Otitis Media and Eustachian Tube Dysfunction R Kent
Otitis Media and Eustachian Tube Dysfunction R. Kent Dyer, Jr. , M. D. Hough Ear Institute Oklahoma City, Oklahoma USA
Incidence of Otitis Media (OM) l Most common disease of childhood after viral URI l 15 million cases of Acute OM/year in U. S. l Cost of treatment: >$5 billion/year
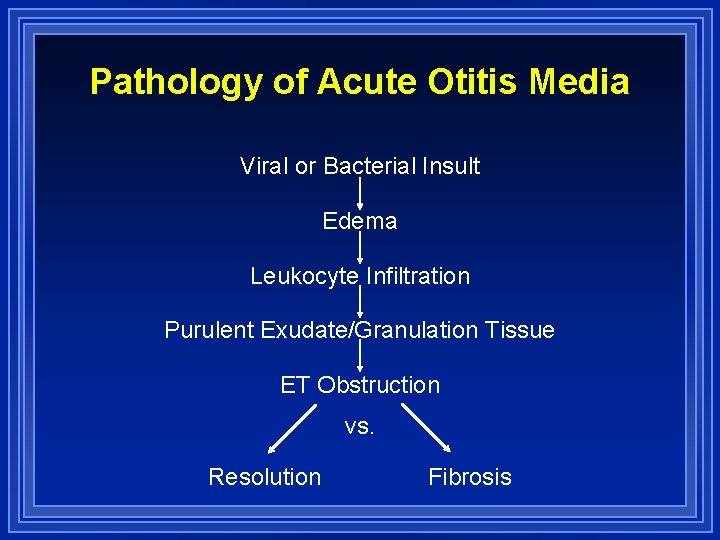
Pathology of Acute Otitis Media Viral or Bacterial Insult Edema Leukocyte Infiltration Purulent Exudate/Granulation Tissue ET Obstruction vs. Resolution Fibrosis
Pathogenesis of Otitis Media l Infection (viral vs. bacterial) l Abnormal eustachian tube function l Allergy (minor role) l Neoplasm (nasopharyngeal carcinoma) l Sinusitis

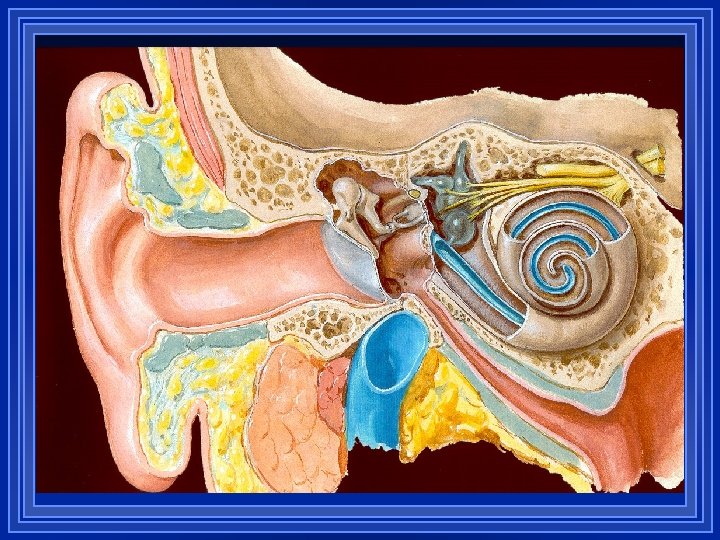
Eustachian Tube Function l Protection from nasopharyngeal secretions l Ventilation l Clearance of middle ear secretions
