OSCE Answer 022015 TMH AED 1 Question 1
- Slides: 70
OSCE Answer 02/2015 TMH AED 1
Question 1 • • • M/69 Known history of HT, IHD, PVD Sudden onset of constant low back pain BP 162/85 mm. Hg P 78/min 2
Question 1 • Suggest 5 differential diagnosis of acute low back pain – Mechanical spinal disease – Non-mechanical spinal disease – Visceral disease 3
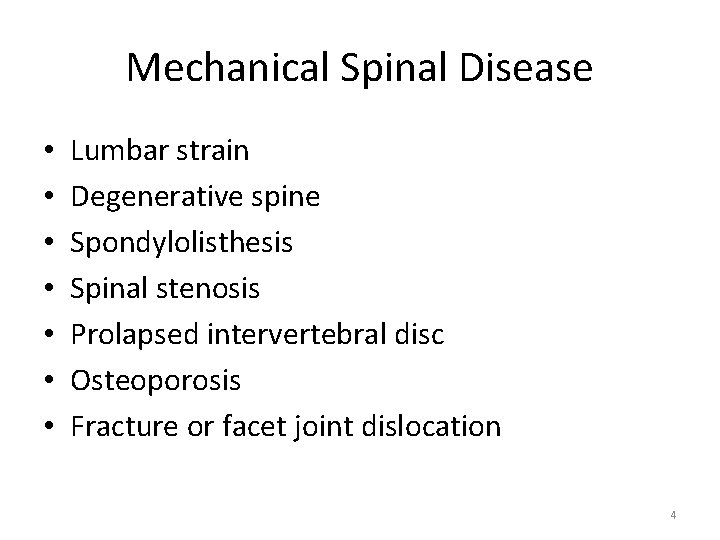
Mechanical Spinal Disease • • Lumbar strain Degenerative spine Spondylolisthesis Spinal stenosis Prolapsed intervertebral disc Osteoporosis Fracture or facet joint dislocation 4
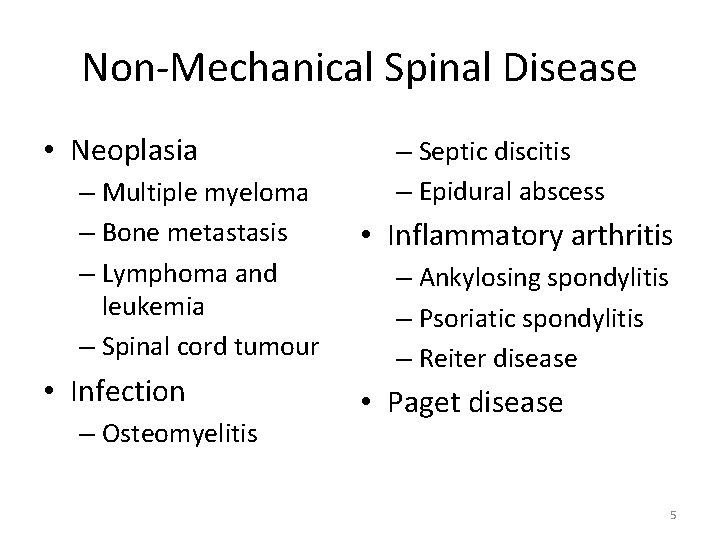
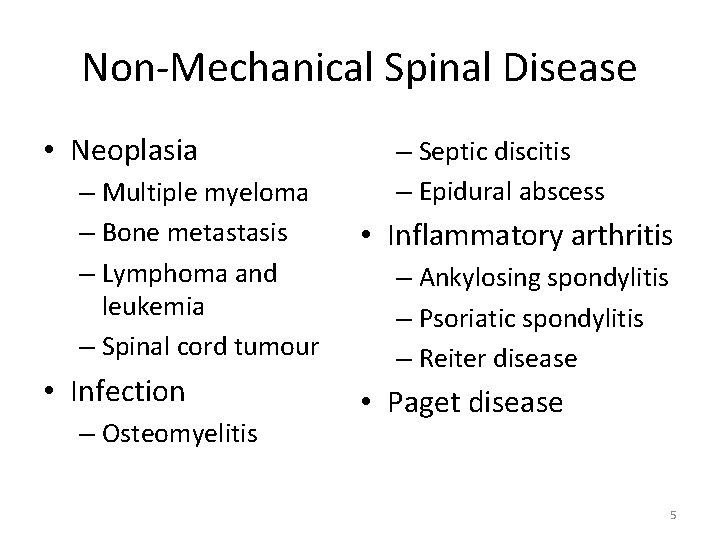
Non-Mechanical Spinal Disease • Neoplasia – Multiple myeloma – Bone metastasis – Lymphoma and leukemia – Spinal cord tumour • Infection – Osteomyelitis – Septic discitis – Epidural abscess • Inflammatory arthritis – Ankylosing spondylitis – Psoriatic spondylitis – Reiter disease • Paget disease 5
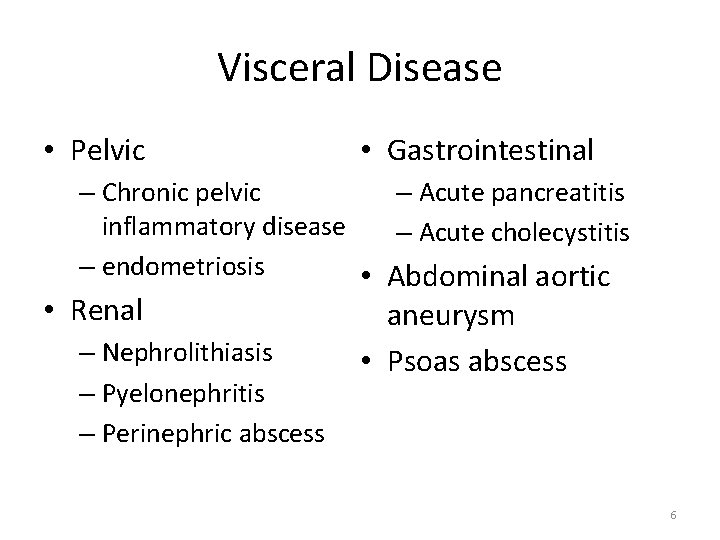
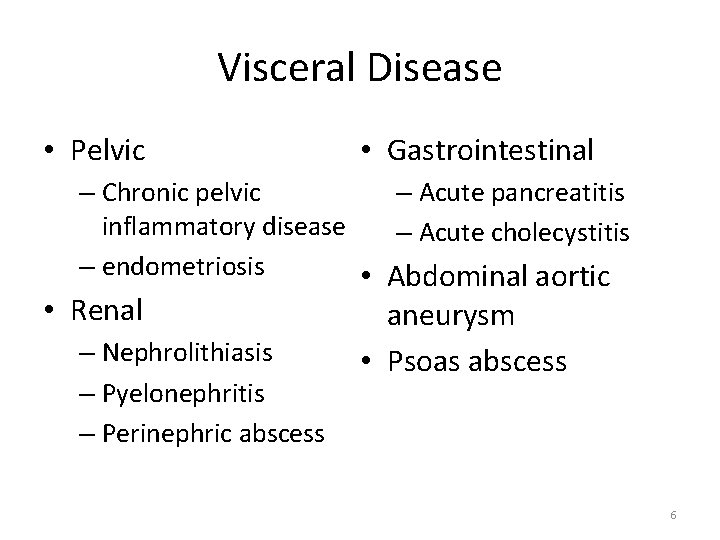
Visceral Disease • Pelvic • Gastrointestinal – Chronic pelvic – Acute pancreatitis inflammatory disease – Acute cholecystitis – endometriosis • Abdominal aortic • Renal – Nephrolithiasis – Pyelonephritis – Perinephric abscess aneurysm • Psoas abscess 6
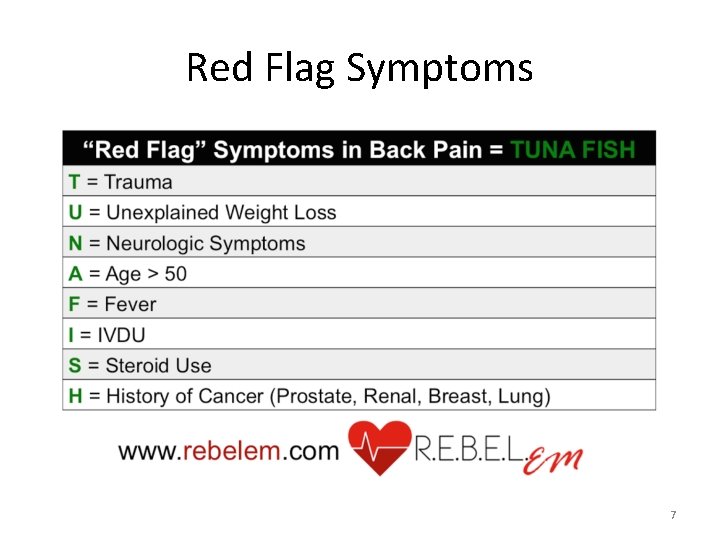
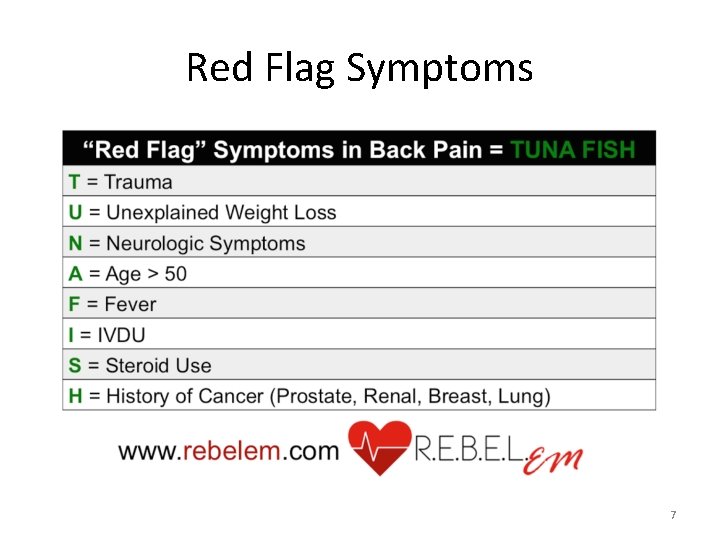
Red Flag Symptoms 7
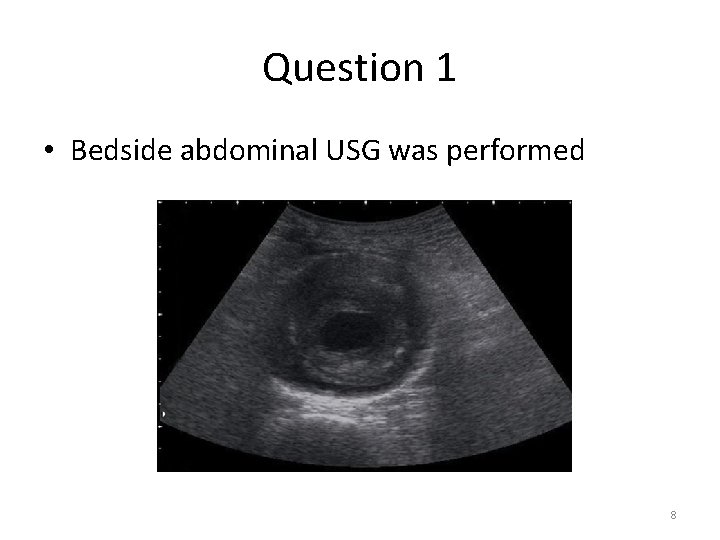
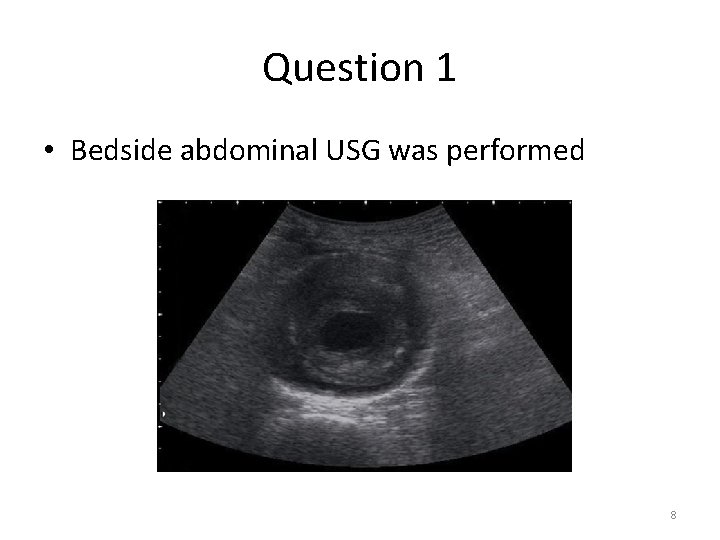
Question 1 • Bedside abdominal USG was performed 8
Question 1 • What’s the sonographic diagnosis? – 7 cm in diameter abdominal aortic aneurysm with concentric hyperechoic lesion signifying thrombus 9
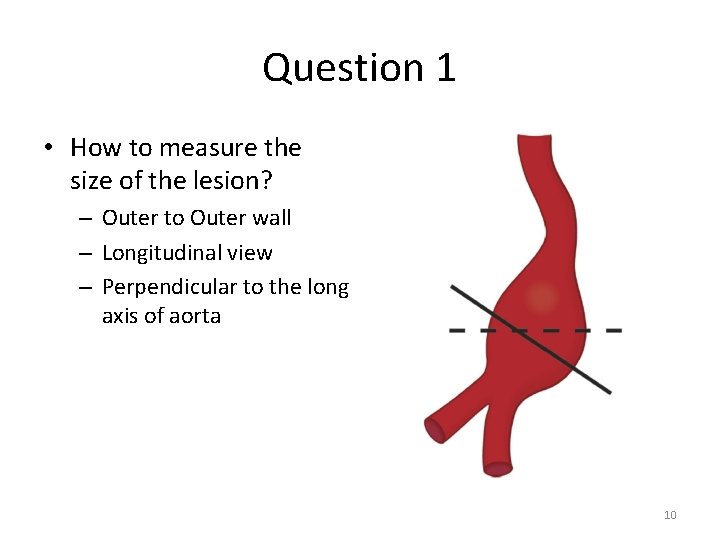
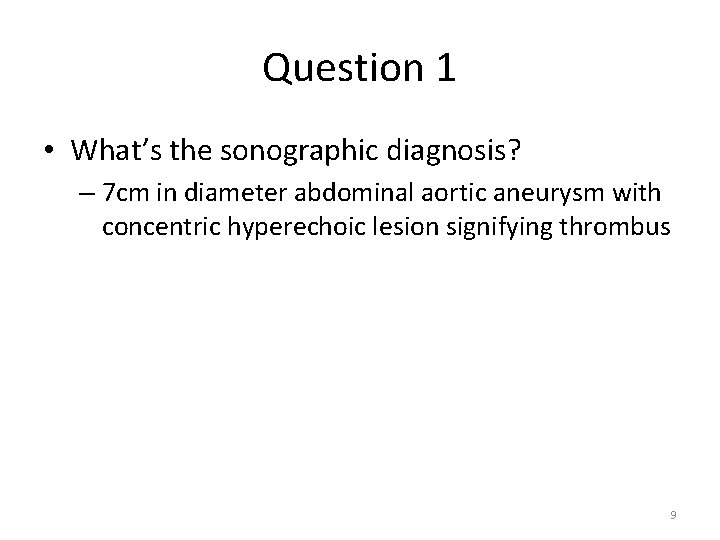
