Oral phosphate binders in patients with kidney failure
Oral phosphate binders in patients with kidney failure N Engl J Med. 2010 Apr 8; 362(14): 1312 -24 신장내과 R 4 강혜란
Hyperphosphatemia § Universal complication of kidney failure § Accompanied by hypocalcemia, low serum levels of vitamin D § Usually lead to severe secondary hyperparathyroidism -> painful fractures, brown tumors, generalized osteopenia § Inorganic phosphorus : essential for multiple biologic functions § intracellular signal transduction § the production and function of cell membranes § energy exchange
Hyperphosphatemia § Body phosphorus § 80% : stored in bone and teeth § found in the intracellular compartment and in serum (primarily in the form of anions : H 2 PO 4 − and HPO 4 2−) § Kidney function is impaired -> excretion of phosphate declines § However, serum phosphate levels do not rise appreciably until the GFR < 30 ml /minute/1. 73 m² BSA § compensatory reduction in tubular resorption mediated by increased levels of serum parathyroid hormone, fibroblast growth factor 23, and phosphate itself
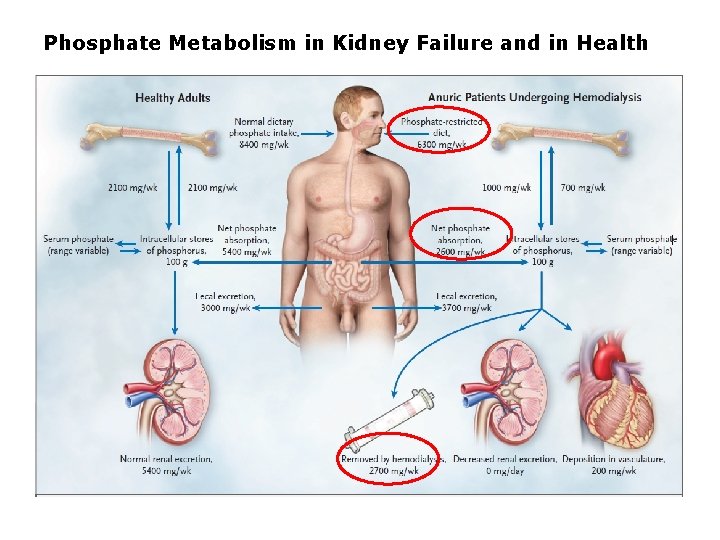
Phosphate Metabolism in Kidney Failure and in Health
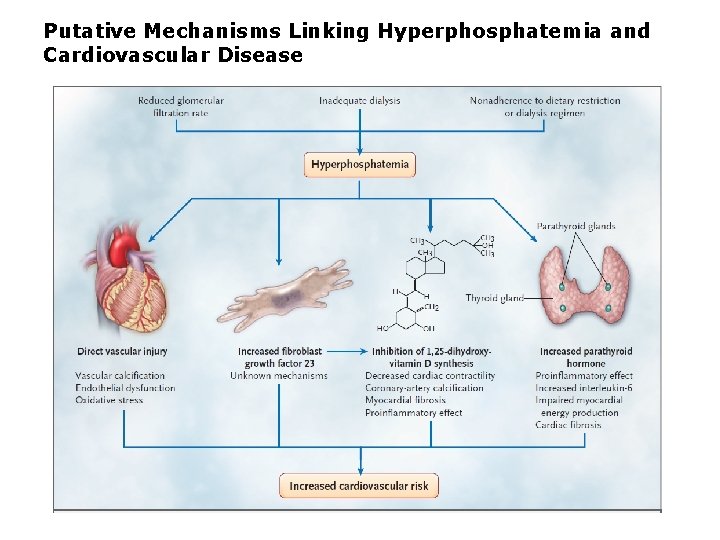
Putative Mechanisms Linking Hyperphosphatemia and Cardiovascular Disease
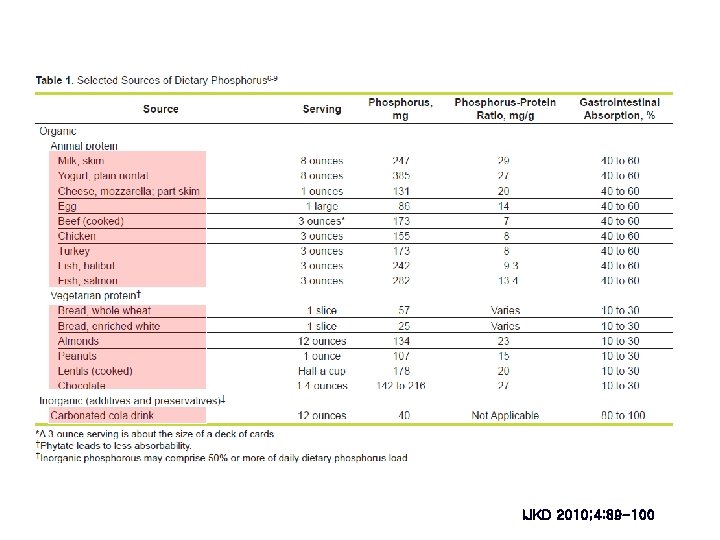
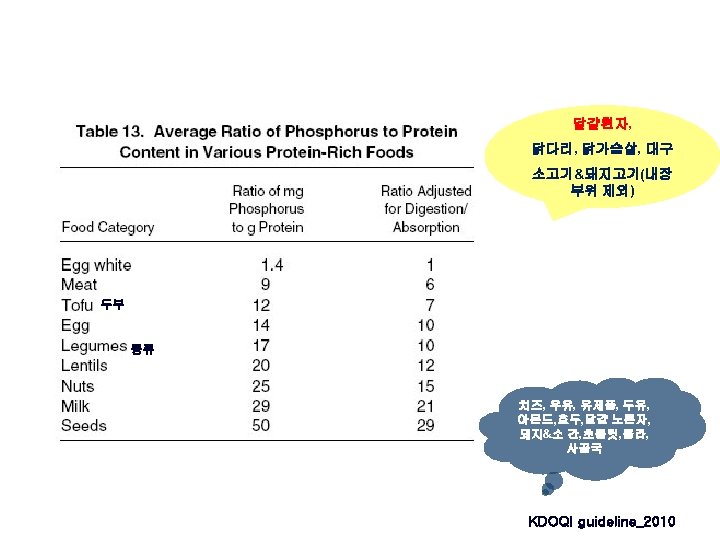
Dietary P restriction IJKD 2010; 4: 89 -100
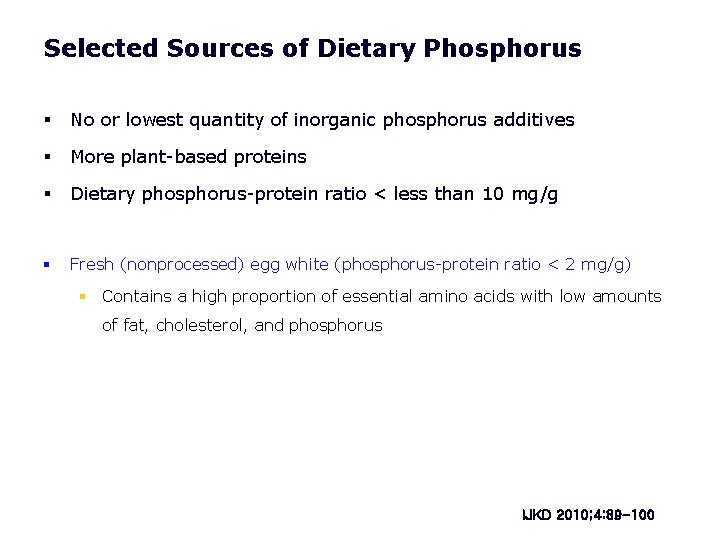
Selected Sources of Dietary Phosphorus § No or lowest quantity of inorganic phosphorus additives § More plant-based proteins § Dietary phosphorus-protein ratio < less than 10 mg/g § Fresh (nonprocessed) egg white (phosphorus-protein ratio < 2 mg/g) § Contains a high proportion of essential amino acids with low amounts of fat, cholesterol, and phosphorus IJKD 2010; 4: 89 -100
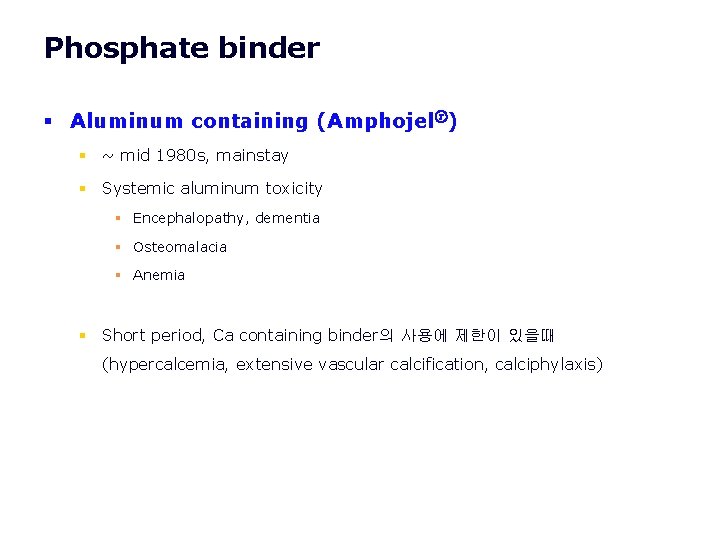
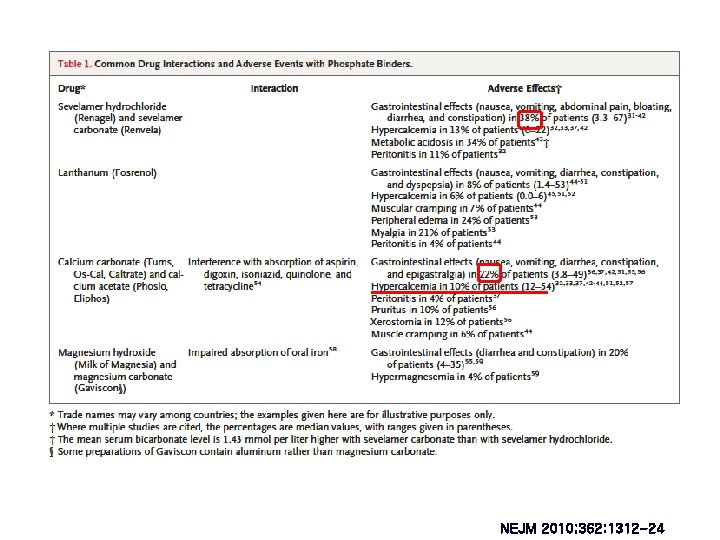
Phosphate binder § Aluminum containing (Amphojelⓡ) § ~ mid 1980 s, mainstay § Systemic aluminum toxicity § Encephalopathy, dementia § Osteomalacia § Anemia § Short period, Ca containing binder의 사용에 제한이 있을때 (hypercalcemia, extensive vascular calcification, calciphylaxis)
