OSA SYNDROME AND ALLERGIC RESPIRATORY DISEASES Upper Airway

- Slides: 25
OSA SYNDROME AND ALLERGIC RESPIRATORY DISEASES Upper Airway Diseases A. Kaditis, MD Pediatric Pulmonology Unit, Sleep Disorders Laboratory First Department of Pediatrics University of Athens School of Medicine and Aghia Sophia Children’s Hospital Athens, Greece
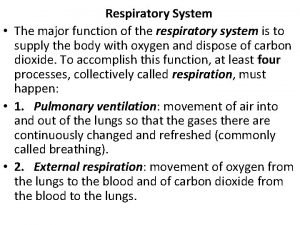
Obstructive Sleep-Disordered Breathing (SDB) Spectrum of abnormal respiratory patterns during sleep characterized by snoring and increased respiratory effort n n Primary snoring Upper airway resistance syndrome Obstructive hypoventilation Obstructive sleep apnea (OSA)
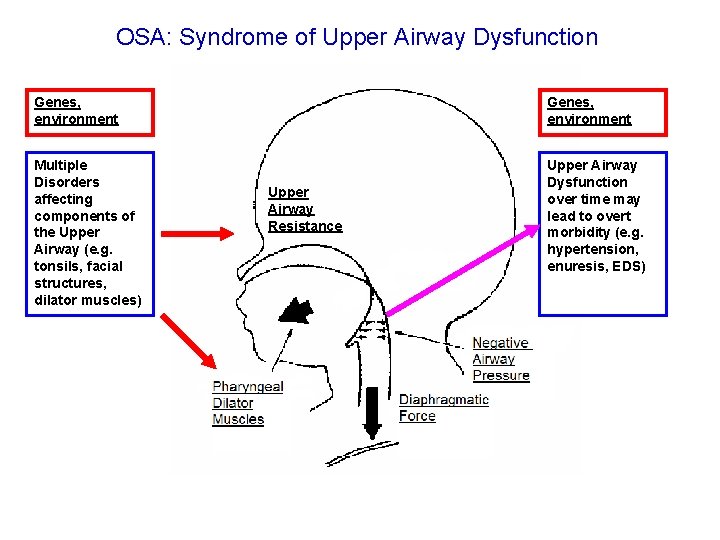
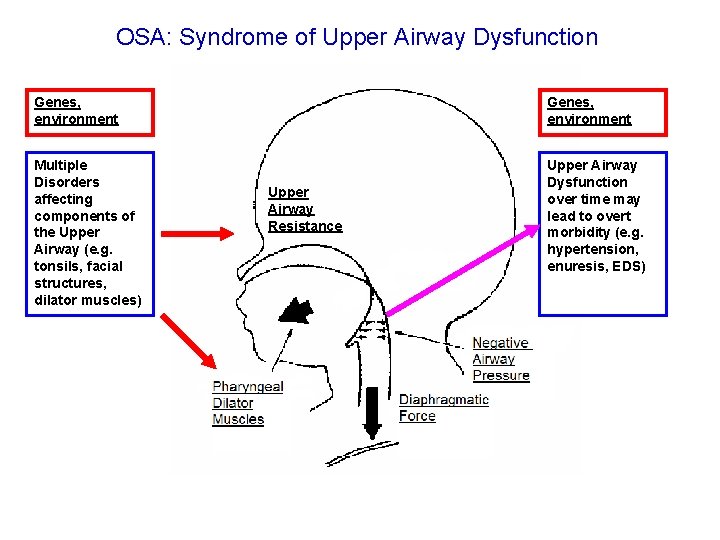
OSA: Syndrome of Upper Airway Dysfunction Genes, environment Multiple Disorders affecting components of the Upper Airway (e. g. tonsils, facial structures, dilator muscles) Upper Airway Dysfunction over time may lead to overt morbidity (e. g. hypertension, enuresis, EDS) Upper Airway Resistance
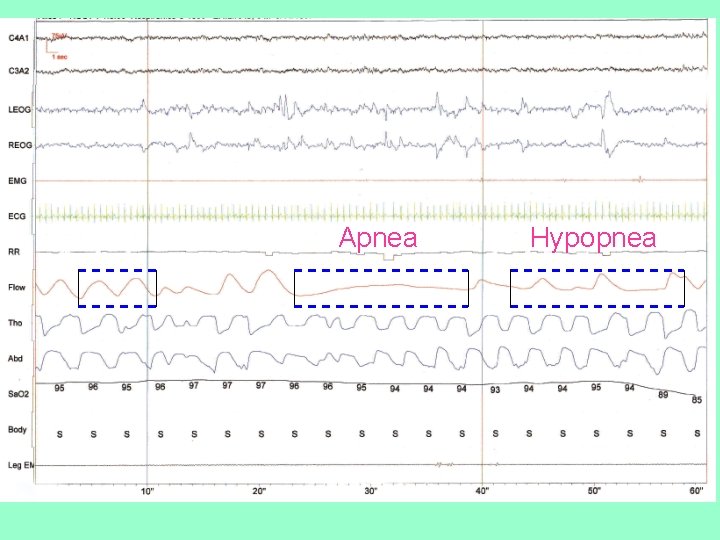
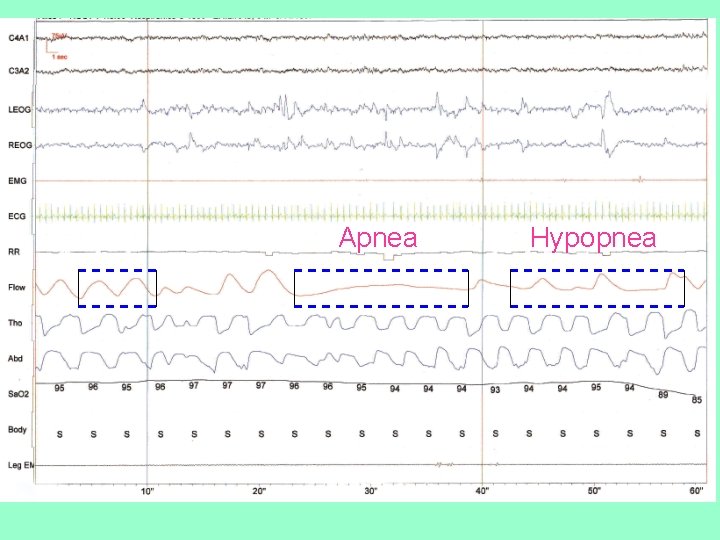
Apnea Hypopnea
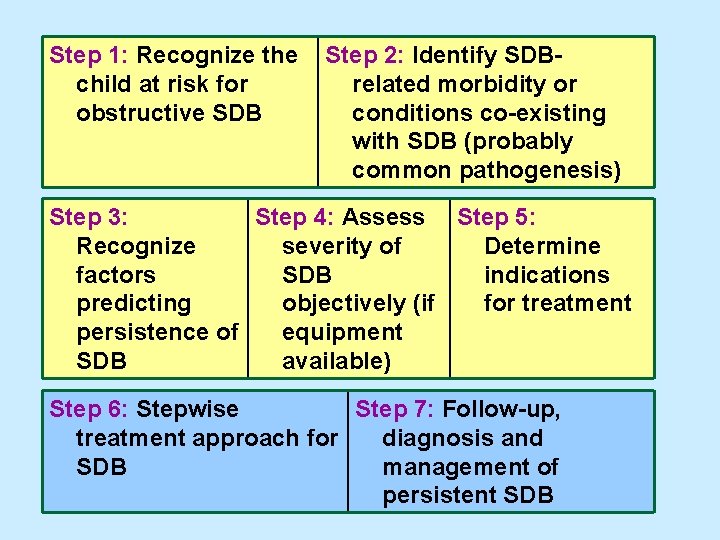
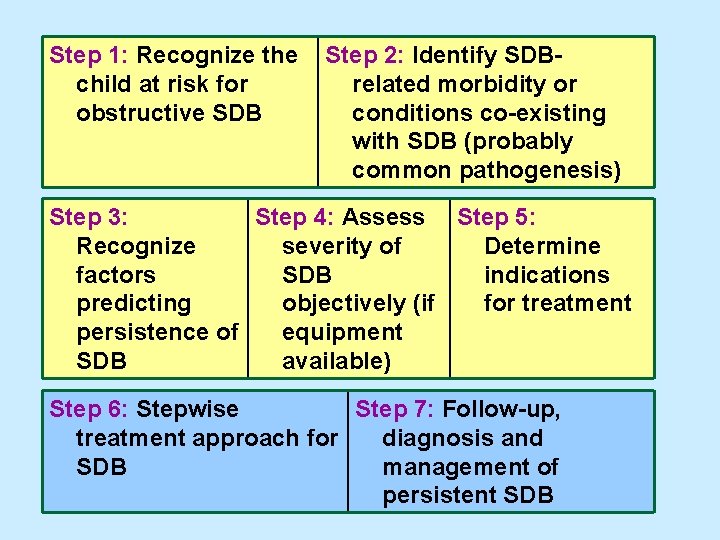
