Orthopedic Causes of Edema John R Bartholomew MD
Orthopedic Causes of Edema • John R. Bartholomew, MD, MSVM, FACC • Section Head - Vascular Medicine • Department of Cardiovascular Medicine • Professor of Medicine - Cleveland Clinic Lerner College of Medicine • Cleveland Clinic
Clinical Causes of Edema • Obstruction of venous and lymphatic drainage • Congestive heart failure • Nephrotic syndrome and other hypoalbuminemic states • Acute glomerulonephritis and other forms of renal failure • Cirrhosis • Hypothyroidism (Myxedema) • Drug-induced edema • Nutritional • Idiopathic edema
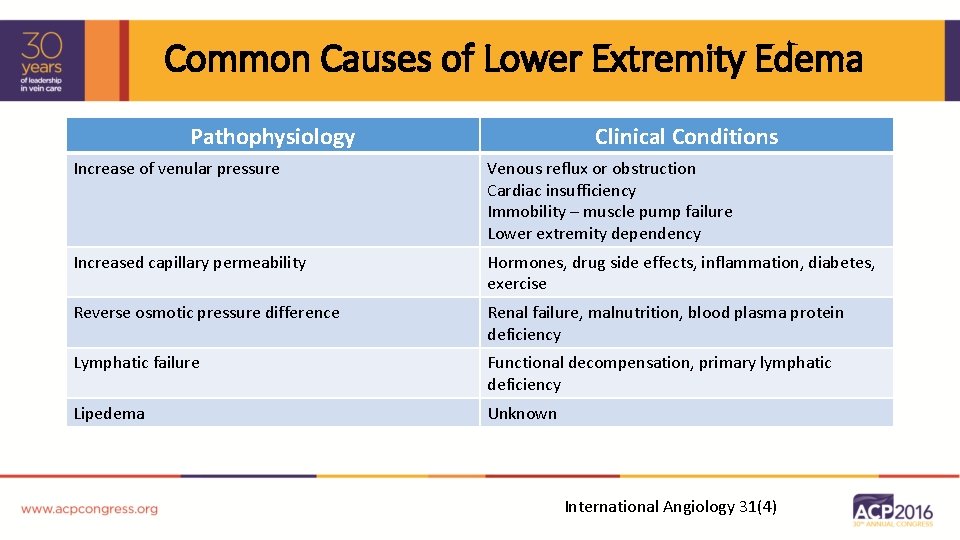
Common Causes of Lower Extremity Edema Pathophysiology Clinical Conditions Increase of venular pressure Venous reflux or obstruction Cardiac insufficiency Immobility – muscle pump failure Lower extremity dependency Increased capillary permeability Hormones, drug side effects, inflammation, diabetes, exercise Reverse osmotic pressure difference Renal failure, malnutrition, blood plasma protein deficiency Lymphatic failure Functional decompensation, primary lymphatic deficiency Lipedema Unknown International Angiology 31(4)
