Optimizing Pediatric Spine MRI Protocols Tips Tricks and
- Slides: 39
Optimizing Pediatric Spine MRI Protocols: Tips, Tricks, and Rationales Ryan Tade, MS, MD Falgun H. Chokshi, MS, MD Nadja Kadom, MD Emory University School of Medicine – Radiology & Imaging Sciences, Atlanta, GA e. Ed. E-211
Disclosures: • Nadja Kadom MD – No disclosures • Falgun H. Chokshi, MD, MS, DABR – No disclosures • Ryan Tade, MS, MD – No disclosures
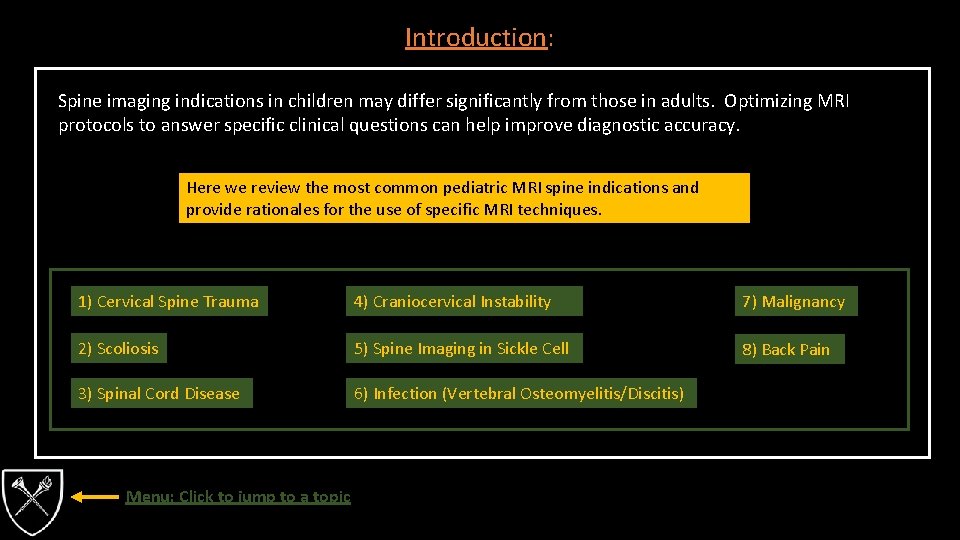
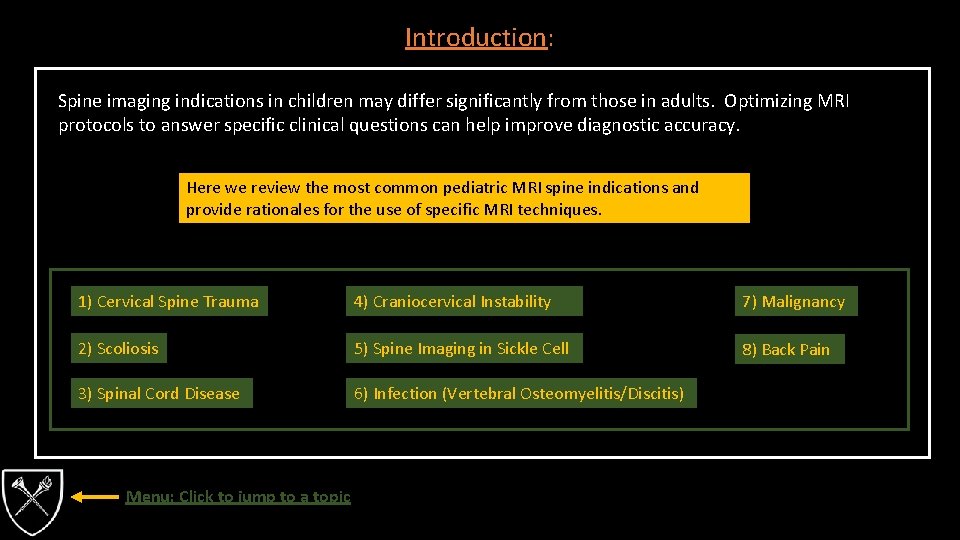
Introduction: Spine imaging indications in children may differ significantly from those in adults. Optimizing MRI protocols to answer specific clinical questions can help improve diagnostic accuracy. Here we review the most common pediatric MRI spine indications and provide rationales for the use of specific MRI techniques. 1) Cervical Spine Trauma 4) Craniocervical Instability 7) Malignancy 2) Scoliosis 5) Spine Imaging in Sickle Cell 8) Back Pain 3) Spinal Cord Disease 6) Infection (Vertebral Osteomyelitis/Discitis) Menu: Click to jump to a topic
1. Cervical Spine Trauma (1/7) • Cervical spine injuries occur only in 1 -3% of pediatric trauma patients. • Higher incidence of neurologic deficits in patients <8 years old, compared to older patients. • Mortality rate is higher in pediatric patients with cervical spine injury compared to adults. • Children <8 years old tend to injure the cervical spine at C 3 or higher. • Younger patients have increased mobility of the cervical spine secondary to underdeveloped spinal processes, horizontal orientation of the vertebral facets and ligamentous laxity. • Increased mobility in combination with increased head-to-body ratio and relatively weaker cervical musculature results in increased incidence of distracting injuries to the upper cervical spine. • Spinal cord injury without radiographic abnormalities (SCIWORA): • Incidence is estimated at 9 -34% of pediatric cervical spine injuries. • Increased laxity of the pediatric cervical spine in patients < 8 years old prevents fractures resulting from low-energy trauma, but increases the risk of SCIWORA. • Trauma that results in cord stretching and subsequent cord contusion, ischemia or rupture (hyperextension, hyperflexion or distracting injury).
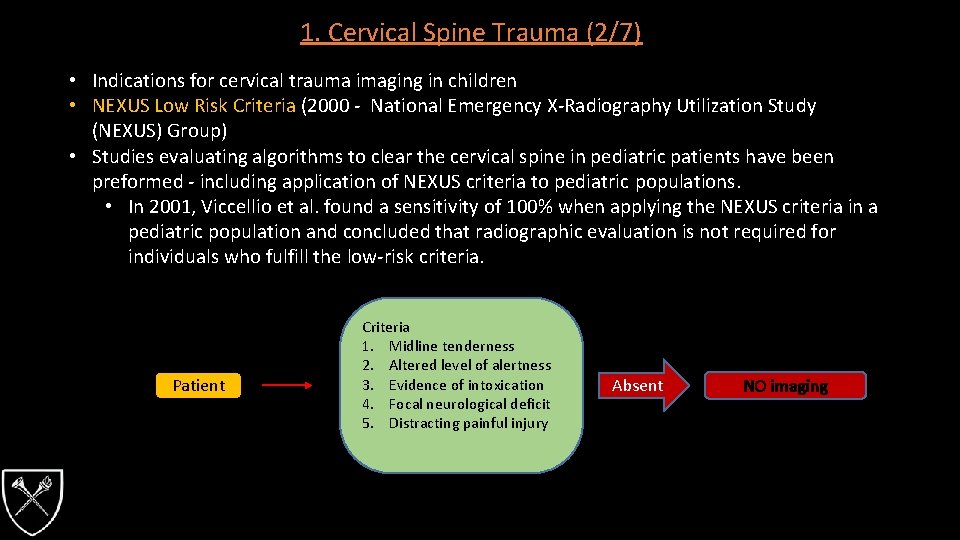
1. Cervical Spine Trauma (2/7) • Indications for cervical trauma imaging in children • NEXUS Low Risk Criteria (2000 - National Emergency X-Radiography Utilization Study (NEXUS) Group) • Studies evaluating algorithms to clear the cervical spine in pediatric patients have been preformed - including application of NEXUS criteria to pediatric populations. • In 2001, Viccellio et al. found a sensitivity of 100% when applying the NEXUS criteria in a pediatric population and concluded that radiographic evaluation is not required for individuals who fulfill the low-risk criteria. Patient Criteria 1. Midline tenderness 2. Altered level of alertness 3. Evidence of intoxication 4. Focal neurological deficit 5. Distracting painful injury Absent NO imaging
