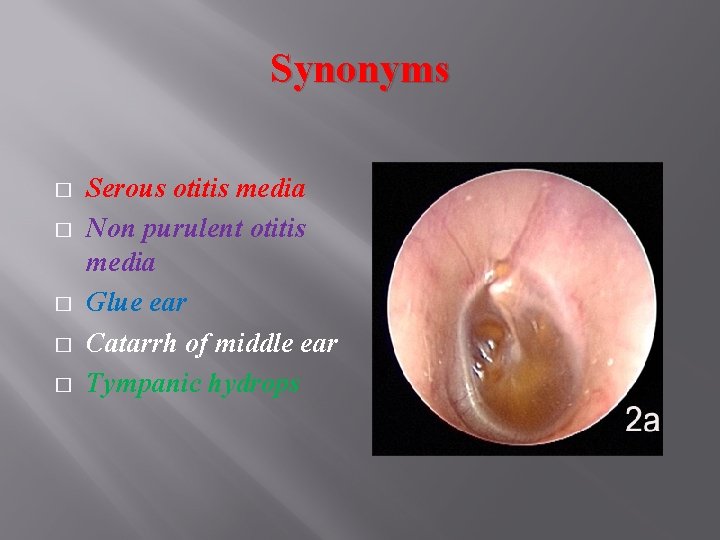
Synonyms � � � Serous otitis media Non purulent otitis media Glue ear Catarrh of middle ear Tympanic hydrops
EPIDEMIOLOGY � < 2 year children - 50% have OME � Highest incidence in 6 to 24 month age group � Prevalence in children 10 to 30 % � Adults make up 15% of OME cases
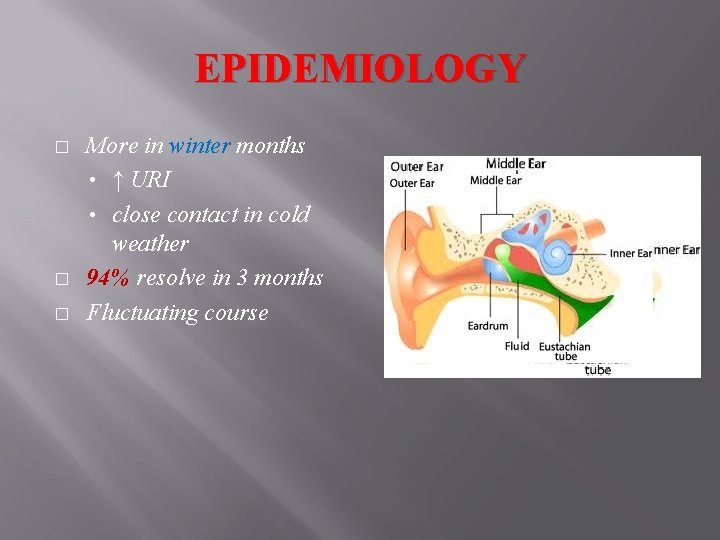
EPIDEMIOLOGY � � � More in winter months • ↑ URI • close contact in cold weather 94% resolve in 3 months Fluctuating course
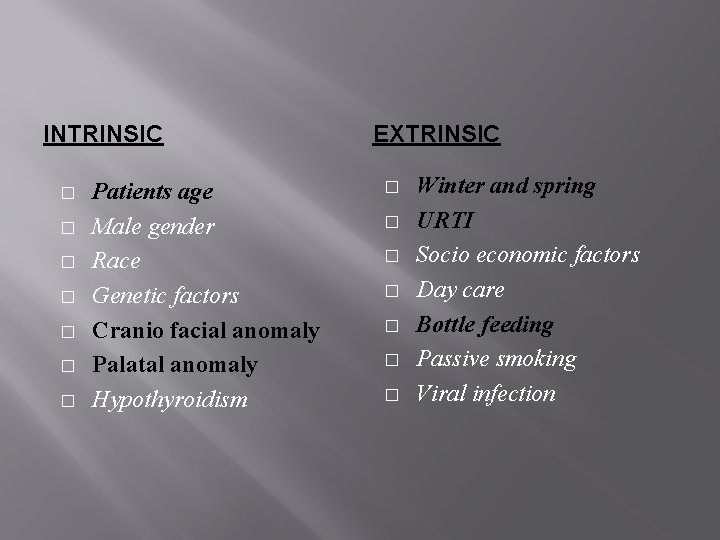
INTRINSIC � � � � Patients age Male gender Race Genetic factors Cranio facial anomaly Palatal anomaly Hypothyroidism EXTRINSIC � � � � Winter and spring URTI Socio economic factors Day care Bottle feeding Passive smoking Viral infection
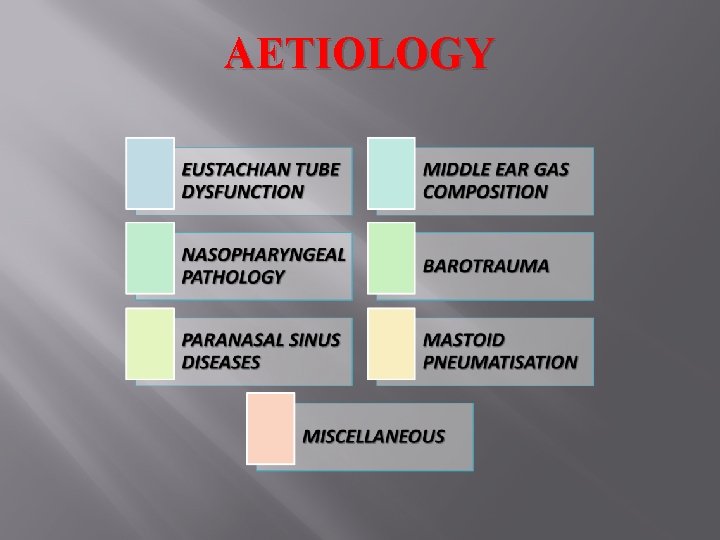
AETIOLOGY
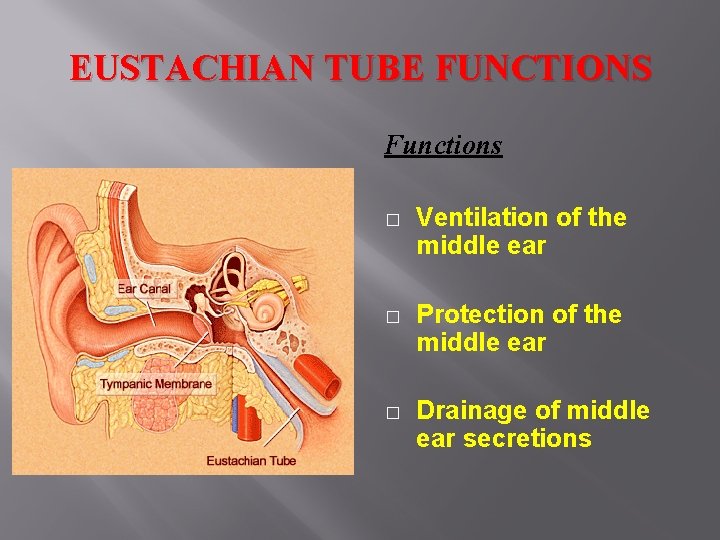
EUSTACHIAN TUBE FUNCTIONS Functions � Ventilation of the middle ear � Protection of the middle ear � Drainage of middle ear secretions
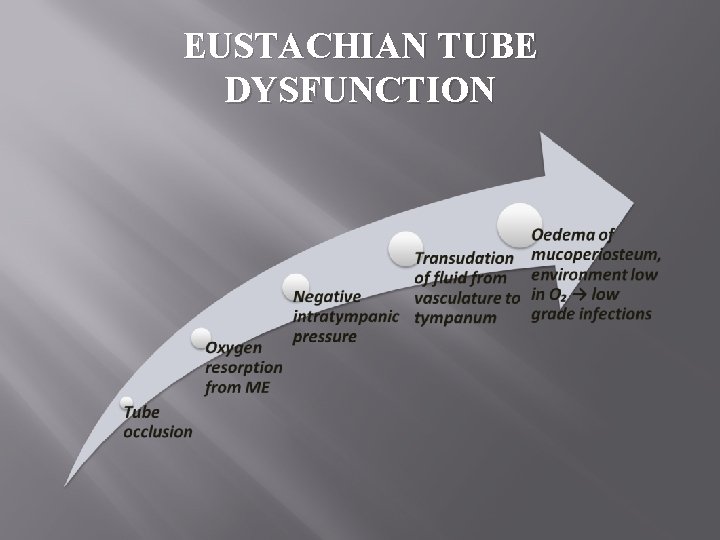
EUSTACHIAN TUBE DYSFUNCTION
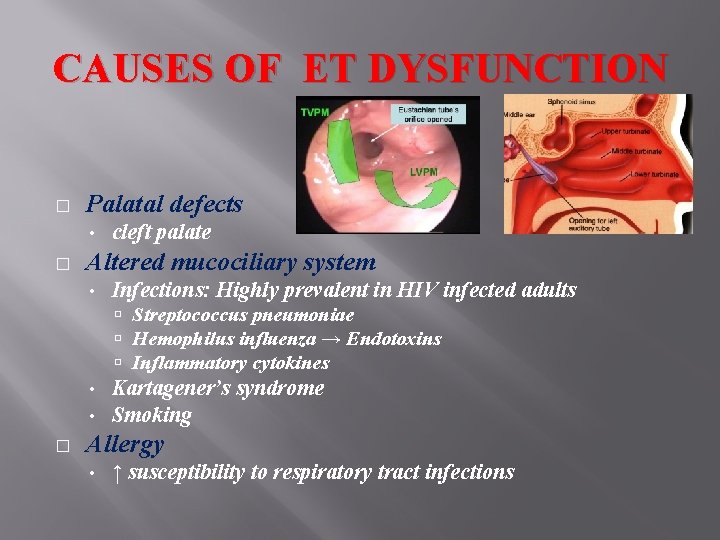
CAUSES OF ET DYSFUNCTION � Palatal defects • � cleft palate Altered mucociliary system • Infections: Highly prevalent in HIV infected adults Streptococcus pneumoniae Hemophilus influenza → Endotoxins Inflammatory cytokines • • � Kartagener’s syndrome Smoking Allergy • ↑ susceptibility to respiratory tract infections
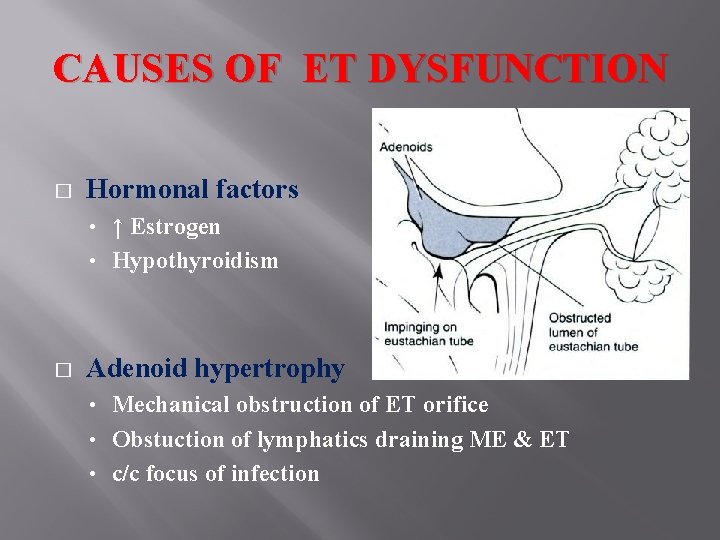