Orthopedic Causes of Edema • Common problem for orthopedic physicians • Number of different causes • Not a disease - a sign of an underlying disorder • May be a minor disorder or a serious problem
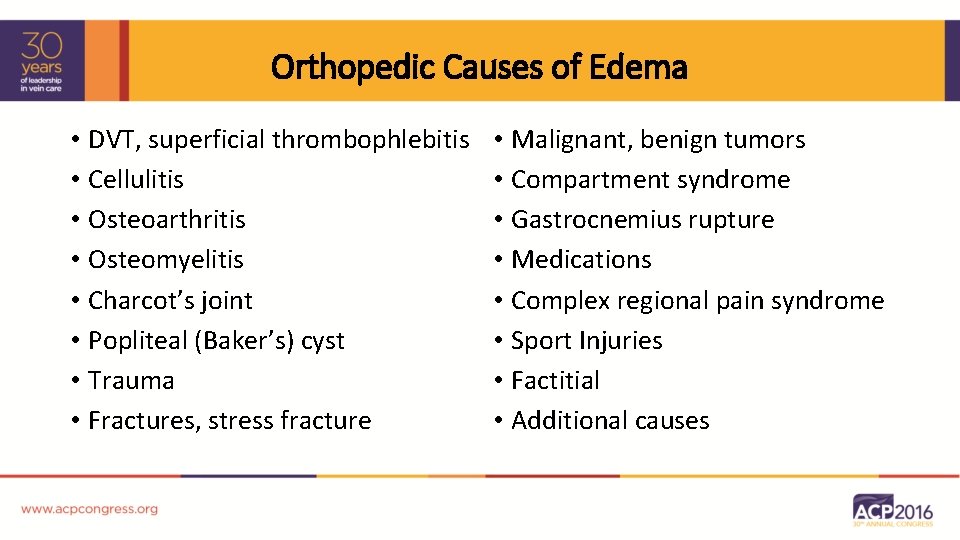
Orthopedic Causes of Edema • DVT, superficial thrombophlebitis • Cellulitis • Osteoarthritis • Osteomyelitis • Charcot’s joint • Popliteal (Baker’s) cyst • Trauma • Fractures, stress fracture • Malignant, benign tumors • Compartment syndrome • Gastrocnemius rupture • Medications • Complex regional pain syndrome • Sport Injuries • Factitial • Additional causes
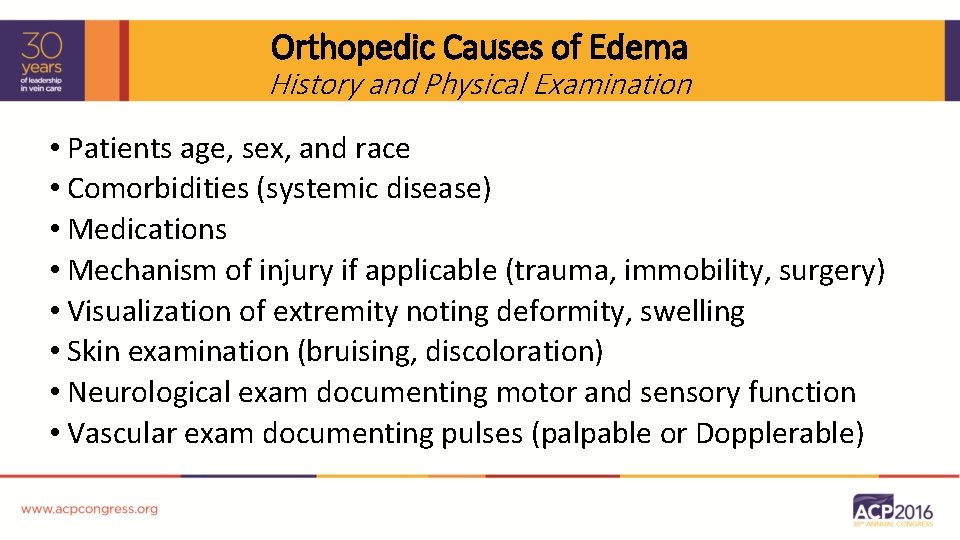
Orthopedic Causes of Edema History and Physical Examination • Patients age, sex, and race • Comorbidities (systemic disease) • Medications • Mechanism of injury if applicable (trauma, immobility, surgery) • Visualization of extremity noting deformity, swelling • Skin examination (bruising, discoloration) • Neurological exam documenting motor and sensory function • Vascular exam documenting pulses (palpable or Dopplerable)
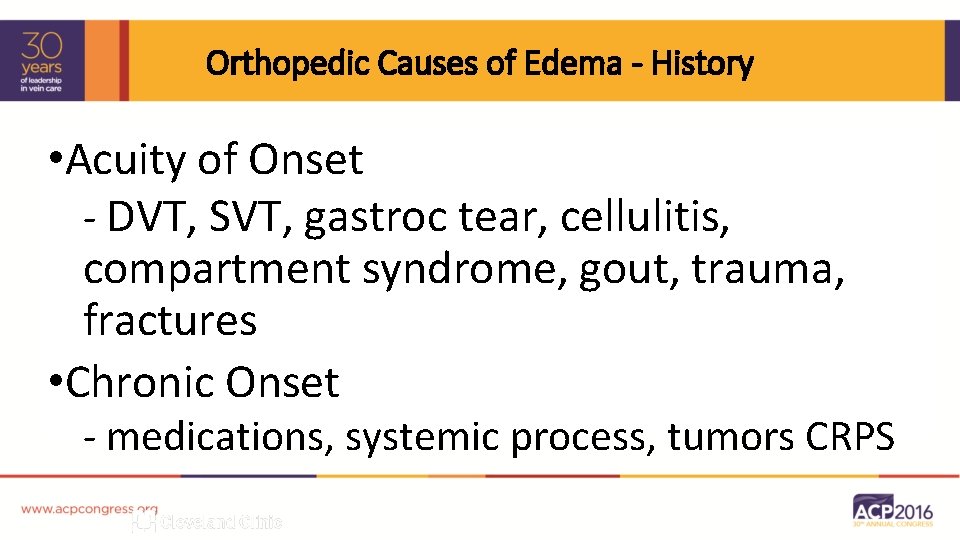
Orthopedic Causes of Edema - History • Acuity of Onset - DVT, SVT, gastroc tear, cellulitis, compartment syndrome, gout, trauma, fractures • Chronic Onset - medications, systemic process, tumors CRPS
