OSSEOUS TISSUE BONE STRUCTURE CHAPTER 6 List and
OSSEOUS TISSUE & BONE STRUCTURE CHAPTER 6
List and describe the functions of bones Describe the classes of bones Discuss the process of bone formation and development Explain how bone repairs itself after a fracture Discuss the effect of exercise, nutrition, and hormones on bone tissue Describe how an imbalance of calcium can affect bone tissue CHAPTER 6 LEARNING OBJECTIVES
FUNCTIONS OF SKELETAL SYSTEM Support • Structural framework for soft tissues and organs Protection • Bones surround delicate and fragile organs Leverage • Function as levers to change magnitude and direction of forces generated by skeletal muscles to produce movements Storage of Minerals Blood Cell Production • Matrix are valuable mineral reserve to maintain normal concentrations of calcium and phosphate ions in the body • Hematopoeisis. Production of RBCs, WBCs, and Platelets
• Adult skeleton has 206 bones • Divided into 2 Areas: – Axial skeleton BONE CLASSIFICATION • Skull • Thorax • vertebral column – Appendicular skeleton • Limbs and shoulder/pelvic girdles
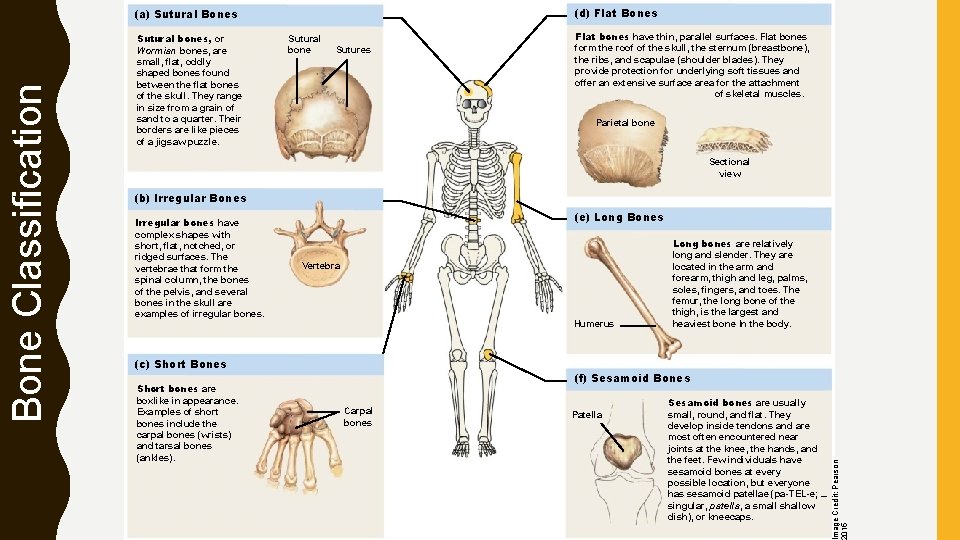
(d) Flat Bones Sutural bones, or Wormian bones, are small, flat, oddly shaped bones found between the flat bones of the skull. They range in size from a grain of sand to a quarter. Their borders are like pieces of a jigsaw puzzle. Sutural bone Sutures Flat bones have thin, parallel surfaces. Flat bones form the roof of the skull, the sternum (breastbone), the ribs, and scapulae (shoulder blades). They provide protection for underlying soft tissues and offer an extensive surface area for the attachment of skeletal muscles. Parietal bone Sectional view (b) Irregular Bones Irregular bones have complex shapes with short, flat, notched, or ridged surfaces. The vertebrae that form the spinal column, the bones of the pelvis, and several bones in the skull are examples of irregular bones. (e) Long Bones Vertebra Humerus (c) Short Bones Short bones are boxlike in appearance. Examples of short bones include the carpal bones (wrists) and tarsal bones (ankles). Long bones are relatively long and slender. They are located in the arm and forearm, thigh and