Otitis Media Classification l Classified according to: – Duration of disease Acute, subacute, chronic – Quality of effusion Serous, mucoid, purulent – Tympanic membrane appearance
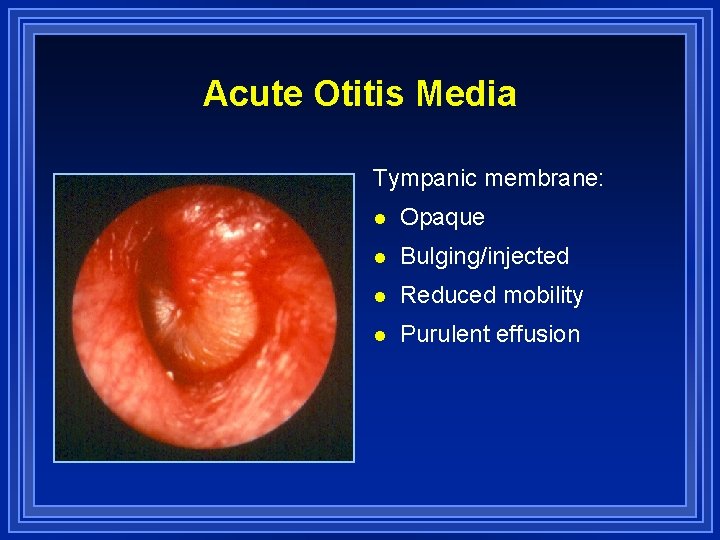
Acute Otitis Media Tympanic membrane: l Opaque l Bulging/injected l Reduced mobility l Purulent effusion

Otitis Media with Effusion Tympanic membrane: l Translucent or opaque l Gray/pink l Reduced mobility l Effusion present +/- air

Chronic Mucoid OM (Glue Ear) Tympanic membrane: l Opaque/gray l Retracted, reduced mobility l Thick effusion, no air l Hearing loss (>20 d. B HL)
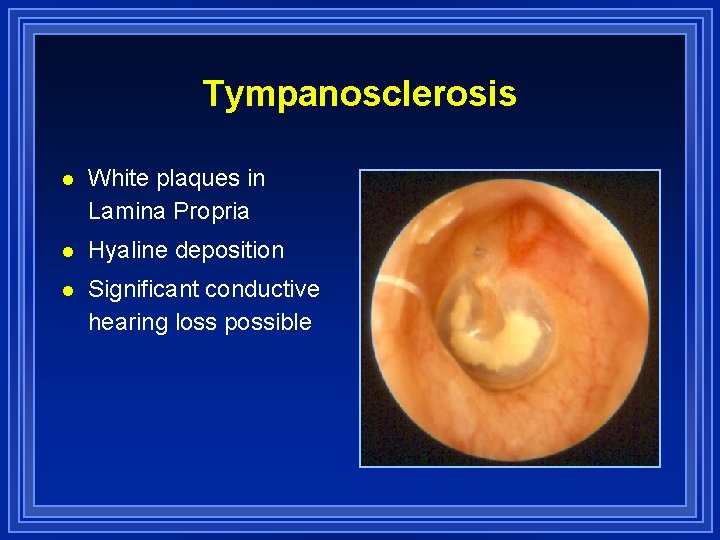
Tympanosclerosis l White plaques in Lamina Propria l Hyaline deposition l Significant conductive hearing loss possible
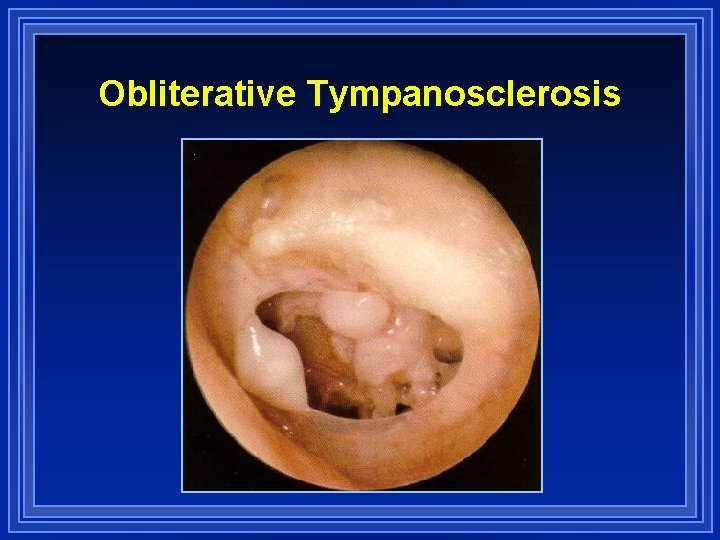
Obliterative Tympanosclerosis

