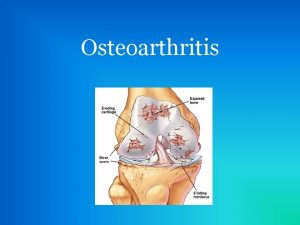
osteoarthritis Dr A Noori Rheumatologist www arrh ir










































- Slides: 126

osteoarthritis Dr. A. Noori Rheumatologist www, arrh. ir
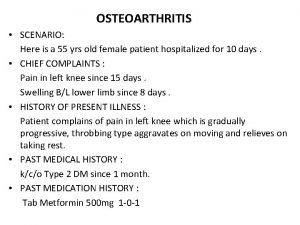
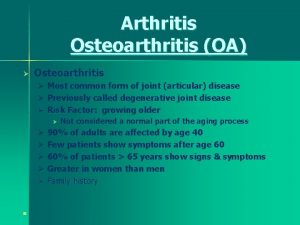
Introduction • Osteoarthritis is a common disorder of synovial joints. • Strongly age-related, being less common before 40 years, but rising in frequency with age, such that most people older than 70 years have radiological evidence of osteoarthritis in some joints.
Epidemiology • • • Most common joint disease in human Most frequent rheumatic compliant Common cause of disability in elderly Over 20 million affected in U. S. About 12% : age>60 y 6%: age>30 y
• Nodal OA involving DIP and PIP joints is more common in women and their first degree female relatives • OA of knee is more common in African American women
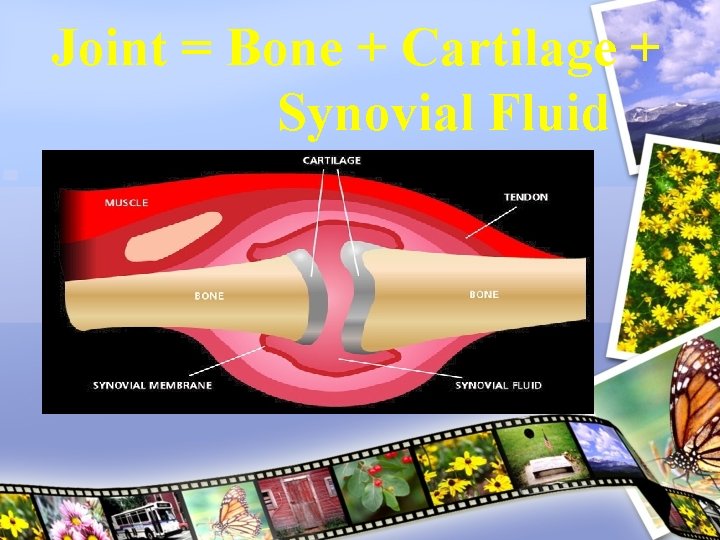
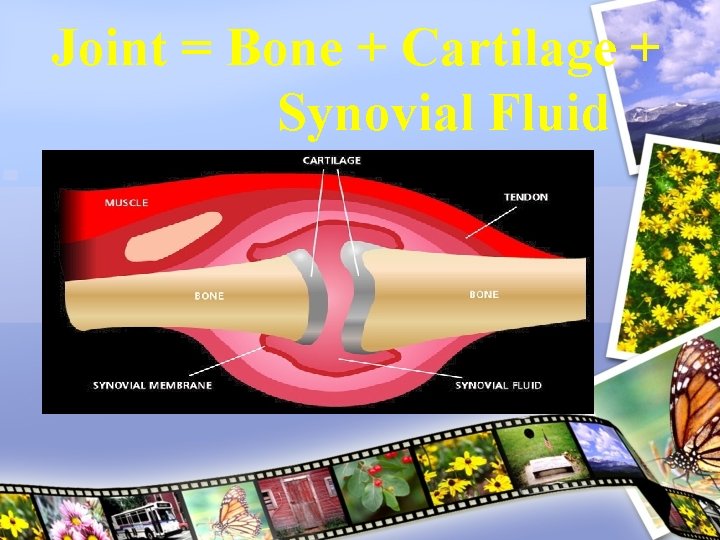
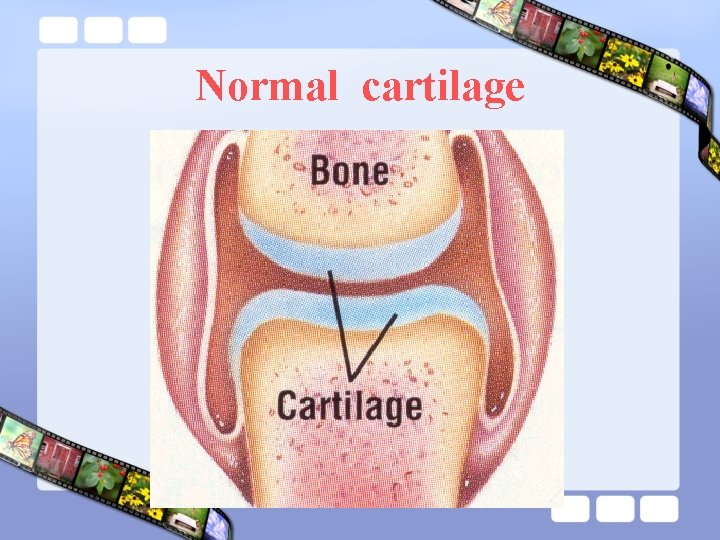
Joint = Bone + Cartilage + Synovial Fluid

Cartilage = Cushion
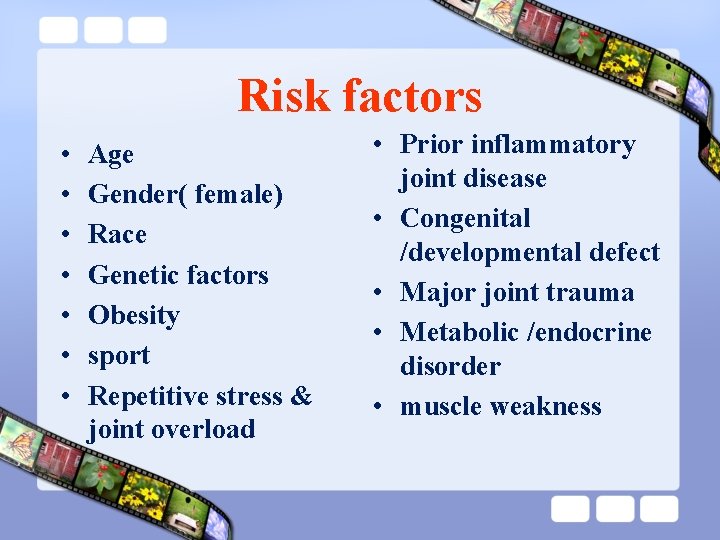
Risk factors • • Age Gender( female) Race Genetic factors Obesity sport Repetitive stress & joint overload • Prior inflammatory joint disease • Congenital /developmental defect • Major joint trauma • Metabolic /endocrine disorder • muscle weakness
Age • OA – Risk Factors Age is the strongest risk factor for OA. Although OA can start in young adulthood, if you are over 45 years old, you are at higher risk. Female gender • In general, arthritis occurs more frequently in women than in men. after age 45, OA is more common in women. OA of the hand is particularly common among women. Joint alignment • People with joints that move or fit together incorrectly, such as bow legs, a dislocated hip, or double-jointedness, are more likely to develop OA in those joints.
OA – Risk Factors Hereditary gene defect • A defect in one of the genes responsible for the cartilage component collagen cause deterioration of cartilage. Joint injury or overuse caused by physical labor or sports • Traumatic injury (ex. Ligament or meniscal tears) to the knee or hip increases your risk for developing OA in these joints. Joints that are used repeatedly in certain jobs may be more likely to develop OA because of injury or overuse. Obesity • Being overweight during midlife or the later years is among the strongest risk factors for OA of the knee.
Risk factors you cannot change • Family history of disease

Risk factors you cannot change • Family history of disease • Increasing age
Risk factors you cannot change • Family history of disease • Increasing age • Being female
Risk factors you can change • Overuse of the joint

Risk factors you can change • Overuse of the joint • Major injury
Strong Risk Factor for OA Obesity • 50% decrease in OA with 11# wt loss • Larger effect in women
Strong Risk Factor for OA Joint Trauma
Risk factors you can change • Overuse of the joint • Major injury • Overweight • Muscle weakness

Risk Factors Mechanical abnormalities
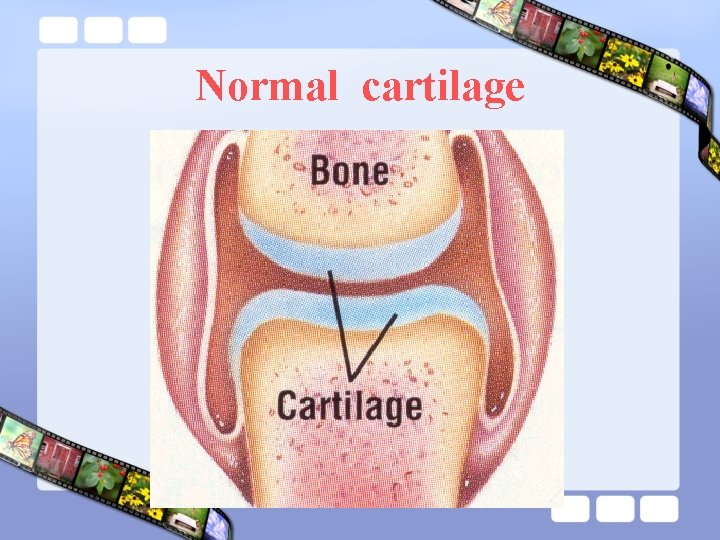
Normal cartilage
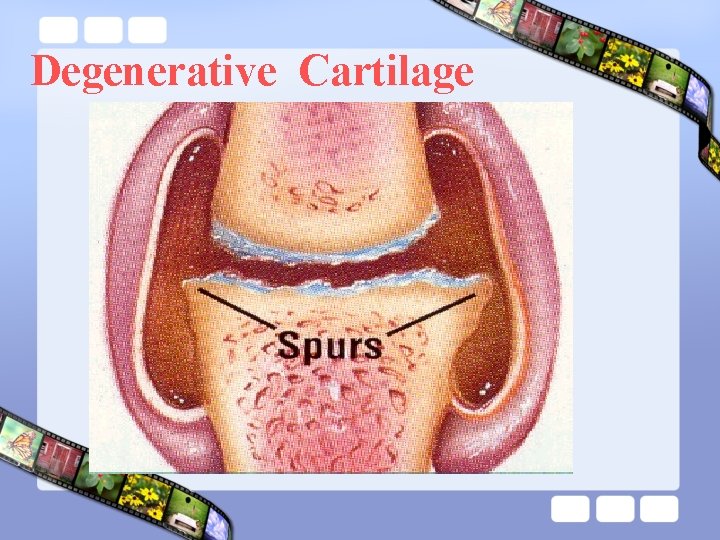
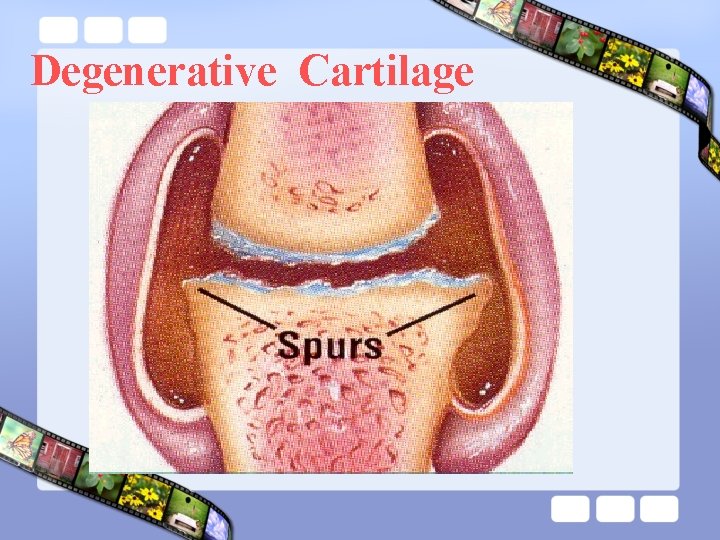
Degenerative Cartilage

Joint • EPIPHYSEAL BONE • CARTILAGE • SYNOVIAL MEMBRANE • CAPSULE • LIGAMENTS • MUSCLE & TENDONS • BURSAE
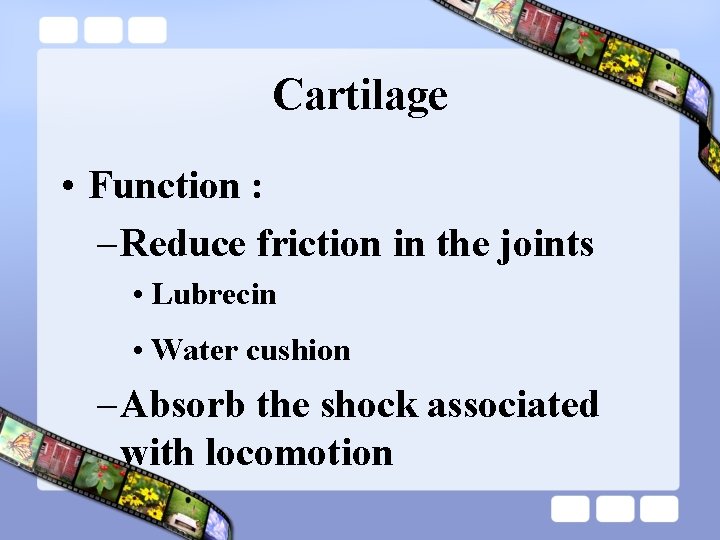
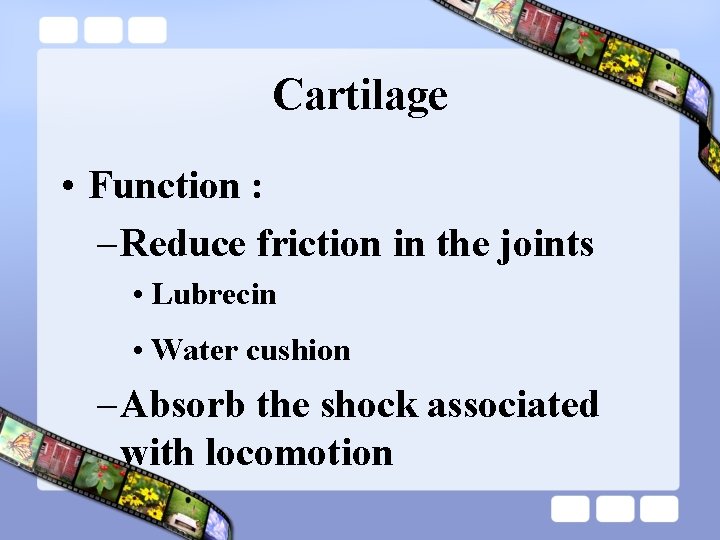
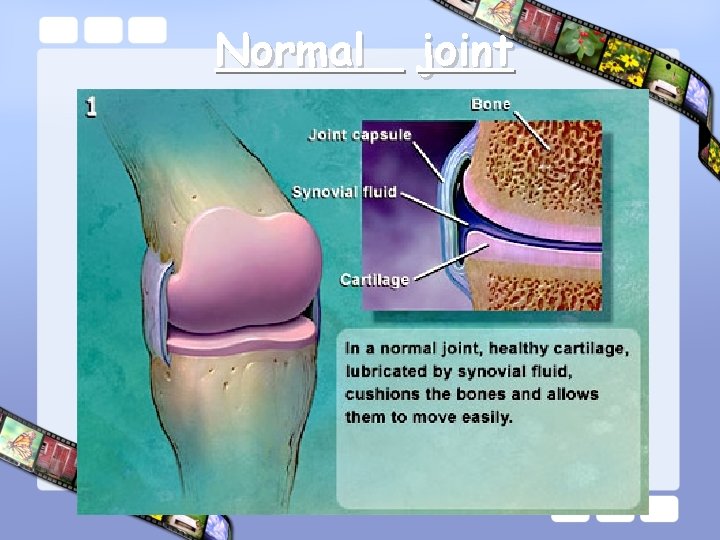
Cartilage • Function : – Reduce friction in the joints • Lubrecin • Water cushion – Absorb the shock associated with locomotion