leg, palms, soles, fingers, and toes. The femur, the long bone of the thigh, is the largest and heaviest bone In the body. (f) Sesamoid Bones Carpal bones Patella Sesamoid bones are usually small, round, and flat. They develop inside tendons and are most often encountered near joints at the knee, the hands, and the feet. Few individuals have sesamoid bones at every possible location, but everyone has sesamoid patellae (pa-TEL-e; – singular, patella, a small shallow dish), or kneecaps. Image Credit: Pearson 2015 Bone Classification (a) Sutural Bones
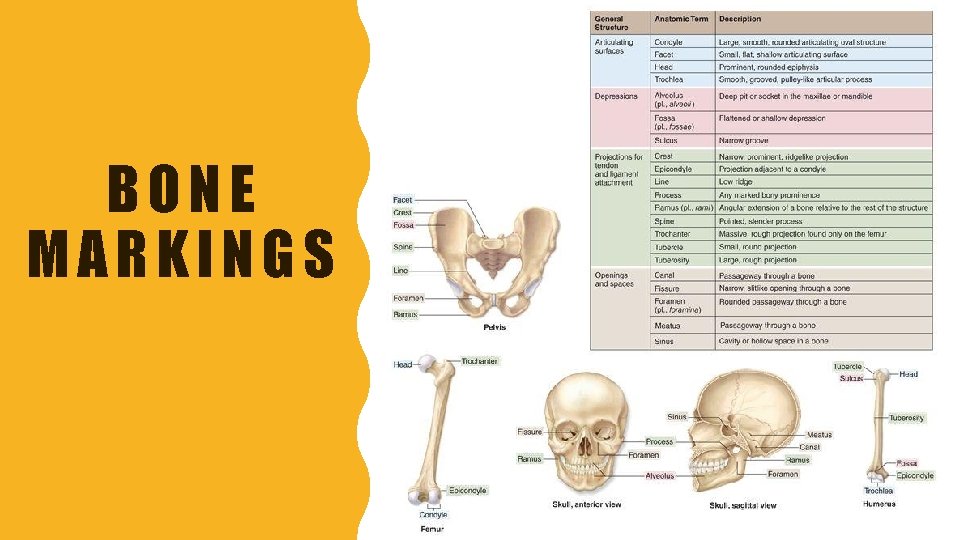
BONE MARKINGS
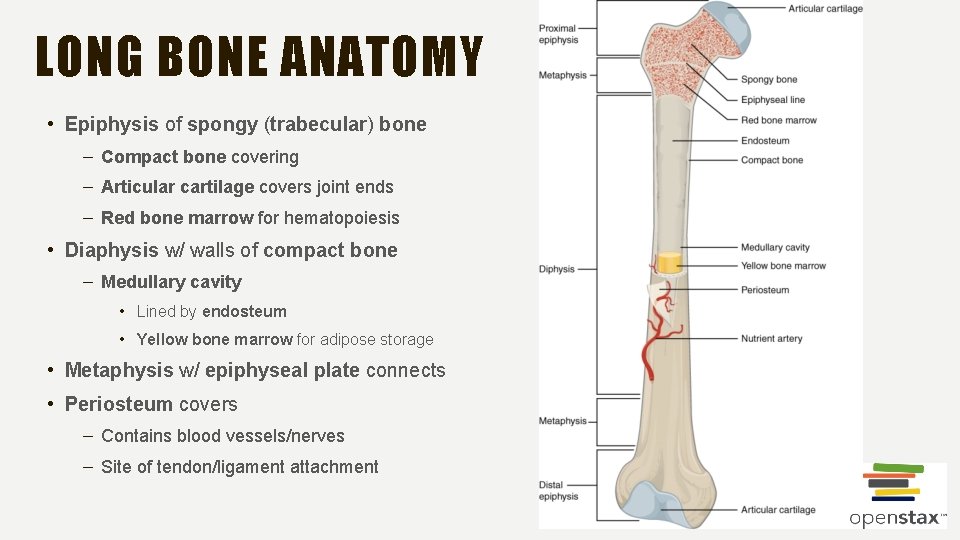
LONG BONE ANATOMY • Epiphysis of spongy (trabecular) bone – Compact bone covering – Articular cartilage covers joint ends – Red bone marrow for hematopoiesis • Diaphysis w/ walls of compact bone – Medullary cavity • Lined by endosteum • Yellow bone marrow for adipose storage • Metaphysis w/ epiphyseal plate connects • Periosteum covers – Contains blood vessels/nerves – Site of tendon/ligament attachment
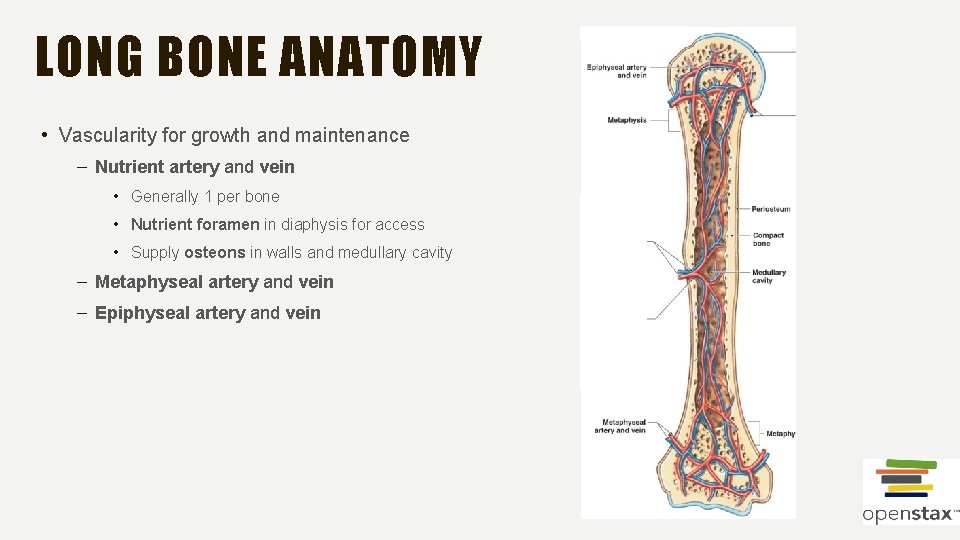
LONG BONE ANATOMY • Vascularity for growth and maintenance – Nutrient artery and vein • Generally 1 per bone • Nutrient foramen in diaphysis for access • Supply osteons in walls and medullary cavity – Metaphyseal artery and vein – Epiphyseal artery and vein
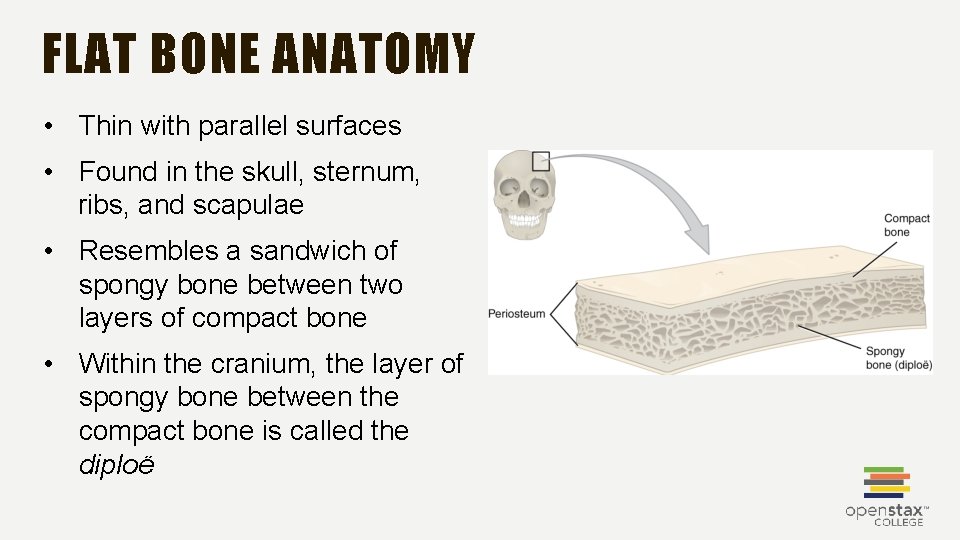
FLAT BONE ANATOMY • Thin with parallel surfaces • Found in the skull, sternum, ribs, and scapulae • Resembles a sandwich of spongy bone between two layers of compact bone • Within the cranium, the layer of spongy bone between the compact bone is called the diploë
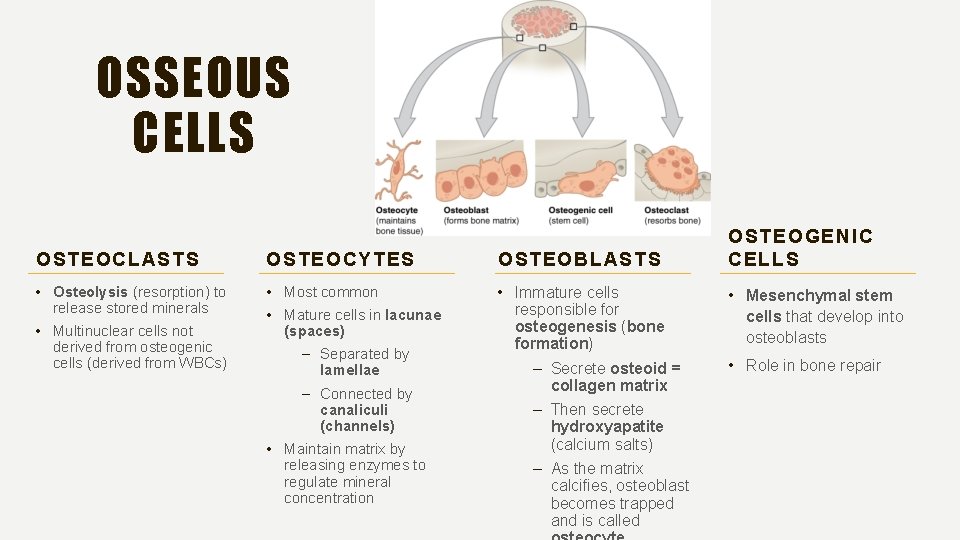
OSSEOUS CELLS OSTEOCLASTS OSTEOCYTES OSTEOBLASTS • Osteolysis (resorption) to release stored minerals • Multinuclear cells not derived from osteogenic cells (derived from WBCs) • Most common • Mature cells in lacunae (spaces) – Separated by lamellae – Connected by canaliculi (channels) • Maintain matrix by releasing enzymes to regulate mineral concentration • Immature cells responsible for osteogenesis (bone formation) – Secrete osteoid = collagen matrix – Then secrete hydroxyapatite (calcium salts) – As the matrix calcifies, osteoblast becomes trapped and is called OSTEOGENIC CELLS • Mesenchymal stem cells that develop into osteoblasts • Role in bone repair
