Organs of respiratory system Nose initial receiving station
- Slides: 29
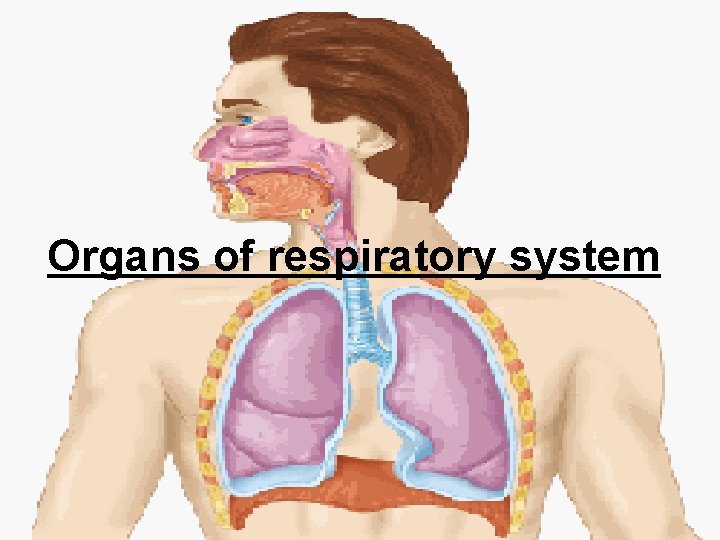
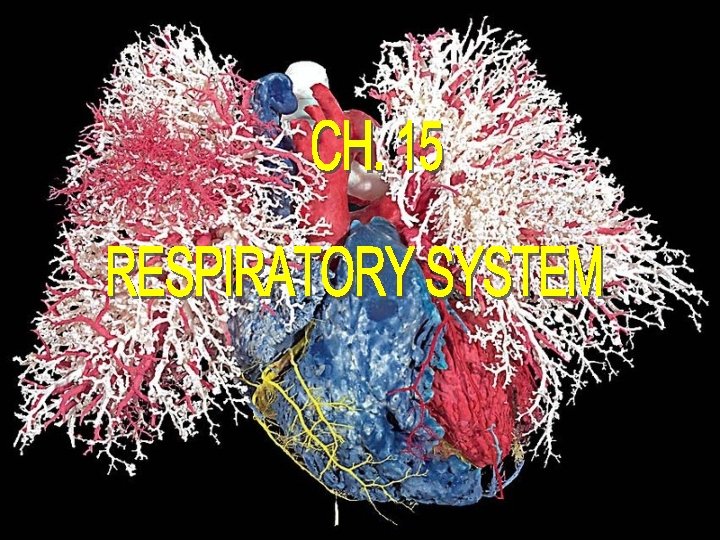
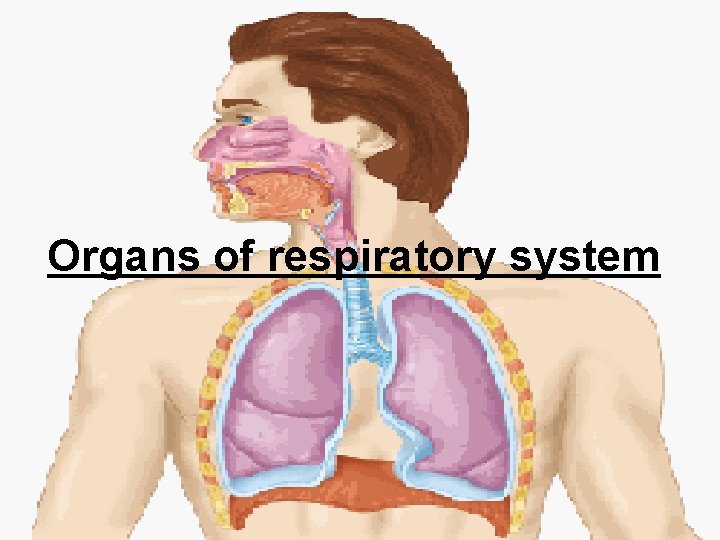
Organs of respiratory system
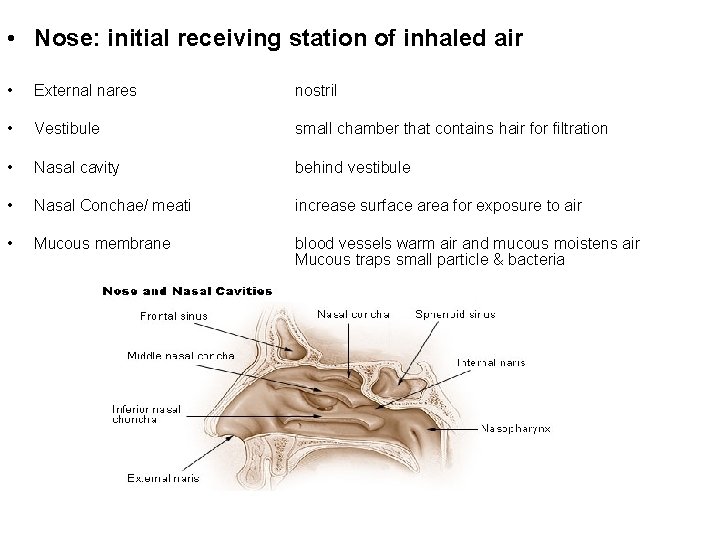
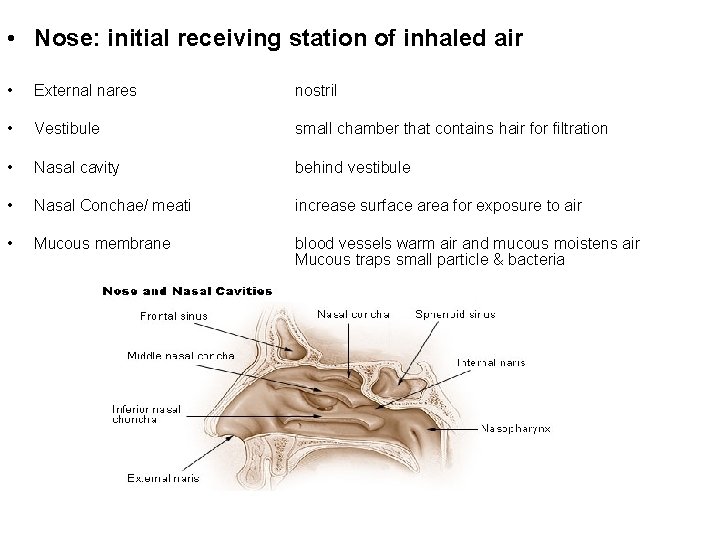
• Nose: initial receiving station of inhaled air • External nares nostril • Vestibule small chamber that contains hair for filtration • Nasal cavity behind vestibule • Nasal Conchae/ meati increase surface area for exposure to air • Mucous membrane blood vessels warm air and mucous moistens air Mucous traps small particle & bacteria
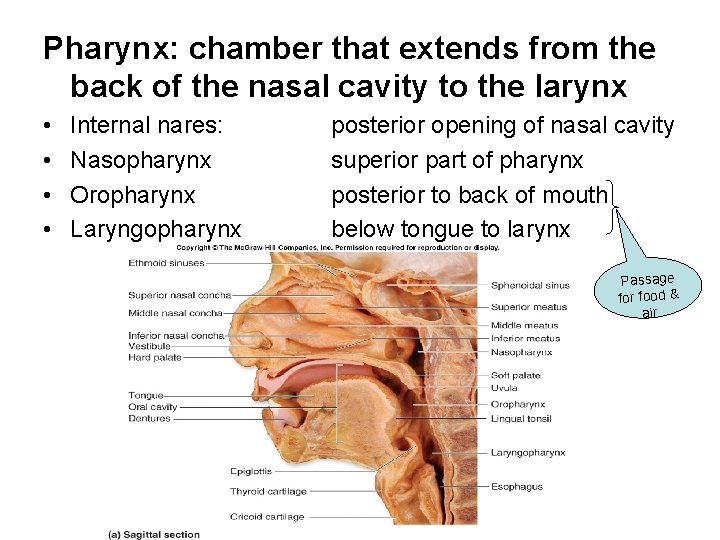
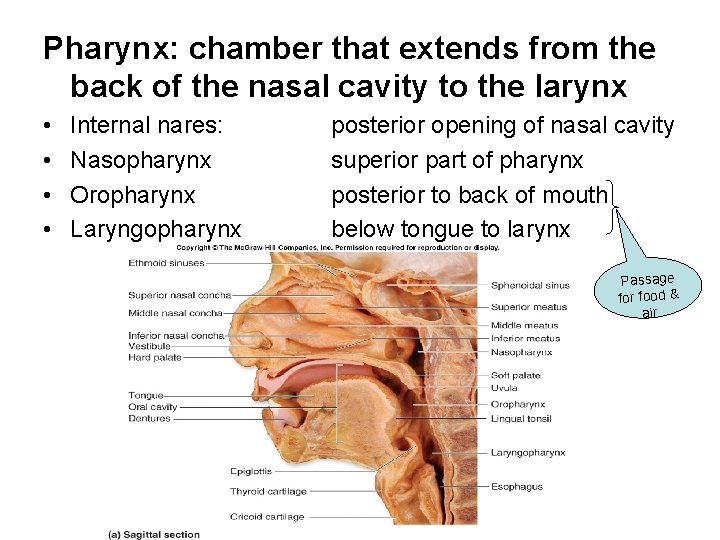
Pharynx: chamber that extends from the back of the nasal cavity to the larynx • • Internal nares: Nasopharynx Oropharynx Laryngopharynx posterior opening of nasal cavity superior part of pharynx posterior to back of mouth below tongue to larynx Passage for food & air