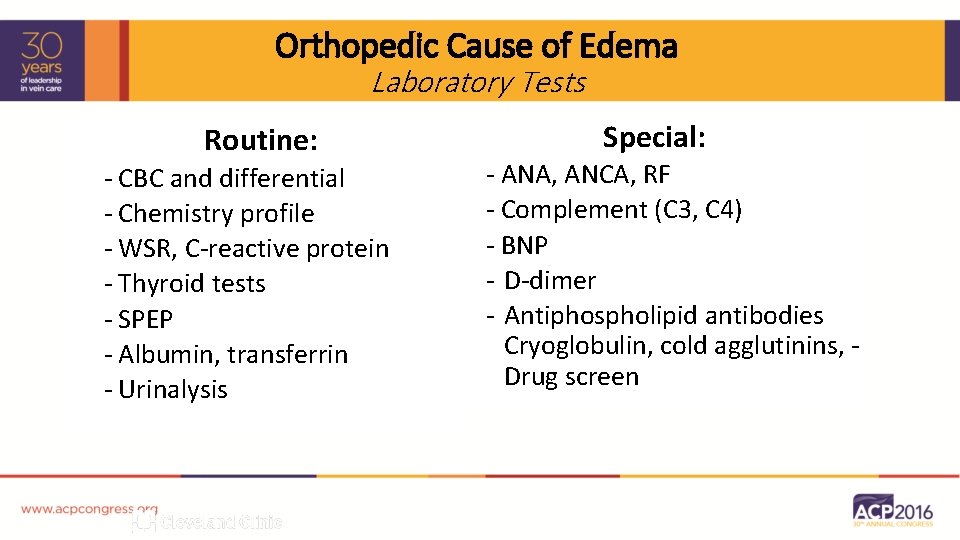
Orthopedic Cause of Edema Laboratory Tests Routine: - CBC and differential - Chemistry profile - WSR, C-reactive protein - Thyroid tests - SPEP - Albumin, transferrin - Urinalysis Special: - ANA, ANCA, RF - Complement (C 3, C 4) - BNP - D-dimer - Antiphospholipid antibodies Cryoglobulin, cold agglutinins, Drug screen
Orthopedic Causes of Edema Imaging and Vascular Laboratory • X-ray • Echocardiogram • Arterial - ABI, Doppler ultrasound - MR angiogram - CT angiogram - Angiography • Venous: - Duplex - Venous incompetency - Contrast venography - IVUS • CT and MR imaging • Lymphatic - Lymphoscintigraphy - Abd/pelvic CT or MRI
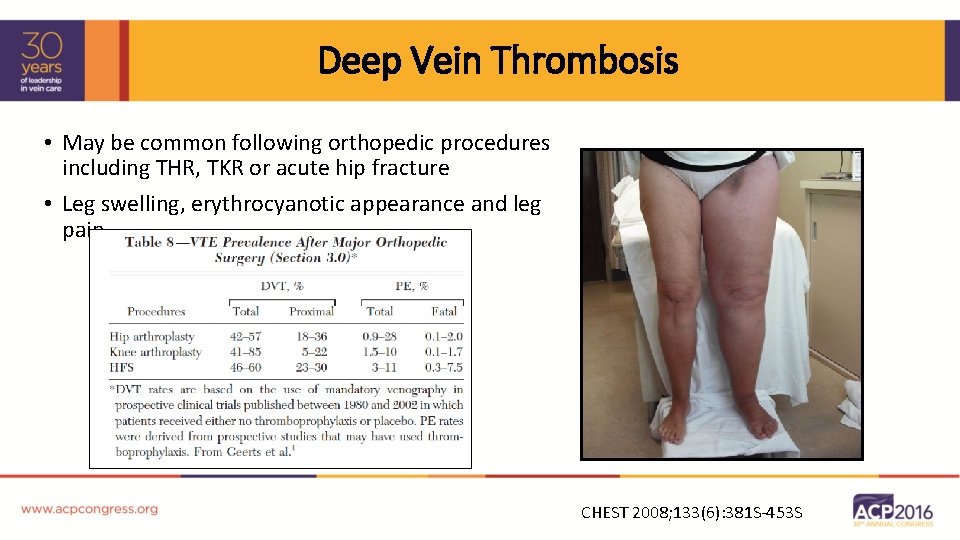
Deep Vein Thrombosis • May be common following orthopedic procedures including THR, TKR or acute hip fracture • Leg swelling, erythrocyanotic appearance and leg pain CHEST 2008; 133(6): 381 S-453 S
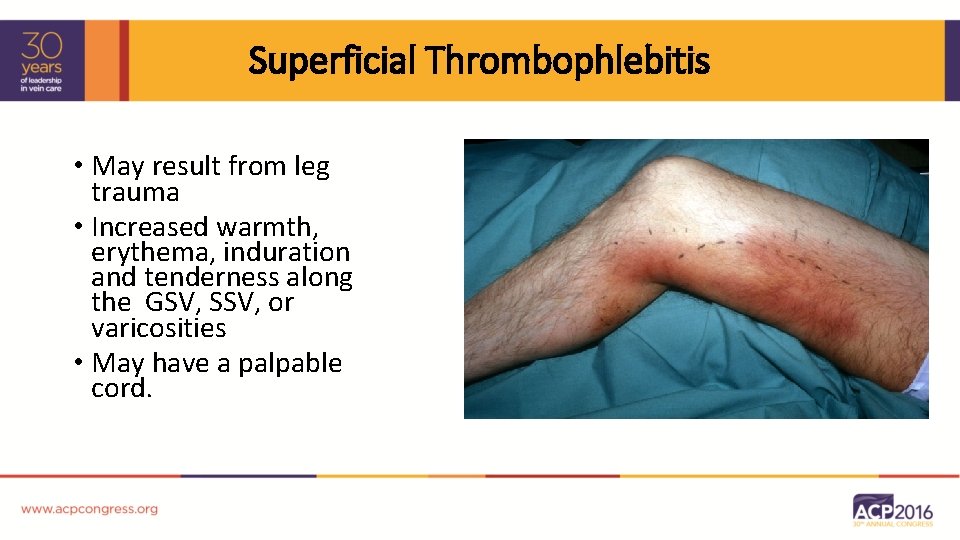
Superficial Thrombophlebitis • May result from leg trauma • Increased warmth, erythema, induration and tenderness along the GSV, SSV, or varicosities • May have a palpable cord.
