OSCE Revision Respiratory Mark Woodhead Honorary Clinical Professor







- Slides: 30

OSCE Revision Respiratory Mark Woodhead Honorary Clinical Professor of Respiratory Medicine
BREATHLESSNESS • Respiratory
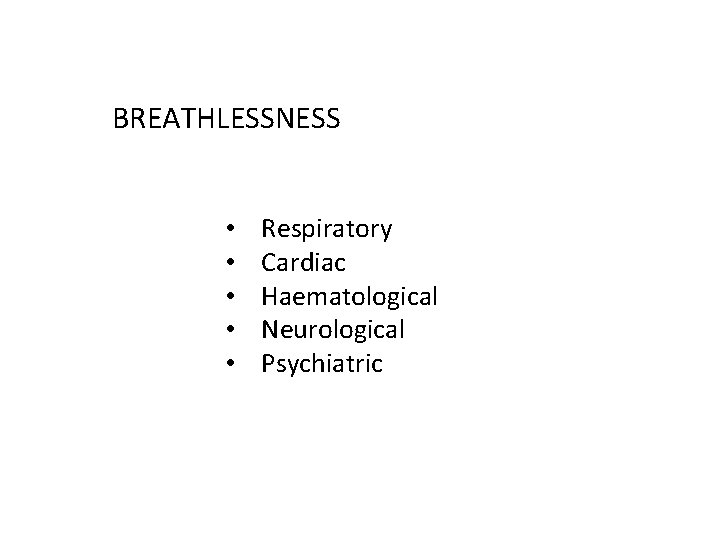
BREATHLESSNESS • • • Respiratory Cardiac Haematological Neurological Psychiatric

BREATHLESSNESS Pattern Age / duration Precipitants and relievers Severity Associated symptoms Exacerbations
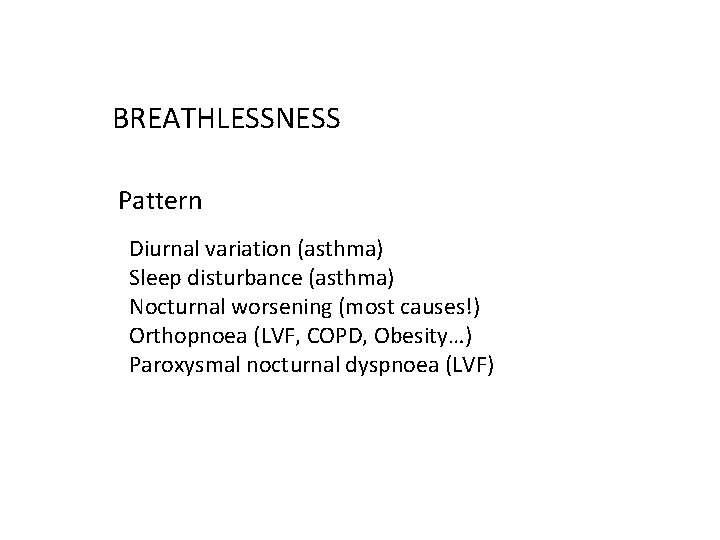
BREATHLESSNESS Pattern Diurnal variation (asthma) Sleep disturbance (asthma) Nocturnal worsening (most causes!) Orthopnoea (LVF, COPD, Obesity…) Paroxysmal nocturnal dyspnoea (LVF)
BREATHLESSNESS Age / duration Age < 30 - asthma, bronchiectasis, psychological (COPD unlikely) Age > 50 - COPD, (asthma), cardiac Present since childhood asthma (bronchiectasis) Present only since 40 s - COPD Recent onset – pneumonia, PVTE, pneumothorax Non-smoker – asthma, Smoker – (asthma) or COPD
BREATHLESSNESS Precipitants and relievers Worse in summer – asthma Worse in winter – most things! Animals, specific irritants – asthma Occupation – specific sensitiser (asthma) or just effort? Risks for PVTE Effort – most causes
BREATHLESSNESS Severity At rest (talking) Effort – how much, distance, stairs ADLs Work Exacerbations – frequency, times in hospital, ever ICU
BREATHLESSNESS Associated symptoms Sputum > 3/12 of year, in consecutive years – COPD, bronchiectasis, asthma Large volume sputum – bronchiectasis Haemoptysis – bronchiectasis, cancer, PVTE Anorexia and weight loss – cancer Ankle swelling – not asthma, cardiac, cor pulmonale Unilateral leg swelling – PVTE Fever, rigors, purulent sputum – pneumonia Pleuritic chest pain – pneumonia, PVTE, pneumothorax
BREATHLESSNESS Exacerbations Yes – asthma, COPD, bronchiectasis Frequency and severity…. .