Question 1 • How to measure the size of the lesion? – Outer to Outer wall – Longitudinal view – Perpendicular to the long axis of aorta 10
Question 1 • How to classify the type of the lesion using ultrasound? – Identify the origin of the SMA, 2 cm below should be the origin of renal arteries – Classify according to the location of the aortic aneurysm • Suprarenal • Juxtarenal • Infrarenal (Ultrasound Clin 2 (2007) 437– 453) 11
Question 1 • State the microbe that is most commonly associated with this condition? – A study in southern Taiwan from 1996 to 2006 on mycotic aneurysm • Salmonella (34. 6%) • Klebsiella (11. 5%) • Staphylococcus aureus (11. 5%) (J Microbiol Immunol Infect 2008; 41(4): 318 -324) 12
Question 2 • F/40 • Good past health • Sudden onset of right sided weakness 1 hour before • BP 180/93 mm. Hg • P 104/min • GCS 15/15 13
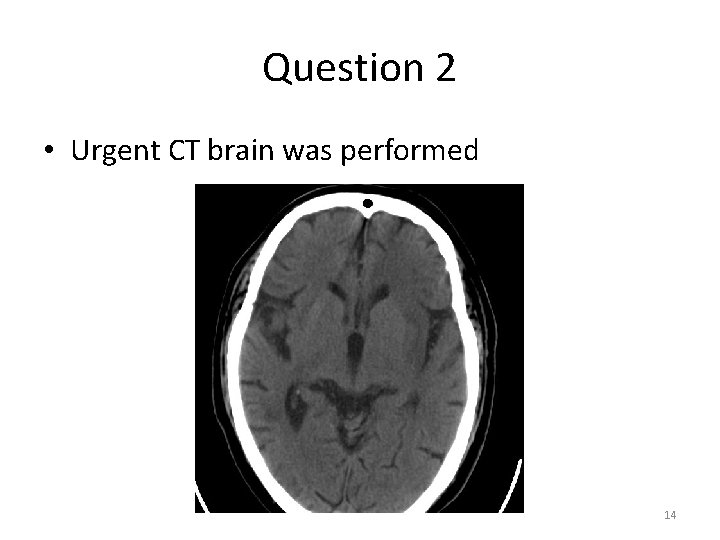
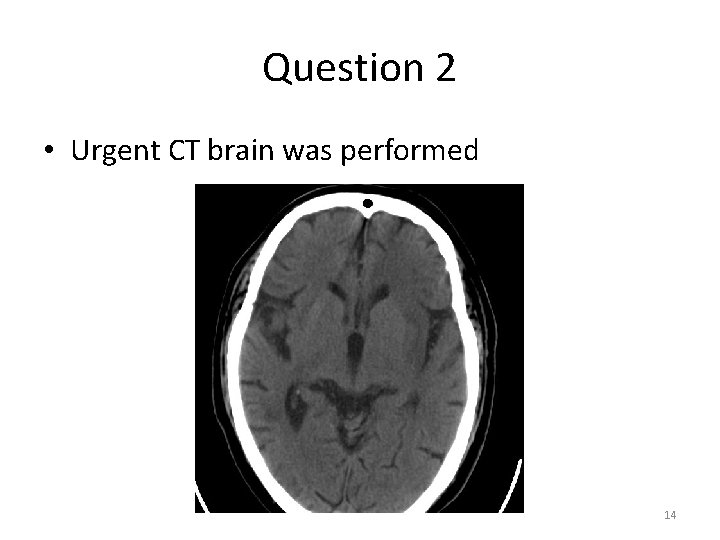
Question 2 • Urgent CT brain was performed 14
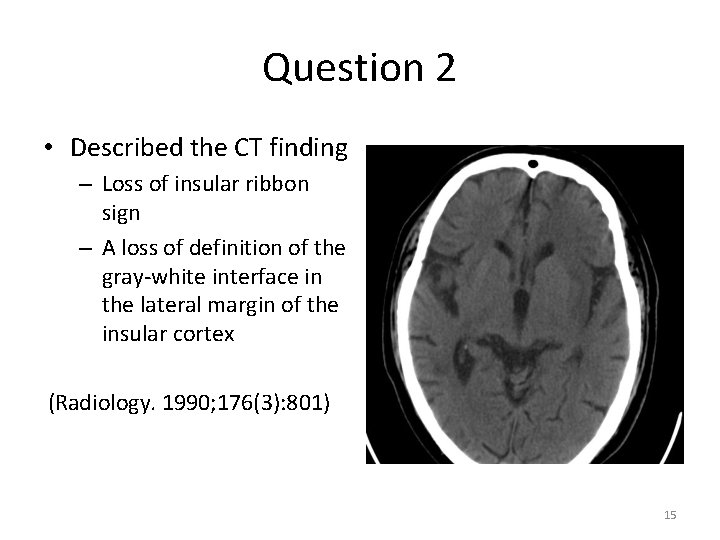
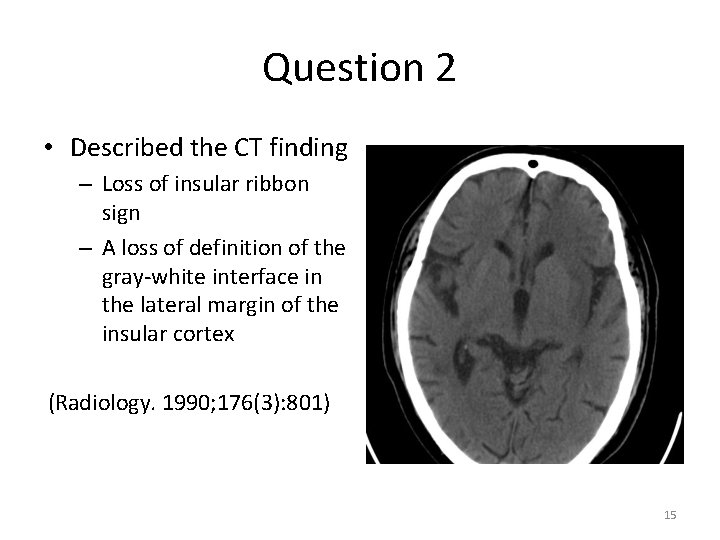
Question 2 • Described the CT finding – Loss of insular ribbon sign – A loss of definition of the gray-white interface in the lateral margin of the insular cortex (Radiology. 1990; 176(3): 801) 15
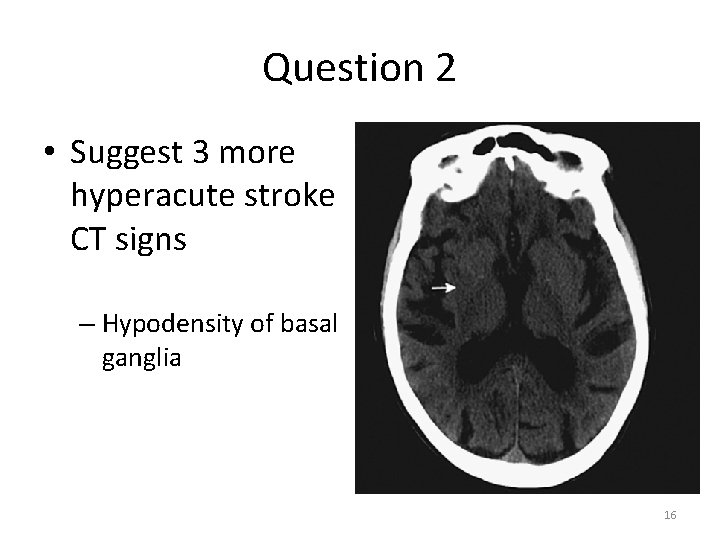
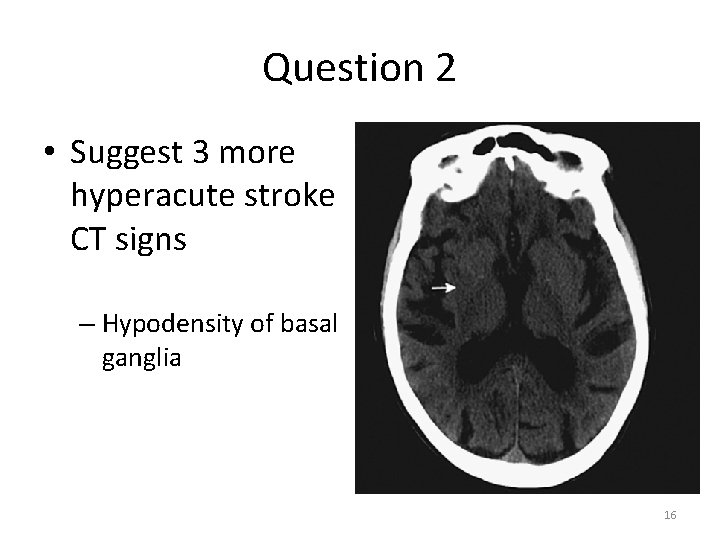
Question 2 • Suggest 3 more hyperacute stroke CT signs – Hypodensity of basal ganglia 16
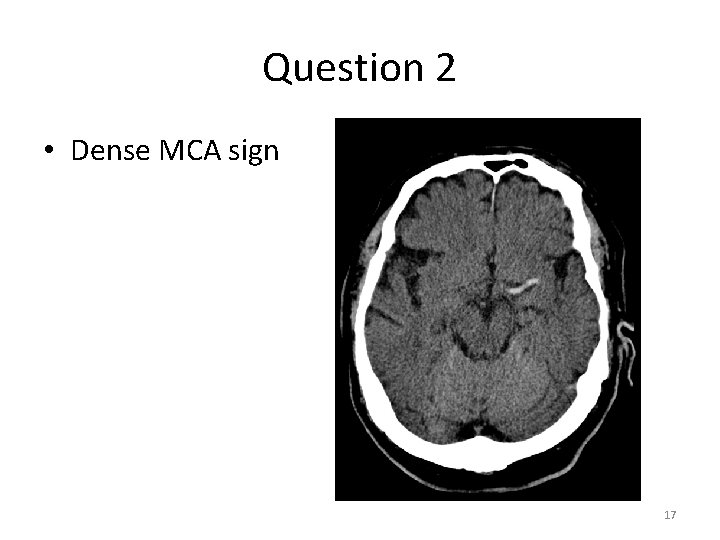
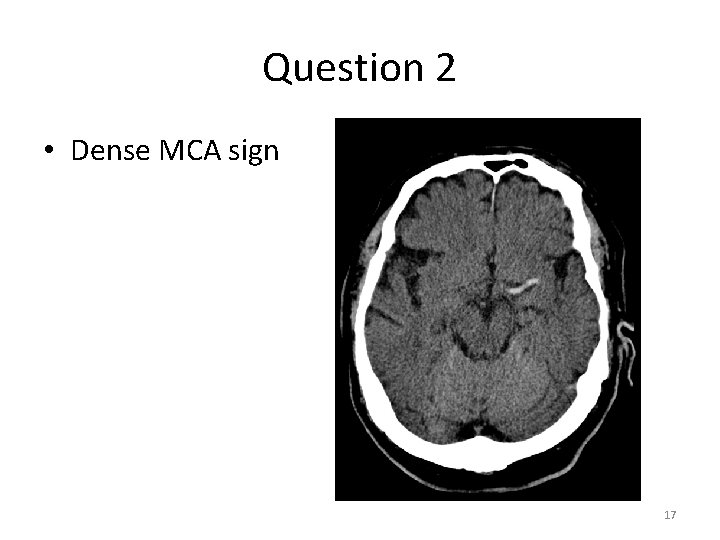
Question 2 • Dense MCA sign 17
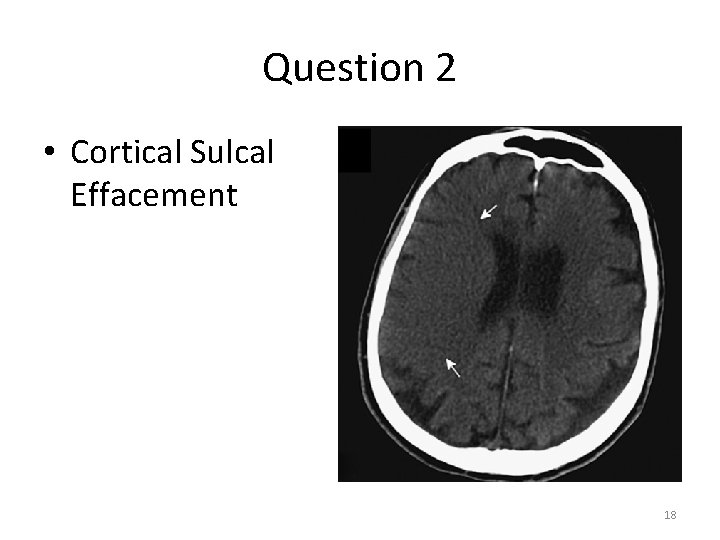
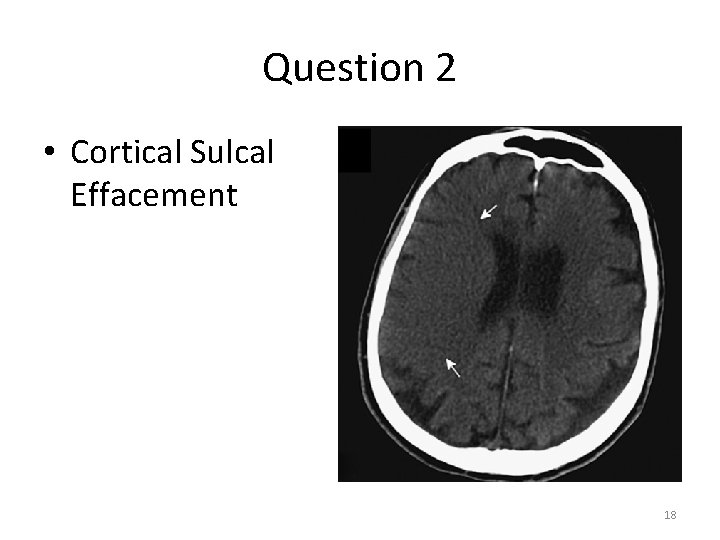
Question 2 • Cortical Sulcal Effacement 18
Question 2 • Outline subsequent management plan for this patient – Stabilization, history taking and physical examination – Baseline investigations like blood tests, ECG, CXR – Consult neurologist for assessment – Stroke management – Reperfusion therapy and anti-platelet agent Emerg Med Clin North Am. 2012 Aug; 30(3): 713 -44 19