1. Cervical Spine Trauma (3/7) Cervical Spine Trauma - MRI Protocol • • • Sag T 1 Sag T 2 with fat saturation Sag DWI Ax T 1 Ax GRE (3 D) Rationale, Tips & Tricks • STIR (short-tau inversion recovery) is more reliable for determining extent of soft tissue injury, as STIR sequences allow for better fat suppression than other fat saturation techniques • DWI for detection of infarction/SCIWORA • GRE best for spinal cord lesions, such as SCIWORA • GRE for blood products in trauma
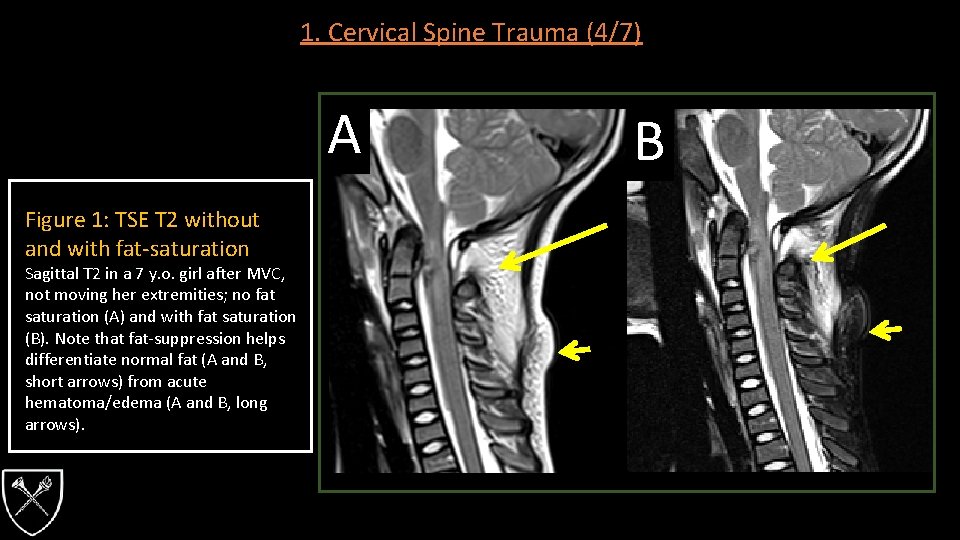
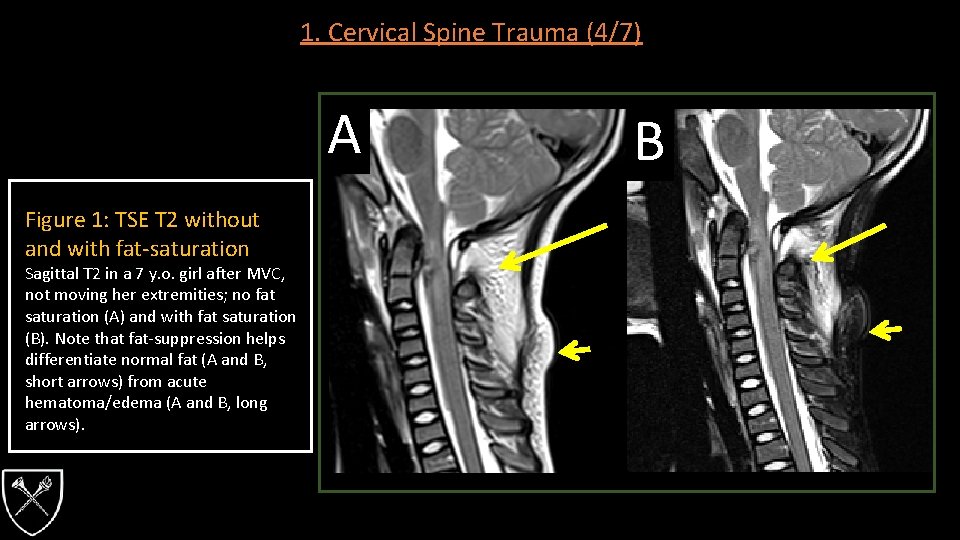
1. Cervical Spine Trauma (4/7) A Figure 1: TSE T 2 without and with fat-saturation Sagittal T 2 in a 7 y. o. girl after MVC, not moving her extremities; no fat saturation (A) and with fat saturation (B). Note that fat-suppression helps differentiate normal fat (A and B, short arrows) from acute hematoma/edema (A and B, long arrows). B
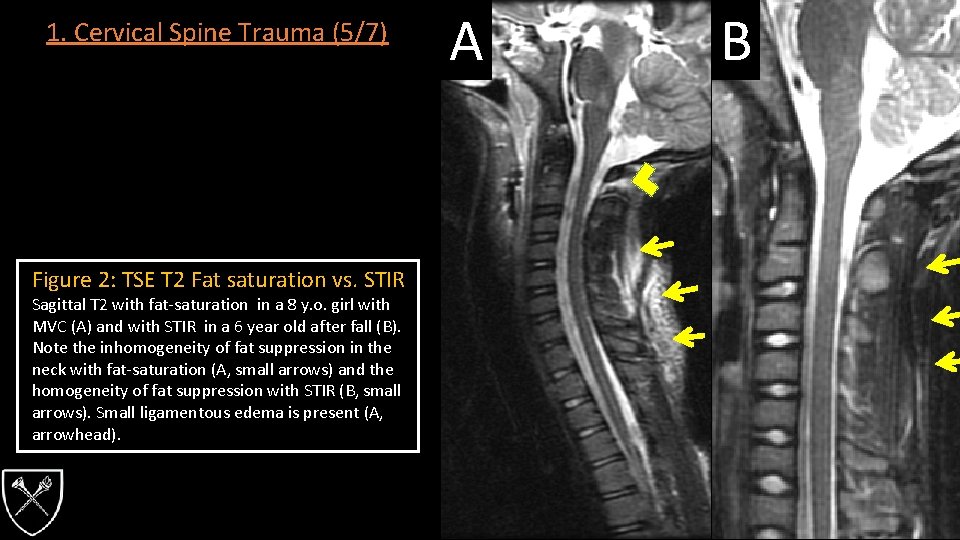
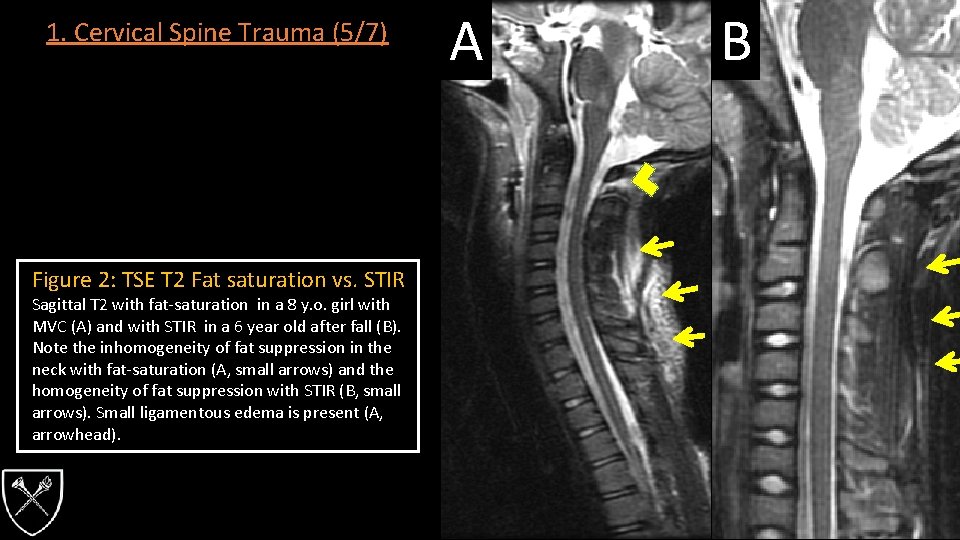
1. Cervical Spine Trauma (5/7) Figure 2: TSE T 2 Fat saturation vs. STIR Sagittal T 2 with fat-saturation in a 8 y. o. girl with MVC (A) and with STIR in a 6 year old after fall (B). Note the inhomogeneity of fat suppression in the neck with fat-saturation (A, small arrows) and the homogeneity of fat suppression with STIR (B, small arrows). Small ligamentous edema is present (A, arrowhead). A B
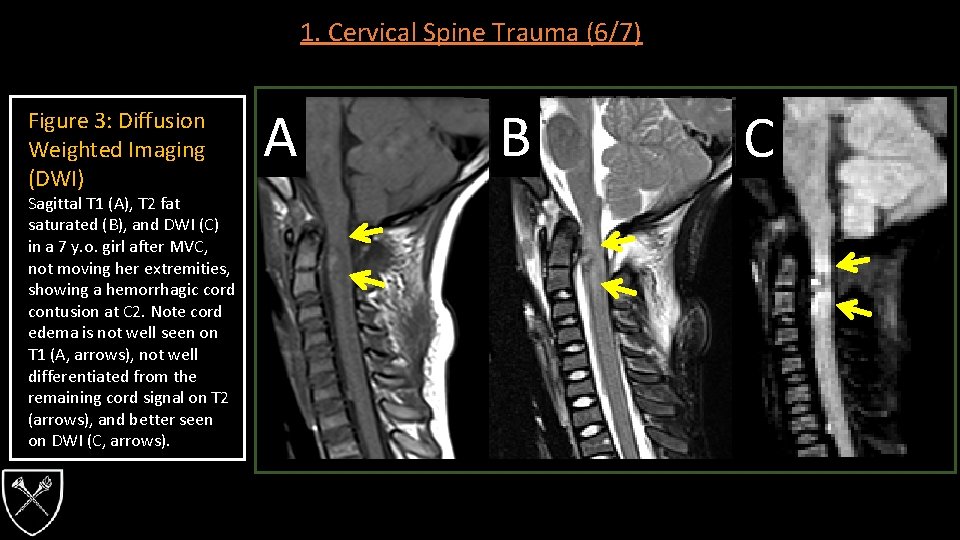
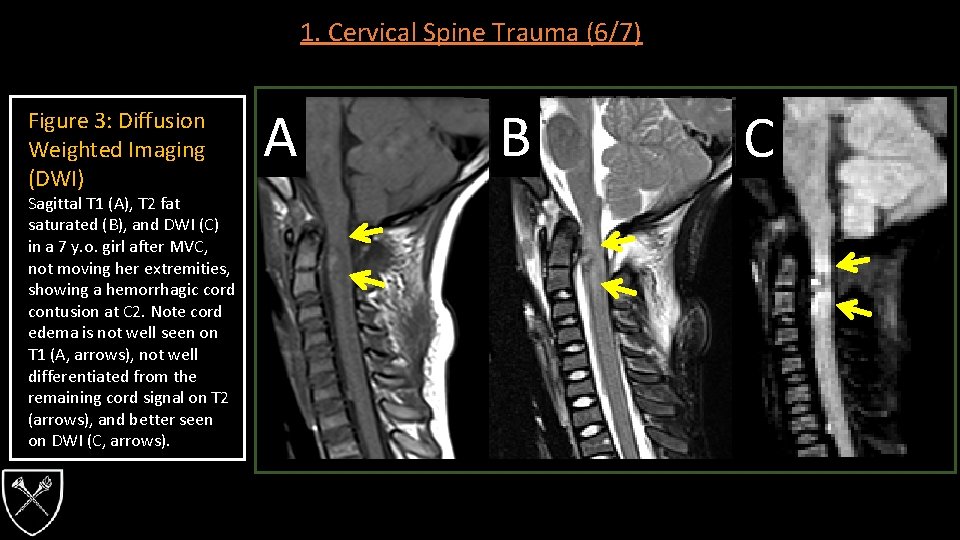
1. Cervical Spine Trauma (6/7) Figure 3: Diffusion Weighted Imaging (DWI) Sagittal T 1 (A), T 2 fat saturated (B), and DWI (C) in a 7 y. o. girl after MVC, not moving her extremities, showing a hemorrhagic cord contusion at C 2. Note cord edema is not well seen on T 1 (A, arrows), not well differentiated from the remaining cord signal on T 2 (arrows), and better seen on DWI (C, arrows). A B C
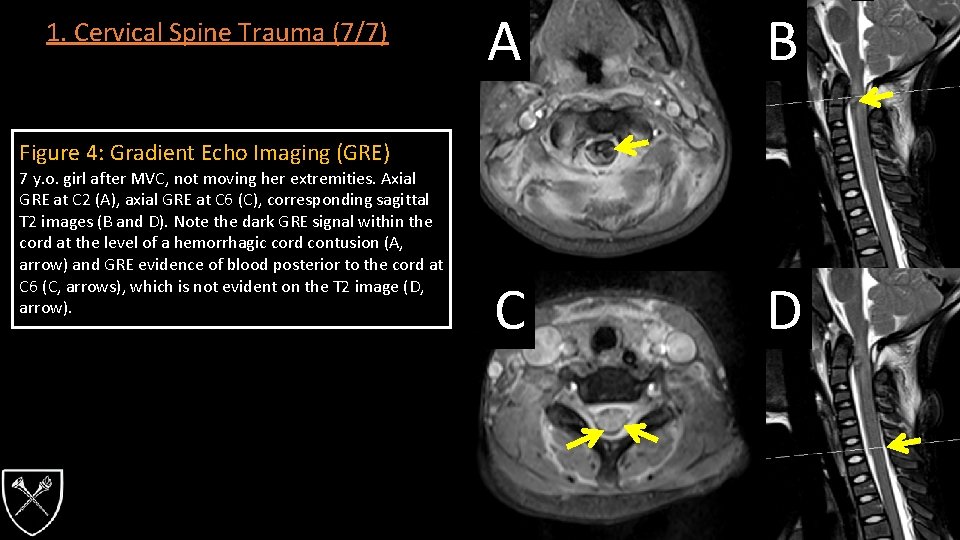
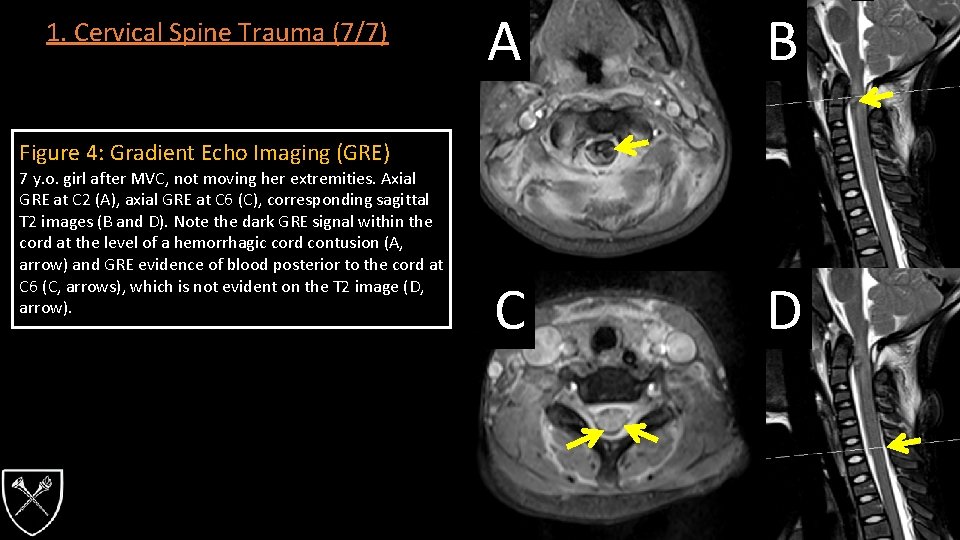
1. Cervical Spine Trauma (7/7) A B C D Figure 4: Gradient Echo Imaging (GRE) 7 y. o. girl after MVC, not moving her extremities. Axial GRE at C 2 (A), axial GRE at C 6 (C), corresponding sagittal T 2 images (B and D). Note the dark GRE signal within the cord at the level of a hemorrhagic cord contusion (A, arrow) and GRE evidence of blood posterior to the cord at C 6 (C, arrows), which is not evident on the T 2 image (D, arrow).