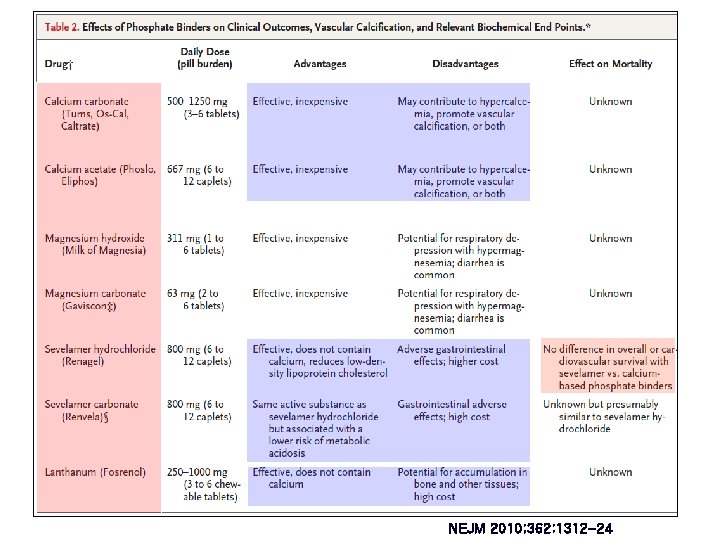
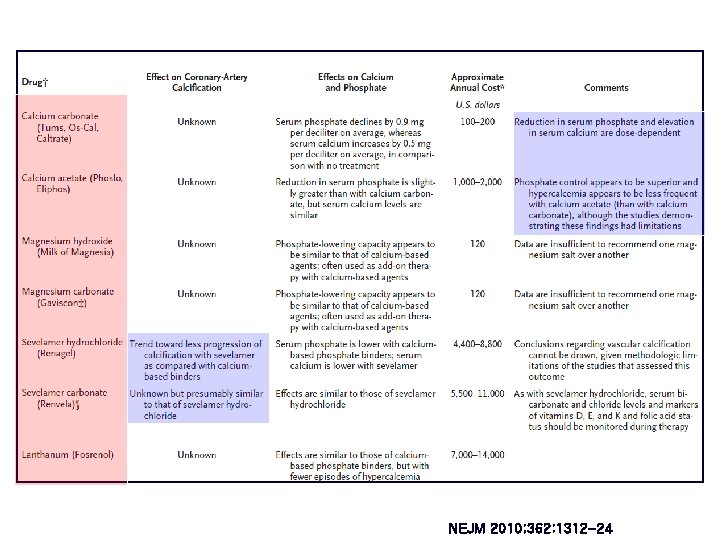
Phosphate binder § Ca based phosphate binders : Ca carbonate, Ca acetate § Most commonly used phosphate binders § Taken with meals effectively binds phosphates and limits their absorption § Doses § Patient’s compliance with dietary phosphate restriction § The CKD stage § Element Ca intake : max. 1500 mg/d (diet + binder; 2000 mg/d 미만) § Hypercalcemia-associated risks § extraskeletal calcification, PTH suppression, adynamic bone disease -> bone의 buffer capacity 감소 -> soft tissue calcium 침착 증가, 심혈관 예후 악화
Phosphate binder § Sevelamer § Non-absorbable, Anion-exchange resin (칼슘, 금속 기반 아닌 인결합제) § Sevelamer hydrochloride (Renagelⓡ) : metabolic acidosis § Sevelamer carbonate (Renvela ⓡ) § Vs Ca based phosphate binders § Low hypercalcemia incidence & vascular calcification § Mortality 차이없음