Atelectasis l Collapse or retraction of tympanic membrane l Often associated with ossicular pathology l Long-standing eustachian tube dysfunction
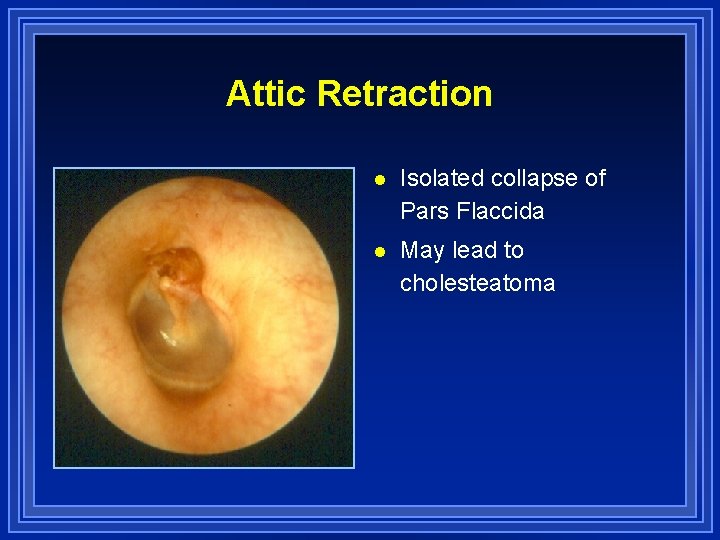
Attic Retraction l Isolated collapse of Pars Flaccida l May lead to cholesteatoma
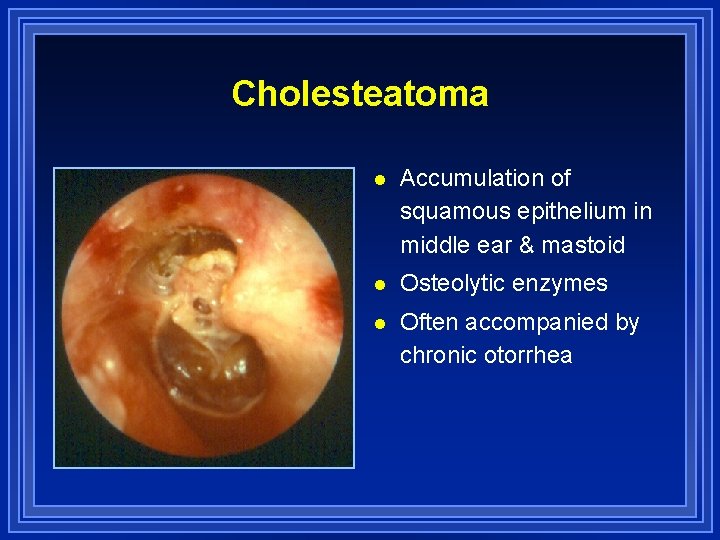
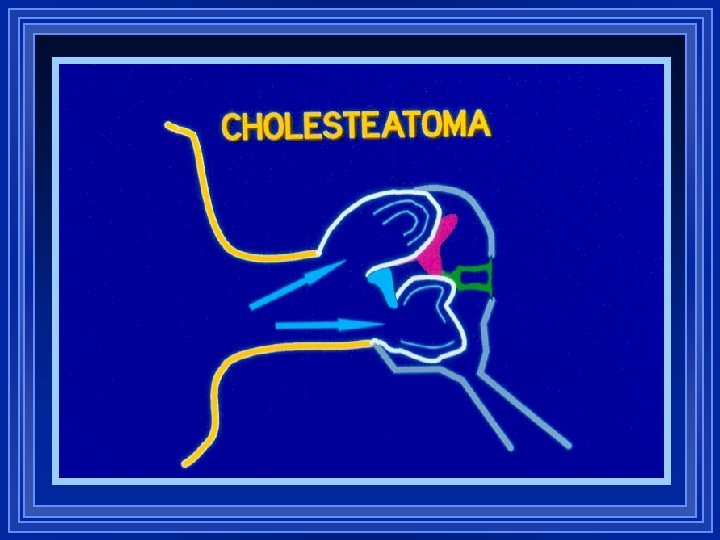
Cholesteatoma l Accumulation of squamous epithelium in middle ear & mastoid l Osteolytic enzymes l Often accompanied by chronic otorrhea
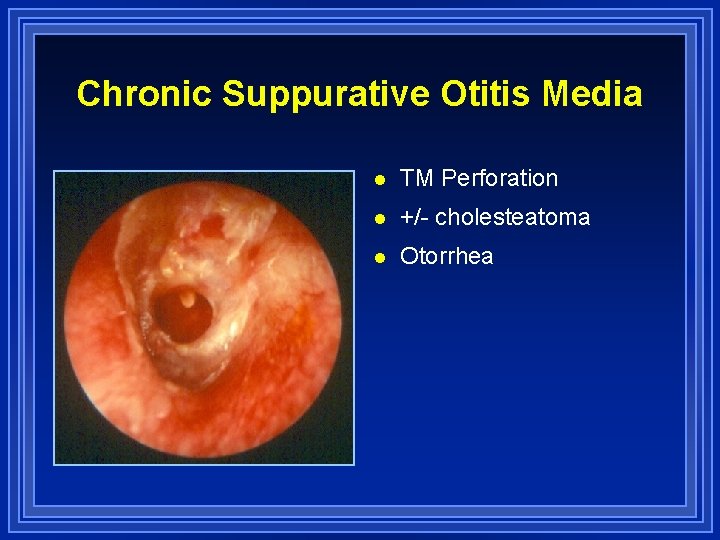
Chronic Suppurative Otitis Media l TM Perforation l +/- cholesteatoma l Otorrhea
Diagnosis of Otitis Media
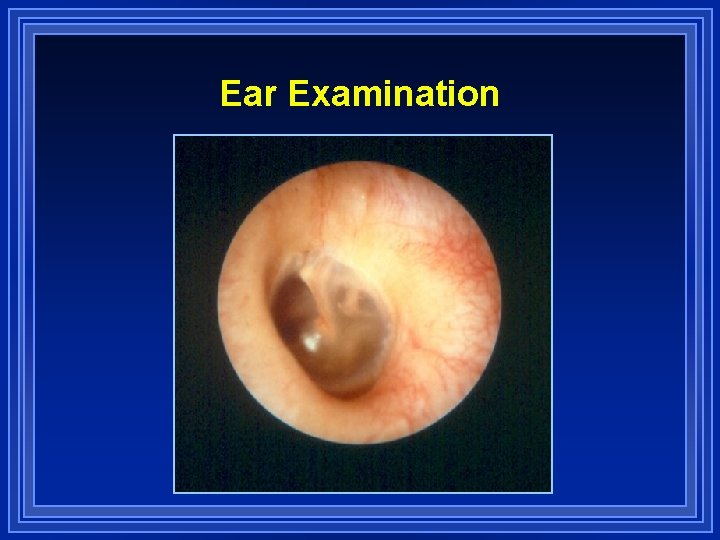
Ear Examination
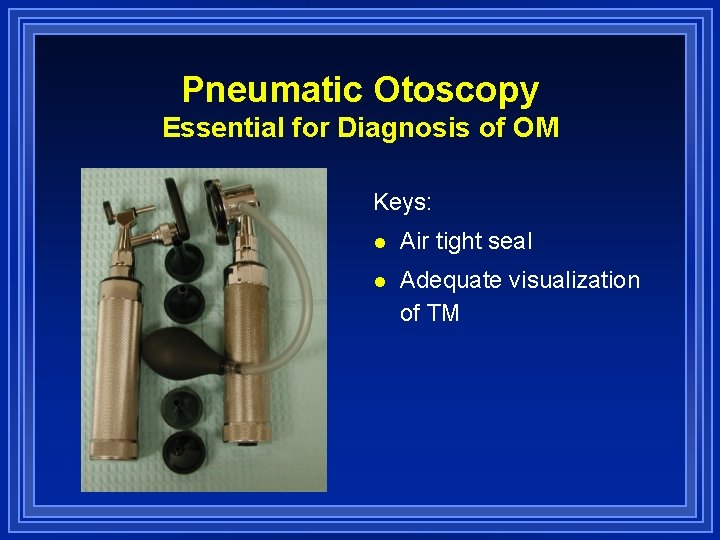
Pneumatic Otoscopy Essential for Diagnosis of OM Keys: l Air tight seal l Adequate visualization of TM
Instrumentation
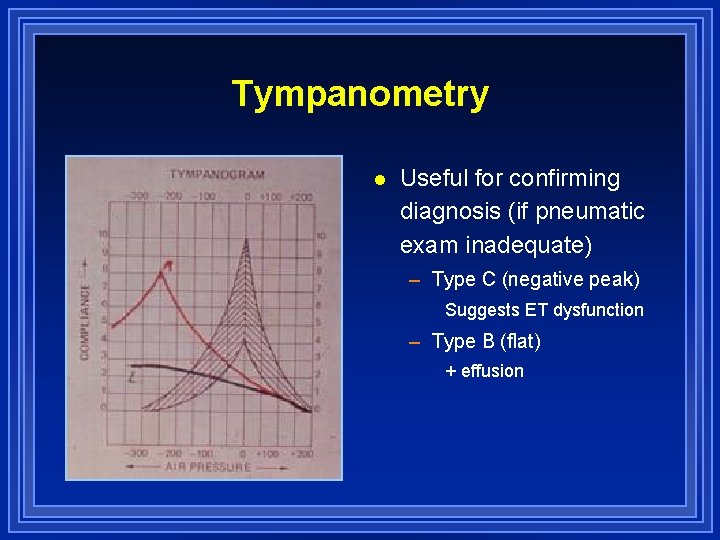