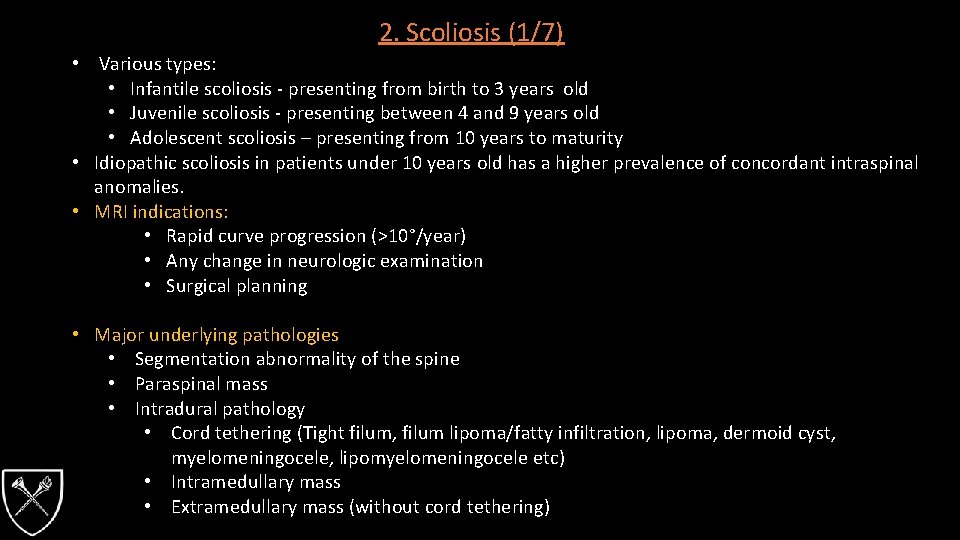
2. Scoliosis (1/7) • Various types: • Infantile scoliosis - presenting from birth to 3 years old • Juvenile scoliosis - presenting between 4 and 9 years old • Adolescent scoliosis – presenting from 10 years to maturity • Idiopathic scoliosis in patients under 10 years old has a higher prevalence of concordant intraspinal anomalies. • MRI indications: • Rapid curve progression (>10°/year) • Any change in neurologic examination • Surgical planning • Major underlying pathologies • Segmentation abnormality of the spine • Paraspinal mass • Intradural pathology • Cord tethering (Tight filum, filum lipoma/fatty infiltration, lipoma, dermoid cyst, myelomeningocele, lipomyelomeningocele etc) • Intramedullary mass • Extramedullary mass (without cord tethering)
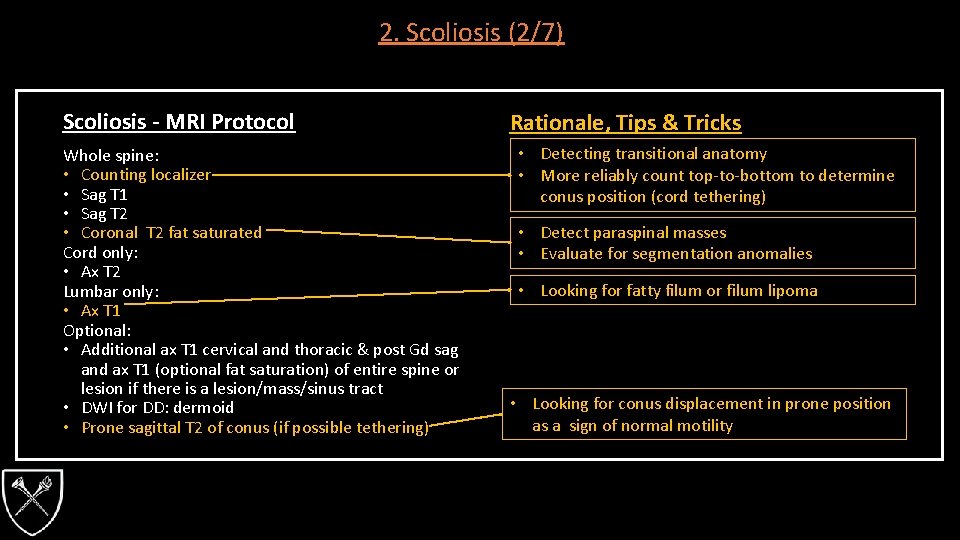
2. Scoliosis (2/7) Scoliosis - MRI Protocol Whole spine: • Counting localizer • Sag T 1 • Sag T 2 • Coronal T 2 fat saturated Cord only: • Ax T 2 Lumbar only: • Ax T 1 Optional: • Additional ax T 1 cervical and thoracic & post Gd sag and ax T 1 (optional fat saturation) of entire spine or lesion if there is a lesion/mass/sinus tract • DWI for DD: dermoid • Prone sagittal T 2 of conus (if possible tethering) Rationale, Tips & Tricks • Detecting transitional anatomy • More reliably count top-to-bottom to determine conus position (cord tethering) • Detect paraspinal masses • Evaluate for segmentation anomalies • Looking for fatty filum or filum lipoma • Looking for conus displacement in prone position as a sign of normal motility
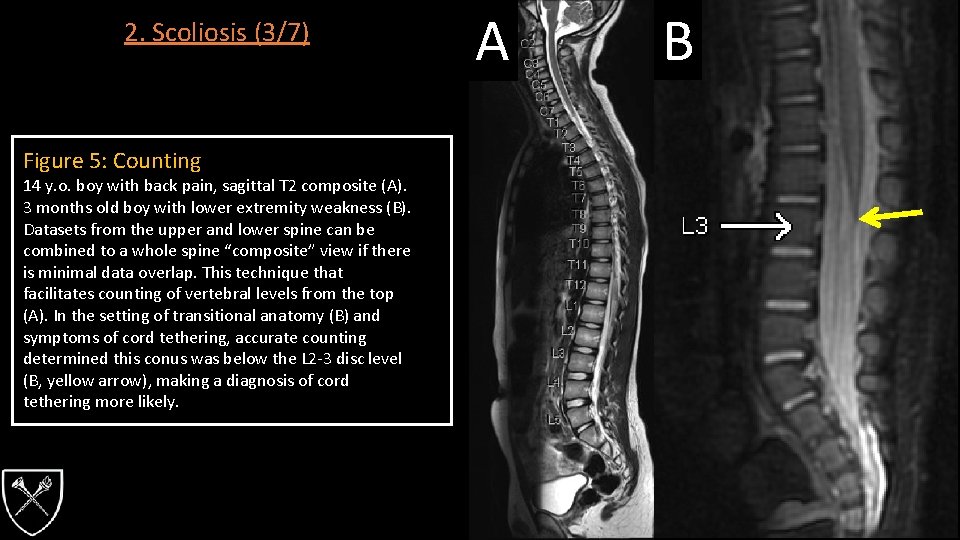
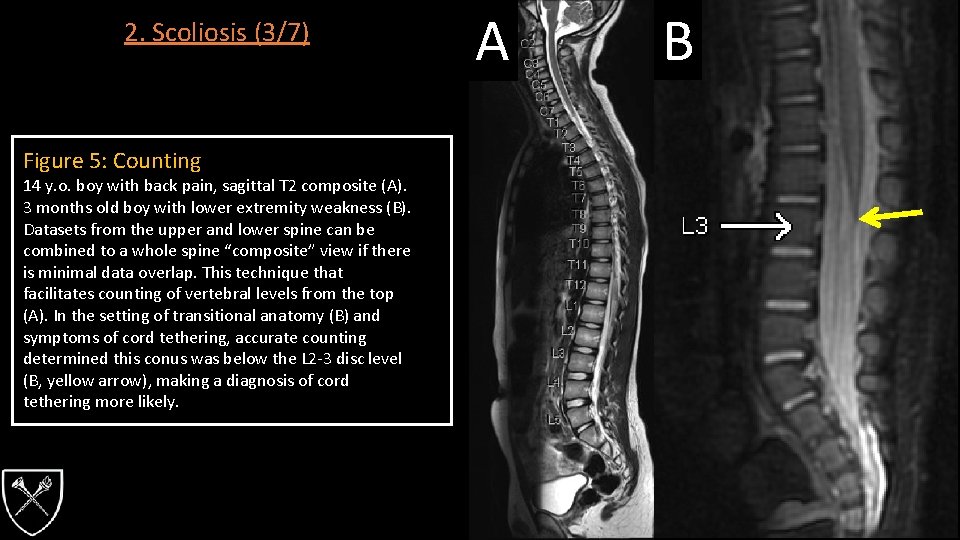
2. Scoliosis (3/7) Figure 5: Counting 14 y. o. boy with back pain, sagittal T 2 composite (A). 3 months old boy with lower extremity weakness (B). Datasets from the upper and lower spine can be combined to a whole spine “composite” view if there is minimal data overlap. This technique that facilitates counting of vertebral levels from the top (A). In the setting of transitional anatomy (B) and symptoms of cord tethering, accurate counting determined this conus was below the L 2 -3 disc level (B, yellow arrow), making a diagnosis of cord tethering more likely. A B
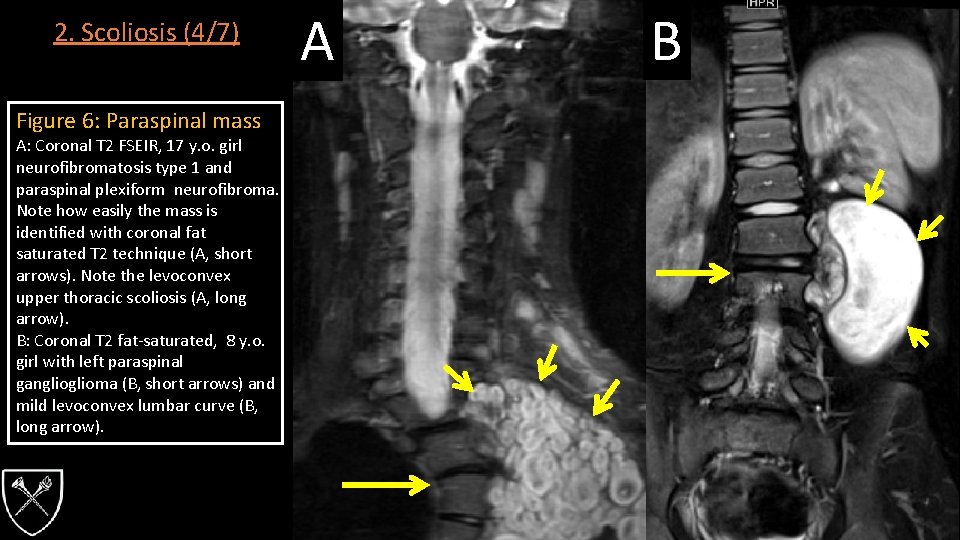
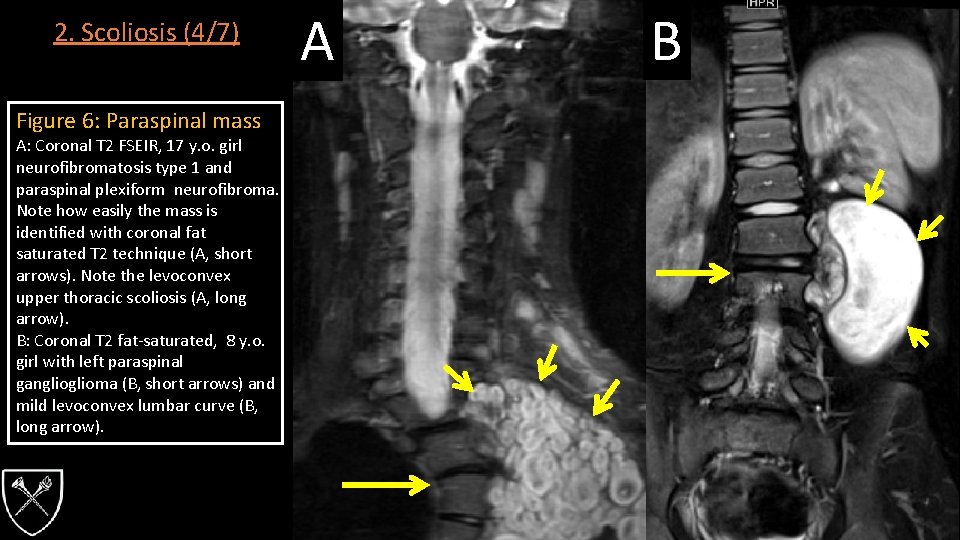
2. Scoliosis (4/7) Figure 6: Paraspinal mass A: Coronal T 2 FSEIR, 17 y. o. girl neurofibromatosis type 1 and paraspinal plexiform neurofibroma. Note how easily the mass is identified with coronal fat saturated T 2 technique (A, short arrows). Note the levoconvex upper thoracic scoliosis (A, long arrow). B: Coronal T 2 fat-saturated, 8 y. o. girl with left paraspinal ganglioma (B, short arrows) and mild levoconvex lumbar curve (B, long arrow). A B
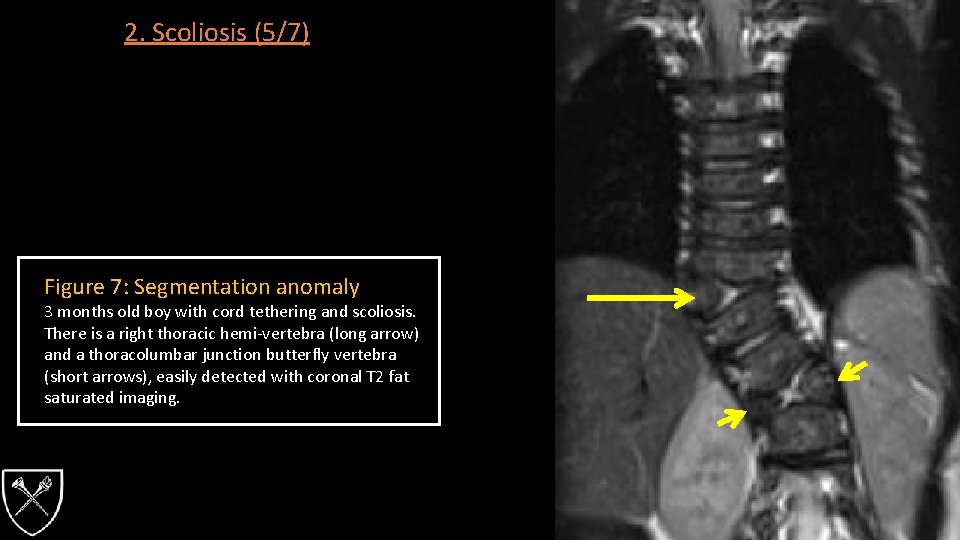
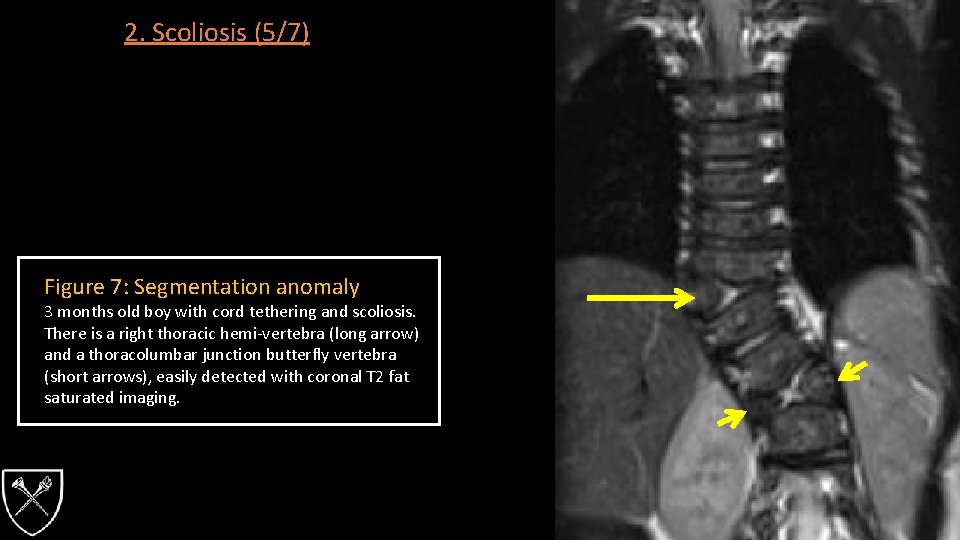
2. Scoliosis (5/7) Figure 7: Segmentation anomaly 3 months old boy with cord tethering and scoliosis. There is a right thoracic hemi-vertebra (long arrow) and a thoracolumbar junction butterfly vertebra (short arrows), easily detected with coronal T 2 fat saturated imaging.
