Oral calcium load test for recurrent stoneformers V

- Slides: 26
Oral calcium load test for recurrent stone-formers V. Castiglione 1, R. Alkouri 2, L. Pieroni 3, M. Leban 2, R. Inaoui 4, R. Araman 5, M. P. Dousseaux 6, E. Cavalier 1, I. Tostivint 5. 1: Clinical Chemistry department, University of Liège, CHU du Sart Tilman, Liège, Belgium, 2: Endocrinology biochemistry laboratory, Pitié Salpêtrière Hospital, Paris, France 3: Biochemistry and Hormonology laboratory, University Hospital of Montpellier (CHU), France 4: Rheumatology, 5: Nephrology, 6: Dietetic, Pitié Salpêtrière Hospital, Paris, France 1
Map � Introduction: � What is the oral calcium load test? � Pak test interpretation � Study: � Population and methods � Results � Conclusions 2
What is Oral calcium load test? � Dynamic test � Urine and blood analysis � Before/after 1 g Ca intake p. o. � C. Pak et al. A simple test for the diagnosis of absorptive, resorptive and renal hypercalciurias. N Engl J Med. 1975 “Pak test” 3
Purpose � Nephrology � Diagnosis of reccurent calcium kidney-stone � Endocrinology � Diagnosis of borderline Hyperparathyroidism (HPT) � Calcium metabolism investigation 4
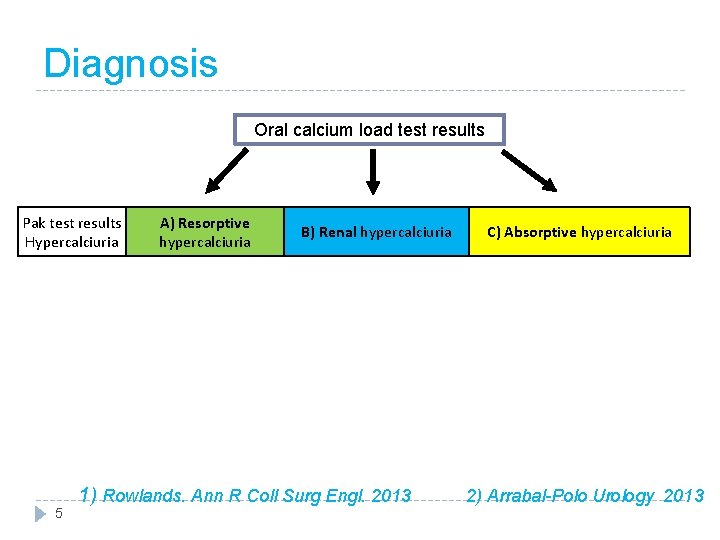
