OSCE Anaesthesia Posting Batch 5 Yr 4 CG
OSCE Anaesthesia Posting Batch 5 Yr 4 : CG 28, 29 & 30 Friday, 2 September 2005
Question 1 You are called to the accident and emergency department to see a 31 -year-old lady, known to have asthma, who has been admitted with acute shortness of breath. 1. How would you make a clinical assessment of the severity of this attack?
Question 1 You are called to the accident and emergency department to see a 31 -year-old lady, known to have asthma, who has been admitted with acute shortness of breath. 2. What investigations might be helpful? (Name THREE, state how it might be helpful)
Question 2 1. Nitrous oxide is contraindicated in patients with pneumothorax, pneumopericardium or intestinal obstruction because it 2. ____________. 2. Thiopentone is short acting because ________.
Question 2 3. Suxamethonium should be used with caution in patients with renal failure because ____________. 4. Name TWO likely complications of the use of epidural morphine for postop analgesia.
Question 2 5. Propofol causes cardiovascular depression by _______.
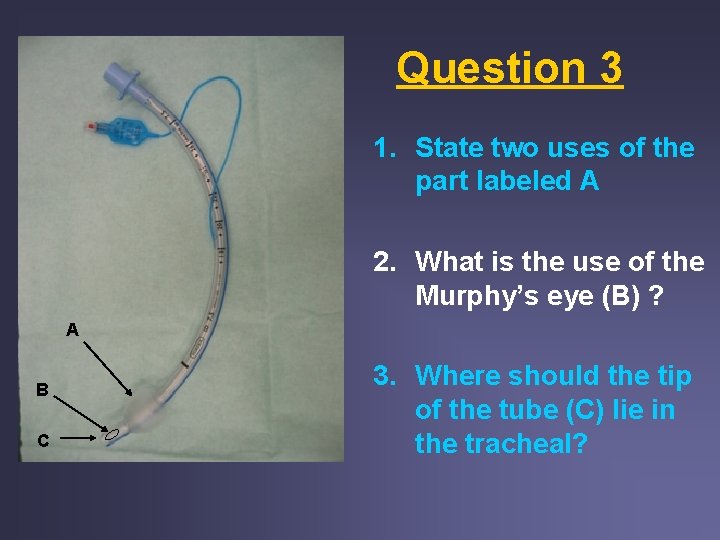
Question 3 1. State two uses of the part labeled A 2. What is the use of the Murphy’s eye (B) ? A B C 3. Where should the tip of the tube (C) lie in the tracheal?
Question 3 4. Name two methods of confirming a trachea intubation 5. State 4 complications of trachea intubation
Question 4 60 year old man had upper abdominal incision for total gastrectomy. 1. Name TWO methods of pain relief appropriate for this patient apart from intra-muscular analgesics. 2. Give THREE medical reasons for providing good post-operative pain relief?
Question 4 3. Different patient require different amount of intramuscular morphine for similar operation. Give TWO reasons why this happens? 4. Write a postoperative order for analgesia for this patient? 5. State TWO complications of this choice of analgesia.