Cellulitis • Most common infectious cause of limb swelling (strep and staph most usual) • Look for portal of entry (skin cracks, fissures, tinea pedis) allowing bacteria to enter/release toxins in the SC tissues
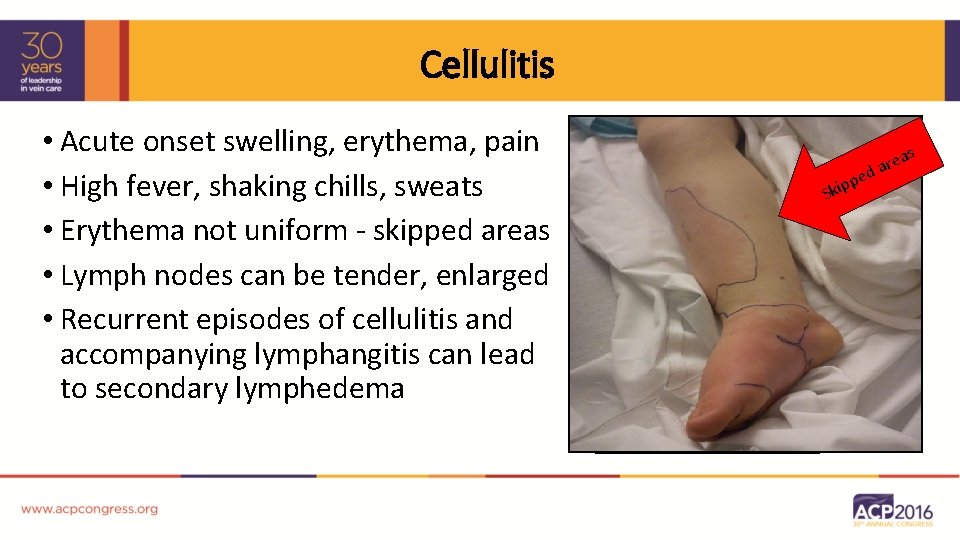
Cellulitis • Acute onset swelling, erythema, pain • High fever, shaking chills, sweats • Erythema not uniform - skipped areas • Lymph nodes can be tender, enlarged • Recurrent episodes of cellulitis and accompanying lymphangitis can lead to secondary lymphedema s p p i k S e rea a d
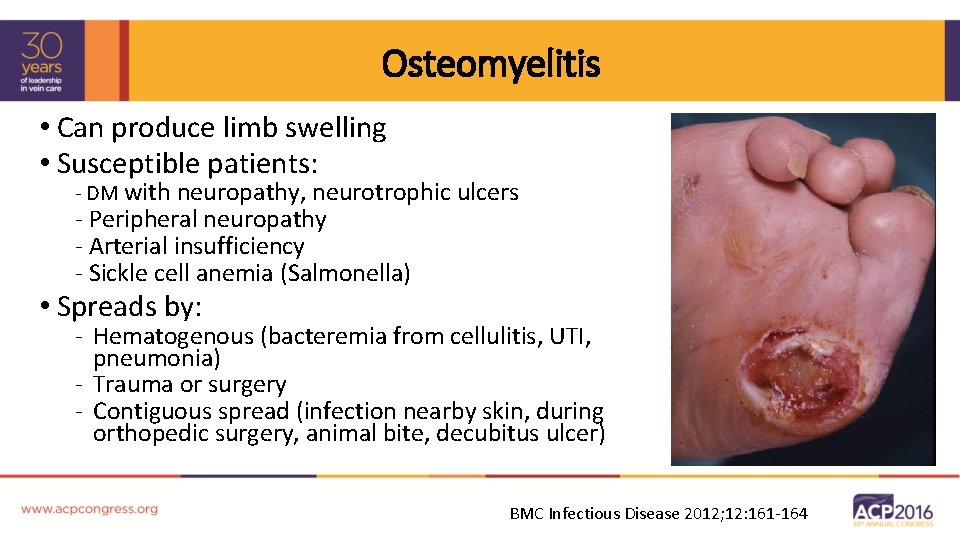
Osteomyelitis • Can produce limb swelling • Susceptible patients: - DM with neuropathy, neurotrophic ulcers - Peripheral neuropathy - Arterial insufficiency - Sickle cell anemia (Salmonella) • Spreads by: - Hematogenous (bacteremia from cellulitis, UTI, pneumonia) - Trauma or surgery - Contiguous spread (infection nearby skin, during orthopedic surgery, animal bite, decubitus ulcer) BMC Infectious Disease 2012; 12: 161 -164
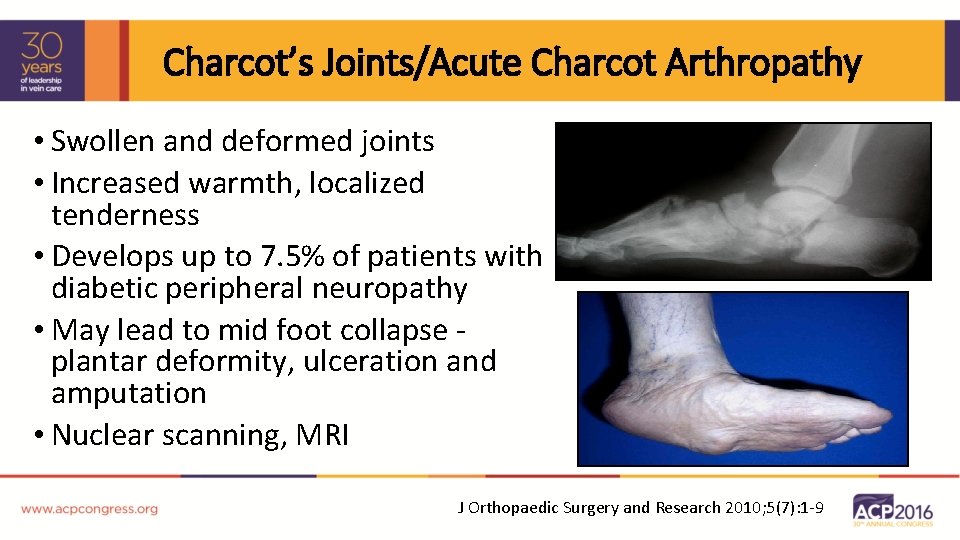
Charcot’s Joints/Acute Charcot Arthropathy • Swollen and deformed joints • Increased warmth, localized tenderness • Develops up to 7. 5% of patients with diabetic peripheral neuropathy • May lead to mid foot collapse plantar deformity, ulceration and amputation • Nuclear scanning, MRI J Orthopaedic Surgery and Research 2010; 5(7): 1 -9