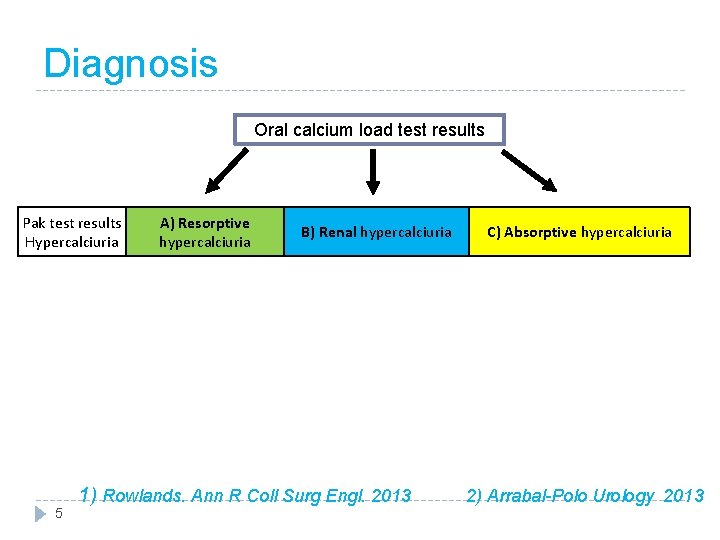
Diagnosis Oral calcium load test results Pak test results Hypercalciuria 5 A) Resorptive hypercalciuria B) Renal hypercalciuria C) Absorptive hypercalciuria 1) Rowlands. Ann R Coll Surg Engl. 2013 2) Arrabal-Polo Urology 2013
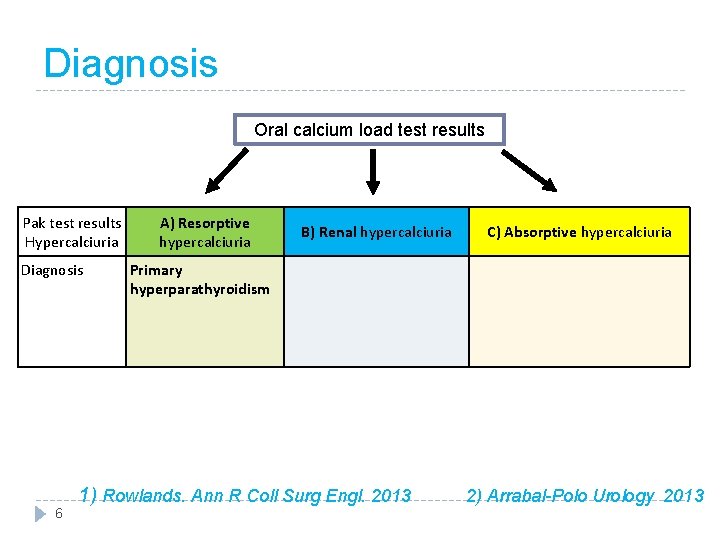
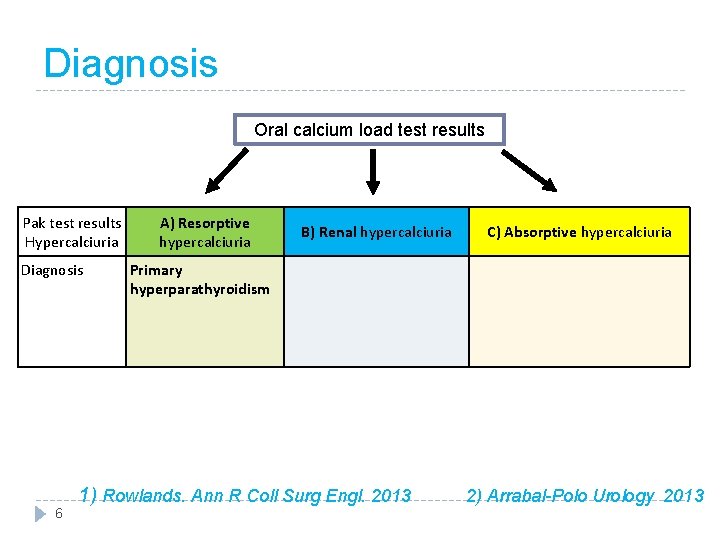
Diagnosis Oral calcium load test results Pak test results Hypercalciuria Diagnosis 6 A) Resorptive hypercalciuria B) Renal hypercalciuria C) Absorptive hypercalciuria Primary hyperparathyroidism 1) Rowlands. Ann R Coll Surg Engl. 2013 2) Arrabal-Polo Urology 2013
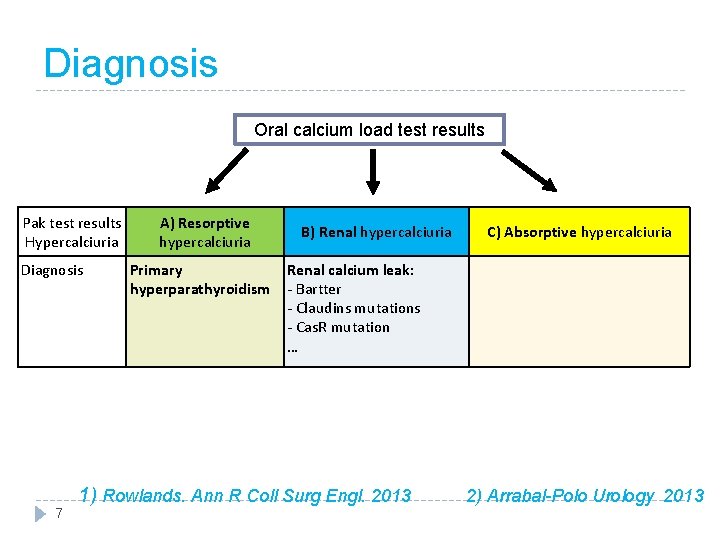
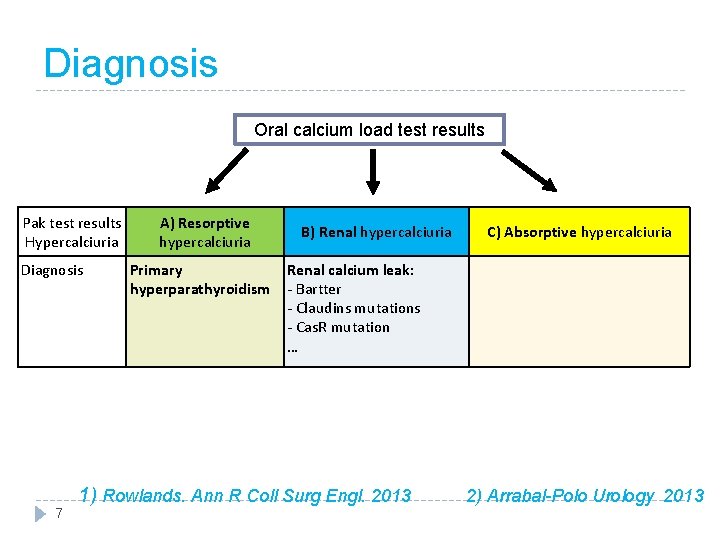
Diagnosis Oral calcium load test results Pak test results Hypercalciuria Diagnosis 7 A) Resorptive hypercalciuria Primary hyperparathyroidism B) Renal hypercalciuria C) Absorptive hypercalciuria Renal calcium leak: - Bartter - Claudins mutations - Cas. R mutation … 1) Rowlands. Ann R Coll Surg Engl. 2013 2) Arrabal-Polo Urology 2013
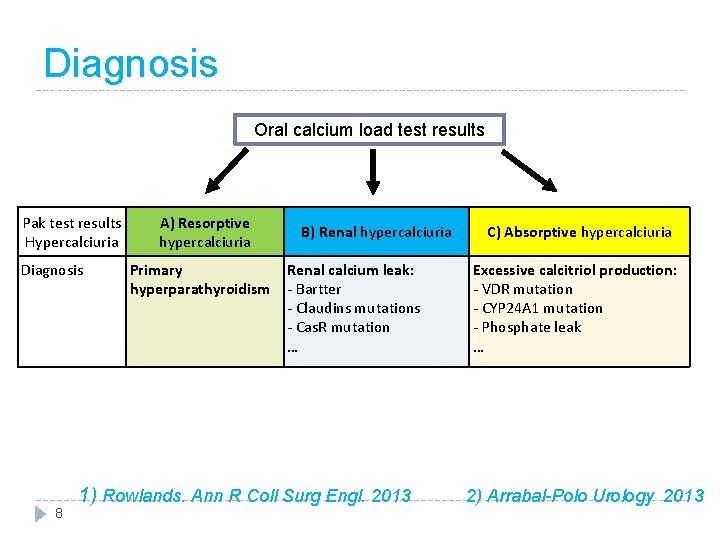
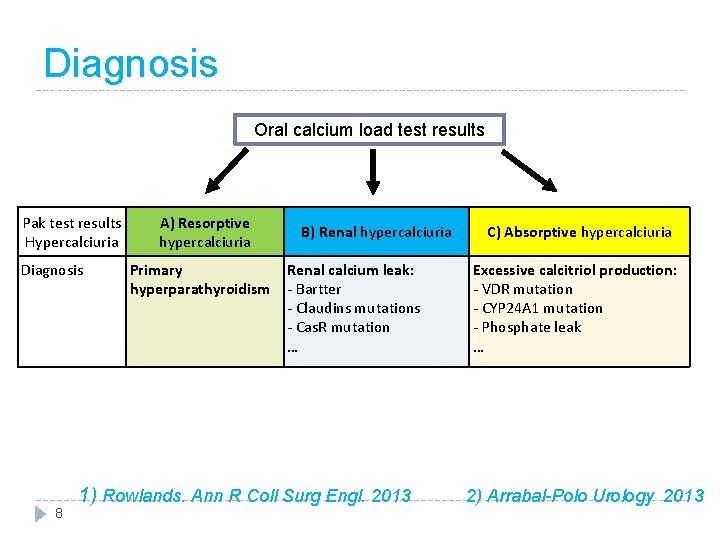