Step 1: Recognize the child at risk for obstructive SDB Step 2: Identify SDBrelated morbidity or conditions co-existing with SDB (probably common pathogenesis) Step 3: Step 4: Assess Step 5: Recognize severity of Determine factors SDB indications predicting objectively (if for treatment persistence of equipment SDB available) Step 6: Stepwise Step 7: Follow-up, treatment approach for diagnosis and SDB management of persistent SDB
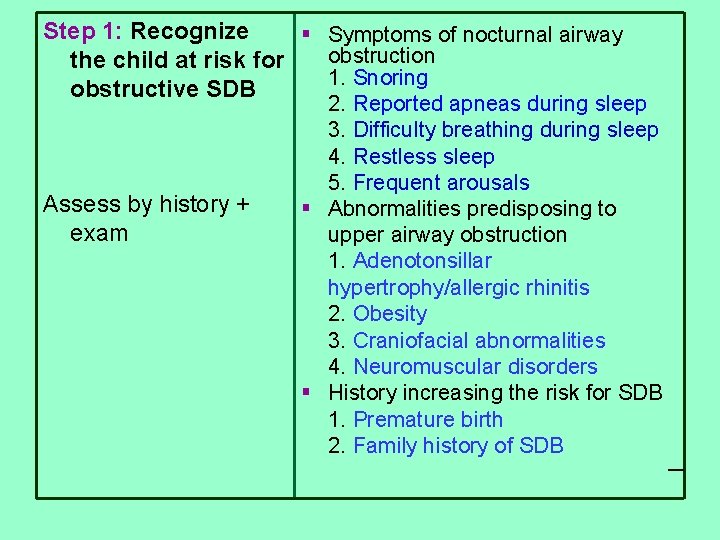
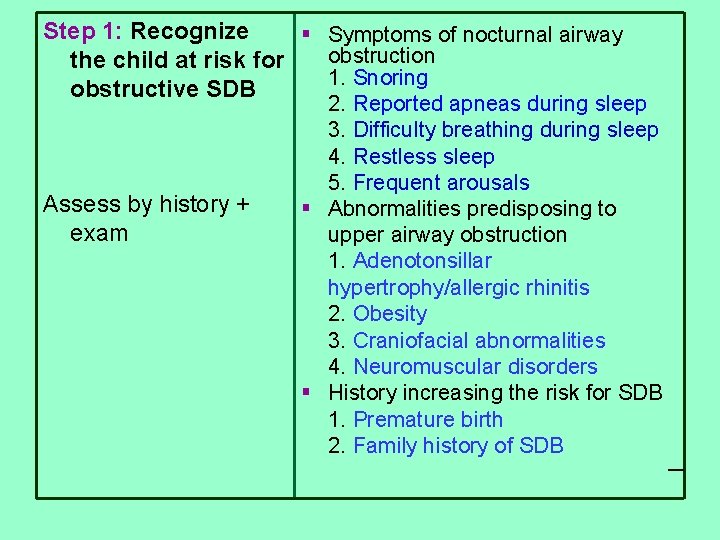
Step 1: Recognize § Symptoms of nocturnal airway obstruction the child at risk for 1. Snoring obstructive SDB Assess by history + exam 2. Reported apneas during sleep 3. Difficulty breathing during sleep 4. Restless sleep 5. Frequent arousals § Abnormalities predisposing to upper airway obstruction 1. Adenotonsillar hypertrophy/allergic rhinitis 2. Obesity 3. Craniofacial abnormalities 4. Neuromuscular disorders § History increasing the risk for SDB 1. Premature birth 2. Family history of SDB
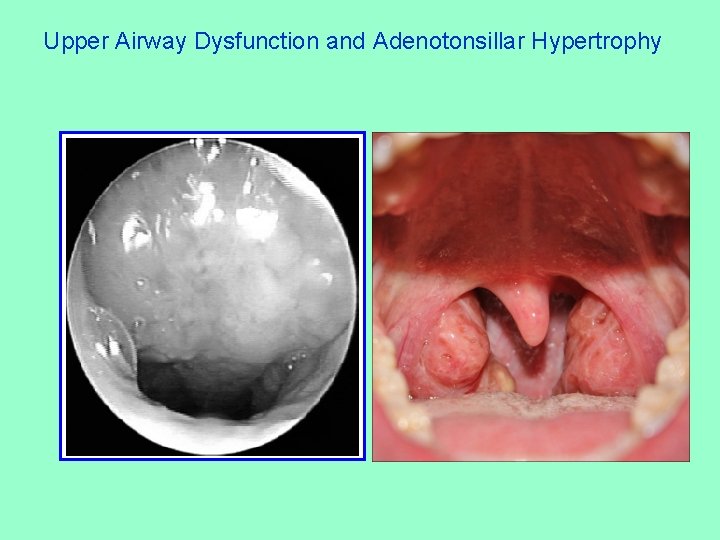
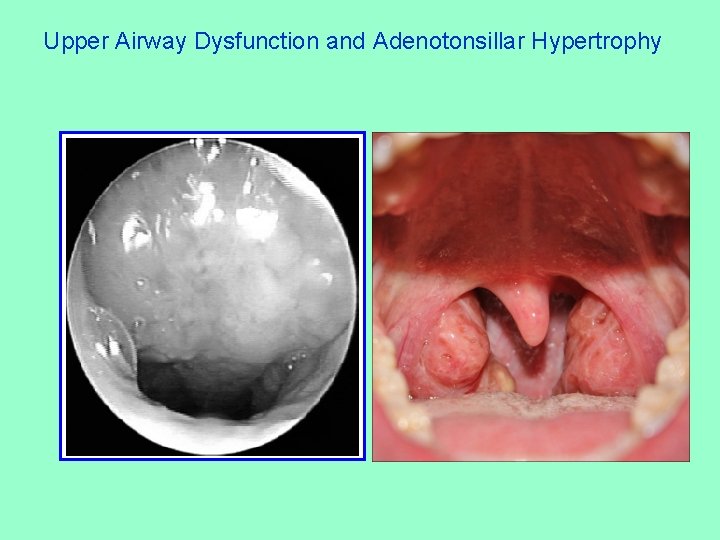
Upper Airway Dysfunction and Adenotonsillar Hypertrophy

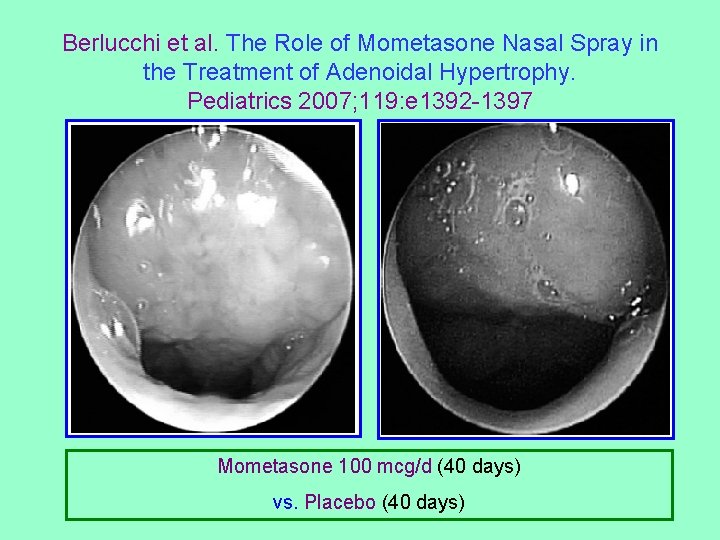
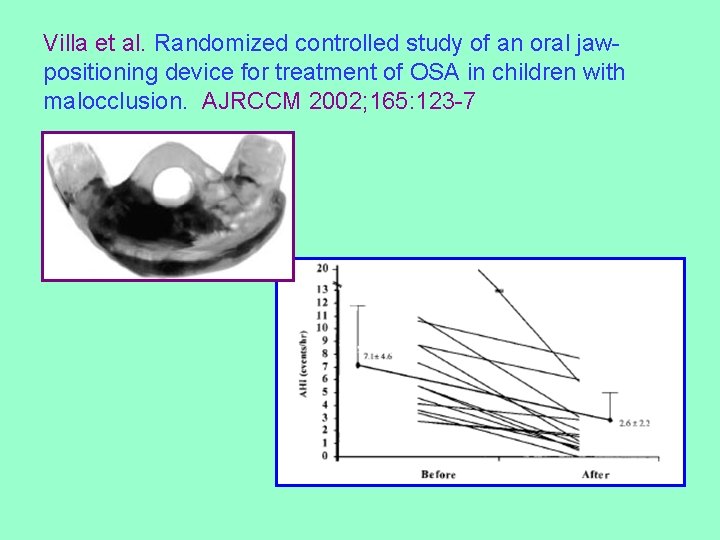