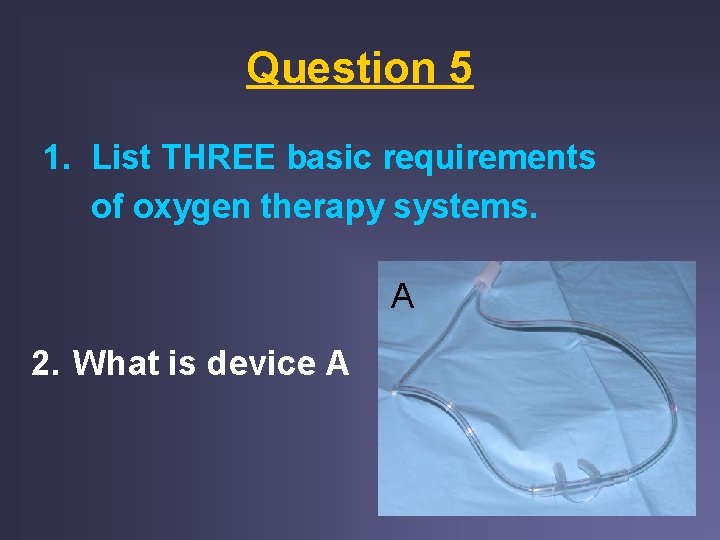
Question 5 1. List THREE basic requirements of oxygen therapy systems. A 2. What is device A
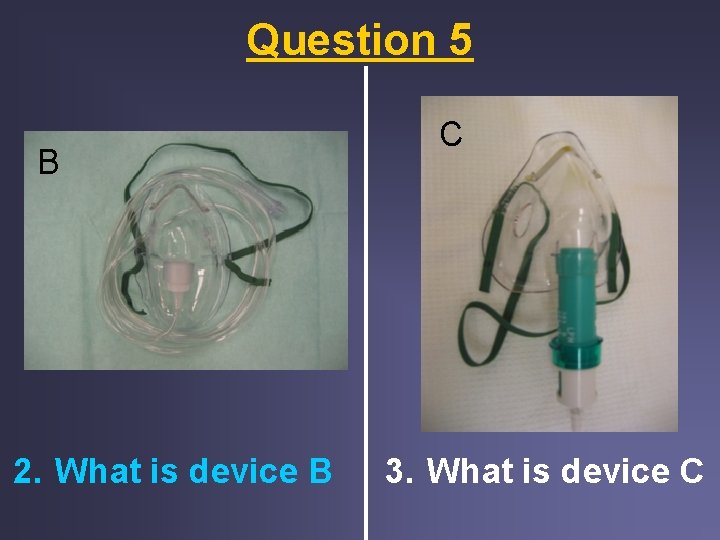
Question 5 B 2. What is device B C 3. What is device C
Question 5 3. Name THREE complications of oxygen therapy.
Question 6 A 60 year old patient is scheduled for a cystocopy under anaesthesia. He gives a history of hypertension. He also had a previous general anaesthesia for haemorrhoidectomy. On examination, his BP was 130/80 mm. Hg. 1. List 3 reasons for conducting a preoperative visit.
Question 6 2. What is his ASA status? 3. List 2 useful anaesthesia related information can you drive from his previous anaesthesia record.
Question 6 4. If the patient appear very anxious, what can be done to help him? State 2 measures. 5. If the patient in on atenolol and nifedipine for hypertension would you stop the medication on the day of surgery?
Question 7 A 51 -year-old sales executive presents for extracton of his wisdom teeth. He has not seen a doctor for many years, and is not taking any medication. On admission to the ward, his blood pressure was found to be 170/110 mm. Hg. He weighs 80 kg. 1. Comment on his blood pressure on admission. How would you check on this reading.
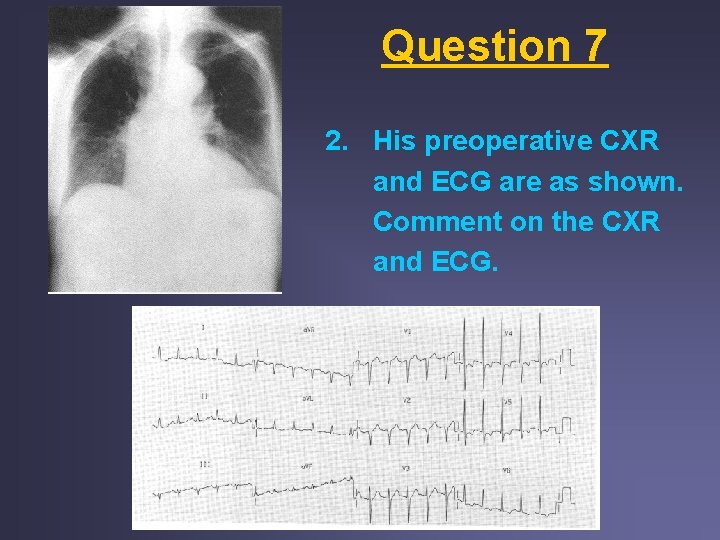
Question 7 2. His preoperative CXR and ECG are as shown. Comment on the CXR and ECG.