Tympanometry l Useful for confirming diagnosis (if pneumatic exam inadequate) – Type C (negative peak) Suggests ET dysfunction – Type B (flat) + effusion
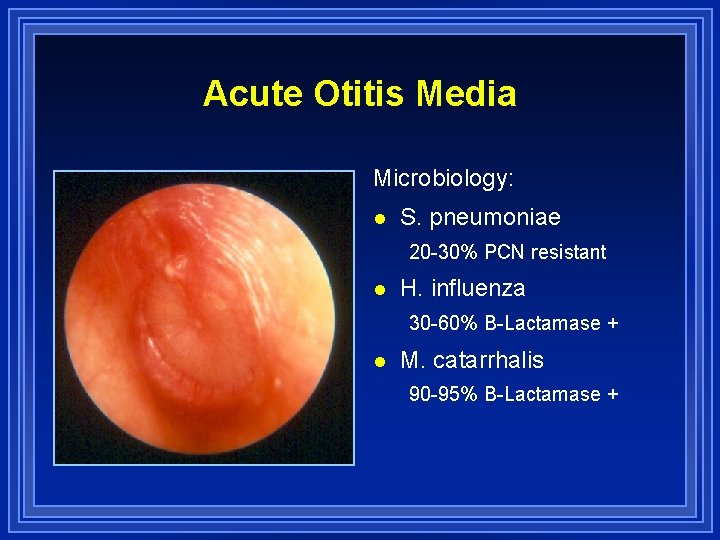
Acute Otitis Media Microbiology: l S. pneumoniae 20 -30% PCN resistant l H. influenza 30 -60% B-Lactamase + l M. catarrhalis 90 -95% B-Lactamase +
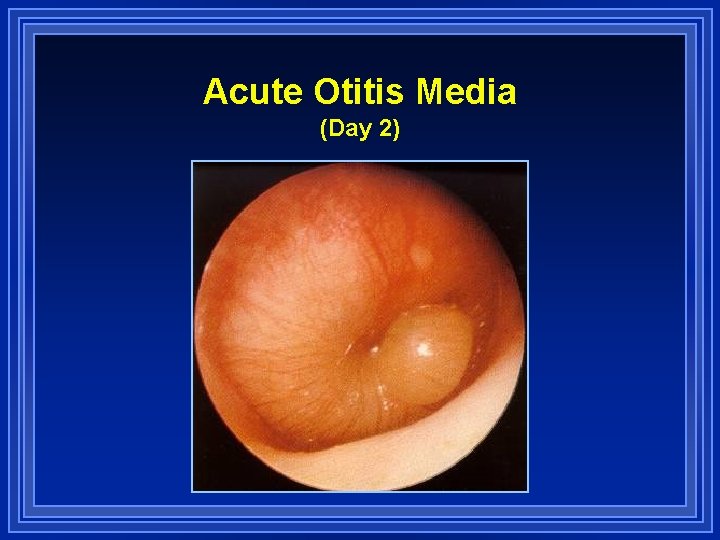
Acute Otitis Media (Day 2)
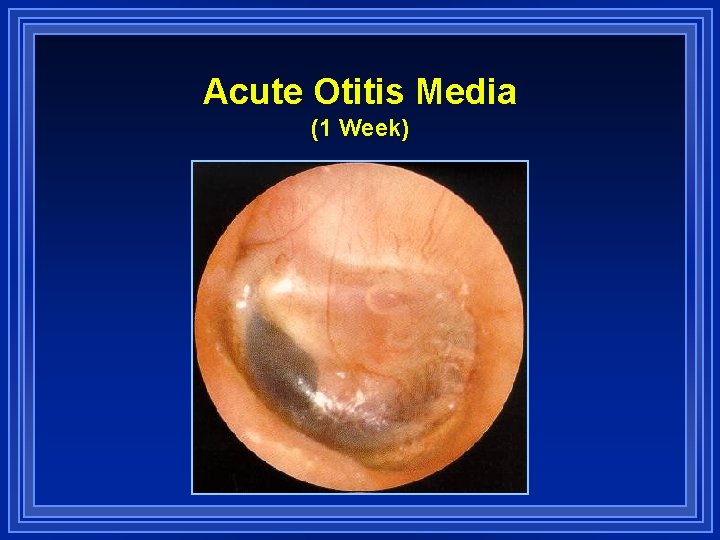
Acute Otitis Media (1 Week)
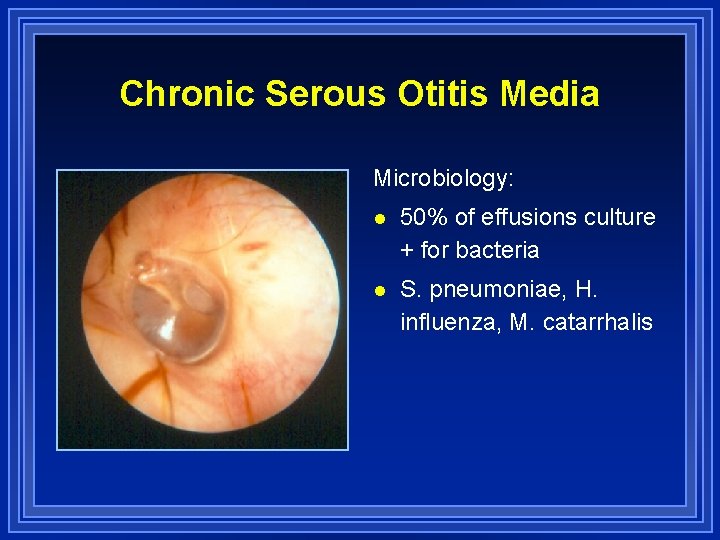
Chronic Serous Otitis Media Microbiology: l 50% of effusions culture + for bacteria l S. pneumoniae, H. influenza, M. catarrhalis
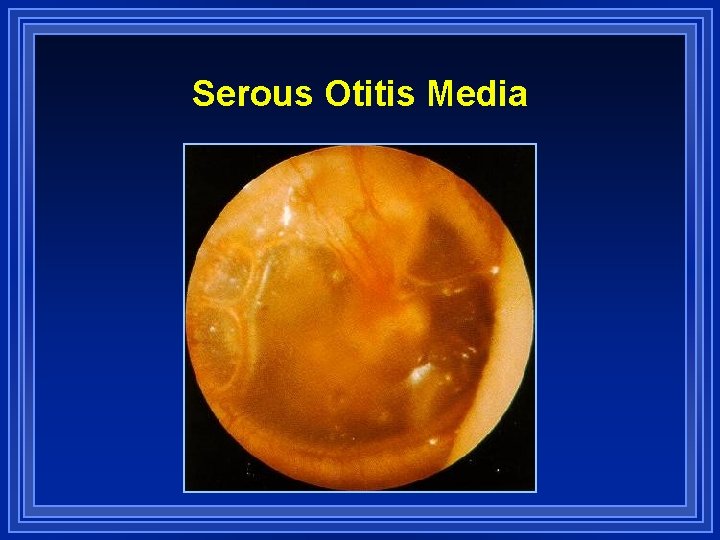
Serous Otitis Media

Chronic Suppurative Otitis Media Microbiology: l P. aeruginosa l S. aureus l Diphtheroids l Klebsiella
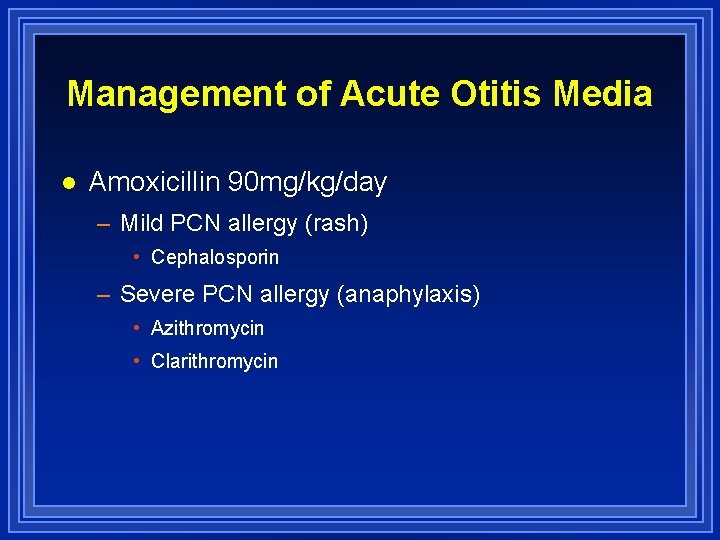
