OSPAP Programme Cardiovascular system Slide 1 of 53









- Slides: 53
OSPAP Programme Cardiovascular system Slide 1 of 53 Cardiovascular System
Cardinal Symptoms Chest Pain (discomfort) Breathlessness Ankle Swelling (Oedema) Syncope/dizziness Slide 2 of 53 Cardiovascular System Palpitations Leg Pain (Intermittent Claudication)
Differential Diagnosis of Chest Pain • Central vs non-central • Exertional vs non-exertional • General vs localised • Specific exacerbations – – – Slide 3 of 53 Ischaemic Pleuritic Dyspeptic Musculoskeletal Anxiety Cardiovascular System
Chest Pain • Cardiac – Crushing, central, tightness – Radiation – jaw, teeth, arms, back, throat • Angina – Precipitated by exertion, emotion, cold, after a meal – Relieved by rest, G. T. N. – Duration less than 15 minutes Slide 4 of 53 Cardiovascular System
Chest Pain View any discomfort in the front or back of the chest precipitated by exertion and relieved by rest as highly suspicious Myocardial infarction – Like angina but NOT relieved by rest or G. T. N. – Associated with pallor, sweating, vomiting, hypotension, tachycardia, bradycardia, arrhythmia Slide 5 of 53 Cardiovascular System

Breathlessness (dyspnoea) • What does the patient mean? How long have they been short of breath? Do they normally get short of breath? Has it got worse recently? Did it come on suddenly or gradually? What were they doing at the time? Is there anything that makes it better or worse? Do they get short of breath on lying flat? How many pillows do they sleep on? (Orthopnoea) • Do they ever wake up in the middle of the night feeling breathless? (Paroxysmal Nocturnal Dyspnoea) • • Slide 6 of 53 Cardiovascular System
Cardiac causes of breathlessness • Mitral stenosis • Chronic Heart Failure – Associated with orthopnoea (dyspnoea worse on lying) – Paroxysmal nocturnal dyspnoea Slide 7 of 53 Cardiovascular System
Palpitations • • • An awareness of heart beating Extra systoles Paroxysmal tachycardia Atrial fibrillation Regular or irregular Fast or slow Slide 8 of 53 Cardiovascular System