Popliteal Cysts (Baker’s Cyst) • Produces swelling behind the knee or distally • May mimic DVT - if compression of the popliteal vein - If ruptures • Physical examination should suggest popliteal cyst in patients with RA or degenerative joint disease • Ultrasound examination confirms unless ruptured
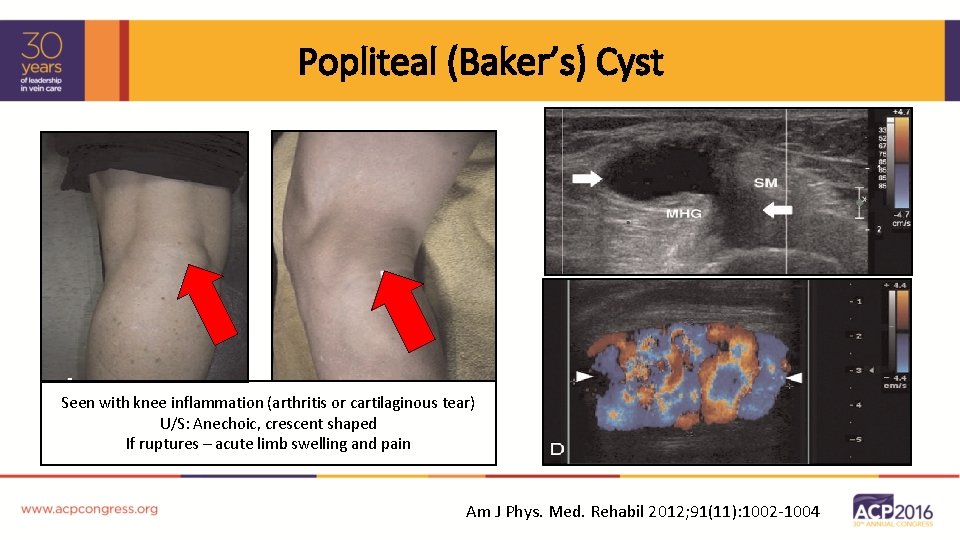
Popliteal (Baker’s) Cyst Seen with knee inflammation (arthritis or cartilaginous tear) U/S: Anechoic, crescent shaped If ruptures – acute limb swelling and pain Am J Phys. Med. Rehabil 2012; 91(11): 1002 -1004
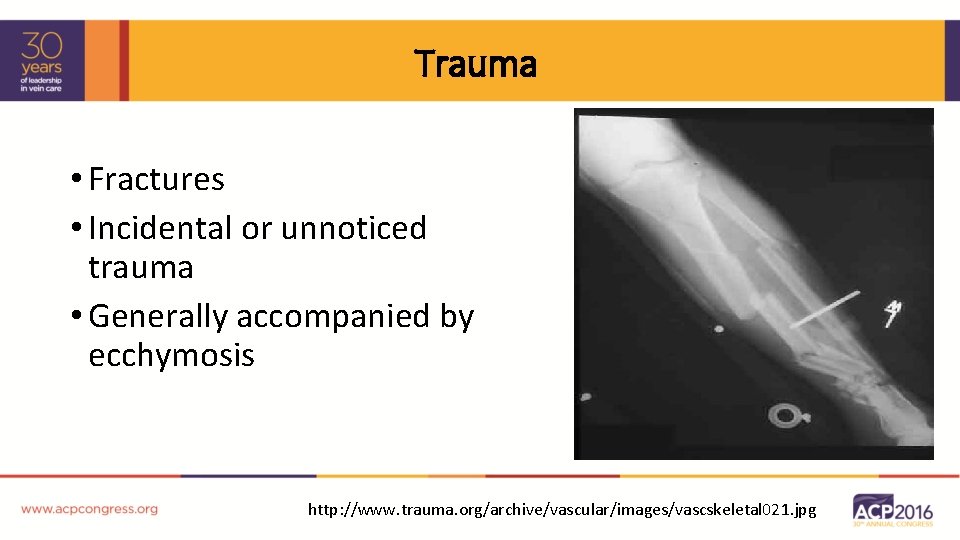
Trauma • Fractures • Incidental or unnoticed trauma • Generally accompanied by ecchymosis http: //www. trauma. org/archive/vascular/images/vascskeletal 021. jpg
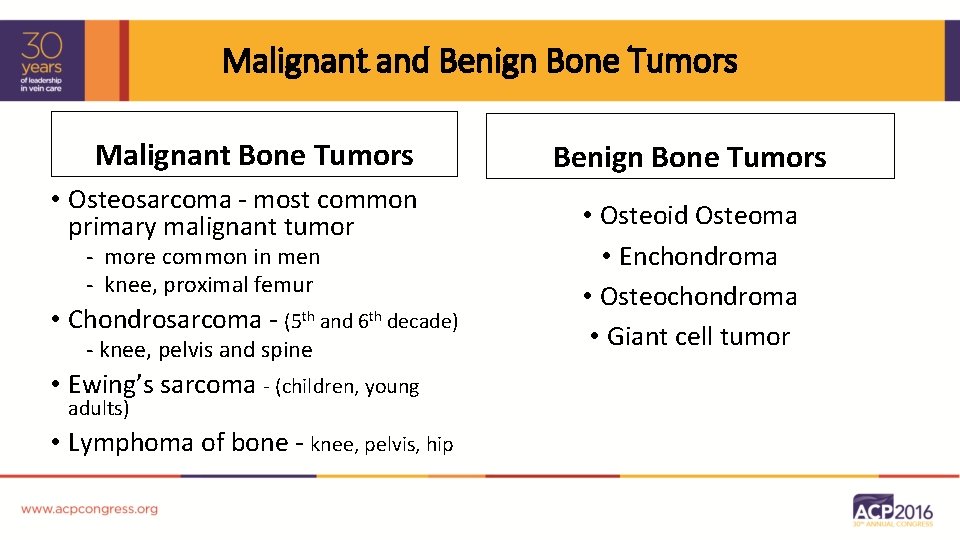
Malignant and Benign Bone Tumors Malignant Bone Tumors • Osteosarcoma - most common primary malignant tumor - more common in men - knee, proximal femur • Chondrosarcoma - (5 th and 6 th decade) - knee, pelvis and spine • Ewing’s sarcoma - (children, young adults) • Lymphoma of bone - knee, pelvis, hip Benign Bone Tumors • Osteoid Osteoma • Enchondroma • Osteochondroma • Giant cell tumor
Compartment Syndrome • Increased pressure in a closed fascial space leading to compromised perfusion and severe tissue damage • Severe pain, induration and edema • Results from local tissue response to severe hypoxemia and/or to restoration of blood flow to an ischemic extremity • The compartments ability to accommodate a sudden increase in volume is limited (in a fixed, enclosed area) especially if other mechanical factors (trauma or encasement bandages or dressings) are present