CHEST PAIN • Respiratory
CHEST PAIN • • Respiratory Cardiac Musculoskeletal Gastrointestinal
CHEST PAIN Site Central – most things Lateral – pneumonia, PVTE, pneumothorax, musculoskeletal Radiation – arm – cardiac - back – most things
CHEST PAIN Type / precipitants Constant / intermittent Effort related – cardiac Pleuritic – pneumonia, PVTE, pneumothorax, musculoskeletal Movement eg arm – musculoskeletal Meals - GI
BRONCHODILATOR THERAPY Concepts of Prevention and regular vs red/brown inhalers LABA, corticosteroid, anti-muscarinic, combinations Relief as required use Blue vs SABA (LABA – formoterol)
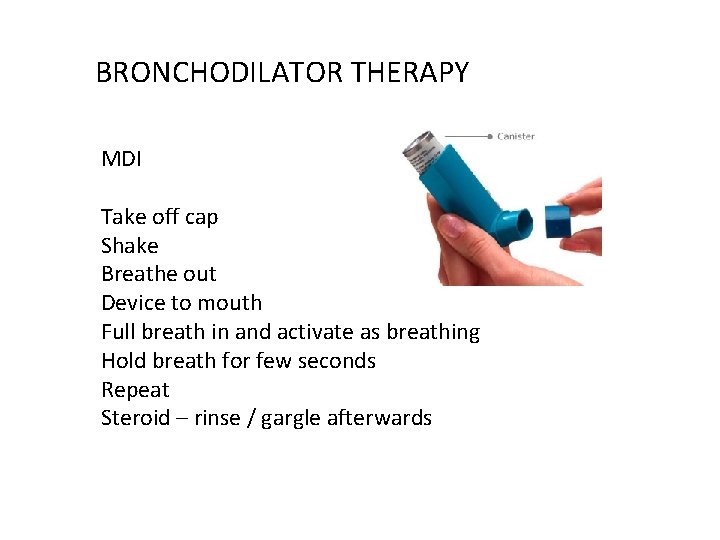
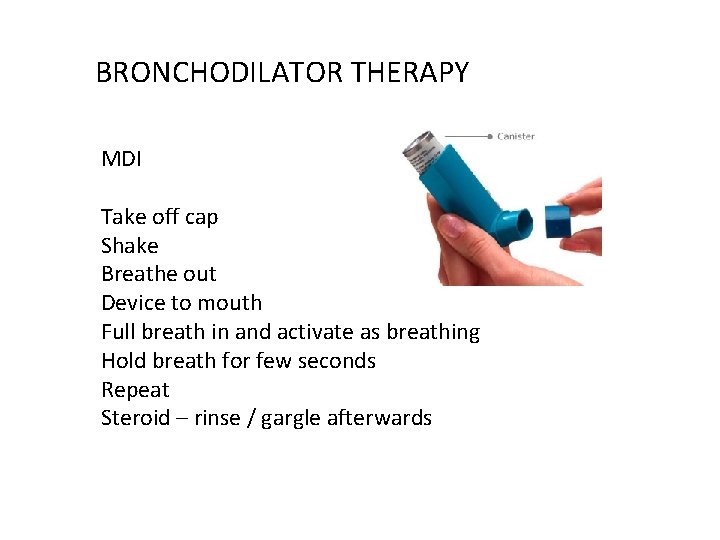
BRONCHODILATOR THERAPY MDI Take off cap Shake Breathe out Device to mouth Full breath in and activate as breathing Hold breath for few seconds Repeat Steroid – rinse / gargle afterwards
LONG TERM CORTICOSTEROID THERAPY Benefits – disease control Harms – dose and duration Short term – hunger, dyspepsia, insomnia, acne Long term – weight gain, hypertension, diabetes, pneumonia osteoporosis, skin thinning, cataracts Balance benefit vs harm, aim for lowest effective dose