CAUSES OF ET DYSFUNCTION � Hormonal factors ↑ Estrogen • Hypothyroidism • � Adenoid hypertrophy Mechanical obstruction of ET orifice • Obstuction of lymphatics draining ME & ET • c/c focus of infection •
NASOPHARYNGEAL CAUSES • � � Nasopharyngeal disproportion • Craniofacial abnormality; Syndromes…. Adenoid hypertrophy Tumors • Nasopharyngeal carcinoma • Tensor veli palatini destruction • Eustachian tube cartilage erosion • Mechanical obstruction
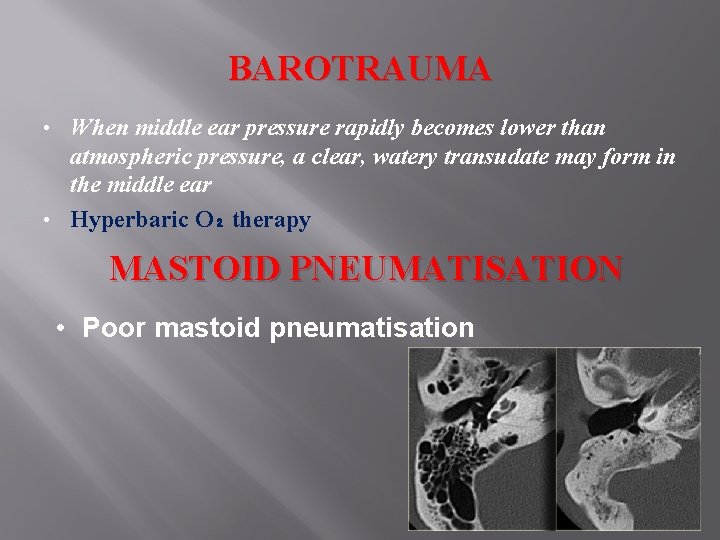
BAROTRAUMA When middle ear pressure rapidly becomes lower than atmospheric pressure, a clear, watery transudate may form in the middle ear • Hyperbaric O₂ therapy • MASTOID PNEUMATISATION • Poor mastoid pneumatisation

MISCELLANEOUS • Iatrogenic • • Inadequate antibiotic therapy Radiation therapy H&N surgeries (Maxillectomy. . ) Prolonged intubation Trauma following adenoidectomy Multiple myeloma Poly Arteritis Nodosa Immune Deficiency Syndromes
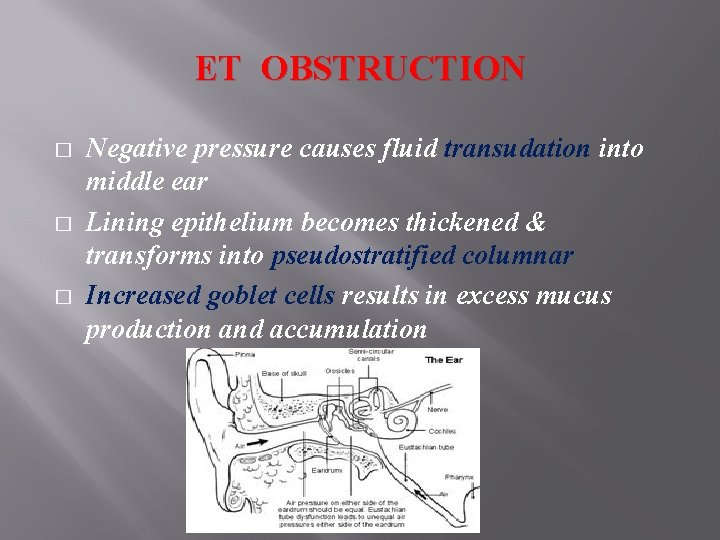
ET OBSTRUCTION � � � Negative pressure causes fluid transudation into middle ear Lining epithelium becomes thickened & transforms into pseudostratified columnar Increased goblet cells results in excess mucus production and accumulation
CLASSIFICATION OF ME FLUID
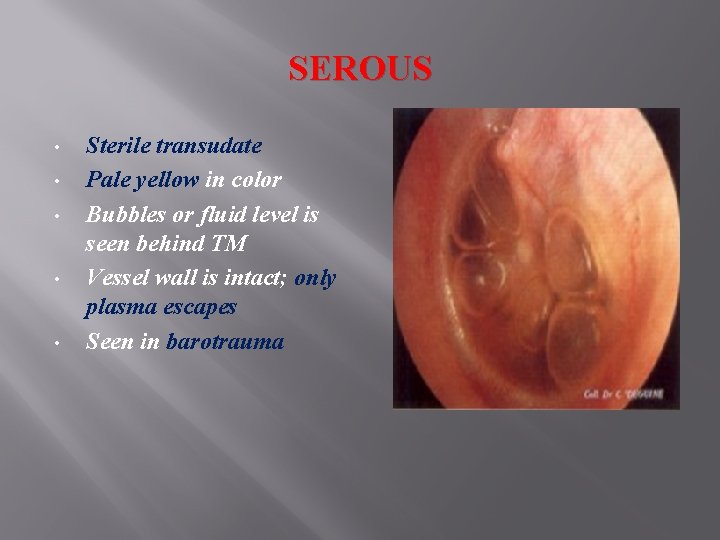
SEROUS • • • Sterile transudate Pale yellow in color Bubbles or fluid level is seen behind TM Vessel wall is intact; only plasma escapes Seen in barotrauma
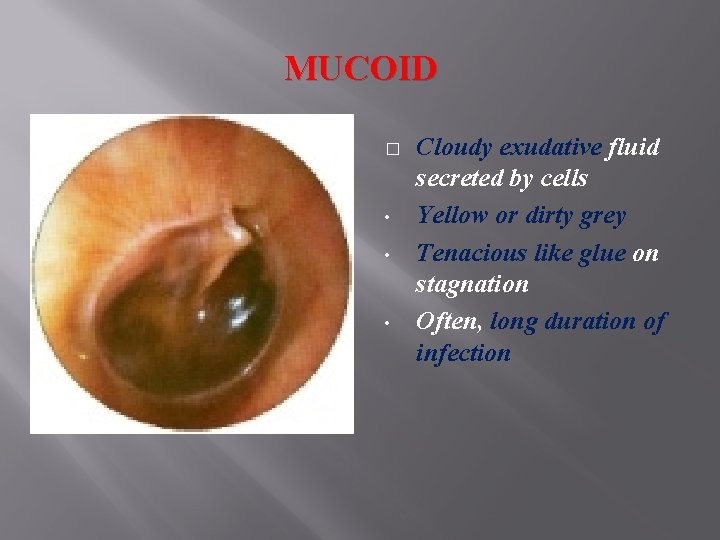