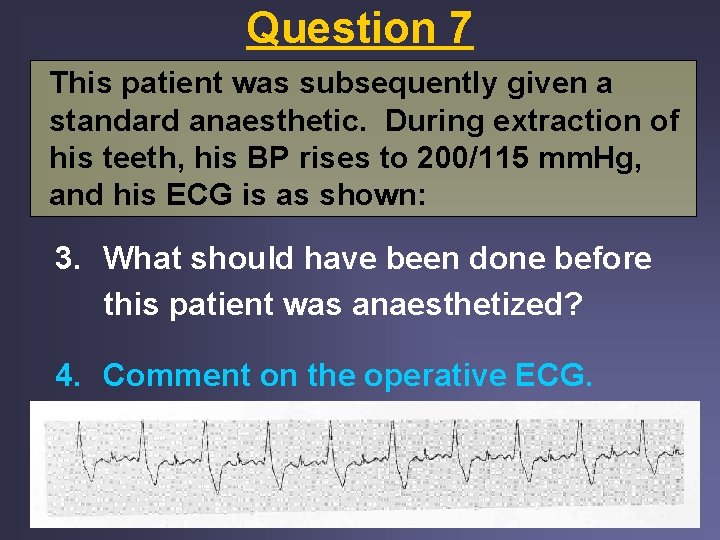
Question 7 This patient was subsequently given a standard anaesthetic. During extraction of his teeth, his BP rises to 200/115 mm. Hg, and his ECG is as shown: 3. What should have been done before this patient was anaesthetized? 4. Comment on the operative ECG.
Question 8 1. In an adult, name a suitable space in which a spinal block can safely be performed? 2. Why is it safe to perform the spinal block at that space? 3. The anaesthetist chose to perform the spinal block with a rounded 27 G spinal needle. What complications was he trying to avoid by using this needle?
Question 8 4. What are the patient risk factors for the above complication? Name TWO factors. 5. How does the anaesthetist know that he has reached the subarachnoid space with the spinal needle. Give ONE answer.
Question 8 6. After establishing that the spinal needle was in the subarachnoid space, the anaesthetist proceeded to inject 2. 5 ml of 0. 5% heavy bupivacaine. The spinal block was established to a level of T 6. What is the likely cardiovascular complications that you will see? Name the most likely.