Palpitations Any specific precipitating factors Any associated features: – chest pain – dyspnoea – dizziness – collapse (syncope) Any manoeuvres that terminate palpitation Slide 9 of 53 Cardiovascular System
Claudication • Chronic ischaemia due to atherosclerosis – Chief feature is intermittent claudication – Cramping pain is felt in the calf or buttock on walking – Signs, absent pulses, cold white legs Slide 10 of 53 Cardiovascular System
Claudication • • • Pain in the calves on walking? Tell me about it How far What helps Impact on lifestyle Slide 11 of 53 Cardiovascular System
Ankle swelling/Oedema May be a symptom of heart failure Usually bilateral and symmetrical Worse in evening, best first thing in the morning With severe failure may extend up the leg to include thigh, genitalia and lower abdomen • In the bed bound patient oedema may be evident over the sacrum • May have associated breathlessness, tiredness, weakness • • Slide 12 of 53 Cardiovascular System
Causes of ankle swelling • Bilateral oedema implies systemic disease with increased venous pressure (right heart failure) or reduced intravascular pressure (reduced albumin e. g. liver failure, malnutrition, malabsorption) • Pitting vs non-pitting • Unilateral oedema ? DVT Slide 13 of 53 Cardiovascular System
Syncope • Syncope is a transient loss of consciousness due to cerebral anoxia, often due to reduced cerebral circulation. • May occur as a result of cardiovascular disease – postural hypotension – cardiac rhythm abnormalities – valve disease – carotid or vertebro-basilar arterial disease Slide 14 of 53 Cardiovascular System
Syncope • Cardiac or CNS causes • Vasovagal syncope – Provoked by emotion, pain, fear or standing for too long due to reflex bradycardia and peripheral vasodilation • Situation syncope – Provoked by cough or effort • Stokes-adams attacks – Transient arrhythmias causing reduced cardiac output and loss of consciousness Slide 15 of 53 Cardiovascular System