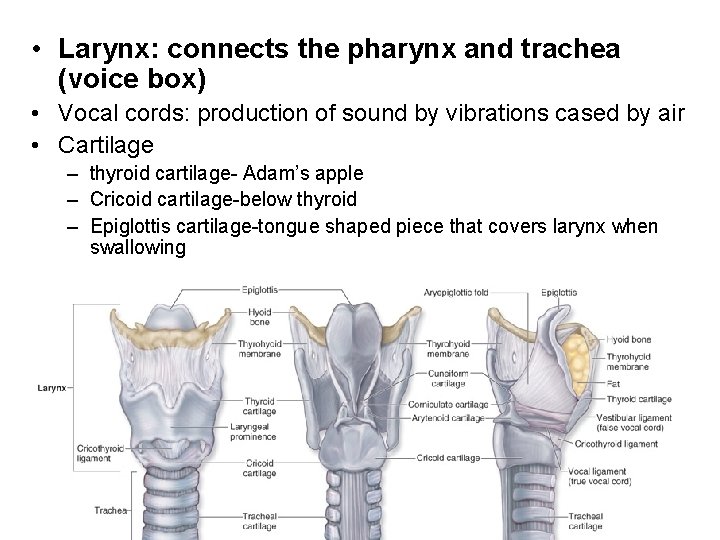
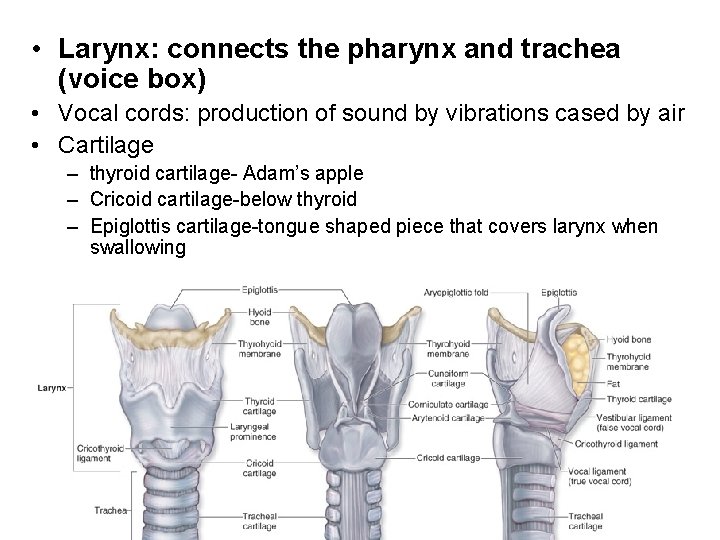
• Larynx: connects the pharynx and trachea (voice box) • Vocal cords: production of sound by vibrations cased by air • Cartilage – thyroid cartilage- Adam’s apple – Cricoid cartilage-below thyroid – Epiglottis cartilage-tongue shaped piece that covers larynx when swallowing
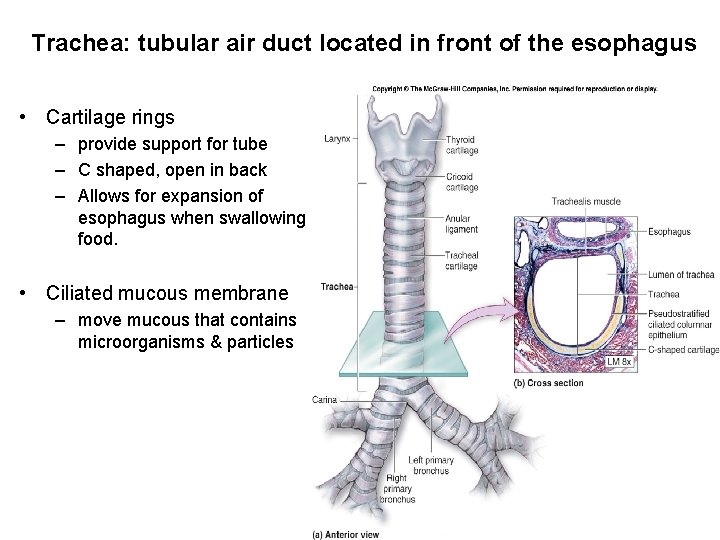
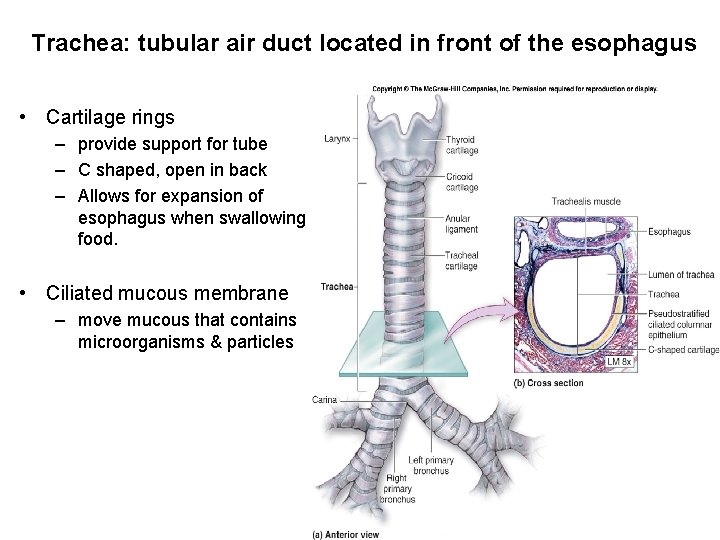
Trachea: tubular air duct located in front of the esophagus • Cartilage rings – provide support for tube – C shaped, open in back – Allows for expansion of esophagus when swallowing food. • Ciliated mucous membrane – move mucous that contains microorganisms & particles
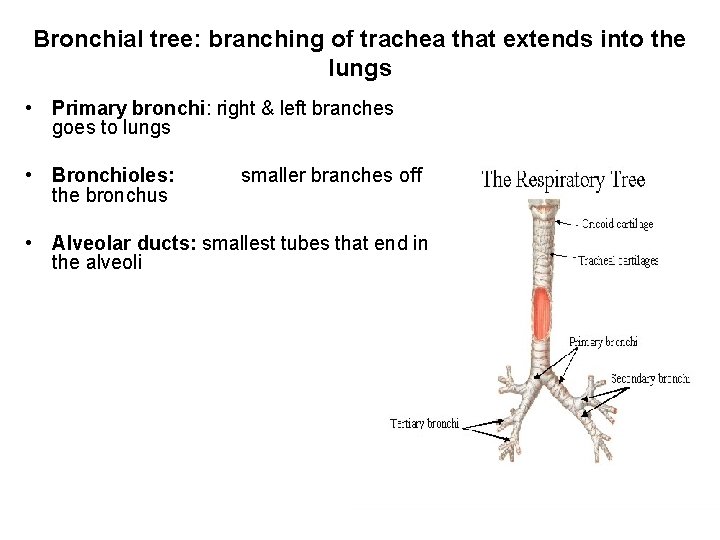
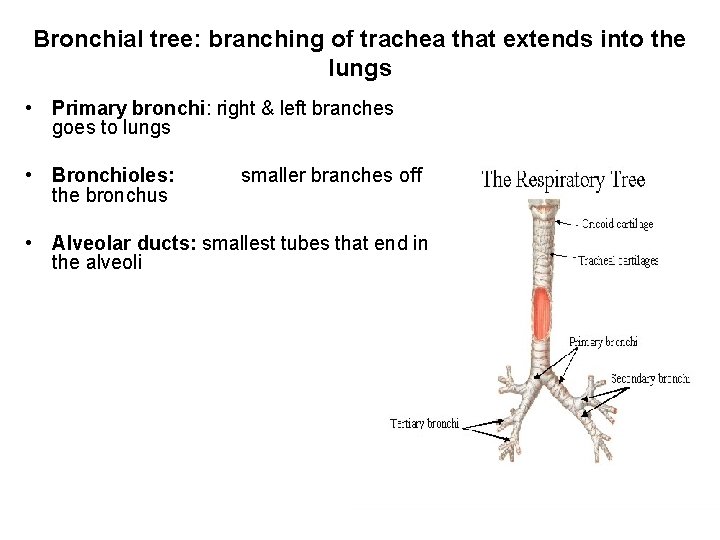
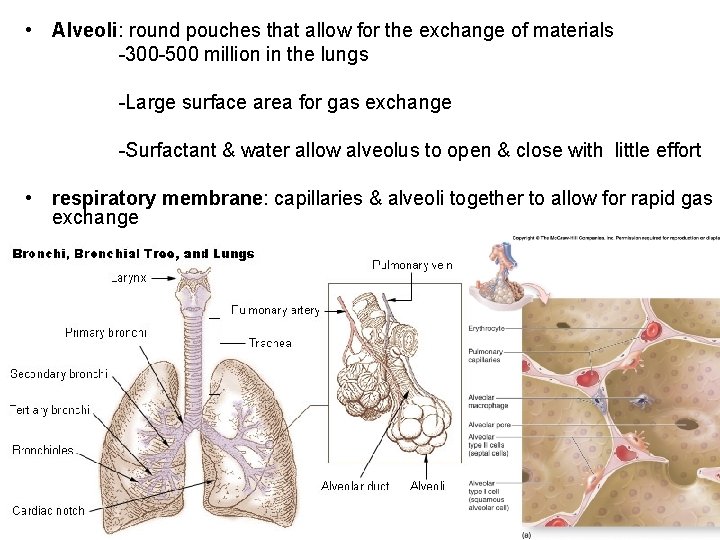
Bronchial tree: branching of trachea that extends into the lungs • Primary bronchi: right & left branches goes to lungs • Bronchioles: the bronchus smaller branches off • Alveolar ducts: smallest tubes that end in the alveoli