Question 8 7. How will you deal with this complication? Name 2 answers. 8. If the block had extended to a level of T 1, what additional cardiovascular complication are you likely to see. Name ONE answer.
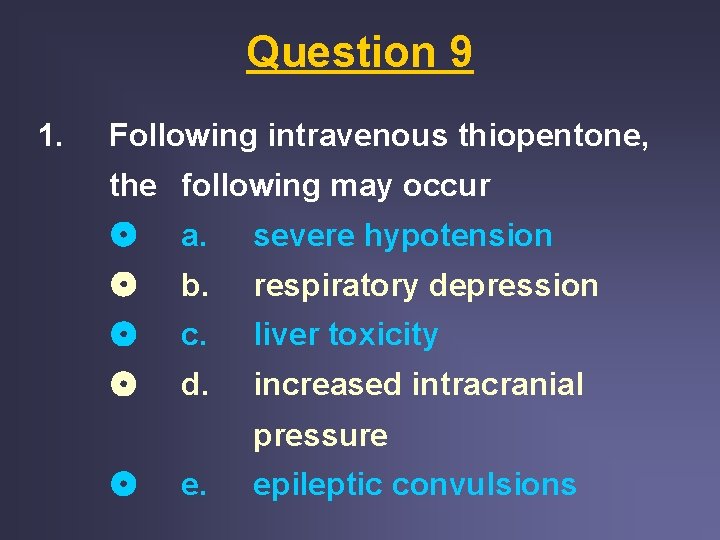
Question 9 1. Following intravenous thiopentone, the following may occur a. severe hypotension b. respiratory depression c. liver toxicity d. increased intracranial pressure e. epileptic convulsions
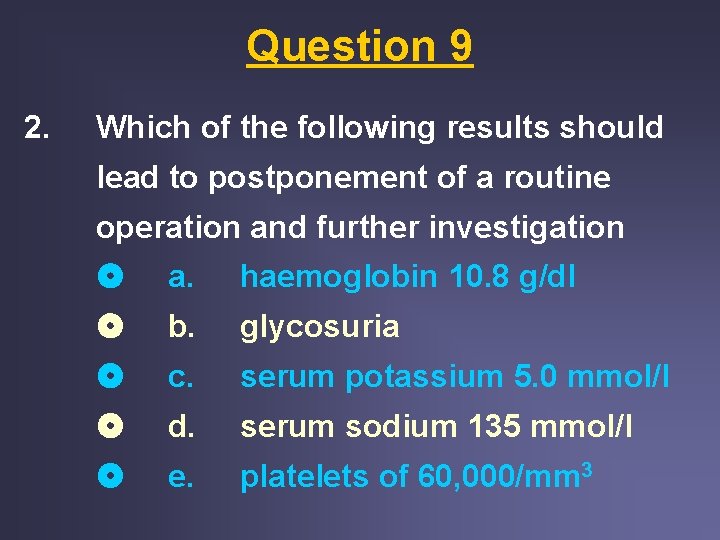
Question 9 2. Which of the following results should lead to postponement of a routine operation and further investigation a. haemoglobin 10. 8 g/dl b. glycosuria c. serum potassium 5. 0 mmol/l d. serum sodium 135 mmol/l e. platelets of 60, 000/mm 3
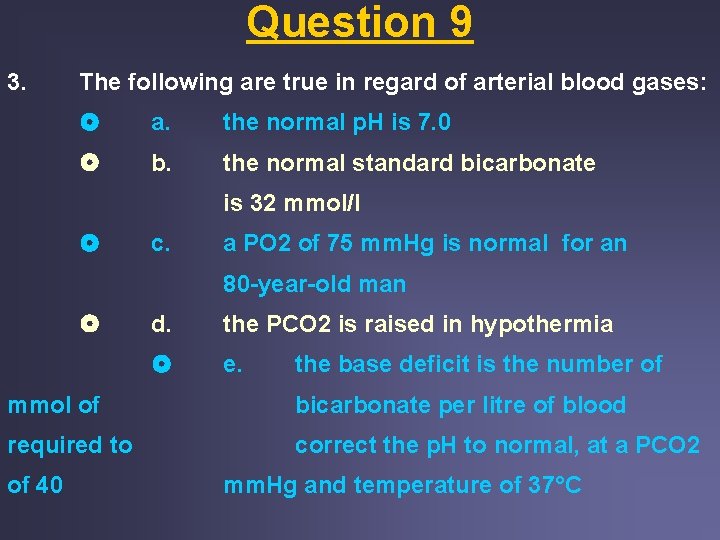
Question 9 3. The following are true in regard of arterial blood gases: a. the normal p. H is 7. 