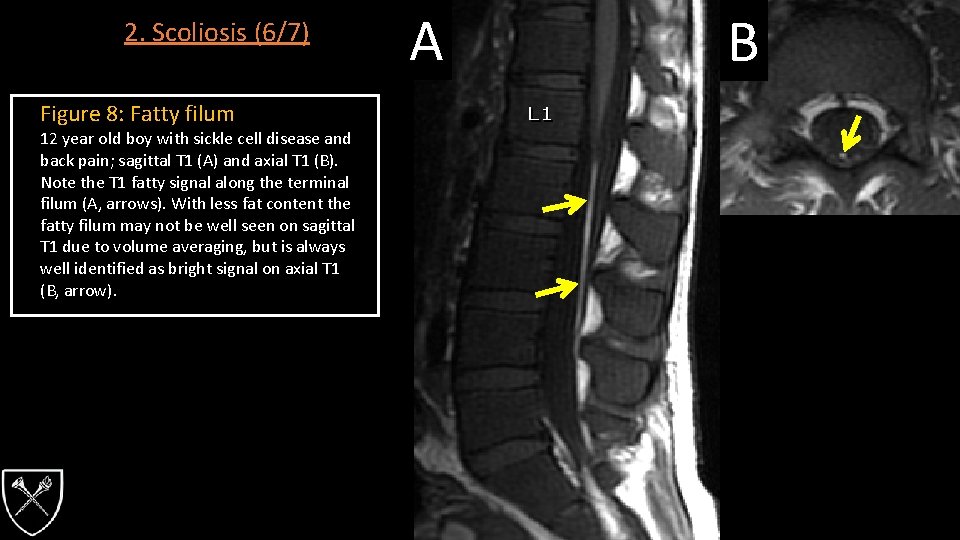
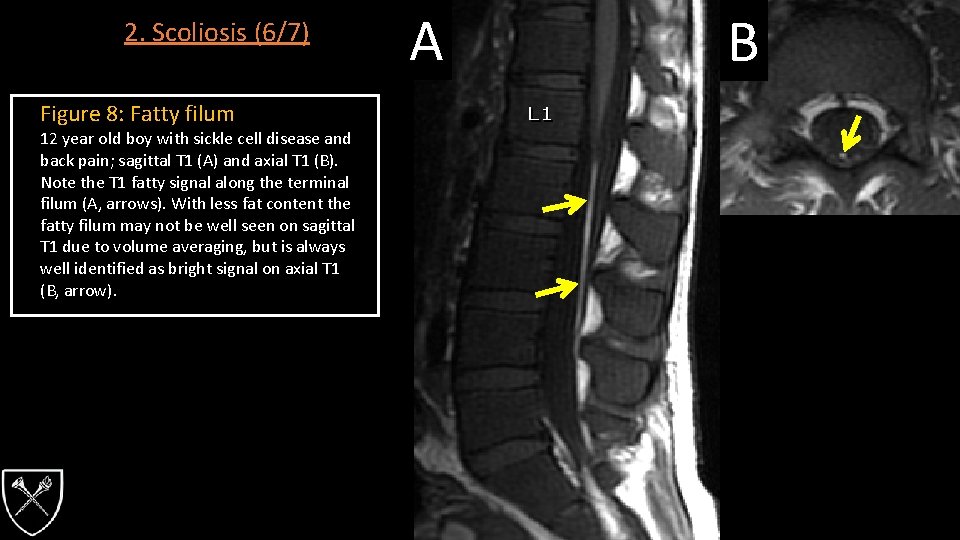
2. Scoliosis (6/7) Figure 8: Fatty filum 12 year old boy with sickle cell disease and back pain; sagittal T 1 (A) and axial T 1 (B). Note the T 1 fatty signal along the terminal filum (A, arrows). With less fat content the fatty filum may not be well seen on sagittal T 1 due to volume averaging, but is always well identified as bright signal on axial T 1 (B, arrow). A B
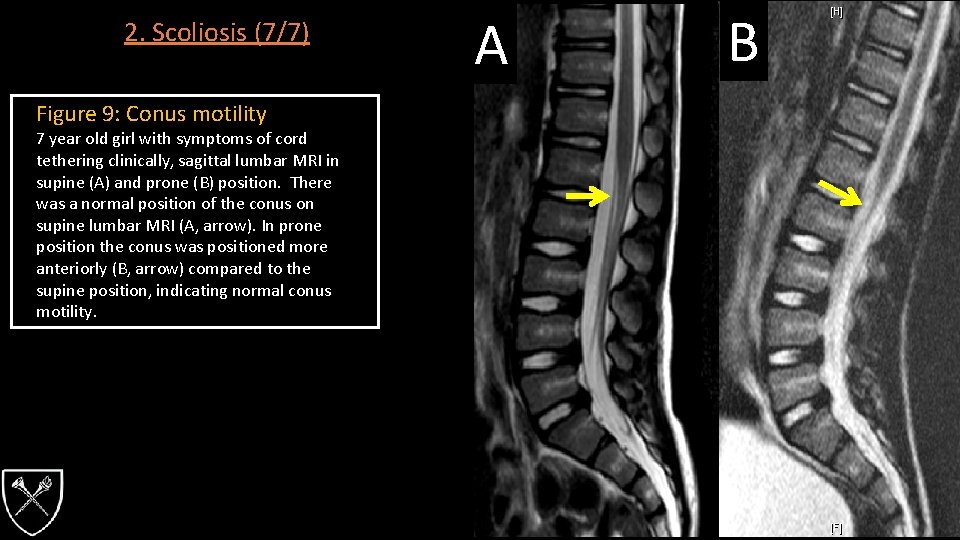
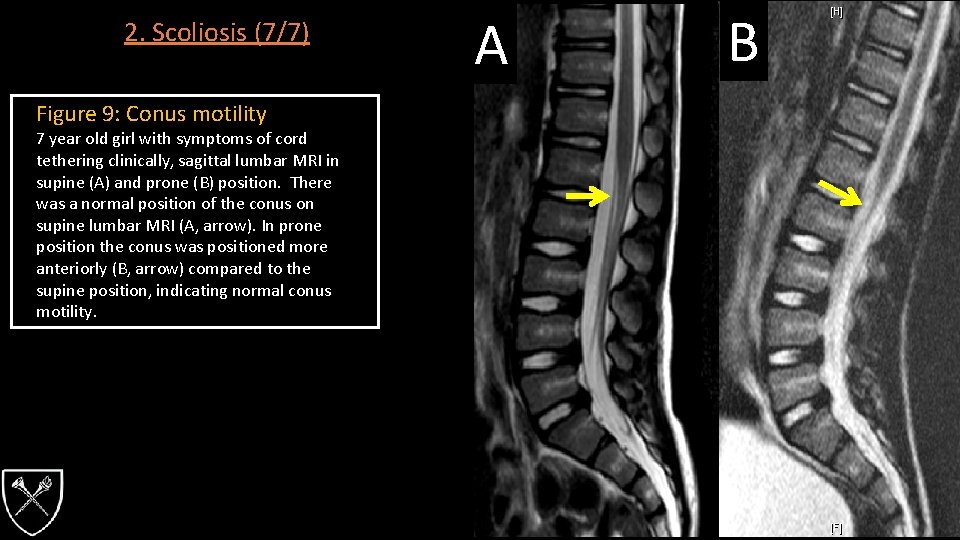
2. Scoliosis (7/7) Figure 9: Conus motility 7 year old girl with symptoms of cord tethering clinically, sagittal lumbar MRI in supine (A) and prone (B) position. There was a normal position of the conus on supine lumbar MRI (A, arrow). In prone position the conus was positioned more anteriorly (B, arrow) compared to the supine position, indicating normal conus motility. A B
3. Spinal Cord Disease (1/3) • Inflammatory demyelinating myelopathies comprise the majority of pediatric non-traumatic spinal cord lesions. • Often called “myelitis” (comprises acute transverse myelitis, NMO and spinal cord lesions in MS). • 20% of new cases of acute transverse myelitis occur in children <18 years old • 30 -62% of patient with transverse myelitis will have long term neurological deficits • Authors have reported poor lesion detection in young children with mild acute myelitis. • Specificity of MRI has been questioned as many demyelinating lesions can mimic transverse myelitis.