Syncope • • • Tell me about the faints or funny turns? How often? When? How long? Reactions of observers? Slide 16 of 53 Cardiovascular System
Past Medical History • • • Angina or previous M. I. Hypertension Hyperlipidaemia Rheumatic Fever Diabetes Mellitus Slide 17 of 53 Cardiovascular System
Family History • • • Any heart problems in the family Myocardial infarction / sudden death Angina Hypertension Hyperlipidaemia Diabetes Mellitus Slide 18 of 53 Cardiovascular System

Social History • • Smoking Alcohol Impact on occupation Diet Slide 19 of 53 Cardiovascular System
Risk Factors for Coronary Heart Disease Fixed Age Male Sex Family History Slide 20 of 53 Cardiovascular System Modifiable Hypertension Dyslipidaemias Obesity Physical Inactivity Pro-coagulant state Smoking
The ECG Slide 21 of 53 Cardiovascular System
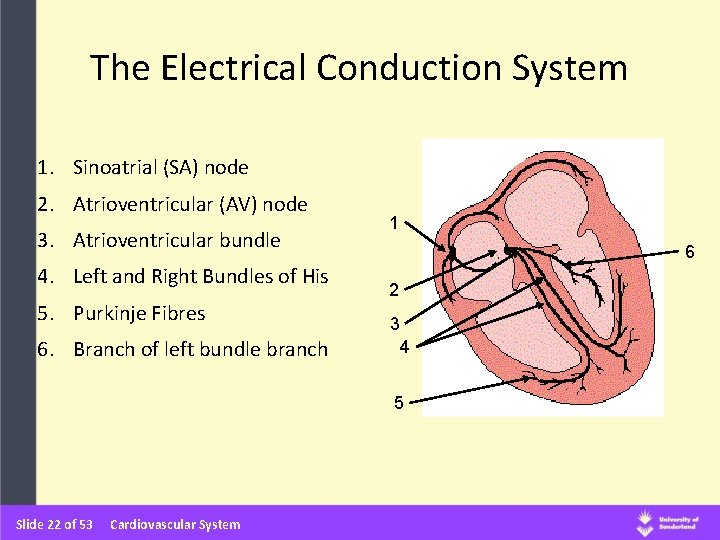
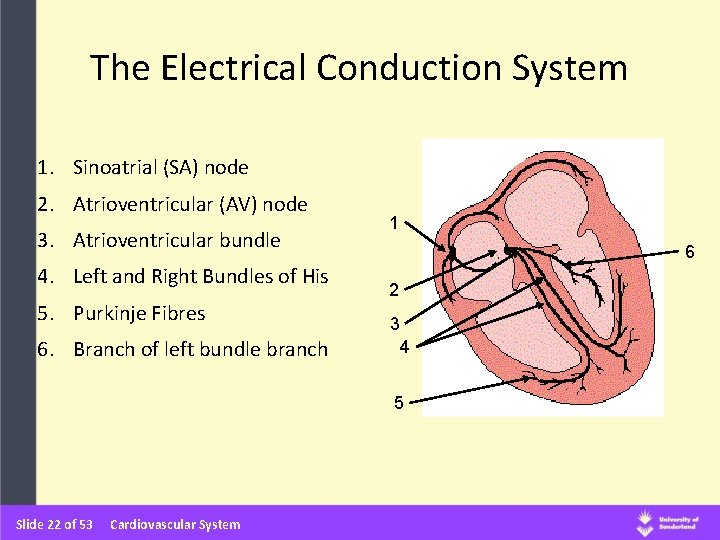
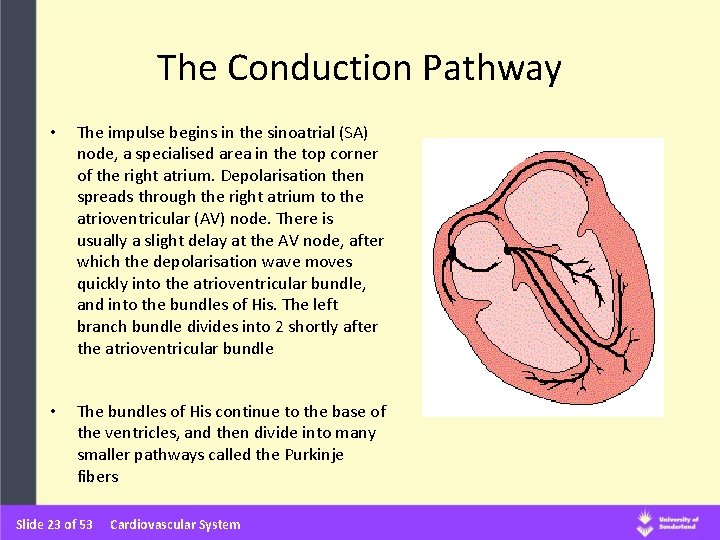
The Electrical Conduction System 1. Sinoatrial (SA) node 2. Atrioventricular (AV) node 3. Atrioventricular bundle 4. Left and Right Bundles of His 5. Purkinje Fibres 6. Branch of left bundle branch 1 6 2 3 4 5 Slide 22 of 53 Cardiovascular System
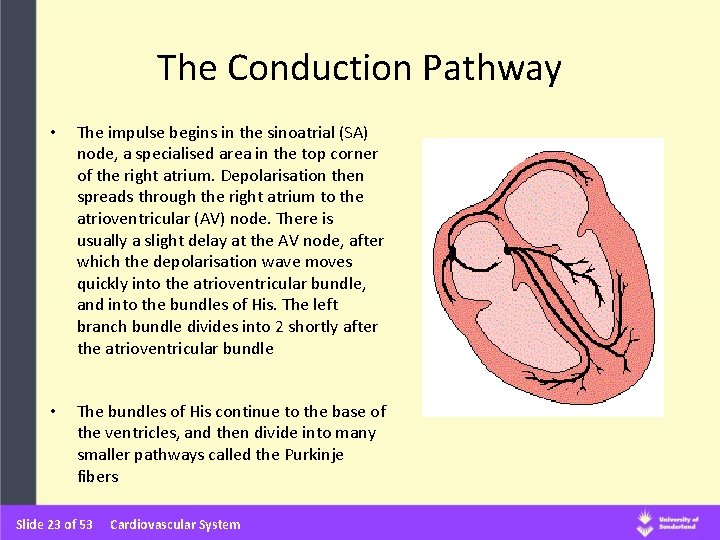
The Conduction Pathway • The impulse begins in the sinoatrial (SA) node, a specialised area in the top corner of the right atrium. Depolarisation then spreads through the right atrium to the atrioventricular (AV) node. There is usually a slight delay at the AV node, after which the depolarisation wave moves quickly into the atrioventricular bundle, and into the bundles of His. The left branch bundle divides into 2 shortly after the atrioventricular bundle • The bundles of His continue to the base of the ventricles, and then divide into many smaller pathways called the Purkinje fibers Slide 23 of 53 Cardiovascular System