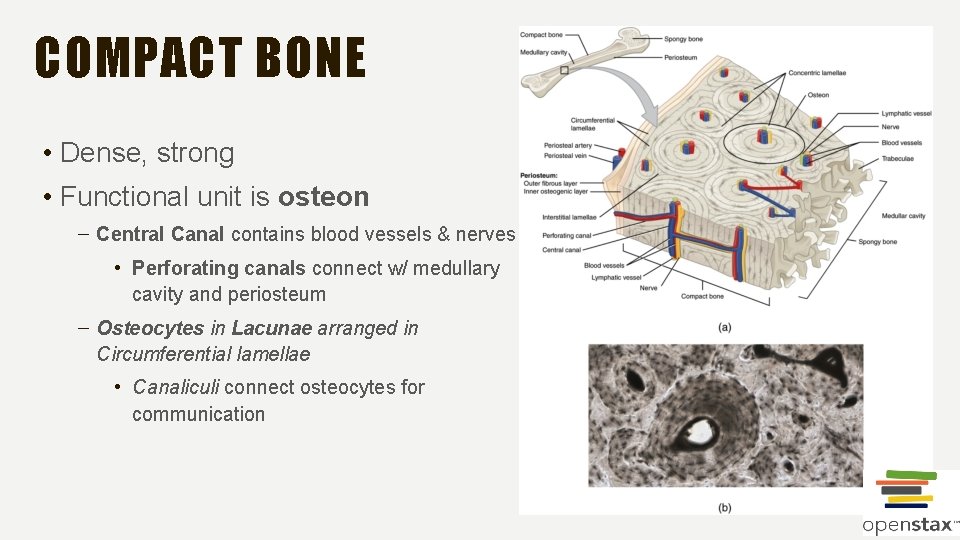
COMPACT BONE • Dense, strong • Functional unit is osteon – Central Canal contains blood vessels & nerves • Perforating canals connect w/ medullary cavity and periosteum – Osteocytes in Lacunae arranged in Circumferential lamellae • Canaliculi connect osteocytes for communication
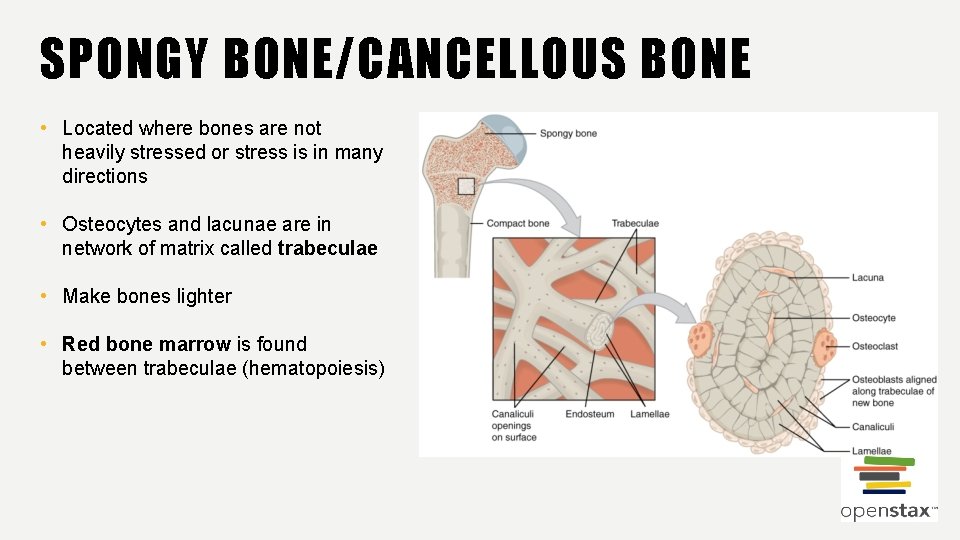
SPONGY BONE/CANCELLOUS BONE • Located where bones are not heavily stressed or stress is in many directions • Osteocytes and lacunae are in network of matrix called trabeculae • Make bones lighter • Red bone marrow is found between trabeculae (hematopoiesis)
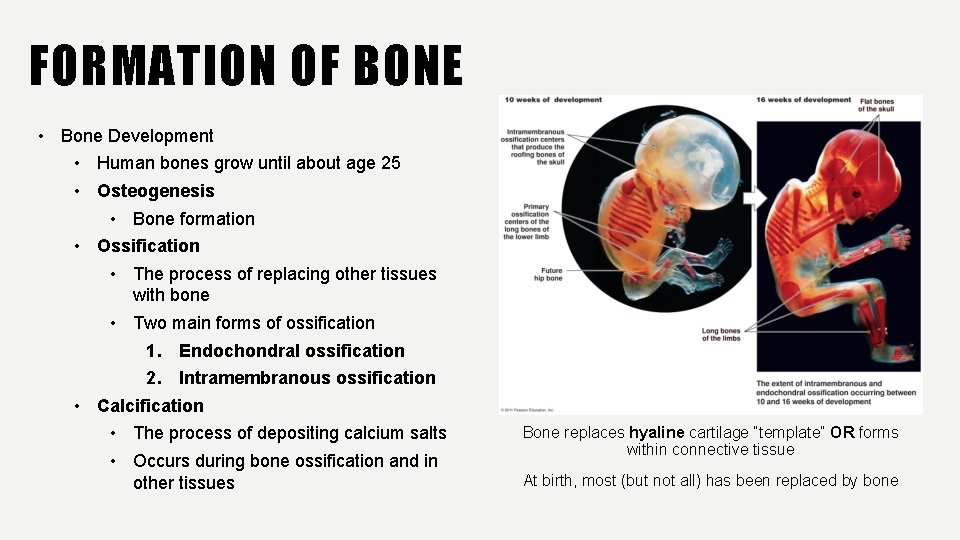
FORMATION OF BONE • Bone Development • Human bones grow until about age 25 • Osteogenesis • Bone formation • Ossification • The process of replacing other tissues with bone • Two main forms of ossification 1. Endochondral ossification 2. Intramembranous ossification • Calcification • The process of depositing calcium salts • Occurs during bone ossification and in other tissues Bone replaces hyaline cartilage “template” OR forms within connective tissue At birth, most (but not all) has been replaced by bone
OSSIFICATION ENDOCHONDRAL OSSIFICATION INTRAMEMBRANOUS OSSIFICATION • Replaces hyaline cartilage w/ bone and lengthens • Mesenchyme (stem) cells transform to osteoblasts in connective tissue • Forms long, short, and irregular bones • Most flat bones of skull, mandible, clavicle • Growth in puberty – Osteoblast activity to outpace chondroblast activity – Epiphyseal plate narrows • Also called dermal ossification because it occurs in the dermis
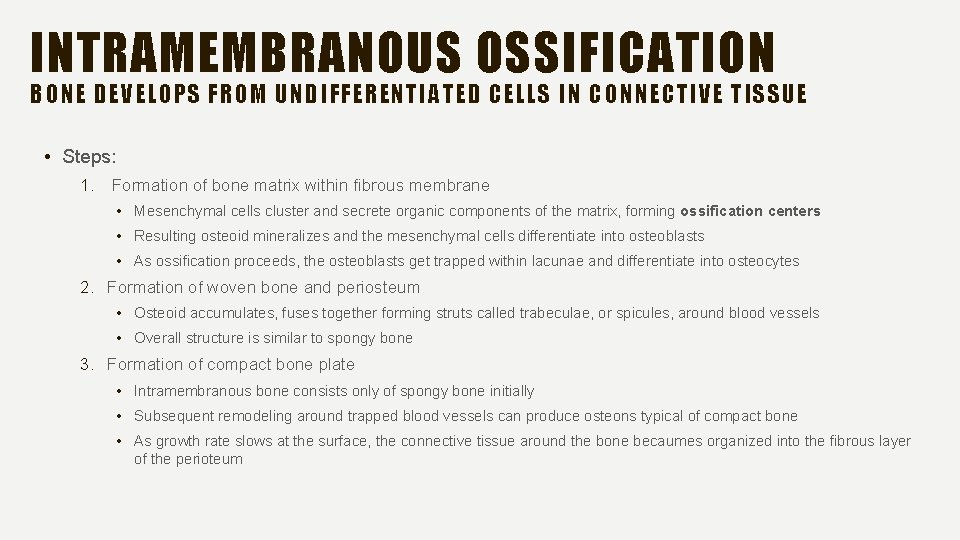
INTRAMEMBRANOUS OSSIFICATION BONE DEVELOPS FROM UNDIFFERENTIATED CELLS IN CONNECTIVE TISSUE • Steps: 1. Formation of bone matrix within fibrous membrane • Mesenchymal cells cluster and secrete organic components of the matrix, forming ossification centers • Resulting osteoid mineralizes and the mesenchymal cells differentiate into osteoblasts • As ossification