3. Spinal Cord Disease (2/3) Spinal Cord Disease - MRI Protocol Whole spine (pre- and post Gd) • Sag T 1 • Ax T 1 Cord only: • Ax 3 D GRE • Ax T 2 • Sag T 2 Rationale, Tips & Tricks • Improved detection of white matter lesions
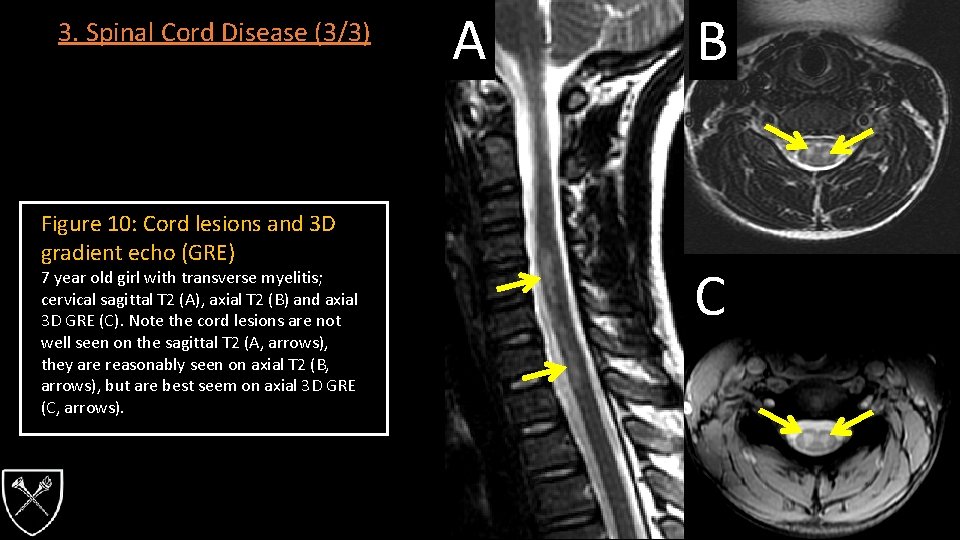
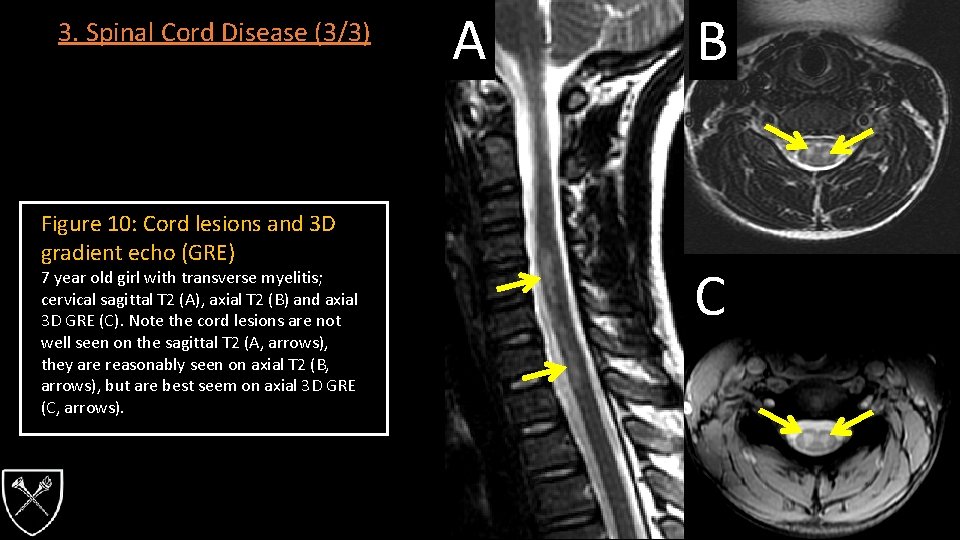
3. Spinal Cord Disease (3/3) Figure 10: Cord lesions and 3 D gradient echo (GRE) 7 year old girl with transverse myelitis; cervical sagittal T 2 (A), axial T 2 (B) and axial 3 D GRE (C). Note the cord lesions are not well seen on the sagittal T 2 (A, arrows), they are reasonably seen on axial T 2 (B, arrows), but are best seem on axial 3 D GRE (C, arrows). A B C
4. Craniocervical Instability (1/3) • Flexion-extension cervical MRI • Allows for the evaluation of dynamic changes in canal diameter resulting in cord compression even without true instability detected on radiographs. • Indicated in skeletal dysplasia with cervical spinal instability and stenosis (Mackenzie 2013) • Achondroplasia • Conradi Hunnerman syndrome • Distarophic dysplasia • Kniest dysplasia • Metatropic dysplasia • Mucopolysaccharidosis • Morquio syndrome • Extensive safety considerations are necessary, including neurological exam to document pre-imaging deficits, airway evaluation by anesthesia, anesthesia assisted sedation (if necessary), extensive patient monitoring during MRI, fast MRI sequences, abortion of scans with cord compression.
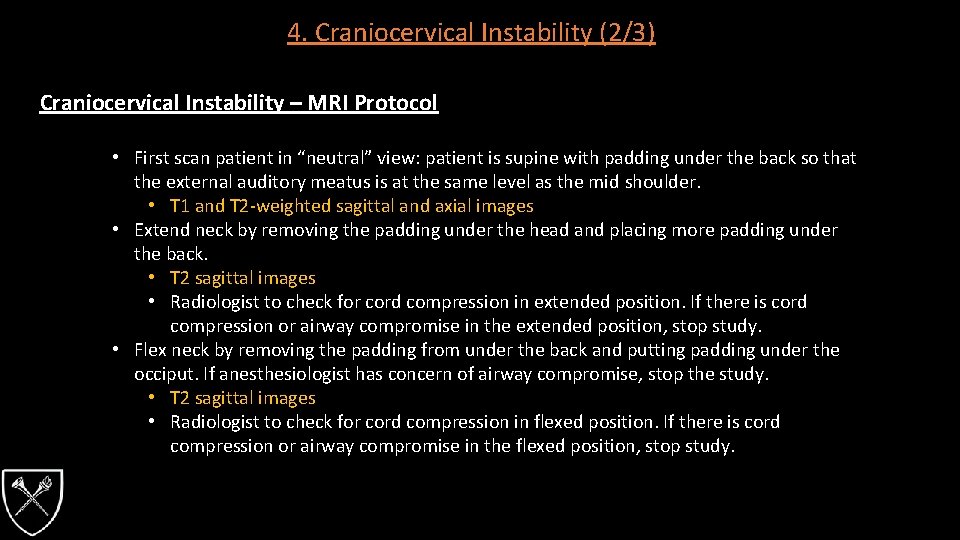
4. Craniocervical Instability (2/3) Craniocervical Instability – MRI Protocol • First scan patient in “neutral” view: patient is supine with padding under the back so that the external auditory meatus is at the same level as the mid shoulder. • T 1 and T 2 -weighted sagittal and axial images • Extend neck by removing the padding under the head and placing more padding under the back. • T 2 sagittal images • Radiologist to check for cord compression in extended position. If there is cord compression or airway compromise in the extended position, stop study. • Flex neck by removing the padding from under the back and putting padding under the occiput. If anesthesiologist has concern of airway compromise, stop the study. • T 2 sagittal images • Radiologist to check for cord compression in flexed position. If there is cord compression or airway compromise in the flexed position, stop study.
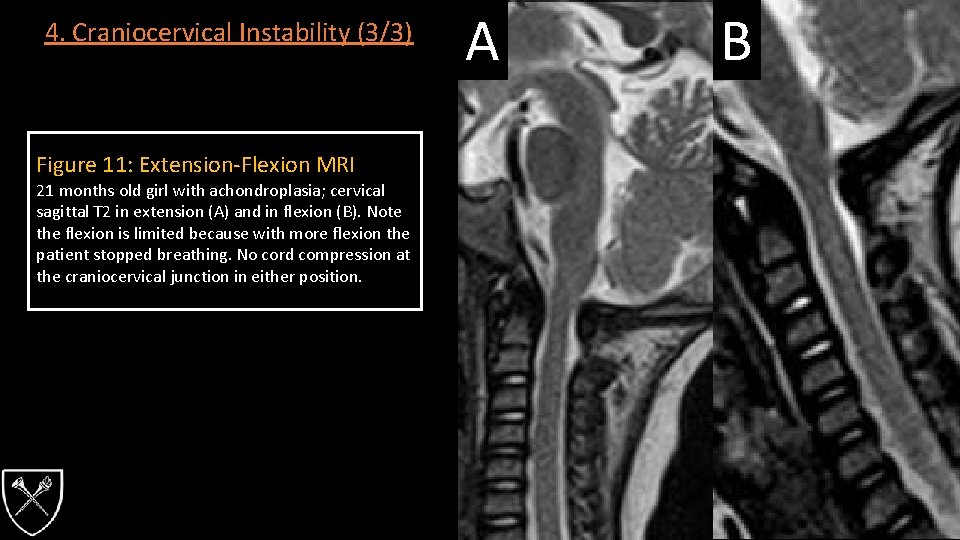
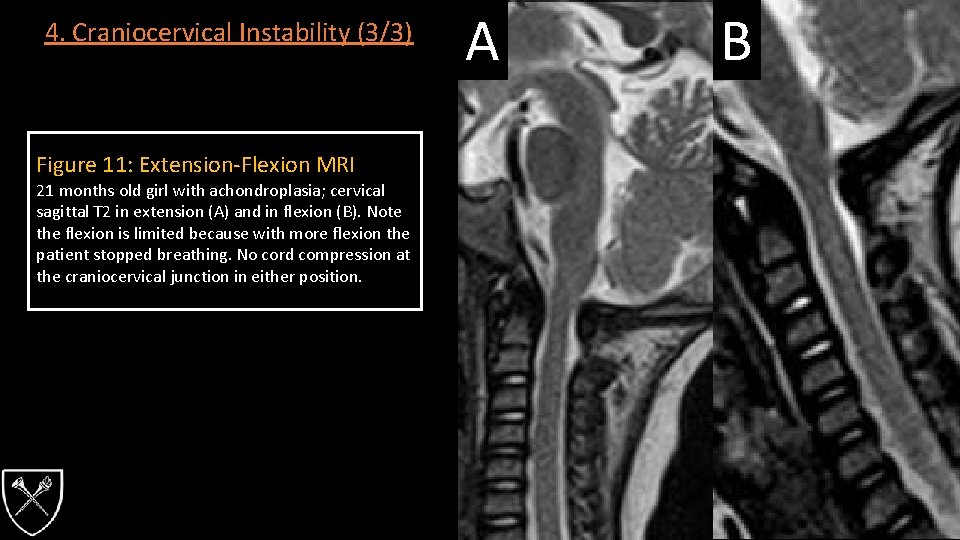
4. Craniocervical Instability (3/3) Figure 11: Extension-Flexion MRI 21 months old girl with achondroplasia; cervical sagittal T 2 in extension (A) and in flexion (B). Note the flexion is limited because with more flexion the patient stopped breathing. No cord compression at the craniocervical junction in either position. A B
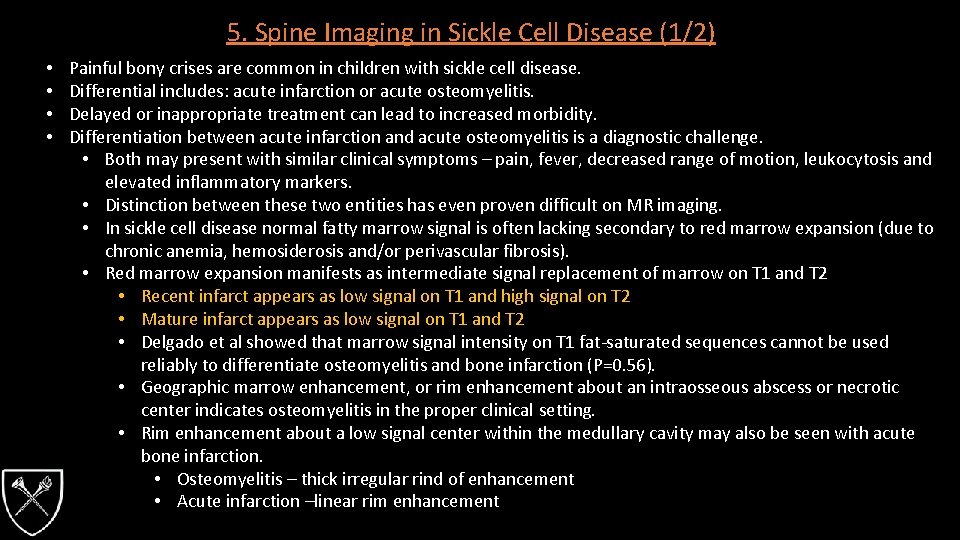
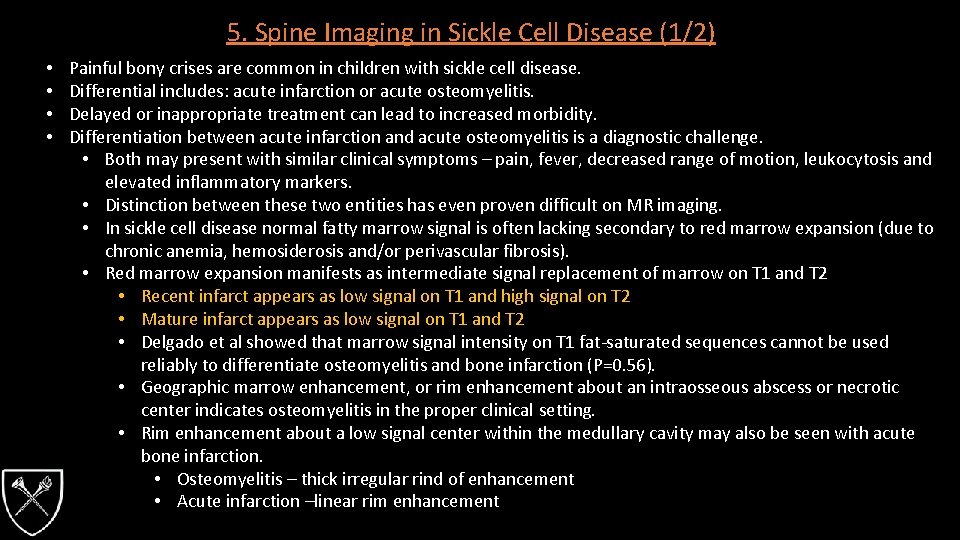
5. Spine Imaging in Sickle Cell Disease (1/2) • • Painful bony crises are common in children with sickle cell disease. Differential includes: acute infarction or acute osteomyelitis. Delayed or inappropriate treatment can lead to increased morbidity. Differentiation between acute infarction and acute osteomyelitis is a diagnostic challenge. • Both may present with similar clinical symptoms – pain, fever, decreased range of motion, leukocytosis and elevated inflammatory markers. • Distinction between these two entities has even proven difficult on MR imaging. • In sickle cell disease normal fatty marrow signal is often lacking secondary to red marrow expansion (due to chronic anemia, hemosiderosis and/or perivascular fibrosis). • Red marrow expansion manifests as intermediate signal replacement of marrow on T 1 and T 2 • Recent infarct appears as low signal on T 1 and high signal on T 2 • Mature infarct appears as low signal on T 1 and T 2 • Delgado et al showed that marrow signal intensity on T 1 fat-saturated sequences cannot be used reliably to differentiate osteomyelitis and bone infarction (P=0. 