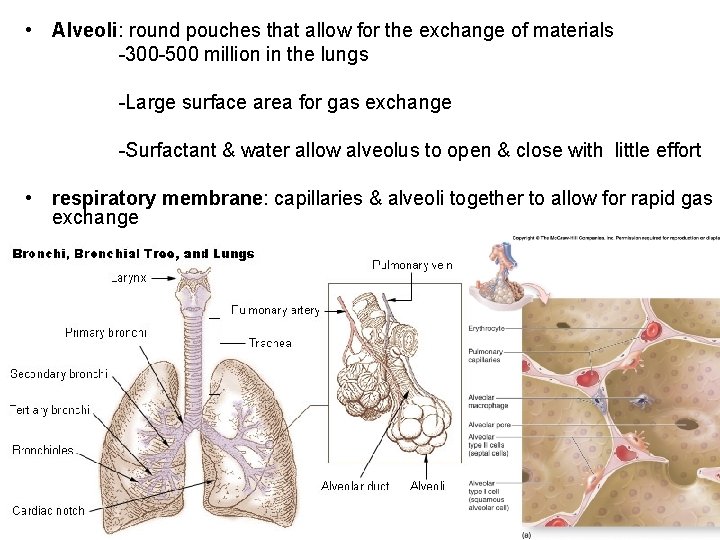
• Alveoli: round pouches that allow for the exchange of materials -300 -500 million in the lungs -Large surface area for gas exchange -Surfactant & water allow alveolus to open & close with little effort • respiratory membrane: capillaries & alveoli together to allow for rapid gas exchange
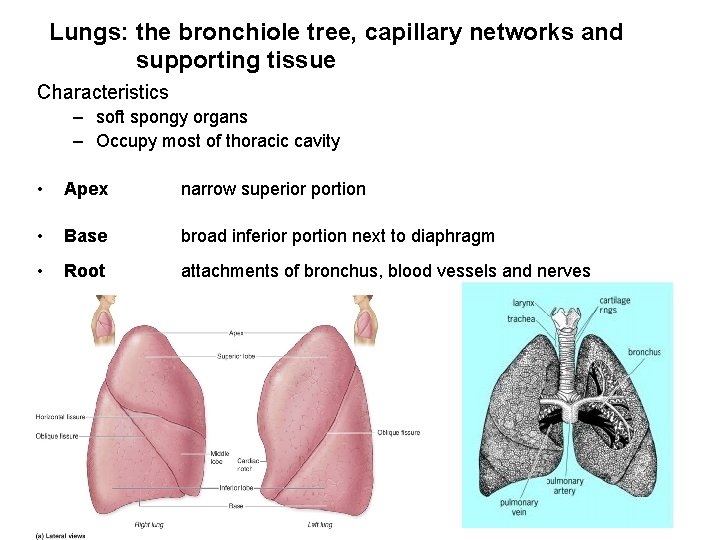
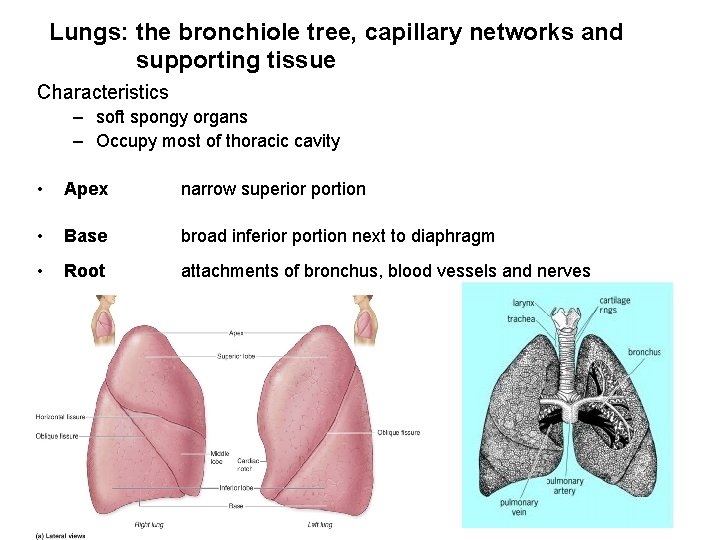
Lungs: the bronchiole tree, capillary networks and supporting tissue Characteristics – soft spongy organs – Occupy most of thoracic cavity • Apex narrow superior portion • Base broad inferior portion next to diaphragm • Root attachments of bronchus, blood vessels and nerves
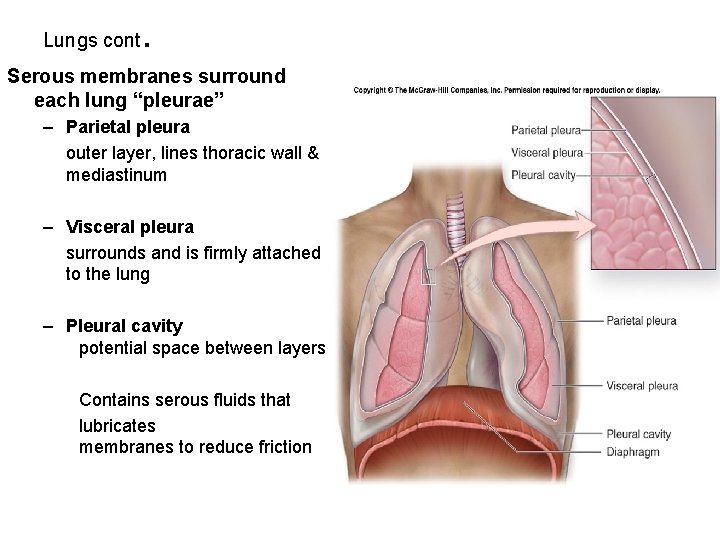
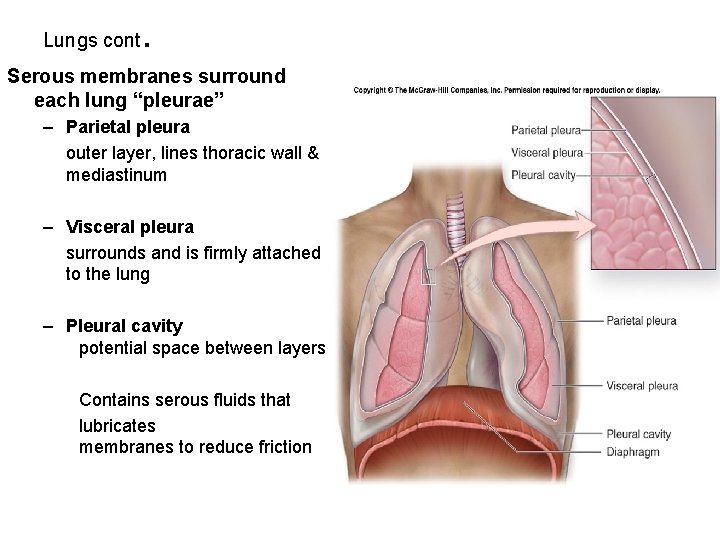