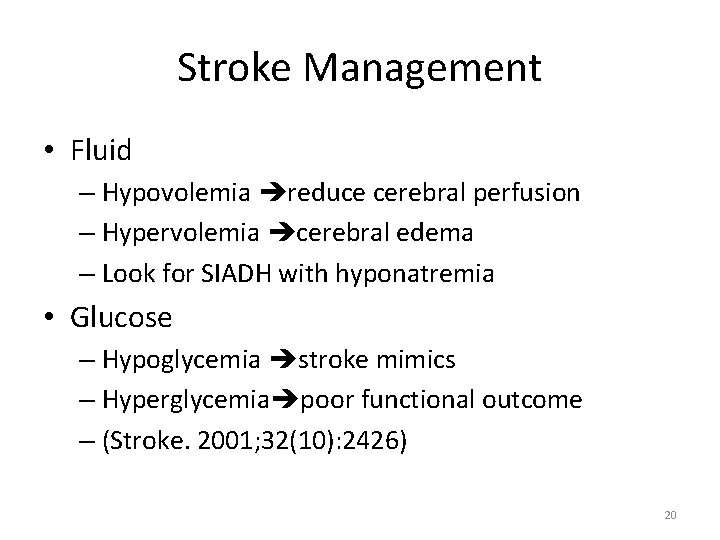
Stroke Management • Fluid – Hypovolemia reduce cerebral perfusion – Hypervolemia cerebral edema – Look for SIADH with hyponatremia • Glucose – Hypoglycemia stroke mimics – Hyperglycemia poor functional outcome – (Stroke. 2001; 32(10): 2426) 20
Stroke Management • Head position – Lying flat would increase mean flow velocity of cerebral artery by 20% in one study (Neurology. 2005; 64(8): 1354) – Prop up 30° in patients with • Raised intracranial pressure • Risk of aspirations • Cardiopulmonary disease or oxygen desaturation 21
Stroke Management • Blood pressure control – Blood pressure control within 7 – 10 days post stroke leads to increase 30 days mortality (The Lancet. 22/10/2014 open access) (http: //dx. doi. org/10. 1016/S 0140 -6736(14)61121 -1) – Goals of blood pressure control • Thrombolytic therapy: SBP < 185 mm. Hg, DBP < 110 mm. Hg • No thrombolytic therapy: SBP <220 mm. Hg, DBP < 120 mm. Hg 22
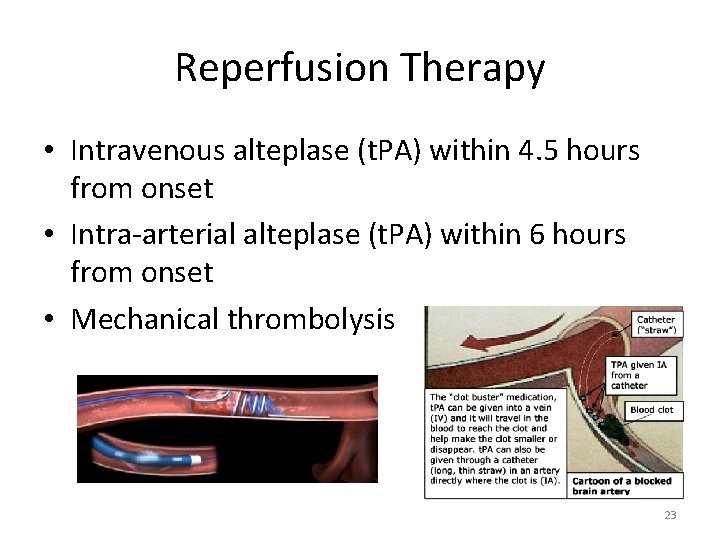
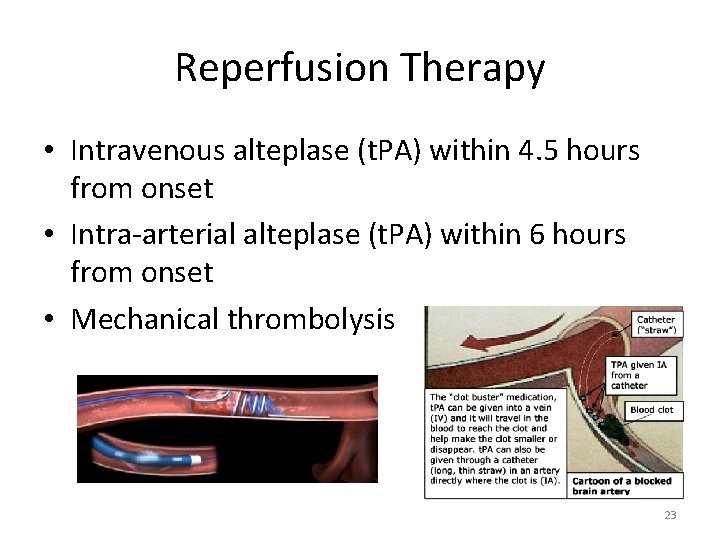
Reperfusion Therapy • Intravenous alteplase (t. PA) within 4. 5 hours from onset • Intra-arterial alteplase (t. PA) within 6 hours from onset • Mechanical thrombolysis 23
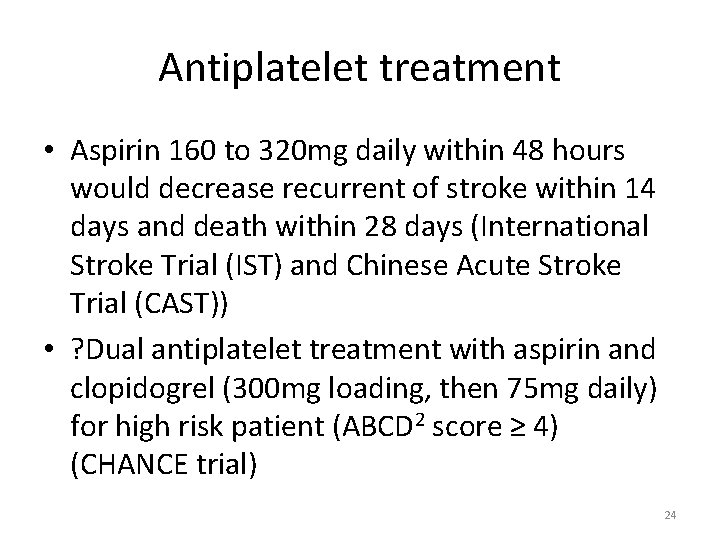
Antiplatelet treatment • Aspirin 160 to 320 mg daily within 48 hours would decrease recurrent of stroke within 14 days and death within 28 days (International Stroke Trial (IST) and Chinese Acute Stroke Trial (CAST)) • ? Dual antiplatelet treatment with aspirin and clopidogrel (300 mg loading, then 75 mg daily) for high risk patient (ABCD 2 score ≥ 4) (CHANCE trial) 24
