Optimizing Radiation Treatment Planning for Tumors Using IMRT
- Slides: 27
Optimizing Radiation Treatment Planning for Tumors Using IMRT Laura D. Goadrich Industrial Engineering & Department of Computer Sciences at University of Wisconsin-Madison April 19, 2004
Overview n Radiotherapy motivation n n Mechanical constraints MIP method n n n Conformal radiotherapy IMRT Input/output Langer, et. al. Approach Monoshape constraints Implementation results References
Motivation n 1. 2 million new cases of cancer each year in U. S. (times 10 globally) Half undergo radiation therapy Some are treated with implants, but most with external beams obtained using radiotherapy treatments.
Radiotherapy Motivation n Used to fight many types of cancer in almost every part of the body Approximately 40% of patients with cancer needs radiation therapy sometime during the course of their disease Over half of those patients who receive radiotherapy are treated with an aim to cure the patient n n n to treat malignancies to shrink the tumor or to provide temporary relief of symptoms In the use of radiation, organ and function preservation are important aims (minimize risk to organs at risk (OAR)).
Planning Radiotherapy. CAT scan n n Conduct scans of the section of the body containing the tumor Allows physicians to see the OAR and surrounding bodily structures
Planning Radiotherapytumor volume contouring n n Isolating the tumor from the surrounding OAR is vital to ensure the patient receives minimal damage from the radiotherapy Identifying the dimensions of the tumor is vital to creating the intensity maps (identifying where to focus the radiation)
Planning Radiotherapybeam angles and creating intensity maps n n Multiple angles are used to create a full treatment plan to treat one tumor. Through a sequence of leaf movements, intensity maps are obtained
Option 1: Conformal Radiotherapy n n The beam of radiation used in treatment is a 10 cm square. Utilizes a uniform beam of radiation n n ensures the target is adequately covered however does nothing to avoid critical structures except usage of some blocks
Option 2: IMRT n n n Intensity Modulated Radiotherapy (IMRT) provides a shaped array of 3 mm beamlets using a Multi-Leaf Collimator (MLC), which is a specialized, computer-controlled device with many tungsten fingers, or leaves, inside the linear accelerator. Allows a finer shaped distribution of the dose to avoid unsustainable damage to the surrounding structures (OARs) Implemented via a Multi-Leaf Collimator (MLC) creating a timevarying opening (leaves can be vertical or horizontal).
Classical vs. IMRT
IMRT machine
IMRT: Planning- intensity map n There is an intensity map for each angle n n 0 means no radiation 100 means maximum dosage of radiation Multiple beam angles spread a healthy dose A collection of shape matrices are created to satisfy each intensity map.