proceeds, the osteoblasts get trapped within lacunae and differentiate into osteocytes 2. Formation of woven bone and periosteum • Osteoid accumulates, fuses together forming struts called trabeculae, or spicules, around blood vessels • Overall structure is similar to spongy bone 3. Formation of compact bone plate • Intramembranous bone consists only of spongy bone initially • Subsequent remodeling around trapped blood vessels can produce osteons typical of compact bone • As growth rate slows at the surface, the connective tissue around the bone becaumes organized into the fibrous layer of the perioteum
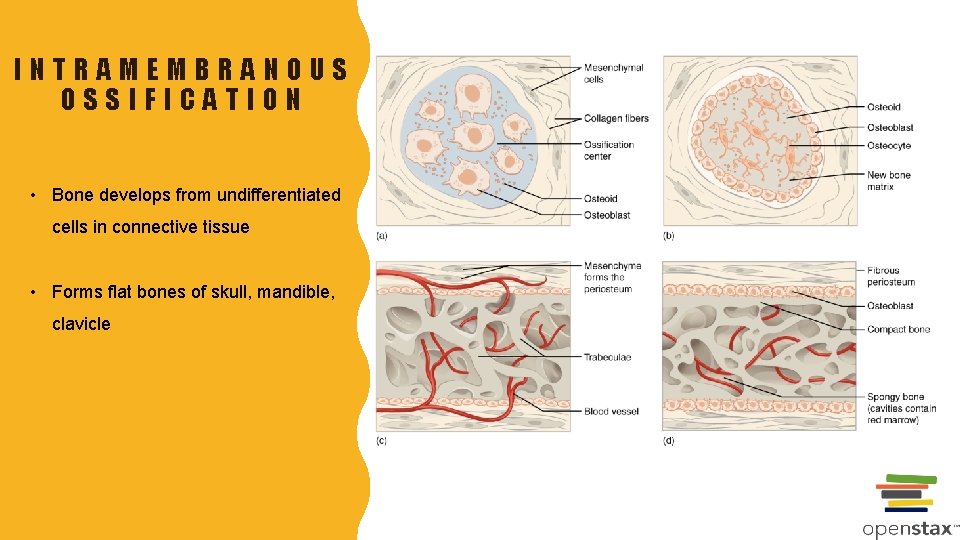
INTRAMEMBRANOUS OSSIFICATION • Bone develops from undifferentiated cells in connective tissue • Forms flat bones of skull, mandible, clavicle
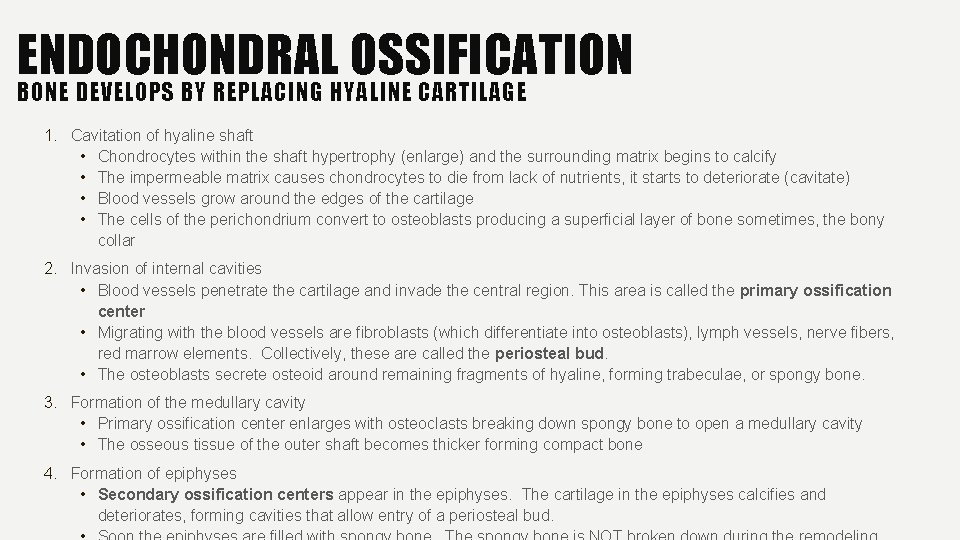
ENDOCHONDRAL OSSIFICATION BONE DEVELOPS BY REPLACING HYALINE CARTILAGE 1. Cavitation of hyaline shaft • Chondrocytes within the shaft hypertrophy (enlarge) and the surrounding matrix begins to calcify • The impermeable matrix causes chondrocytes to die from lack of nutrients, it starts to deteriorate (cavitate) • Blood vessels grow around the edges of the cartilage • The cells of the perichondrium convert to osteoblasts producing a superficial layer of bone sometimes, the bony collar 2. Invasion of internal cavities • Blood vessels penetrate the cartilage and invade the central region. This area is called the primary ossification center • Migrating with the blood vessels are fibroblasts (which differentiate into osteoblasts), lymph vessels, nerve fibers, red marrow elements. Collectively, these are called the periosteal bud. • The osteoblasts secrete osteoid around remaining fragments of hyaline, forming trabeculae, or spongy bone. 3. Formation of the medullary cavity • Primary ossification center enlarges with osteoclasts breaking down spongy bone to open a medullary cavity • The osseous tissue of the outer shaft becomes thicker forming compact bone 4. Formation of epiphyses • Secondary ossification centers appear in the epiphyses. The cartilage in the epiphyses calcifies and deteriorates, forming cavities that allow entry of a periosteal bud.