Phosphate binder § Lanthanum carbonate (Fosrenolⓡ) § Nonaluminum, noncalcium phosphate-binding agent § Some lanthanum appears to accumulate in bone and liver § No good quality studies have been powered to examine the effect of lanthanum § Vs Ca based phosphate binders § Similarly effective in reducing serum phosphate concentrations (limitation : lack of blinding, loss to follow-up) § Adverse events were more frequent : peripheral edema, myalgia
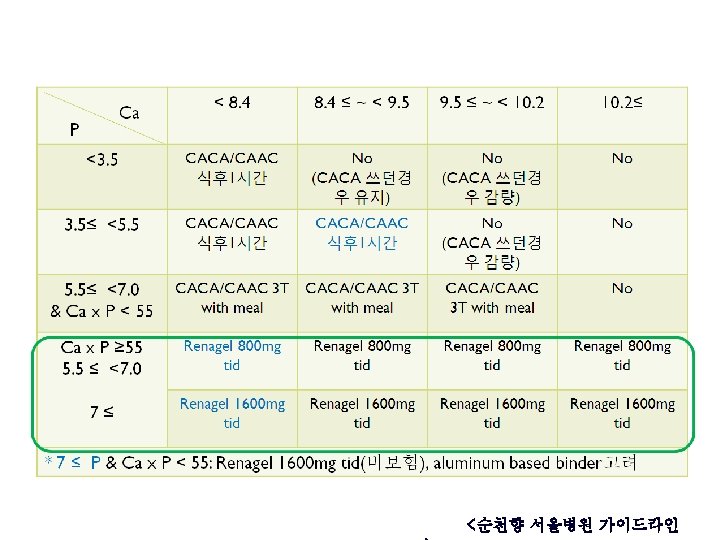
Phosphate binder § Calcium-containing phosphate binders : cost-effective first-line treatment option for the control of hyperphosphatemia, although the risk of long-term calcium exposure remains a concern § Persistent hyperphosphatemia -> Sevelamer • Sevelamer 800 mg/1 T 877원 > 2. 4 g/d복용 시 78930원/month • Ca. CO 3 500 mg 1 T 30원 > 1. 5 g (element Ca 600 mg)/d 복용 시 2700원/month • Sevelamer 보험기준 : 투석을 받고 있는 ESRD 환자중 혈액검사상(매월 1회정도) 혈중 인(P) 수치가 5. 5㎎/㎗ 이상이면서 Ca× P산물(product)이 55 mg 2/㎗ 2 이상인 환자에게 인정
NEJM 2010; 362: 1312 -24
Phosphate binder NEJM 2010; 362: 1312 -24
NEJM 2010; 362: 1312 -24