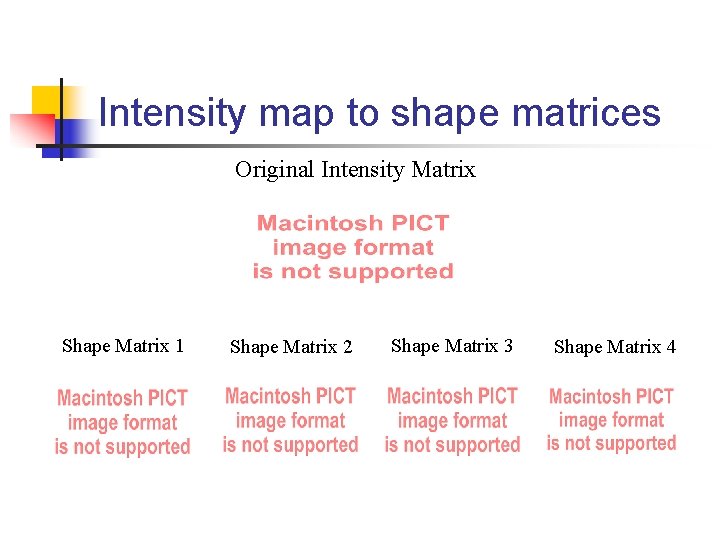
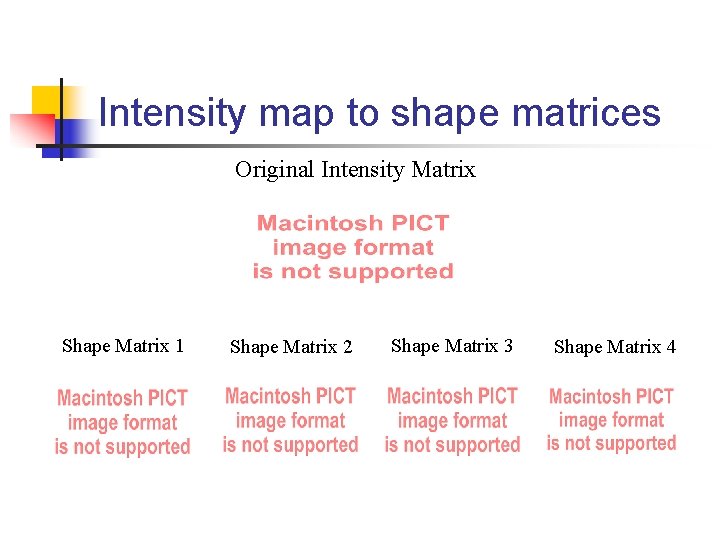
Intensity map to shape matrices Original Intensity Matrix Shape Matrix 1 Shape Matrix 2 Shape Matrix 3 Shape Matrix 4
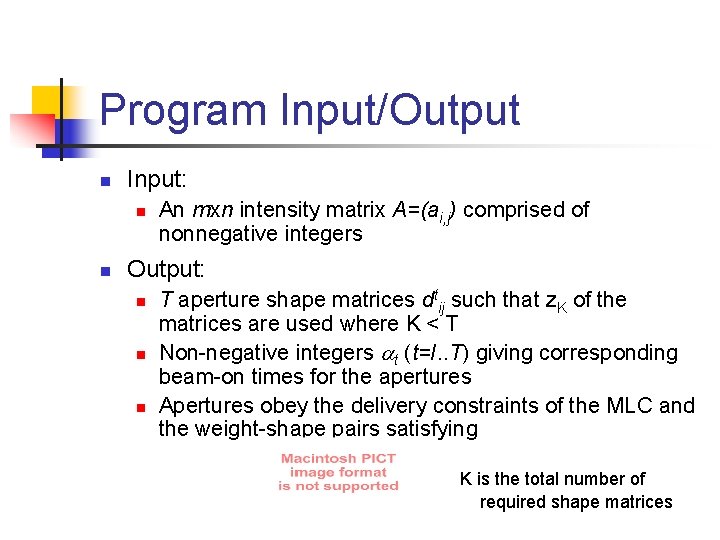
Program Input/Output n Input: n n An mxn intensity matrix A=(ai, j) comprised of nonnegative integers Output: n n n T aperture shape matrices dtij such that z. K of the matrices are used where K < T Non-negative integers t (t=I. . T) giving corresponding beam-on times for the apertures Apertures obey the delivery constraints of the MLC and the weight-shape pairs satisfying K is the total number of required shape matrices
Mechanical Constraints n n n After receiving the intensity maps, machine specific shape matrices must be created for treatment There are numerous types of IMRT machines currently in clinical use, with slightly different physical constraints that determine the leaf positions (hence the shape matrices) possible for the device Each machine has varying setup times which can dominate the radiation delivery time (beam-on time) To limit patient discomfort and subtle movement from initial placing: limit the time the patient is on the table Goals: n n Minimize beam-on time Minimize number of different shapes
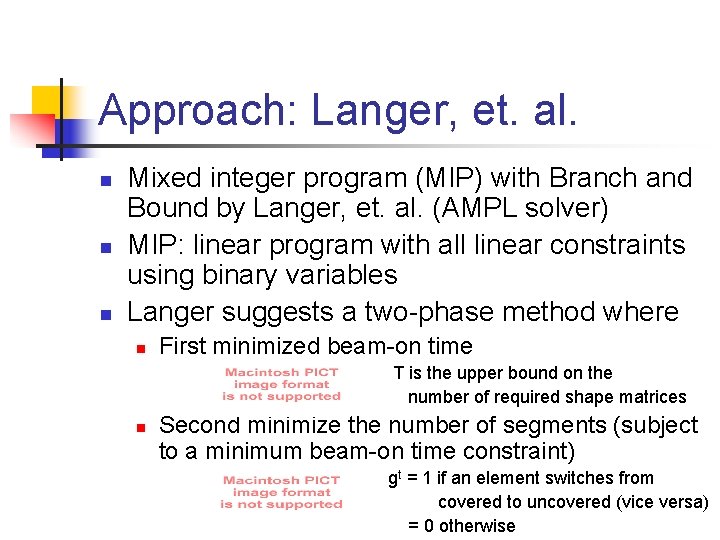
Approach: Langer, et. al. n n n Mixed integer program (MIP) with Branch and Bound by Langer, et. al. (AMPL solver) MIP: linear program with all linear constraints using binary variables Langer suggests a two-phase method where n First minimized beam-on time T is the upper bound on the number of required shape matrices n Second minimize the number of segments (subject to a minimum beam-on time constraint) gt = 1 if an element switches from covered to uncovered (vice versa) = 0 otherwise
In Practice n n While Langer, et. al. reports that solving both minimizations takes a reasonable amount of time, he does not report numbers and we have found that the time demands are impractical for real application. To obtain a balance between the need for a small number of shape matrices and a low beam-on time we have found that num. Shape. Matricies*7 + beam-on time n Initializing T close to the optimal number of matrices + 1 required reduces the solution space and solution time
Constraint: Leaves cannot overlap from right and left n To satisfy the requirement that leaves of a row cannot override each other implies that one beam element cannot be covered by the left and right leaf at the same time ptij= 1 if beam element in row i, column j is covered by the right leaf when the tth monitor unit is delivered = 0 otherwise ltij is similar for the right leaf dtij contains the final tth monitor unit
Constraint: Full leaves and intensity matrix requirements n Every element between the leaf and the side of the collimator to which the leaf is connected is also covered (no holes in leaves).