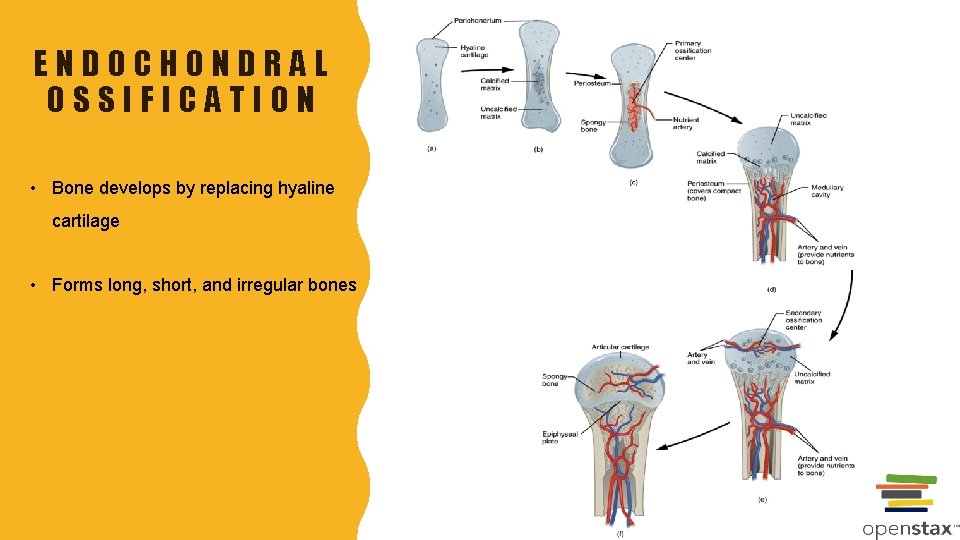
ENDOCHONDRAL OSSIFICATION • Bone develops by replacing hyaline cartilage • Forms long, short, and irregular bones
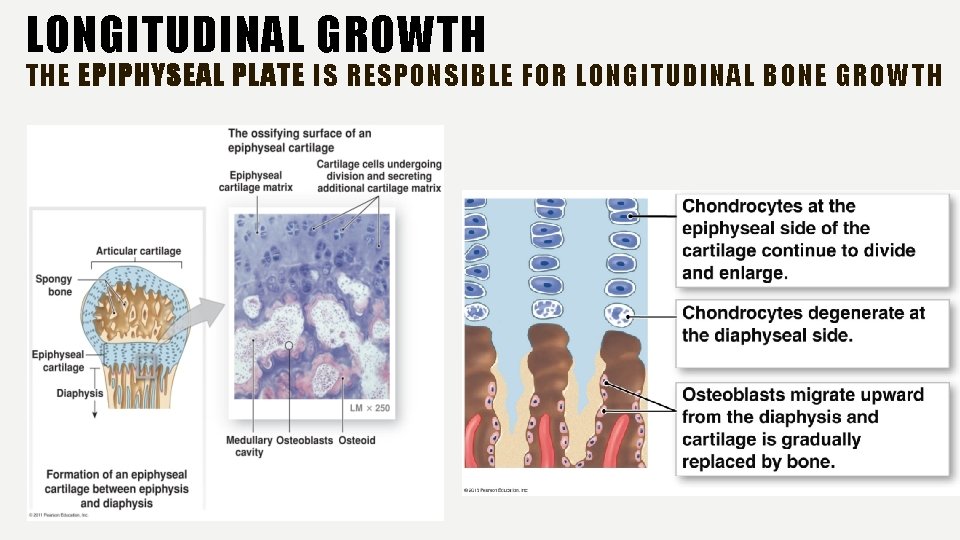
LONGITUDINAL GROWTH THE EPIPHYSEAL PLATE IS RESPONSIBLE FOR LONGITUDINAL BONE GROWTH
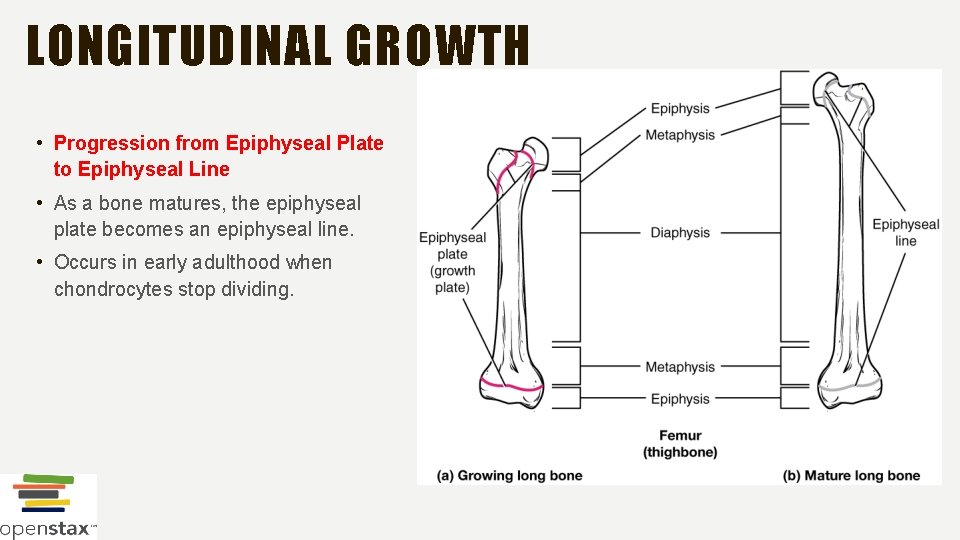
LONGITUDINAL GROWTH • Progression from Epiphyseal Plate to Epiphyseal Line • As a bone matures, the epiphyseal plate becomes an epiphyseal line. • Occurs in early adulthood when chondrocytes stop dividing.
