Optimizing Stroke Treatment for Women Susan M Brown
Optimizing Stroke Treatment for Women Susan M. Brown, M. D. Coastal Neurology, Beaufort, S. C.
Goals • Teach your patients stroke recognition and aggressive treatment of symptoms • Stroke screening for risk factors • Treat stroke patients in pregnancy • Counsel patients regarding future stroke risk
Stroke Incidence in Women • In 1999, 102, 000 women died of stroke • Women have less strokes than men but higher mortality (60% vs 34%)
Stroke Warning Symptoms • Weakness, numbness or tingling on one side of the body • Confusion • Trouble speaking • Difficulty understanding speech • Loss of balance or coordination • Severe headache
Pattern Recognition Carotid Artery Symptoms • Partial loss of vision or complete blindness • Double vision • A gray shading or fogging within the field of vision

Pattern Recognition Anterior and Middle Cerebral Artery Strokes • ACA: Contralateral leg weakness, grasp reflex, urinary incontinence, perseveration, gait disorder • MCA: Left: Contralateral face and arm > leg, Broca’s aphasia Right: Contralateral face and arm with neglect
Pattern Recognition Vertebrobasilar Strokes • Crossed motor or sensory signs • Cerebellar signs – ataxia, vertigo, nausea • Cranial nerve deficits
Pattern Recognition Lacunar Syndromes • Pure motor or sensory symptoms involving face, arm, and leg • Represent smaller artery lipohyalinosis • Basal ganglia, thalamus, pons • Treated with ASA +/- Plavix
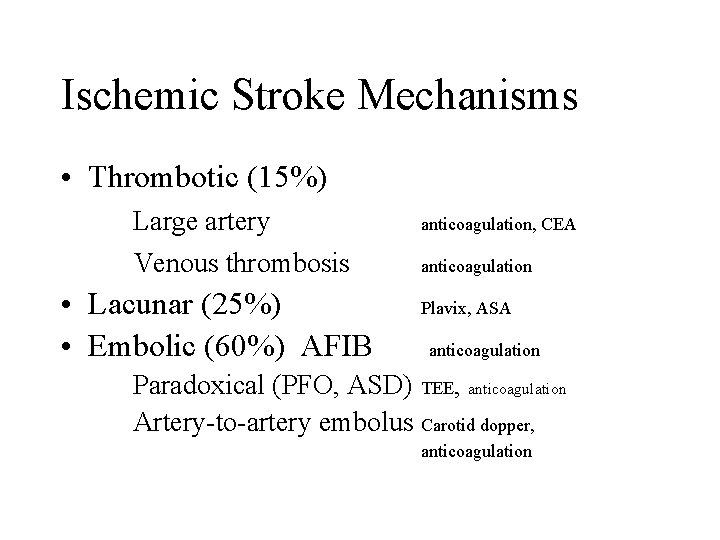
Ischemic Stroke Mechanisms • Thrombotic (15%) Large artery anticoagulation, CEA Venous thrombosis anticoagulation • Lacunar (25%) • Embolic (60%) AFIB Plavix, ASA anticoagulation Paradoxical (PFO, ASD) TEE, anticoagulation Artery-to-artery embolus Carotid dopper, anticoagulation