Question 2 • State 3 etiologies for young onset stroke – Cardiac • Congenital heart disease • Endocarditis, cardiomyopathy, prosthetic valve replacement – Haematologic • sickle cell disease • Prothrombolic conditions like antiphospholipid syndrome, protein C deficiency, protein S deficiency etc 25
Question 2 • State 3 etiologies for young onset stroke – Vasculopathy • Moyamoya disease (primary or secondary) • Dissection • Vasculitis – Substance abuse 26
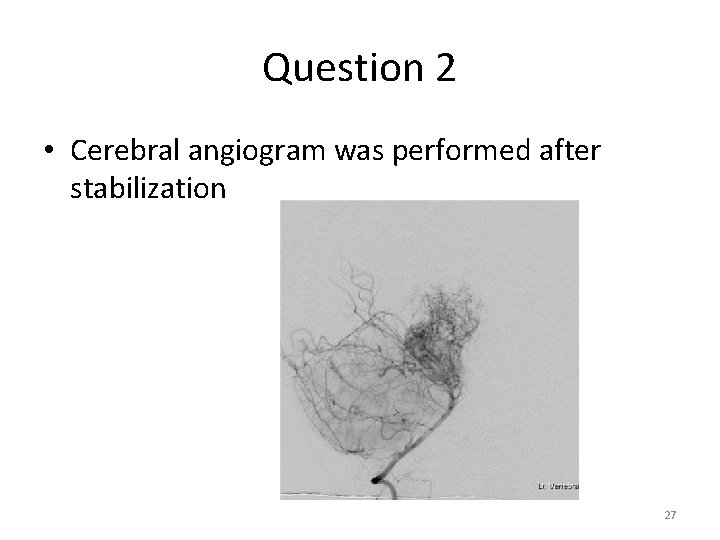
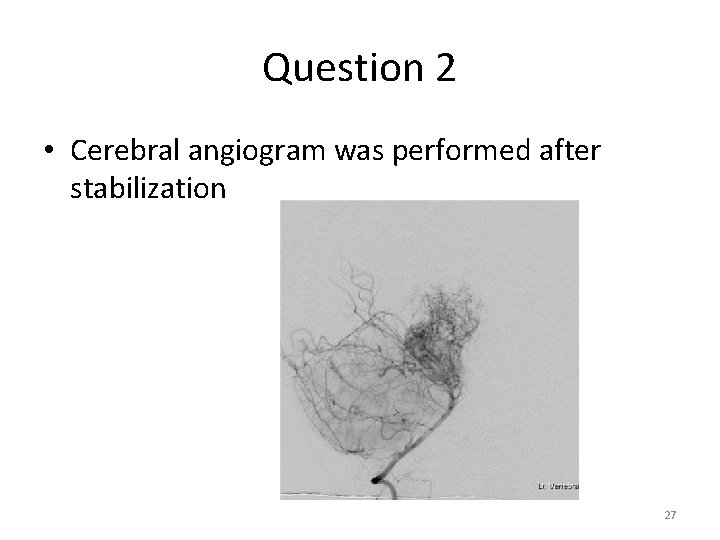
Question 2 • Cerebral angiogram was performed after stabilization 27
Question 2 • Describe the finding – Puff of smoke appearance – Due to collateral vasculature • What is the diagnosis? – Moyamoya disease 28
Moyamoya Disease • Bilateral stenosis or occlusion of vessels around circle of Willis with prominent collateral circulation • Moyamoya is Japanese, meaning hazy like a puff of smoke in the air • Can lead to both ischemic and haemorrhagic stroke 29
Question 3 • F/56 • Good past health • Vehicle-pedestrian collision with left knee injury • BP 153/79 mm. Hg • P 95/min 30
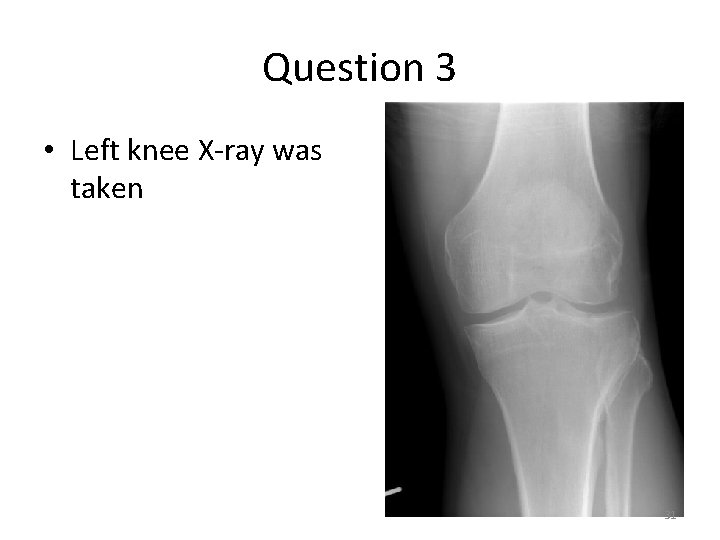
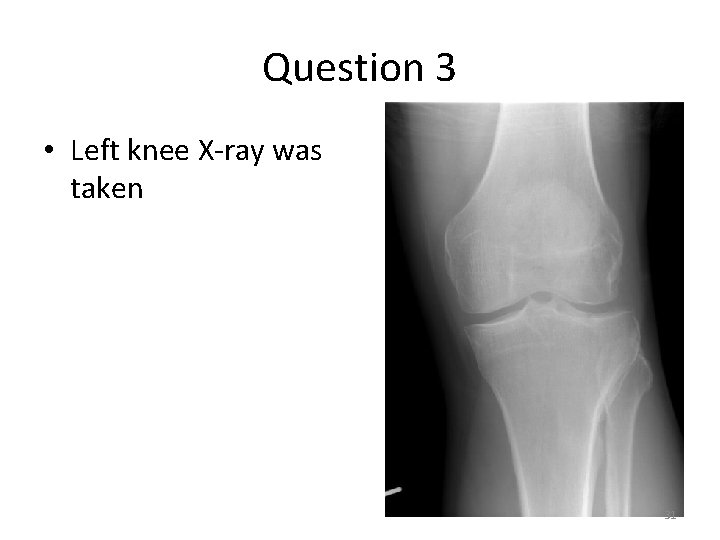
Question 3 • Left knee X-ray was taken 31
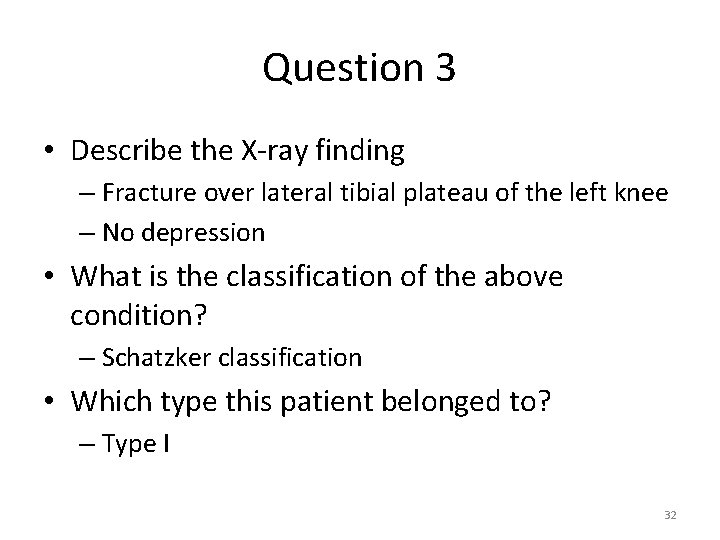
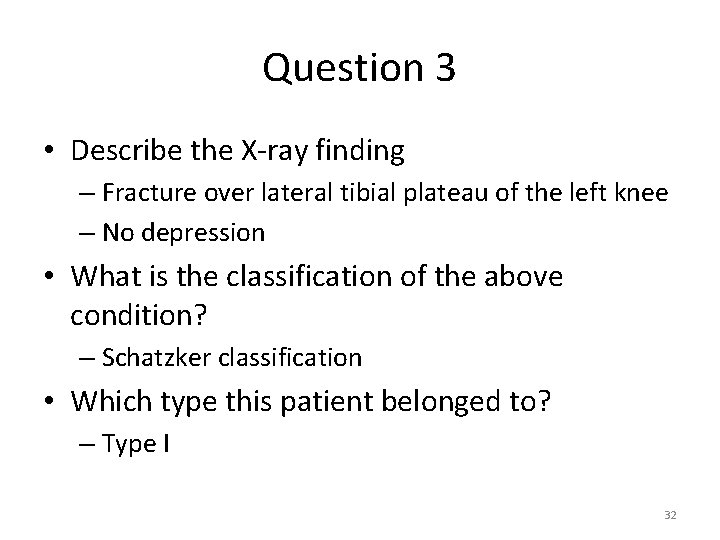
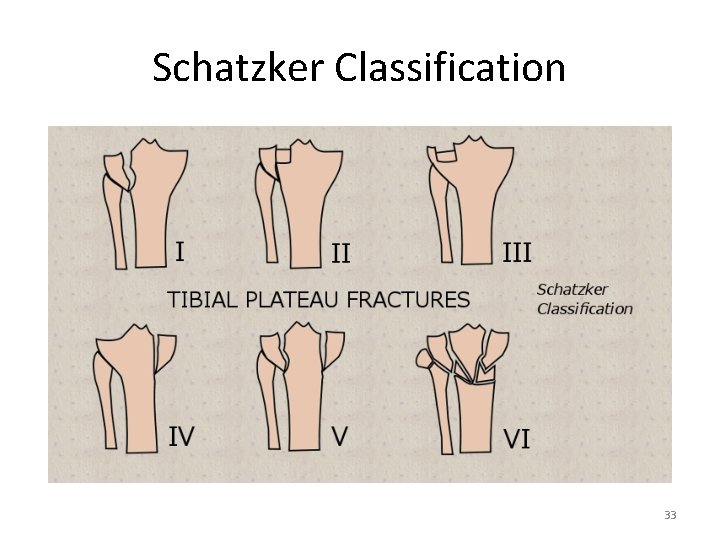
Question 3 • Describe the X-ray finding – Fracture over lateral tibial plateau of the left knee – No depression • What is the classification of the above condition? – Schatzker classification • Which type this patient belonged to? – Type I 32
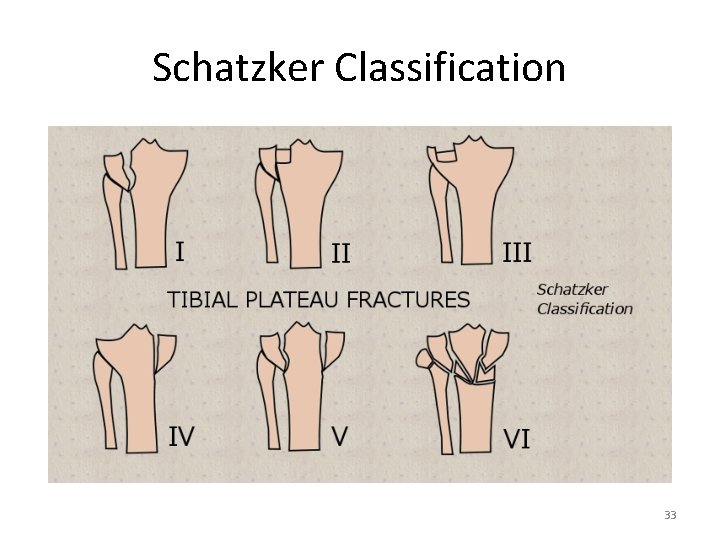
Schatzker Classification 33
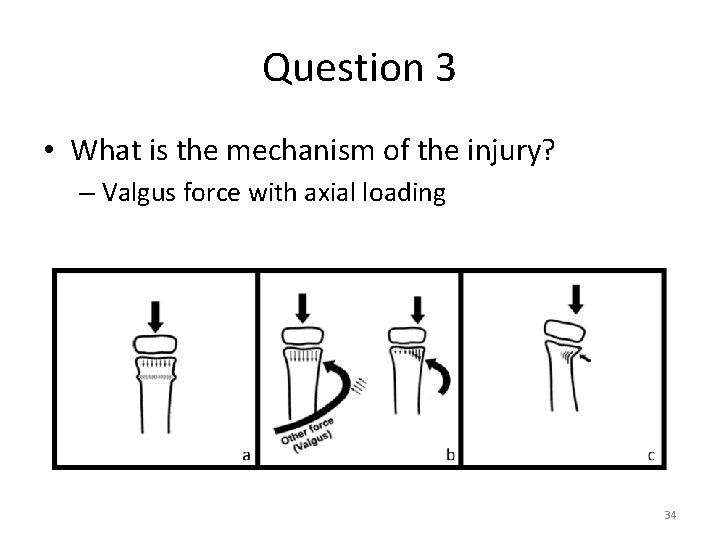
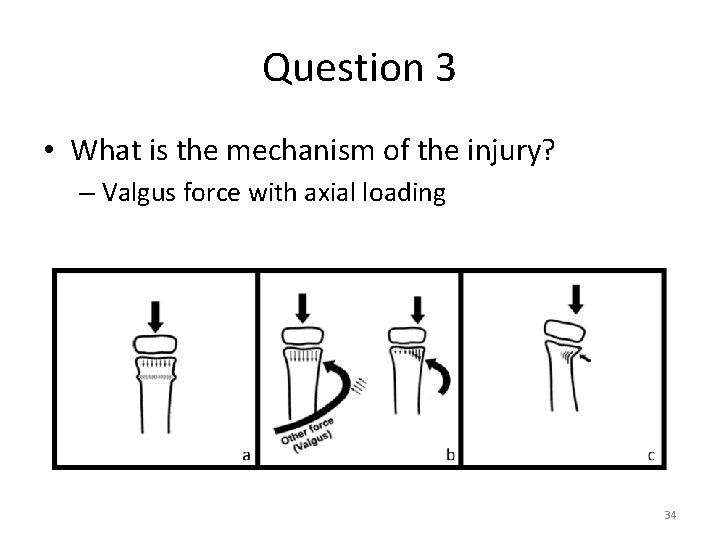
Question 3 • What is the mechanism of the injury? – Valgus force with axial loading 34