Lungs cont . Serous membranes surround each lung “pleurae” – Parietal pleura outer layer, lines thoracic wall & mediastinum – Visceral pleura surrounds and is firmly attached to the lung – Pleural cavity potential space between layers Contains serous fluids that lubricates membranes to reduce friction
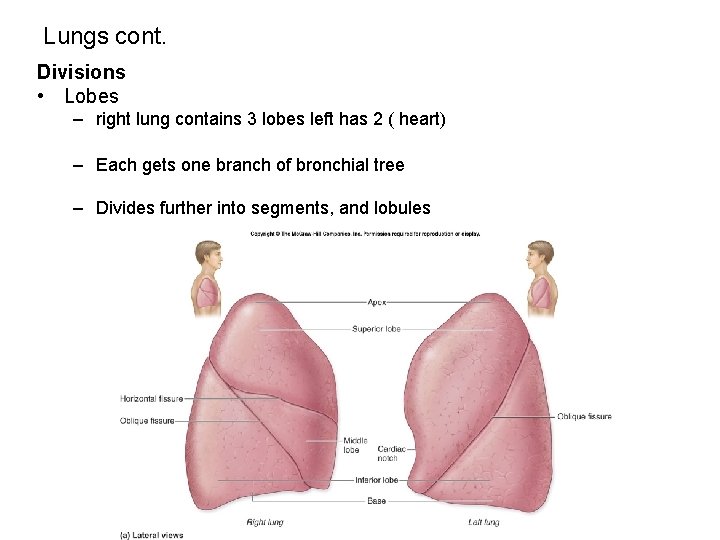
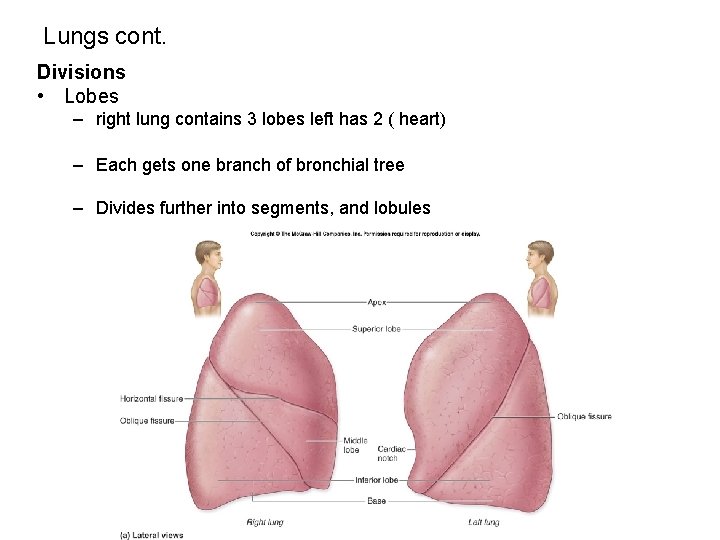
Lungs cont. Divisions • Lobes – right lung contains 3 lobes left has 2 ( heart) – Each gets one branch of bronchial tree – Divides further into segments, and lobules
Mechanisms of breathing
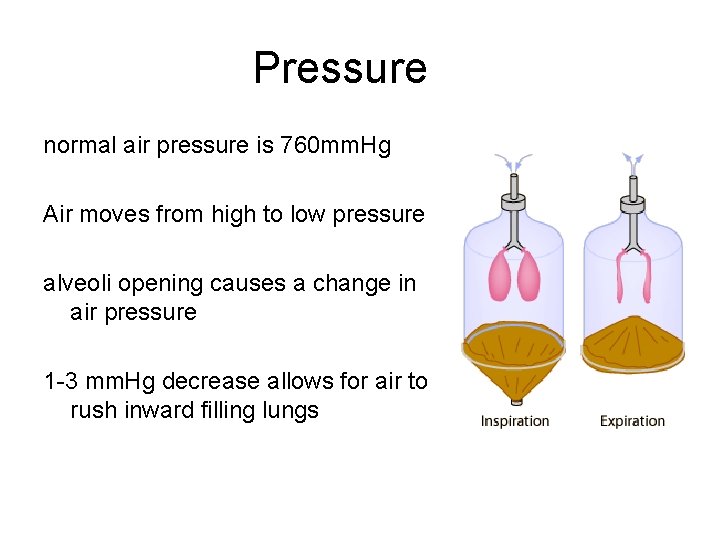
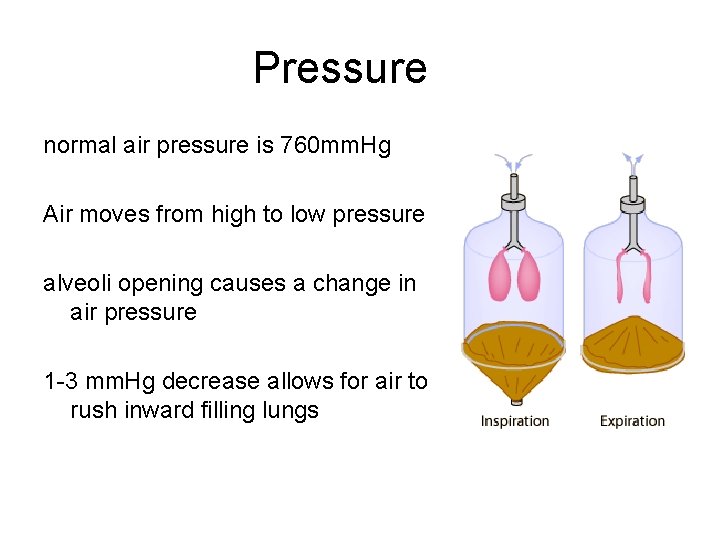
Pressure normal air pressure is 760 mm. Hg Air moves from high to low pressure alveoli opening causes a change in air pressure 1 -3 mm. Hg decrease allows for air to rush inward filling lungs
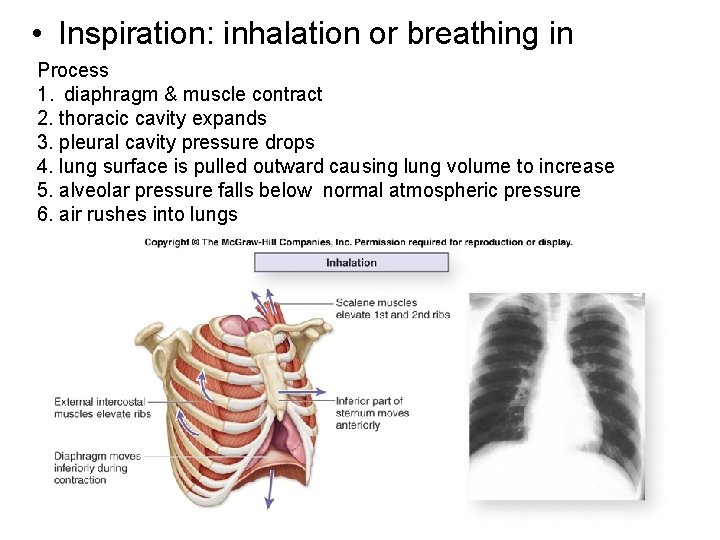
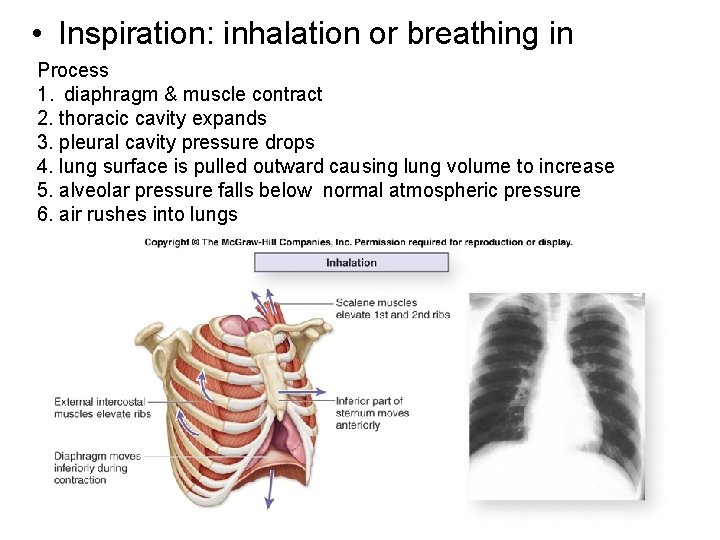