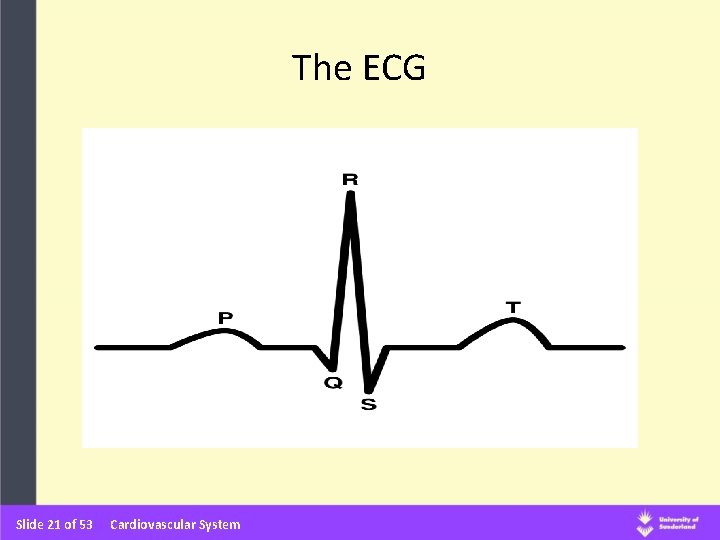
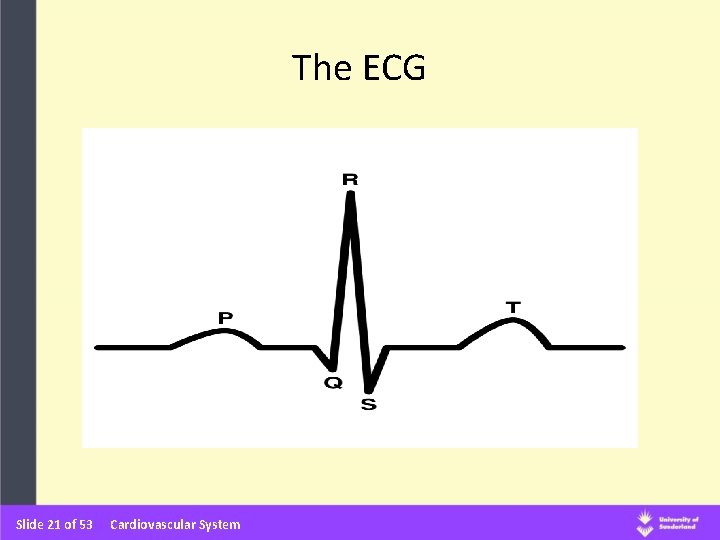
“PQRST” Slide 24 of 53 Cardiovascular System
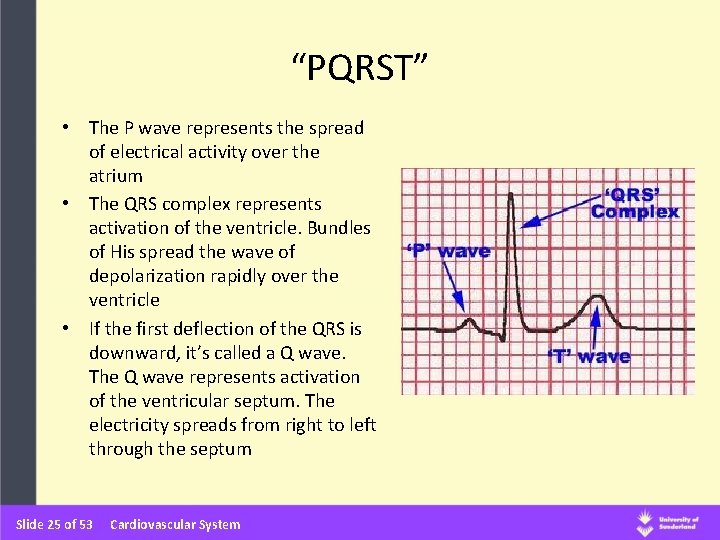
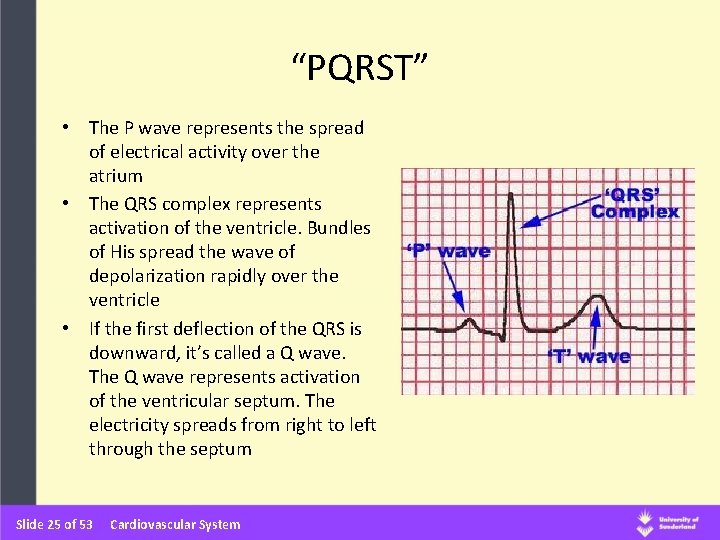
“PQRST” • The P wave represents the spread of electrical activity over the atrium • The QRS complex represents activation of the ventricle. Bundles of His spread the wave of depolarization rapidly over the ventricle • If the first deflection of the QRS is downward, it’s called a Q wave. The Q wave represents activation of the ventricular septum. The electricity spreads from right to left through the septum Slide 25 of 53 Cardiovascular System
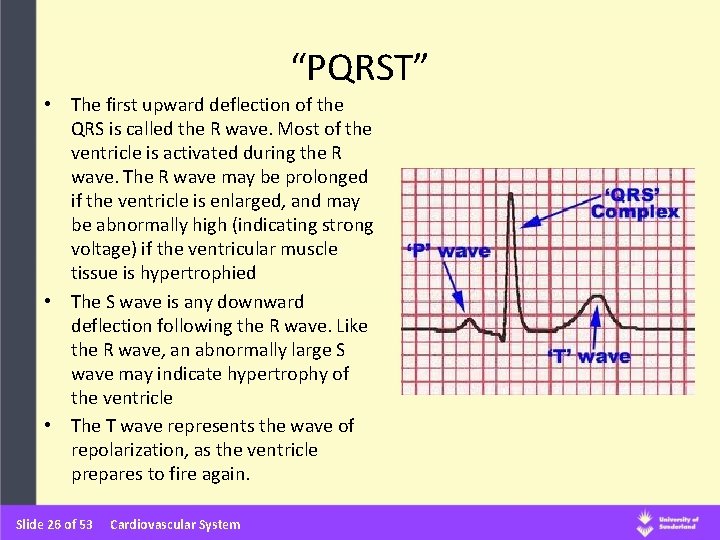
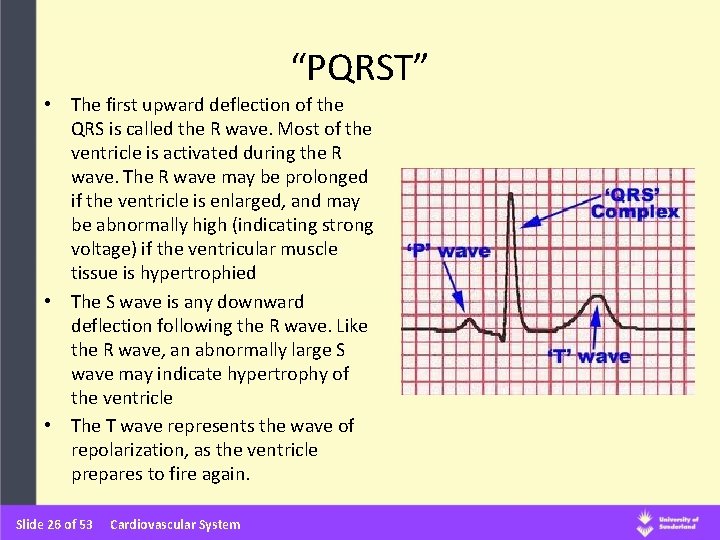
“PQRST” • The first upward deflection of the QRS is called the R wave. Most of the ventricle is activated during the R wave. The R wave may be prolonged if the ventricle is enlarged, and may be abnormally high (indicating strong voltage) if the ventricular muscle tissue is hypertrophied • The S wave is any downward deflection following the R wave. Like the R wave, an abnormally large S wave may indicate hypertrophy of the ventricle • The T wave represents the wave of repolarization, as the ventricle prepares to fire again. Slide 26 of 53 Cardiovascular System

12 Lead ECG Slide 27 of 53 Cardiovascular System
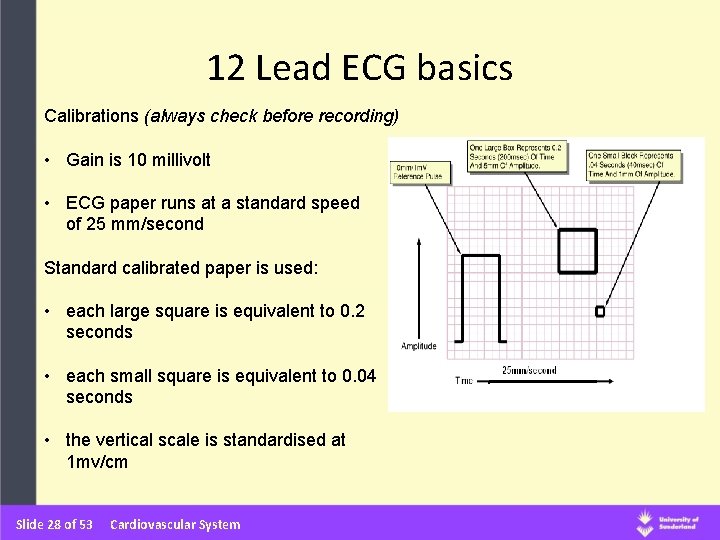
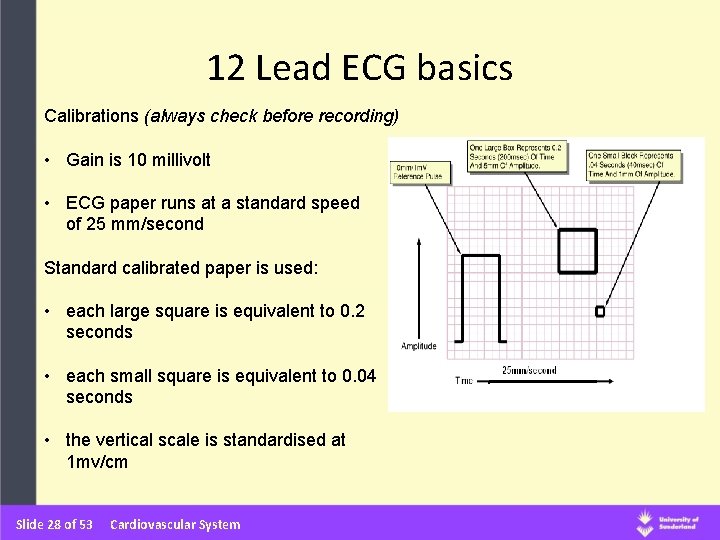
12 Lead ECG basics Calibrations (always check before recording) • Gain is 10 millivolt • ECG paper runs at a standard speed of 25 mm/second Standard calibrated paper is used: • each large square is equivalent to 0. 2 seconds • each small square is equivalent to 0. 04 seconds • the vertical scale is standardised at 1 mv/cm Slide 28 of 53 Cardiovascular System
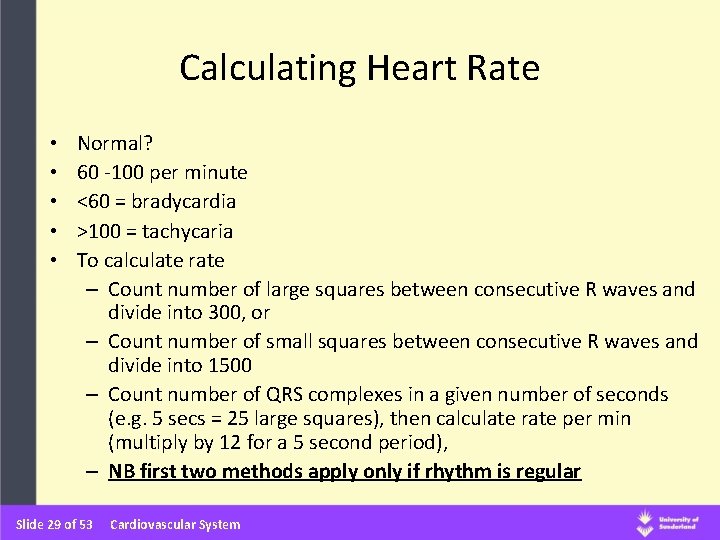