MUCOID � • • • Cloudy exudative fluid secreted by cells Yellow or dirty grey Tenacious like glue on stagnation Often, long duration of infection
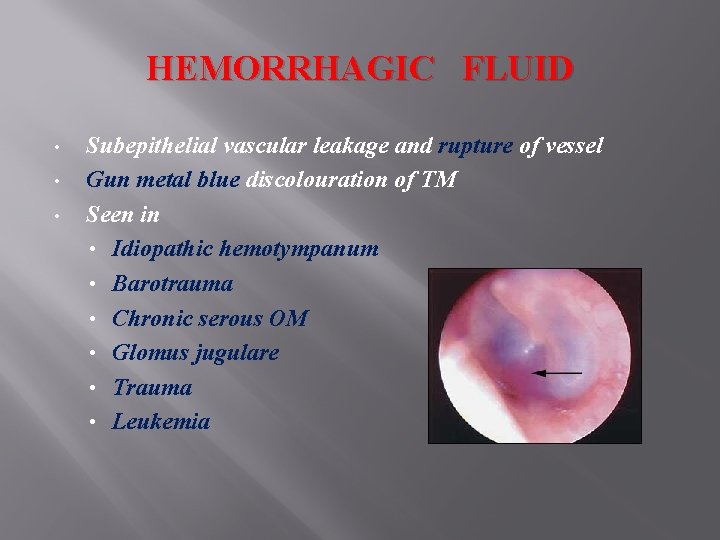
HEMORRHAGIC FLUID • • • Subepithelial vascular leakage and rupture of vessel Gun metal blue discolouration of TM Seen in • Idiopathic hemotympanum • Barotrauma • Chronic serous OM • Glomus jugulare • Trauma • Leukemia
CLINICAL FEATURES • • Fluctuating hearing loss Rhinosinusitis & Allergy In children: • Impaired speech and language in children • Behavioral and scholastic difficulties In adults: • Plugged up or blocked feeling • Decreased hearing • Otalgia • Otorrhoea • Pulsatile & crackling tinnitus
PHYSICAL FINDINGS AND EVALUATION • • • Otoscopy Nasopharyngeal examination Audiological examination Radiological evaluation Allergic testing Myringotomy
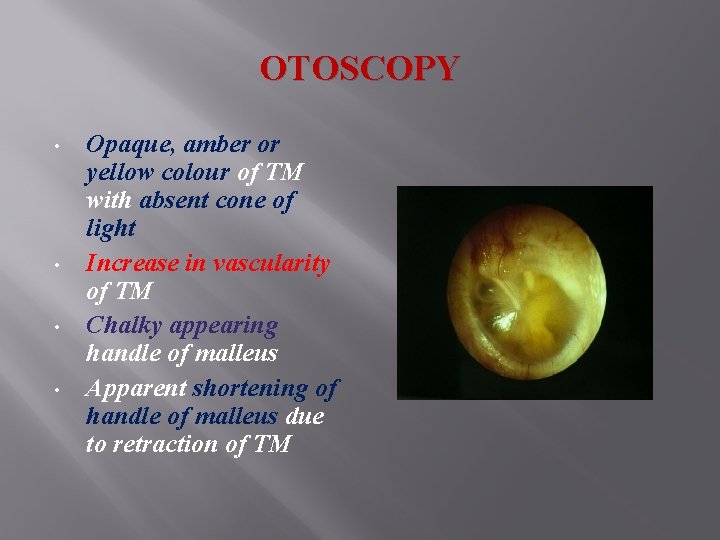
OTOSCOPY • • Opaque, amber or yellow colour of TM with absent cone of light Increase in vascularity of TM Chalky appearing handle of malleus Apparent shortening of handle of malleus due to retraction of TM
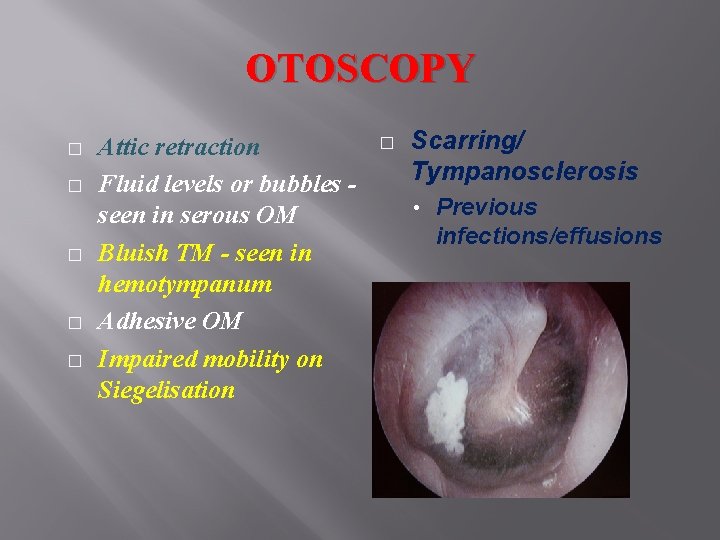
OTOSCOPY � � � Attic retraction Fluid levels or bubbles seen in serous OM Bluish TM - seen in hemotympanum Adhesive OM Impaired mobility on Siegelisation � Scarring/ Tympanosclerosis • Previous infections/effusions
NASAL AND NASOPHARYNGEAL EXAMINATION � Important in unilateral MEE to rule out nasopharyngeal tumor