Diagnosis Oral calcium load test results Pak test results Hypercalciuria Diagnosis 8 A) Resorptive hypercalciuria Primary hyperparathyroidism B) Renal hypercalciuria Renal calcium leak: - Bartter - Claudins mutations - Cas. R mutation … C) Absorptive hypercalciuria Excessive calcitriol production: - VDR mutation - CYP 24 A 1 mutation - Phosphate leak … 1) Rowlands. Ann R Coll Surg Engl. 2013 2) Arrabal-Polo Urology 2013
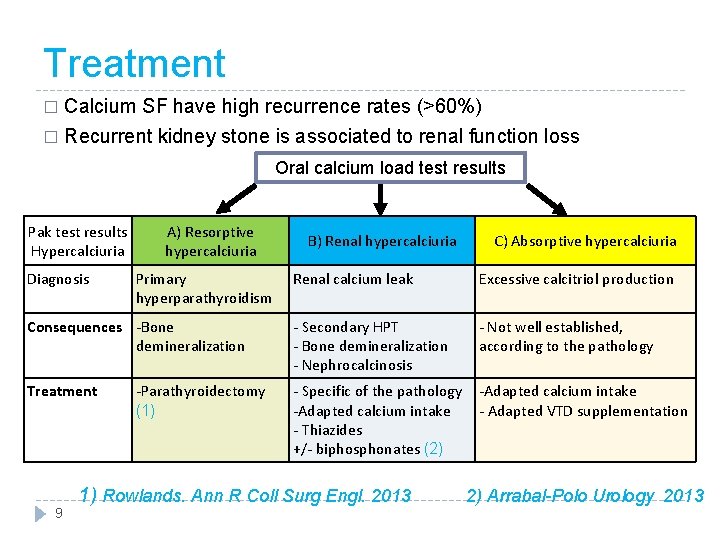
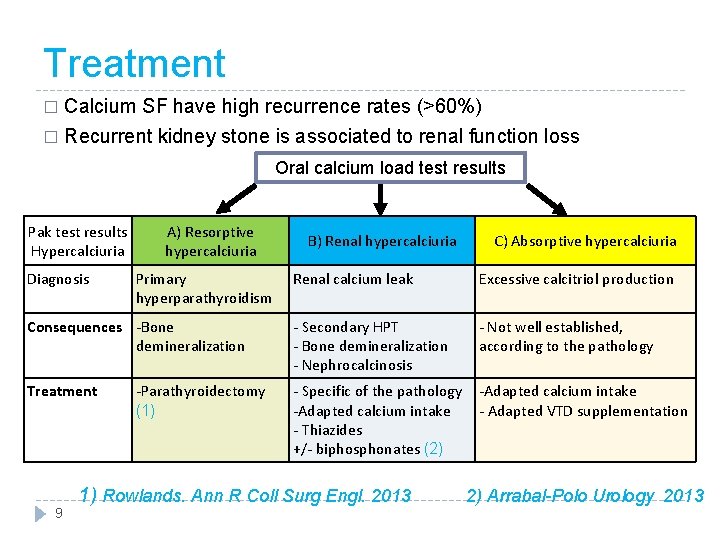
Treatment Calcium SF have high recurrence rates (>60%) � Recurrent kidney stone is associated to renal function loss � Oral calcium load test results Pak test results Hypercalciuria Diagnosis A) Resorptive hypercalciuria Primary hyperparathyroidism Consequences -Bone demineralization Treatment 9 -Parathyroidectomy (1) B) Renal hypercalciuria C) Absorptive hypercalciuria Renal calcium leak Excessive calcitriol production - Secondary HPT - Bone demineralization - Nephrocalcinosis - Not well established, according to the pathology - Specific of the pathology -Adapted calcium intake - Thiazides +/- biphosphonates (2) -Adapted calcium intake - Adapted VTD supplementation 1) Rowlands. Ann R Coll Surg Engl. 2013 2) Arrabal-Polo Urology 2013