Management of hyperphosphatemia § Dietary phosphate restriction effectively § Oral phosphate binders § Improve phosphate control § Patient’s pill burden § Risk of adverse events § Cost
References § Kidney International (2009) § § Iran J Kidney Dis. 2010 Apr; 4(2): 89 -100 § § KDIGO Clinical Practice Guideline for the Diagnosis, Evaluation, Prevention, and Treatment of Chronic Kidney Disease-Mineral and Bone Disorder (CKD-MBD) Organic and inorganic dietary phosphorus and its management in chronic kidney disease N Engl J Med. 2010 Apr 8; 362(14): 1312 -24 § Oral phosphate binders in patients with kidney failure
Treatment of abnormal PTH level
Secondary hyperparathyroidism § VDRA( Vit D receptor activator ) § Calcimimetics § Parathyroidectomy
Vitamin D therapy § Calcitriol (1, 25 -dihydroxyvitamin D) (Rocaltrolⓡ) § Parathyroid gland의 the vitamin D receptor (VDR) 에 작용하여 PTH transcription을 억제, Parathyroid cell 증식 감소 § 뼈와 장에서 칼슘 흡수 증가시켜 혈청 칼슘을 증가 -> PTH분비 억제 § S/E : Hypercalcemia, hyperphosphatemia, vascular