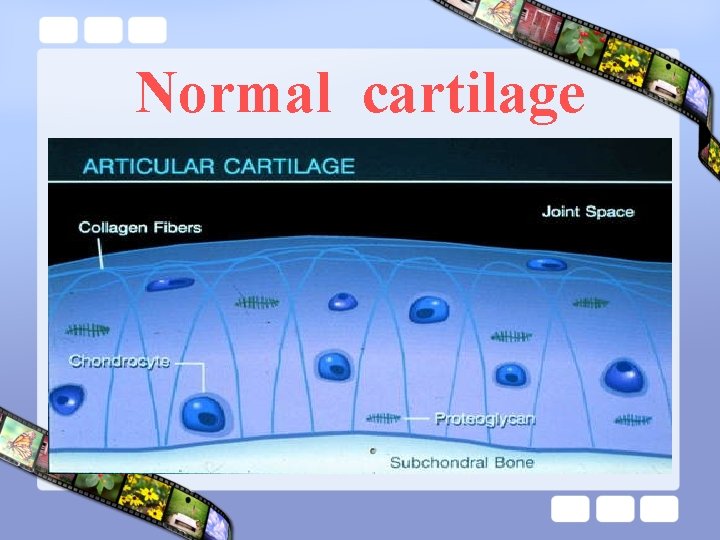
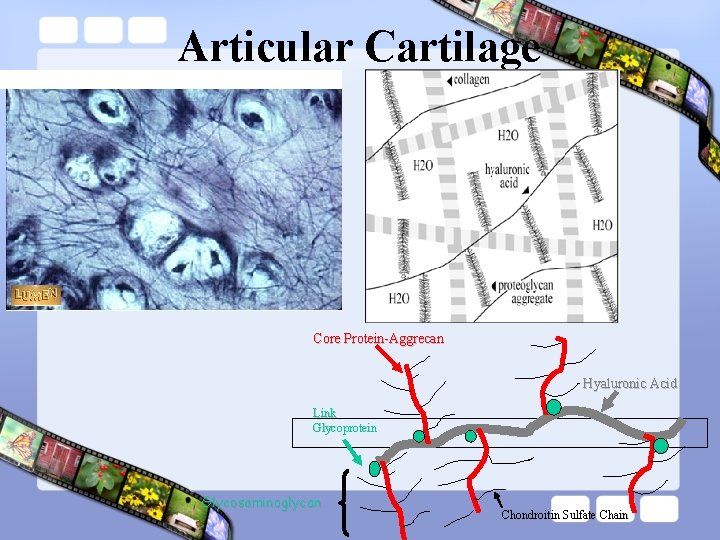
Cartilage • Consist of : – Water : 70% – Type II collagen – Proteoglycan : • Aggrecan Sub Unit – Core Protein – Glycosaminoglycans, Link Protein • Hyaluronic Acid – Chondrocyte
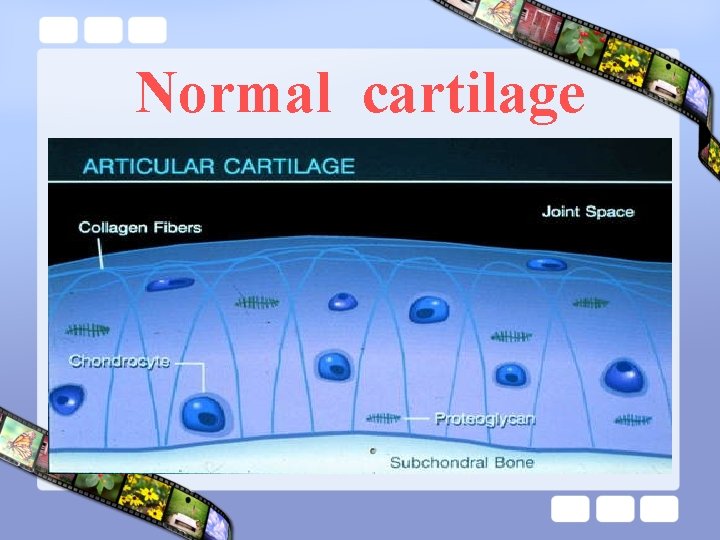
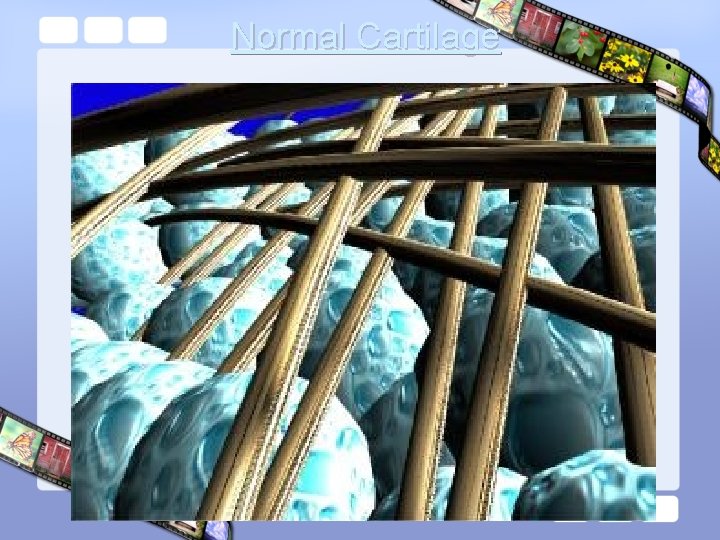
Normal cartilage
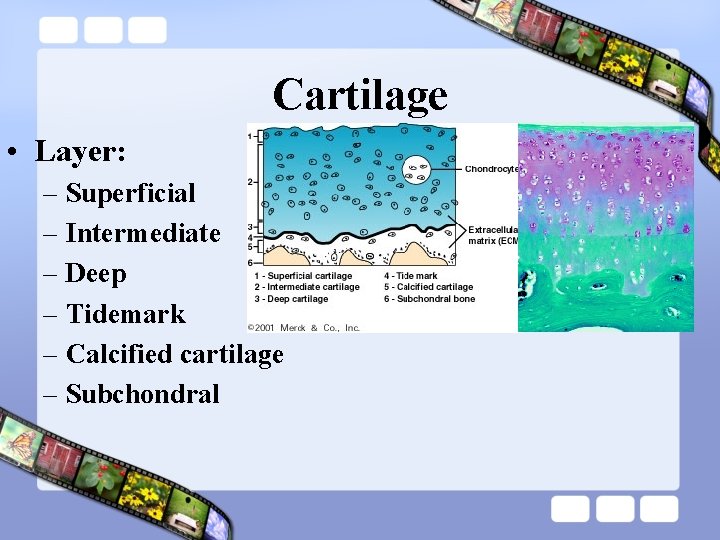
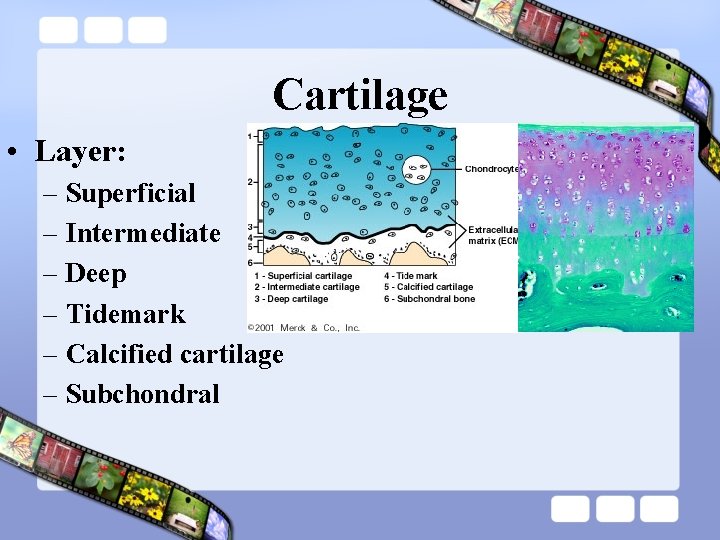
Cartilage • Layer: – Superficial – Intermediate – Deep – Tidemark – Calcified cartilage – Subchondral
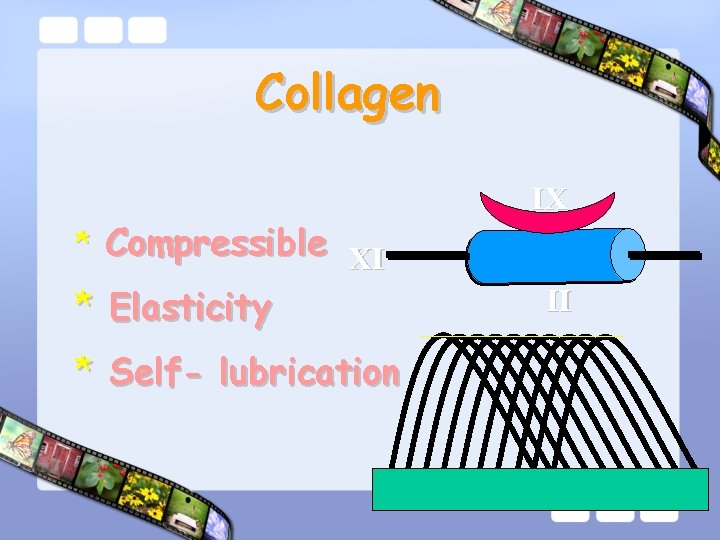
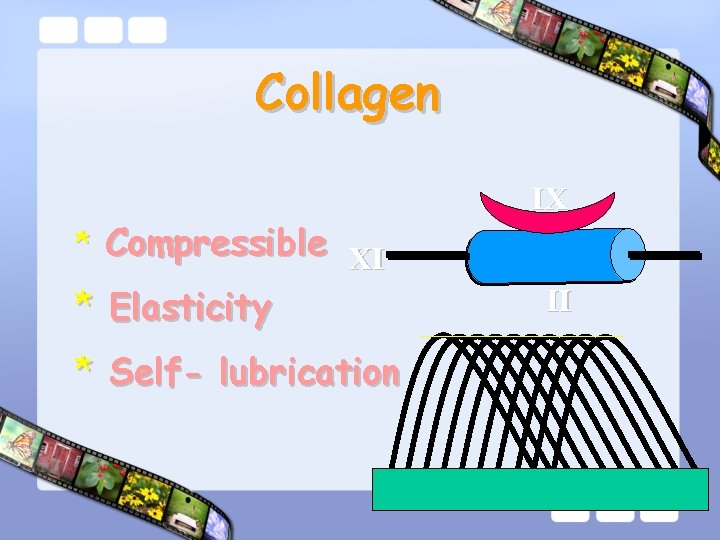
Collagen * Compressible XI * Elasticity * Self- lubrication IX II

Cartilage

Cartilage

Biomechanic of Joint
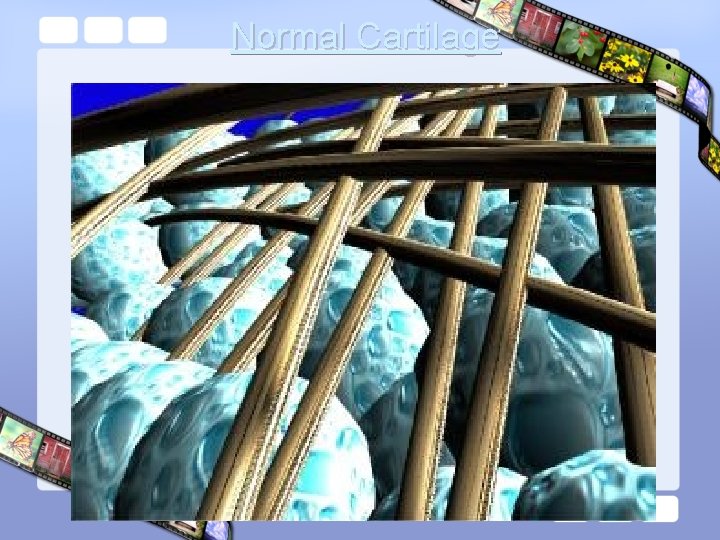
Normal Cartilage
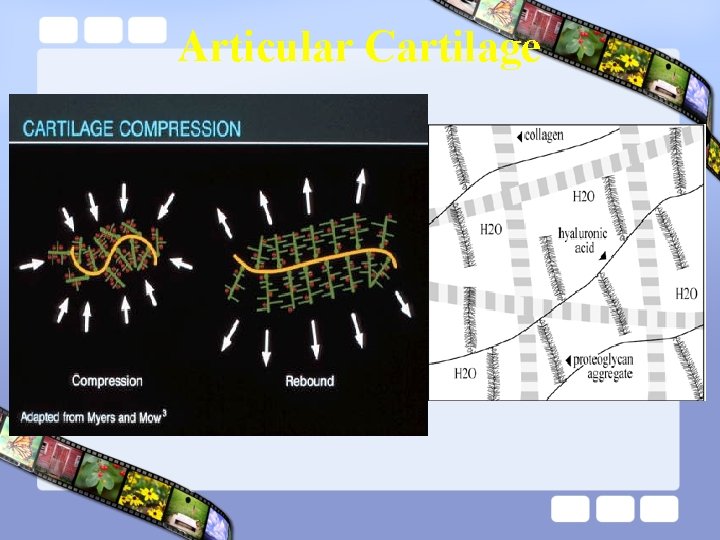
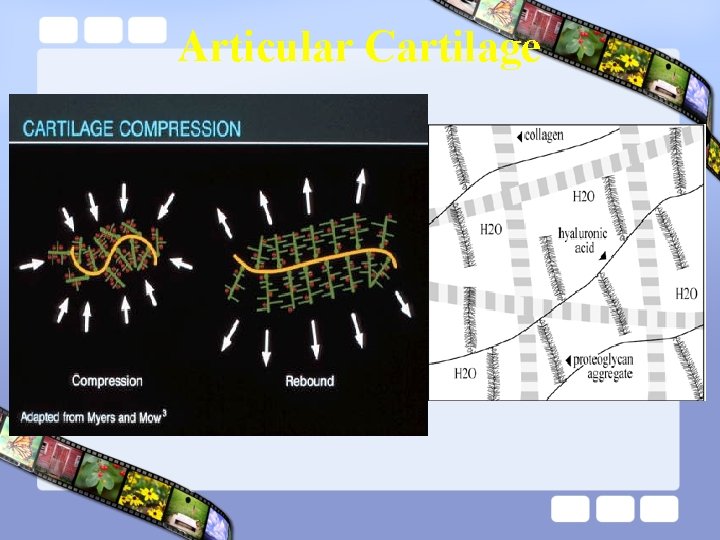
Articular Cartilage

Cartilage Layers

Cartilage metabolism • Cartilage is metabolically active – Synthesis matrix – Destruct matrix