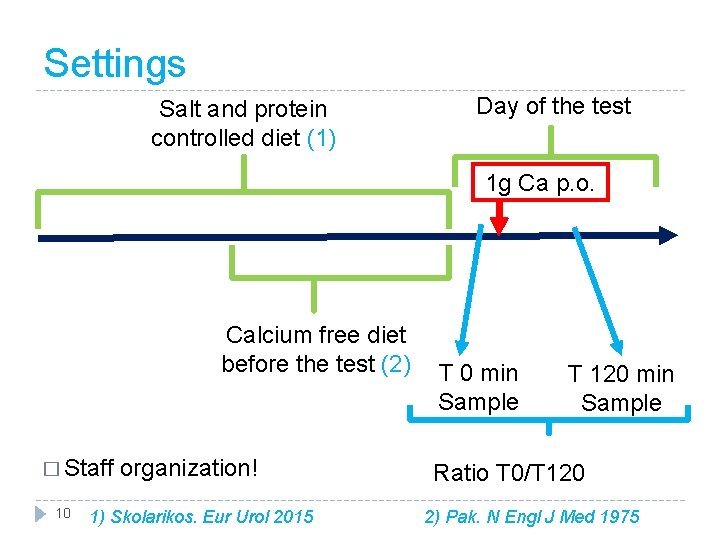
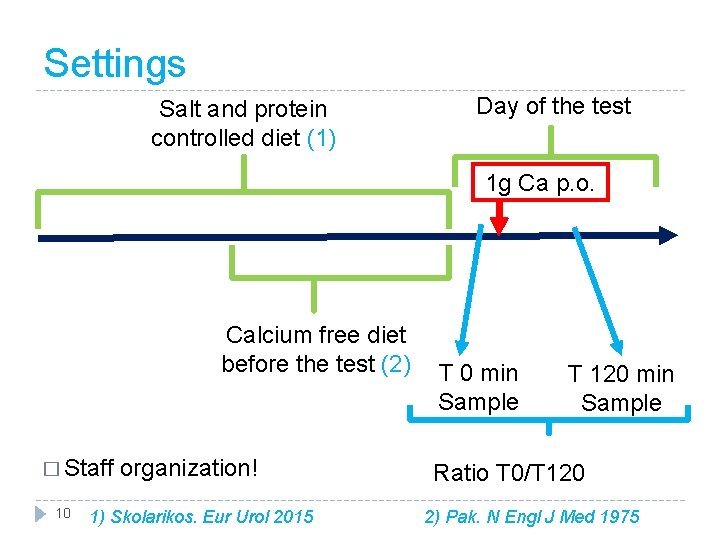
Settings Salt and protein controlled diet (1) Day of the test 1 g Ca p. o. Calcium free diet before the test (2) � Staff organization! 10 T 0 min Sample T 120 min Sample Ratio T 0/T 120 1) Skolarikos. Eur Urol 2015 2) Pak. N Engl J Med 1975
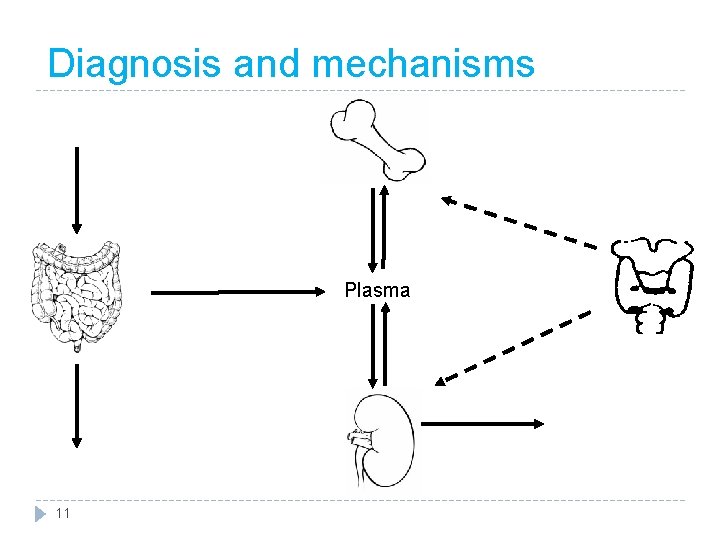
Diagnosis and mechanisms Plasma 11
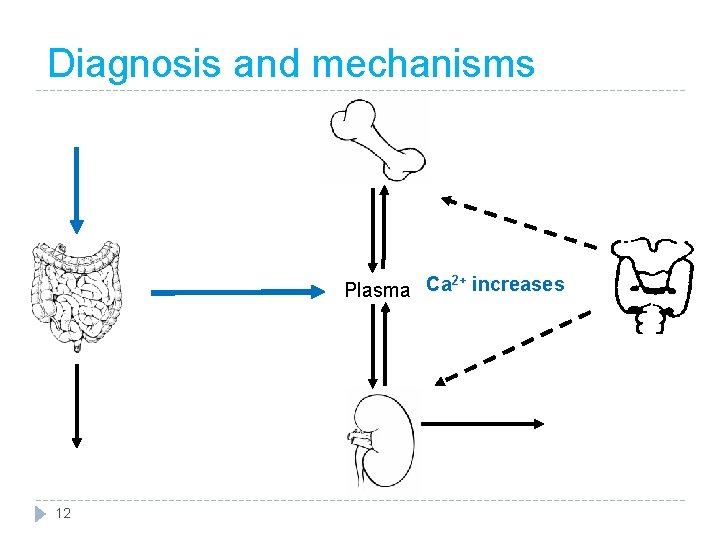
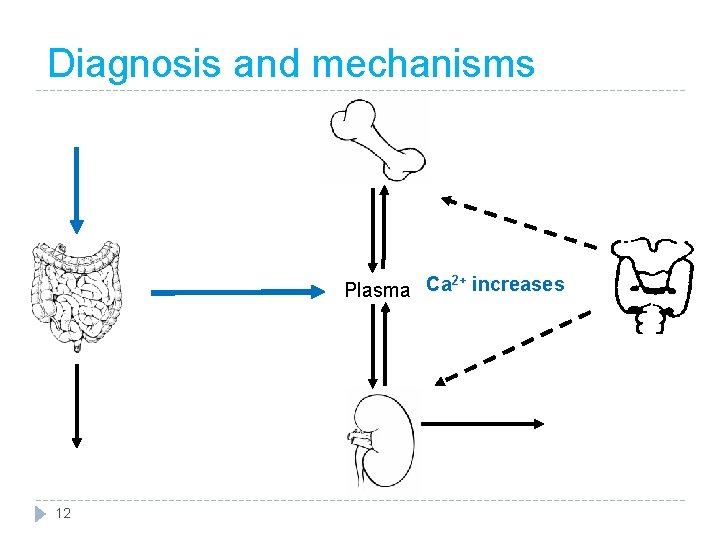
Diagnosis and mechanisms 2+ Plasma Ca increases 12
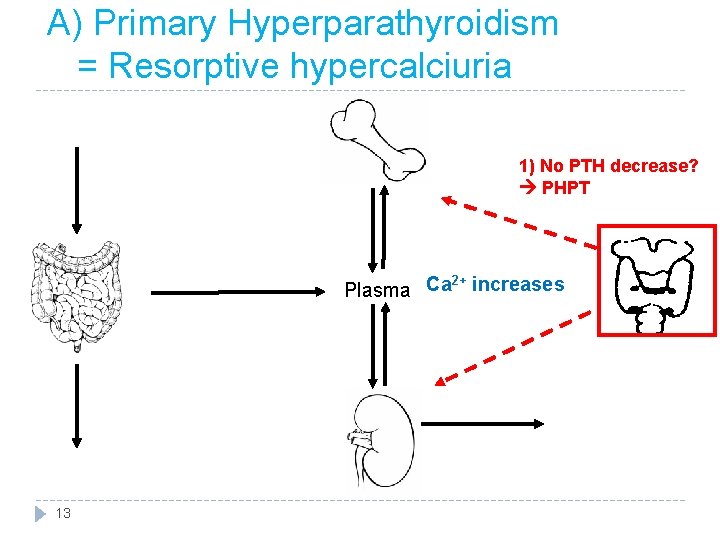
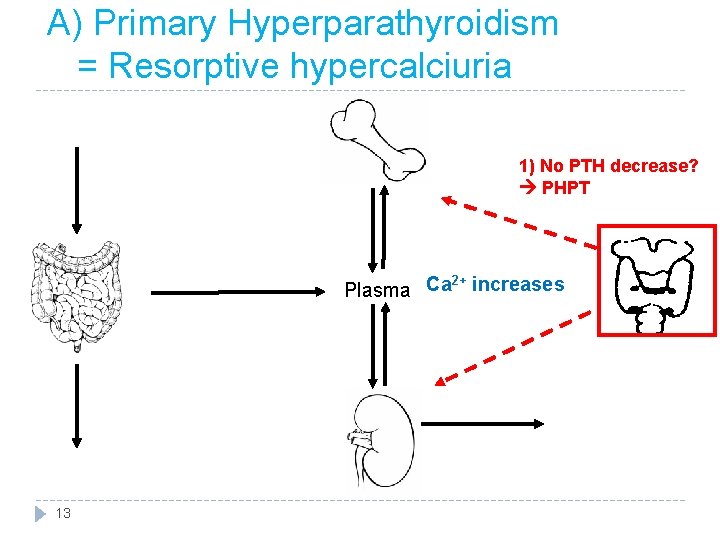
A) Primary Hyperparathyroidism = Resorptive hypercalciuria 1) No PTH decrease? PHPT 2+ Plasma Ca increases 13
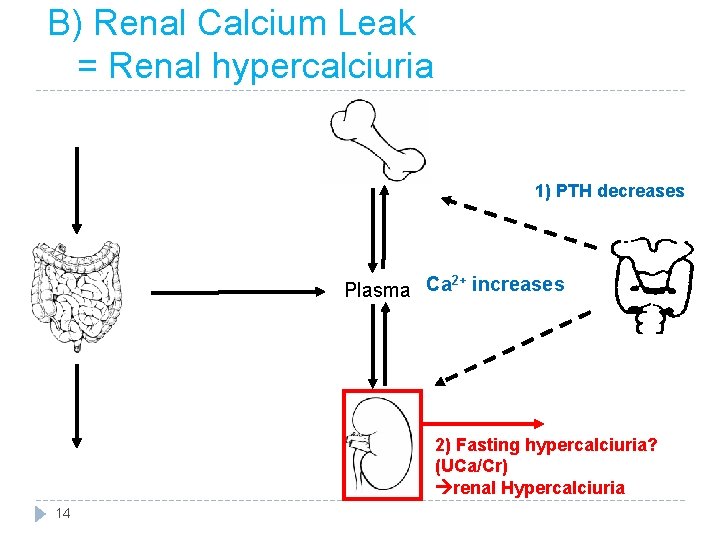
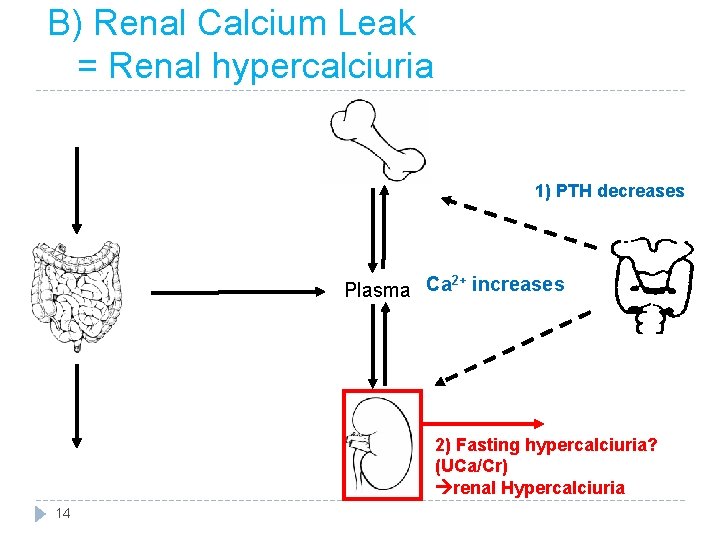
B) Renal Calcium Leak = Renal hypercalciuria 1) PTH decreases 2+ Plasma Ca increases 2) Fasting hypercalciuria? (UCa/Cr) renal Hypercalciuria 14
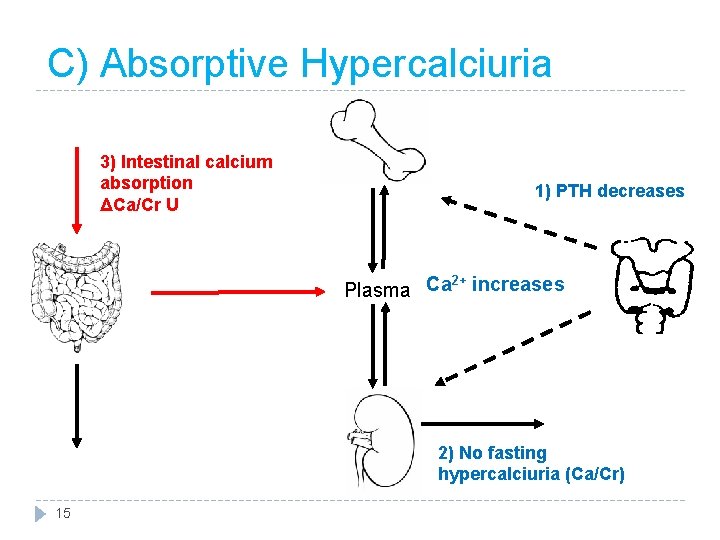
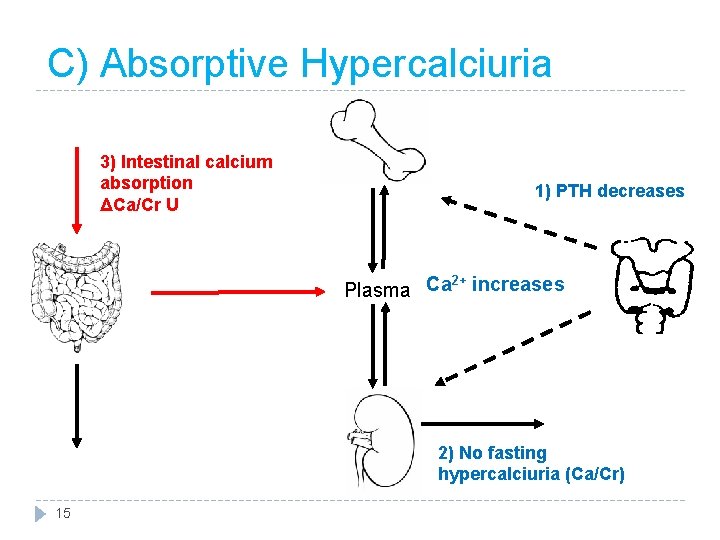
C) Absorptive Hypercalciuria 3) Intestinal calcium absorption ΔCa/Cr U 1) PTH decreases 2+ Plasma Ca increases 2) No fasting hypercalciuria (Ca/Cr) 15