• Inspiration: inhalation or breathing in Process 1. diaphragm & muscle contract 2. thoracic cavity expands 3. pleural cavity pressure drops 4. lung surface is pulled outward causing lung volume to increase 5. alveolar pressure falls below normal atmospheric pressure 6. air rushes into lungs
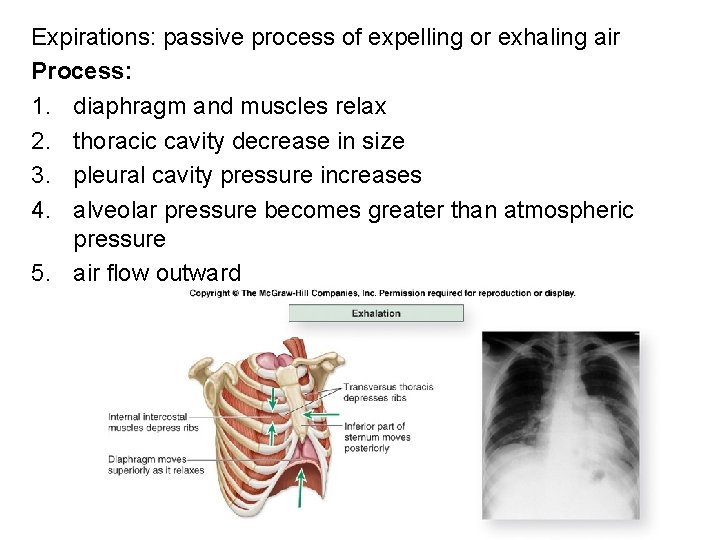
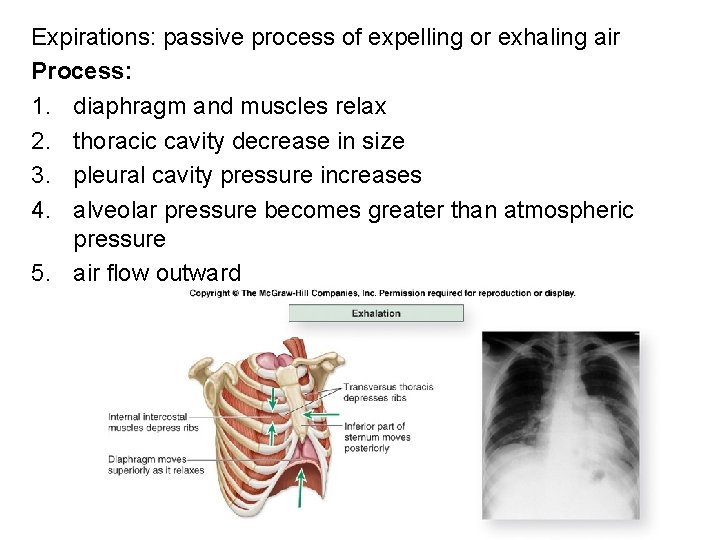
Expirations: passive process of expelling or exhaling air Process: 1. diaphragm and muscles relax 2. thoracic cavity decrease in size 3. pleural cavity pressure increases 4. alveolar pressure becomes greater than atmospheric pressure 5. air flow outward
Respiratory Volumes
Lung volumes • Factor influencing – activities – Physical differences between individuals – Health • Measurement – Spirometer • Dry vs. wet
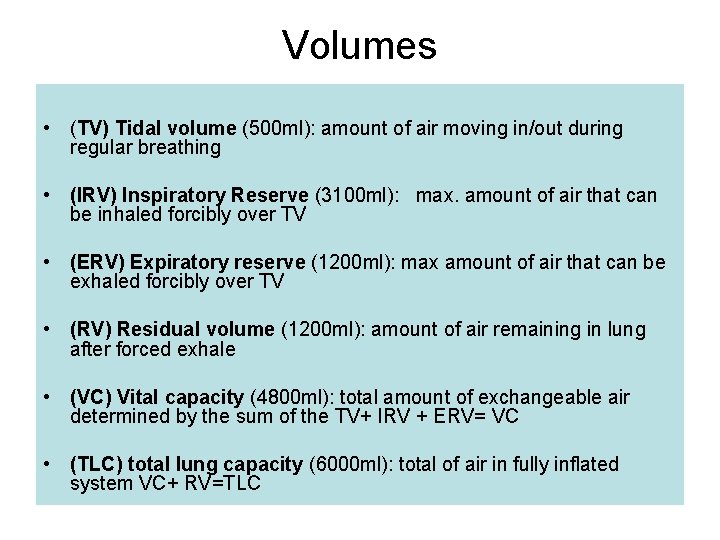
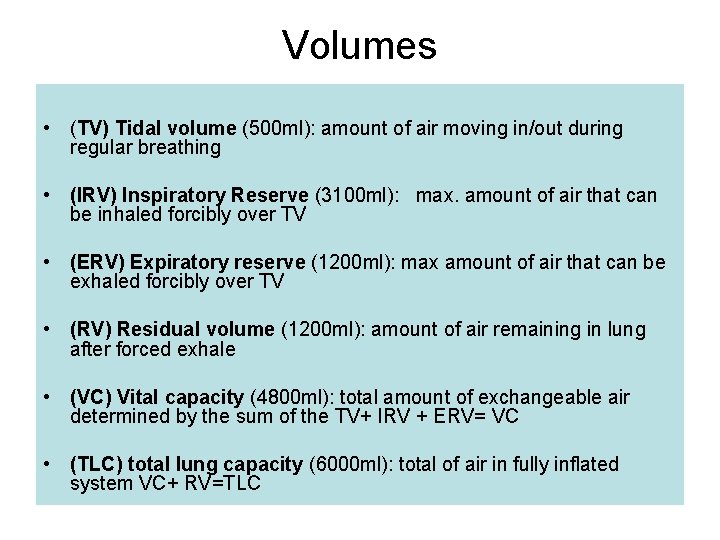
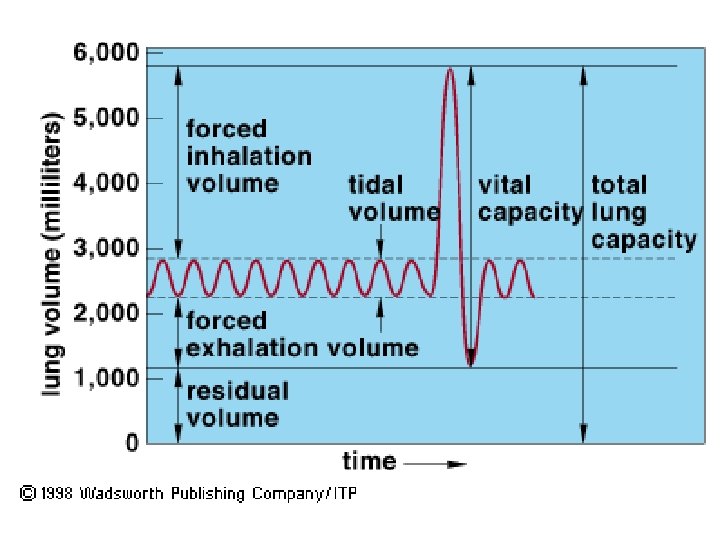
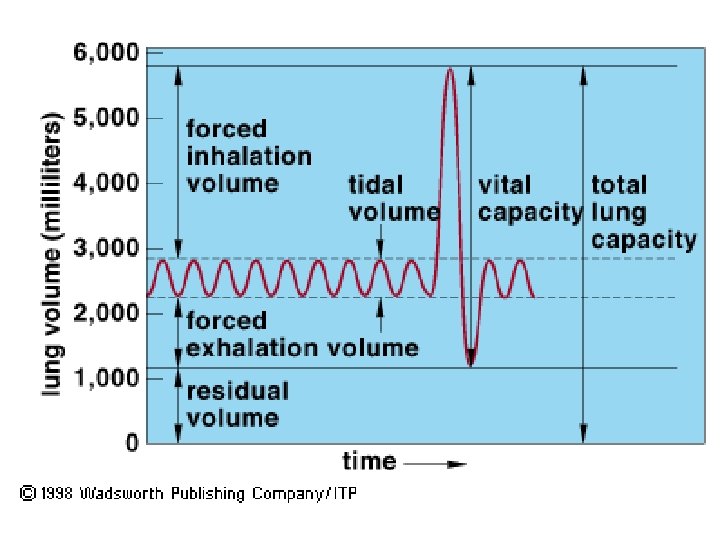
Volumes • (TV) Tidal volume (500 ml): amount of air moving in/out during regular breathing • (IRV) Inspiratory Reserve (3100 ml): max. amount of air that can