0 b. the normal standard bicarbonate is 32 mmol/l c. a PO 2 of 75 mm. Hg is normal for an 80 -year-old man d. the PCO 2 is raised in hypothermia e. the base deficit is the number of mmol of bicarbonate per litre of blood required to correct the p. H to normal, at a PCO 2 of 40 mm. Hg and temperature of 37°C
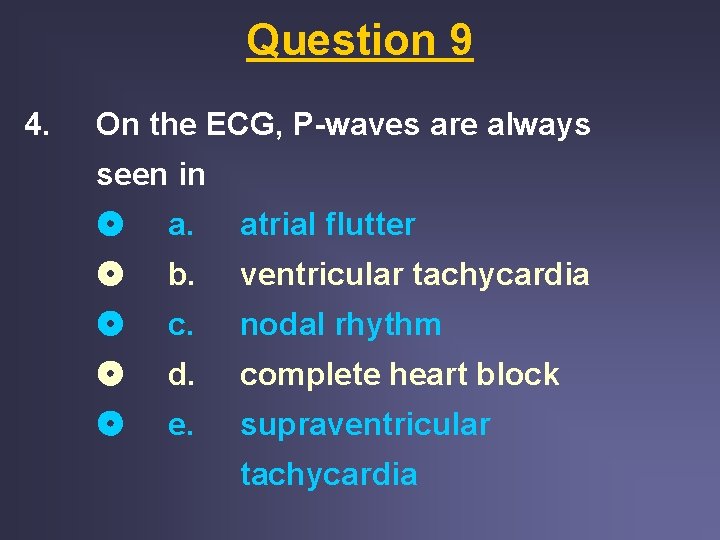
Question 9 4. On the ECG, P-waves are always seen in a. atrial flutter b. ventricular tachycardia c. nodal rhythm d. complete heart block e. supraventricular tachycardia
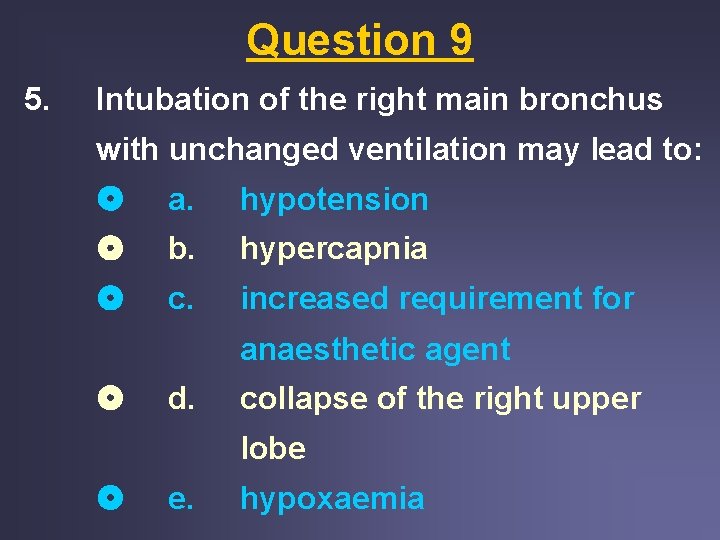
Question 9 5. Intubation of the right main bronchus with unchanged ventilation may lead to: a. hypotension b. hypercapnia c. increased requirement for anaesthetic agent d. collapse of the right upper lobe e. hypoxaemia
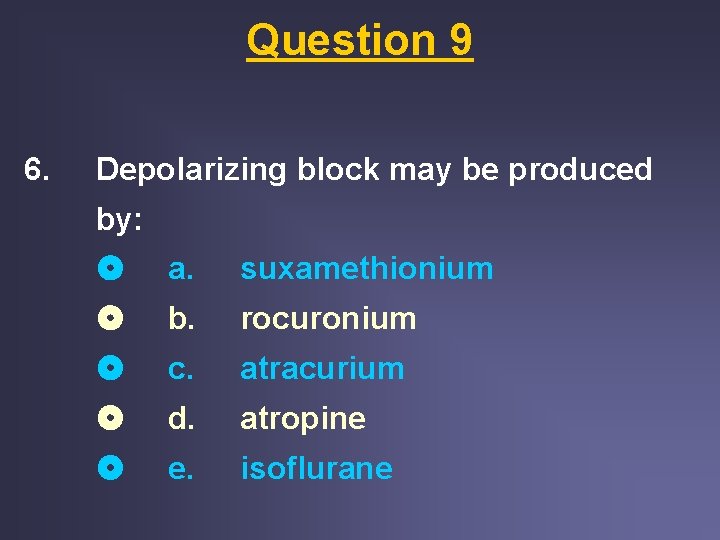
Question 9 6. Depolarizing block may be produced by: a. suxamethionium b. rocuronium c. atracurium d. atropine e. isoflurane
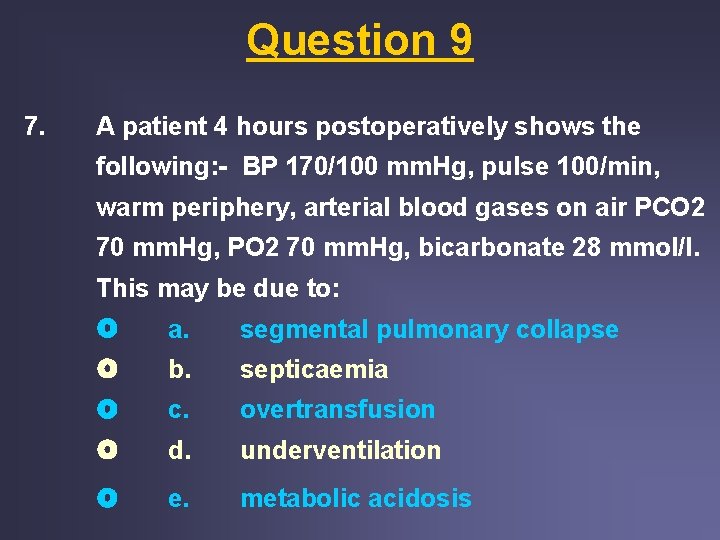