Serine proteases Plasmine TPA factor Elastase Collagenases Proteinases Metloproteinases (MMP) Systeine proteases Gelatinases Stromelysines Catepsines
Cartilage remodeling Synthetic activities Degradative activities
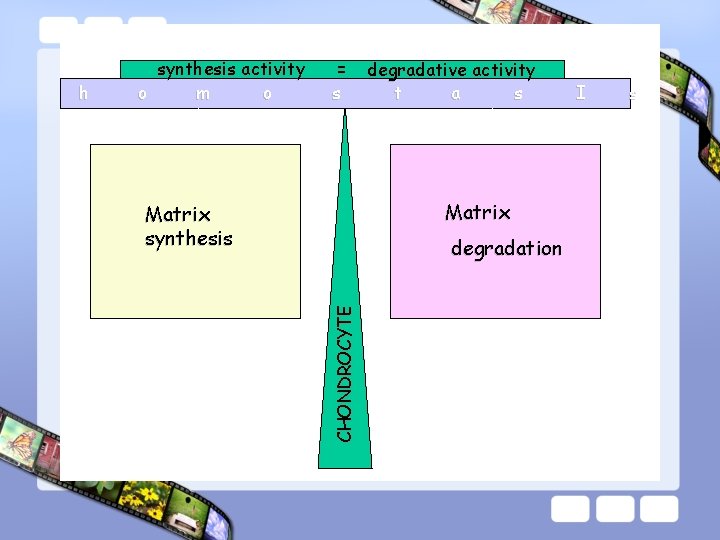
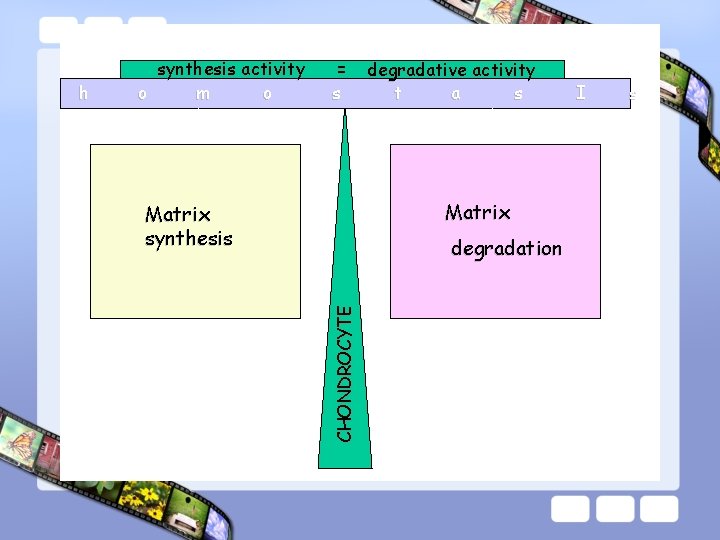
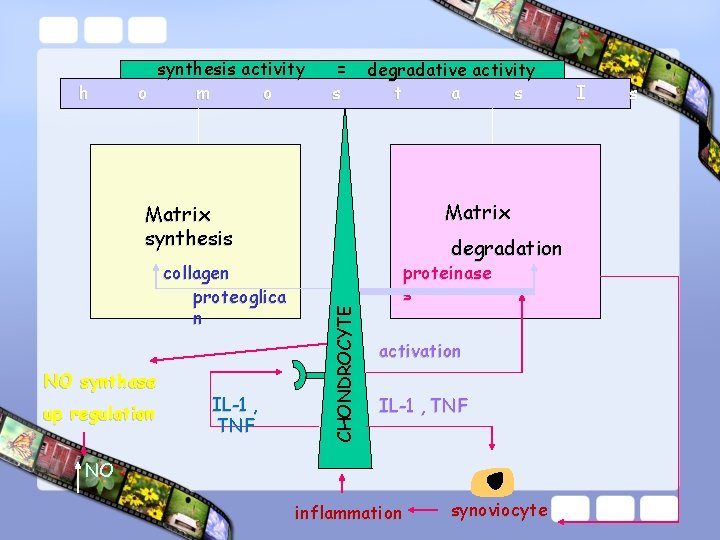
= s degradative activity t a s Matrix synthesis degradation CHONDROCYTE h synthesis activity o m o I s
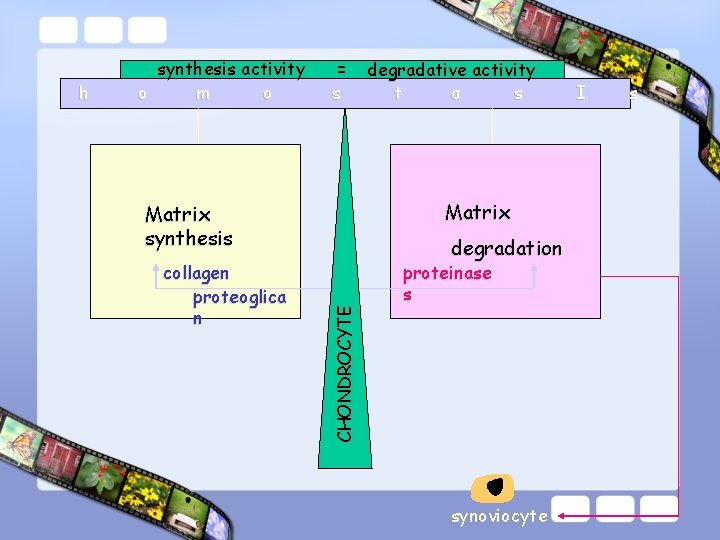
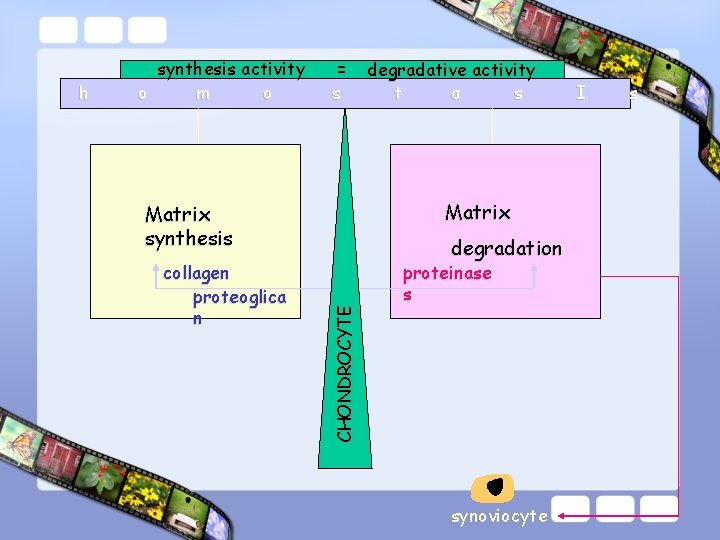
= s collagen proteoglica n degradative activity t a s Matrix synthesis degradation CHONDROCYTE h synthesis activity o m o proteinase s synoviocyte I s
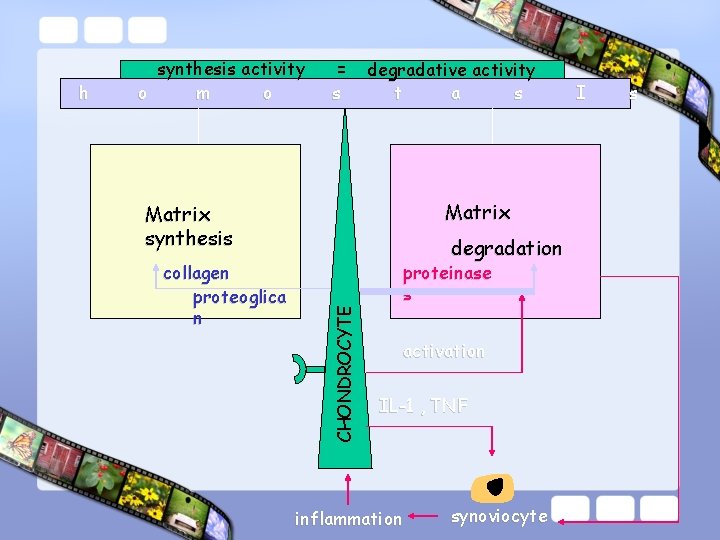
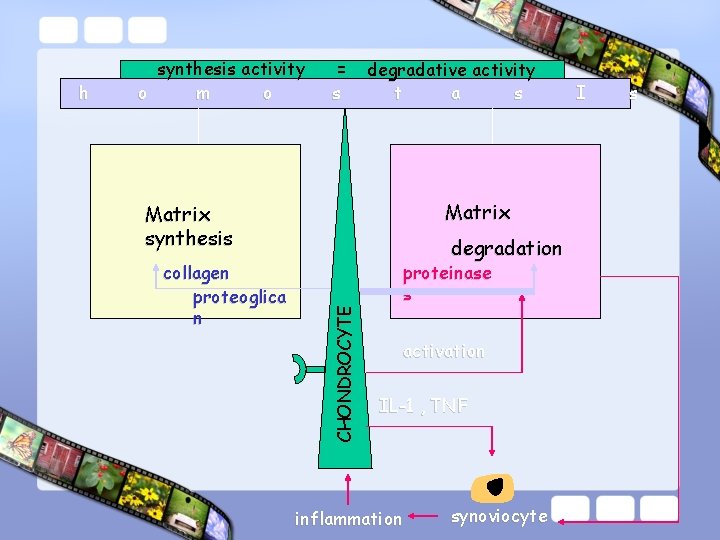
= s degradative activity t a s Matrix synthesis collagen proteoglica n degradation CHONDROCYTE h synthesis activity o m o proteinase s activation IL-1 , TNF inflammation synoviocyte I s
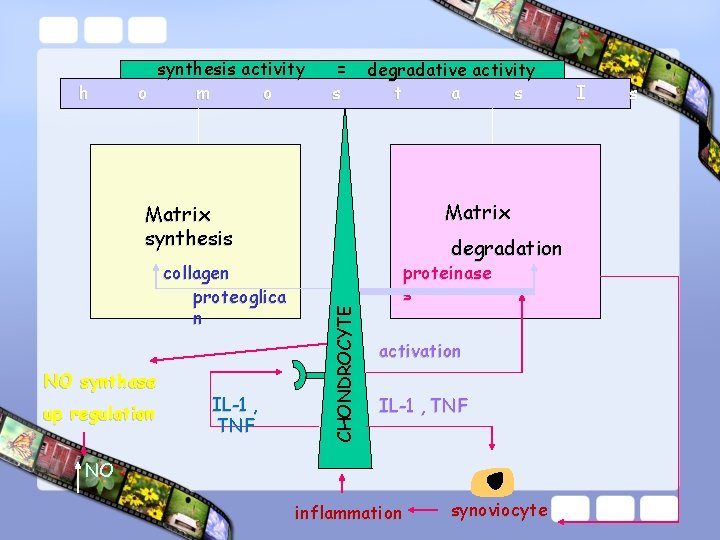
h synthesis activity o m o = s degradative activity t a s Matrix synthesis NO synthase up regulation IL-1 , TNF CHONDROCYTE collagen proteoglica n degradation proteinase s activation IL-1 , TNF NO inflammation synoviocyte I s