Calculating Heart Rate • • • Normal? 60 -100 per minute <60 = bradycardia >100 = tachycaria To calculate rate – Count number of large squares between consecutive R waves and divide into 300, or – Count number of small squares between consecutive R waves and divide into 1500 – Count number of QRS complexes in a given number of seconds (e. g. 5 secs = 25 large squares), then calculate rate per min (multiply by 12 for a 5 second period), – NB first two methods apply only if rhythm is regular Slide 29 of 53 Cardiovascular System
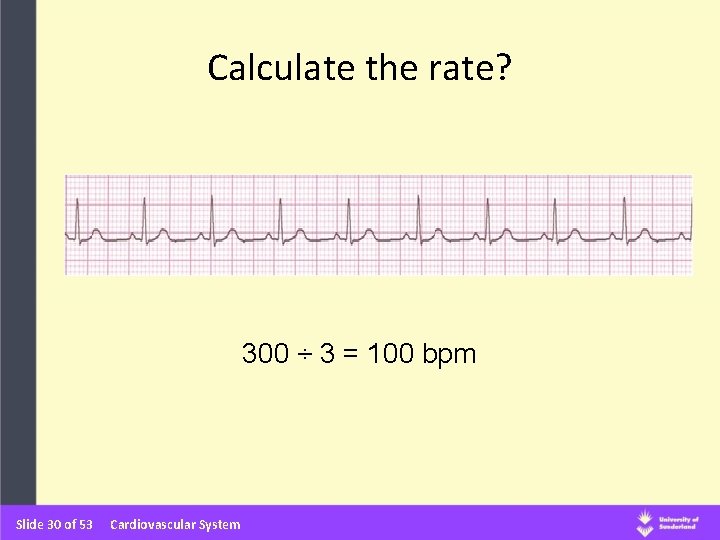
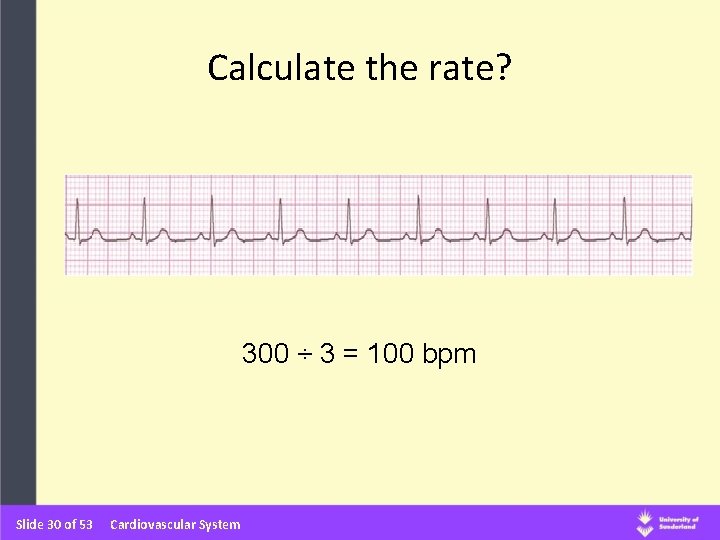
Calculate the rate? 300 ÷ 3 = 100 bpm Slide 30 of 53 Cardiovascular System
Clinical examination of the cardiovascular system Structure: • • Inspection Palpation Percussion Auscultation Slide 31 of 53 Cardiovascular System
Inspection General Appearance • Colour • Sweating • Respiration Rate / Distress • Trauma • Surgical Scars (sternotomy, thoracotomy etc) • Environmental Factors (heart monitor, GTN etc) • Obesity / Cachexia • Marfanoid Features (high arched palate) • Pallor Slide 32 of 53 Cardiovascular System
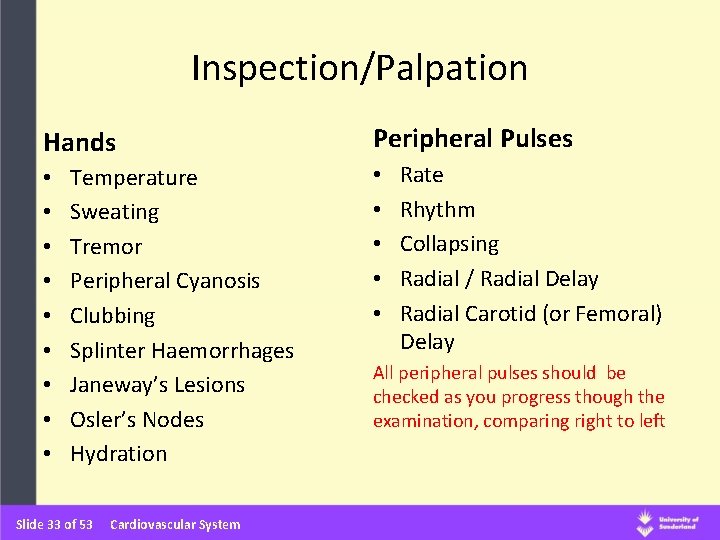
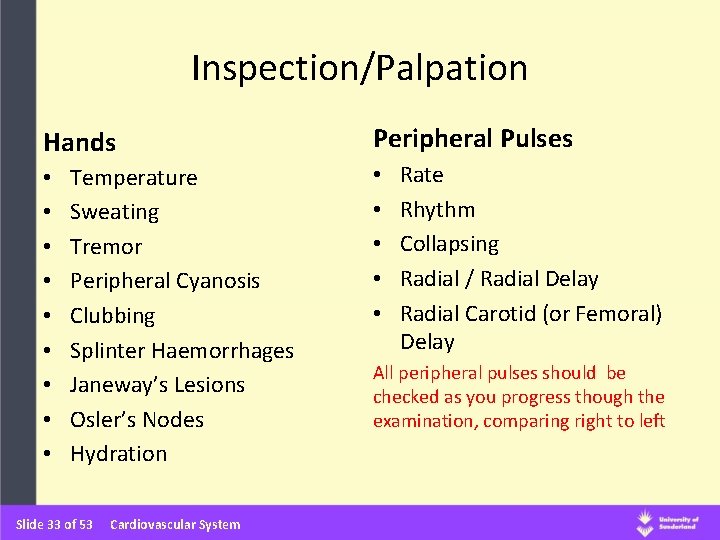
Inspection/Palpation Hands • • • Temperature Sweating Tremor Peripheral Cyanosis Clubbing Splinter Haemorrhages Janeway’s Lesions Osler’s Nodes Hydration Slide 33 of 53 Cardiovascular System Peripheral Pulses • • • Rate Rhythm Collapsing Radial / Radial Delay Radial Carotid (or Femoral) Delay All peripheral pulses should be checked as you progress though the examination, comparing right to left
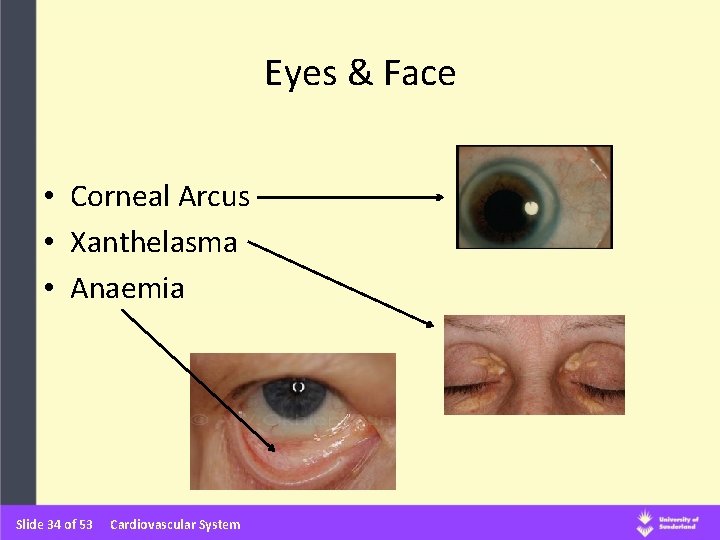
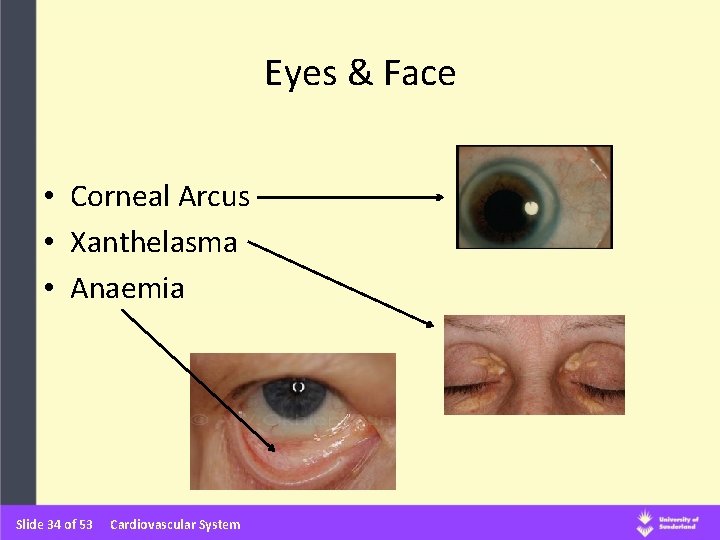
Eyes & Face • Corneal Arcus • Xanthelasma • Anaemia Slide 34 of 53 Cardiovascular System
Mouth • Central Cyanosis • Peripheral Cyanosis • Hydration • Dentition • Palate Anatomy • Petechial Haemorrhage Slide 35 of 53 Cardiovascular System
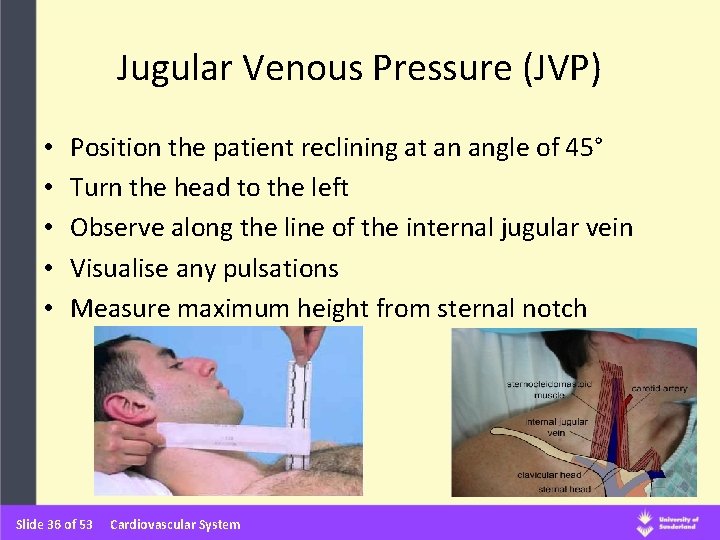
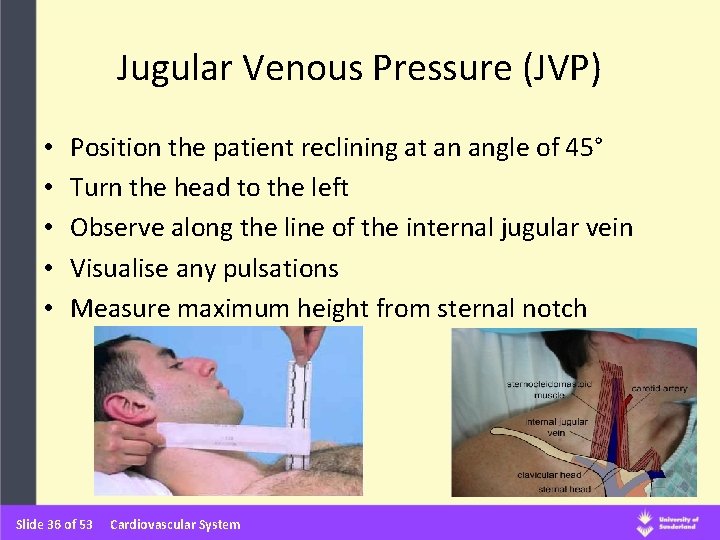