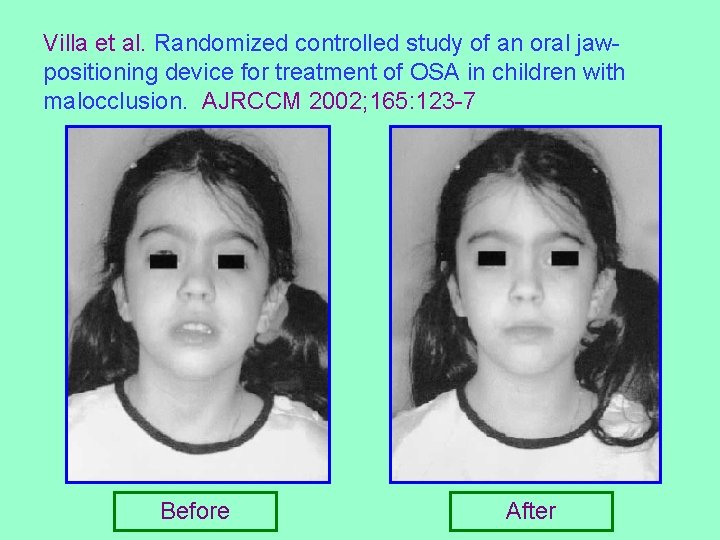
Villa et al. Randomized controlled study of an oral jaw-positioning device for treatment of OSA in children with malocclusion. AJRCCM 2002; 165: 123 -7
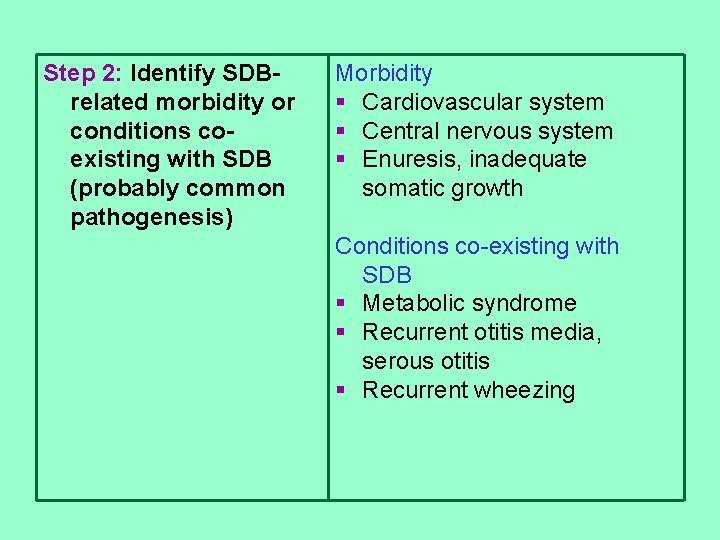
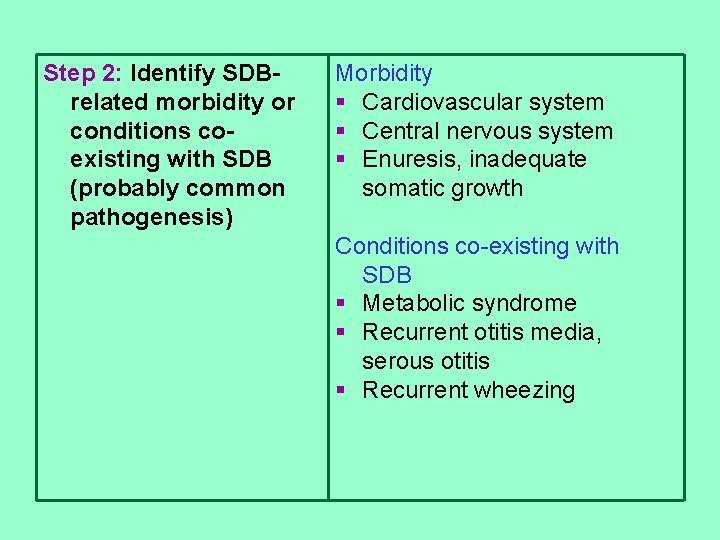
Step 2: Identify SDBrelated morbidity or conditions coexisting with SDB (probably common pathogenesis) Morbidity § Cardiovascular system § Central nervous system § Enuresis, inadequate somatic growth Conditions co-existing with SDB § Metabolic syndrome § Recurrent otitis media, serous otitis § Recurrent wheezing
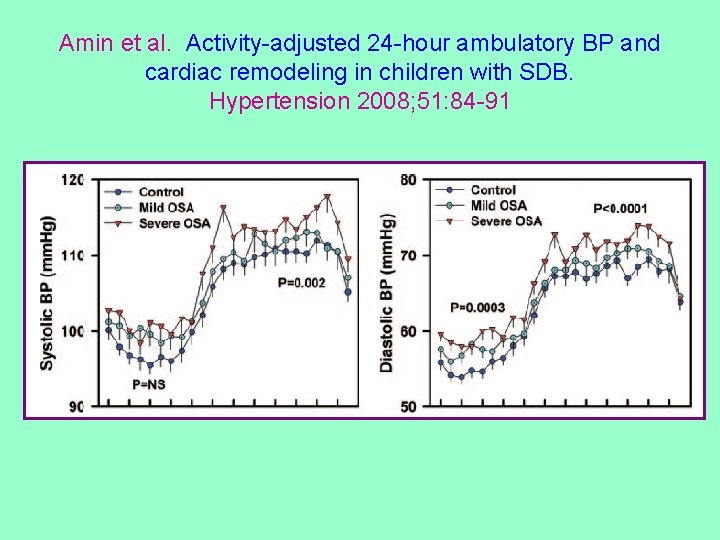
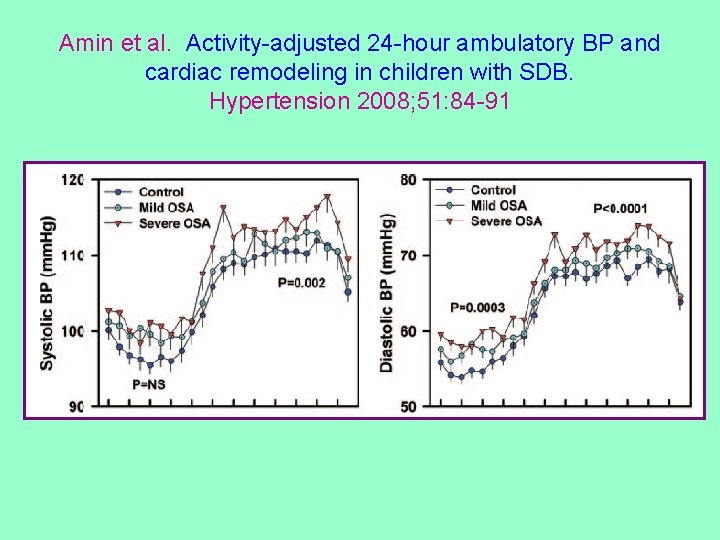
Amin et al. Activity-adjusted 24 -hour ambulatory BP and cardiac remodeling in children with SDB. Hypertension 2008; 51: 84 -91
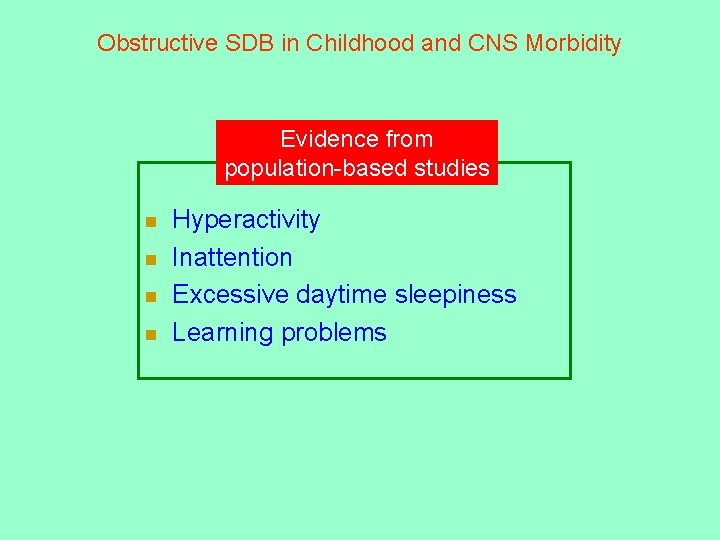
Obstructive SDB in Childhood and CNS Morbidity Evidence from population-based studies n n Hyperactivity Inattention Excessive daytime sleepiness Learning problems
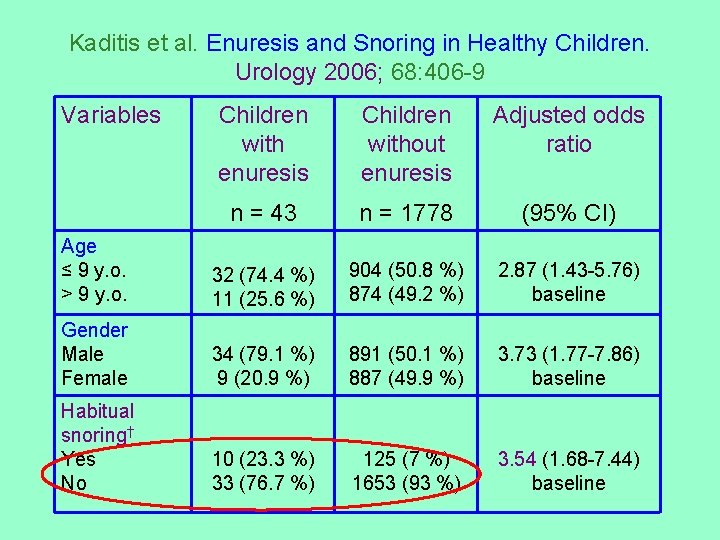
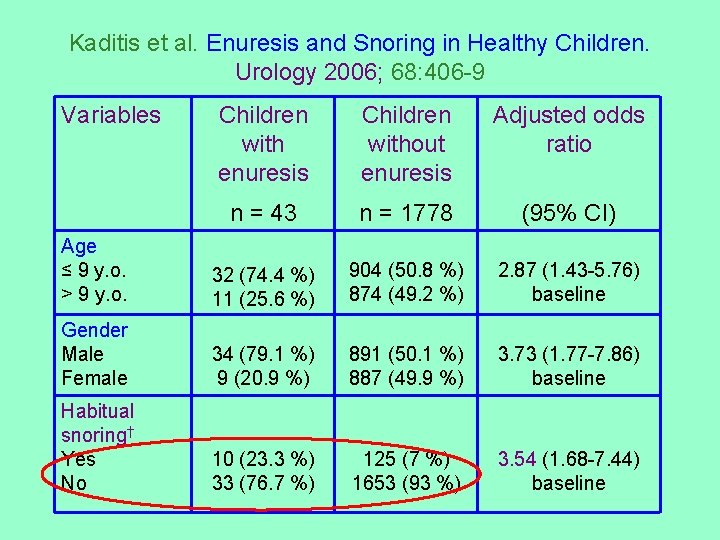