h synthesis activity o m o = s degradative activity t a s Matrix synthesis NO synthase Up regulation IL-1 , TNF CHONDROCYTE apoptosis collagen proteoglica n degradation proteinase s activation IL-1 , TNF NO inflammation synoviocyte I s
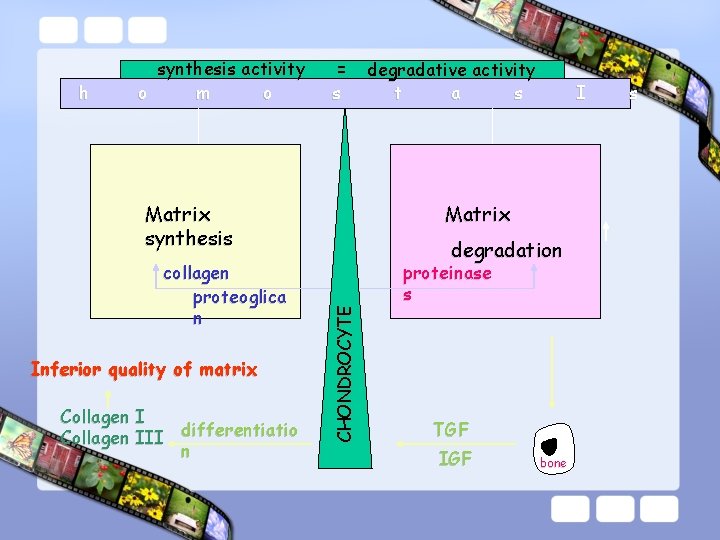
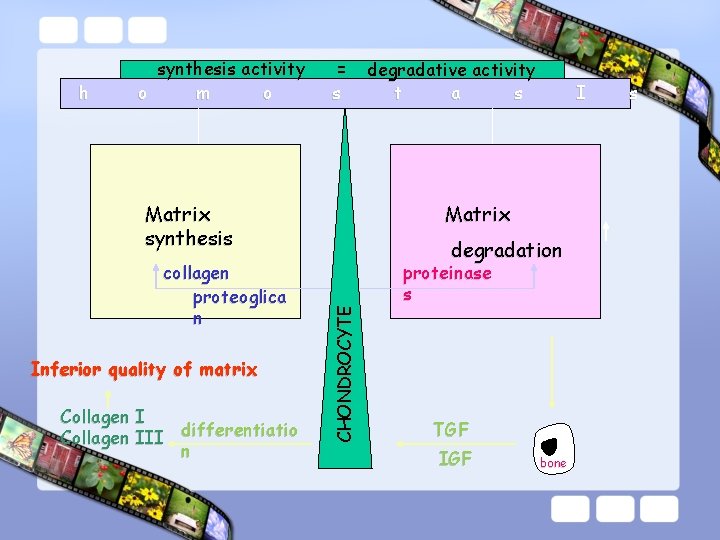
h synthesis activity o m o = s Matrix synthesis Inferior quality of matrix Collagen I differentiatio Collagen III n I Matrix degradation CHONDROCYTE collagen proteoglica n degradative activity t a s proteinase s TGF IGF bone s
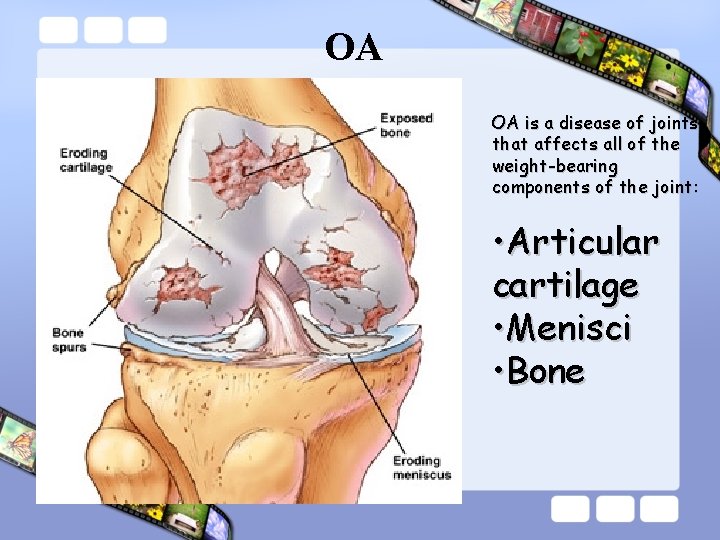
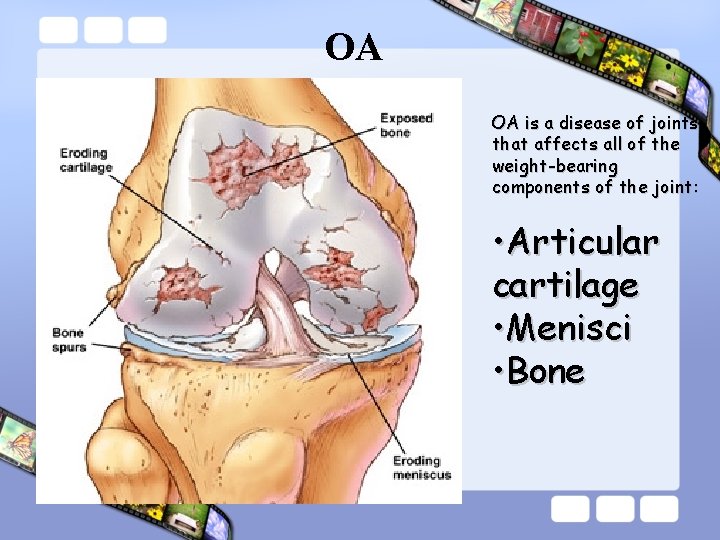
OA OA is a disease of joints that affects all of the weight-bearing components of the joint: • Articular cartilage • Menisci • Bone
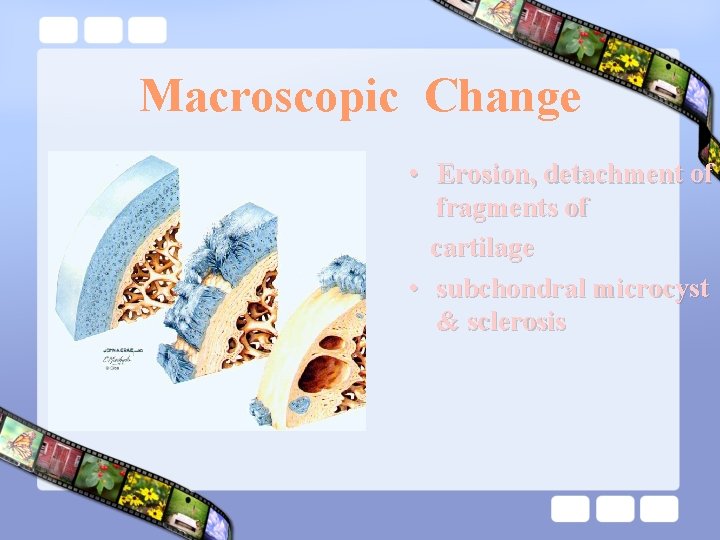
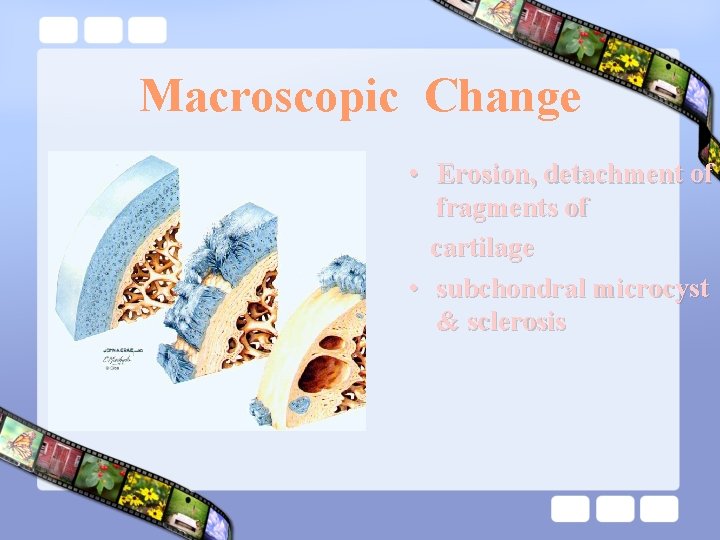
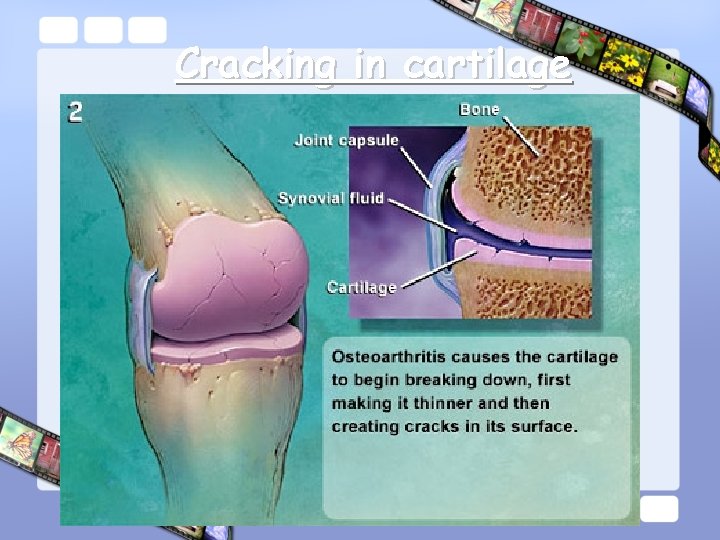
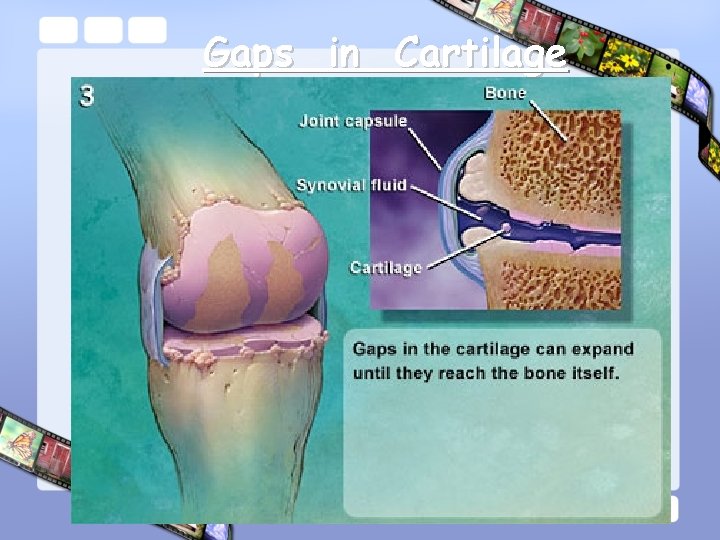
Macroscopic Change • Erosion, detachment of fragments of cartilage • subchondral microcyst & sclerosis
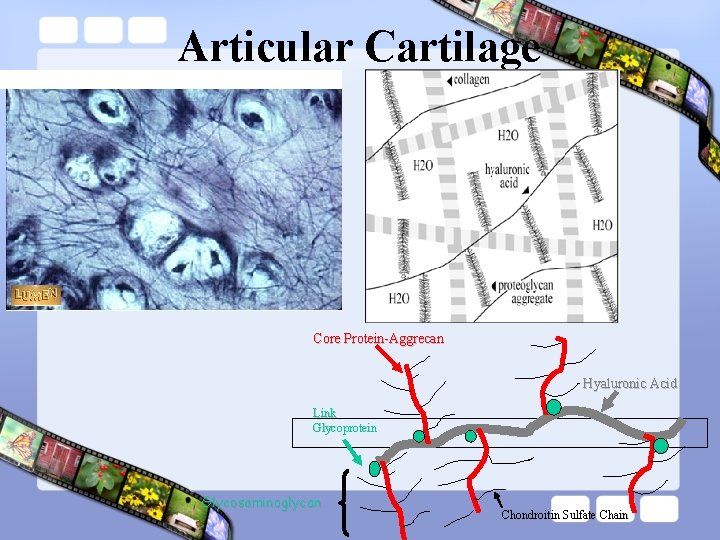
Articular Cartilage Core Protein-Aggrecan Hyaluronic Acid Link Glycoprotein Glycosaminoglycan Chondroitin Sulfate Chain
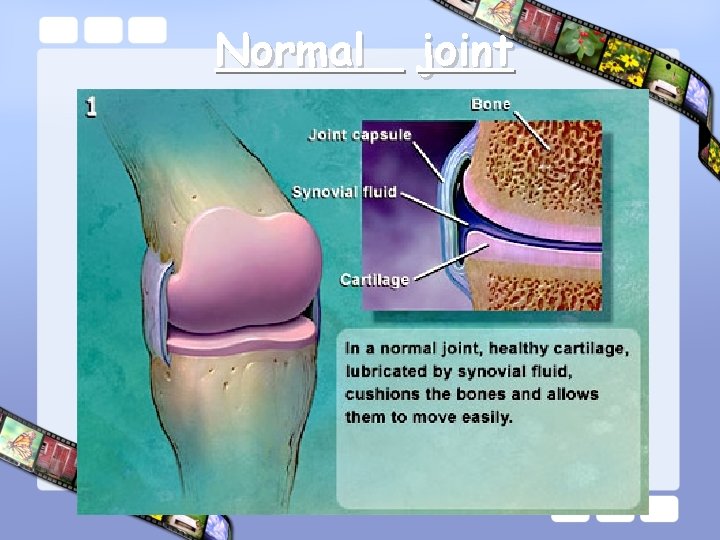
Normal joint
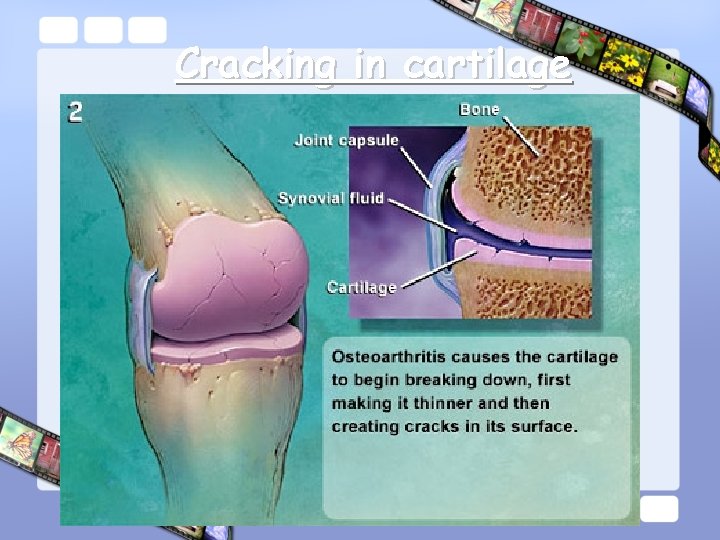
Cracking in cartilage
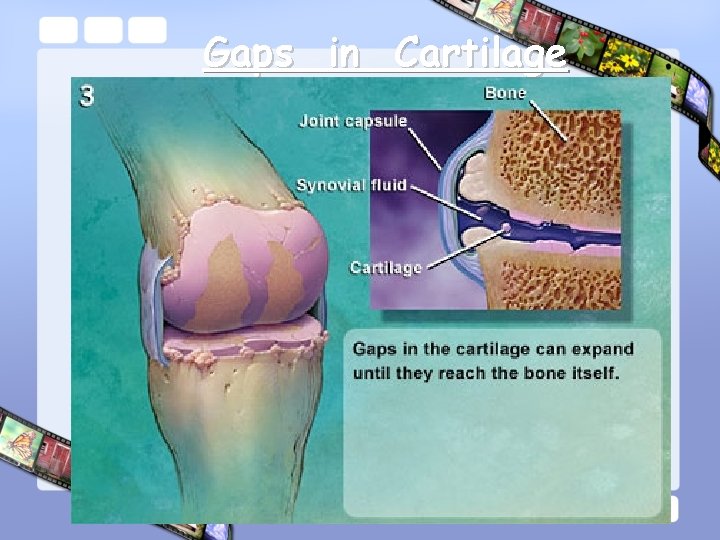
Gaps in Cartilage
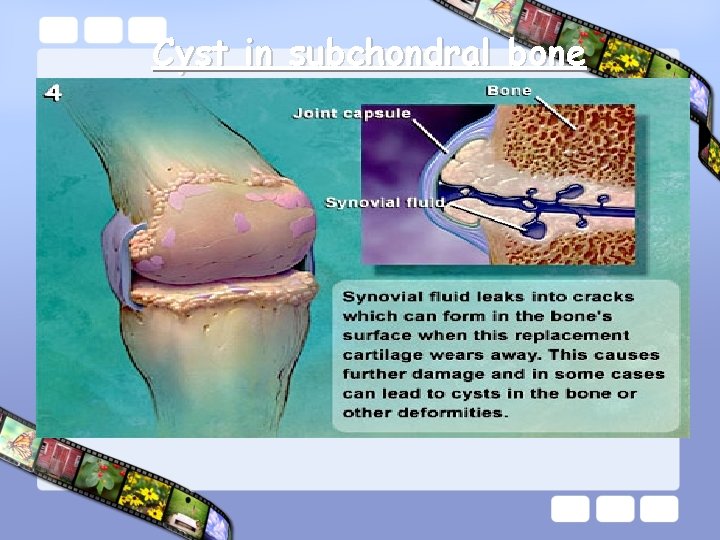
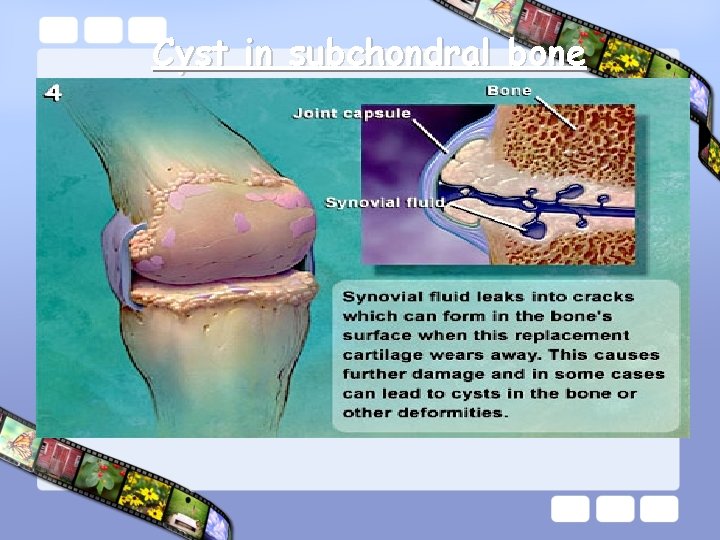
Cyst in subchondral bone
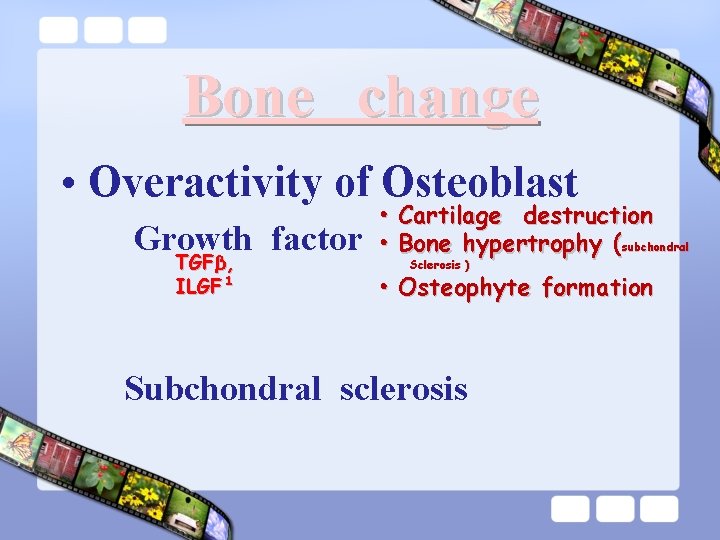
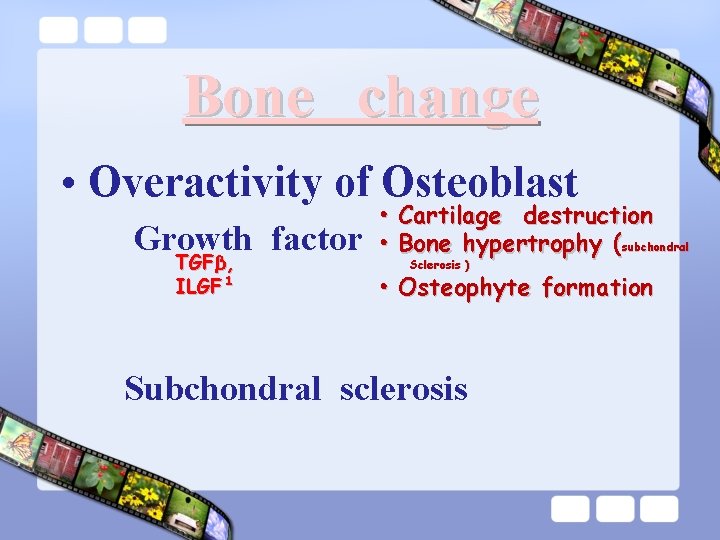
Bone change • Overactivity of Osteoblast Growth factor TGFβ, ILGF¹ • Cartilage destruction • Bone hypertrophy (subchondral Sclerosis ) • Osteophyte formation Subchondral sclerosis
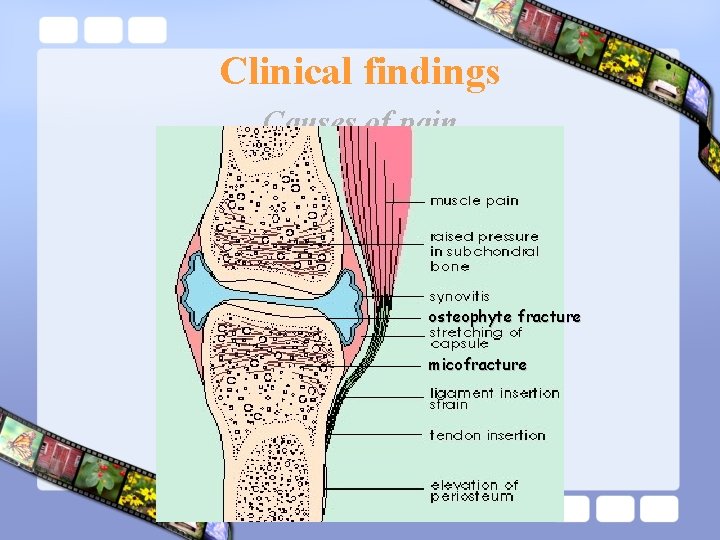
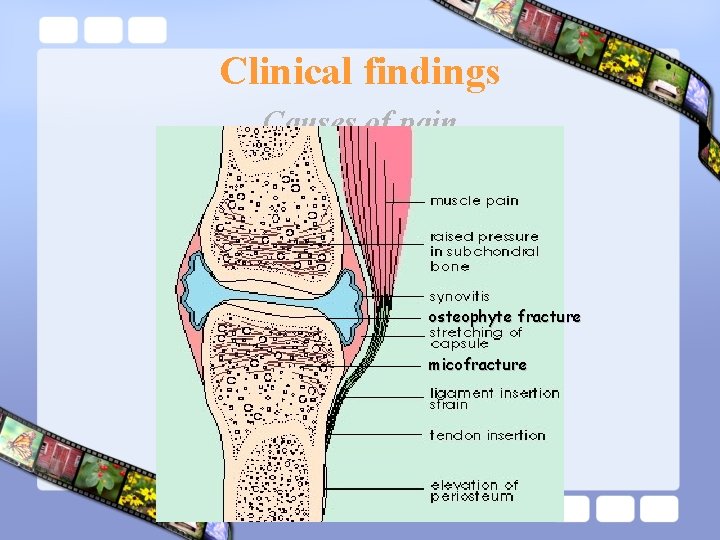
Clinical findings Causes of pain osteophyte fracture micofracture