EXAMINATION

EXAMINATION - PNEUMONECTOMY Affected side Thoracotomy scar Reduced movement / expansion Dull to percussion VF up or down Reduced breath sounds Mediastinum towards the affected side (trachea, apex beat) Differential pleural effusion – mediastinum away from affected side
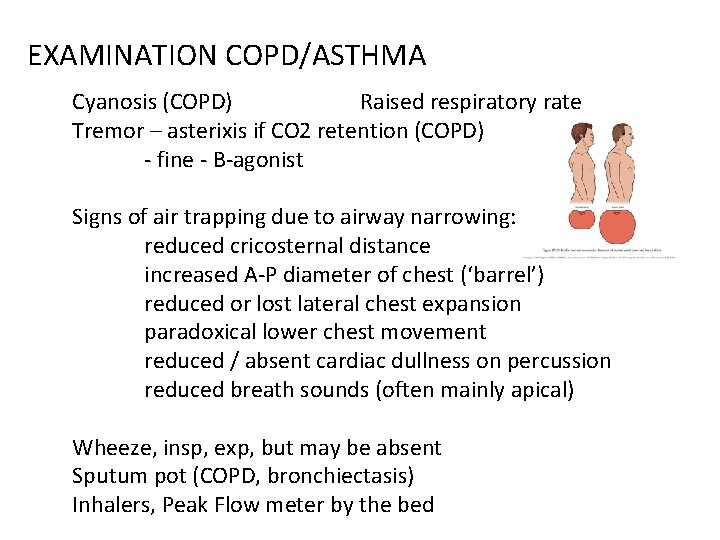
EXAMINATION COPD/ASTHMA Cyanosis (COPD) Raised respiratory rate Tremor – asterixis if CO 2 retention (COPD) - fine - B-agonist Signs of air trapping due to airway narrowing: reduced cricosternal distance increased A-P diameter of chest (‘barrel’) reduced or lost lateral chest expansion paradoxical lower chest movement reduced / absent cardiac dullness on percussion reduced breath sounds (often mainly apical) Wheeze, insp, exp, but may be absent Sputum pot (COPD, bronchiectasis) Inhalers, Peak Flow meter by the bed
