Oral speech mechanism exercises in dysarthria following stroke

- Slides: 17

Oral speech mechanism exercises in dysarthria following stroke: speech and language therapists' practice and influences on it Catherine Mackenzie Margaret Muir Carolyn Allen Department of Educational and Professional Studies
Definitions Oral speech mechanism exercises Movements of the oral muscles, usually repetitive, without phonation e. g. lip spreading, tongue protrusion Commonly described in dysarthria therapy resource manuals dysarthria Acquired neuro-muscular motor speech disorder
Do oral speech mechanism exercises benefit speech? An important area for dysarthria efficacy research (Duffy, 2007) No robust direct evidence of speech improvement attributable to OSM exercises Ongoing debate as to whether the movement basis for OSM exercises is relevant to speech (Weismer, 2006)
Postal survey of current SLT practice SLTs identified by service heads/managers as working with adults with acquired dysarthria Scotland: 208 Wales: 99 N Ireland: 34 Total distribution: 341 Completed return: 191 (56%)
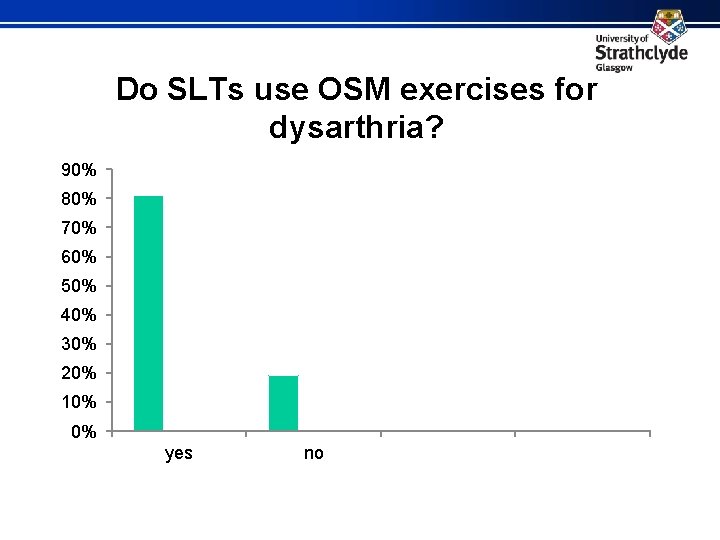
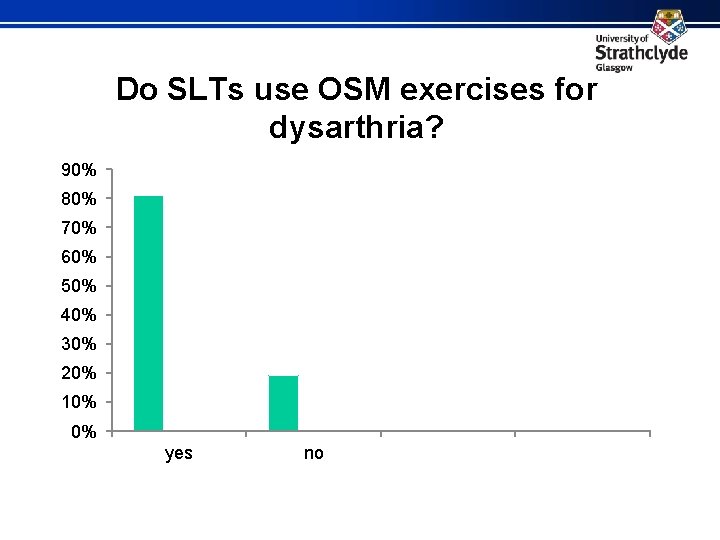
Do SLTs use OSM exercises for dysarthria? 90% 80% 70% 60% 50% 40% 30% 20% 10% 0% yes no
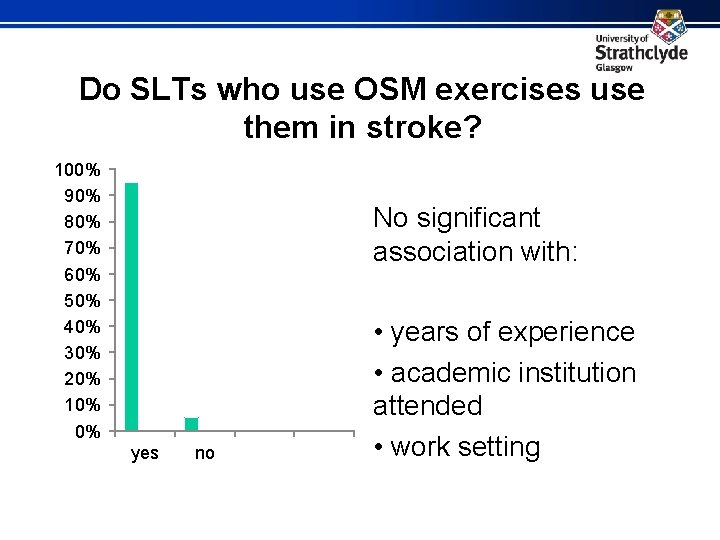
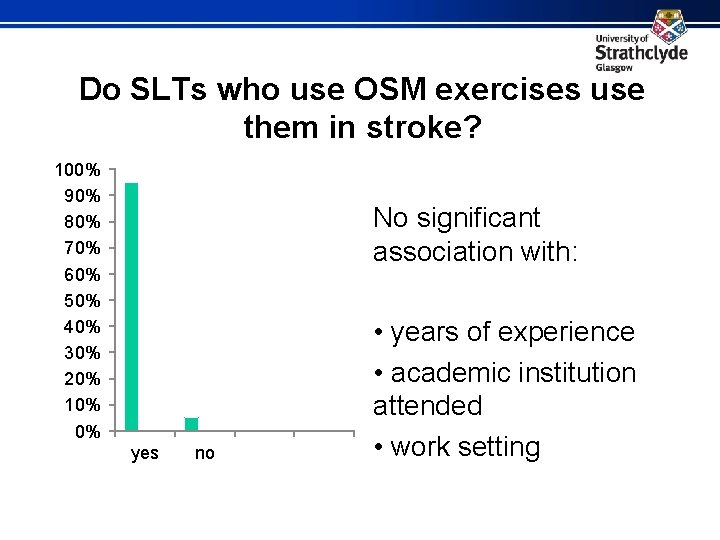
Do SLTs who use OSM exercises use them in stroke? 100% 90% 80% 70% 60% 50% 40% 30% 20% 10% 0% No significant association with: yes no • years of experience • academic institution attended • work setting