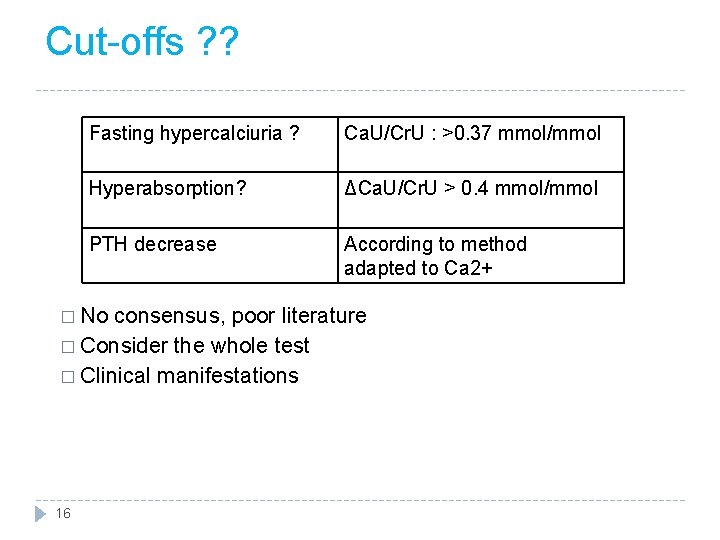
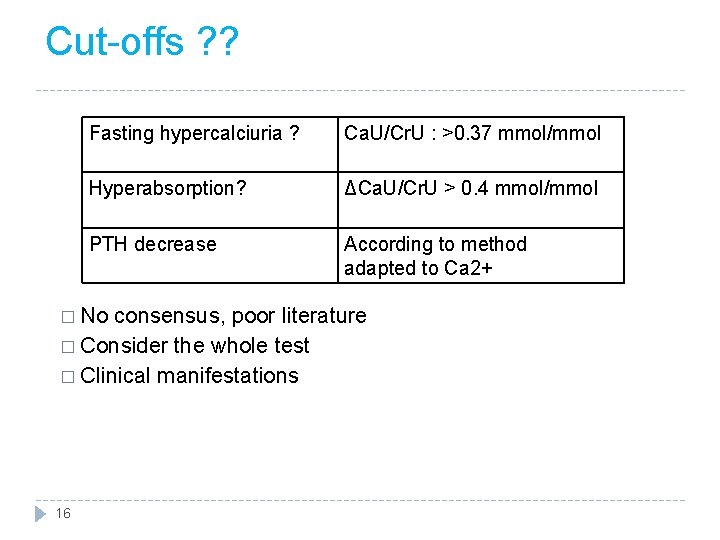
Cut-offs ? ? Fasting hypercalciuria ? Ca. U/Cr. U : >0. 37 mmol/mmol Hyperabsorption? ΔCa. U/Cr. U > 0. 4 mmol/mmol PTH decrease According to method adapted to Ca 2+ � No consensus, poor literature � Consider the whole test � Clinical manifestations 16
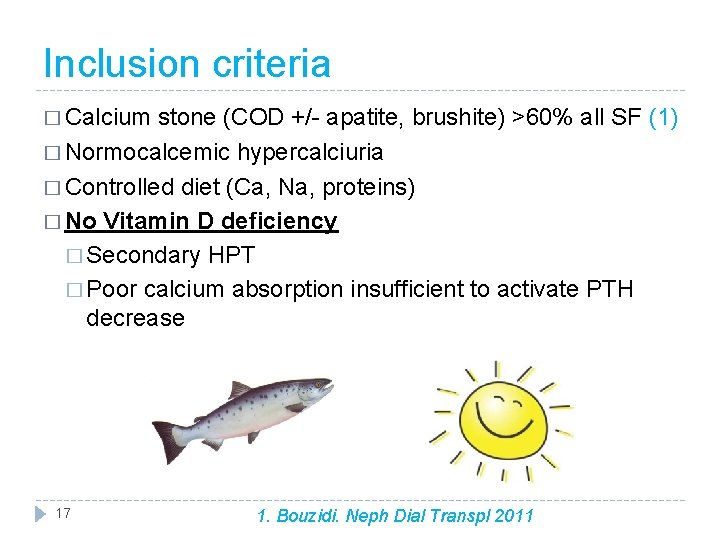
Inclusion criteria � Calcium stone (COD +/- apatite, brushite) >60% all SF (1) � Normocalcemic hypercalciuria � Controlled diet (Ca, Na, proteins) � No Vitamin D deficiency � Secondary HPT � Poor calcium absorption insufficient to activate PTH decrease 17 1. Bouzidi. Neph Dial Transpl 2011
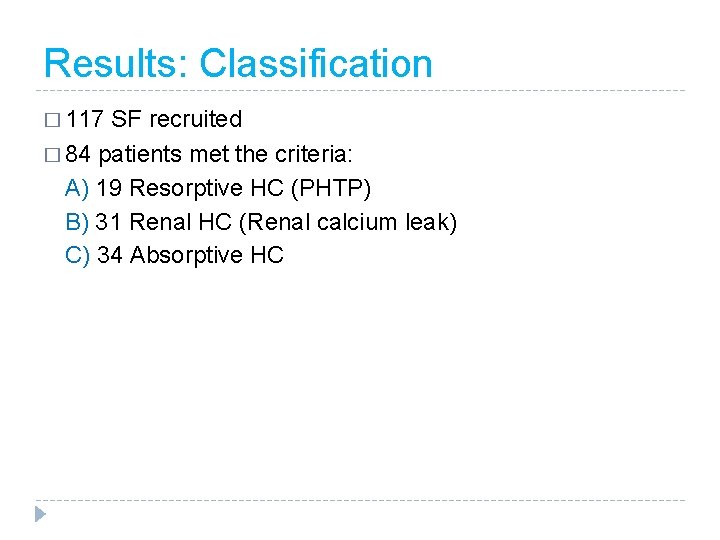
Results: Classification � 117 SF recruited � 84 patients met the criteria: A) 19 Resorptive HC (PHTP) B) 31 Renal HC (Renal calcium leak) C) 34 Absorptive HC
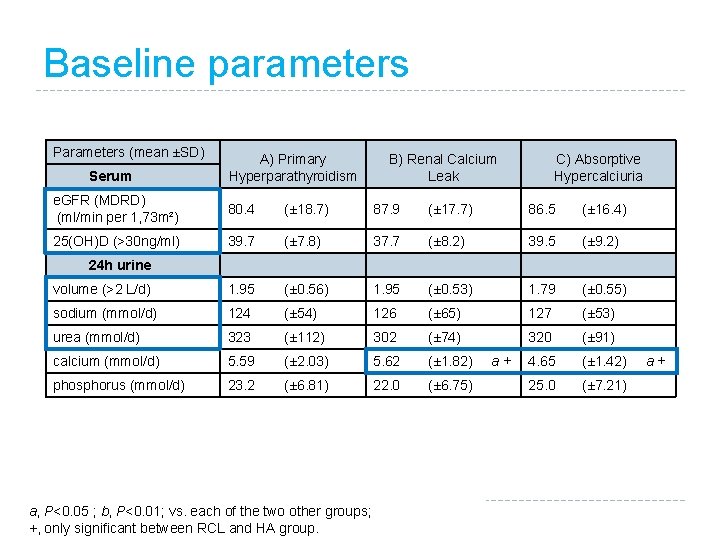
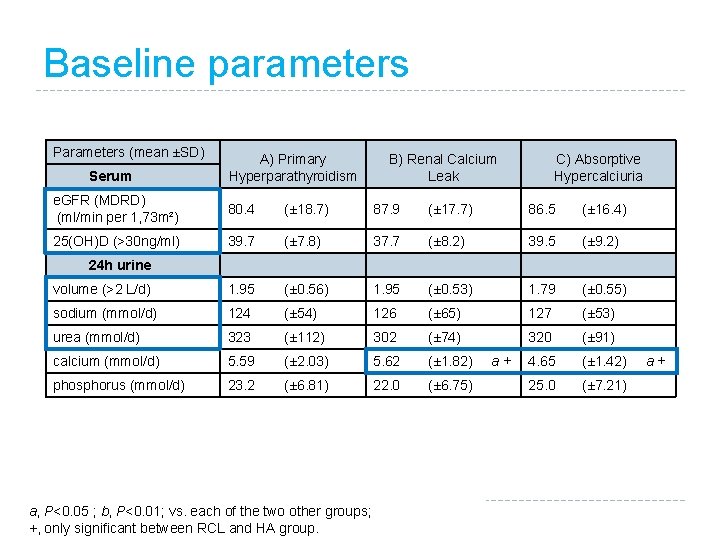
Baseline parameters Parameters (mean ±SD) Serum A) Primary Hyperparathyroidism B) Renal Calcium Leak C) Absorptive Hypercalciuria e. GFR (MDRD) (ml/min per 1, 73 m²) 80. 4 (± 18. 7) 87. 9 (± 17. 7) 86. 5 (± 16. 4) 25(OH)D (>30 ng/ml) 39. 7 (± 7. 8) 37. 7 (± 8. 