Kaditis et al. Enuresis and Snoring in Healthy Children. Urology 2006; 68: 406 -9 Variables Children with enuresis Children without enuresis Adjusted odds ratio n = 43 n = 1778 (95% CI) Age ≤ 9 y. o. > 9 y. o. 32 (74. 4 %) 11 (25. 6 %) 904 (50. 8 %) 874 (49. 2 %) 2. 87 (1. 43 -5. 76) baseline Gender Male Female 34 (79. 1 %) 9 (20. 9 %) 891 (50. 1 %) 887 (49. 9 %) 3. 73 (1. 77 -7. 86) baseline Habitual snoring† Yes No 10 (23. 3 %) 33 (76. 7 %) 125 (7 %) 1653 (93 %) 3. 54 (1. 68 -7. 44) baseline
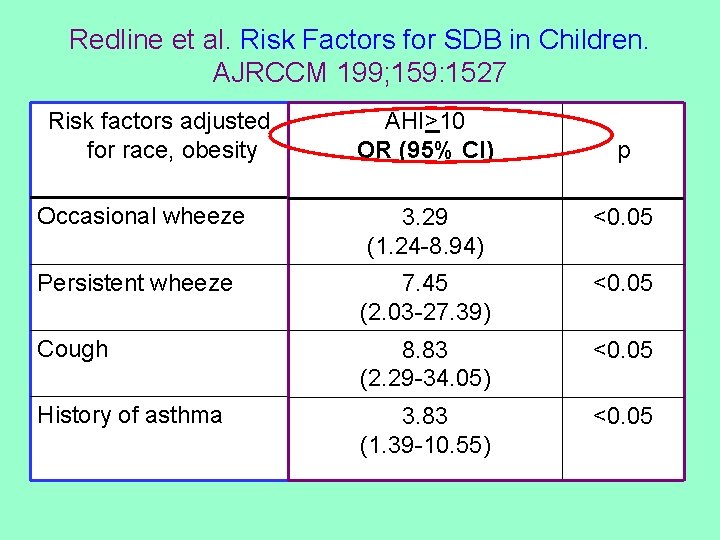
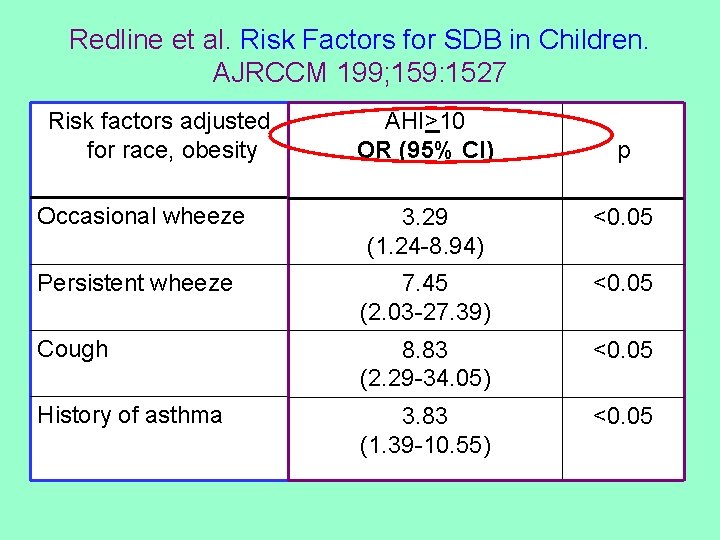
Redline et al. Risk Factors for SDB in Children. AJRCCM 199; 159: 1527 Risk factors adjusted for race, obesity AHI>10 OR (95% CI) p Occasional wheeze 3. 29 (1. 24 -8. 94) <0. 05 Persistent wheeze 7. 45 (2. 03 -27. 39) <0. 05 Cough 8. 83 (2. 29 -34. 05) <0. 05 History of asthma 3. 83 (1. 39 -10. 55) <0. 05
Step 3: Recognize factors predicting § Male gender persistence of SDB in § Obesity the long term § Increasing body mass index percentile
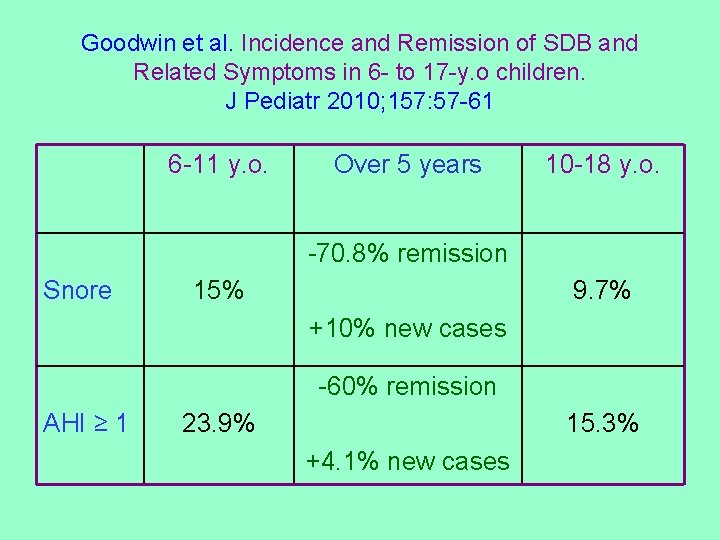
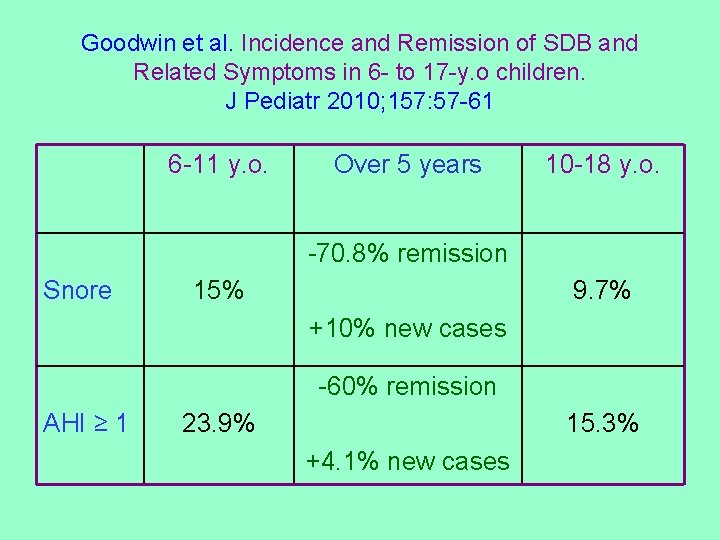
Goodwin et al. Incidence and Remission of SDB and Related Symptoms in 6 - to 17 -y. o children. J Pediatr 2010; 157: 57 -61 6 -11 y. o. Over 5 years 10 -18 y. o. -70. 8% remission Snore 15% 9. 7% +10% new cases -60% remission AHI ≥ 1 23. 9% 15. 3% +4. 1% new cases