C R R CLINICAL FEATURES Periosteal Capsule • Pain Subchondral • Mechanic • • • Inflammatory • Night pain Stiffness 5 -30 mi Joint swelling Synovitis Deformity Crepitus
Signs Of Osteoarthritis ♥ ♥ ♥ ♥ Bony enlargement Tenderness at joint margins Limitation of motion Periarticular muscle weakness Joint instability Locking of joint during motion Crepitus Joint effusion
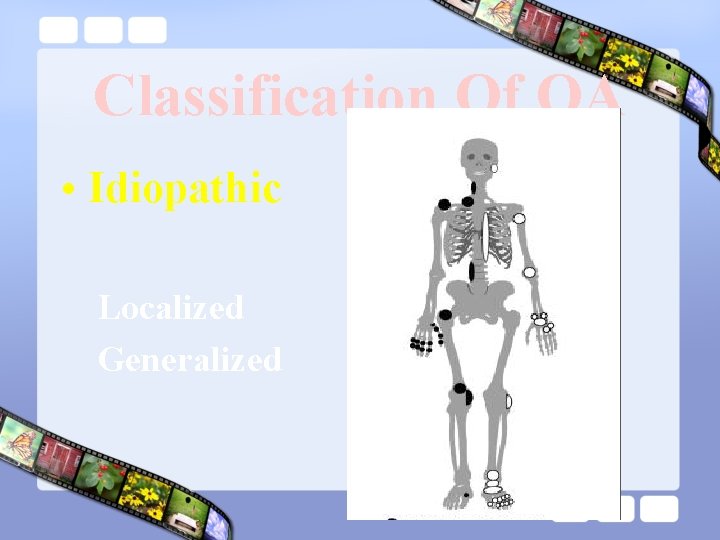
Classification Of OA • Idiopathic Localized Generalized • Secondary

Classification Of OA : heberden, Bouchard, erosive • Idiopathic* Hand Rhizarthrosis Localized Rhizarthrosis * Knee: Medial, Lateral, Patellofemoral * Hip: Eccentric, Concentric, Diffuse * Spine: Apophysial , intervertebral, Spondylosis * Others
Generalized Osteoarthritis
Hand Osteoarthritis
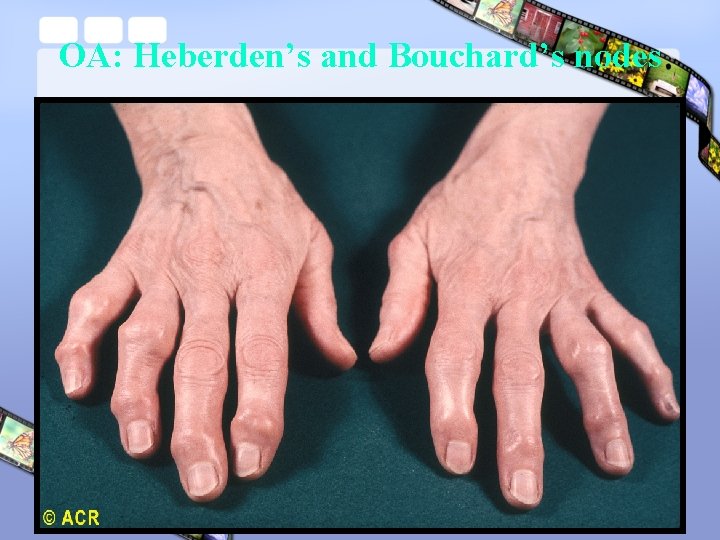
Artherosis of hand’s joints • F/m : 4/1 • • • 20 -65 ( >45 ) years Hereditary: 50% Associated with Knee disease & obesity DIP ( Heberden’s node ) PIP ( Buchardd’s node ) CMC 1 ( Rhizarthrosis )

Normal hand
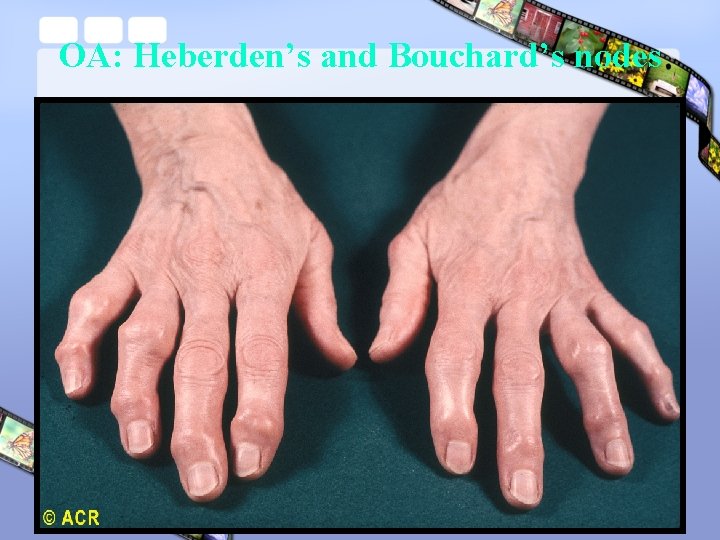
OA: Heberden’s and Bouchard’s nodes
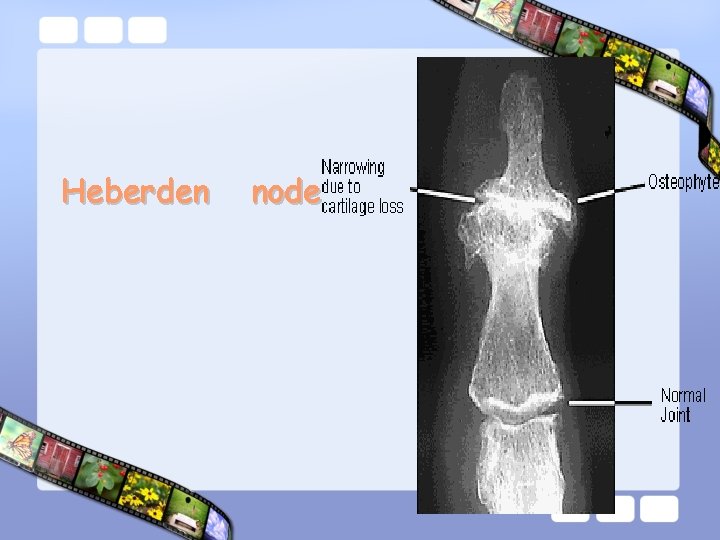
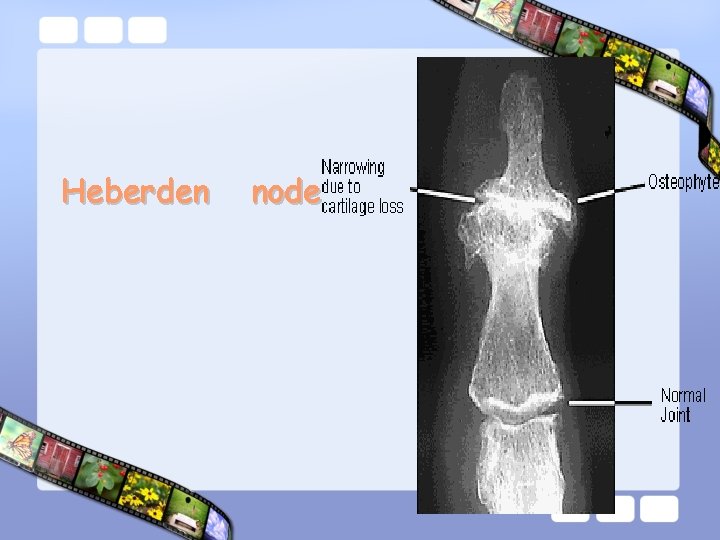
Heberden node


OA: first carpometacarpal joint (radiograph)
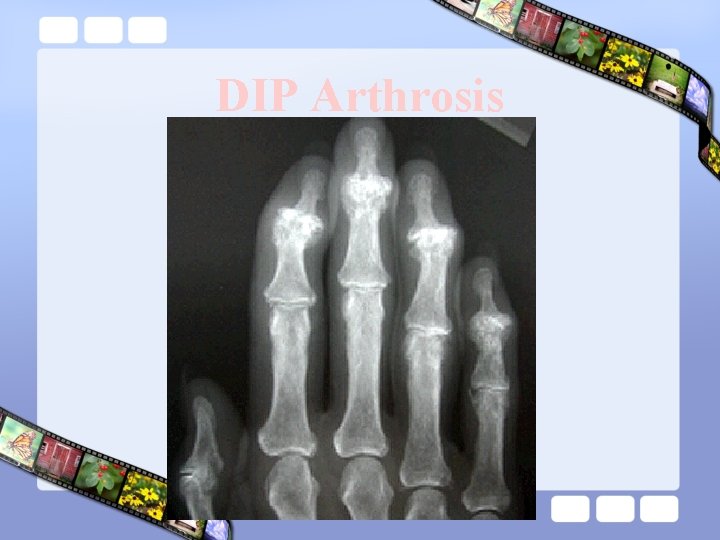
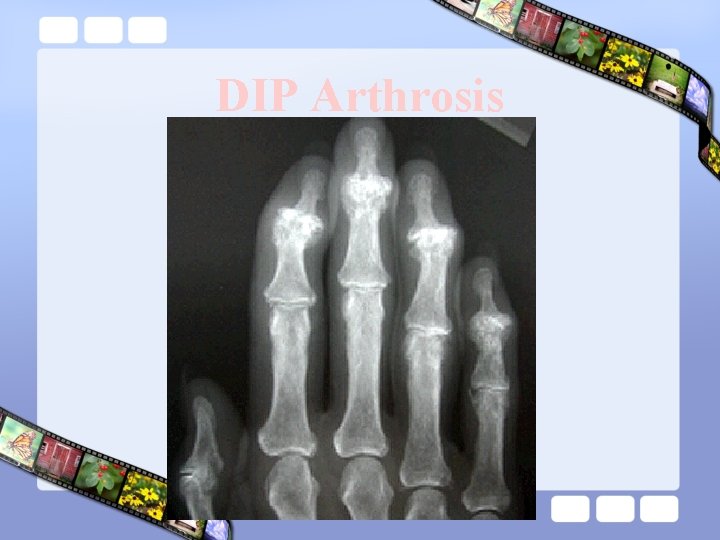
DIP Arthrosis
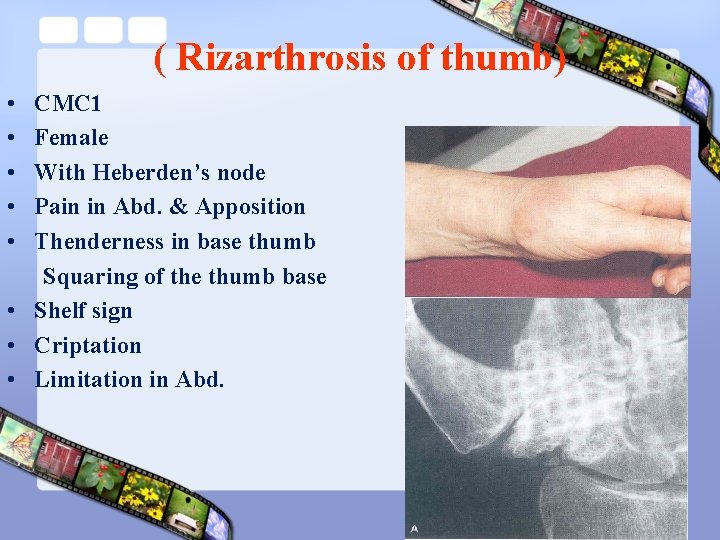
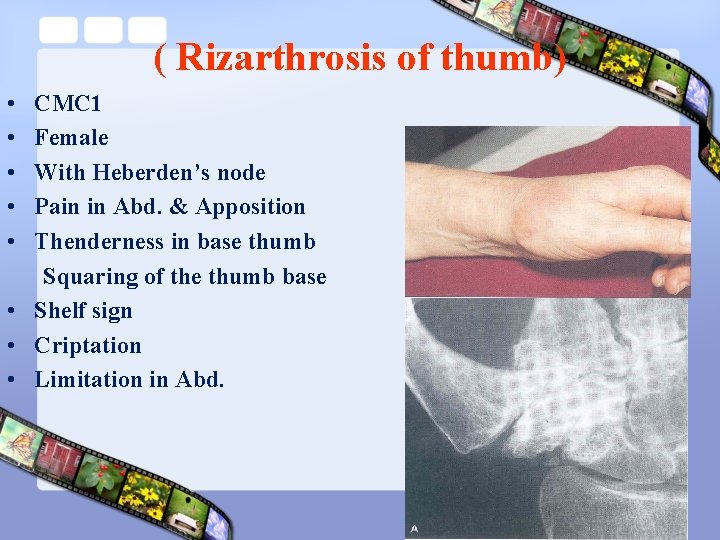
( Rizarthrosis of thumb) • • • CMC 1 Female With Heberden’s node Pain in Abd. & Apposition Thenderness in base thumb Squaring of the thumb base • Shelf sign • Criptation • Limitation in Abd.

