Osseous Tissue Bone Tissue Classification of Bone by
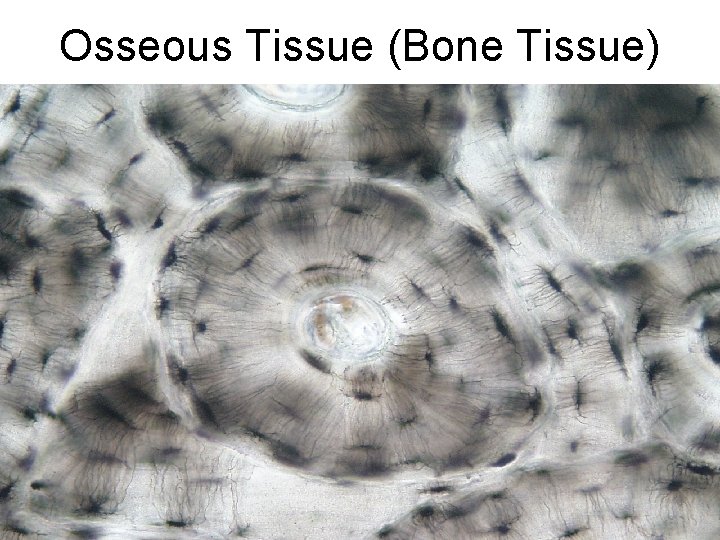
Osseous Tissue (Bone Tissue)
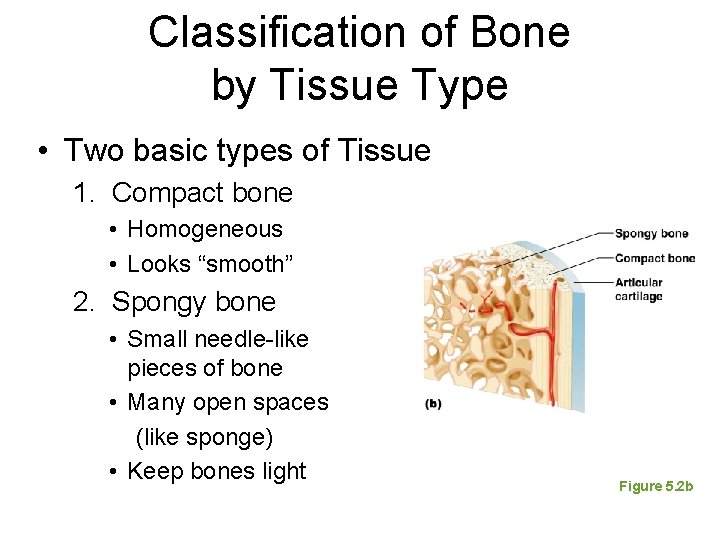
Classification of Bone by Tissue Type • Two basic types of Tissue 1. Compact bone • Homogeneous • Looks “smooth” 2. Spongy bone • Small needle-like pieces of bone • Many open spaces (like sponge) • Keep bones light Figure 5. 2 b
Review: • Bone is a type of connective tissue 2 Parts: 1. Cells (living) 2. Matrix (nonliving substance released by cells) A. Fiber B. Ground Substance
Formation of the Human Skeleton • In embryos, the skeleton is primarily hyaline cartilage • During development, much of this cartilage is replaced by bone • Cartilage remains in isolated areas – Bridge of the nose – Parts of ribs – Joints
Bone Growth (Ossification) • Epiphyseal Plate: epi- above physean- to grow • plates allow for lengthwise growth of long bones during childhood – New cartilage is continuously formed – Older cartilage becomes ossified • Cartilage is broken down • Enclosed cartilage is digested away, opening up a medullary cavity • Bone replaces cartilage through the action of osteoblasts