be inhaled forcibly over TV • (ERV) Expiratory reserve (1200 ml): max amount of air that can be exhaled forcibly over TV • (RV) Residual volume (1200 ml): amount of air remaining in lung after forced exhale • (VC) Vital capacity (4800 ml): total amount of exchangeable air determined by the sum of the TV+ IRV + ERV= VC • (TLC) total lung capacity (6000 ml): total of air in fully inflated system VC+ RV=TLC
Exchange of gases
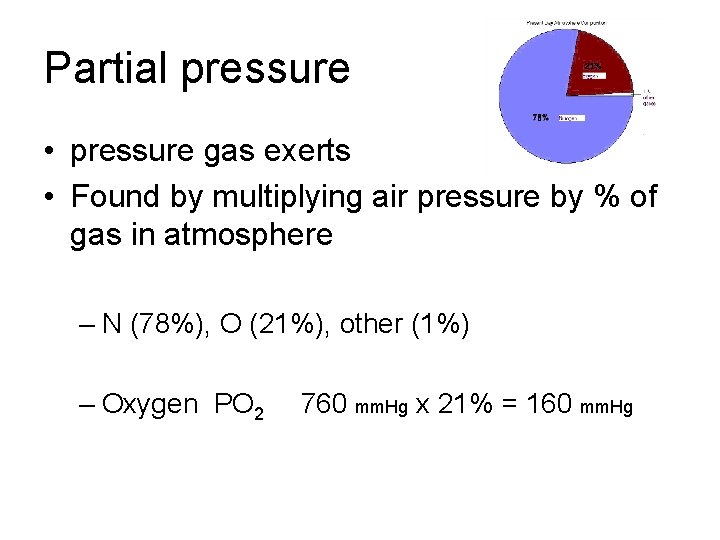
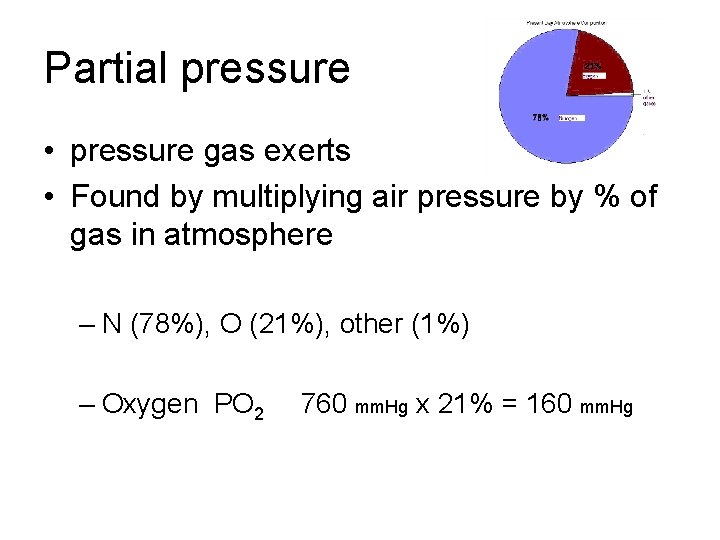
Partial pressure • pressure gas exerts • Found by multiplying air pressure by % of gas in atmosphere – N (78%), O (21%), other (1%) – Oxygen PO 2 760 mm. Hg x 21% = 160 mm. Hg
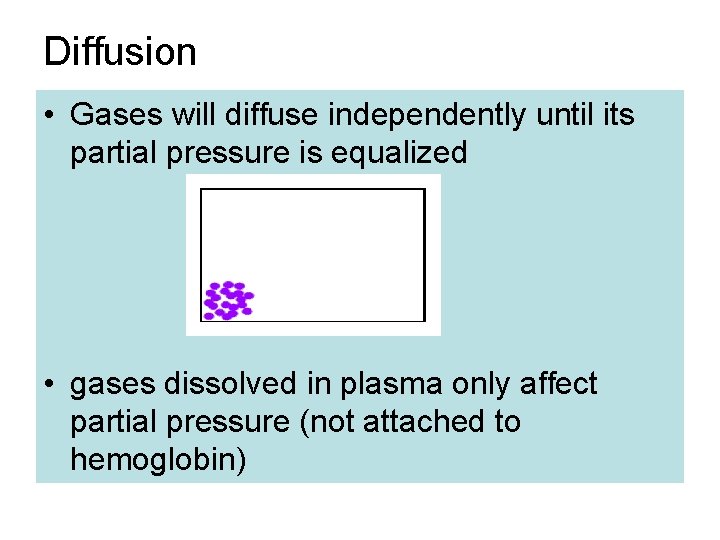
Diffusion • Gases will diffuse independently until its partial pressure is equalized • gases dissolved in plasma only affect partial pressure (not attached to hemoglobin)
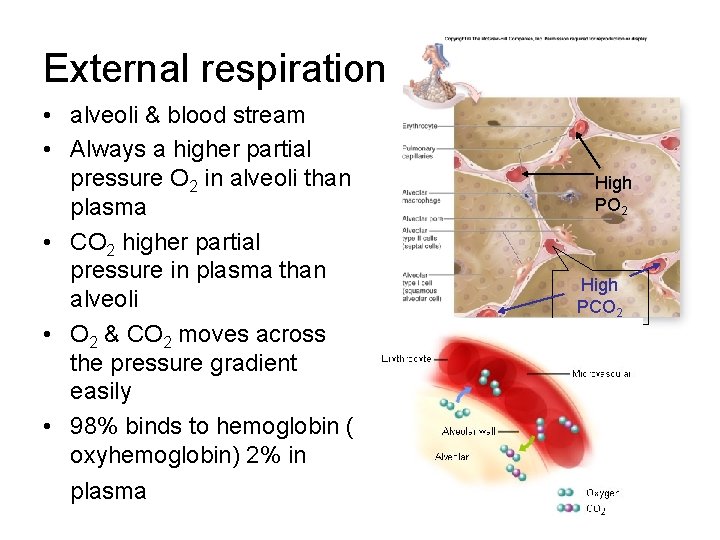
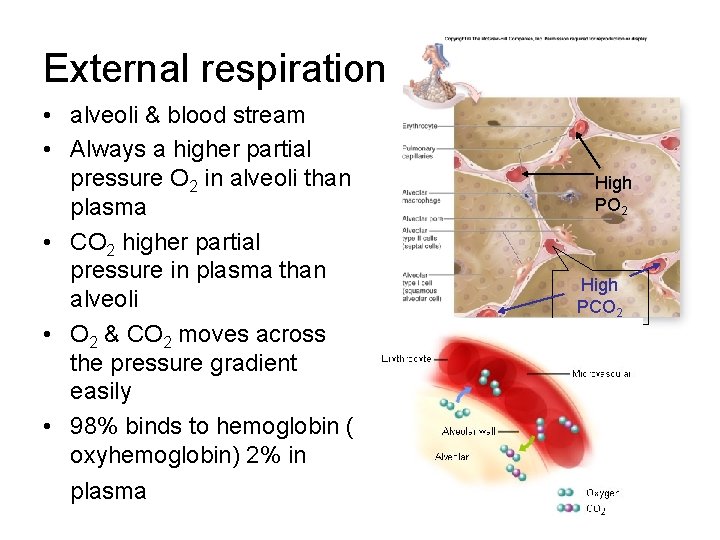