OA: Heberden’s nodes, inflammation
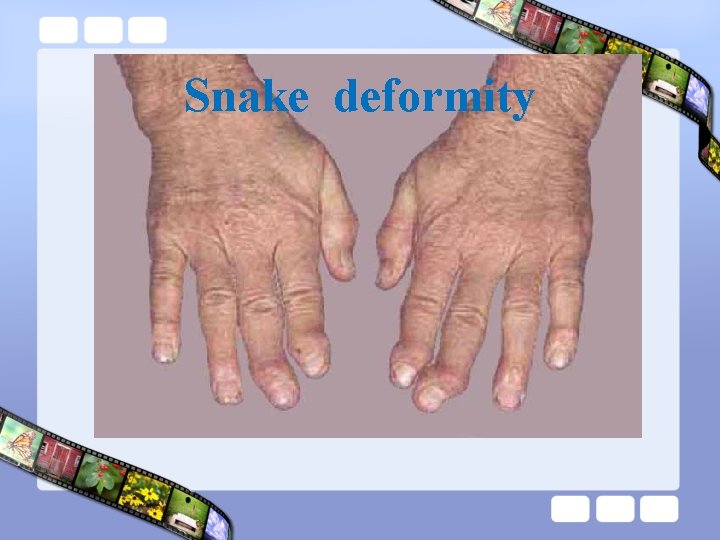
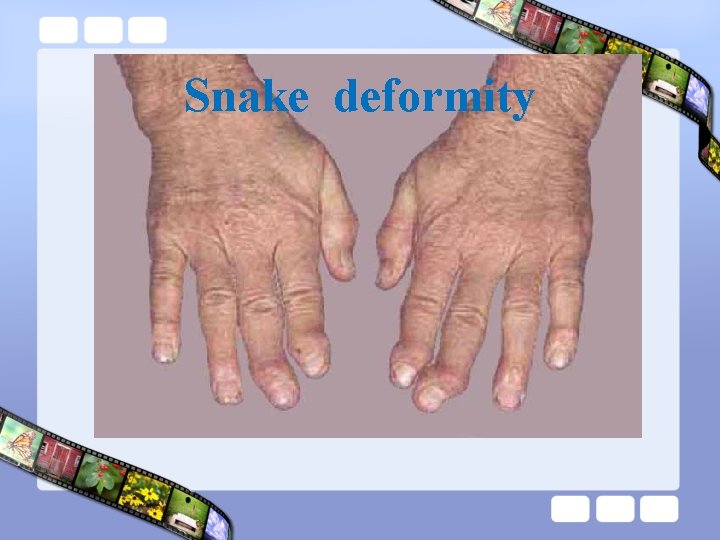
Snake deformity

KNEE OSTEOARTHRITIS
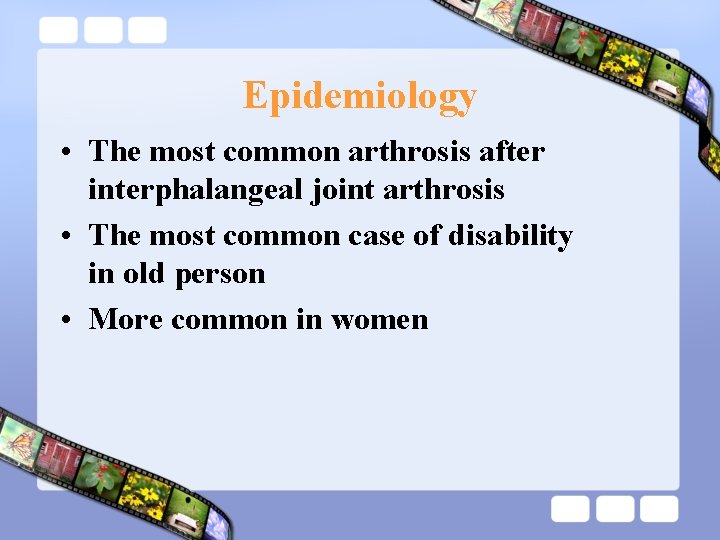
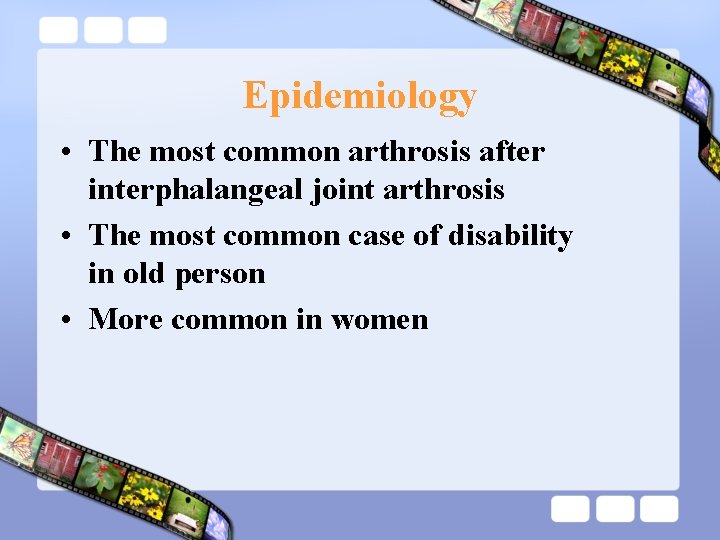
Epidemiology • The most common arthrosis after interphalangeal joint arthrosis • The most common case of disability in old person • More common in women
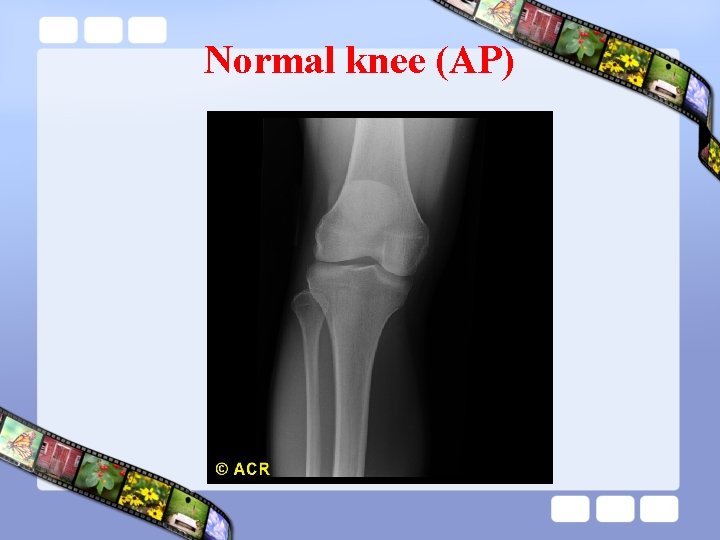
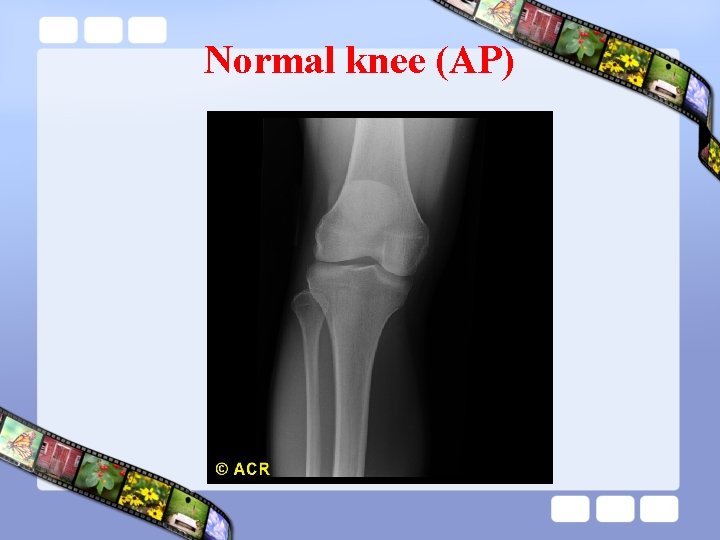
Normal knee (AP)
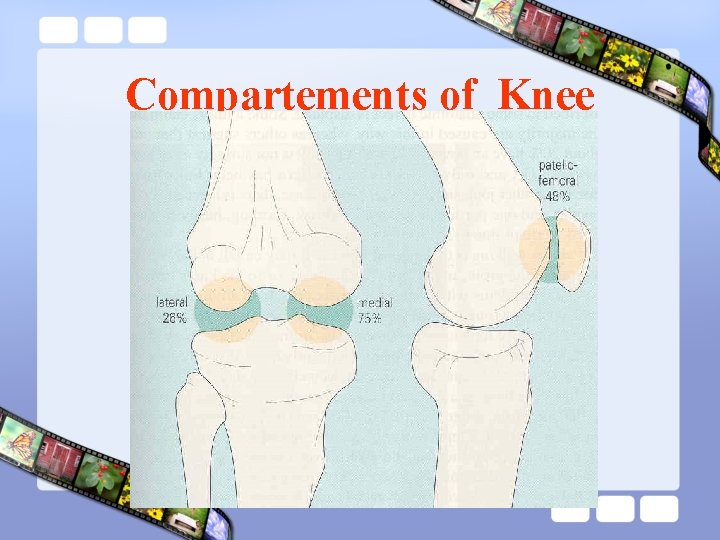
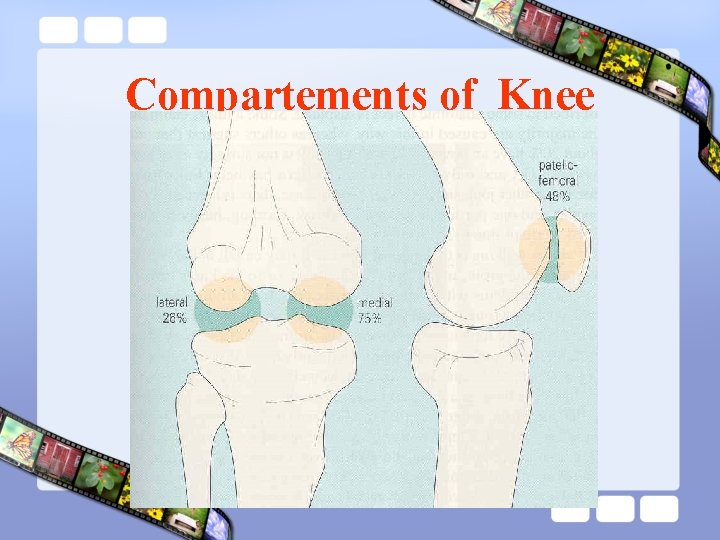
Compartements of Knee
Clinical findings • • • Symptoms Pain Joint stiffness Limitation of motion Alteration in joint shape Crepitus Feeling of instability
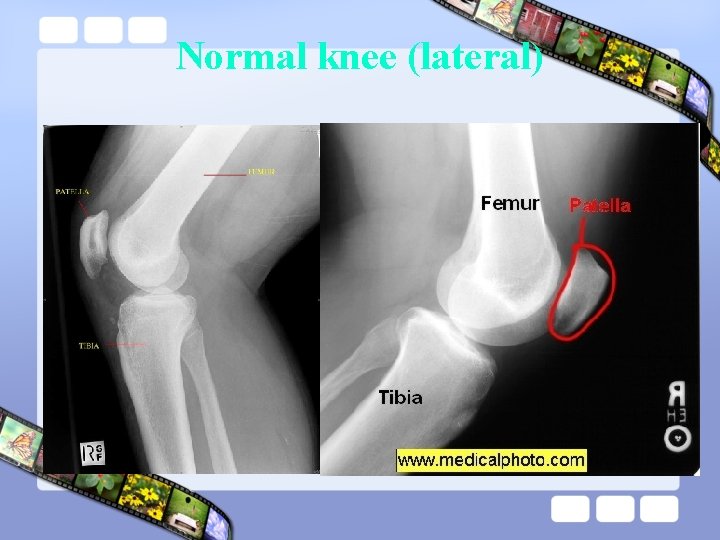
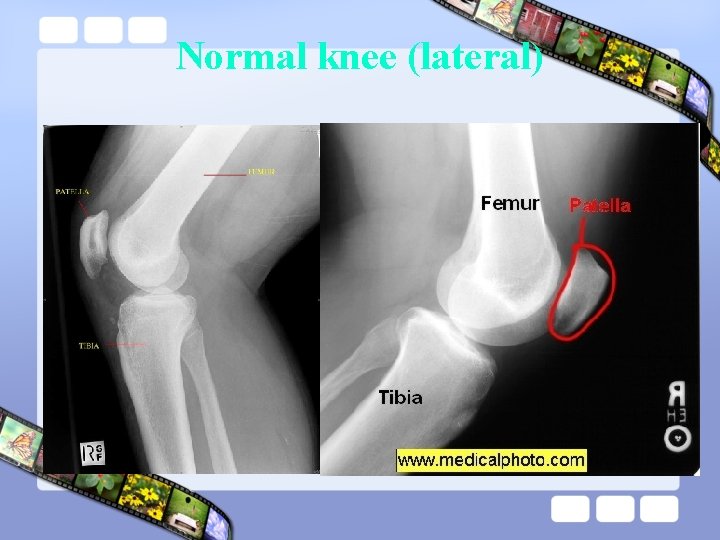
Normal knee (lateral)

OA: knees, medial and lateral cartilage degeneration

OA: knee, advanced disease

Risk Factors Mechanical abnormalities
Clinical findings • • • Crepitus Restriction of motion Tenderness Rabot’s sign and shrug’s sign Bone hypertrophy Effusion Angular deformity Limp Muscle atrophy Instability Signs

Knee Varus deformity

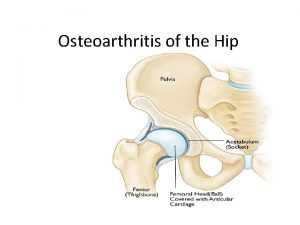
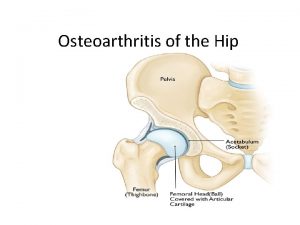
Hip Osteoarthritis

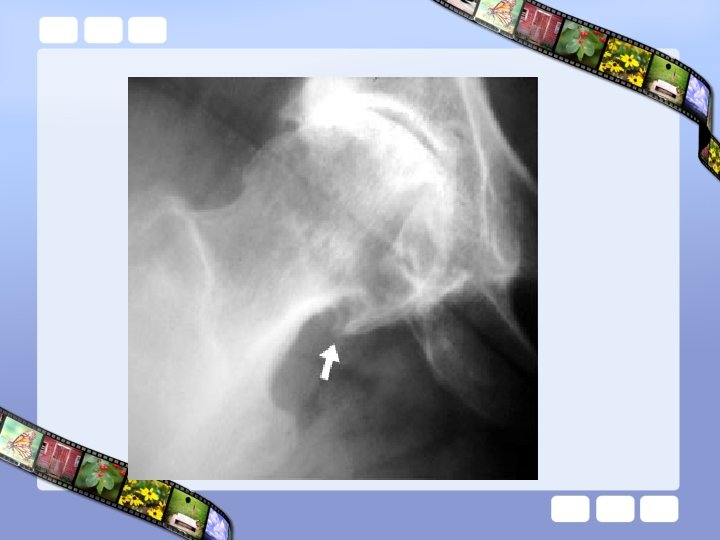
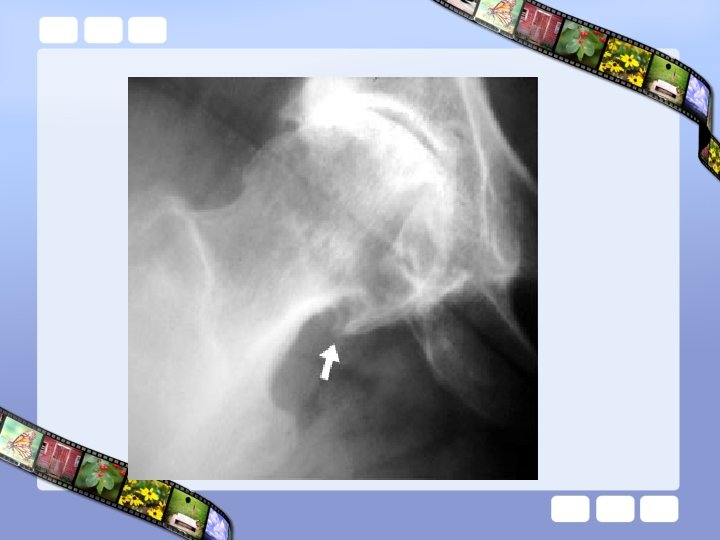
Osteoarthritis of Hip