Management of Acute Otitis Media l Amoxicillin 90 mg/kg/day – Mild PCN allergy (rash) • Cephalosporin – Severe PCN allergy (anaphylaxis) • Azithromycin • Clarithromycin
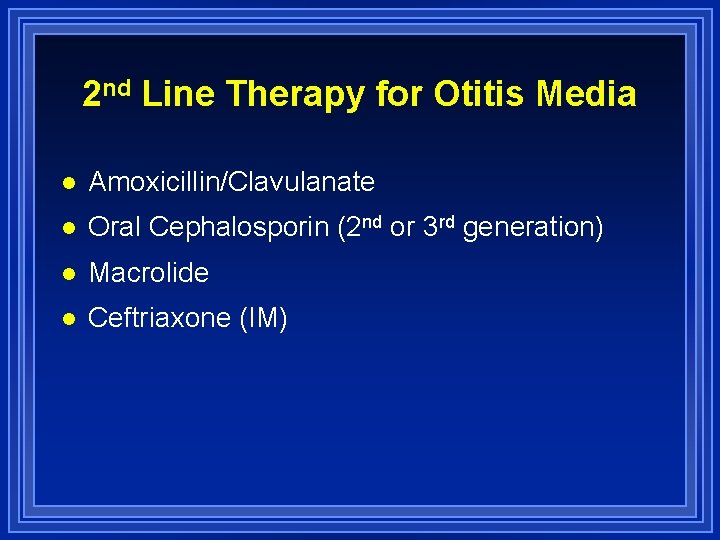
2 nd Line Therapy for Otitis Media l Amoxicillin/Clavulanate l Oral Cephalosporin (2 nd or 3 rd generation) l Macrolide l Ceftriaxone (IM)
When to Consider 2 nd Line Rx l Group day care l Antibiotic Rx within last 30 days l Failure of antibiotic prophylaxis l Refractory AOM Failure to improve with 72 hours
Management of Persistent OM l Watchful waiting 90% of effusions will resolve within 3 months l Additional 2 nd line antibiotics l Intranasal steroids l Eustachian tube inflation Valsalva vs. Otovent l Nasal endoscopy
Factors to Consider with Long-standing Effusions l Degree of hearing loss (>20 d. B HL) l Vertigo/imbalance l Tympanic membrane changes (retraction) l Speech & language delay l Behavioral changes l Frequency & severity of AOM