56). • Geographic marrow enhancement, or rim enhancement about an intraosseous abscess or necrotic center indicates osteomyelitis in the proper clinical setting. • Rim enhancement about a low signal center within the medullary cavity may also be seen with acute bone infarction. • Osteomyelitis – thick irregular rind of enhancement • Acute infarction –linear rim enhancement
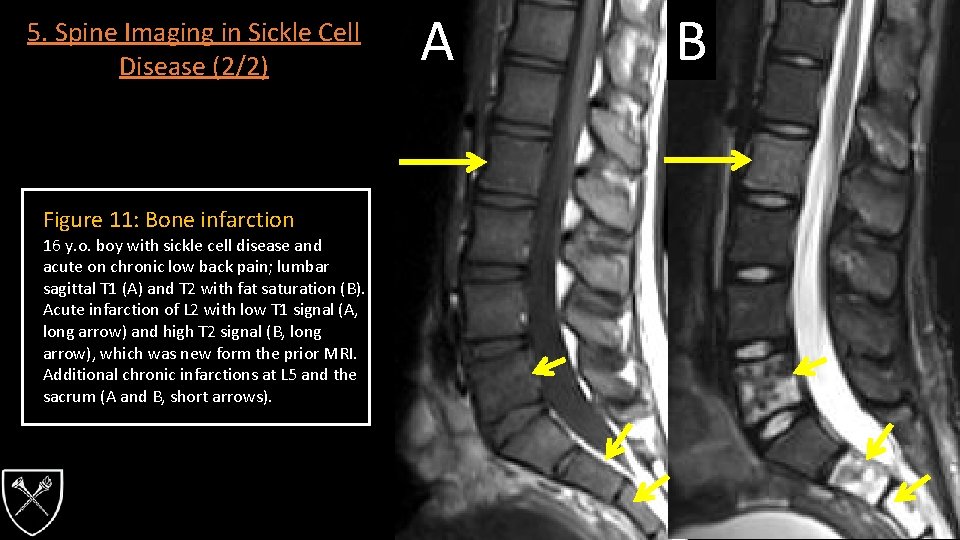
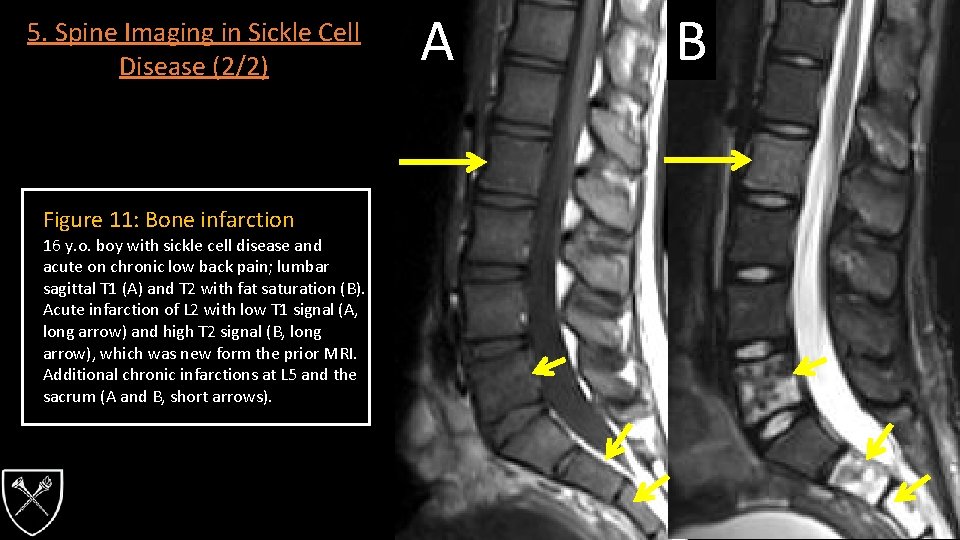
5. Spine Imaging in Sickle Cell Disease (2/2) Figure 11: Bone infarction 16 y. o. boy with sickle cell disease and acute on chronic low back pain; lumbar sagittal T 1 (A) and T 2 with fat saturation (B). Acute infarction of L 2 with low T 1 signal (A, long arrow) and high T 2 signal (B, long arrow), which was new form the prior MRI. Additional chronic infarctions at L 5 and the sacrum (A and B, short arrows). AA BB
6. Infection (Vertebral Osteomyelitis/Discitis) (1/3) • Intervertebral discitis and vertebral osteomyelitis are relatively uncommon entities. • Discitis – generally affects children < 5 years old with no or low grade fever. • Occurs almost exclusively in the lumbar region – causing refusal to walk or progressive limp. • Thought to occur due to the presence in childhood of vascular channels in the cartilaginous region of the disk space that disappear later in life, as well as abundant intraosseous arterial anastomoses in childhood. • Vertebral Osteomyelitis – typically effects older children who are febrile with back pain in the lumbar, thoracic or cervical region. • Accounts for only 1 -2% of all children with osteomyelitis • Thought to occur when microorganisms lodge in the low-flow, end-organ vasculature adjacent to the subchondrial plate region. • MRI found to have a 96% sensitivity and 93% specificity for diagnosis of vertebral osteomyelitis.
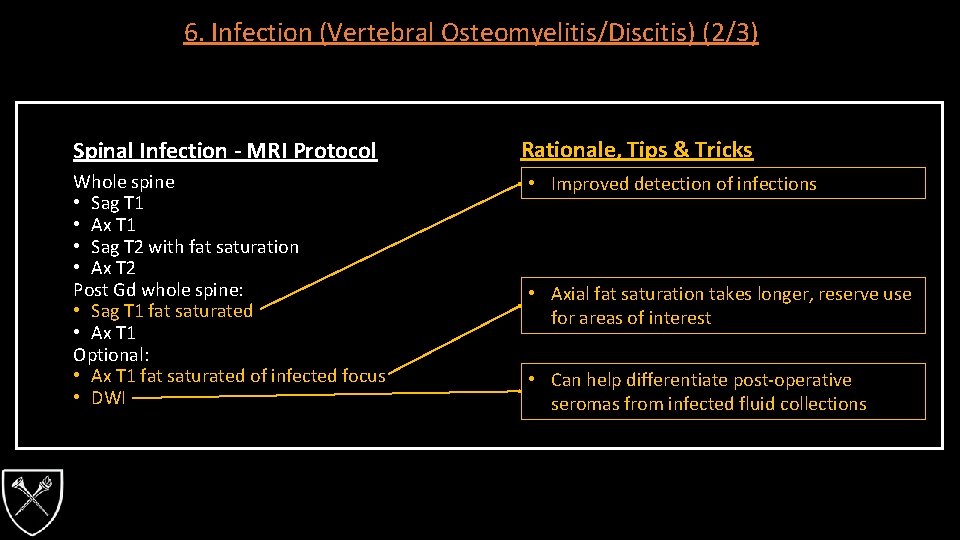
6. Infection (Vertebral Osteomyelitis/Discitis) (2/3) Spinal Infection - MRI Protocol Whole spine • Sag T 1 • Ax T 1 • Sag T 2 with fat saturation • Ax T 2 Post Gd whole spine: • Sag T 1 fat saturated • Ax T 1 Optional: • Ax T 1 fat saturated of infected focus • DWI Rationale, Tips & Tricks • Improved detection of infections • Axial fat saturation takes longer, reserve use for areas of interest • Can help differentiate post-operative seromas from infected fluid collections
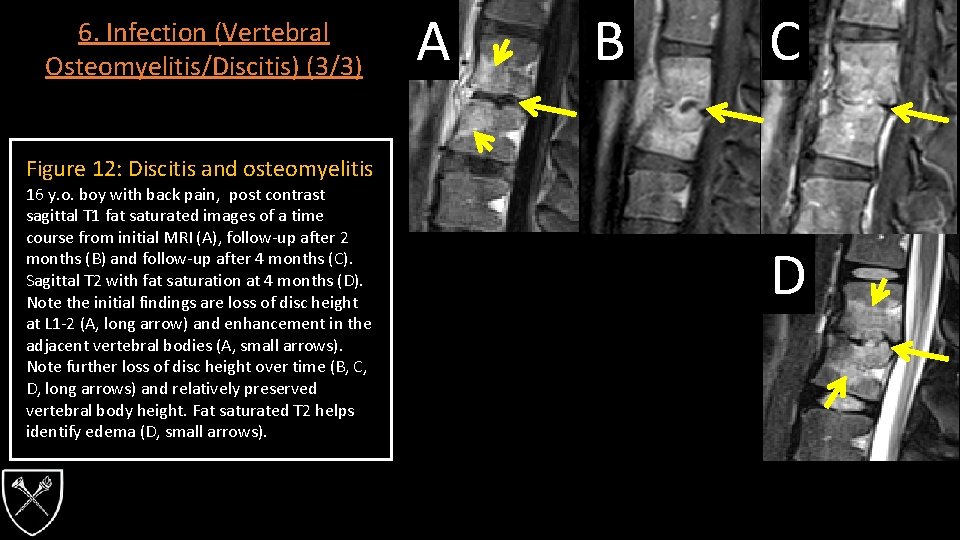
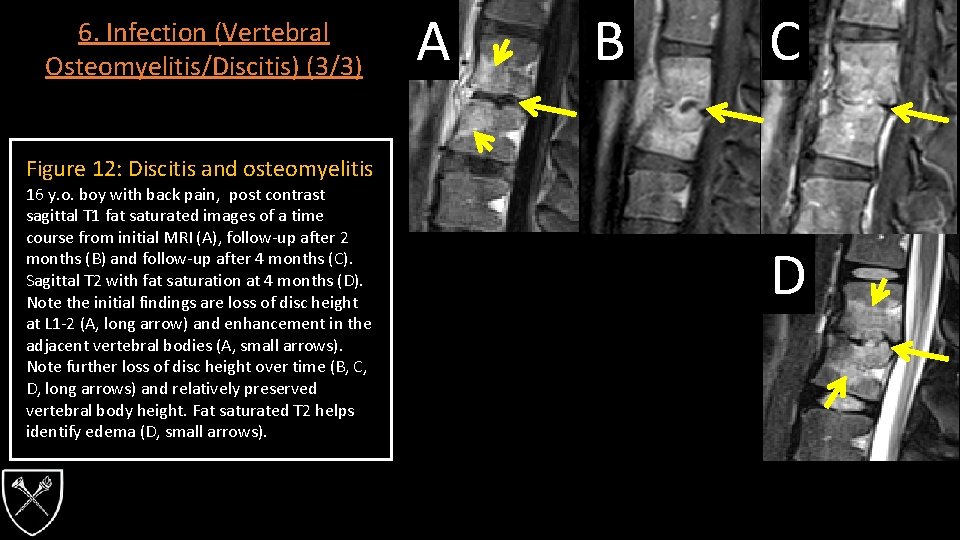
6. Infection (Vertebral Osteomyelitis/Discitis) (3/3) A B C Figure 12: Discitis and osteomyelitis 16 y. o. boy with back pain, post contrast sagittal T 1 fat saturated images of a time course from initial MRI (A), follow-up after 2 months (B) and follow-up after 4 months (C). Sagittal T 2 with fat saturation at 4 months (D). Note the initial findings are loss of disc height at L 1 -2 (A, long arrow) and enhancement in the adjacent vertebral bodies (A, small arrows). Note further loss of disc height over time (B, C, D, long arrows) and relatively preserved vertebral body height. Fat saturated T 2 helps identify edema (D, small arrows). D