Question 3 • Name 4 potential complications – Early complications • • • Compartment syndrome Vascular injury (popliteal artery) Nerve injury (peroneal nerve) Infection Deep vein thrombosis 35
Question 3 • Name 4 potential complications – Late complications • • • Knee stiffness Knee instability Osteoarthritis Malunion, nonunion Angular deformity Late collapse 36
Question 4 • M/72 • History of DM, HT, SSS on pacemaker • Sudden onset of severe chest pain for 3 hours, only partially relieved by TNG • BP 164/88 mm. Hg • P 62/min 37
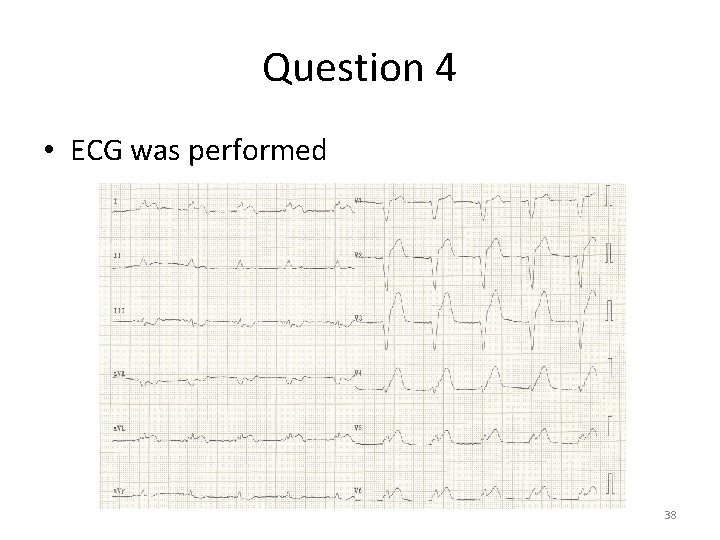
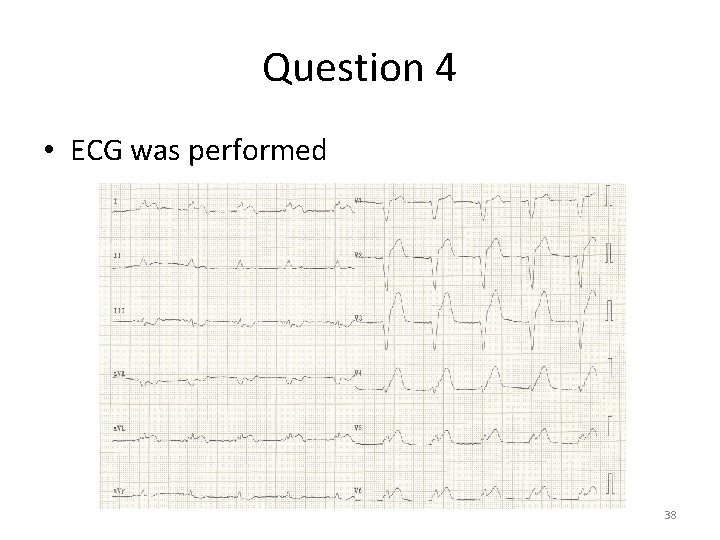
Question 4 • ECG was performed 38
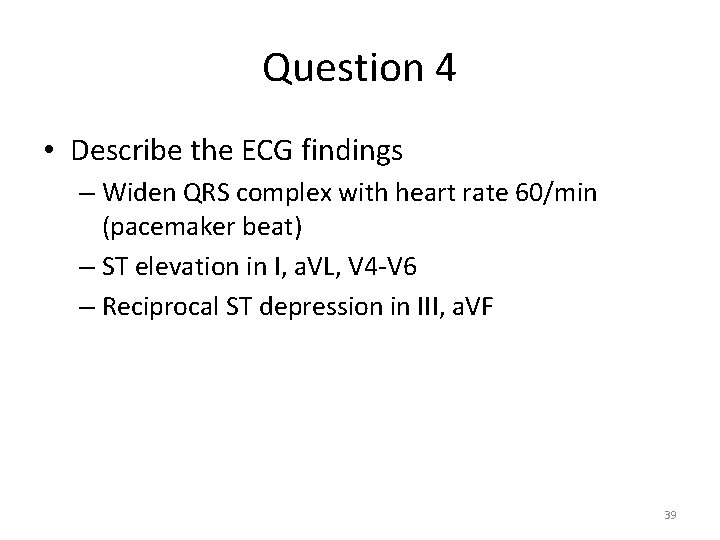
Question 4 • Describe the ECG findings – Widen QRS complex with heart rate 60/min (pacemaker beat) – ST elevation in I, a. VL, V 4 -V 6 – Reciprocal ST depression in III, a. VF 39
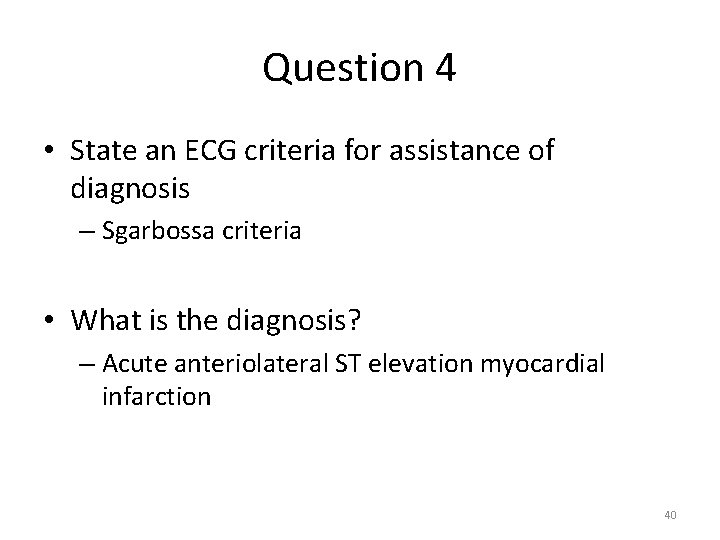
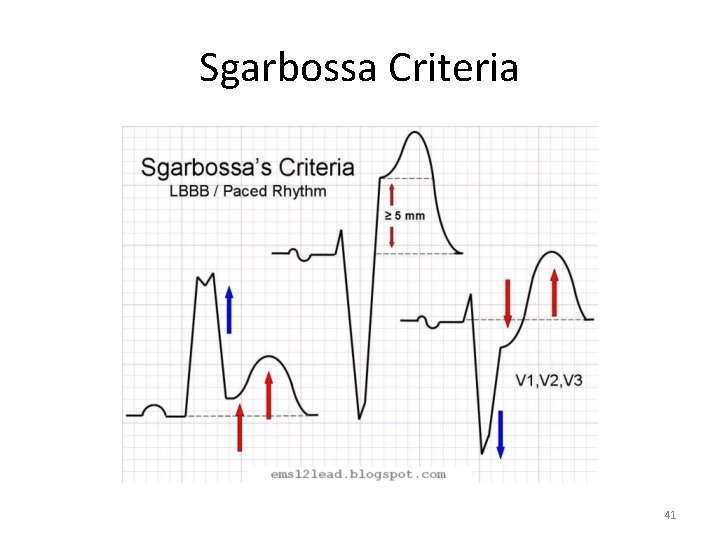
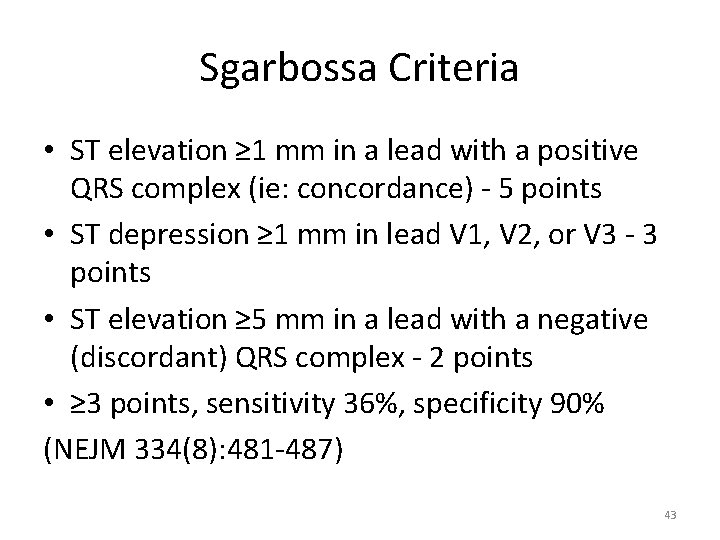
Question 4 • State an ECG criteria for assistance of diagnosis – Sgarbossa criteria • What is the diagnosis? – Acute anteriolateral ST elevation myocardial infarction 40
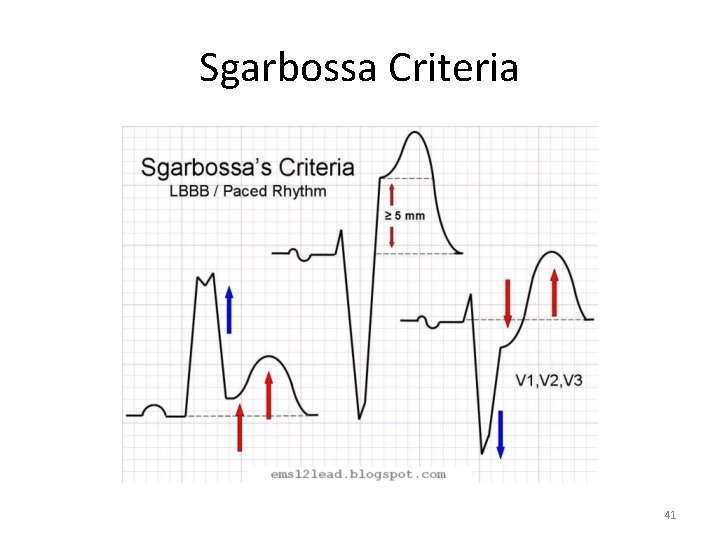
Sgarbossa Criteria 41
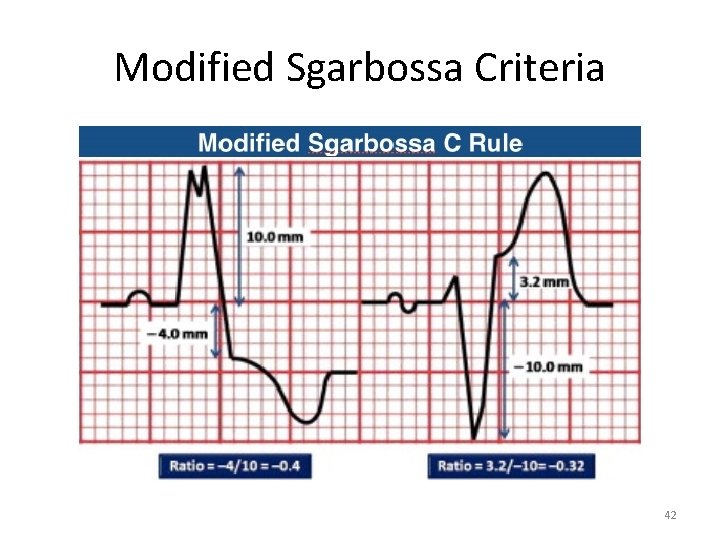
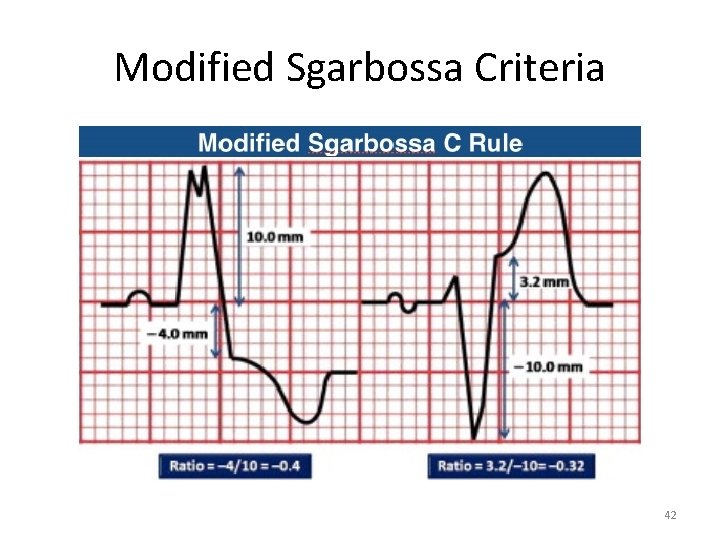
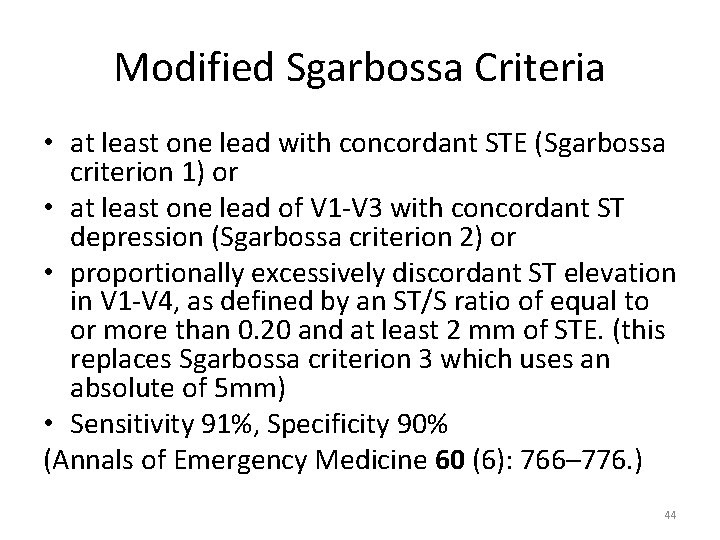
Modified Sgarbossa Criteria 42
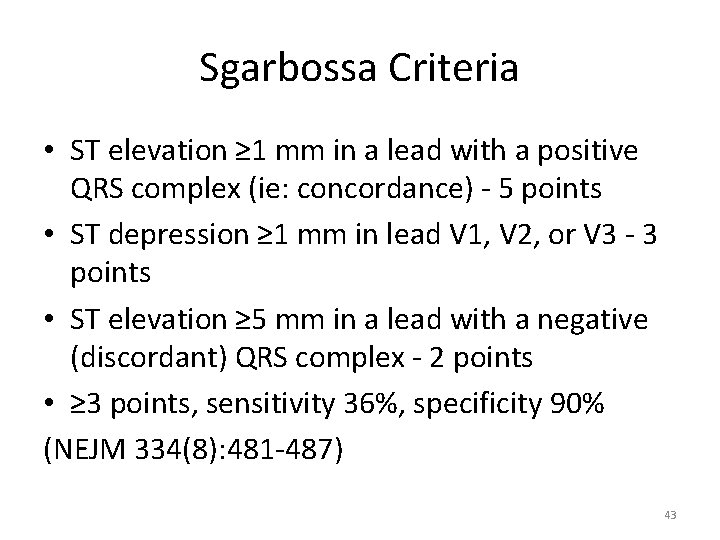
Sgarbossa Criteria • ST elevation ≥ 1 mm in a lead with a positive QRS complex (ie: concordance) - 5 points • ST depression ≥ 1 mm in lead V 1, V 2, or V 3 - 3 points • ST elevation ≥ 5 mm in a lead with a negative (discordant) QRS complex - 2 points • ≥ 3 points, sensitivity 36%, specificity 90% (NEJM 334(8): 481 -487) 43
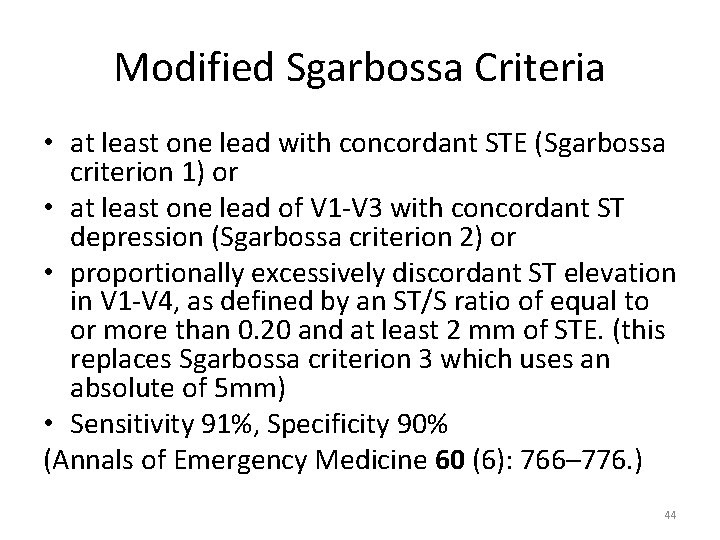