AUDIOLOGICAL EXAMINATION • • Tuning fork test - for children > 4 years Rinne test negative Weber test lateralised to ear with effusion In children, speech testing should be included
PTA • • • Limited value only To assess the severity To monitor progress and effect of treatment
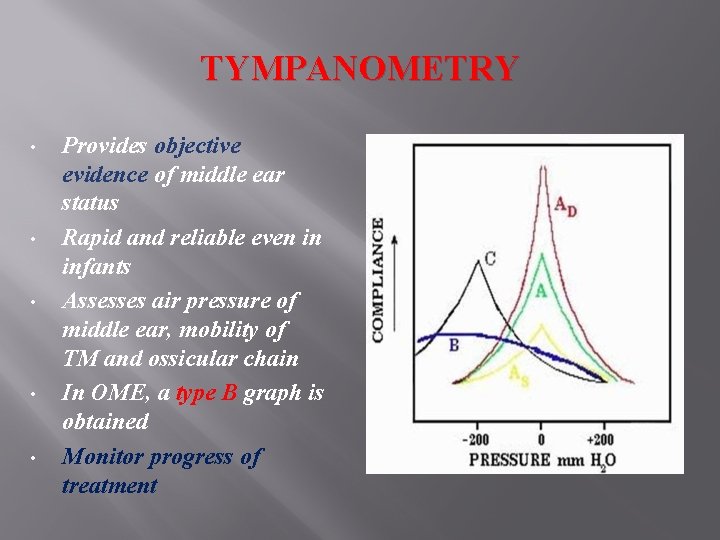
TYMPANOMETRY • • • Provides objective evidence of middle ear status Rapid and reliable even in infants Assesses air pressure of middle ear, mobility of TM and ossicular chain In OME, a type B graph is obtained Monitor progress of treatment
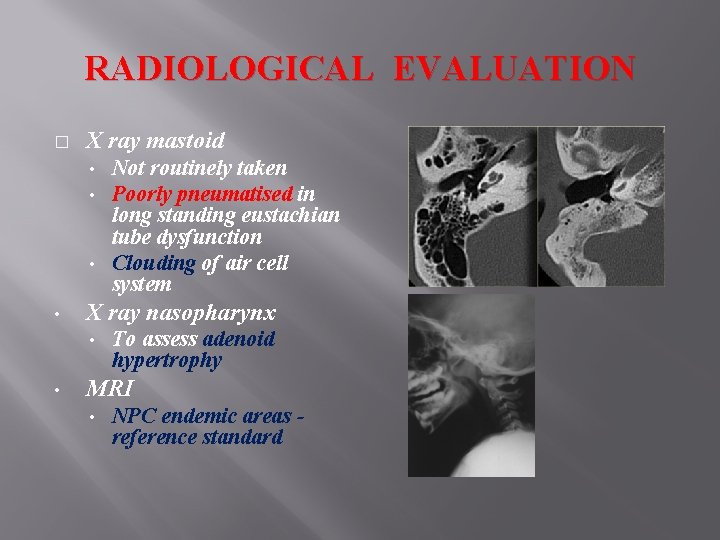
RADIOLOGICAL EVALUATION � X ray mastoid Not routinely taken Poorly pneumatised in long standing eustachian tube dysfunction • Clouding of air cell system • • • X ray nasopharynx • • To assess adenoid hypertrophy MRI • NPC endemic areas reference standard

MYRINGOTOMY / TYMPANOCENTESIS � Gold standard for diagnosis of middle ear effusion in earlier days
MANAGEMENT � Medical • Antibiotics, antihistaminics and decongestants • Exercises to ventilate ET; Autoinflation • Allergic hyposensitisation; dietary elimination • Corticosteroids – nasal spray or systemic • Anti-pneumococcal vaccination • Surgical Note – 50 % resolve spontaneously within 3 months •
ANTIBIOTICS • • Indicated in purulent OM May be useful in patients in whom inadequate initial therapy during AOM Persistent mucopurulent or seropurulent effusion Amoxycillin has been the standard drug