Plan of Therapy Amoxil
Plan of Therapy Amoxil If No Improvement in 72 hrs.
Plan of Therapy Amoxil If No Improvement in 72 hrs. 2 nd Line Antibiotic
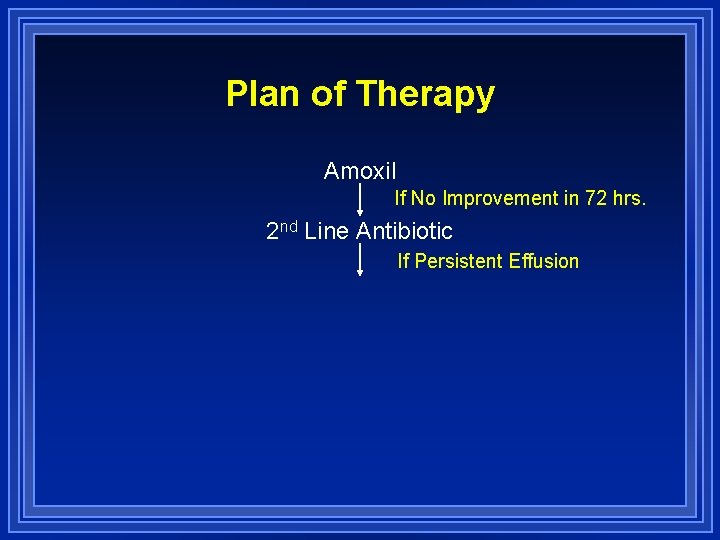
Plan of Therapy Amoxil If No Improvement in 72 hrs. 2 nd Line Antibiotic If Persistent Effusion
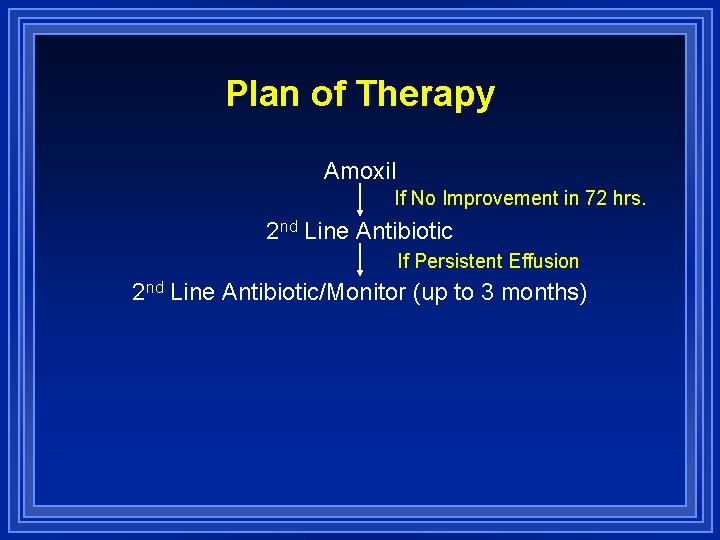
Plan of Therapy Amoxil If No Improvement in 72 hrs. 2 nd Line Antibiotic If Persistent Effusion 2 nd Line Antibiotic/Monitor (up to 3 months)
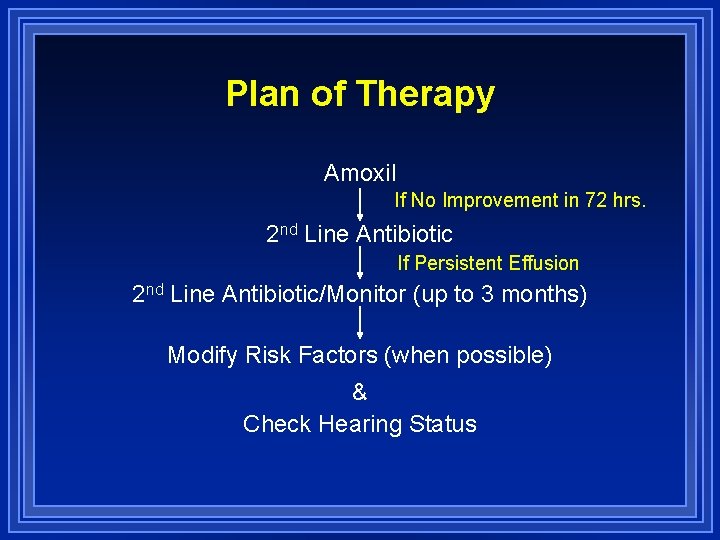
Plan of Therapy Amoxil If No Improvement in 72 hrs. 2 nd Line Antibiotic If Persistent Effusion 2 nd Line Antibiotic/Monitor (up to 3 months) Modify Risk Factors (when possible) & Check Hearing Status
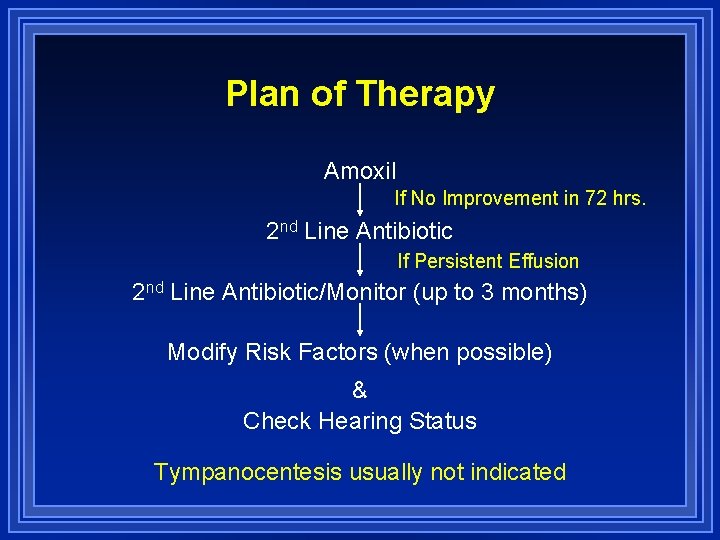