Jugular Venous Pressure (JVP) • • • Position the patient reclining at an angle of 45° Turn the head to the left Observe along the line of the internal jugular vein Visualise any pulsations Measure maximum height from sternal notch Slide 36 of 53 Cardiovascular System
Palpation • Pre-Cordium – Apex beat – Other palpable impulses • Heave at the left sternal edge (LSE) in right ventricular hypertrophy • Left ventricular heave at apex • Thrill - a palpable murmur (atrial enlargement) – Chest wall tenderness Slide 37 of 53 Cardiovascular System

Apex Beat • Normal position 5 th Intercostal space Mid-Clavicular Line • To find the apex beat - place flat of hand on chest wall, with palm over 5 th ICS MCL and index finger placed laterally along 4 th space, middle along 5 th space and ring along 6 th space • Gradually bring tips of fingers medially until you feel the beat • Normally a short, sharp impulse • Forceful, sustained heave in left ventricular hypertrophy • Impalpable apex beat – Obesity (most commonly) – Emphysema (chest over-inflated) – Pericardial effusion Slide 38 of 53 Cardiovascular System
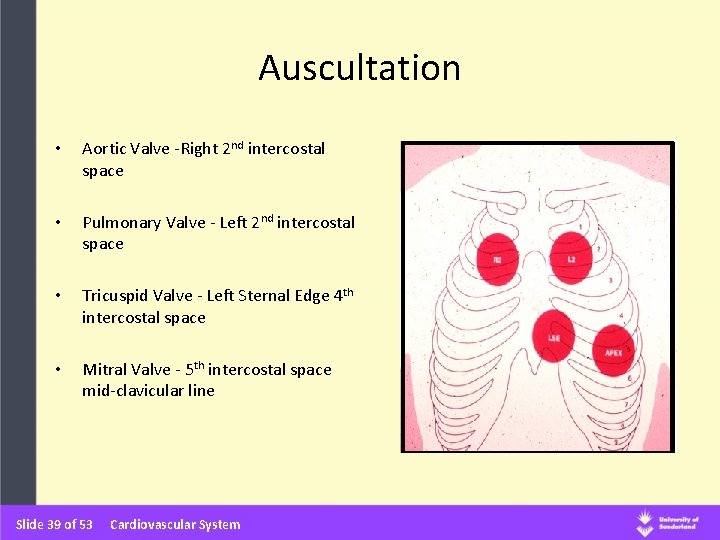
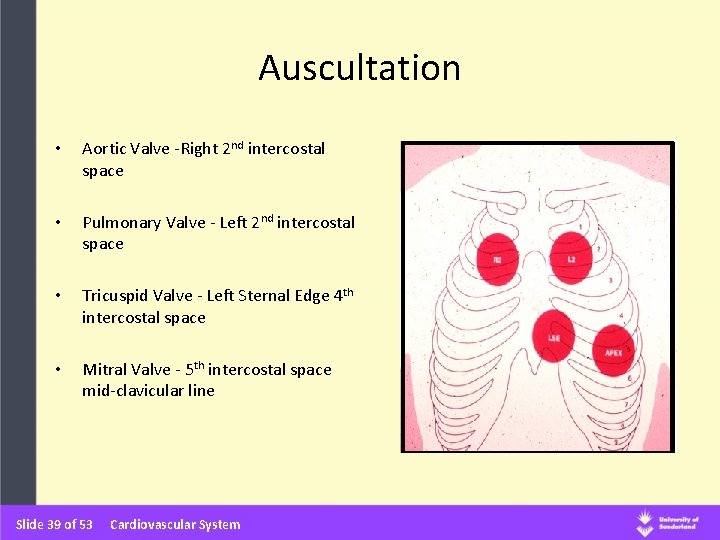
Auscultation • Aortic Valve -Right 2 nd intercostal space • Pulmonary Valve - Left 2 nd intercostal space • Tricuspid Valve - Left Sternal Edge 4 th intercostal space • Mitral Valve - 5 th intercostal space mid-clavicular line Slide 39 of 53 Cardiovascular System
Auscultatory Technique • Palpate the APEX with the patient at 450 • Auscultate the APEX with the bell & diaphragm • Auscultate LSE and with bell & diaphram (time with pulse) • Auscultate R 2 ICS • Auscultate L 2 ICS • Get patient to sit forward exhale and hold breath - Auscultate at LSE and APEX Slide 40 of 53 Cardiovascular System
1 st and 2 nd Heart Sounds • When the heart goes into systole (contraction), the pressure in the ventricles increases and causes the mitral (left atrial valve) and tricuspid (right atrial valve) valves to close (1 st heart sound), At the same time the aortic and pulmonary valves open • Non-diseased valves do not make a noise when they open • The 1 st heart sound can be identified by palpating a central arterial pulse (ideally the carotid) during auscultation • On or about the systolic pulse the 1 st heart sound will be audible Slide 41 of 53 Cardiovascular System