Question 9 7. A patient 4 hours postoperatively shows the following: - BP 170/100 mm. Hg, pulse 100/min, warm periphery, arterial blood gases on air PCO 2 70 mm. Hg, PO 2 70 mm. Hg, bicarbonate 28 mmol/l. This may be due to: a. segmental pulmonary collapse b. septicaemia c. overtransfusion d. underventilation e. metabolic acidosis
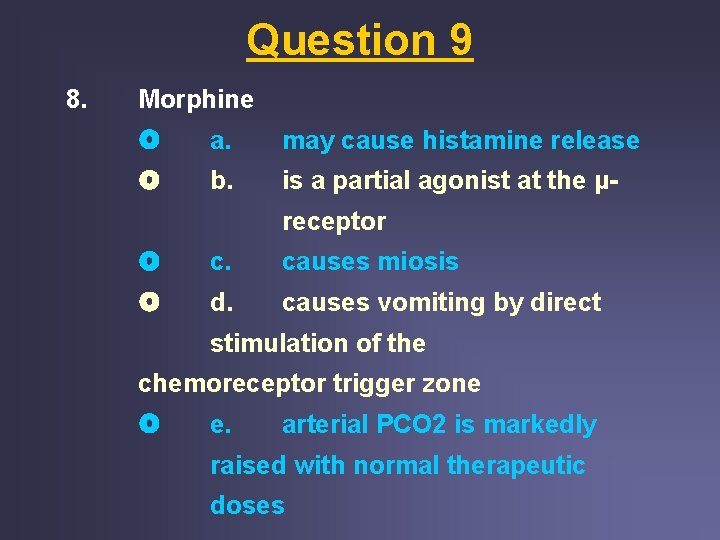
Question 9 8. Morphine a. may cause histamine release b. is a partial agonist at the μreceptor c. causes miosis d. causes vomiting by direct stimulation of the chemoreceptor trigger zone e. arterial PCO 2 is markedly raised with normal therapeutic doses
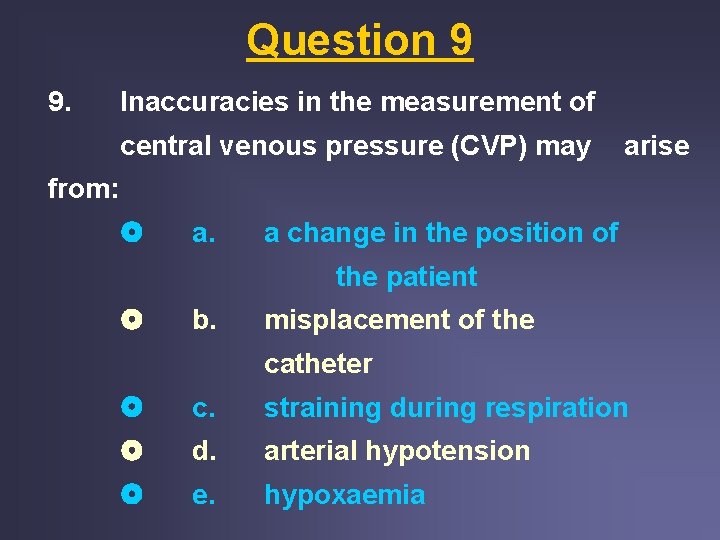
Question 9 9. Inaccuracies in the measurement of central venous pressure (CVP) may arise from: a. a change in the position of the patient b. misplacement of the catheter c. straining during respiration d. arterial hypotension e. hypoxaemia
Question 9 10. Cardiac output is increased by: a. a rise in venous filling pressure b. a rise in body temperature c. an increased metabolic rate d. standing up from the lying position e. pregnancy in the last trimester

THE END ****
- Slides: 34