Compartment Syndrome Fasciotomy (prophylactic or therapeutic) may be necessary Surg Clin N Am 2013; 93: 789 -812 Surg Clin N Am 2012; 92(4): 987 -1007
Drug-Induced • Bilateral, soft, pitting edema • Generally resolves once drug withdrawn • Corticosteroids, nonsteroidal anti -inflammatory drugs (NSAIDs) • Hormones (estrogens, testosterone, androgen)
Sports/Runner Injuries • 10% to 20% of Americans run regularly • 19% to 79% of runners are injured • Most running-related injuries related to overuse • Risks for running-related injuries include: • • Systemic (gender, weight, knee alignment, flexibility Running/training related (frequency, terrain, distance) Health (previous injuries/medical problems) Lifestyle (sedentary, work, tobacco, cross training Med Clin N Am 2014; 851 -868
Sports/Runner Injuries - Other Causes of Edema Orthopedic Conditions Encountered in Runners • Stress fractures • Gastrocnemius/Soleus Strain/Rupture • Iliotibial Band Syndrome (ITBS) • Patellofemoral Pain Syndrome (PFPS) • Meniscal injuries • MTSS • Achilles tendinopathy Med Clin N Am 2014; 851 -868
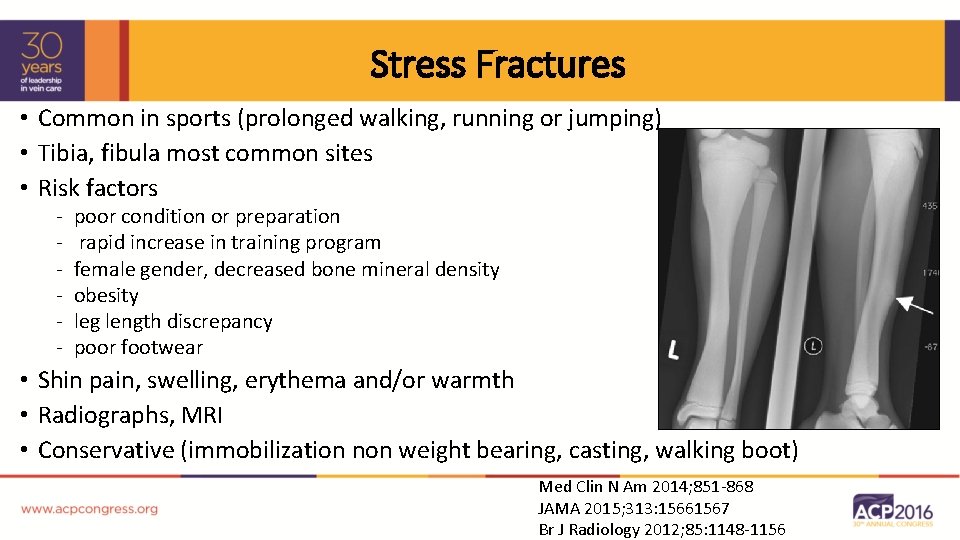
Stress Fractures • Common in sports (prolonged walking, running or jumping) • Tibia, fibula most common sites • Risk factors - poor condition or preparation rapid increase in training program female gender, decreased bone mineral density obesity leg length discrepancy poor footwear • Shin pain, swelling, erythema and/or warmth • Radiographs, MRI • Conservative (immobilization non weight bearing, casting, walking boot) Med Clin N Am 2014; 851 -868 JAMA 2015; 313: 15661567 Br J Radiology 2012; 85: 1148 -1156