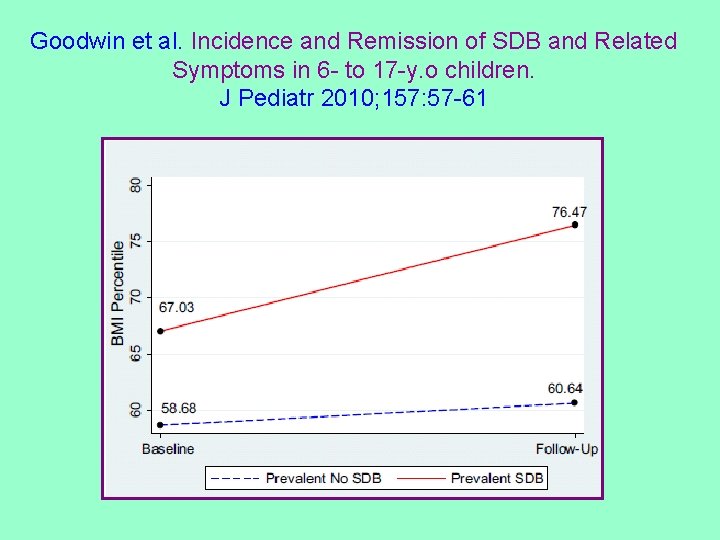
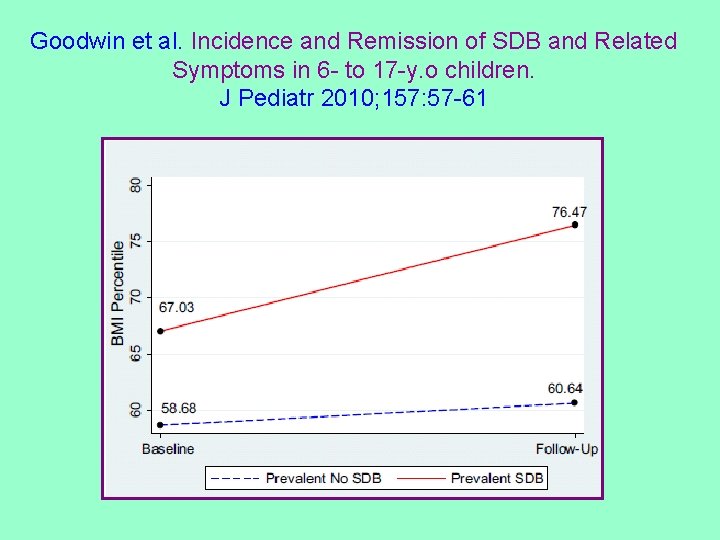
Goodwin et al. Incidence and Remission of SDB and Related Symptoms in 6 - to 17 -y. o children. J Pediatr 2010; 157: 57 -61
Step 4: Assess severity of SDB objectively (if § Nocturnal polysomnography equipment available) § Nocturnal polygraphy § Nocturnal oximetry
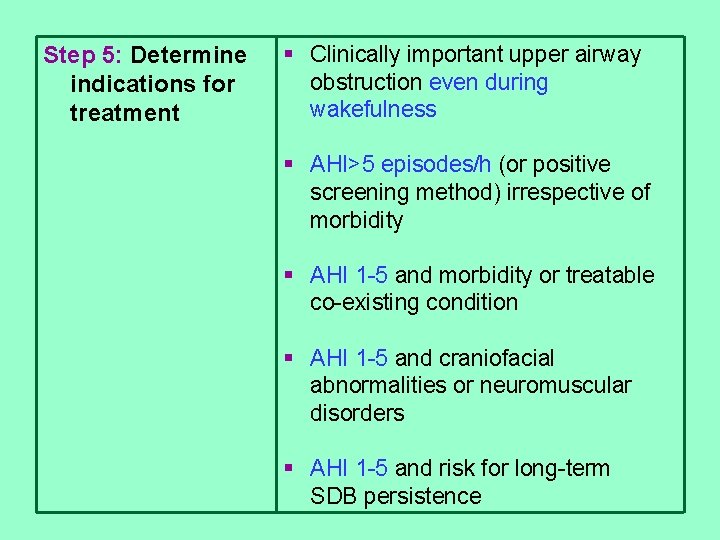
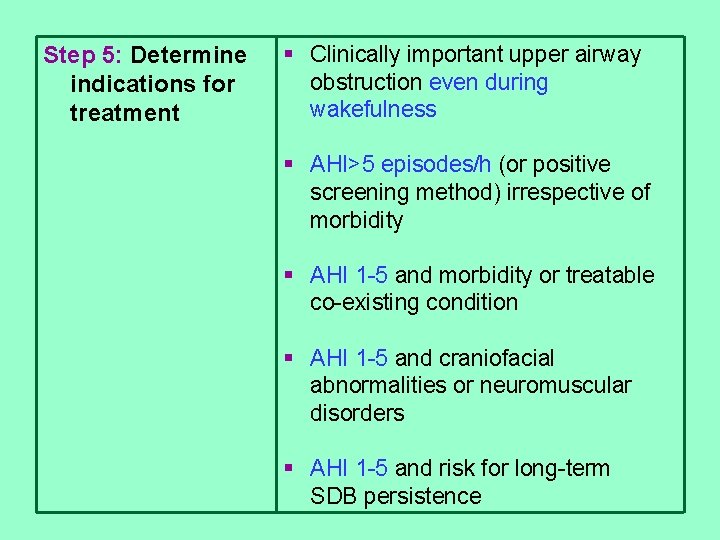
Step 5: Determine indications for treatment § Clinically important upper airway obstruction even during wakefulness § AHI>5 episodes/h (or positive screening method) irrespective of morbidity § AHI 1 -5 and morbidity or treatable co-existing condition § AHI 1 -5 and craniofacial abnormalities or neuromuscular disorders § AHI 1 -5 and risk for long-term SDB persistence
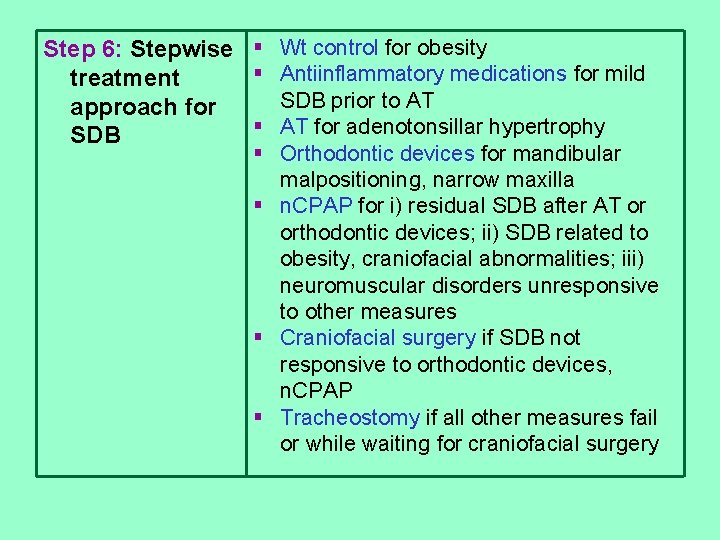
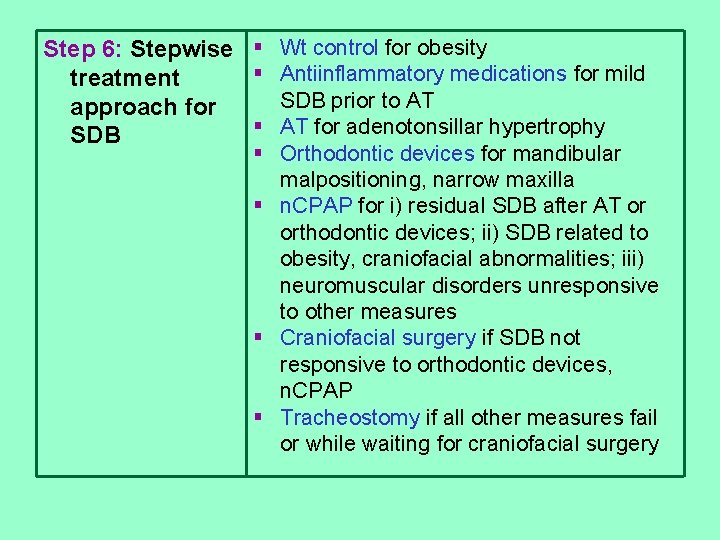
Step 6: Stepwise § Wt control for obesity § Antiinflammatory medications for mild treatment SDB prior to AT approach for § AT for adenotonsillar hypertrophy SDB § Orthodontic devices for mandibular malpositioning, narrow maxilla § n. CPAP for i) residual SDB after AT or orthodontic