7. Malignancy (1/5) • Pediatric spinal tumors are commonly categorized by their location, which also directs clinical management. • Intramedullary • < 10% of all pediatric central nervous system (CNS) lesions • Imaging features commonly include – • Expansion of the spinal cord • Syringohydromyelia • Tumoral or nontumoral cysts • Glial neoplasms most common intramedullary lesions • Ependymomas are rare before the 10 years of age (30%) • Astrocytomas are most common in early childhood (60%) • Commonly centered at the cervical-thoracic junction, eccentric, hemorrhage is uncommon • Gangliomas are seen in children <3 years old (15 -30%) • Considered benign and slow growing • Frequently associated with tumoral cyst, and reported to extend up to 8 vertebral bodies
7. Malignancy (2/5) • Extramedullary intradural • Displace and compress the cord, expanding the ipsilateral thecal sac, commonly situated in neural foramina and the filum terminale. • Nerve sheath tumors – neurofibromas and schwannomas • Meningiomas – relatively uncommon in pediatric patients • Clear cell type more common in children • Paragangliomas • Myxopapillary Ependymomas • Lipomas and dermoids • Metastatic disease • Primary CNS tumors commonly assoiciated with CSF dissemination – medulloblastomas, ependymomas, choroid plexus tumors, PNETs and high-grad gliomas. • Secondary spine involvement can occur with ewing sarcoma, neuroblastoma, osteogenic sarcoma, rhabdomyosarcoma and lymphoma. • T 1 post contrast fat suppression can help to augment metastatic conspicuity
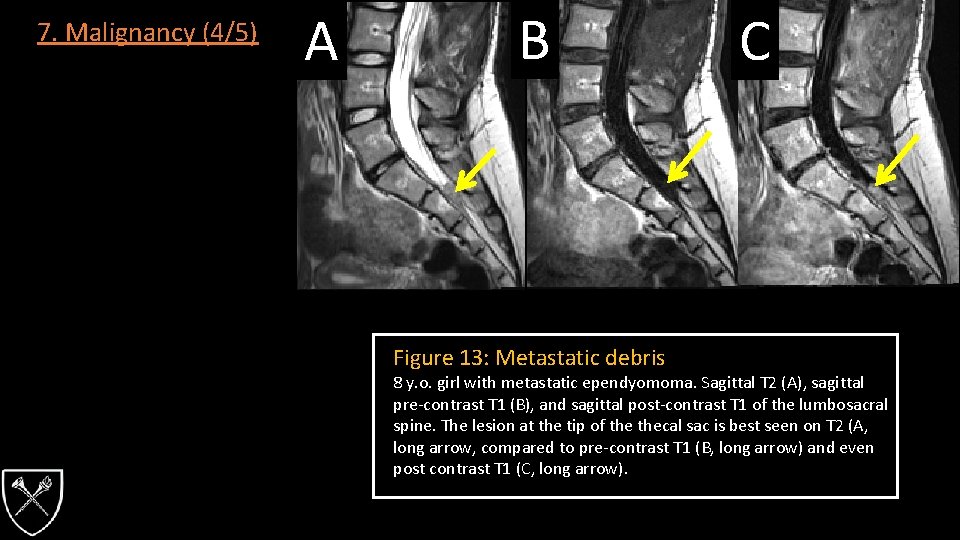
7. Malignancy (3/5) Malignancy - MRI Protocol Whole spine • Sag T 1 (pre- and post Gd) • Ax T 1 (pre- and post Gd) • Sag T 2 • Sag DWI • Ax T 2 • 3 D T 2 lumbosacral junction Rationale, Tips & Tricks • Omit pre-contrast images for follow-up studies screening for spinal metastatic disease • Best for medulloblastoma metastasis which may be non-enhancing and/or small • Look for metastatic debris layering at the bottom of thecal sac
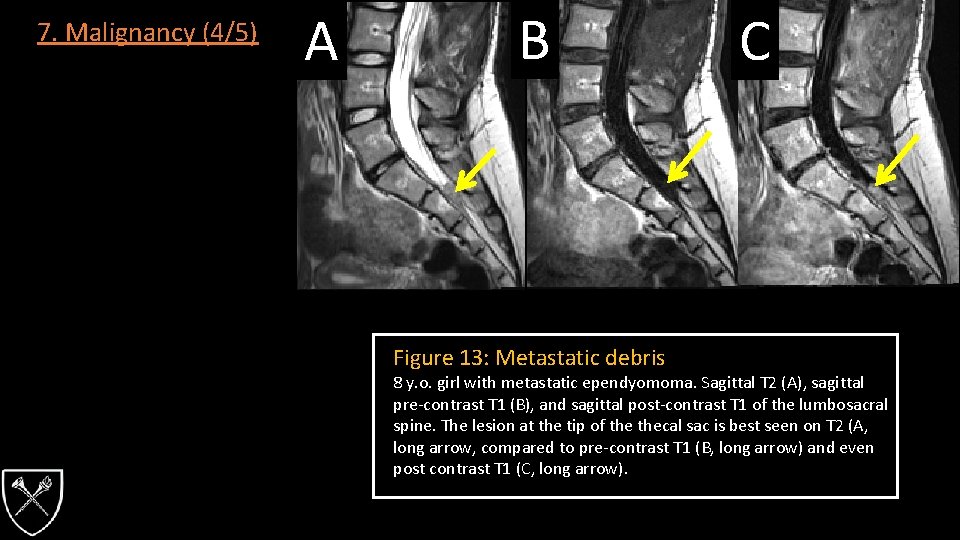
7. Malignancy (4/5) A B Figure 13: Metastatic debris C 8 y. o. girl with metastatic ependyomoma. Sagittal T 2 (A), sagittal pre-contrast T 1 (B), and sagittal post-contrast T 1 of the lumbosacral spine. The lesion at the tip of thecal sac is best seen on T 2 (A, long arrow, compared to pre-contrast T 1 (B, long arrow) and even post contrast T 1 (C, long arrow).
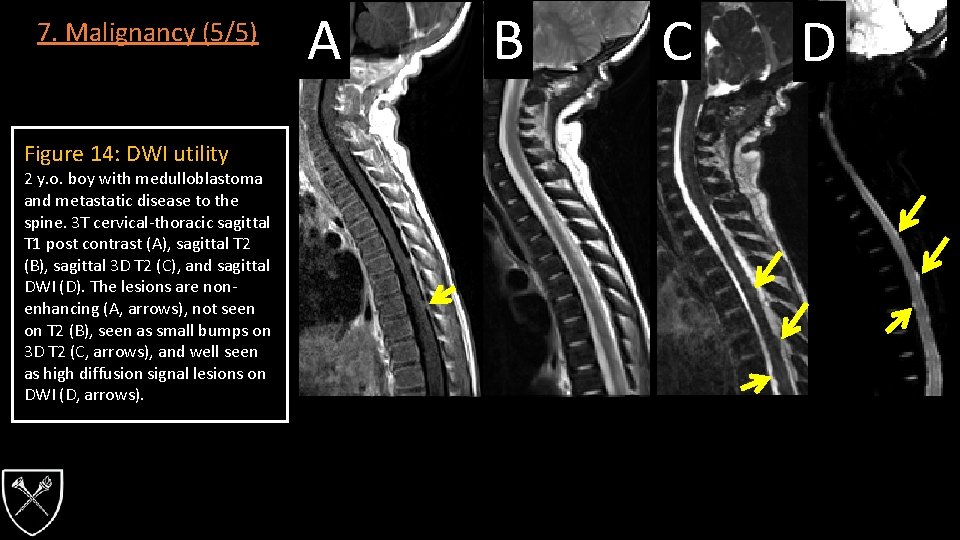
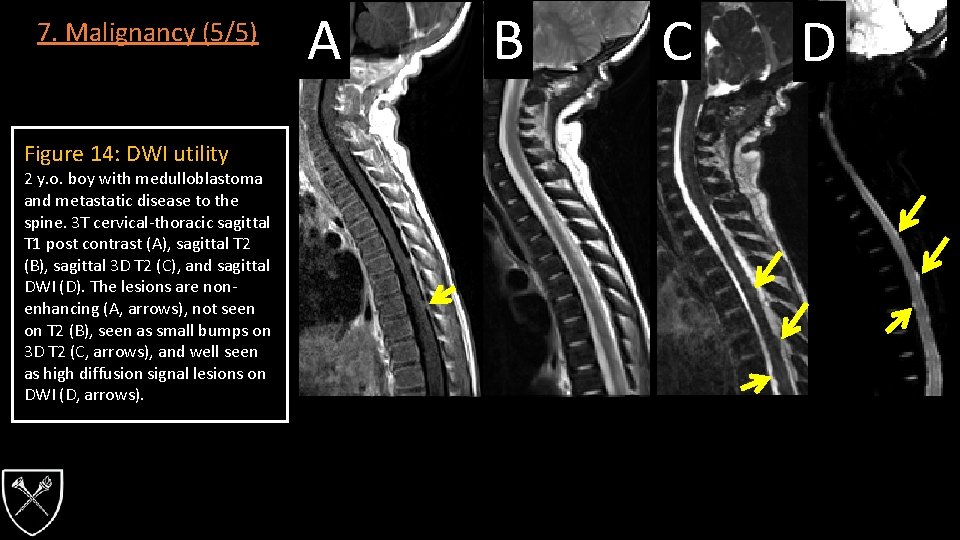
7. Malignancy (5/5) Figure 14: DWI utility 2 y. o. boy with medulloblastoma and metastatic disease to the spine. 3 T cervical-thoracic sagittal T 1 post contrast (A), sagittal T 2 (B), sagittal 3 D T 2 (C), and sagittal DWI (D). The lesions are nonenhancing (A, arrows), not seen on T 2 (B), seen as small bumps on 3 D T 2 (C, arrows), and well seen as high diffusion signal lesions on DWI (D, arrows). A B C D
8. Back Pain (1/4) • Persistent back pain is rare in health children who have no history of trauma and therefore must be taken seriously. • Persistent back pain may be the manifestation of infections (ex osteomyelitis), congenital (ex tethered cord), neoplastic (ex lymphoma), or traumatic (ex spondylolithesis) causes. • Adolescent athletes may experience low back pain associated with repetitive stress. • PA and Lateral spinal radiographs will pick up the large majority of abnormalities. • MRI should be considered with normal radiographs and red flag symptoms (radicular symptoms, weakness, stiffness, or other neurological signs). • Spondylolysis – defect of the pars interarticularis (PI) considered to be a form of stress fracture, often associated with rigorous sporting activities during the growth period. • Most common in the lumbar spine • Changes in the MRI signal intensity in the PI are useful in the early diagnosis of spondylolysis. • Presence of low signal intensity in the PI on T 1 W images appears prior to spondylolysis on plain radiographs or CT. • Low T 1 signal intensity may be due to hemorrhage in the PI or edema of the adjacent tissues.