Gastrocnemius Rupture • Weekend athlete, steps off curb (4 th-5 th decade) • Sudden onset of sharp pain in calf, leg swelling • Ecchymosis (gravitational dissection of blood from the torn muscle through muscle tissue plains) • Crescent shape (Scimitar Sign) beneath the malleoli • Rupture medial head of gastrocnemius muscle • Patients may describe a snap or pop “Tennis Leg”
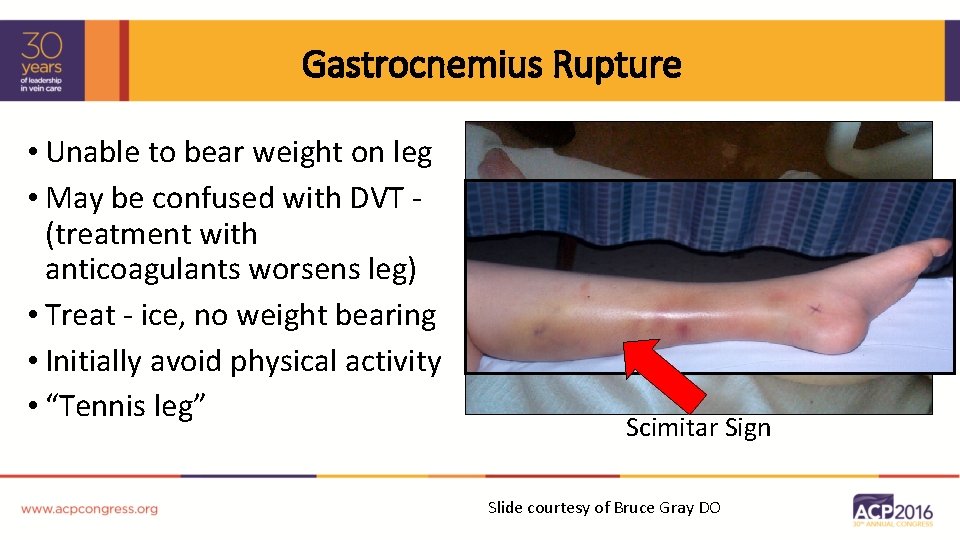
Gastrocnemius Rupture • Unable to bear weight on leg • May be confused with DVT (treatment with anticoagulants worsens leg) • Treat - ice, no weight bearing • Initially avoid physical activity • “Tennis leg” Scimitar Sign Slide courtesy of Bruce Gray DO
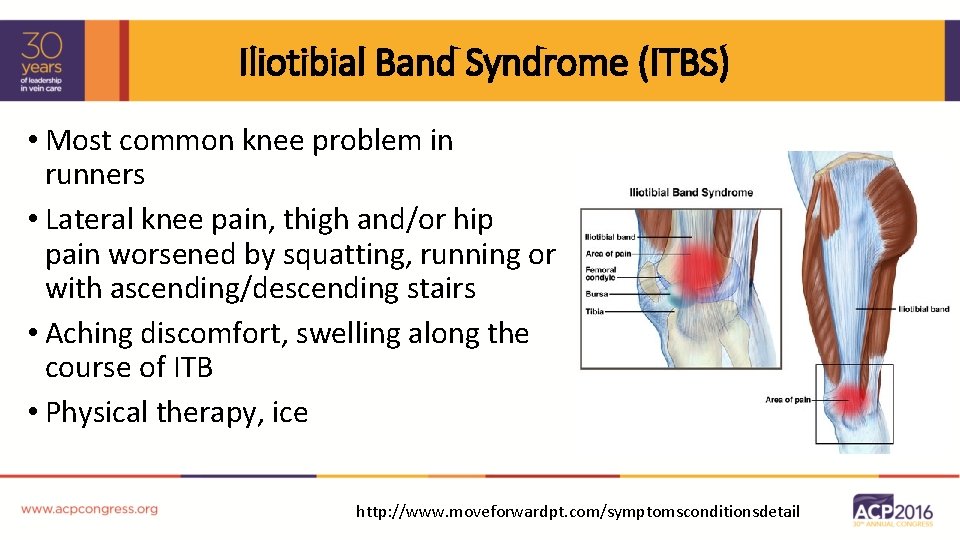
Iliotibial Band Syndrome (ITBS) • Most common knee problem in runners • Lateral knee pain, thigh and/or hip pain worsened by squatting, running or with ascending/descending stairs • Aching discomfort, swelling along the course of ITB • Physical therapy, ice http: //www. moveforwardpt. com/symptomsconditionsdetail
Patellofemoral Pain Syndrome (PFPS) • Found commonly in young runners • Pain around kneecap • Sitting with knee flexed for a long period of time (theater sign), climbing stairs and/or running exacerbate the pain • Physical exam - popping, snapping or grinding under the kneecap - mild swelling and small effusion • Treatment – physical therapy, heat-molded orthotics http: //www. sportalignment. com/img/pfs_top. jpg