Ischemic Stroke Management • Keep systolic pressure 140 -200 or about 20 mm Hg higher than pt’s baseline • Avoid fever and high blood sugars • NPO until swallowing proved safe • Early PT/OT/Speech Therapy
Hemorrhagic Stroke • Intracranial hemorrhage (SAH, SDH, EDH) • Intracerebral hemorrhage • AVM – Arteriovenous malformation Raise HOB Drain hematomas Lower BP gently Shunt hydrocephalus Steroids, Mannitol, Hyperventilation Correct bleeding diathesis Control vasospasm
TPA Intravenous: • Giving TPA within 3 hours of onset uncertain conditions, improves outcome by 30 -34% over a 3 month interval. • Contraindicated with severe deficits or large vessel strokes • Giving TPA doubles the risk of intracerebral hemorrhage from stroke to 6 -8%
Intra-arterial TPA • Safer local delivery at the site of the clot 64% of lesions recanalize • 18% hemorrhage rate • Better for embolic than thrombotic lesions • More effective than heparin
Future Interventions • Neuroprotection during the stroke • Adjunct agents to enhance TPA • Stenting carotid arteries
Anticoagulation • • Chew ASA Plavix +/- ASA Aggrenox Heparin – cardioembolic, fresh thrombi or severe stenosis in large arteries – goal PTT 1. 5 – 2 times normal, rarely bolus • Coumadin – goal INR 2 - 3
Differential Diagnosis of Stroke • • Hypoglycemia Complicated migraine Seizure (Todd’s paralysis) Meningitis Multiple Sclerosis flare Bell’s palsy Spinal cord lesion Vasculitis
Prevention of Strokes • • Hypertension Cholesterol Statins Smoking/Alcohol Blood sugar/diet/exercise management Hyperhomocysteinemia fol/B 6/B 12 Migraine with aura + BCP + smoking Heart disease, diabetes, AFIB Family history
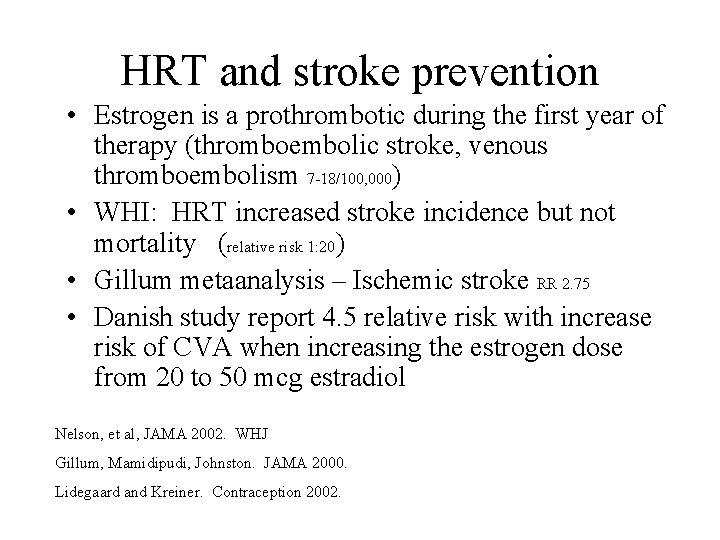