Plan of Therapy Amoxil If No Improvement in 72 hrs. 2 nd Line Antibiotic If Persistent Effusion 2 nd Line Antibiotic/Monitor (up to 3 months) Modify Risk Factors (when possible) & Check Hearing Status Tympanocentesis usually not indicated
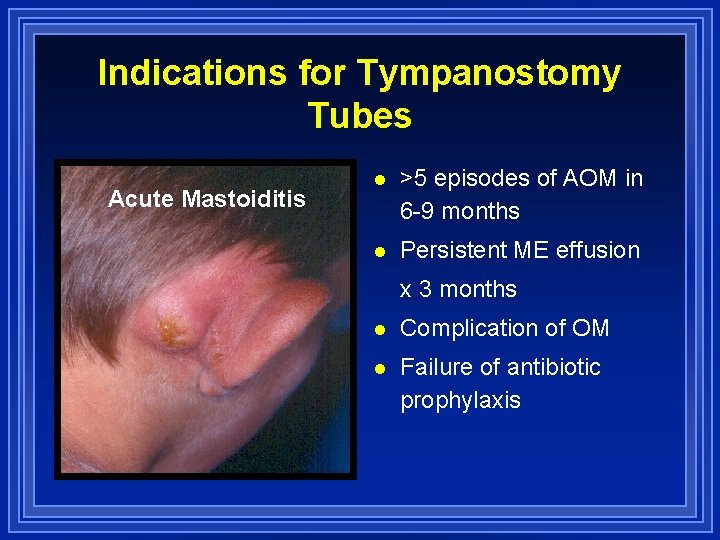
Indications for Tympanostomy Tubes Acute Mastoiditis l >5 episodes of AOM in 6 -9 months l Persistent ME effusion x 3 months l Complication of OM l Failure of antibiotic prophylaxis
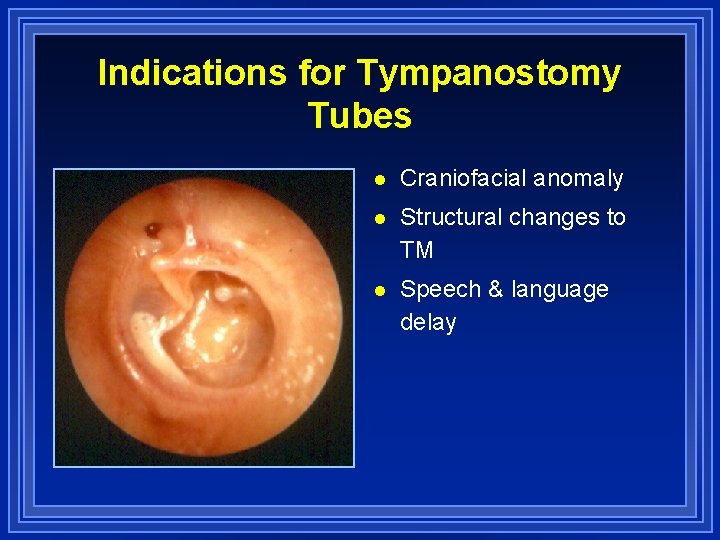
Indications for Tympanostomy Tubes l Craniofacial anomaly l Structural changes to TM l Speech & language delay
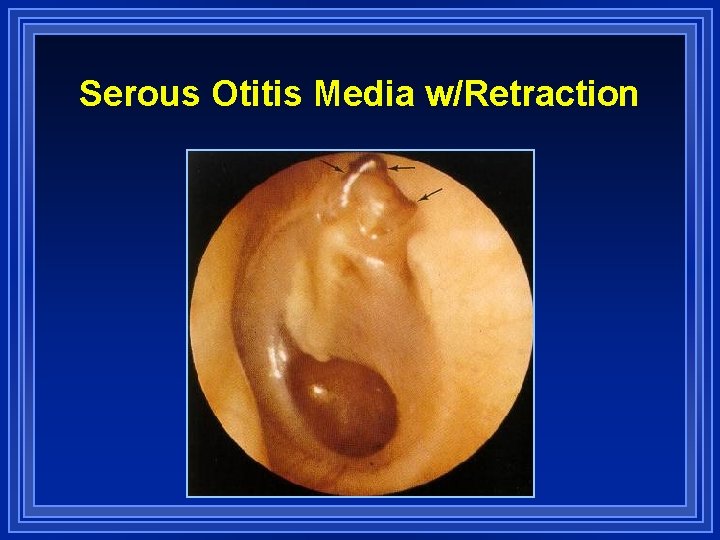
Serous Otitis Media w/Retraction
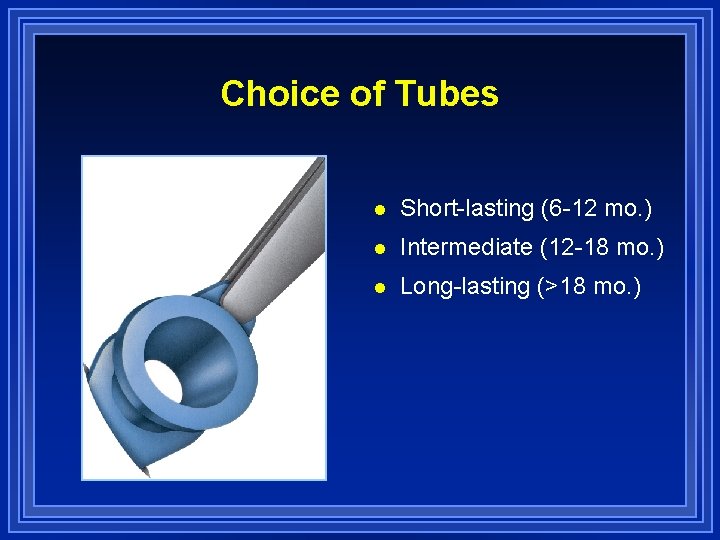
Choice of Tubes l Short-lasting (6 -12 mo. ) l Intermediate (12 -18 mo. ) l Long-lasting (>18 mo. )
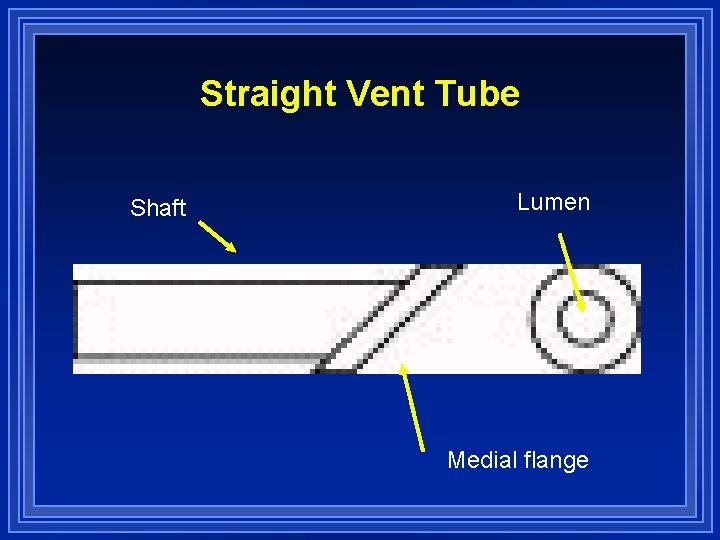