calcification, adynamic bone disease § Paricalcitol (19 -nor-1 -alpha, 25 -dihydroxyvitamin D 2 ( Zemplarⓡ) § "second generation" vitamin D analogue. Selective VDRA § less severe increments in serum calcium and phosphate (prospective randomized trial is needed) § Vitamin D derivatives should not be given until the serum phosphate concentration has been controlled ( < 5. 5 mg/d. L) and the serum calcium is less than 9. 5 mg/d. L : metastatic calcification risk (P <5. 5 & Ca<9. 5 가 아니라면 vitamin D 투여 금기)
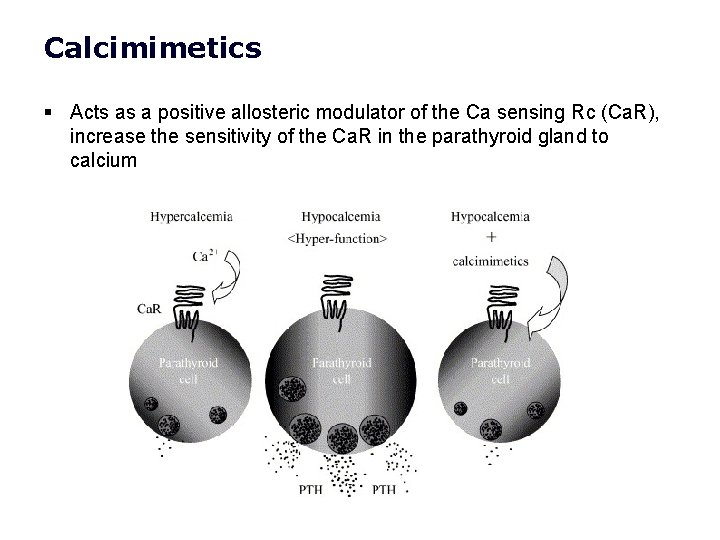
Calcimimetics § Acts as a positive allosteric modulator of the Ca sensing Rc (Ca. R), increase the sensitivity of the Ca. R in the parathyroid gland to calcium
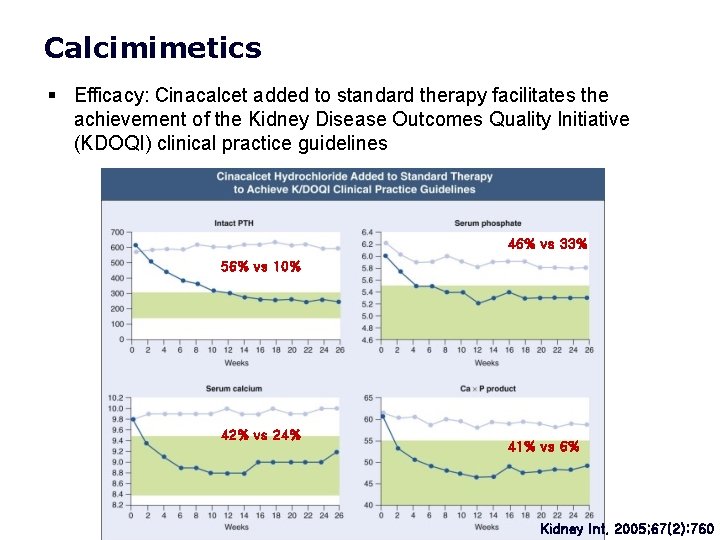
Calcimimetics § Efficacy: Cinacalcet added to standard therapy facilitates the achievement of the Kidney Disease Outcomes Quality Initiative (KDOQI) clinical practice guidelines 46% vs 33% 56% vs 10% 42% vs 24% 41% vs 6% Kidney Int. 2005; 67(2): 760