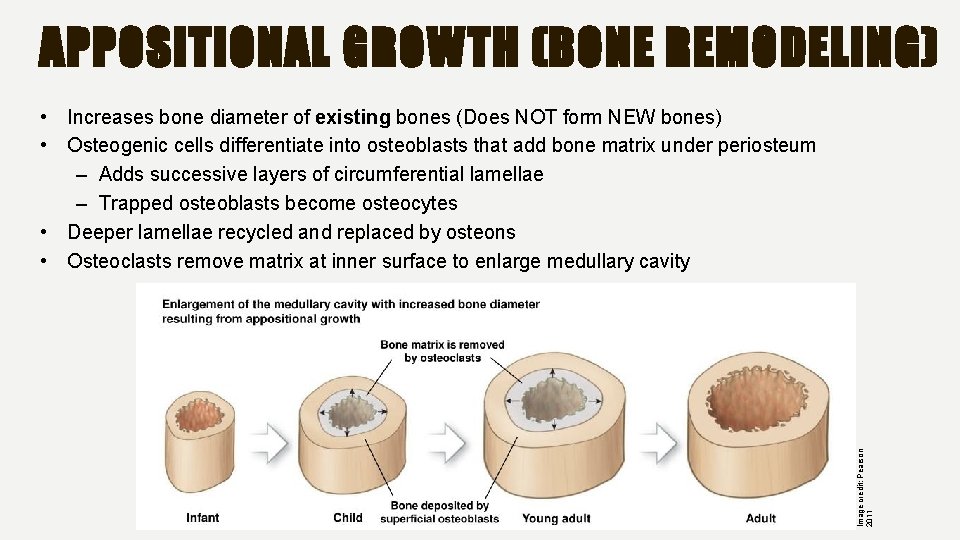
APPOSITIONAL GROWTH (BONE REMODELING) Image credit: Pearson 2011 • Increases bone diameter of existing bones (Does NOT form NEW bones) • Osteogenic cells differentiate into osteoblasts that add bone matrix under periosteum – Adds successive layers of circumferential lamellae – Trapped osteoblasts become osteocytes • Deeper lamellae recycled and replaced by osteons • Osteoclasts remove matrix at inner surface to enlarge medullary cavity
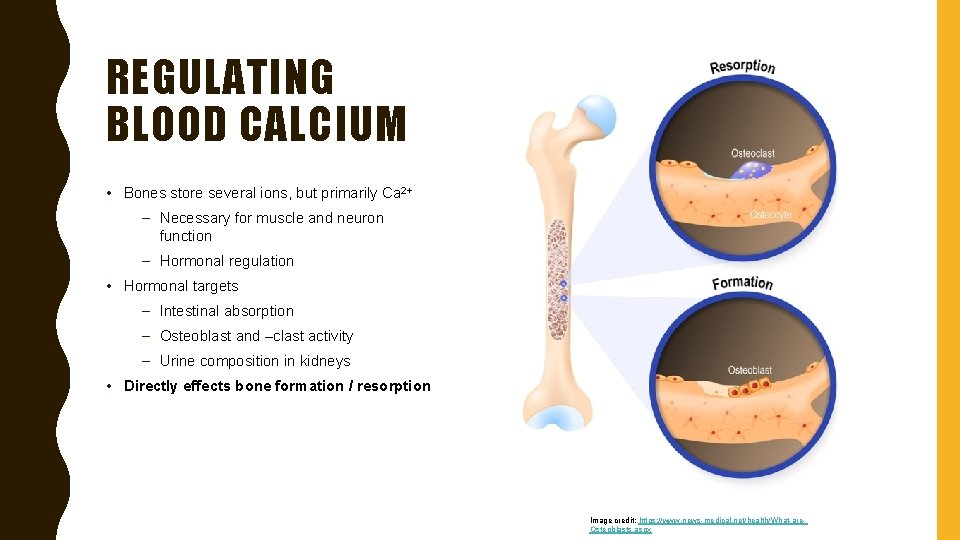
REGULATING BLOOD CALCIUM • Bones store several ions, but primarily Ca 2+ – Necessary for muscle and neuron function – Hormonal regulation • Hormonal targets – Intestinal absorption – Osteoblast and –clast activity – Urine composition in kidneys • Directly effects bone formation / resorption Image credit: https: //www. news-medical. net/health/What-are. Osteoblasts. aspx
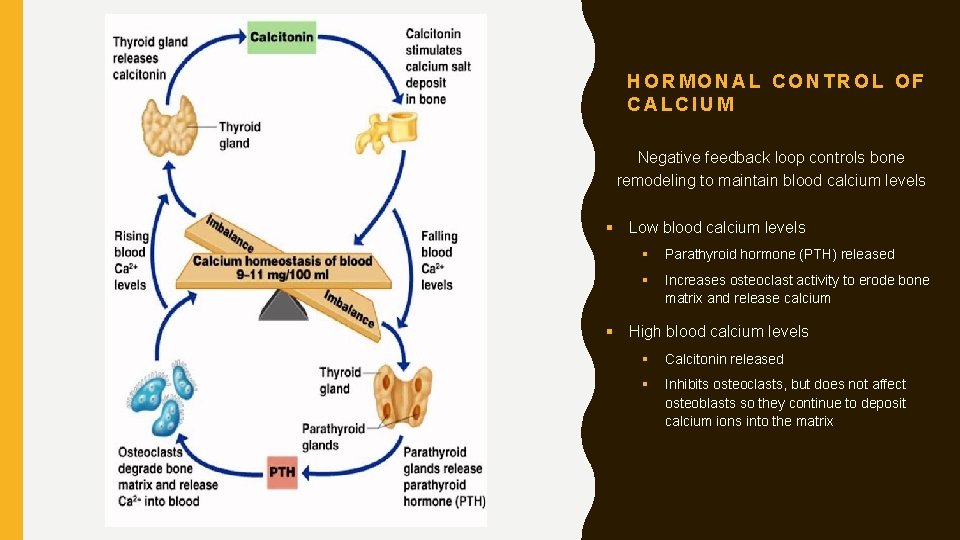
HORMONAL CONTROL OF CALCIUM Negative feedback loop controls bone remodeling to maintain blood calcium levels § Low blood calcium levels § Parathyroid hormone (PTH) released § Increases osteoclast activity to erode bone matrix and release calcium § High blood calcium levels § Calcitonin released § Inhibits osteoclasts, but does not affect osteoblasts so they continue to deposit calcium ions into the matrix
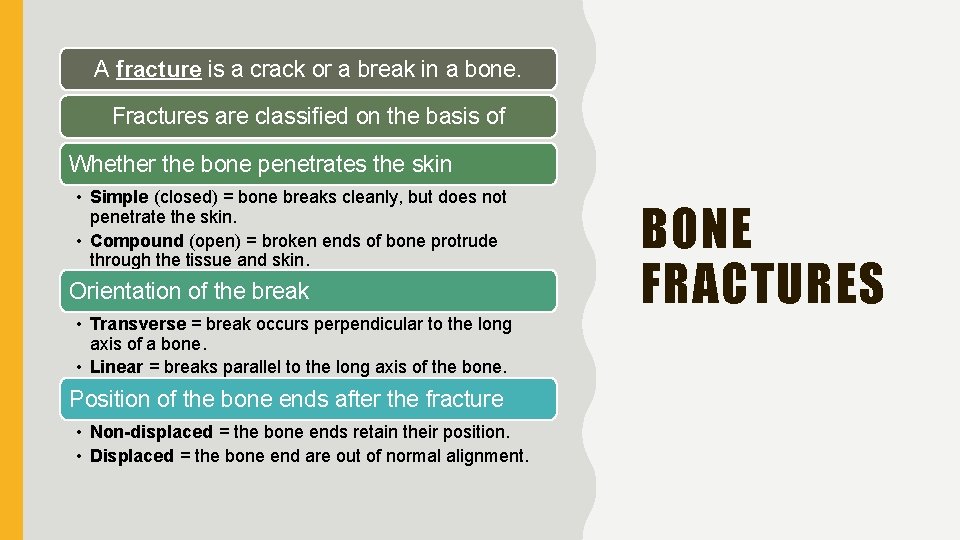
A fracture is a crack or a break in a bone. Fractures are classified on the basis of Whether the bone penetrates the skin • Simple (closed) = bone breaks cleanly, but does not penetrate the skin. • Compound (open) = broken ends of bone protrude through the tissue and skin. Orientation of the break • Transverse = break occurs perpendicular to the long axis of a bone. • Linear = breaks parallel to the long axis of the bone. Position of the bone ends after the fracture • Non-displaced = the bone ends retain their position. • Displaced = the bone end are out of normal alignment. BONE FRACTURES
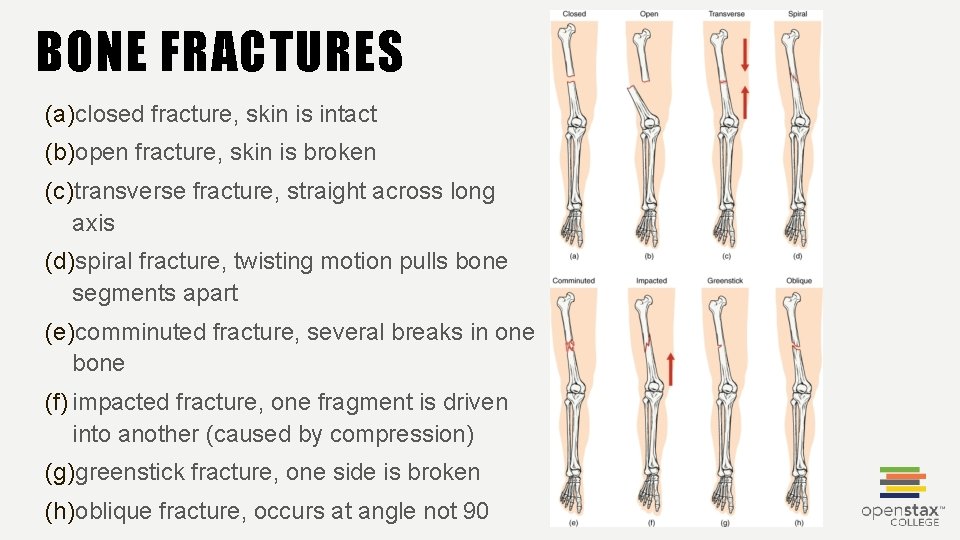