ANTIHISTAMINES / DECONGESTANTS � � � Reduce the congestion of ET Shrinkage of mucosa in nose and PNS Shrinkage of ET mucosa ET AUTOINFLATION • Chewing gum, frequent swallows • Valsalva and Toynbee maneuver • Politzerisation
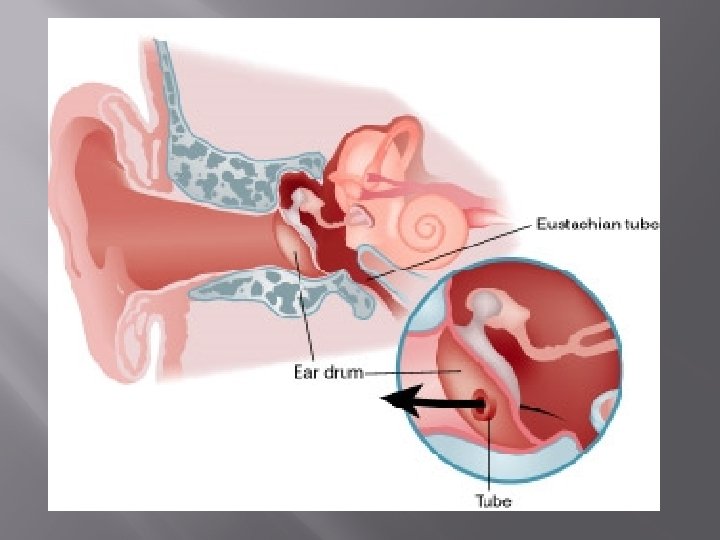
SURGICAL TREATMENT � Control of regional inflammation and obstructive foci • � Nasal/Sinus procedures, Adenoidectomy, Tonsillectomy Myringotomy with grommet insertion
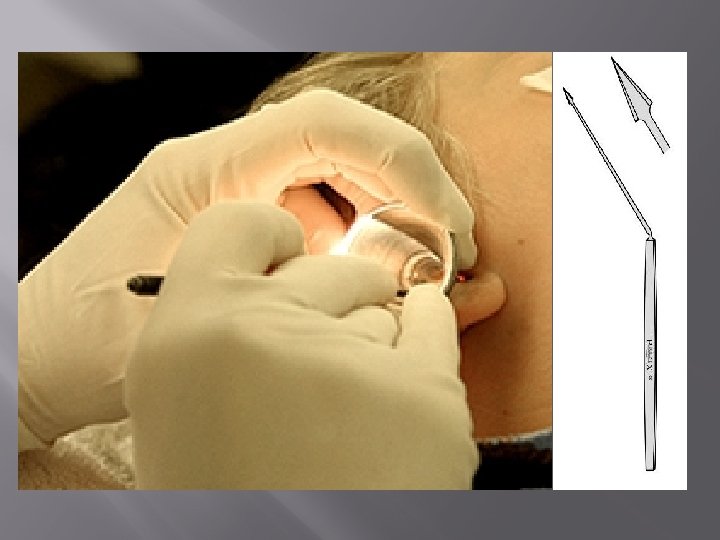
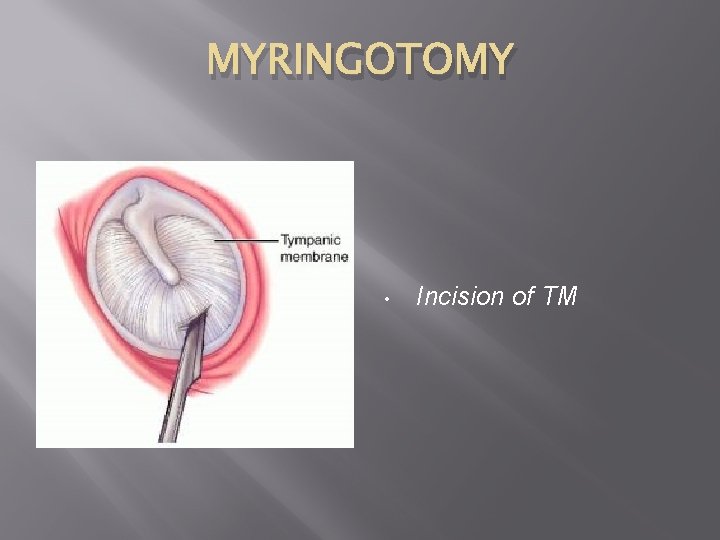
MYRINGOTOMY • Incision of TM
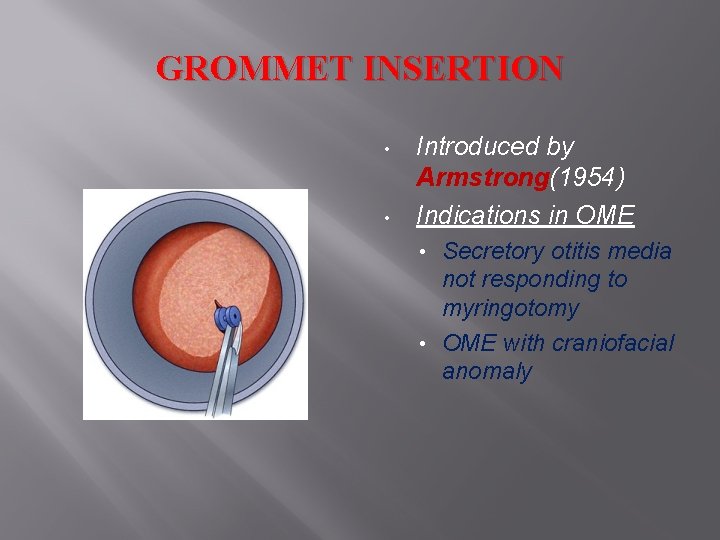
GROMMET INSERTION • • Introduced by Armstrong(1954) Indications in OME Secretory otitis media not responding to myringotomy • OME with craniofacial anomaly •
VETILATION TUBES
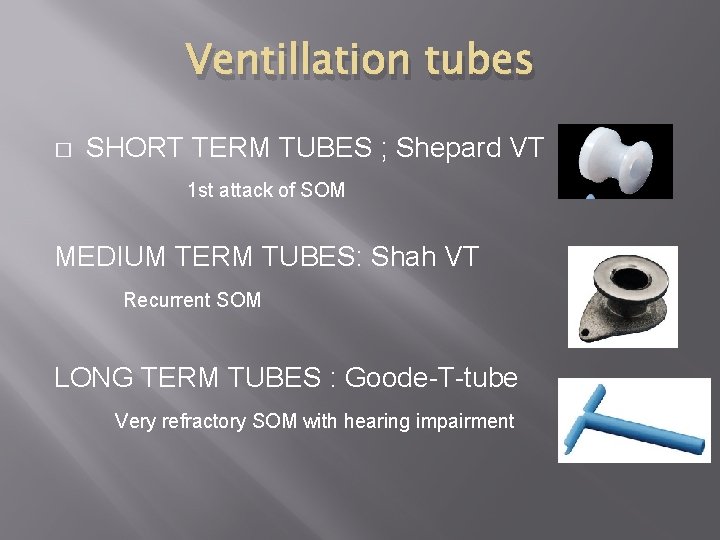
Ventillation tubes � SHORT TERM TUBES ; Shepard VT 1 st attack of SOM MEDIUM TERM TUBES: Shah VT Recurrent SOM LONG TERM TUBES : Goode-T-tube Very refractory SOM with hearing impairment
POST OP CARE � � � Follow up audiometry • Residual 10 d. B hearing loss → ossicular immobility Residual fluid/mucosal edema around Periodic review Avoid entry of water in to the ear
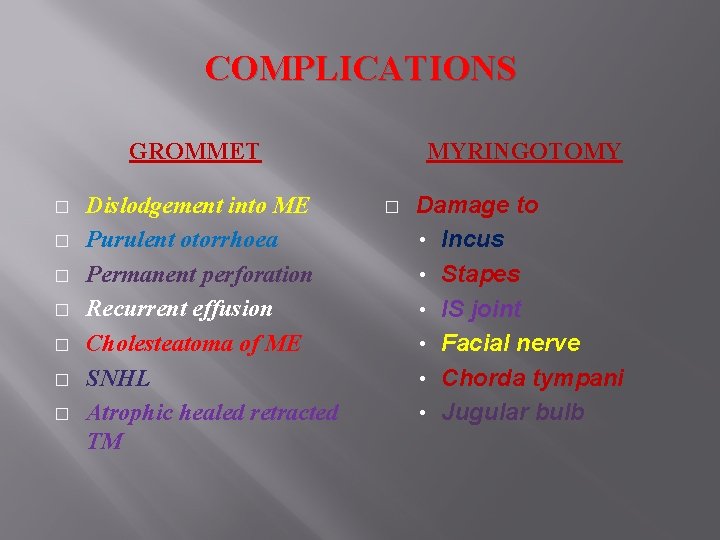
COMPLICATIONS GROMMET � � � � Dislodgement into ME Purulent otorrhoea Permanent perforation Recurrent effusion Cholesteatoma of ME SNHL Atrophic healed retracted TM MYRINGOTOMY � Damage to • Incus • Stapes • IS joint • Facial nerve • Chorda tympani • Jugular bulb
HEARING AIDS � � Beneficial in Downs syndrome, Cleft palate Give aided thresholds May cause noise trauma once OME resolves Safer option → Bone Anchored Hearing Aids