EXAMINATION PULMONARY FIBROSIS Finger clubbing (50%) Cyanosis (if severe) Raised respiratory rate Reduced chest expansion (‘restriction’) Persistent, bi-basal, fine, late inspiratory crackles
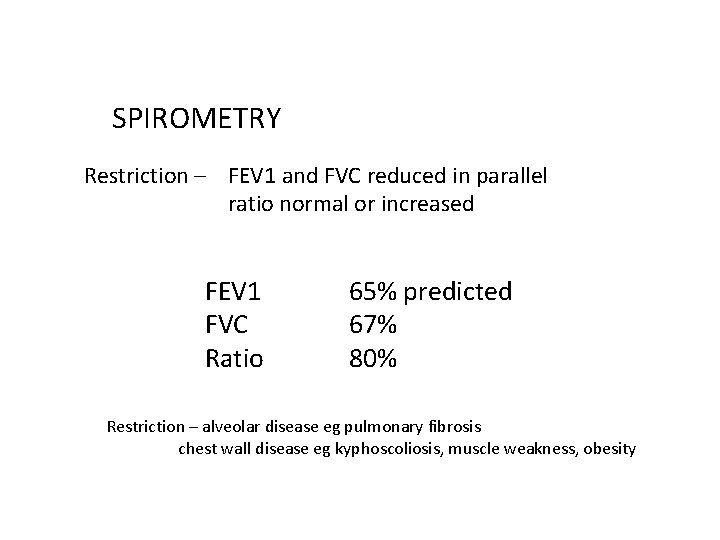
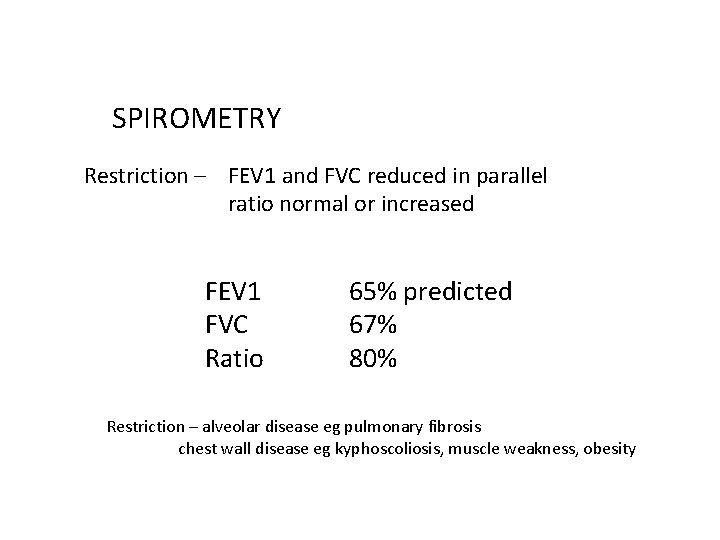
SPIROMETRY Restriction – FEV 1 and FVC reduced in parallel ratio normal or increased FEV 1 FVC Ratio 65% predicted 67% 80% Restriction – alveolar disease eg pulmonary fibrosis chest wall disease eg kyphoscoliosis, muscle weakness, obesity

SPIROMETRY Obstruction – FEV 1 reduced more than FVC ratio less than 70% FEV 1 FVC Ratio 65% predicted 80% 64% Obstruction – airway diseases eg asthma, COPD, bronchiectasis
BLOOD GASES Always look at p. H first normal means normal or compensation has occurred PO 2 cannot be interpreted without Fi. O 2
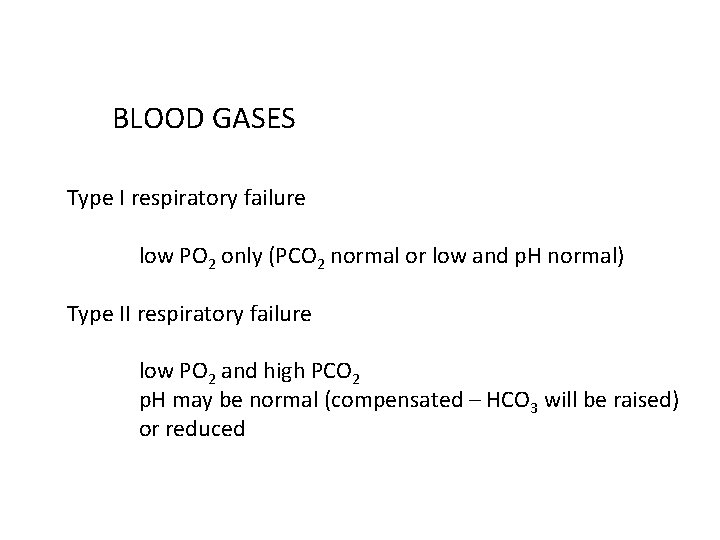
BLOOD GASES Type I respiratory failure low PO 2 only (PCO 2 normal or low and p. H normal) Type II respiratory failure low PO 2 and high PCO 2 p. H may be normal (compensated – HCO 3 will be raised) or reduced