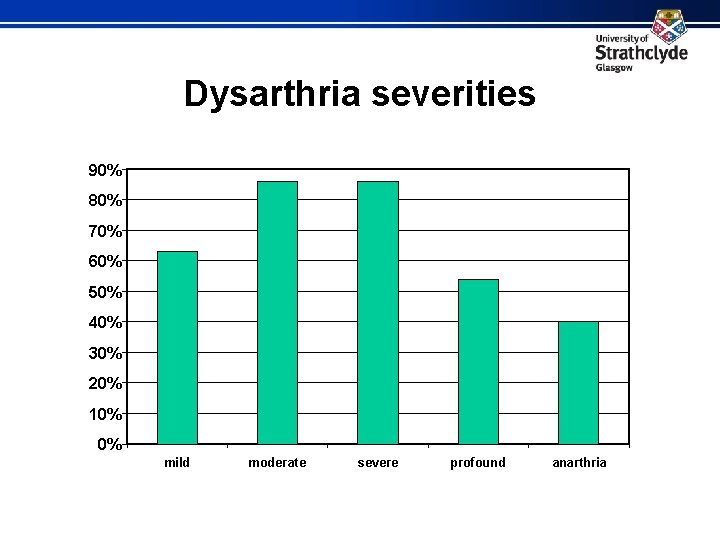
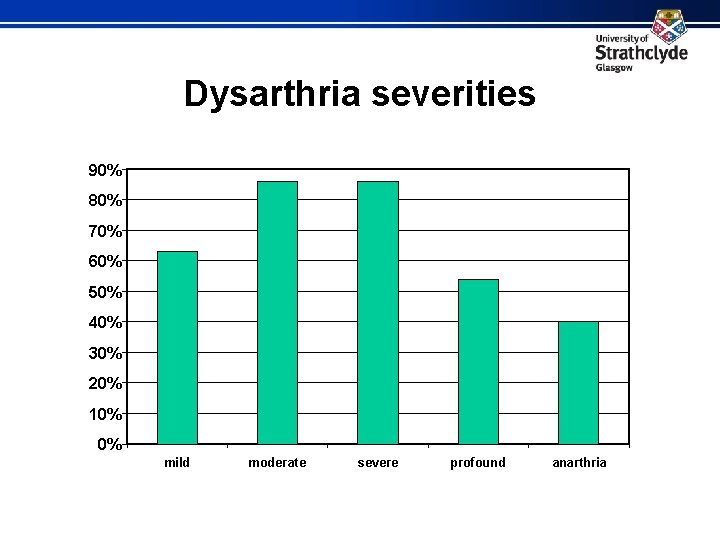
Dysarthria severities 90% 80% 70% 60% 50% 40% 30% 20% 10% 0% mild moderate severe profound anarthria
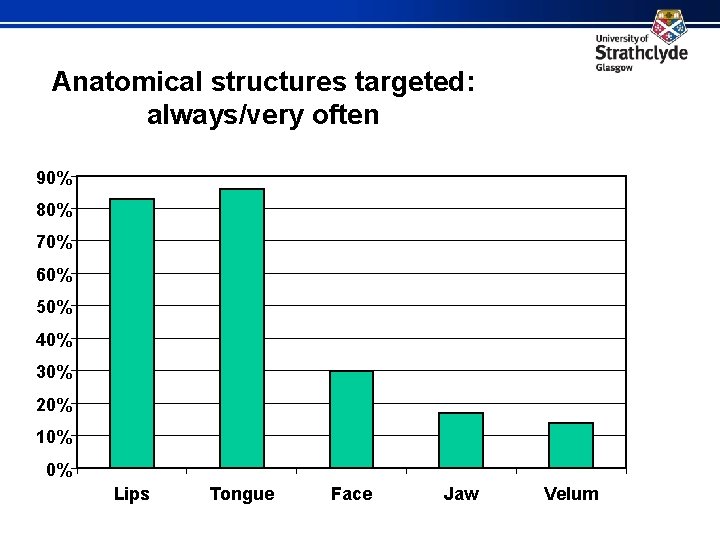
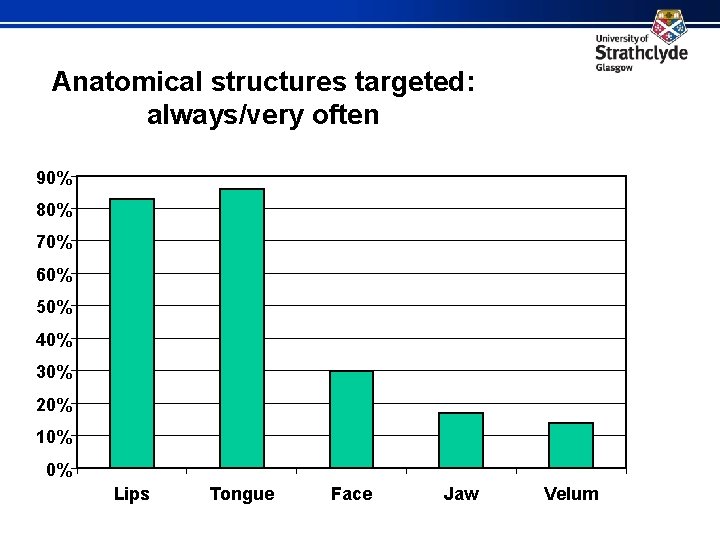
Anatomical structures targeted: always/very often 90% 80% 70% 60% 50% 40% 30% 20% 10% 0% Lips Tongue Face Jaw Velum
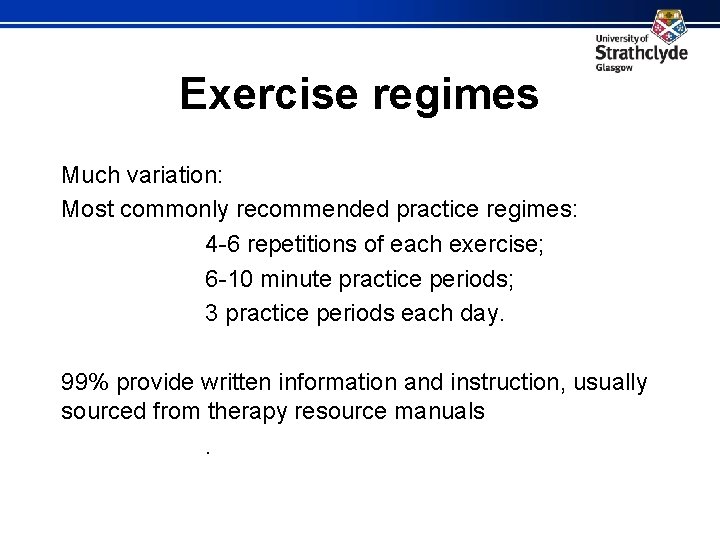
Exercise regimes Much variation: Most commonly recommended practice regimes: 4 -6 repetitions of each exercise; 6 -10 minute practice periods; 3 practice periods each day. 99% provide written information and instruction, usually sourced from therapy resource manuals.