Bone Growth (Ossification) • Bones are remodeled and lengthened until growth stops – Bones are remodeled in response to two factors • Blood calcium levels • Pull of gravity and muscles on the skeleton – Bones grow in width (called appositional growth)
1. Cells • • • Osteocytes— mature bone cells Osteoblasts— bone-forming cells (germ cells or “bud” cells) Osteoclasts —bone-destroying cells (“breakers”) 2. Matrix A. primarily collagen fibers flexibility tensile strength (the strength to endure stretching forces) B. calcium salts (hardness) contain calcium and phosphorus great compressional strength (the strength to endure squeezing forces)
Bone Remodeling constant balance of bone deposit and removal that occurs throughout your life bone deposit occurs at a greater rate when bone is injured bone resorption allows calcium of degraded bone matrix to move into the blood. About 10% of bone is replaced every year in an adult skeleton
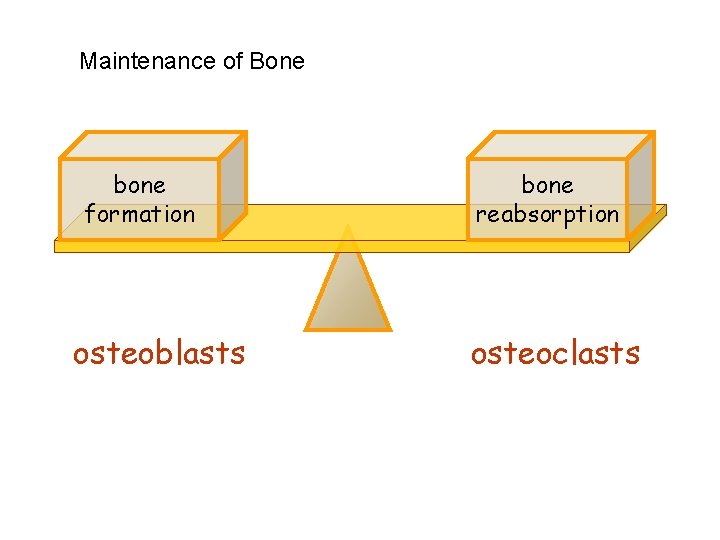
Maintenance of Bone bone formation osteoblasts bone reabsorption osteoclasts