2) 39. 5 (± 9. 2) volume (>2 L/d) 1. 95 (± 0. 56) 1. 95 (± 0. 53) 1. 79 (± 0. 55) sodium (mmol/d) 124 (± 54) 126 (± 65) 127 (± 53) urea (mmol/d) 323 (± 112) 302 (± 74) 320 (± 91) calcium (mmol/d) 5. 59 (± 2. 03) 5. 62 (± 1. 82) 4. 65 (± 1. 42) phosphorus (mmol/d) 23. 2 (± 6. 81) 22. 0 (± 6. 75) 25. 0 (± 7. 21) 24 h urine a, P<0. 05 ; b, P<0. 01; vs. each of the two other groups; +, only significant between RCL and HA group. a +
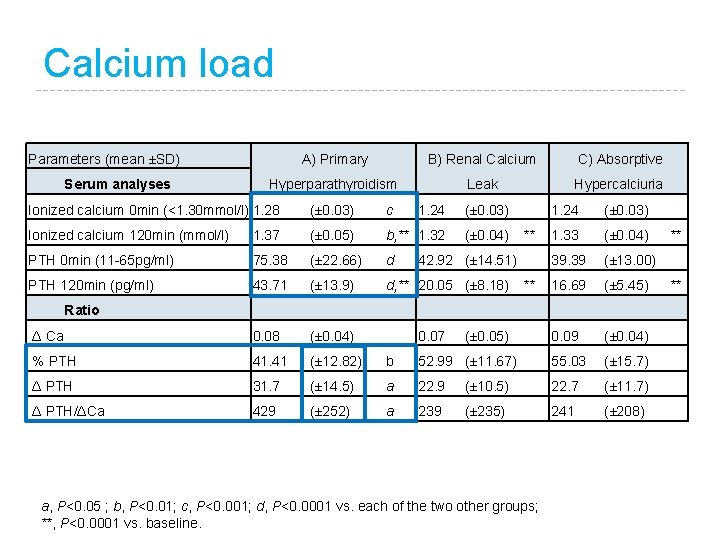
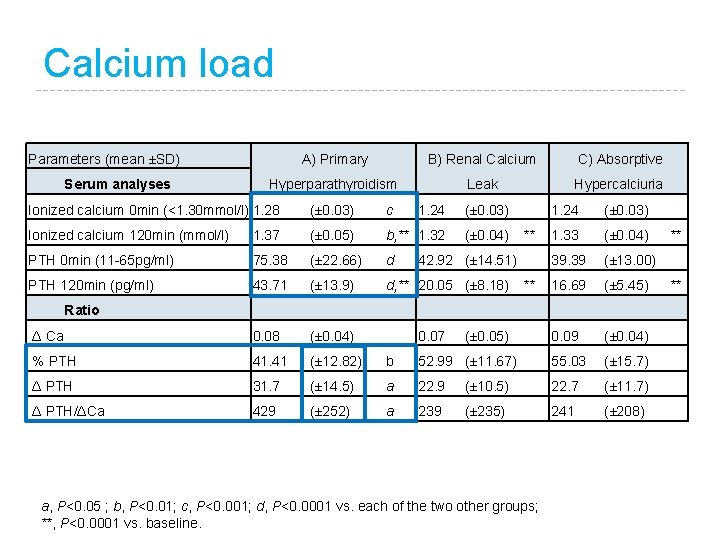
Calcium load Parameters (mean ±SD) Serum analyses A) Primary B) Renal Calcium C) Absorptive Hyperparathyroidism Leak Hypercalciuria Ionized calcium 0 min (<1. 30 mmol/l) 1. 28 (± 0. 03) c 1. 24 (± 0. 03) Ionized calcium 120 min (mmol/l) 1. 37 (± 0. 05) b, ** 1. 32 (± 0. 04) 1. 33 (± 0. 04) PTH 0 min (11 -65 pg/ml) 75. 38 (± 22. 66) d 39. 39 (± 13. 00) PTH 120 min (pg/ml) 43. 71 (± 13. 9) d, ** 20. 05 (± 8. 18) 16. 69 (± 5. 45) Δ Ca 0. 08 (± 0. 04) 0. 09 (± 0. 04) % PTH 41. 41 (± 12. 82) b 52. 99 (± 11. 67) 55. 03 (± 15. 7) Δ PTH 31. 7 (± 14. 5) a 22. 9 (± 10. 5) 22. 7 (± 11. 7) Δ PTH/ΔCa 429 (± 252) a 239 (± 235) 241 (± 208) ** 42. 92 (± 14. 51) ** Ratio 0. 07 (± 0. 05) a, P<0. 05 ; b, P<0. 01; c, P<0. 001; d, P<0. 0001 vs. each of the two other groups; **, P<0. 0001 vs. baseline. ** **