Modified Sgarbossa Criteria • at least one lead with concordant STE (Sgarbossa criterion 1) or • at least one lead of V 1 -V 3 with concordant ST depression (Sgarbossa criterion 2) or • proportionally excessively discordant ST elevation in V 1 -V 4, as defined by an ST/S ratio of equal to or more than 0. 20 and at least 2 mm of STE. (this replaces Sgarbossa criterion 3 which uses an absolute of 5 mm) • Sensitivity 91%, Specificity 90% (Annals of Emergency Medicine 60 (6): 766– 776. ) 44
Question 4 • Outline the management in AED – Recognize emergency condition and manage in resuscitation room with resuscitation equipments standby – Monitoring devices – Set up large bore IV access, blood tests, CXR – Consult cardiologist for assessment – MONA – Reperfusion therapy – Antithrombotic therapy and antiplatelet therapy 45
Primary PCI • Door to balloon time – 90 minutes in PCI capable hospital – 120 minutes in non-PCI capable hospital • Patients presented more than 12 hours, with cardiogenic shock, electrical instability or persistent ischemic symptoms (2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction) 46
Thrombolytic therapy • Symptoms within 12 hours with primary PCI not available within 120 minutes • Door to needle time less than 30 minutes • Facilitated PCI is not recommended • Rescue PCI if failed fibrinolysis (2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction) 47
Thrombolytic therapy • First generation fibrinolytic agents (eg streptokinase) indiscriminately induce activation of circulating plasminogen and clot-associated plasminogen • Second generation fibrinolytic agents (eg t-PA) preferentially activate plasminogen in the fibrin domain • Second generation fibrinolytic agents improve 24 hours, 30 days and 1 year mortality rate in GUSTO trial (Circulation. Oct 10 2000; 102(15): 1761 -5. ) 48