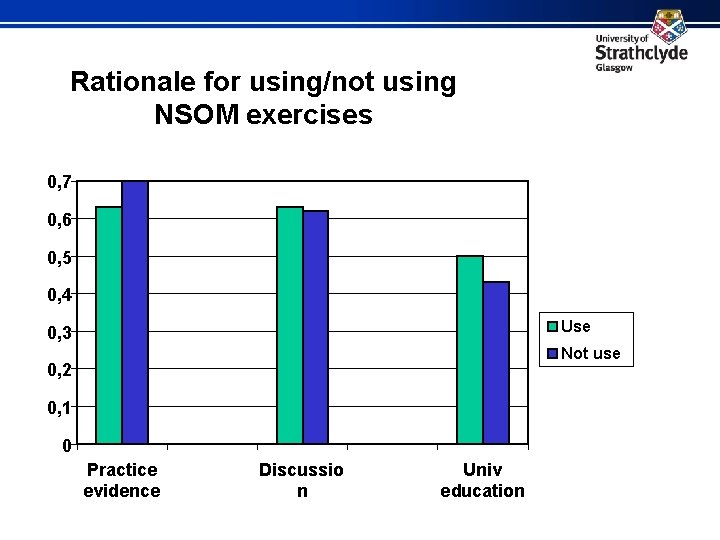
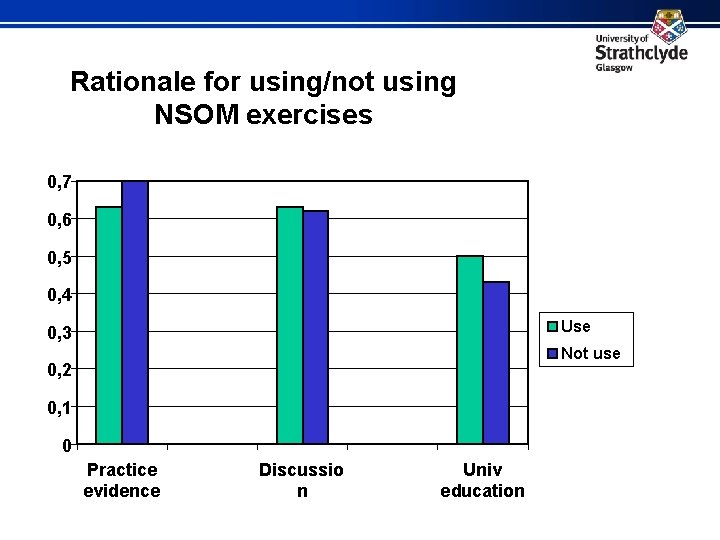
Rationale for using/not using NSOM exercises 0, 7 0, 6 0, 5 0, 4 Use 0, 3 Not use 0, 2 0, 1 0 Practice evidence Discussio n Univ education
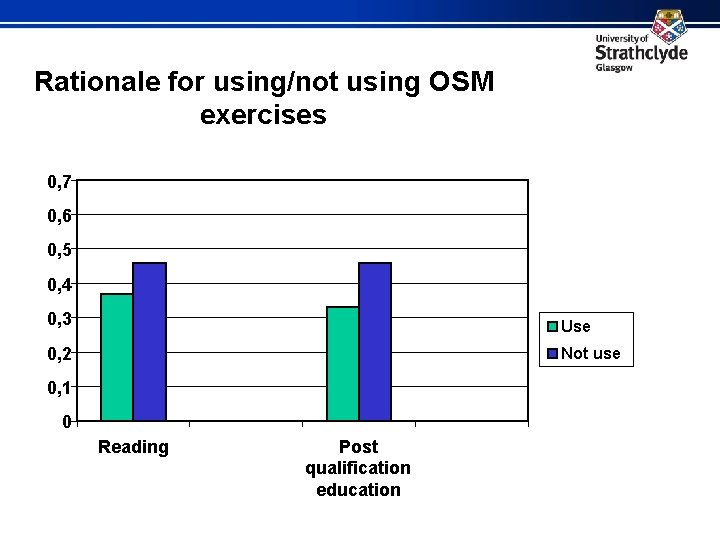
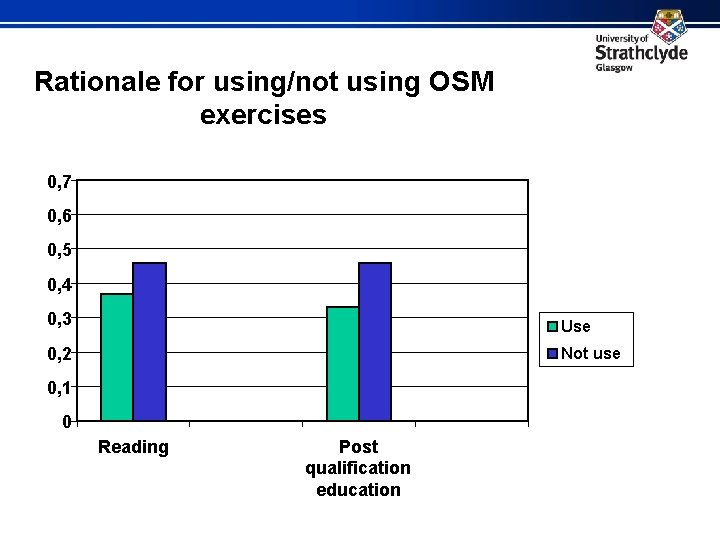
Rationale for using/not using OSM exercises 0, 7 0, 6 0, 5 0, 4 0, 3 Use 0, 2 Not use 0, 1 0 Reading Post qualification education
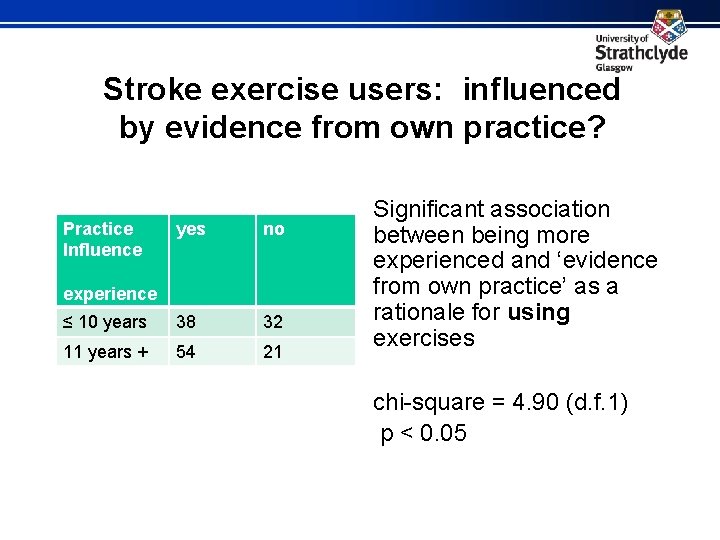
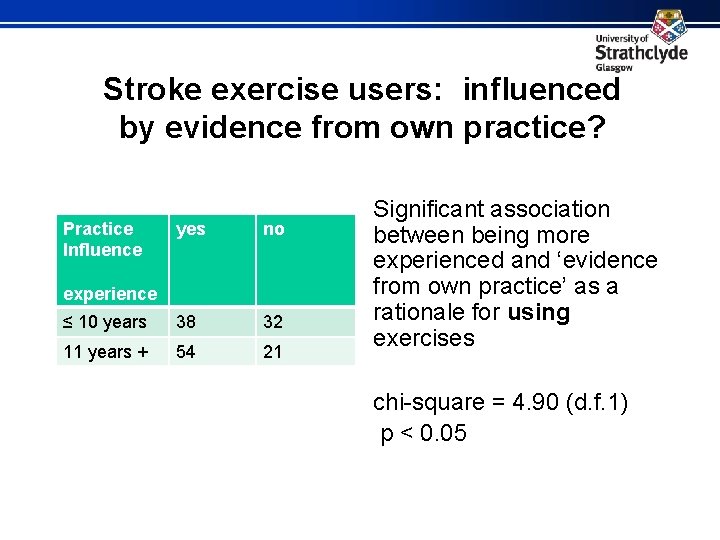
Stroke exercise users: influenced by evidence from own practice? Practice Influence yes no ≤ 10 years 38 32 11 years + 54 21 experience Significant association between being more experienced and ‘evidence from own practice’ as a rationale for using exercises chi-square = 4. 90 (d. f. 1) p < 0. 05