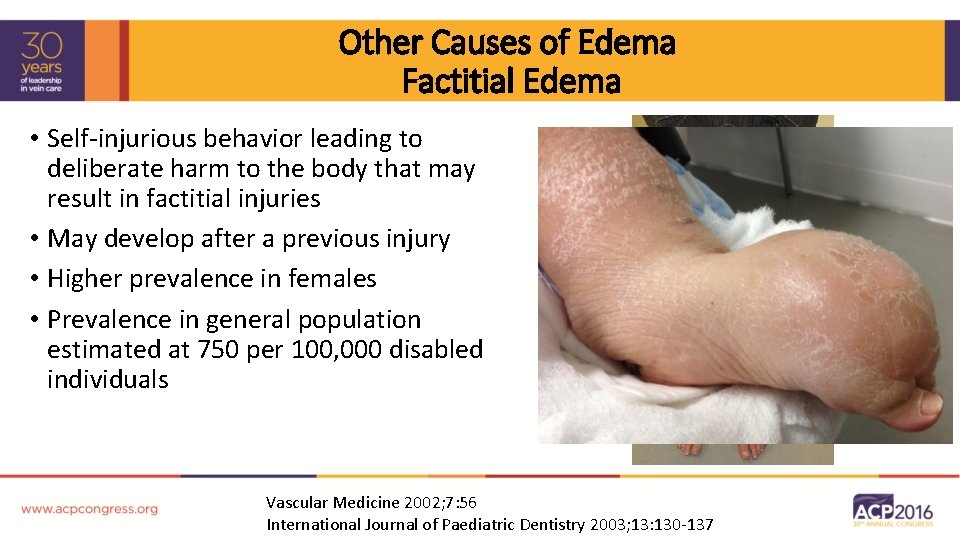
Other Causes of Edema Factitial Edema • Self-injurious behavior leading to deliberate harm to the body that may result in factitial injuries • May develop after a previous injury • Higher prevalence in females • Prevalence in general population estimated at 750 per 100, 000 disabled individuals Vascular Medicine 2002; 7: 56 International Journal of Paediatric Dentistry 2003; 13: 130 -137
Other Causes of Edema Cystic Adventitial Disease • Rare condition - mucinous cysts form within the adventitia of arteries and veins • Can lead to lumen occlusion • Young to middle-aged men • Popliteal artery most involved site • Painless swelling if popliteal venous cyst J Vasc Surg 2014; 60: 235 -245 J Vasc Interv Radiol 1996; 7: 583 -586
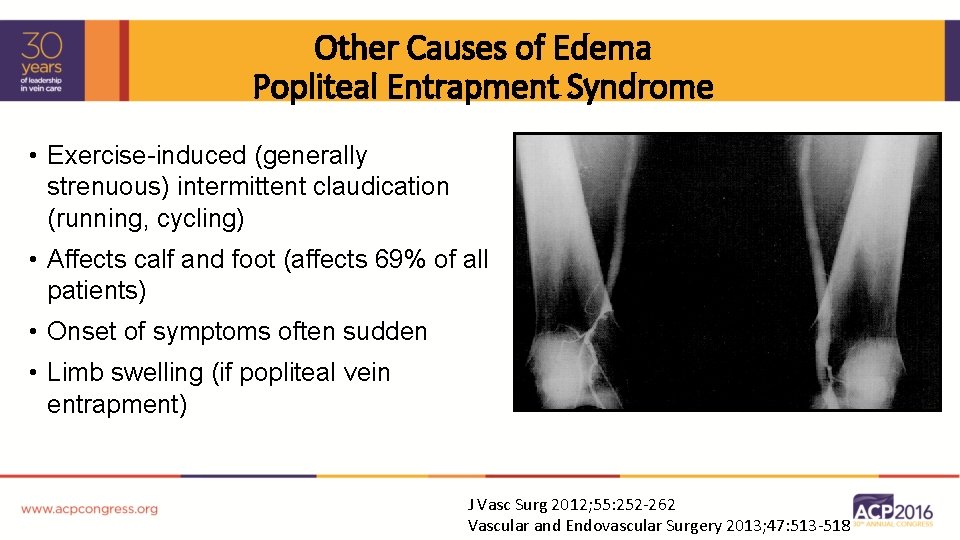
Other Causes of Edema Popliteal Entrapment Syndrome • Exercise-induced (generally strenuous) intermittent claudication (running, cycling) • Affects calf and foot (affects 69% of all patients) • Onset of symptoms often sudden • Limb swelling (if popliteal vein entrapment) J Vasc Surg 2012; 55: 252 -262 Vascular and Endovascular Surgery 2013; 47: 513 -518
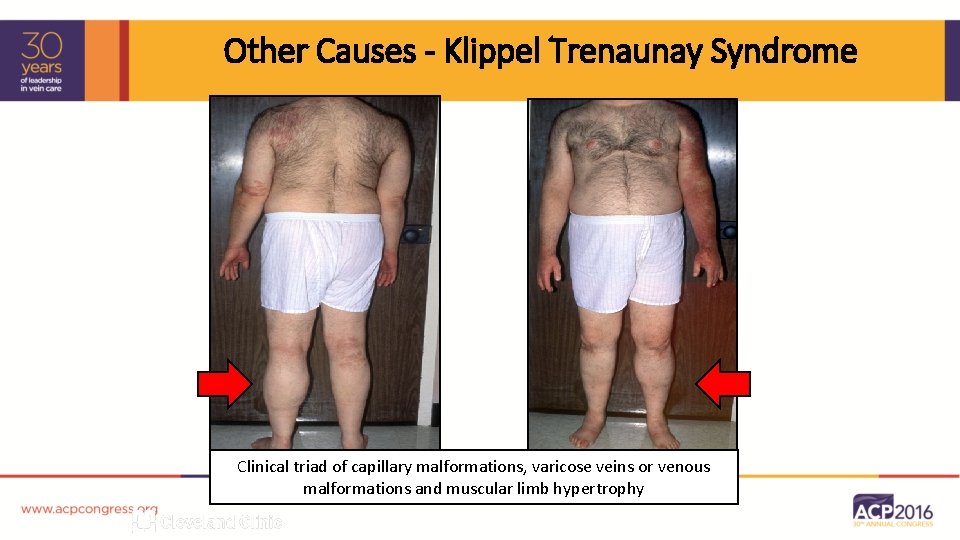
Other Causes - Klippel Trenaunay Syndrome Clinical triad of capillary malformations, varicose veins or venous malformations and muscular limb hypertrophy
- Slides: 33