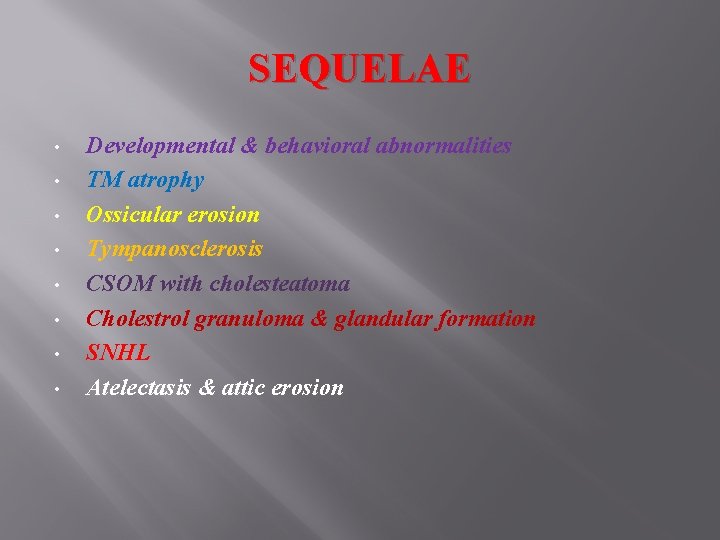
SEQUELAE • • Developmental & behavioral abnormalities TM atrophy Ossicular erosion Tympanosclerosis CSOM with cholesteatoma Cholestrol granuloma & glandular formation SNHL Atelectasis & attic erosion
Tuberculosis of middle ear Jean Louis Petit first described TB of middle ear cleft INCIDENCE ( 0. 4% to 0. 9% )
Tubercular Otitis Media � Route of spread - Secondary to pulmonary TB Lymphatic spread - Direct entry through tympanic membrane perforation � Blood borne from focus from lungs , tonsils , cervical or mesenteric LN � Seen in children and young adult
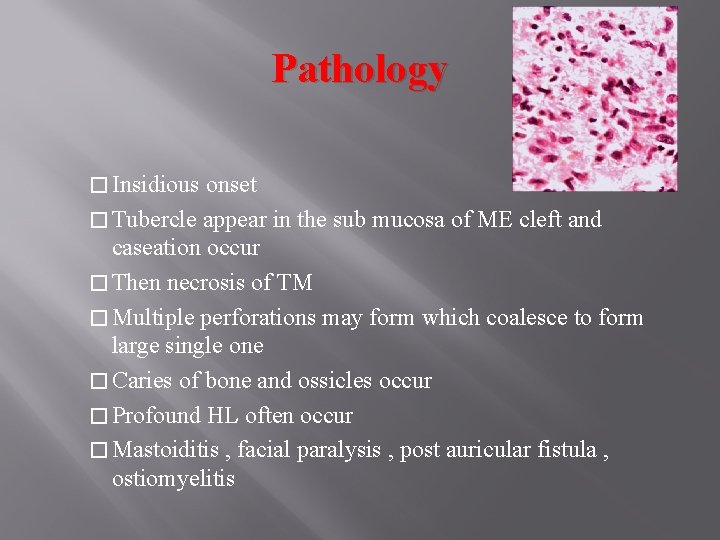
Pathology � Insidious onset � Tubercle appear in the sub mucosa of ME cleft and caseation occur � Then necrosis of TM � Multiple perforations may form which coalesce to form large single one � Caries of bone and ossicles occur � Profound HL often occur � Mastoiditis , facial paralysis , post auricular fistula , ostiomyelitis
Symptoms : 1)Defective hearing –COHL, not progressing, SNHL due to involvement of labyrinth 2)Tinnitus 3)Fullness in the ear 4)Painless otorrhoea-initially thin, scanty, odourless, later more mucoid, copious, thicker & foul smelling 5 Facial paralysis
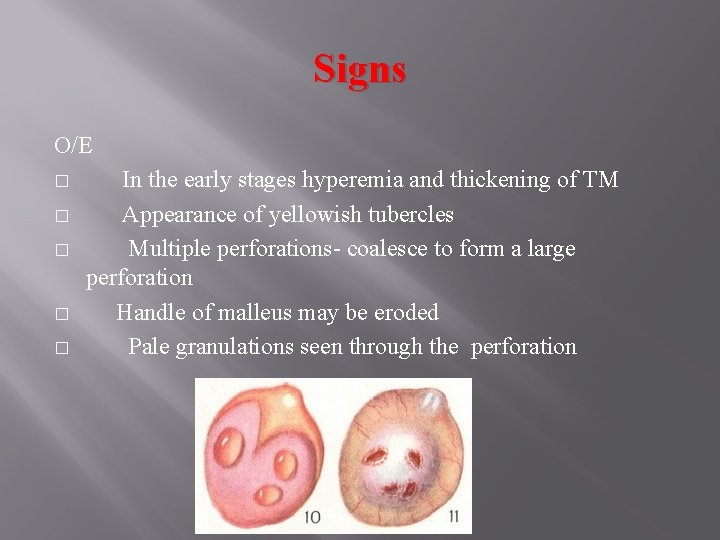
Signs O/E � � � In the early stages hyperemia and thickening of TM Appearance of yellowish tubercles Multiple perforations- coalesce to form a large perforation Handle of malleus may be eroded Pale granulations seen through the perforation