HRT and stroke prevention • Estrogen is a prothrombotic during the first year of therapy (thromboembolic stroke, venous thromboembolism 7 -18/100, 000) • WHI: HRT increased stroke incidence but not mortality (relative risk 1: 20) • Gillum metaanalysis – Ischemic stroke RR 2. 75 • Danish study report 4. 5 relative risk with increase risk of CVA when increasing the estrogen dose from 20 to 50 mcg estradiol Nelson, et al, JAMA 2002. WHJ Gillum, Mamidipudi, Johnston. JAMA 2000. Lidegaard and Kreiner. Contraception 2002.
HRT and Post Stroke Care • HRT does not improve mortality after stroke in postmenopausal women • HRT does not prevent a second stroke
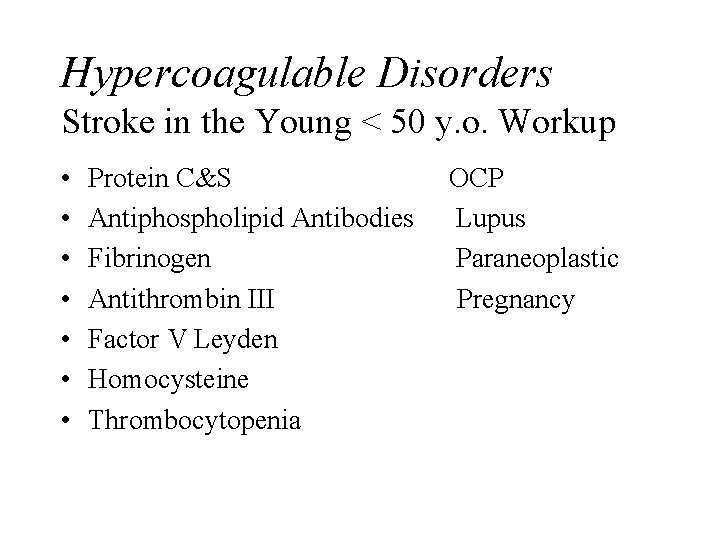
Hypercoagulable Disorders Stroke in the Young < 50 y. o. Workup • • Protein C&S Antiphospholipid Antibodies Fibrinogen Antithrombin III Factor V Leyden Homocysteine Thrombocytopenia OCP Lupus Paraneoplastic Pregnancy
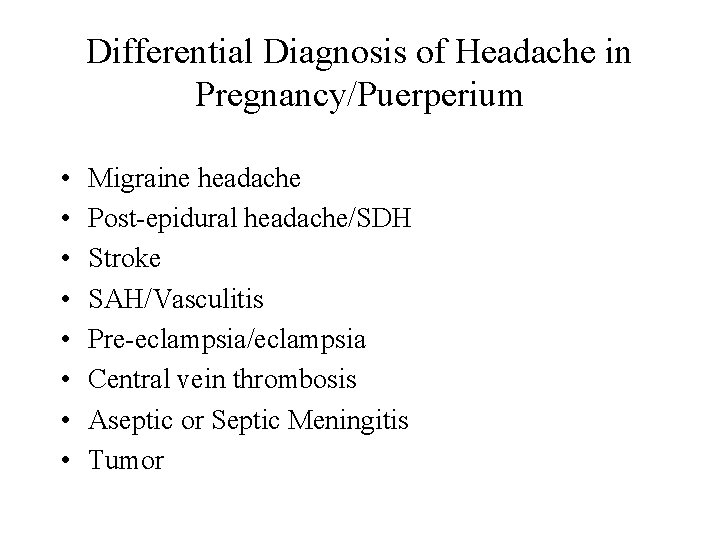
Differential Diagnosis of Headache in Pregnancy/Puerperium • • Migraine headache Post-epidural headache/SDH Stroke SAH/Vasculitis Pre-eclampsia/eclampsia Central vein thrombosis Aseptic or Septic Meningitis Tumor
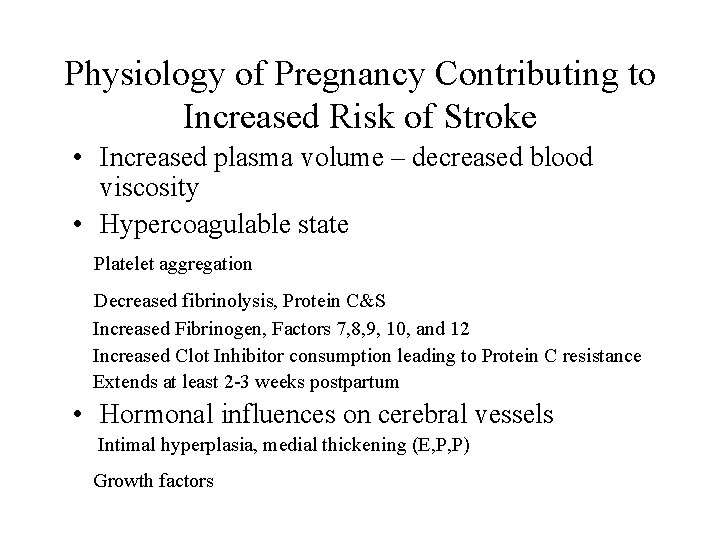
Physiology of Pregnancy Contributing to Increased Risk of Stroke • Increased plasma volume – decreased blood viscosity • Hypercoagulable state Platelet aggregation Decreased fibrinolysis, Protein C&S Increased Fibrinogen, Factors 7, 8, 9, 10, and 12 Increased Clot Inhibitor consumption leading to Protein C resistance Extends at least 2 -3 weeks postpartum • Hormonal influences on cerebral vessels Intimal hyperplasia, medial thickening (E, P, P) Growth factors
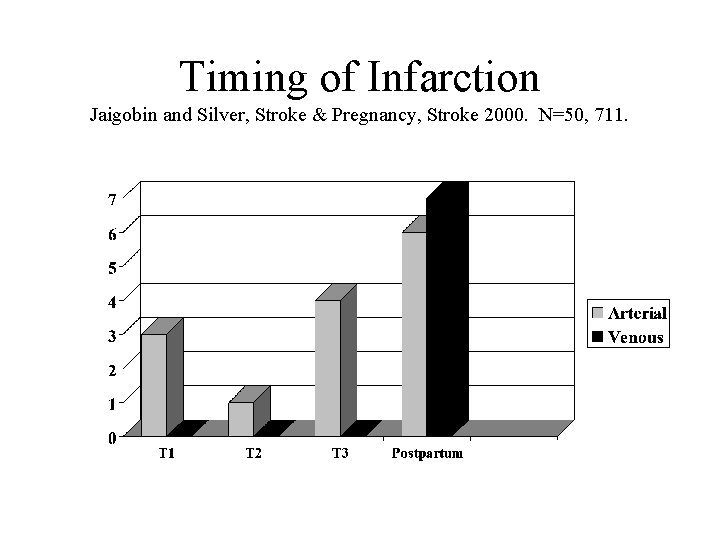
Timing of Infarction Jaigobin and Silver, Stroke & Pregnancy, Stroke 2000. N=50, 711.