External respiration • alveoli & blood stream • Always a higher partial pressure O 2 in alveoli than plasma • CO 2 higher partial pressure in plasma than alveoli • O 2 & CO 2 moves across the pressure gradient easily • 98% binds to hemoglobin ( oxyhemoglobin) 2% in plasma High PO 2 High PCO 2
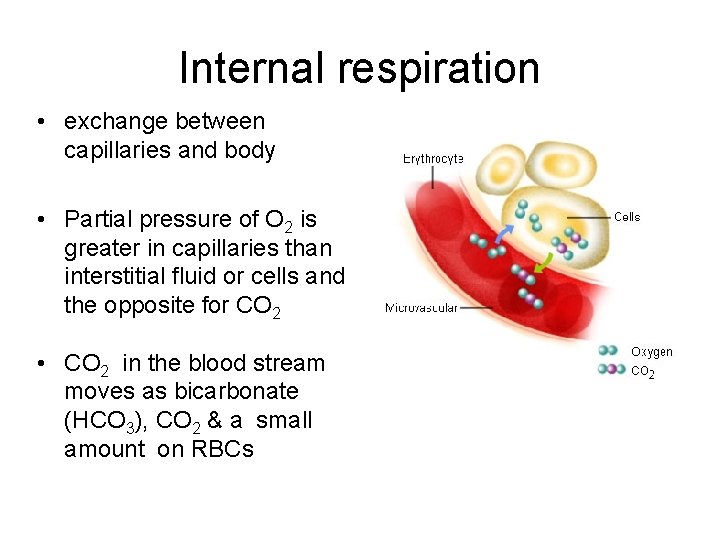
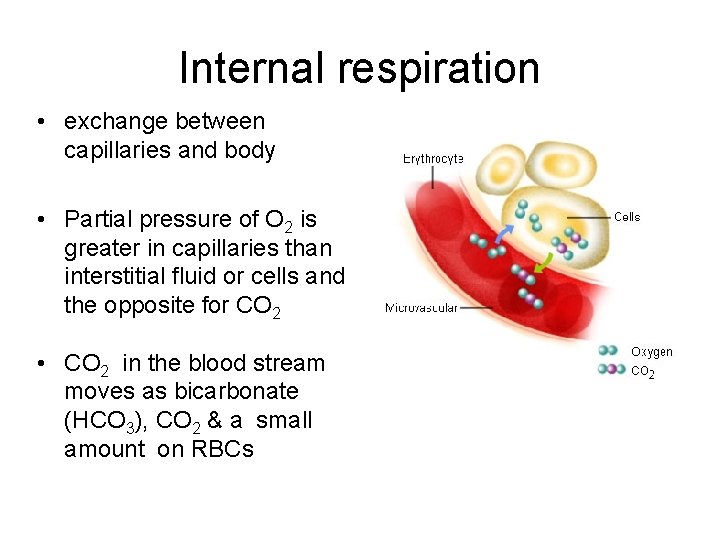
Internal respiration • exchange between capillaries and body • Partial pressure of O 2 is greater in capillaries than interstitial fluid or cells and the opposite for CO 2 • CO 2 in the blood stream moves as bicarbonate (HCO 3), CO 2 & a small amount on RBCs
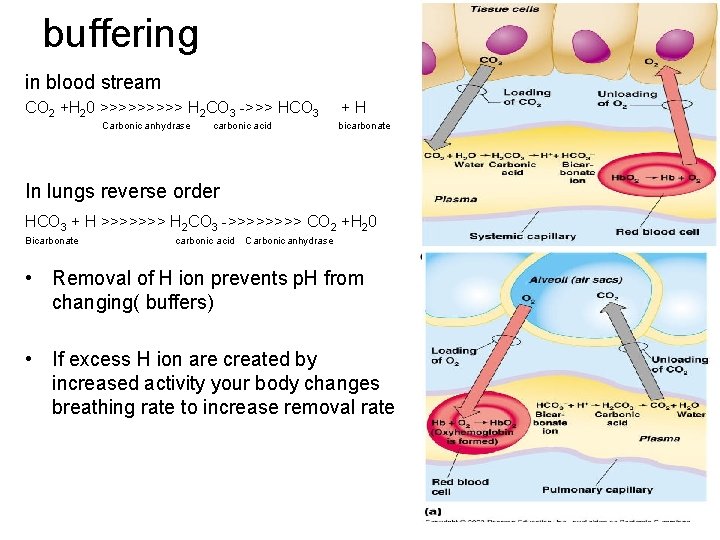
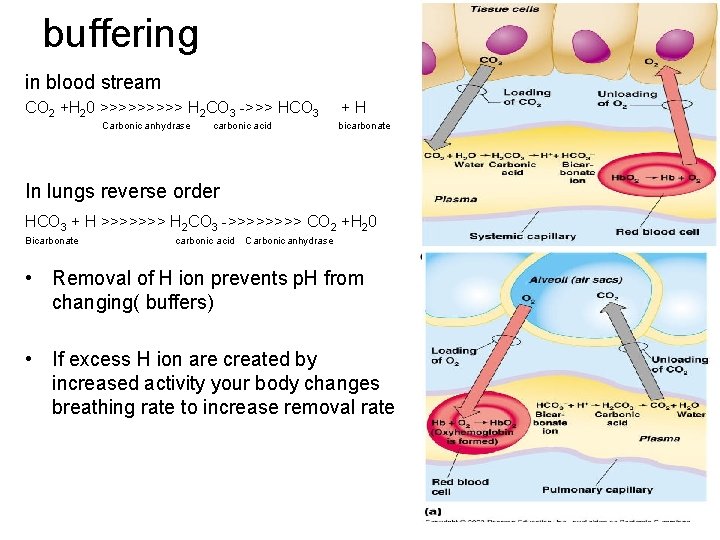
buffering in blood stream CO 2 +H 20 >>>>> H 2 CO 3 ->>> HCO 3 Carbonic anhydrase carbonic acid +H bicarbonate In lungs reverse order HCO 3 + H >>>>>>> H 2 CO 3 ->>>> CO 2 +H 20 Bicarbonate carbonic acid Carbonic anhydrase • Removal of H ion prevents p. H from changing( buffers) • If excess H ion are created by increased activity your body changes breathing rate to increase removal rate