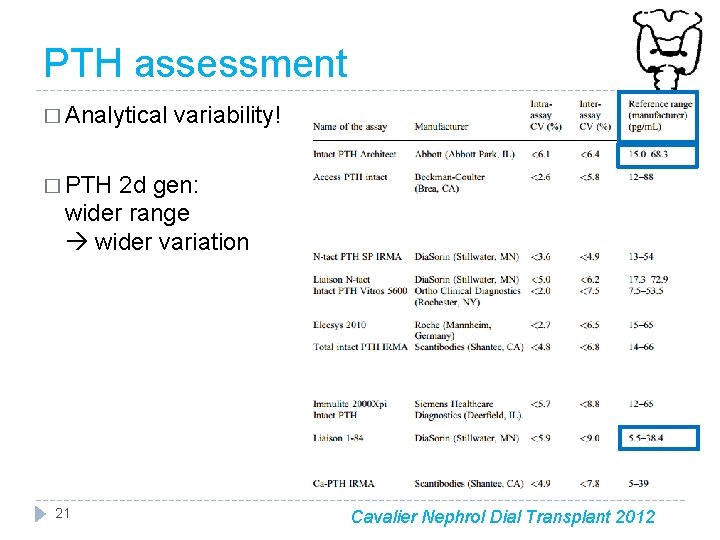
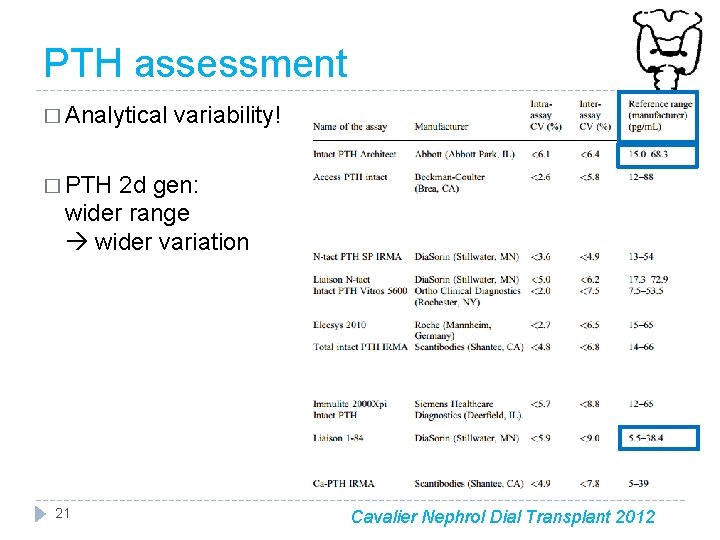
PTH assessment � Analytical variability! � PTH 2 d gen: wider range wider variation 21 Cavalier Nephrol Dial Transplant 2012
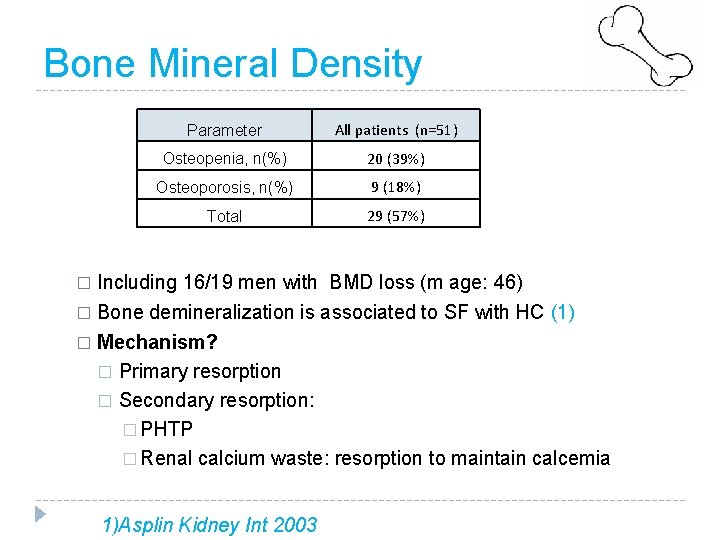
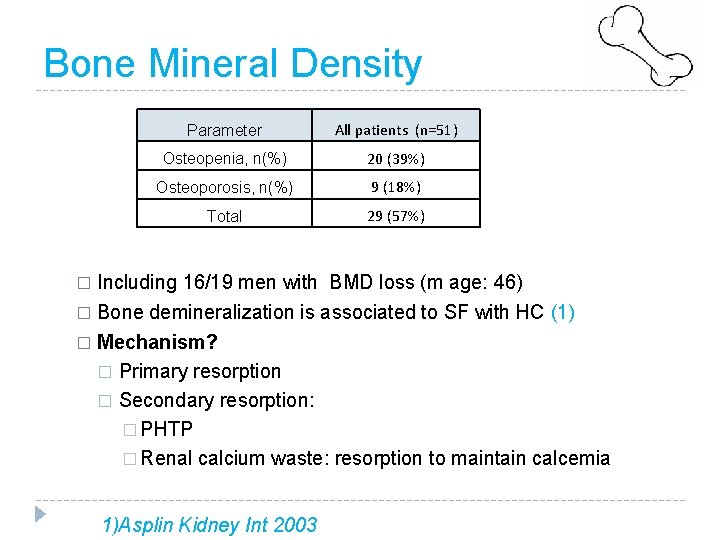
Bone Mineral Density Parameter All patients (n=51) Osteopenia, n(%) 20 (39%) Osteoporosis, n(%) 9 (18%) Total 29 (57%) Including 16/19 men with BMD loss (m age: 46) � Bone demineralization is associated to SF with HC (1) � � Mechanism? � Primary resorption � Secondary resorption: � PHTP � Renal calcium waste: resorption to maintain calcemia 1)Asplin Kidney Int 2003
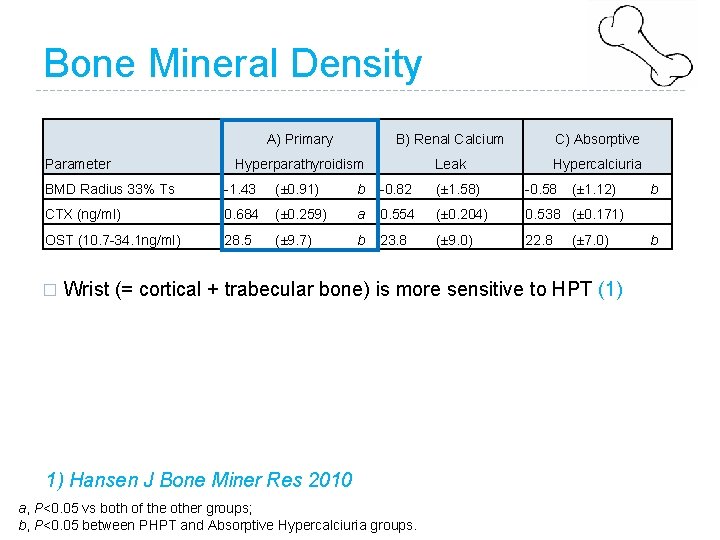
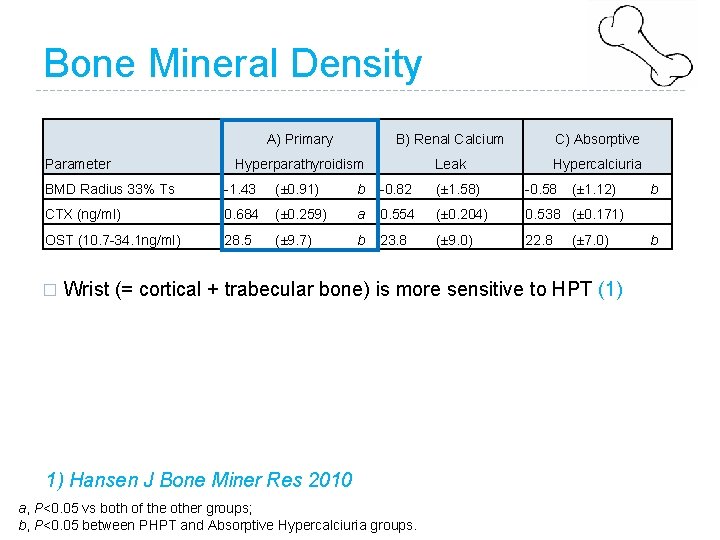
Bone Mineral Density Parameter A) Primary B) Renal Calcium C) Absorptive Hyperparathyroidism Leak Hypercalciuria BMD Radius 33% Ts -1. 43 (± 0. 91) b -0. 82 (± 1. 58) -0. 58 CTX (ng/ml) 0. 684 (± 0. 259) a 0. 554 (± 0. 204) 0. 538 (± 0. 171) OST (10. 7 -34. 1 ng/ml) 28. 5 (± 9. 7) b 23. 8 (± 9. 0) 22. 8 � (± 1. 12) (± 7. 