1 st and 2 nd Heart Sounds • The heart then goes into diastole (relaxation) and the resulting drop in pressure causes the aortic and pulmonary vales to close • The pitch of the sound is different and they are often recognised as `LUB` and `DUB` • S 1 and S 2 are considered to be discrete sounds, remember that each is created by the near-instantaneous closing of two separate valves • For the most part, it is enough to consider that these sounds are single and instantaneous Slide 42 of 53 Cardiovascular System
Finally! • • • Sacral Oedema Ankle Oedema Peripheral Pulses (Dorsalis Pedis / Posterior Tibial) Temperature Hair Distribution Varicouse Veins Ulcers (arterial / venous) Skin colour and Tone Petechial Haemorrhages Slide 43 of 53 Cardiovascular System
Blood Pressure Slide 44 of 53 Cardiovascular System
The pressure exerted by the blood against the walls of the blood vessels. (The most simple indicator of haemodynamic well-being) Slide 45 of 53 Cardiovascular System mm Hg
Physiological Factors Affecting Blood Pressure • The pumping action of the heart • The amount of resistance to the blood within the circulation - systemic vascular resistance / peripheral resistance (relates to the diameter of the blood vessels) • The volume of the blood • The viscosity of the blood • Elasticity of the arteries Slide 46 of 53 Cardiovascular System

Determinants of Blood Pressure BLOOD PRESSURE = Cardiac output x Systemic Vascular Resistance CO x SVR Mean Arterial Blood Pressure (MAP) = systolic BP + (diastolic x 2) 3 Slide 47 of 53 Cardiovascular System
Definitions • Hypertension: – Systolic > 140 mm. Hg – Diastolic > 90 mm. Hg either/or • Hypotension: – Systolic < 90 mm. Hg – Diastolic < 60 m. Hg either/or Blood Pressure Association Slide 52 of 53 Cardiovascular System