8. Back Pain (2/4) Low Back Pain - MRI Protocol Lumbar spine • Sag T 1 • Ax T 1 • Sag T 2 with fat saturation • Ax T 2 Optional • Hi res T 1 oblique (0. 625 mm) Rationale, Tips & Tricks • Detect edema as early manifestation of spondylolysis • Best for MRI depiction of spondylolysis
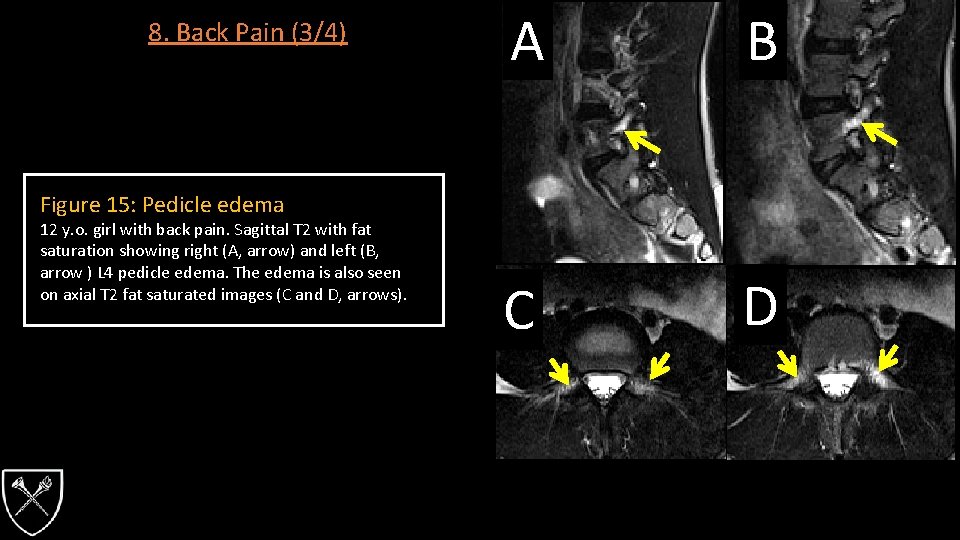
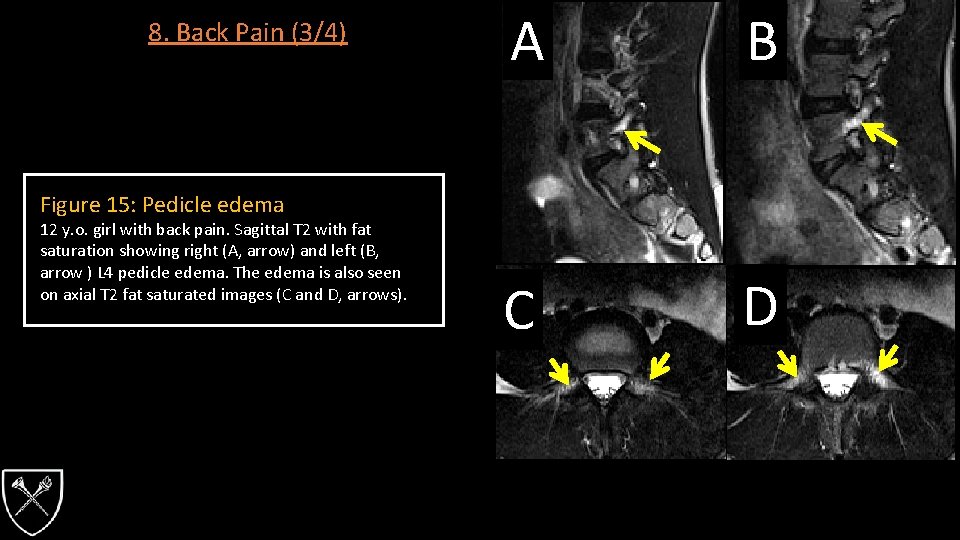
8. Back Pain (3/4) A B C D Figure 15: Pedicle edema 12 y. o. girl with back pain. Sagittal T 2 with fat saturation showing right (A, arrow) and left (B, arrow ) L 4 pedicle edema. The edema is also seen on axial T 2 fat saturated images (C and D, arrows).
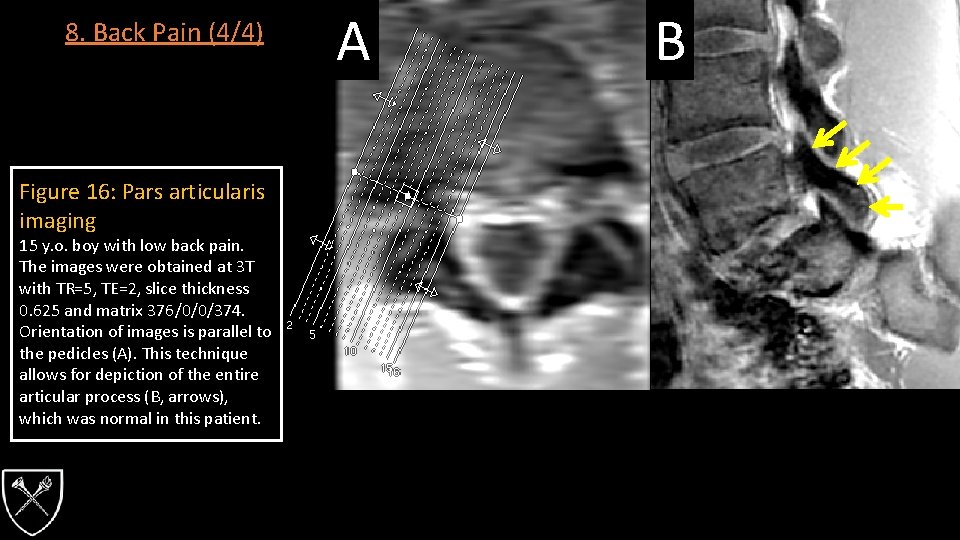
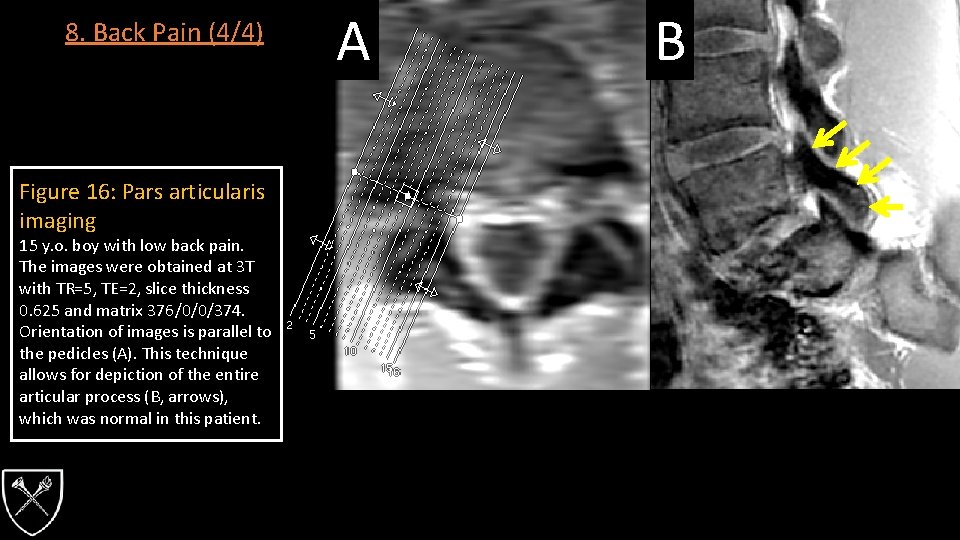
8. Back Pain (4/4) Figure 16: Pars articularis imaging 15 y. o. boy with low back pain. The images were obtained at 3 T with TR=5, TE=2, slice thickness 0. 625 and matrix 376/0/0/374. Orientation of images is parallel to the pedicles (A). This technique allows for depiction of the entire articular process (B, arrows), which was normal in this patient. A B
• • References 1. Spinal trauma • Egloff, A. M. , Kadom, N. , Vezina, G. , & Bulas, D. (2009). Pediatric cervical spine trauma imaging: a practical approach. Pediatr Radiol, 39(5), 447456. • Henry, M. , Scarlata, K. , Riesenburger, R. I. , Kryzanski, J. , Rideout, L. , Samdani, A. , . . . Hwang, S. W. (2013). Utility of STIR MRI in pediatric cervical spine clearance after trauma. J Neurosurg Pediatr, 12(1), 30 -36. • Kadom, N. , Khademian, Z. , Vezina, G. , Shalaby-Rana, E. , Rice, A. , & Hinds, T. (2014). Usefulness of MRI detection of cervical spine and brain injuries in the evaluation of abusive head trauma. Pediatr Radiol, 44(7), 839 -848. 2. Scoliosis • Courvoisier, A. , Belvisi, B. , Faguet, R. , Eid, A. , Bourgeois, E. , & Griffet, J. (2015). A New Paradigm for the Management of Thoracolumbar Pediatric Spine Traumas. Pediatr Emerg Care. • Dobbs, M. B. , Lenke, L. G. , Szymanski, D. A. , Morcuende, J. A. , Weinstein, S. L. , Bridwell, K. H. , & Sponseller, P. D. (2002). Prevalence of neural axis abnormalities in patients with infantile idiopathic scoliosis. J Bone Joint Surg Am, 84 -A(12), 2230 -2234. • Gupta, P. , Lenke, L. G. , & Bridwell, K. H. (1998). Incidence of neural axis abnormalities in infantile and juvenile patients with spinal deformity. Is a magnetic resonance image screening necessary? Spine (Phila Pa 1976), 23(2), 206 -210. • Pahys, J. M. , Samdani, A. F. , & Betz, R. R. (2009). Intraspinal anomalies in infantile idiopathic scoliosis: prevalence and role of magnetic resonance imaging. Spine (Phila Pa 1976), 34(12), E 434 -438. 3. Spinal Cord Disease • Barakat, N. , Gorman, M. P. , Benson, L. , Becerra, L. , & Borsook, D. (2015). Pain and spinal cord imaging measures in children with demyelinating disease. Neuroimage Clin, 9, 338 -347. • Thomas, T. , Branson, H. M. , Verhey, L. H. , Shroff, M. , Stephens, D. , Magalhaes, S. , & Banwell, B. (2012). The demographic, clinical, and magnetic resonance imaging (MRI) features of transverse myelitis in children. J Child Neurol, 27(1), 11 -21. 4. Craniocervical Junction • Mackenzie, W. , Dhawale, A. , Demczko, M. , Ditro, C. , Rogers, K. , Bober, M. , Campbell, J. , Grissom, L. (2013). Flexion-Extension Cervical Spine MRI in Children With Skeletal Dysplasia: Is It Safe and Effective? Journal of Pediatric Orthopaedics, 33(1), 91 -98. • Weng, M. , & Haynes, R. (1996). Flexion and Extension Cervical MRI in a Pediatric Population. Journal of Pediatric Orthopaedics, 16(3), 359 -363. • Zhang, L. , Zeitoun, D. , Rangel, A. , Lazennec, J. Y. , Catonne, Y. , & Pascal-Moussellard, H. (2011). Preoperative evaluation of the cervical spondylotic myelopathy with flexion-extension magnetic resonance imaging: about a prospective study of fifty patients. Spine (Phila Pa 1976), 36(17), E 1134 -1139.
References • • 5. Sickle Cell Disease • Bonnerot, V. , Sebag, G. , de Montalembert, M. , Wioland, M. , Glorion, C. , Girot, R. , & Lallemand, D. (1994). Gadolinium-DOTA enhanced MRI of painful osseous crises in children with sickle cell anemia. Pediatr Radiol, 24(2), 92 -95. • Delgado, J. , Bedoya, M. A. , Green, A. M. , Jaramillo, D. , & Ho-Fung, V. (2015). Utility of unenhanced fat-suppressed T 1 -weighted MRI in children with sickle cell disease -- can it differentiate bone infarcts from acute osteomyelitis? Pediatr Radiol, 45(13), 1981 -1987. • Umans, H. , Haramati, N. , & Flusser, G. (2000). The diagnostic role of gadolinium enhanced MRI in distinguishing between acute medullary bone infarct and osteomyelitis. Magn Reson Imaging, 18(3), 255 -262. 6. Infection • Fernandez, M. , Carrol, C. L. , & Baker, C. J. (2000). Discitis and vertebral osteomyelitis in children: an 18 -year review. Pediatrics, 105(6), 1299 -1304. • Rossi, A. (2015). Pediatric spinal infection and inflammation. Neuroimaging Clin N Am, 25(2), 173 -191. 7. Malignancy • Hayes, L. L. , Jones, R. A. , Palasis, S. , Aguilera, D. , & Porter, D. A. (2012). Drop metastases to the pediatric spine revealed with diffusionweighted MR imaging. Pediatr Radiol, 42(8), 1009 -1013. • Menashe, S. J. , & Iyer, R. S. (2013). Pediatric spinal neoplasia: a practical imaging overview of intramedullary, intradural, and osseous tumors. Curr Probl Diagn Radiol, 42(6), 249 -265. 8. Back Pain • Campbell, R. S. , Grainger, A. J. , Hide, I. G. , Papastefanou, S. , & Greenough, C. G. (2005). Juvenile spondylolysis: a comparative analysis of CT, SPECT and MRI. Skeletal Radiol, 34(2), 63 -73. • Taxter, A. J. , Chauvin, N. A. , & Weiss, P. F. (2014). Diagnosis and treatment of low back pain in the pediatric population. Phys Sportsmed, 42(1), 94 -104. • Yamane, T. , Yoshida, T. , & Mimatsu, K. (1993). Early diagnosis of lumbar spondylolysis by MRI. J Bone Joint Surg Br, 75(5), 764 -768.