Calcimimetics § Cinacalcet(Regparaⓡ) § Indication : PTH > 300 pg/m. L, s. Ca > 8. 4 mg/d. L § Dose § Starting dose 30 mg/d, § Stepwise increments to 60, 90, 180 mg/d q 4 wks § Should not be started if serum calcium is below 8. 4 mg/d. L
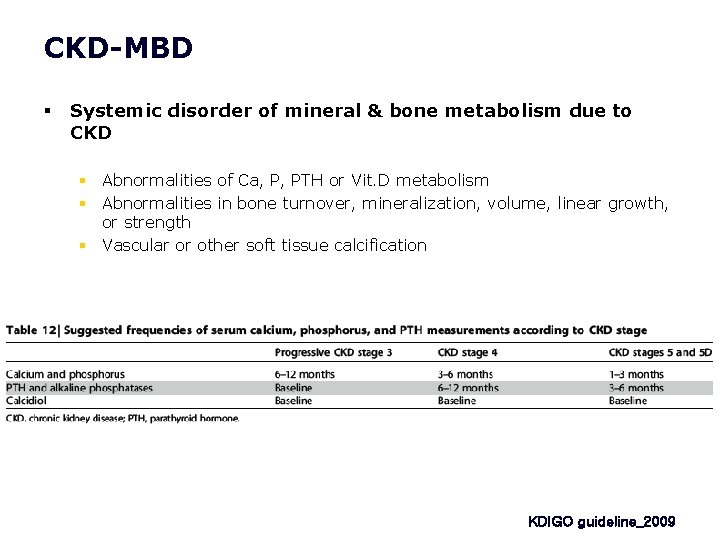
CKD-MBD § Systemic disorder of mineral & bone metabolism due to CKD § Abnormalities of Ca, P, PTH or Vit. D metabolism § Abnormalities in bone turnover, mineralization, volume, linear growth, or strength § Vascular or other soft tissue calcification KDIGO guideline_2009
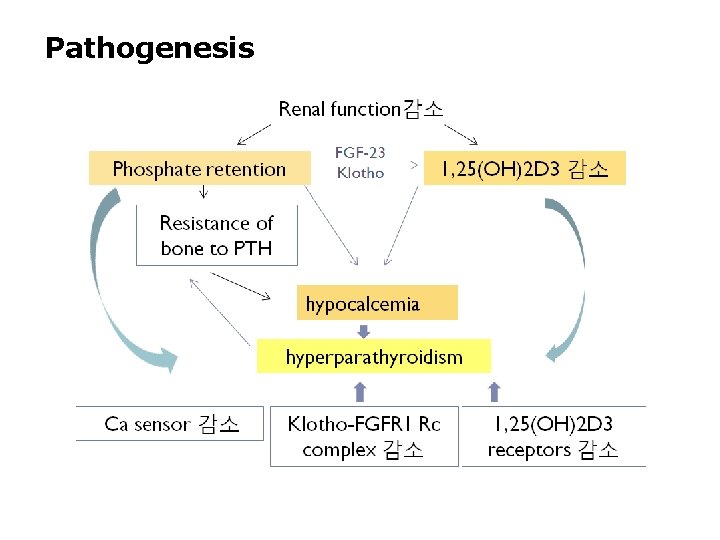
Pathogenesis
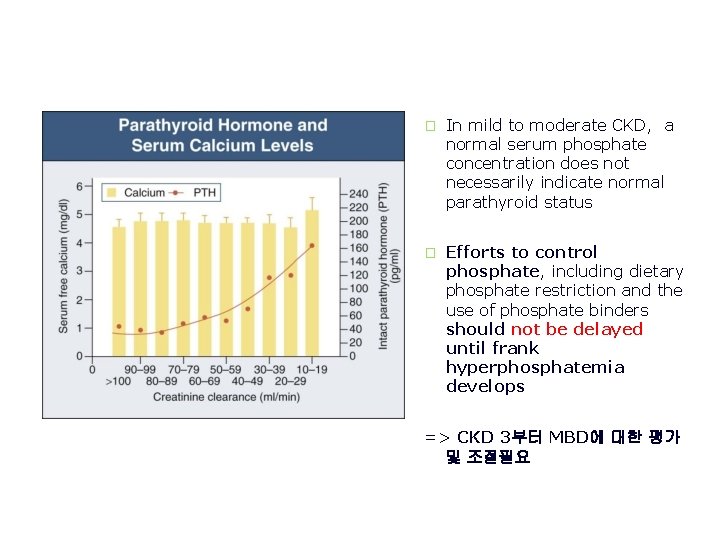
� In mild to moderate CKD, a normal serum phosphate concentration does not necessarily indicate normal parathyroid status � Efforts to control phosphate, including dietary phosphate restriction and the use of phosphate binders should not be delayed until frank hyperphosphatemia develops => CKD 3부터 MBD에 대한 평가 및 조절필요
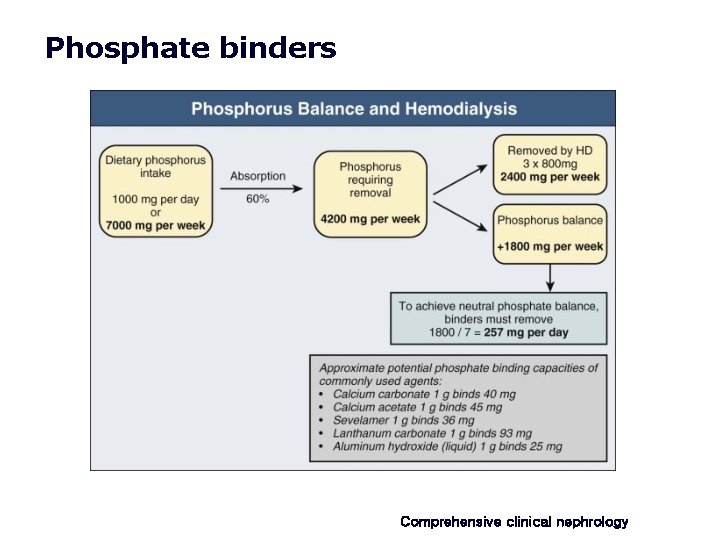
Phosphate binders Comprehensive clinical nephrology
- Slides: 29