devices; ii) SDB related to obesity, craniofacial abnormalities; iii) neuromuscular disorders unresponsive to other measures § Craniofacial surgery if SDB not responsive to orthodontic devices, n. CPAP § Tracheostomy if all other measures fail or while waiting for craniofacial surgery
Berlucchi et al. The Role of Mometasone Nasal Spray in the Treatment of Adenoidal Hypertrophy. Pediatrics 2007; 119: e 1392 -1397 Mometasone 100 mcg/d (40 days) vs. Placebo (40 days)
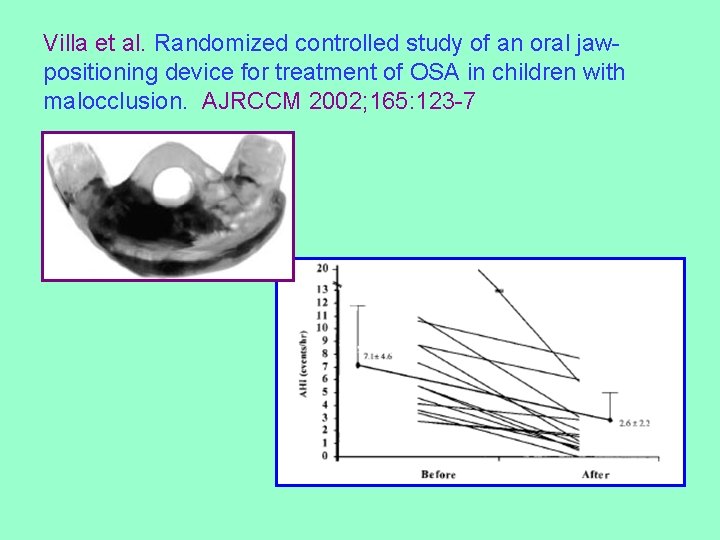
Villa et al. Randomized controlled study of an oral jawpositioning device for treatment of OSA in children with malocclusion. AJRCCM 2002; 165: 123 -7
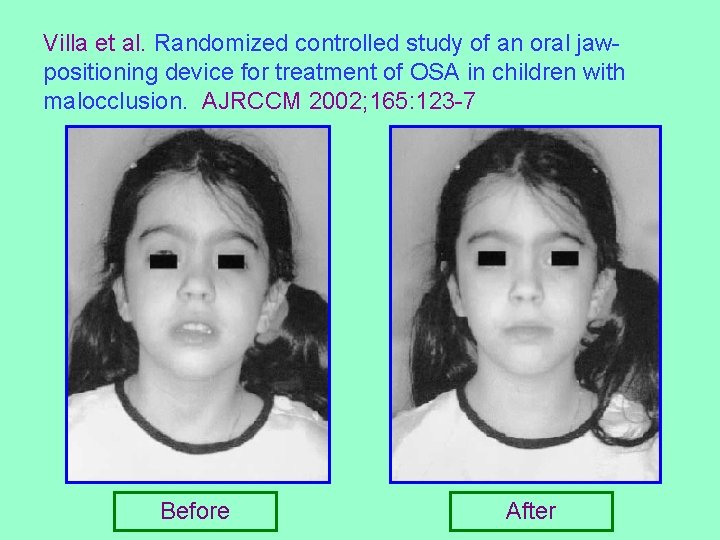
Villa et al. Randomized controlled study of an oral jawpositioning device for treatment of OSA in children with malocclusion. AJRCCM 2002; 165: 123 -7 Before After
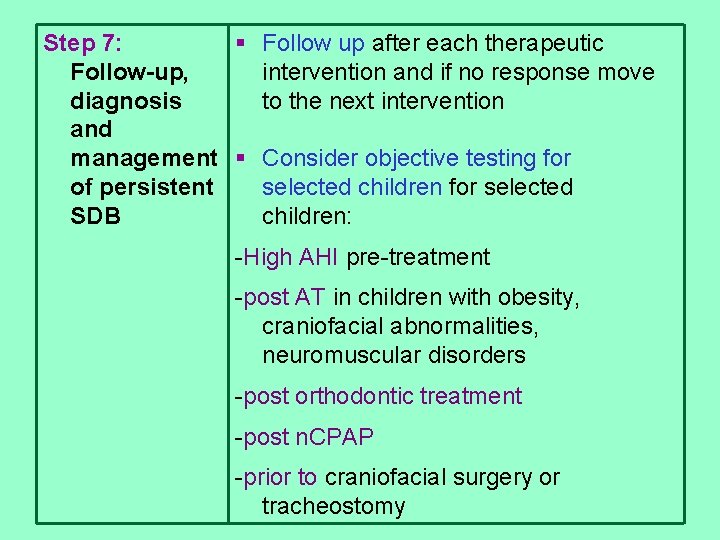
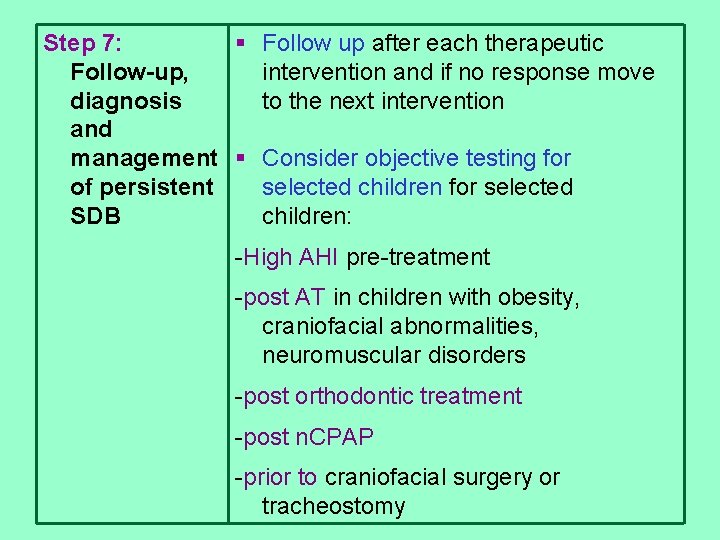
Step 7: § Follow up after each therapeutic Follow-up, intervention and if no response move diagnosis to the next intervention and management § Consider objective testing for of persistent selected children for selected SDB children: -High AHI pre-treatment -post AT in children with obesity, craniofacial abnormalities, neuromuscular disorders -post orthodontic treatment -post n. CPAP -prior to craniofacial surgery or tracheostomy