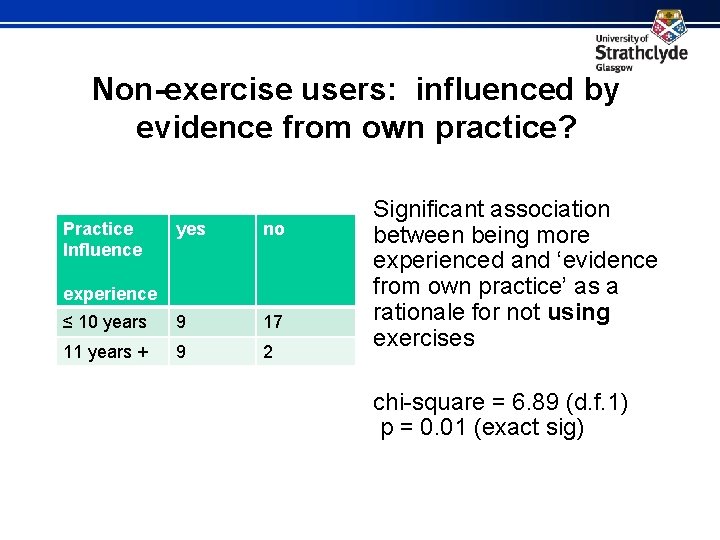
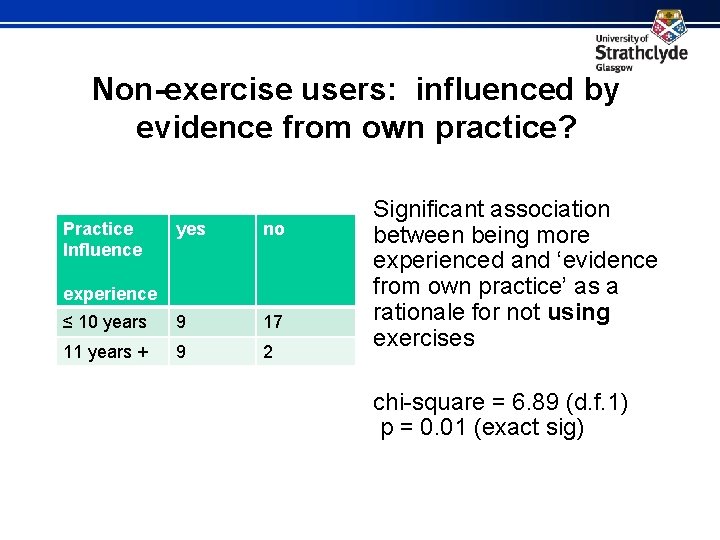
Non-exercise users: influenced by evidence from own practice? Practice Influence yes no ≤ 10 years 9 17 11 years + 9 2 experience Significant association between being more experienced and ‘evidence from own practice’ as a rationale for not using exercises chi-square = 6. 89 (d. f. 1) p = 0. 01 (exact sig)
Conclusions Despite the lack of published robust evidence that OSM exercises are or are not effective in improving speech, SLTs are strongly influenced by what they see as evidence from their own practice – both to use and to not use OSM exercises – in both instances this reason is more likely to be given by more experienced SLTs.
Conclusions • 3 out of 4 SLTs working with adult dysarthria use OSM exercises with dysarthric stroke patients • SLTs who use OSM exercises are not more or less experienced than those who do not • OSM exercises are used with all dysarthria severities
Conclusions There is a foundation for progressing to the next stage of research – assessing outcome in dysarthric stroke patients whose management does and does not include oral speech mechanism exercises
References Mackenzie, C, Muir, M and Allen, C. Non-speech oro-motor exercise use in acquired dysarthria management: regimes and rationales. International Journal of Language and Communication Disorders (in press) Duffy, JR, 2007, Motor speech disorders: History, current practice, future trends and goals. In G. Weismer (ed. ), Motor Speech Disorders (pp. 7 -56) (San Diego: Plural). Weismer, G, 2006, Philosophy of research in motor speech disorders. Clinical Linguistics and Phonetics, 20, 315 -349.