Complications � � � � Labyrinthitis: occurs at early stage of disease, may end up with extensive caries of bone. Bone necrosis with sequestration of ossicles. Intracranial extension: meningitis, brain abscess, tuberculoma, lateral sinus thrombophlebitis Petrositis Facial paralysis Preauricular lymphadenitis Discharging sinus
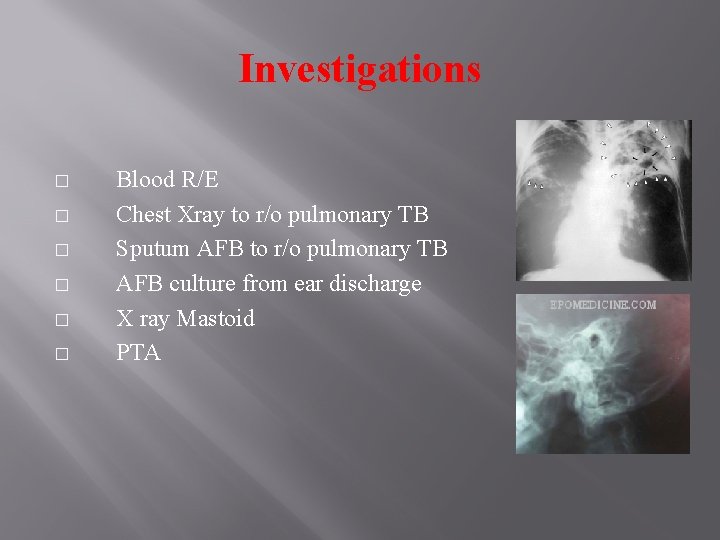
Investigations � � � Blood R/E Chest Xray to r/o pulmonary TB Sputum AFB to r/o pulmonary TB AFB culture from ear discharge X ray Mastoid PTA
� � ATT Persistent discharge: 20% solution of PAS in Glycerine. Boric acid in alcohol Surgery-Mastoidectomy in case of complications, done to clear pus, granulations and sequestrum and to enable antituberculous drugs to act on the remaining disease to prevent complications.
ADHEHESIVE OTITIS MEDIA Chronic Catarrhal Otitis Media Abacterial inflammation of middle ear and adjoining pneumatic spaces Fibous adhehesive process of mucosa of the tympanic cavity with the formation of adhesions and ossicular chain stiffness and progressive deterioration of hearing
Pathology Recurrent infections of middle ear Fibrosis and necrosis of middle ear structure Fibrosis will pull in the TM TM is adherent to the ossicles and promontory
3 Stages of OM Acute Stage of Otosalpingitis Inflammation of middle ear cleft -> mucosal damage and fibrinous exudate Intermediate Stage Organization of the exudate and formation of adhehesions Terminal Stage Fibrous adhesions and diminished aeration of mastoid air cells > Bone resorptions