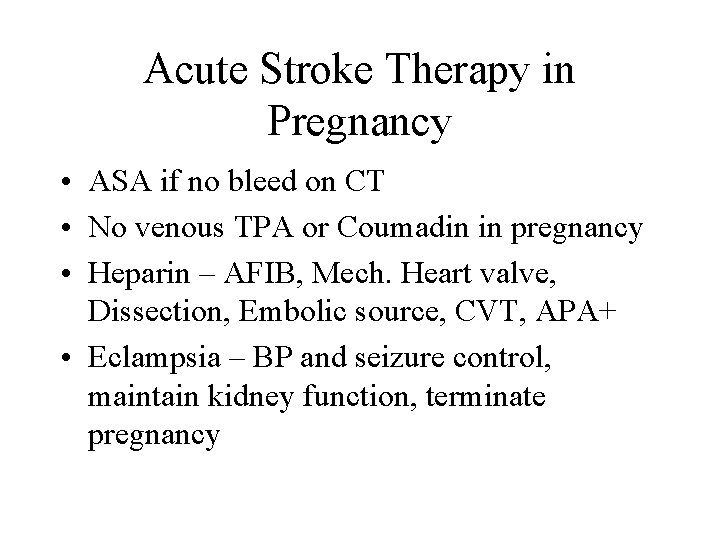
Acute Stroke Therapy in Pregnancy • ASA if no bleed on CT • No venous TPA or Coumadin in pregnancy • Heparin – AFIB, Mech. Heart valve, Dissection, Embolic source, CVT, APA+ • Eclampsia – BP and seizure control, maintain kidney function, terminate pregnancy
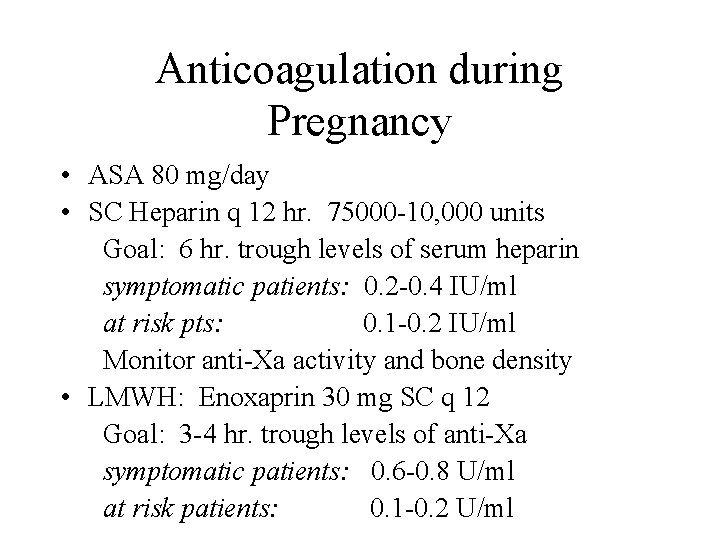
Anticoagulation during Pregnancy • ASA 80 mg/day • SC Heparin q 12 hr. 75000 -10, 000 units Goal: 6 hr. trough levels of serum heparin symptomatic patients: 0. 2 -0. 4 IU/ml at risk pts: 0. 1 -0. 2 IU/ml Monitor anti-Xa activity and bone density • LMWH: Enoxaprin 30 mg SC q 12 Goal: 3 -4 hr. trough levels of anti-Xa symptomatic patients: 0. 6 -0. 8 U/ml at risk patients: 0. 1 -0. 2 U/ml
Risk of Recurrent Ischemic Stroke Larry, Hamon, Cost, and Mas, Neurology 2000; 55: 269 -274. • A previous ischemic stroke is not a contraindication to subsequent pregnancy • Confirmed risk of stroke increased postpartum • 441 women (373 arterial ischemic; 68 with CVT) with 5 year follow-up • 13 arterial strokes recurred (11 outside pregnancy/2 in) • Overall risk 1% in 1 yr and 2. 3% in 5 yr • Outcome of subsequent pregnancies similar to general population except when additional risk factor identified
Does pregnancy increase the risk of bleeding from AVMs or Aneurysms? • AVMs: 3. 5 -85% • Wait until 1 year after AVM event before getting pregnant or until embolic therapy is completed • Vaginal delivery is not associated with increasing rate of bleed
Dias 1994 Aneurysms & AVMs • Higher incidence of bleeding from aneurysms • Incidence of hemorrhage is higher for in 2 nd and 3 rd trimesters • Maternal morbidity is higher for aneurysms (35%) vs. AVM (28%) …than in nongravid patients Dias and Sekhar, Neurosurgery 1990 N=154 ICH Aneurysms 77% and AVM 23%
Aneurysm Treatment Recommendations • Aneurysms: Surgical intervention during pregnancy reduces mortality Dias & Stoodley • Gestational age <26 weeks – treat aneurysm Symptomatic >26 wks – C-section or rapid vaginal delivery • Vaginal delivery and C-section are equally efficacious
Summary • Acute stroke should be investigated aggressively • Make proper diagnosis for proper treatment (BP management, surgery, heparin, ASA) • Patients want recommendations about future prevention and treatment choices
Summary, cont. • More descriptive information is available than treatment data (acute and prophylaxis) • Recommendations have become more open to vaginal delivery, recurrent pregnancy
- Slides: 31