Control of Breathing
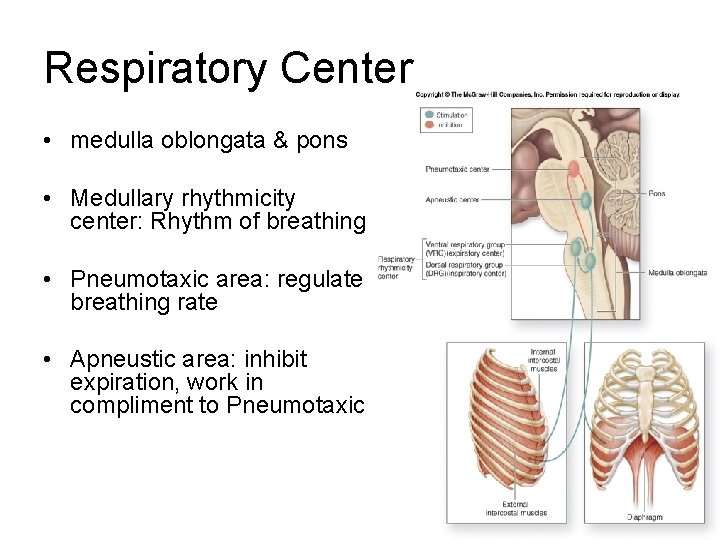
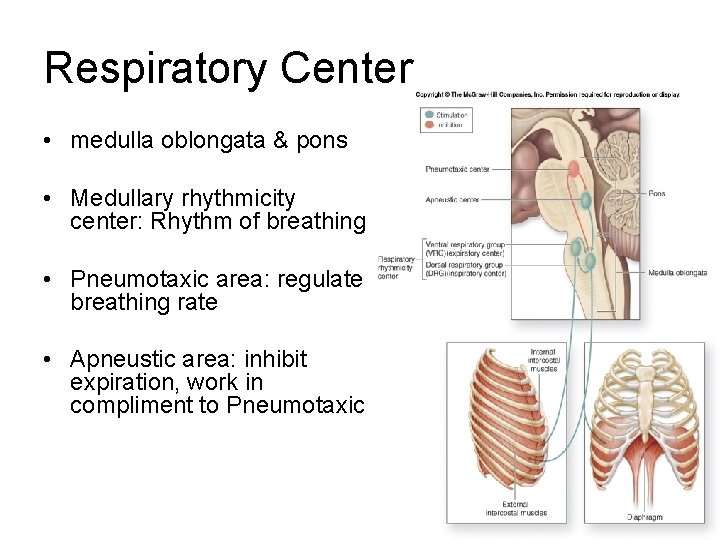
Respiratory Center • medulla oblongata & pons • Medullary rhythmicity center: Rhythm of breathing • Pneumotaxic area: regulate breathing rate • Apneustic area: inhibit expiration, work in compliment to Pneumotaxic
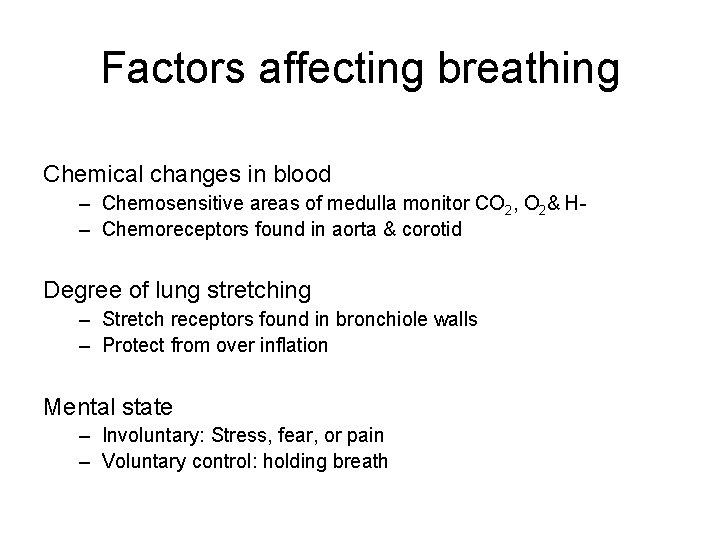
Factors affecting breathing Chemical changes in blood – Chemosensitive areas of medulla monitor CO 2, O 2& H– Chemoreceptors found in aorta & corotid Degree of lung stretching – Stretch receptors found in bronchiole walls – Protect from over inflation Mental state – Involuntary: Stress, fear, or pain – Voluntary control: holding breath
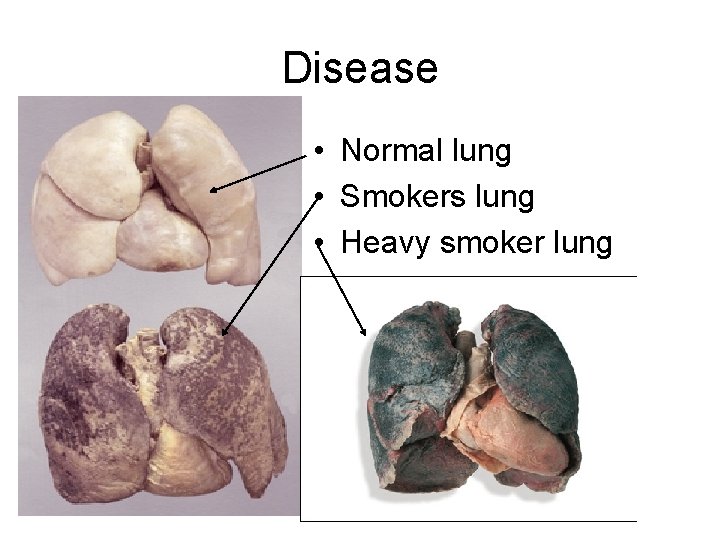
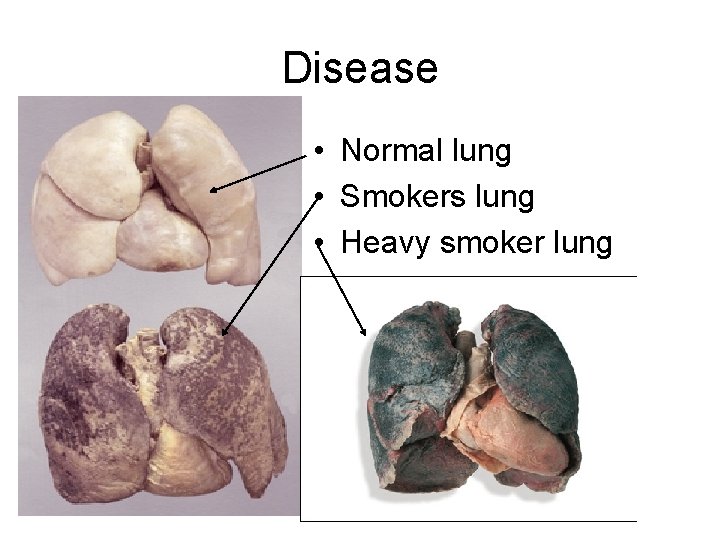
Disease • Normal lung • Smokers lung • Heavy smoker lung