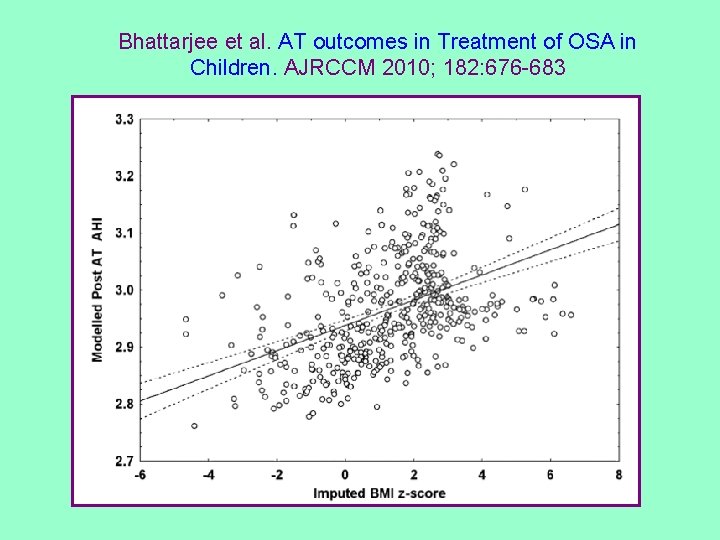
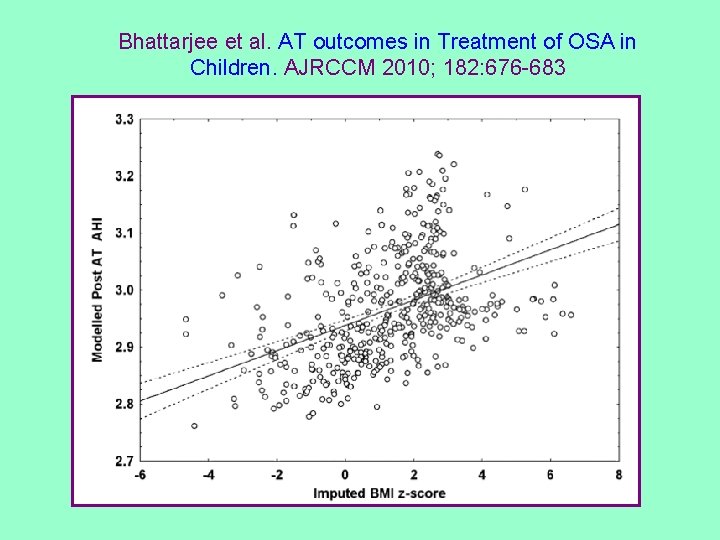
Bhattarjee et al. AT outcomes in Treatment of OSA in Children. AJRCCM 2010; 182: 676 -683
Conclusions Intermittent upper airway obstruction during sleep in childhood: § Is associated with disorders affecting upper airway resistance and pharyngeal neuromotor tone § Is related to morbidity from the CNS and the cardiovascular system § Severe upper airway obstruction during sleep and mild obstruction with morbidity or risk factors for persistence should be treated § All disorders leading to upper airway obstruction should be addressed in a stepwise fashion
 Airway grade view
Airway grade view Norwich terrier upper airway syndrome
Norwich terrier upper airway syndrome Pulmonary tract
Pulmonary tract Respiratory airway secretary
Respiratory airway secretary Sphyx medical term
Sphyx medical term Global alliance against chronic respiratory diseases
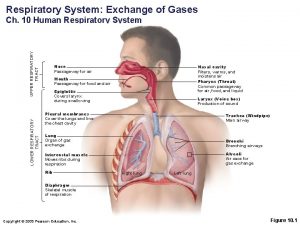
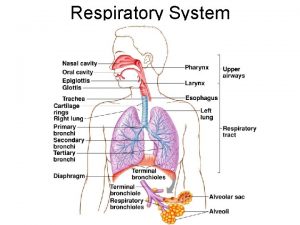
Global alliance against chronic respiratory diseases Upper and lower respiratory system
Upper and lower respiratory system Respiratory zone
Respiratory zone Upper respiratory tract anatomy
Upper respiratory tract anatomy Classification of upper respiratory tract infection
Classification of upper respiratory tract infection Anatomy of the upper respiratory tract
Anatomy of the upper respiratory tract Phelebetomy
Phelebetomy Upper rti
Upper rti Upper respiratory tract
Upper respiratory tract Acute upper respiratory infection unspecified คือ
Acute upper respiratory infection unspecified คือ Upper cross syndrome
Upper cross syndrome Allergic conjunctivitis case report
Allergic conjunctivitis case report Wolowitz allergic reaction
Wolowitz allergic reaction Allergic conjunctivitis icd-9
Allergic conjunctivitis icd-9 Type of allergic reaction
Type of allergic reaction Atopic dermatitis vs contact dermatitis
Atopic dermatitis vs contact dermatitis Management of allergic rhinitis
Management of allergic rhinitis Aria classification of allergic rhinitis
Aria classification of allergic rhinitis Allergy shiners
Allergy shiners Hemolytic transfusion reaction
Hemolytic transfusion reaction Rhinitis medicamentosa
Rhinitis medicamentosa