Antithrombotic therapy • Enoxaparin 0. 5 mg/kg significant reduced clinical ischemic outcome compared with unfractionated heparin in STEMI patient undergoing primary PCI (ATOLL trial. Lancet. Aug 20 2011; 378(9792): 693 -703. ) 49
Antiplatelet agents • Aspirin should be given immediately • Adding clopidogrel 300 mg (CLARITY-TIMI 28) is safe and effective • Increase clopidogrel to 600 mg in patient with STEMI prior to primary PCI was associated with a smaller infarct size (ARMYDA-6 MI) (J Am Coll Cardiol. Oct 4 2011; 58(15): 1592 -9. ) 50
Question 5 • M/62 • Repeated vomiting for 1 day, with mild epigastric pain after an alcohol binge • First vomited out undigested food and then mild blood streak 51
Question 5 • BP 123/59 mm. Hg • P 84/min • Abdominal examination was unremarkable. Per rectal examination noted brownish stool. • CXR was normal 52
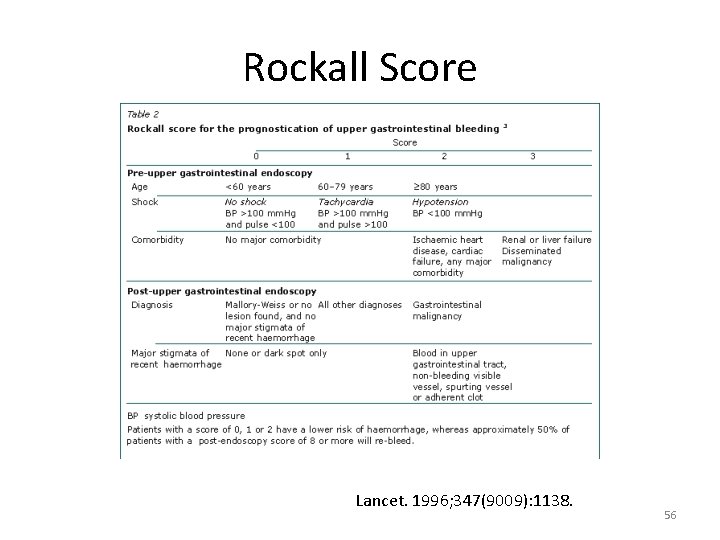
Question 5 • Name 3 clinical prediction rules/scores in upper gastrointestinal bleeding to risk stratification – Glasgow-Blatchford bleeding score – Rockall score – AIMS 65 53
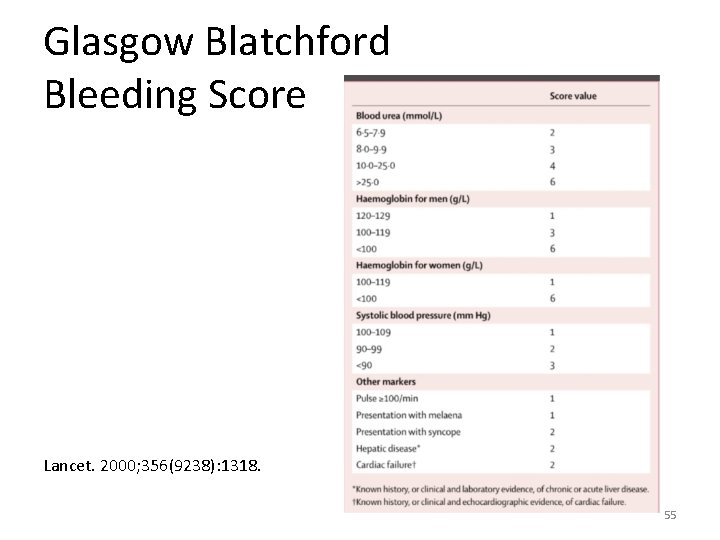
Question 5 • He asked if his condition could be managed without hospital admission • State which score is the most relevant in this scenario? What cut-off and associated clinical implication for the score? – Glasgow Blatchford bleeding score – Score 6 or more has more than 50% risk of needing an intervention 54
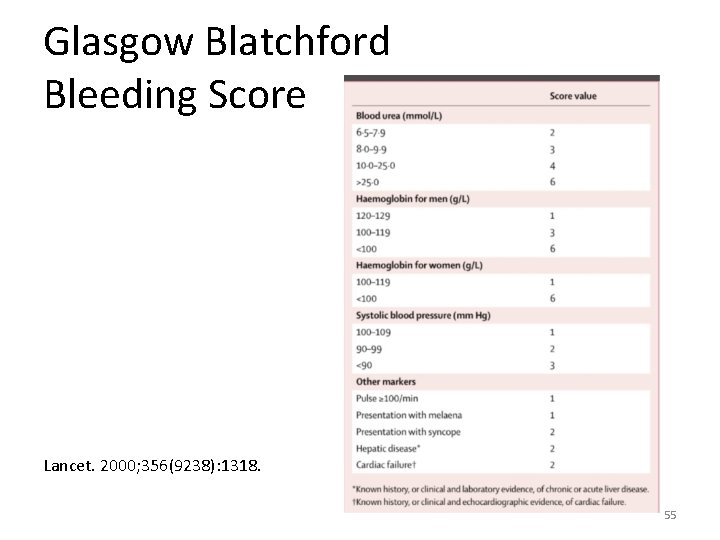
Glasgow Blatchford Bleeding Score Lancet. 2000; 356(9238): 1318. 55
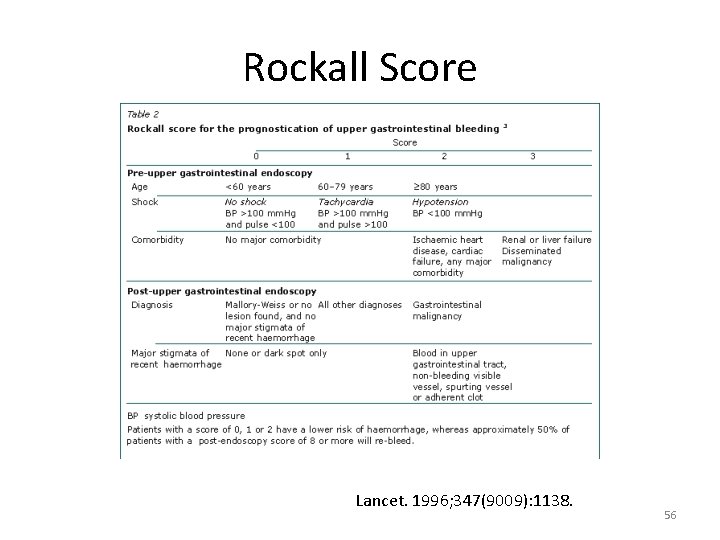
Rockall Score Lancet. 1996; 347(9009): 1138. 56
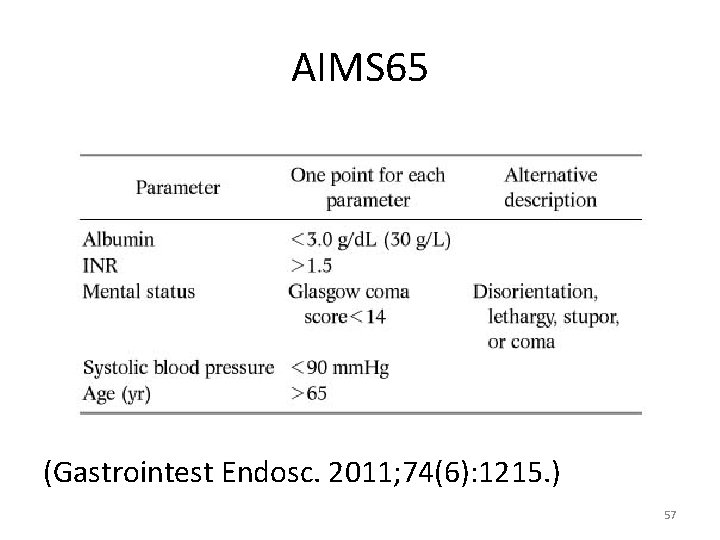
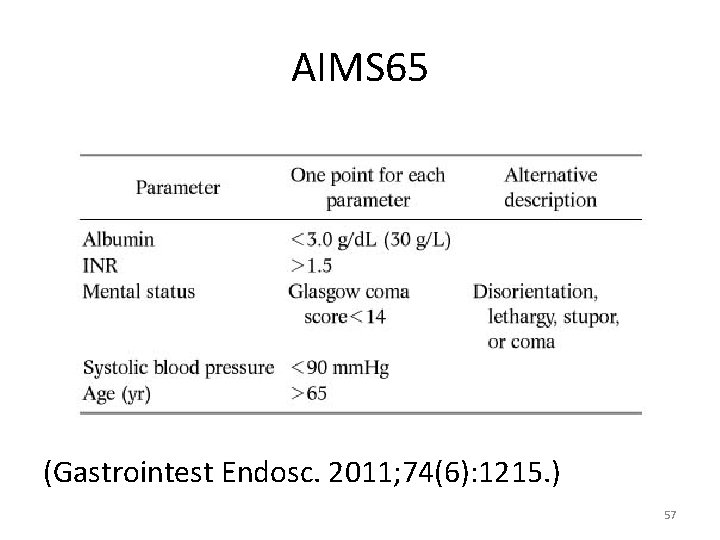
AIMS 65 (Gastrointest Endosc. 2011; 74(6): 1215. ) 57
Question 5 • More history was taken and he had known alcoholic with alcoholic liver cirrhosis • Blood tests result: – Hb 13. 4 g/d. L – Urea 7. 8 mmol/L 58