BONE FRACTURES (a)closed fracture, skin is intact (b)open fracture, skin is broken (c)transverse fracture, straight across long axis (d)spiral fracture, twisting motion pulls bone segments apart (e)comminuted fracture, several breaks in one bone (f) impacted fracture, one fragment is driven into another (caused by compression) (g)greenstick fracture, one side is broken (h)oblique fracture, occurs at angle not 90
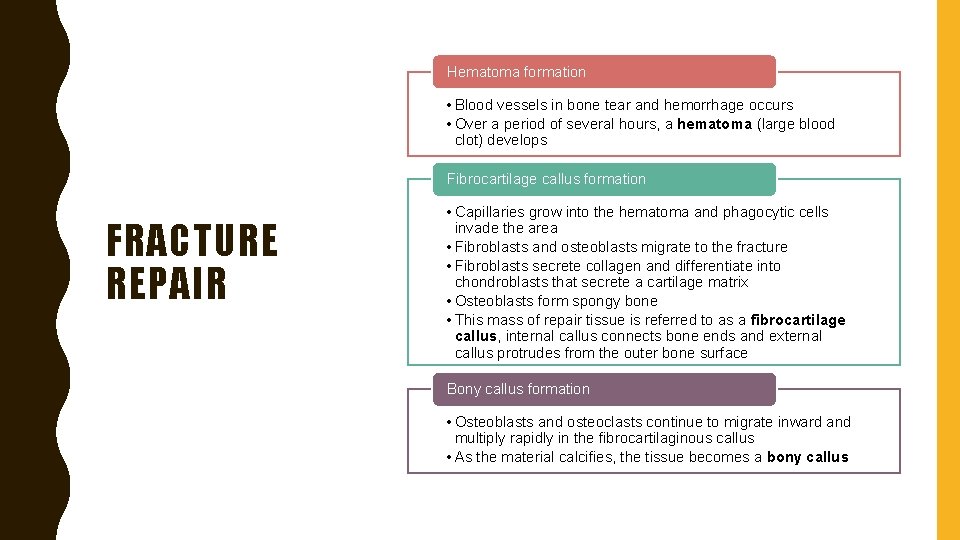
Hematoma formation • Blood vessels in bone tear and hemorrhage occurs • Over a period of several hours, a hematoma (large blood clot) develops Fibrocartilage callus formation FRACTURE REPAIR • Capillaries grow into the hematoma and phagocytic cells invade the area • Fibroblasts and osteoblasts migrate to the fracture • Fibroblasts secrete collagen and differentiate into chondroblasts that secrete a cartilage matrix • Osteoblasts form spongy bone • This mass of repair tissue is referred to as a fibrocartilage callus, internal callus connects bone ends and external callus protrudes from the outer bone surface Bony callus formation • Osteoblasts and osteoclasts continue to migrate inward and multiply rapidly in the fibrocartilaginous callus • As the material calcifies, the tissue becomes a bony callus
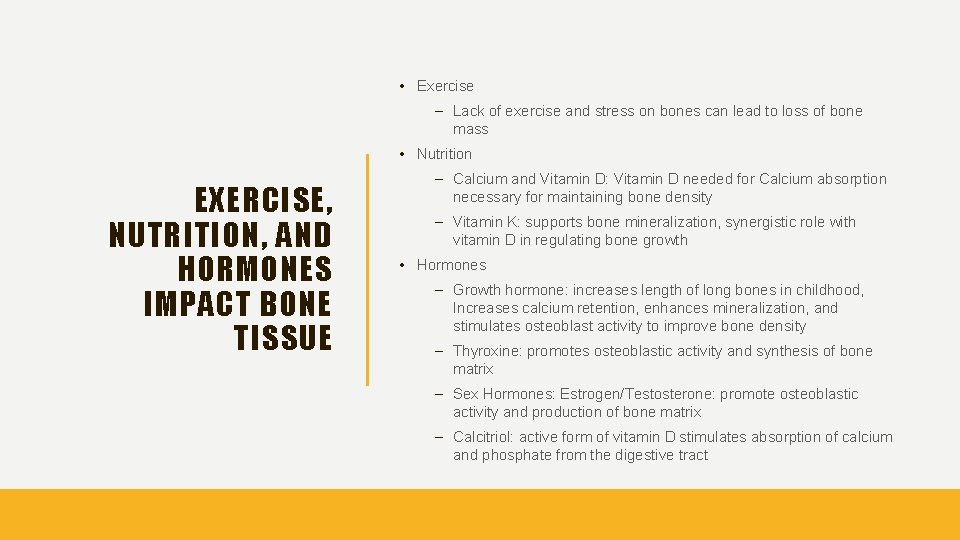
• Exercise – Lack of exercise and stress on bones can lead to loss of bone mass • Nutrition EXERCISE, NUTRITION, AND HORMONES IMPACT BONE TISSUE – Calcium and Vitamin D: Vitamin D needed for Calcium absorption necessary for maintaining bone density – Vitamin K: supports bone mineralization, synergistic role with vitamin D in regulating bone growth • Hormones – Growth hormone: increases length of long bones in childhood, Increases calcium retention, enhances mineralization, and stimulates osteoblast activity to improve bone density – Thyroxine: promotes osteoblastic activity and synthesis of bone matrix – Sex Hormones: Estrogen/Testosterone: promote osteoblastic activity and production of bone matrix – Calcitriol: active form of vitamin D stimulates absorption of calcium and phosphate from the digestive tract