Factors To Consider • When to take a blood pressure (white coat hypertension)? • How often should the BP be recorded ? • What is “normal” for each individual patient ? • When should I be concerned ? • When do I need to summon help? • Who shall I call ? Slide 48 of 53 Cardiovascular System
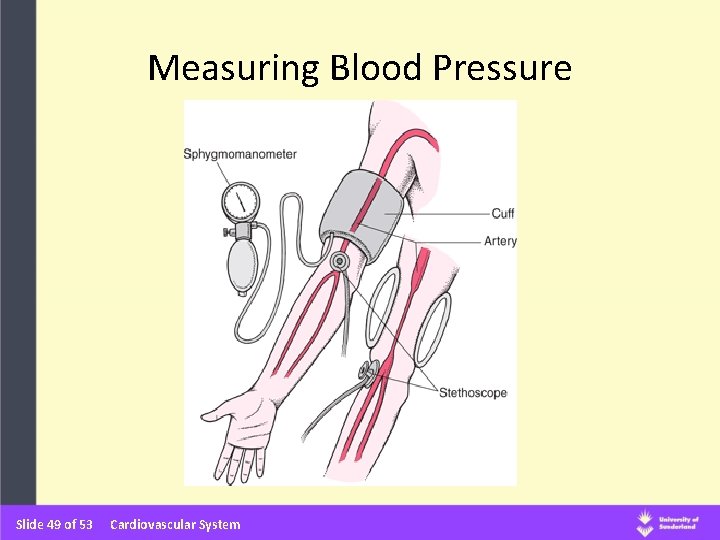
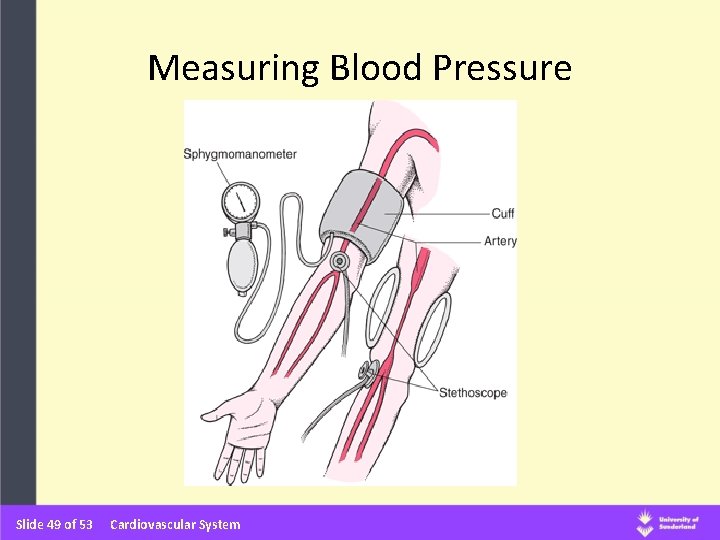
Measuring Blood Pressure Slide 49 of 53 Cardiovascular System

Korotkoff’s Sounds Phase 1 -The first appearance of faint clear tapping sounds which gradually increase in intensity. The systolic pressure is heard for at least two consecutive beats, and this correlates well with intra-arterial pressure. Phase 2 -The softening of sounds, which may become swishing. Phase 3 -The return of sharper sounds, which become crisper but never fully regain the intensity of phase 1 sounds. (Neither phase 2 nor phase 3 has any known clinical importance). Phase 4 -The distinct abrupt muffling of sounds, which become soft and blowing. Phase 5 -The point at which all sounds disappear completely. http: //www. abdn. ac. uk/medical/bhs/tutorial/q 1. htm Slide 51 of 53 Cardiovascular System

Examination Sequence • Ensure patient is rested and comfortable (seated if possible) • Support patient’s arm at about the level of the heart (either arm can be used unless otherwise indicated) • Apply the cuff to the upper arm • Palpate brachial/radial artery • Inflate the cuff until the pulse is impalpable (rough estimate of systolic) • Inflate cuff 10 -20 mm. Hg further • Place stethoscope over brachial artery • Deflate cuff slowly (2 -3 mm. Hg/sec) until regular sounds are heard – systolic pressure (Korotkoff’s sound Phase 1) • Continue to deflate cuff until sounds disappear completely – diastolic pressure (Korotkoff’s sound Phase 5) Slide 50 of 53 Cardiovascular System

Slide 53 of 53 Cardiovascular System