Constraint: No leaf collisions n Due to mechanical requirements, leaves can move in only one direction (i. e. the right leaf to the right). On one row, the right and left leaves cannot overlap
Constraint: Shape matrices reqs n The total number of shape matrices expended it tallied z= 1 when at least one beam element reamins exposed when the tth monitor unit in the sequence is delivered = 0 otherwise I is the number of rows J is the number of columns n Must satisfy the intensity matrix for each monitor unit. I is the intensity assigned to beam element ij
Constraint: Monoshape n n The IMRT delivery is required to contain only one shape matrix per monitor unit, a monoshape First determine which rows in each monitor unit are open to deliver radiation deliveryit=1 if the ith row is being used a time t = 0 otherwise n Determine if the preceding row in the monitor unit delivers radiation dropit=1 if the preceding row (i-1) in a shape is non-zero and the current row (i) is 0 = 0 otherwise
Constraint: Monoshape n Determine when the monoshape ends jumpit=1 if the preceding row (i-1) in a shape is zero and the current row (i) is nonzero = 0 otherwise n There can be only one row where the monoshape begins and one row to end
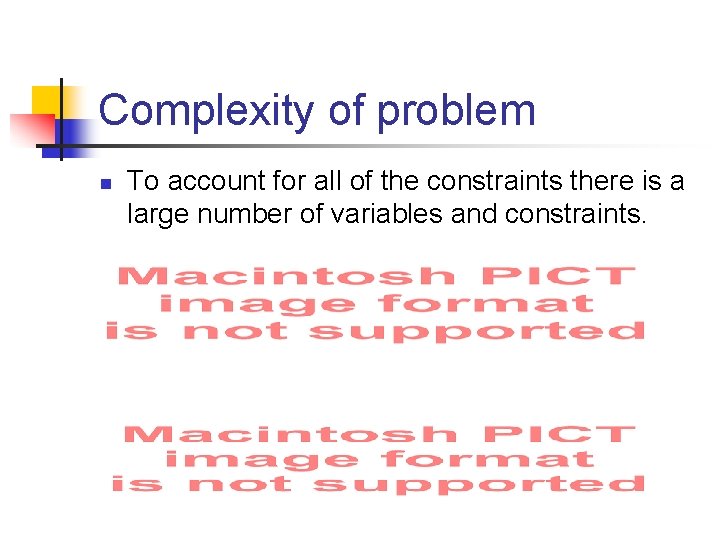
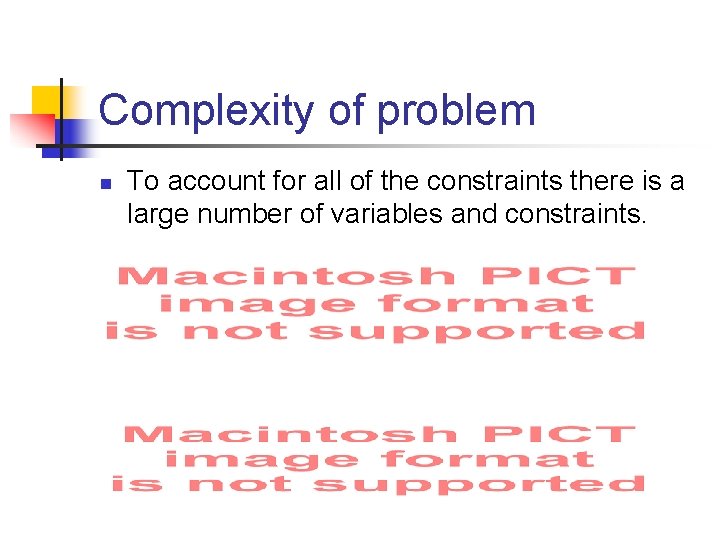
Complexity of problem n To account for all of the constraints there is a large number of variables and constraints.
Comparison of results n Corvus version 4. 0
Comparison of results n Corvus version 5. 0
Referenced Papers n n n N. Boland, H. W. Hamacher, and F. Lenzen. “Minimizing beam-on time in cancer radiation treatment using multileaf collimators. ” Neworks, 2002. Mark Langer, Van Thai, and Lech Papiez, “Improved leaf sequencing reduces segments or monitor units needed to deliver IMRT using multileaf collimators, ” Medical Physics, 28(12), 2001. Ping Xia, Lynn J. Verhey, “Multileaf collimator leaf sequencing algorithm for intensity modulated beams with multiple static segments, ” Med. Phys. 25 (8), 1998. T. R. Bortfield, D. L. Kahler, T. J Waldron and A. L. Boyer, X-ray field compensation with multileaf collimators. Int. J. Radiat. Oncol. Biol. 28 (1994), pp. 723 -730. Bortfield, Thomas, et. al. “Current IMRT optimization algorithms: principles, potential and limitations” Presentation 2000. Dink, Delal, S. Orcun, M. P. Langer, J. F. Pekny, G. V. Reklaitis, R. L. Rardin, “Importance of sensitivity analysis in intensity modulated radiation therapy (IMRT)” 2003.