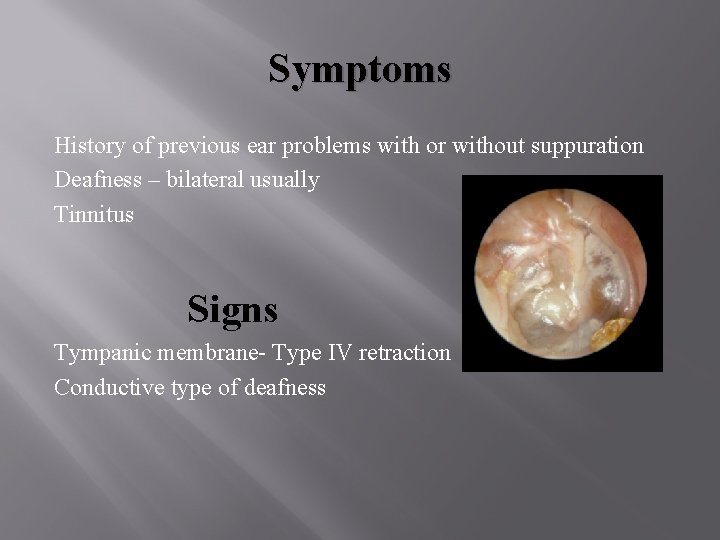
Symptoms History of previous ear problems with or without suppuration Deafness – bilateral usually Tinnitus Signs Tympanic membrane- Type IV retraction Conductive type of deafness
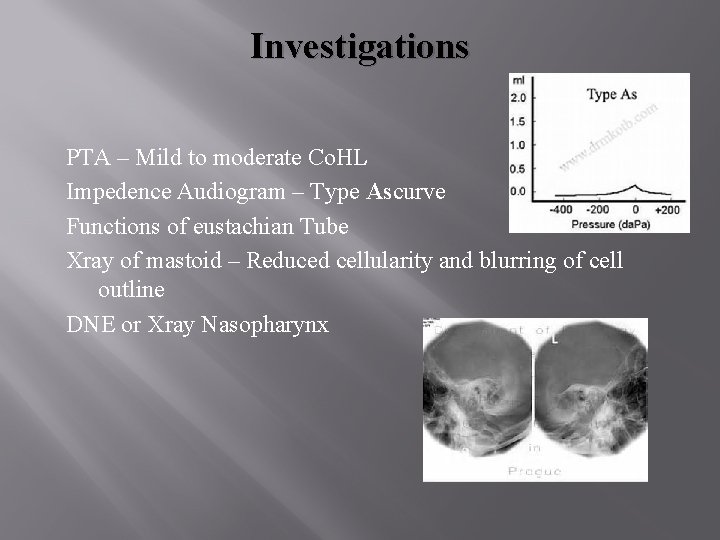
Investigations PTA – Mild to moderate Co. HL Impedence Audiogram – Type Ascurve Functions of eustachian Tube Xray of mastoid – Reduced cellularity and blurring of cell outline DNE or Xray Nasopharynx

TREATMENT Surgical Tympanoplasty Removal of adhesions, Silastic sheet between promontary and graft Second stage surgery Ossicular chain reconstruction after 6 months
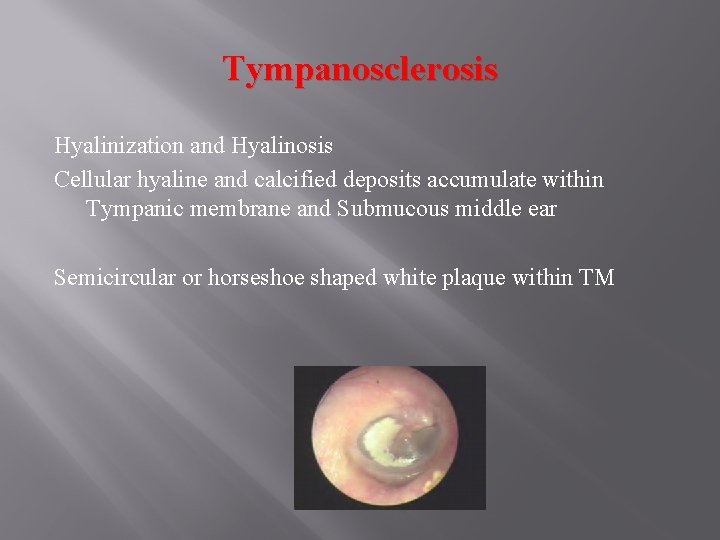
Tympanosclerosis Hyalinization and Hyalinosis Cellular hyaline and calcified deposits accumulate within Tympanic membrane and Submucous middle ear Semicircular or horseshoe shaped white plaque within TM
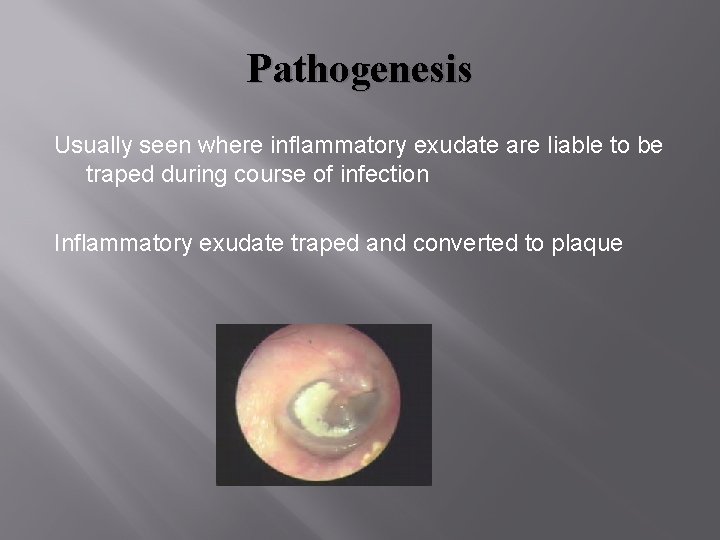
Pathogenesis Usually seen where inflammatory exudate are liable to be traped during course of infection Inflammatory exudate traped and converted to plaque
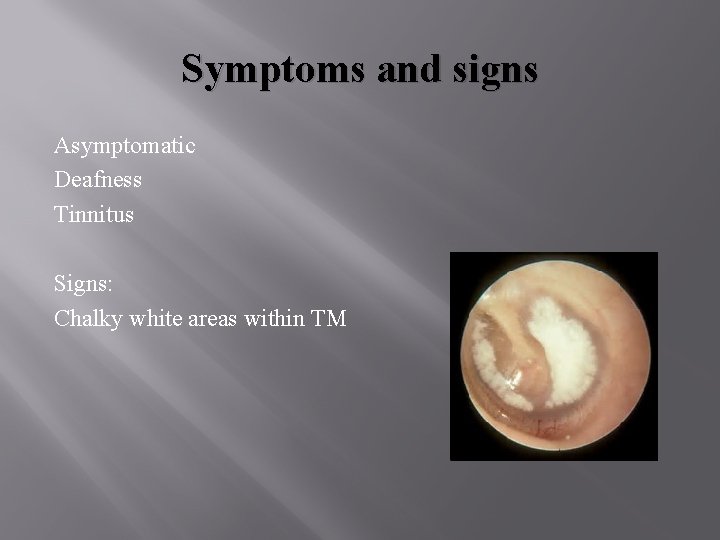
Symptoms and signs Asymptomatic Deafness Tinnitus Signs: Chalky white areas within TM
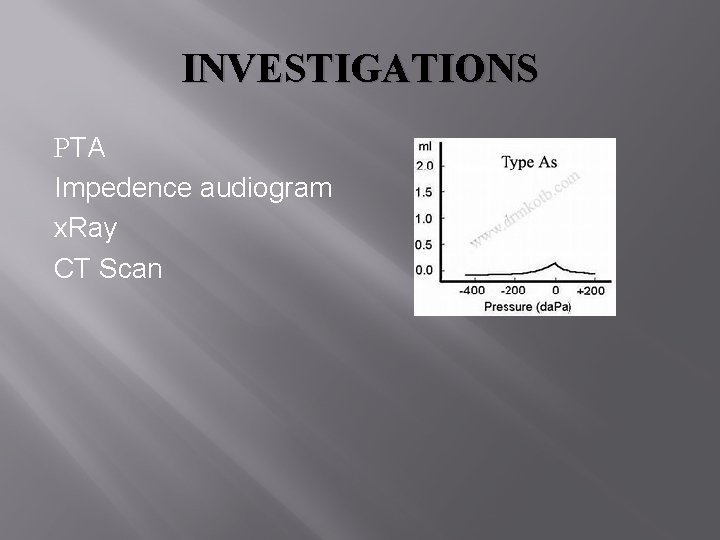
INVESTIGATIONS PTA Impedence audiogram x. Ray CT Scan
Treatment Removal of Tympanosclerosis
- Slides: 64