Question 5 • How would you management this patient? – GBS 4 – Admit to EMW for observation • NPO • IV fluid • Type and screen, clotting profile 59
Question 5 • He developed gross haematemesis during his stay in AED • BP 96/49 mm. Hg • P 106/min 60
Question 5 • How would you manage this patient in addition to the management you ordered before? – Manage in resuscitation room – Nasogastric tube insertion, suction with airway protection – IV fluid resuscitation and hemodynamic resuscitation – Consult surgeon for urgent OGD – IV somatostatin analog, vasopressin – Balloon tamponade 61
Question 6 • M/69 • History of HT, DM, old CVA • Decrease general condition for 1 month 62
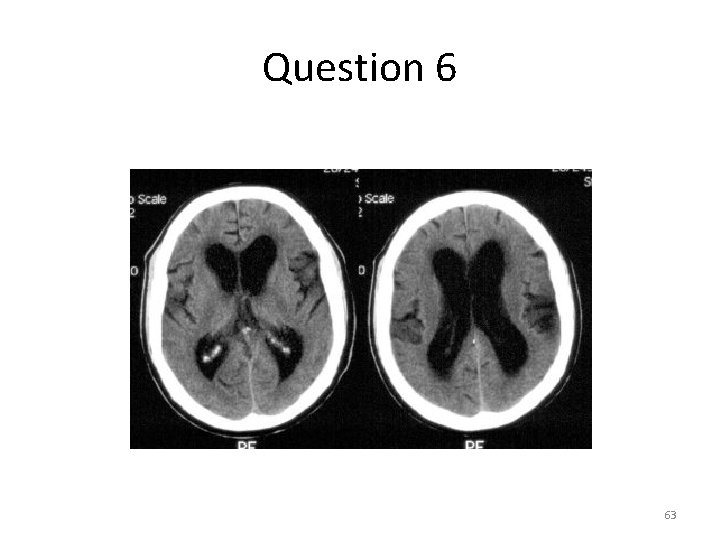
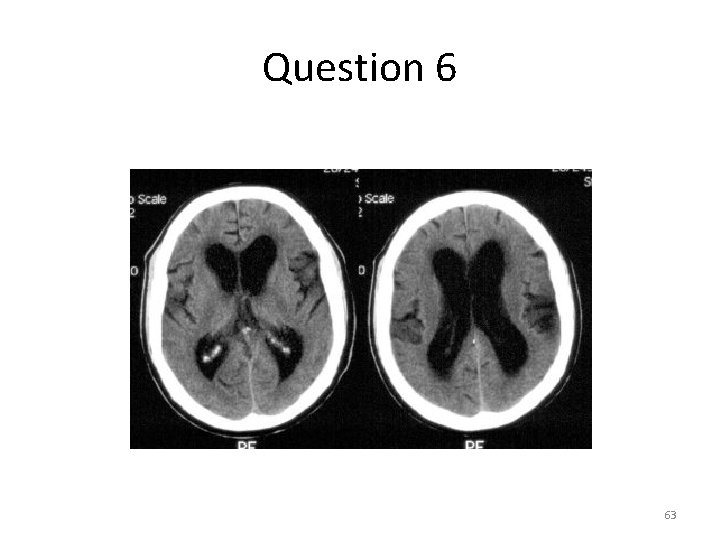
Question 6 63
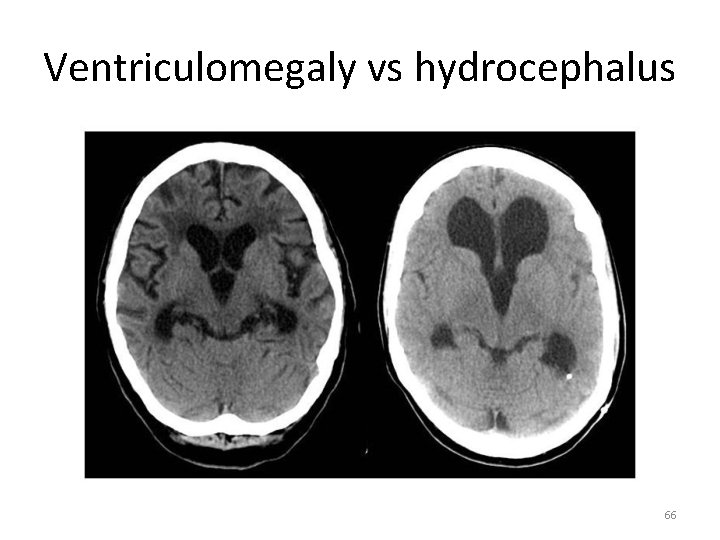
Question 6 • Describe the CT finding – Hydrocephalus 64
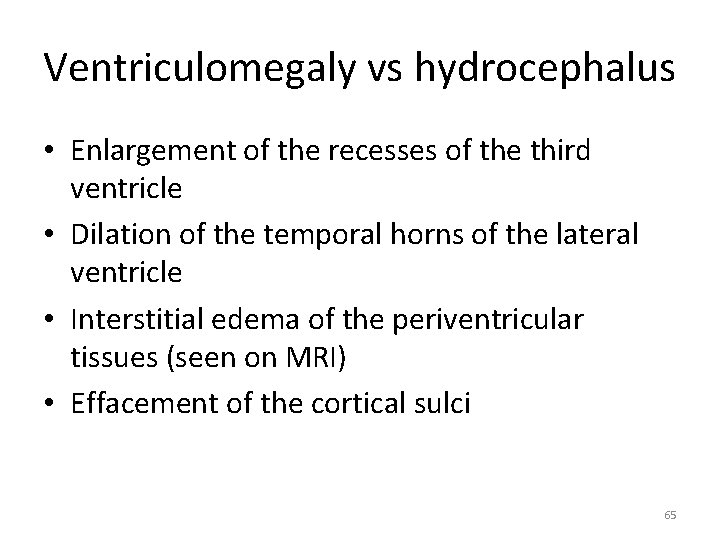
Ventriculomegaly vs hydrocephalus • Enlargement of the recesses of the third ventricle • Dilation of the temporal horns of the lateral ventricle • Interstitial edema of the periventricular tissues (seen on MRI) • Effacement of the cortical sulci 65
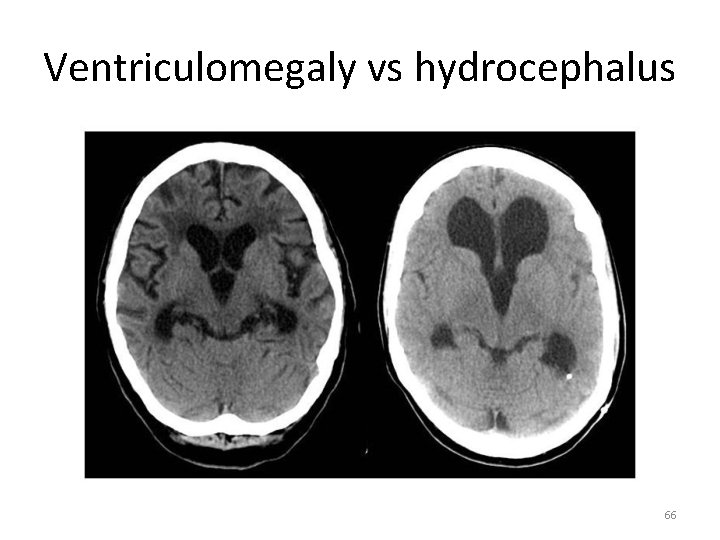
Ventriculomegaly vs hydrocephalus 66
Question 6 • What further investigations would you proceed? – MRI – Lumbar puncture 67
Question 6 • If the opening pressure of the lumbar puncture is 12 cm H 2 O • What is the condition called? – Normal Pressure Hydrocephalus • What is the classic triad of this condition? – Gait instability (magnetic gait) – Cognitive impairment – Urinary incontinence 68
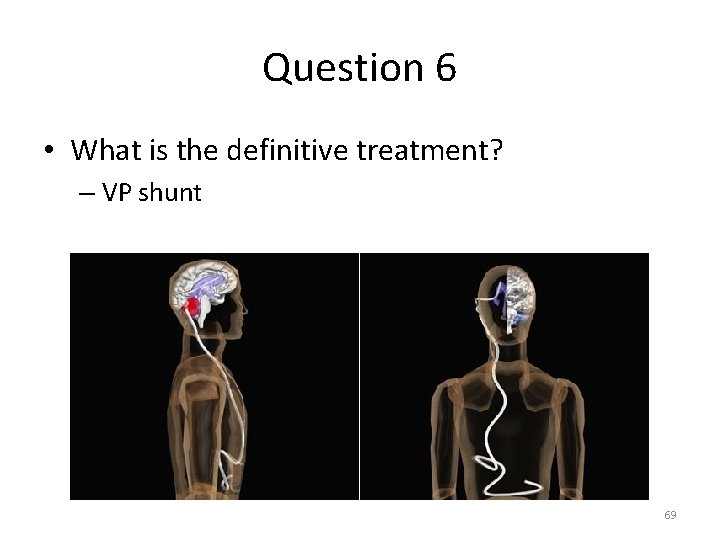
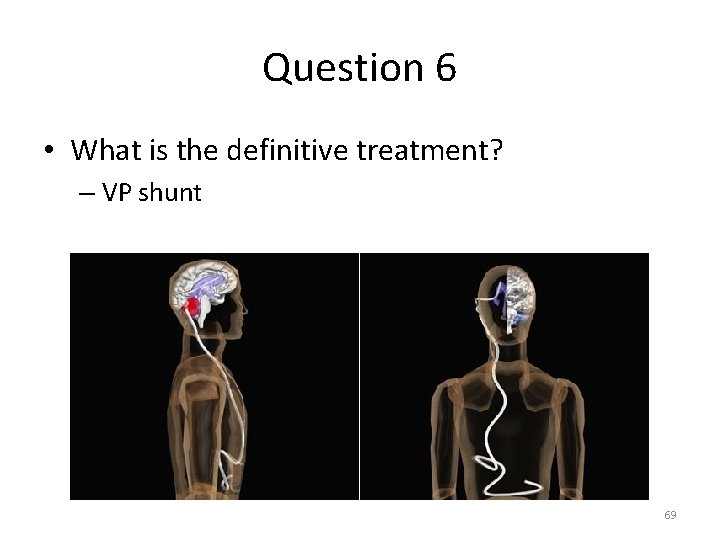
Question 6 • What is the definitive treatment? – VP shunt 69
70