Straight Vent Tube Shaft Lumen Medial flange
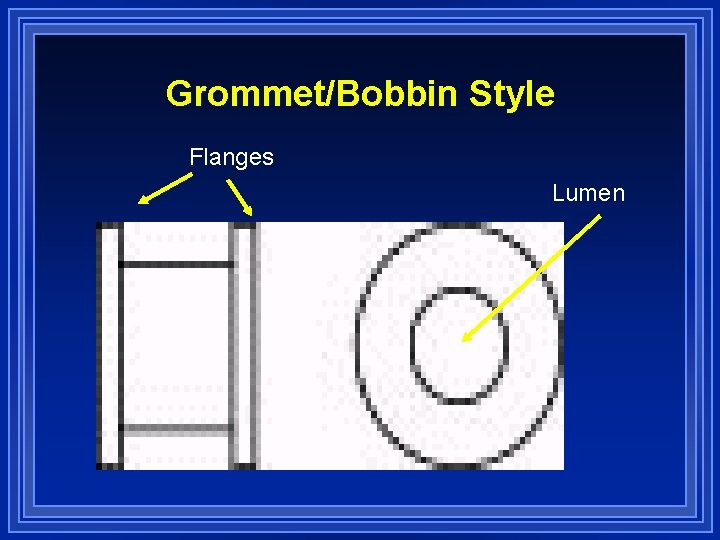
Grommet/Bobbin Style Flanges Lumen
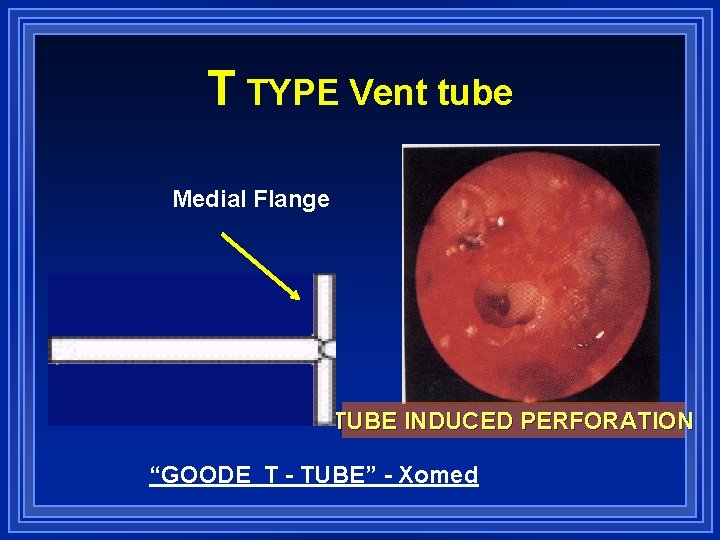
T TYPE Vent tube Medial Flange Shaft TUBE INDUCED PERFORATION “GOODE T - TUBE” - Xomed
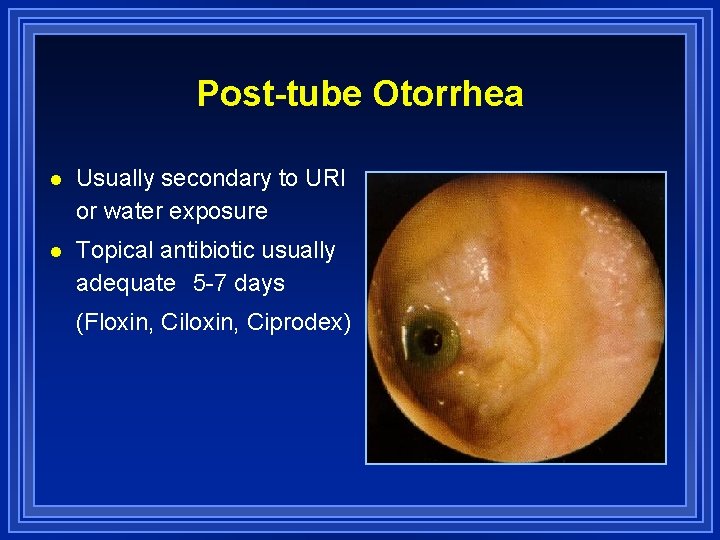
Post-tube Otorrhea l Usually secondary to URI or water exposure l Topical antibiotic usually adequate 5 -7 days (Floxin, Ciprodex)
Water Precautions l Cotton + Vaseline when bathing l Plug l Ear Band-It when swimming
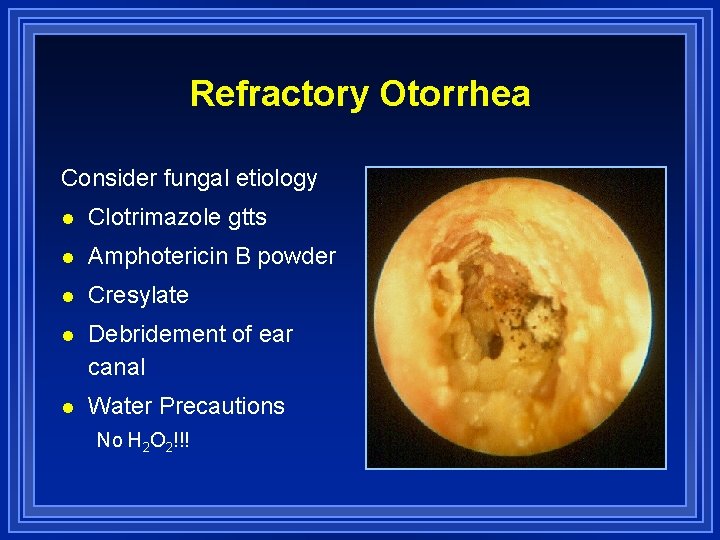
Refractory Otorrhea Consider fungal etiology l Clotrimazole gtts l Amphotericin B powder l Cresylate l Debridement of ear canal l Water Precautions No H 2 O 2!!!
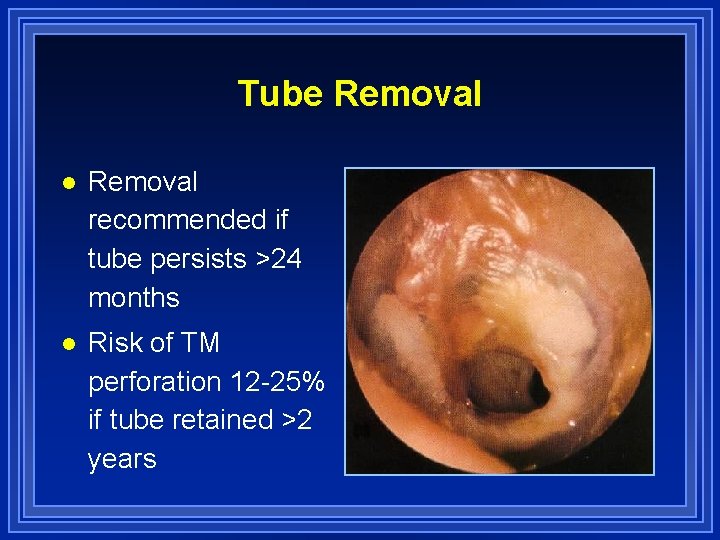
Tube Removal l Removal recommended if tube persists >24 months l Risk of TM perforation 12 -25% if tube retained >2 years
- Slides: 51