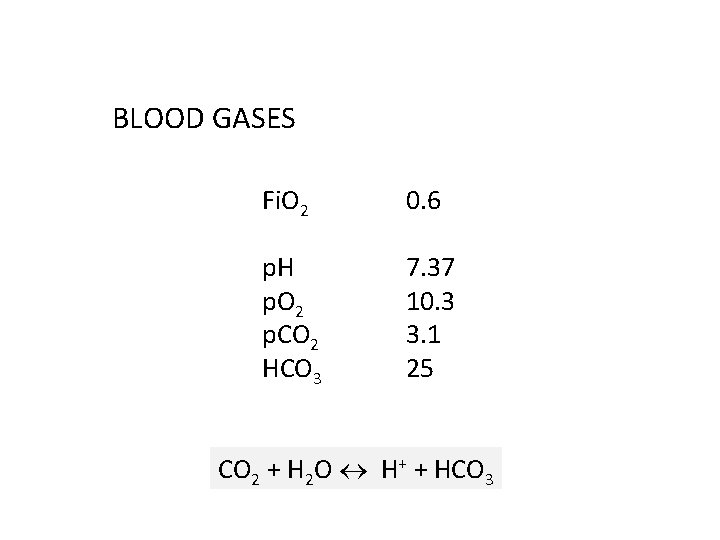
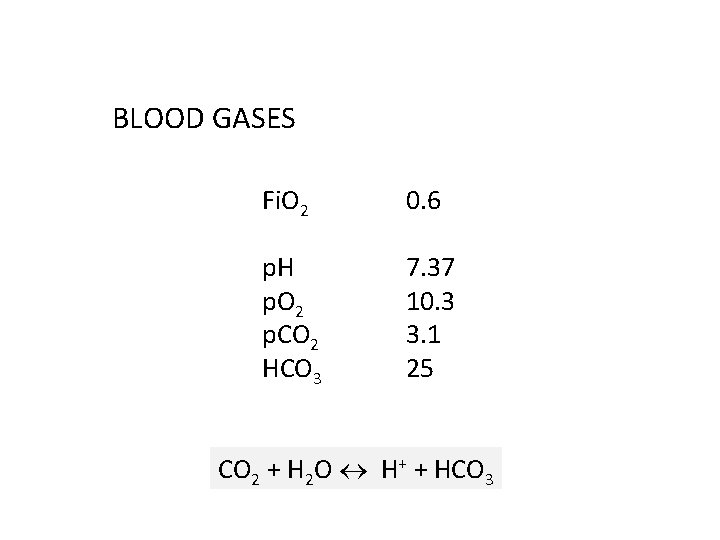
BLOOD GASES Fi. O 2 0. 6 p. H p. O 2 p. CO 2 HCO 3 7. 37 10. 3 3. 1 25 CO 2 + H 2 O H+ + HCO 3
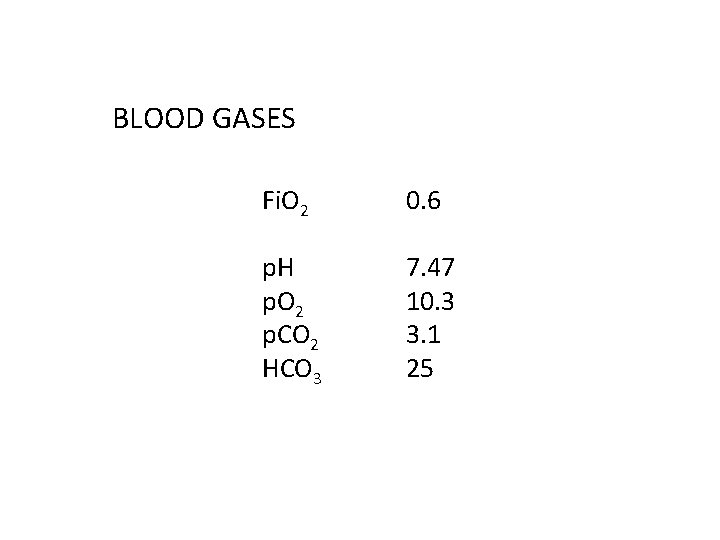
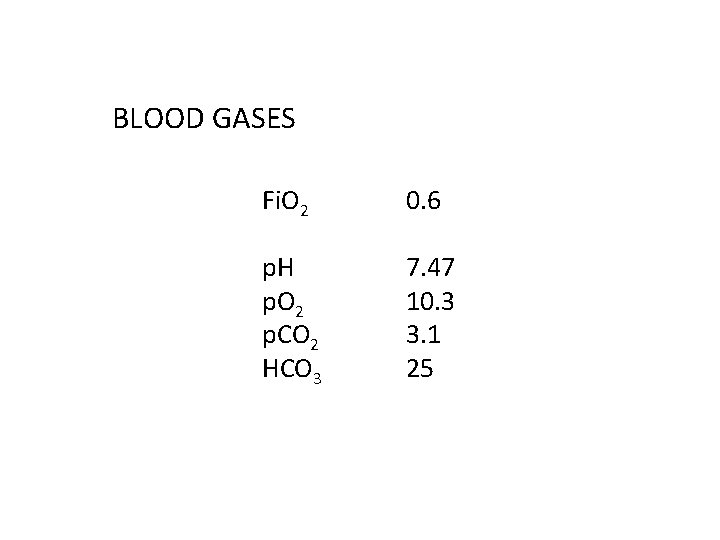
BLOOD GASES Fi. O 2 0. 6 p. H p. O 2 p. CO 2 HCO 3 7. 47 10. 3 3. 1 25

BLOOD GASES Fi. O 2 0. 28 p. H p. O 2 p. CO 2 HCO 3 7. 37 10. 3 8. 4 35

BLOOD GASES Fi. O 2 0. 6 p. H p. O 2 p. CO 2 HCO 3 7. 31 10. 3 8. 4 24
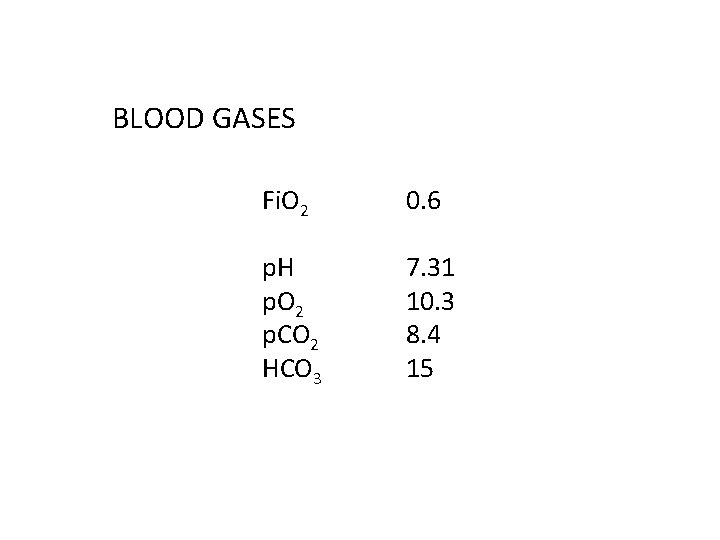
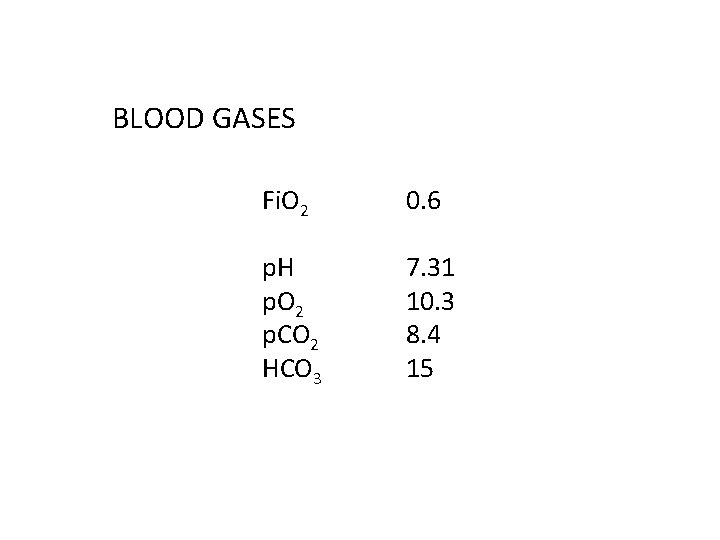
BLOOD GASES Fi. O 2 0. 6 p. H p. O 2 p. CO 2 HCO 3 7. 31 10. 3 8. 4 15
 Cornyebacteria
Cornyebacteria The honorary shepherds
The honorary shepherds Ffa honorary membership
Ffa honorary membership Ieee honorary membership
Ieee honorary membership Passive sentence
Passive sentence Promotion from assistant to associate professor
Promotion from assistant to associate professor Conductive zone vs respiratory zone
Conductive zone vs respiratory zone Abc's of skin cancer
Abc's of skin cancer Osce komprehensif adalah
Osce komprehensif adalah Ranzcp guidelines
Ranzcp guidelines Osce documentation centre in prague
Osce documentation centre in prague Cranial nerve osce
Cranial nerve osce Osce
Osce Osce
Osce Paediatric history osce scenarios
Paediatric history osce scenarios Ice osce
Ice osce Rutherford-morrison scar
Rutherford-morrison scar Procedimiento de selección osce
Procedimiento de selección osce Osce medical
Osce medical Stroke osce
Stroke osce Ospe and osce
Ospe and osce Dnacpr osce
Dnacpr osce Osce data interpretation
Osce data interpretation Professor mark ferguson
Professor mark ferguson Professor mark radford
Professor mark radford Macbeth revision booklet
Macbeth revision booklet Geography paper 1 case studies aqa
Geography paper 1 case studies aqa Revision.english.outwood
Revision.english.outwood Yahmad ict chapter 1
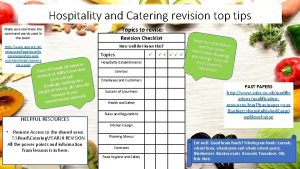
Yahmad ict chapter 1 Hospitality and catering revision
Hospitality and catering revision Has been vreme
Has been vreme