Control of Remodeling Hormonal – Rising blood Ca 2+ levels trigger the thyroid to release calcitonin – Calcitonin stimulates calcium salt deposit in bone – Falling blood Ca 2+ levels signal the parathyroid glands to release Parathyroid hormone (PTH) – PTH signals osteoclasts to degrade bone matrix and release Ca 2+ into the blood
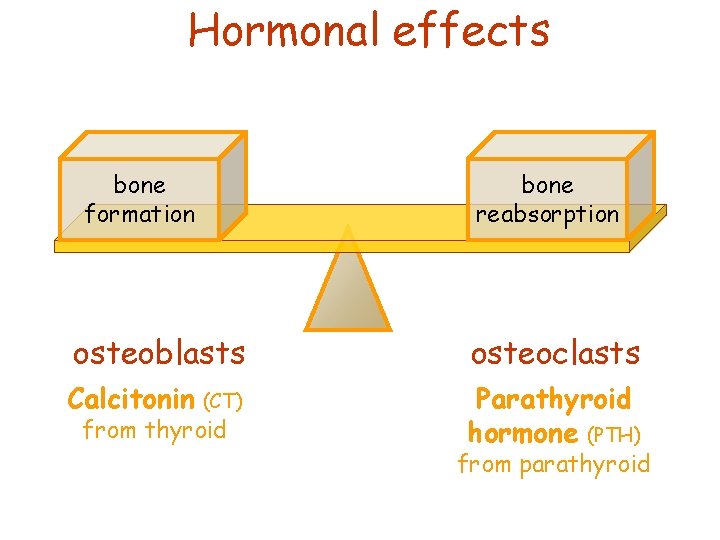
Hormonal effects bone formation bone reabsorption osteoblasts osteoclasts Calcitonin Parathyroid hormone (PTH) (CT) from thyroid from parathyroid
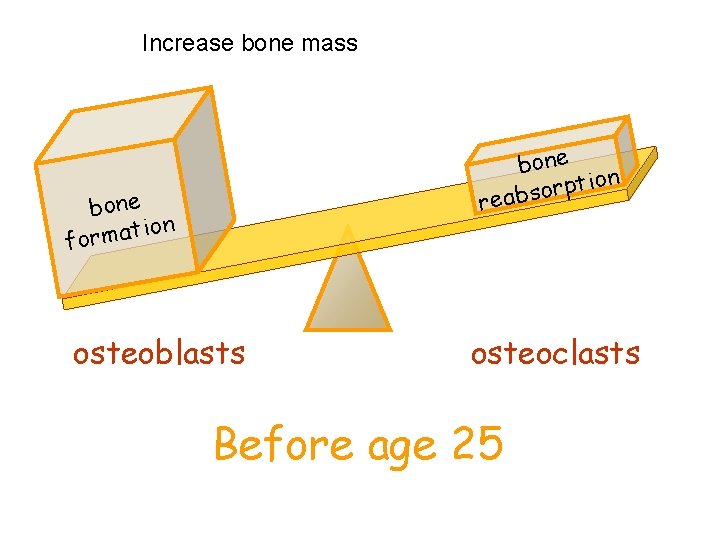
Increase bone mass bone on i t p r o reabs bone ion t a m r o f osteoblasts osteoclasts Before age 25
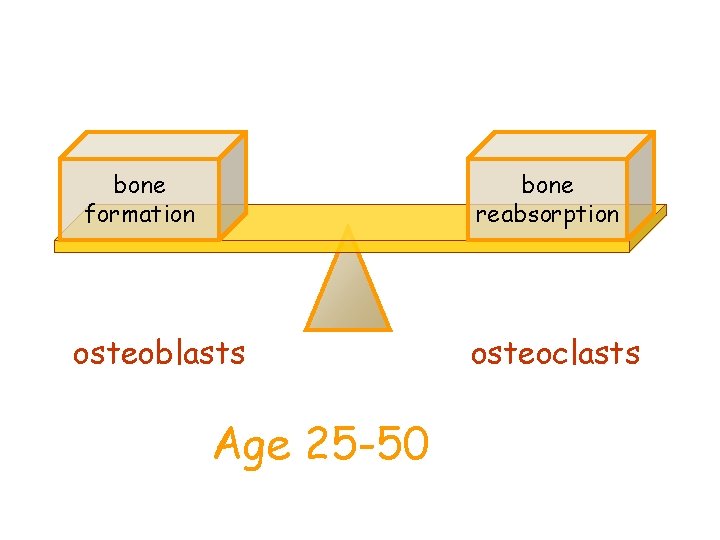
bone formation bone reabsorption osteoblasts Age 25 -50 osteoclasts
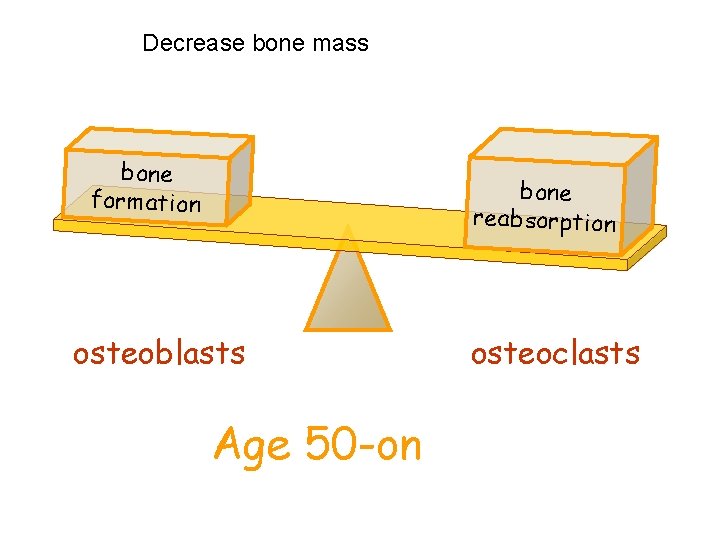
Decrease bone mass bone formation bone reabsorption osteoblasts Age 50 -on osteoclasts
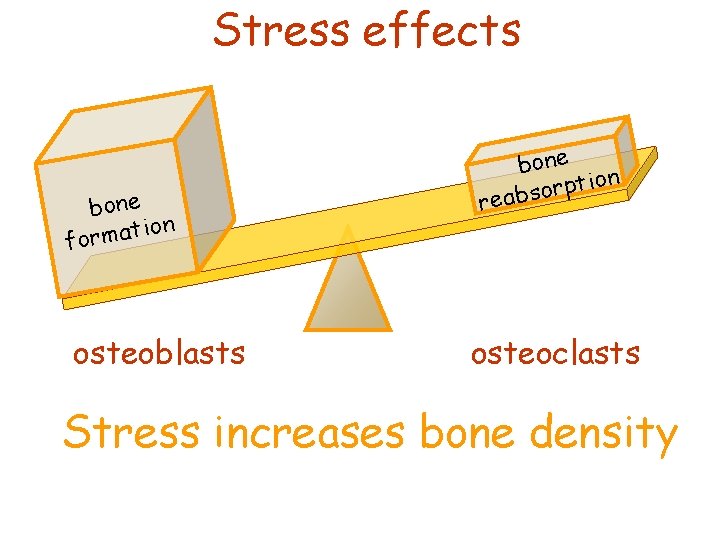
Stress effects bone ion t a m r o f osteoblasts bone on i t p r o reabs osteoclasts Stress increases bone density
Increasing bone stress can reduce or eliminate age-related bone loss
http: //www. youtube. com/watch? v=y. FJ 4 isw. Riu 4&feature=related
- Slides: 17