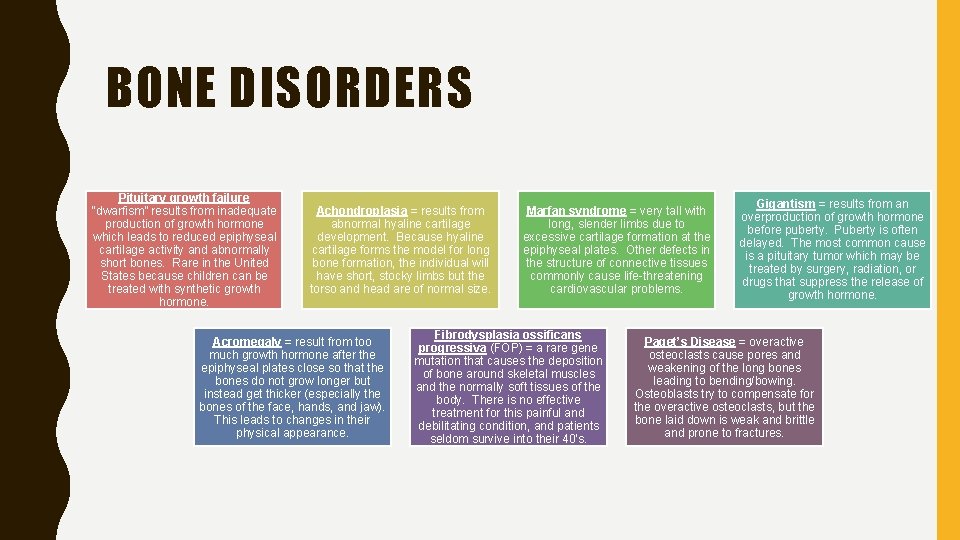
BONE DISORDERS Pituitary growth failure “dwarfism” results from inadequate production of growth hormone which leads to reduced epiphyseal cartilage activity and abnormally short bones. Rare in the United States because children can be treated with synthetic growth hormone. Achondroplasia = results from abnormal hyaline cartilage development. Because hyaline cartilage forms the model for long bone formation, the individual will have short, stocky limbs but the torso and head are of normal size. Acromegaly = result from too much growth hormone after the epiphyseal plates close so that the bones do not grow longer but instead get thicker (especially the bones of the face, hands, and jaw). This leads to changes in their physical appearance. Marfan syndrome = very tall with long, slender limbs due to excessive cartilage formation at the epiphyseal plates. Other defects in the structure of connective tissues commonly cause life-threatening cardiovascular problems. Fibrodysplasia ossificans progressiva (FOP) = a rare gene mutation that causes the deposition of bone around skeletal muscles and the normally soft tissues of the body. There is no effective treatment for this painful and debilitating condition, and patients seldom survive into their 40’s. Gigantism = results from an overproduction of growth hormone before puberty. Puberty is often delayed. The most common cause is a pituitary tumor which may be treated by surgery, radiation, or drugs that suppress the release of growth hormone. Paget’s Disease = overactive osteoclasts cause pores and weakening of the long bones leading to bending/bowing. Osteoblasts try to compensate for the overactive osteoclasts, but the bone laid down is weak and brittle and prone to fractures.
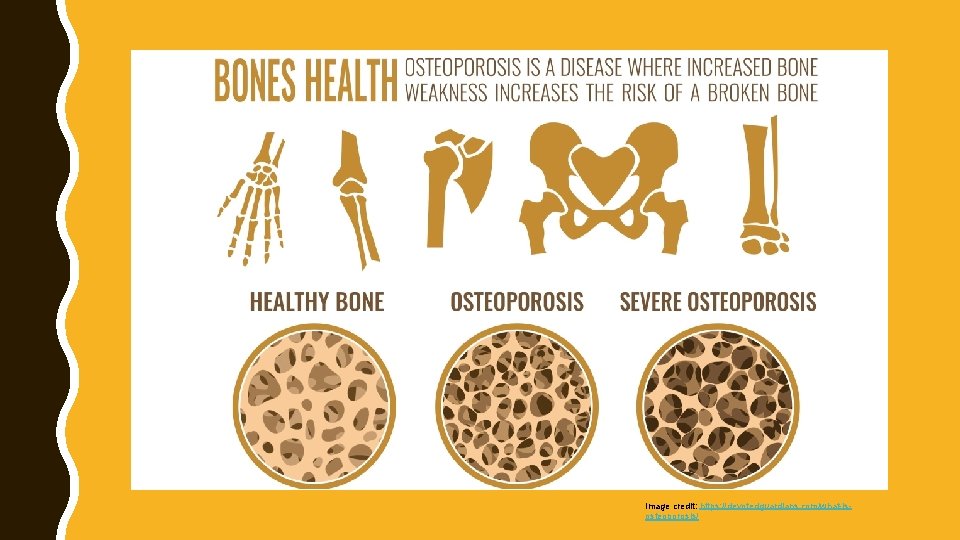
Image credit: https: //devotedguardians. com/what-isosteoporosis/
- Slides: 29