0) Wrist (= cortical + trabecular bone) is more sensitive to HPT (1) 1) Hansen J Bone Miner Res 2010 a, P<0. 05 vs both of the other groups; b, P<0. 05 between PHPT and Absorptive Hypercalciuria groups. b b
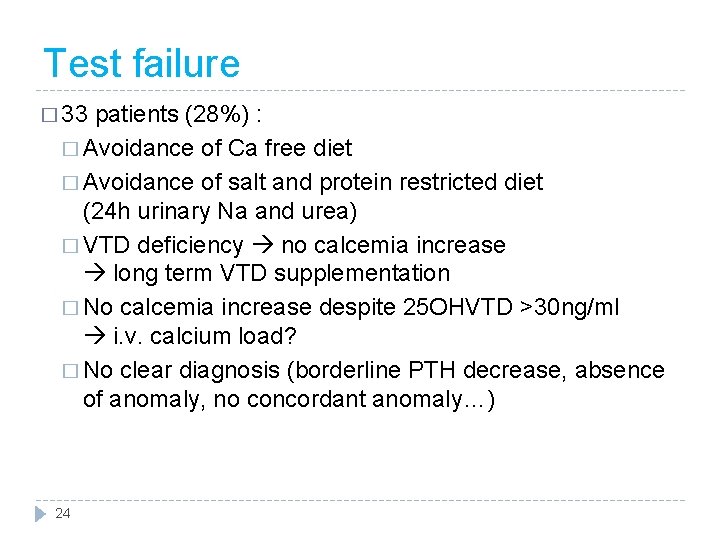
Test failure � 33 patients (28%) : � Avoidance of Ca free diet � Avoidance of salt and protein restricted diet (24 h urinary Na and urea) � VTD deficiency no calcemia increase long term VTD supplementation � No calcemia increase despite 25 OHVTD >30 ng/ml i. v. calcium load? � No clear diagnosis (borderline PTH decrease, absence of anomaly, no concordant anomaly…) 24
Conclusions � The set up and interpretation of the test requires preparation � The oral calcium load test is useful to � Determine the origin of hypercalciuria in stone-formers � Diagnose normocalcemic hyperparathyroidism �Select adapted treatment � Ionized calcium is mandatory to PTH interpretation � PTH ratios are of limited use � High prevalence of Bone Mineral Density loss in recurrent calcium stone-formers, men included 25

Thank you for your attention Thank you: Rana Alkouri Laurence Pieroni Monique Leban Rachida Inaoui Marie-Paule Dousseaux Etienne Cavalier Isabelle Tostivint