Protrusio acetabuli

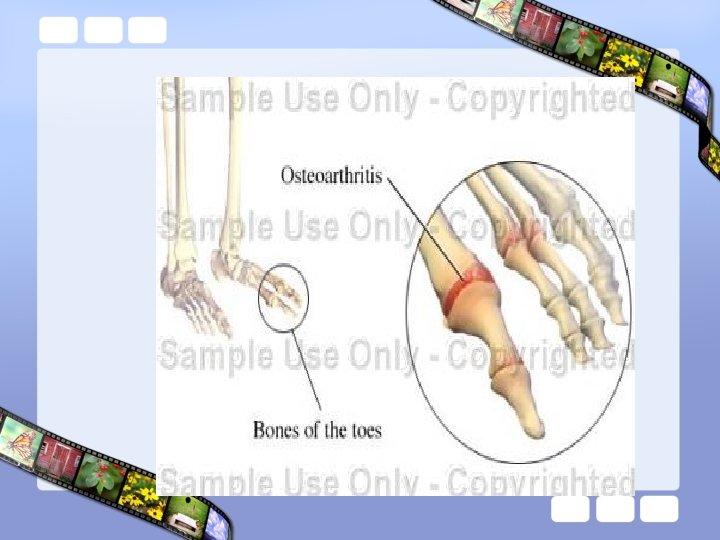
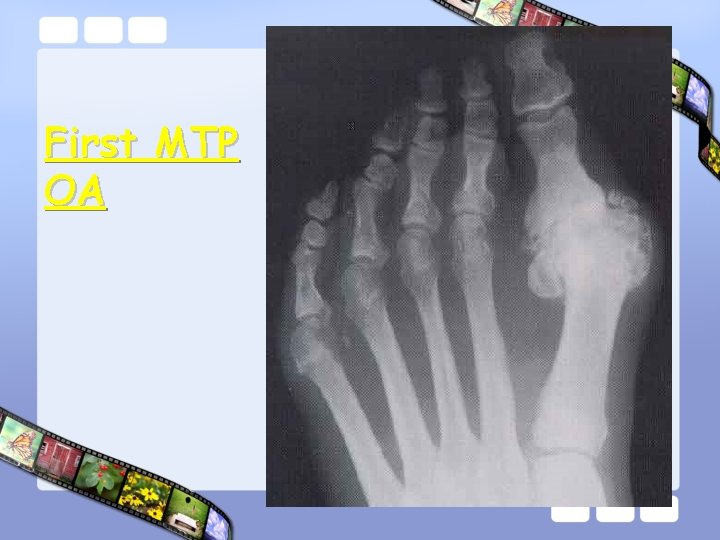
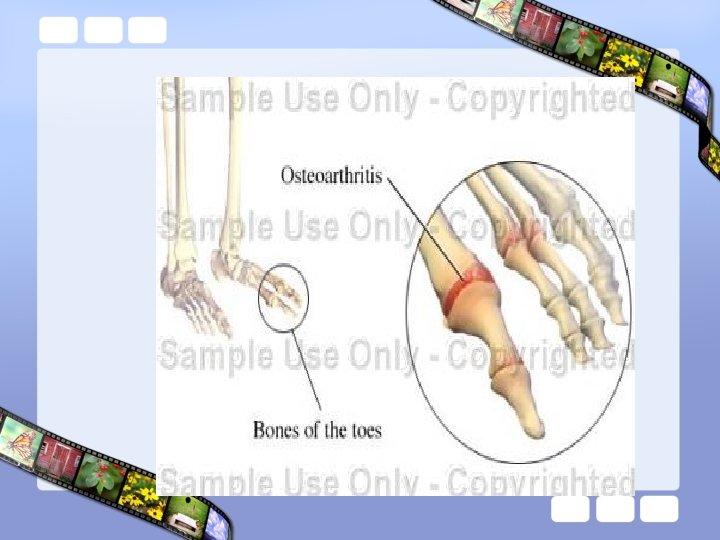
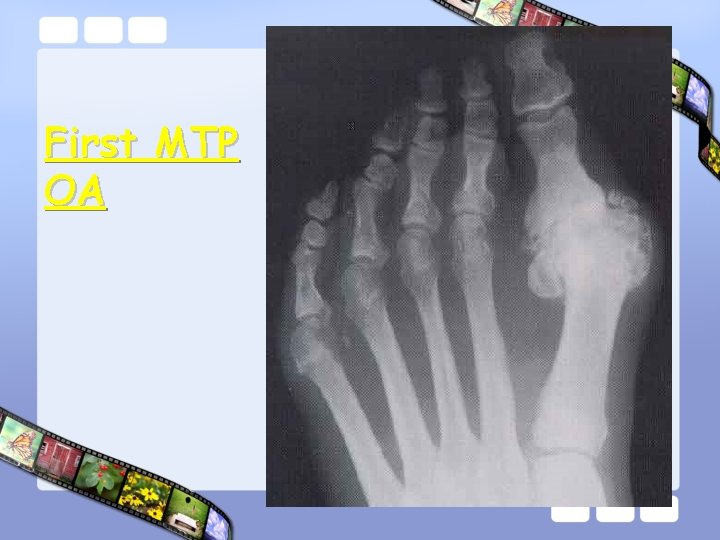
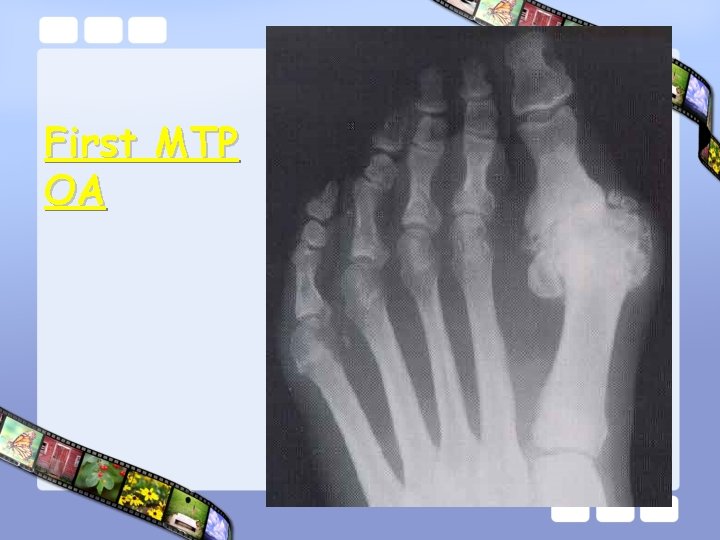
First MTP OA
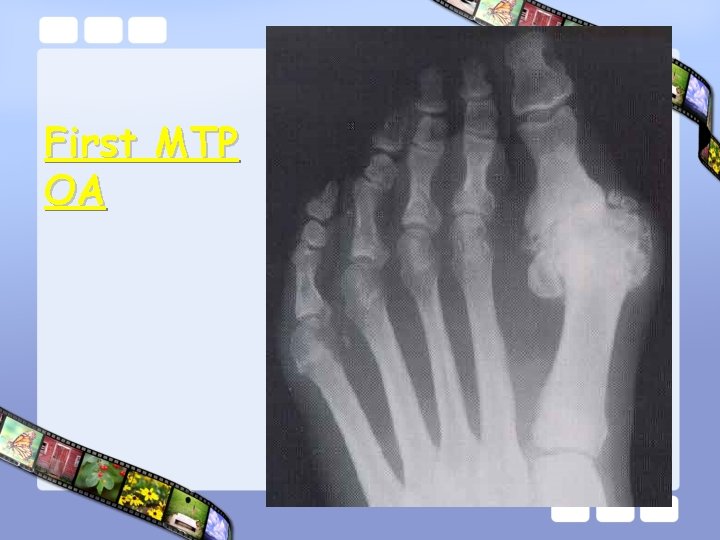
First MTP OA
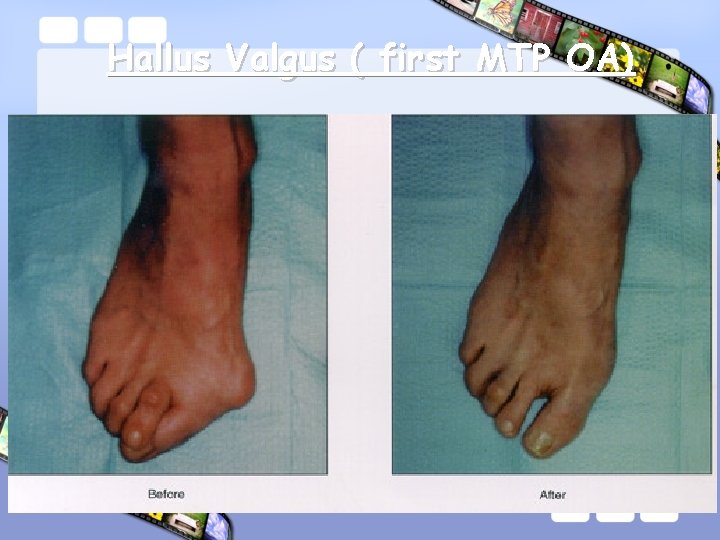
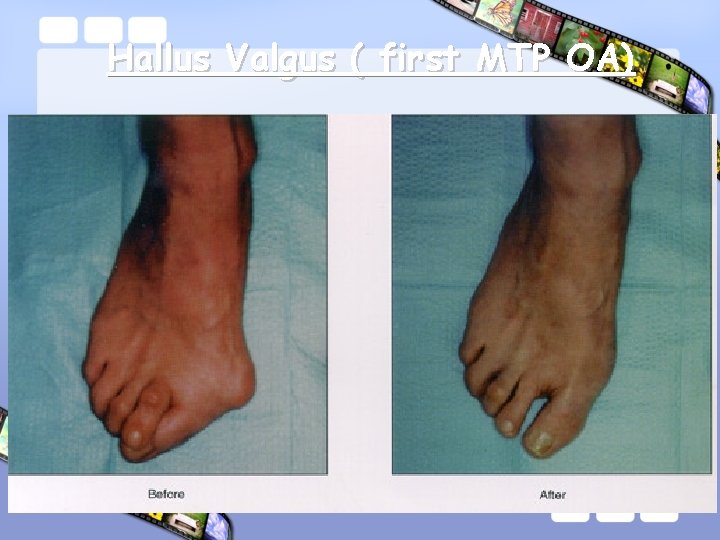
Hallus Valgus ( first MTP OA)

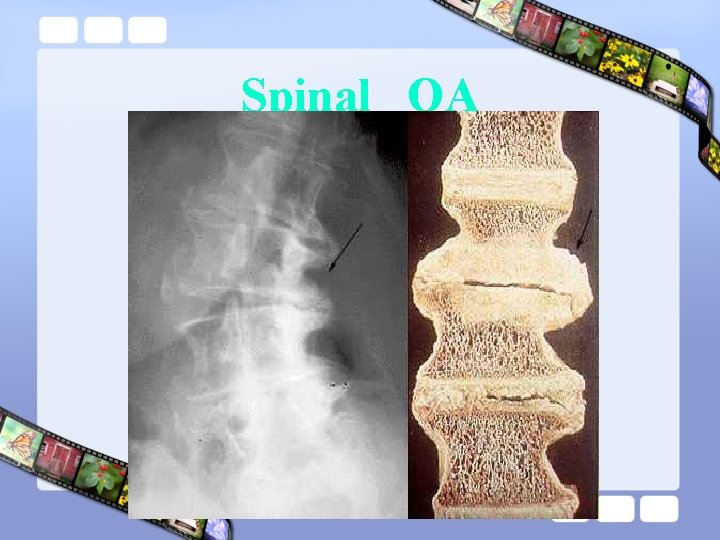
Spine OA
Classification Of OA • Idiopathic Localized Generalized
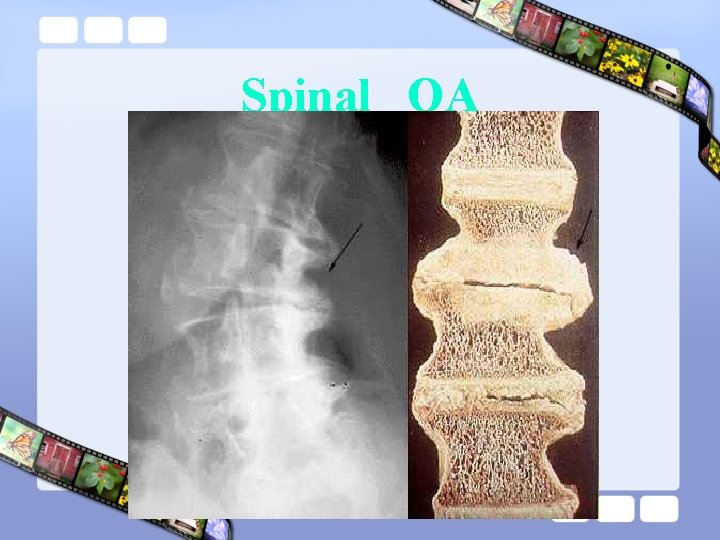
Spinal OA

Cervical osteoarthritis
Laboratory findings • • Normal ESR Negative CRP Negative autoantibodies Normal other tests
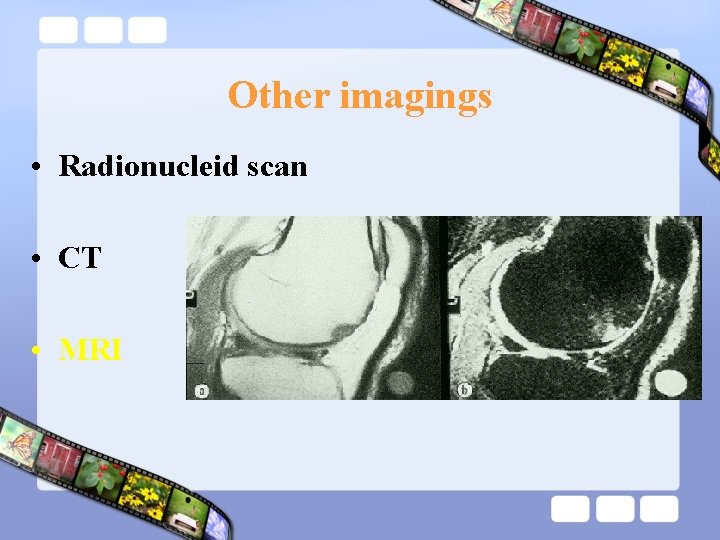
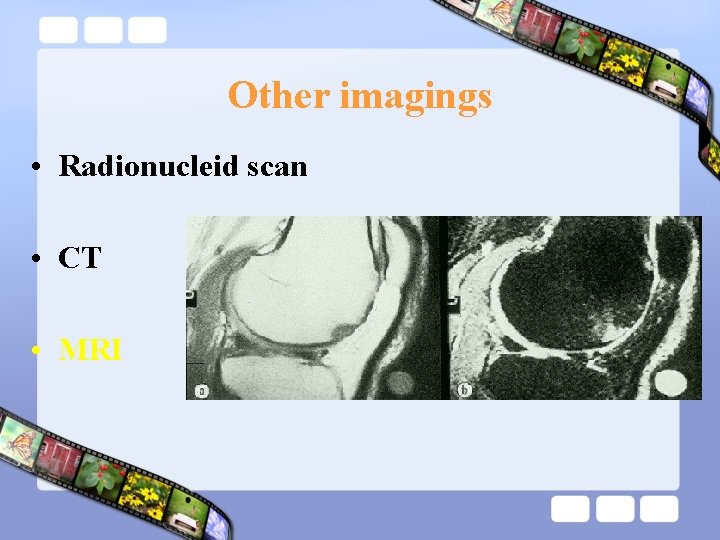
Other imagings • Radionucleid scan • CT • MRI
• 1. 2. 3. Treatment Reduction of knee loading Weight reduction Rest Recommendation to avoidance of activities that case excessive loading of the knee 4. Modification of workplace and life style 5. Cane
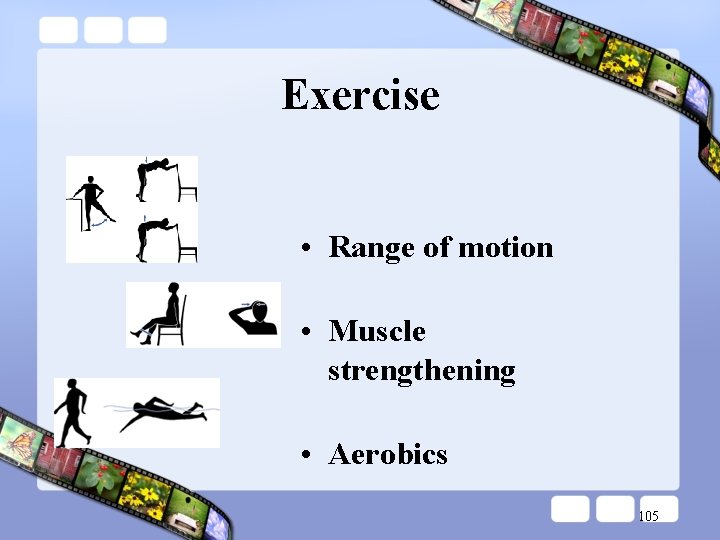
Evidence for Benefit from Exercise in Treating Knee and Hip OA • Regular aerobic walking for (Ia) • Home-based quad strength exercises (Ia) • Water-based aerobic exercise (Ia)
EXercise
Exercise
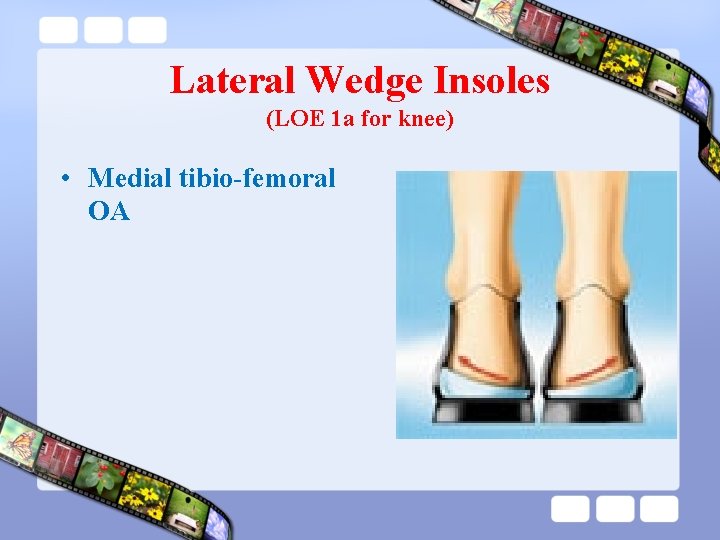
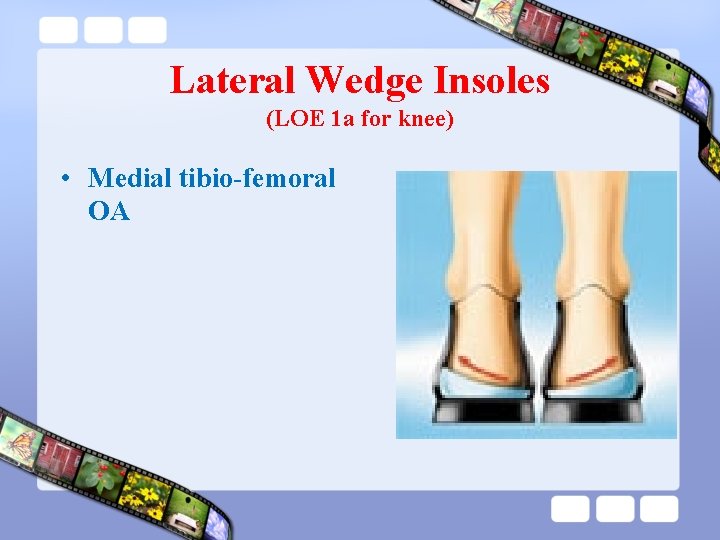
Lateral Wedge Insoles (LOE 1 a for knee) • Medial tibio-femoral OA

Brace
Treatment • Pain reduction 1. 2. 3. 4. Acetaminophen NSAID’s Capsaicin Opioids

Guidelines • Non-pharmacologic measures ─ Used with or without pharmacotherapy • Pharmacologic measures – Systemic pharmacotherapy • Acetaminophen • NSAIDs • -Topical NSAID and Analgesic – IA injection- steroids or hyaluronic acid – Topical capsaicin – surgery 103
Nonpharmacology -therapy • Exercise- regular aerobic, muscle strengthening and ROM exercises • Obesity reduction • Yoga • Low –energy lasers • Ultrasound • Therapeutic massage/Acupuncture • Patient education 104 • Reduction of joint load
Exercise • Range of motion • Muscle strengthening • Aerobics 105
Reducing joint load • Cane • Walker • Wedged lateral insoles 106
Vitamins • OA: less liklely to worsen in people who have high dietary intake of Vit C and Vit D. 107

Pharmacologic therapy • Systemic drugs • Topical applications • Intra-articular injections 108
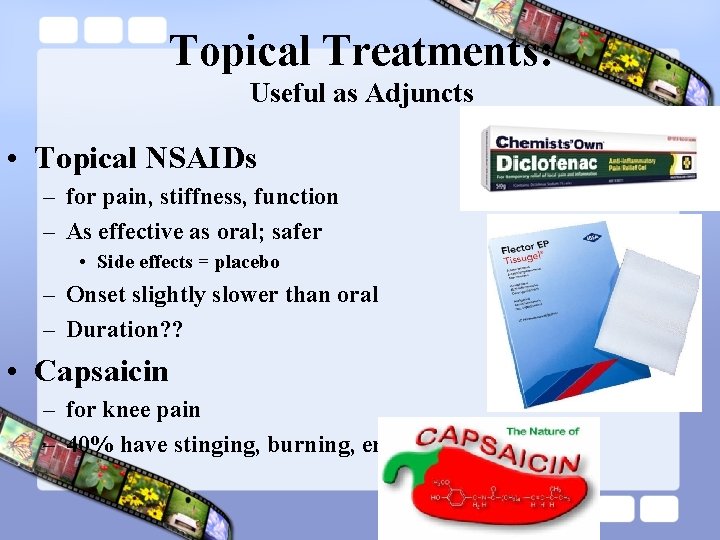
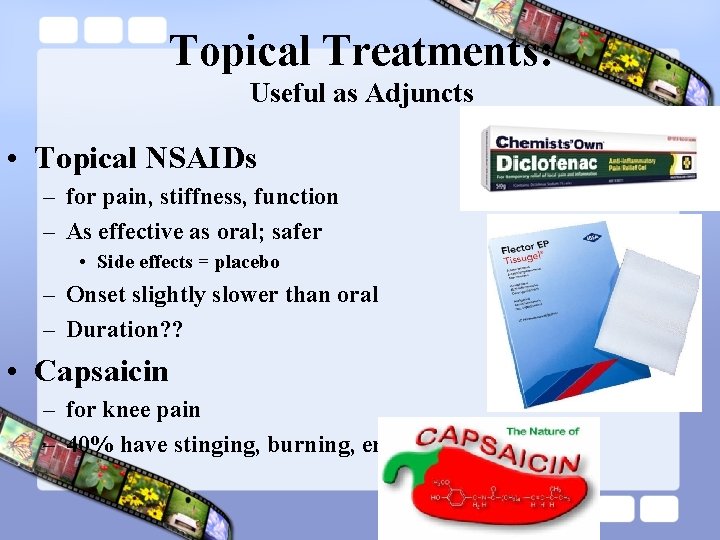
Topical Treatments: Useful as Adjuncts • Topical NSAIDs – for pain, stiffness, function – As effective as oral; safer • Side effects = placebo – Onset slightly slower than oral – Duration? ? • Capsaicin – for knee pain – 40% have stinging, burning, erythema

Non-steroidal antiinflammatory drugs • NSAIDs both analgesic and antiinflammatory • Non-selective NSAIDs inhibit both COX-1 and COX-2 enzymes • Use of NSAIDs is associated with many adverse effects 110

Diacerein • Inhibit IL-1 and reduce cartilage breckdown and major adverse event is diarrhea(is dose dependent) 111
Opioids • For moderately severe to severe pain, opioids can be used – acetaminophen+ codein – Tramadol 112
Acetaminophen (ACET( • Analgesic by elevating pain threshold • No gastric irritation • Consistently recommended by all major guidelines as the first drug of choice for OA pain • Inexpensive • Up to 4 grams daily if no liver 113 problems, for mild to moderate
Piascledine • Avocado/soybean: is commonly used for hip and knee OA in europe the evidence of its efficacy is small. 114
Colchicine • Recommended for inflammatory OA that doesnot improve with nonpharmmacologic therapies and NSAID. • Recommend colchicine for flar of OA that is resistant to other treatment. 115
Hydroxychloroqine • Recommended for sever inflammatory OA and who have bone damage related to OA. 116
Glucosamine/Chondroitin- • recommend in patients with knee and hip OA – GS 1500 mg/ CS 800 mg • 3 month trial, evaluate efficacy; continue if helping • Consider indefinite use even if no pain relief for joint space preservation
Intra-articular injections • Intra-articular injection used for OA pain due to inflammation or effusions • Corticosteroids or hyaluronan 118
Intra-articular glucocorticoid • Supress inflammation and relieve arthritis symptoms. • Recommended for OA who still have pain despite use of NSAID or who donot get adequate pain relif with them. • 3 -4 injection per year

Intra-articular Hyaluronate • Recommended for OA who cannot use of NSAID or who donot get adequate pain relif with them. • Pain relif may last for several months.

Surgery • Arthroscopy synovectomy/ • Realignment • Fusion • Joint replacement • Cartilage grafting
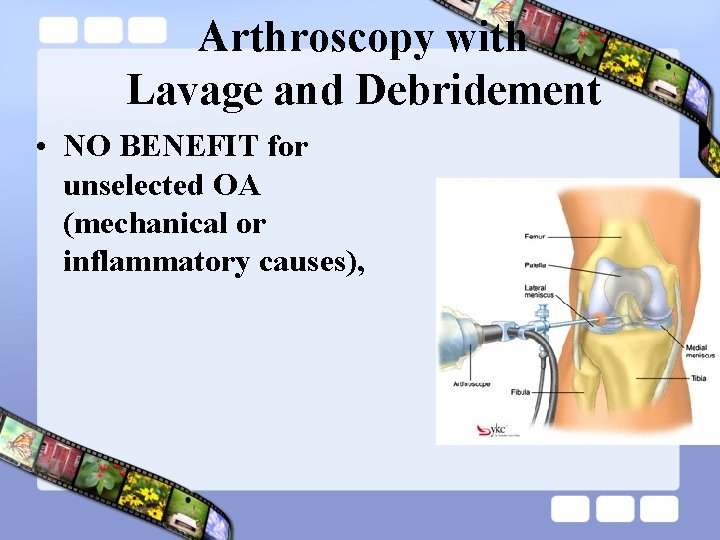
Arthroscopy with Lavage and Debridement • NO BENEFIT for unselected OA (mechanical or inflammatory causes),
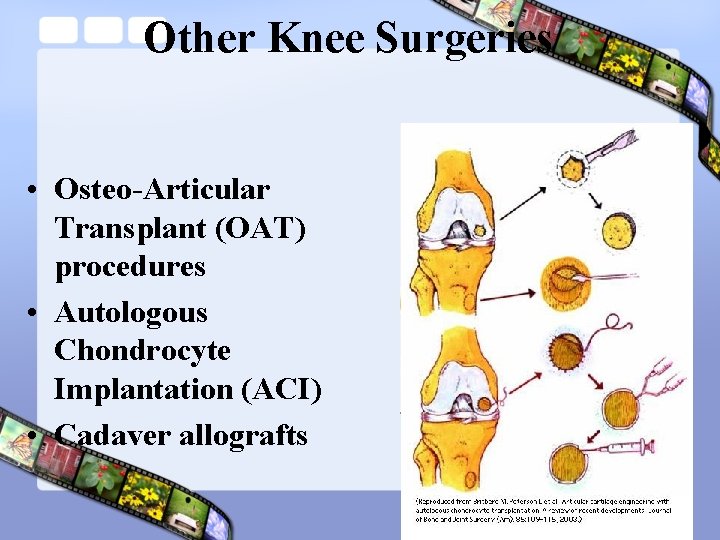
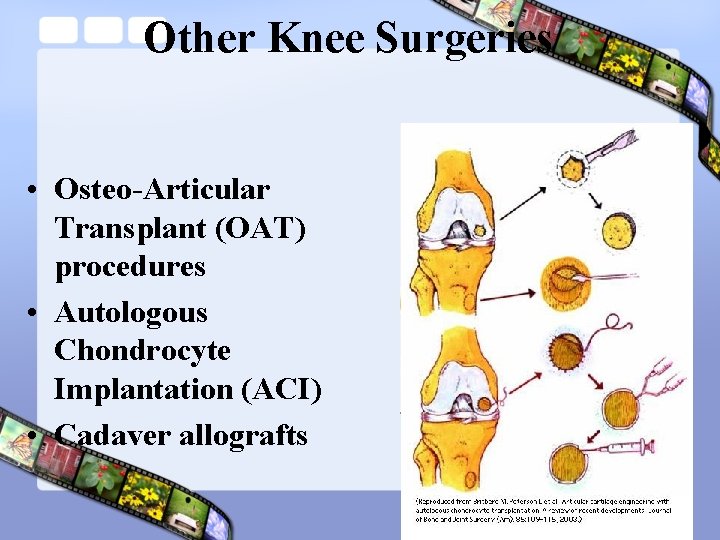
Other Knee Surgeries • Osteo-Articular Transplant (OAT) procedures • Autologous Chondrocyte Implantation (ACI) • Cadaver allografts
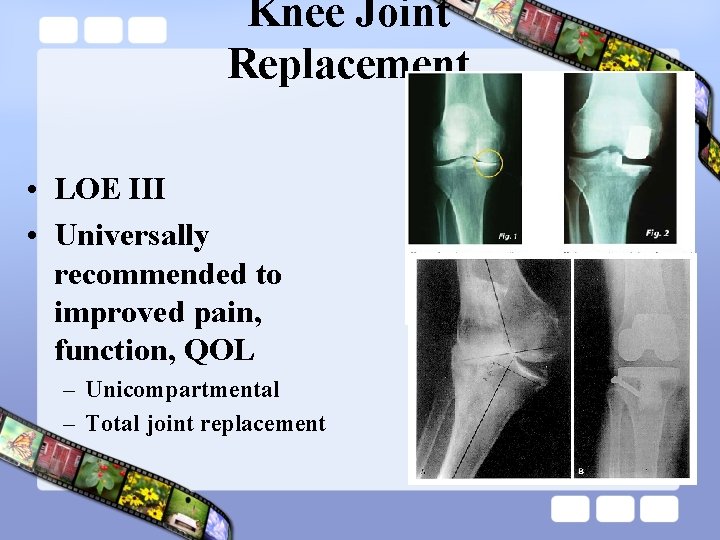
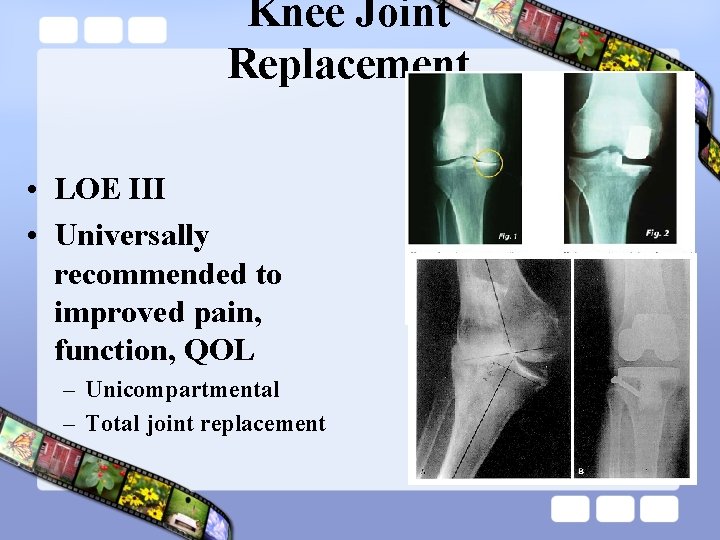
Knee Joint Replacement • LOE III • Universally recommended to improved pain, function, QOL – Unicompartmental – Total joint replacement
NO inhibitors • Fluxetin, Tricyclic antidepressant ♠ • Vitamin : ♠ ♠ ♠ Vit Vit A D C E

Arthroplasty

Gelling pain

128
 Dr eugene lim rheumatologist
Dr eugene lim rheumatologist Rheumatologist carefirst bcbs
Rheumatologist carefirst bcbs Rheumatologist vsp
Rheumatologist vsp Dr forghani rheumatologist
Dr forghani rheumatologist Dr susan wallis rheumatologist
Dr susan wallis rheumatologist Dr muna noori
Dr muna noori Muna noori
Muna noori Dr. sheak rashed haider noori
Dr. sheak rashed haider noori Meerangdo leirangdo part 66
Meerangdo leirangdo part 66 Nodus heberden dan bouchard
Nodus heberden dan bouchard Atlantoaxial osteoarthritis
Atlantoaxial osteoarthritis Osteoarthritis
Osteoarthritis Pictures of rheumatoid arthritis vs osteoarthritis
Pictures of rheumatoid arthritis vs osteoarthritis Osteoarthritis
Osteoarthritis Osteoarthritis
Osteoarthritis Generalised osteoarthritis
Generalised osteoarthritis Nursing management of arthritis
Nursing management of arthritis Osteoarthritis location
Osteoarthritis location Grade oa
Grade oa Osteoarthritis soap note
Osteoarthritis soap note Muscle loss icd 10
Muscle loss icd 10