OPTIMA Optimal Timing of PCI in Unstable Angina
OPTIMA: Optimal Timing of PCI in Unstable Angina Prospective, Randomized Evaluation of Immediate Versus Deferred Angioplasty in Patients with High Risk Acute Coronary Syndromes Current controlled trial number: ISRCTN 80874637 RK Riezebos 1, E Ronner 1, E Ter Bals 1, T Slagboom 1, F Kiemeneij 1, G Amoroso 1, MS Patterson 1, JG Tijssen 2, MJ Suttorp 3, GJ Laarman 1 1 Onze Lieve Vrouwe Gasthuis, Amsterdam, The Netherlands Medical Center, Amsterdam, The Netherlands 3 St Antonius Hospital, Nieuwegein, The Netherlands 2 Amsterdam
Introduction • Current guidelines recommend an early invasive strategy in high risk NSTE-ACS • The precise timing of early PCI is controversial. ¡ Immediate PCI may prevent (spontaneous) cardiac events ¡ Deferred PCI may lead to less peri-procedural complications

OPTIMA trial • Optimal timing of PCI in unstable angina • To compare immediate with 24– 48 hours deferred PCI in the early invasive management of NSTE-ACS • Hypothesis: In high risk NSTE-ACS immediate PCI reduces cardiac events
Patients • Patients with high risk NSTE-ACS • No indication for urgent PCI • Immediate coronary angiography • Culprit lesion amenable for PCI

Randomized treatments • Randomization in cathlab after angiography • Immediate PCI ¡ PCI of culprit lesion in same session • Deferred PCI ¡ PCI of culprit lesion after repeat angiography 24 -48 hours later • Triple antiplatelet therapy ¡ Abciximab, clopidogrel and aspirin
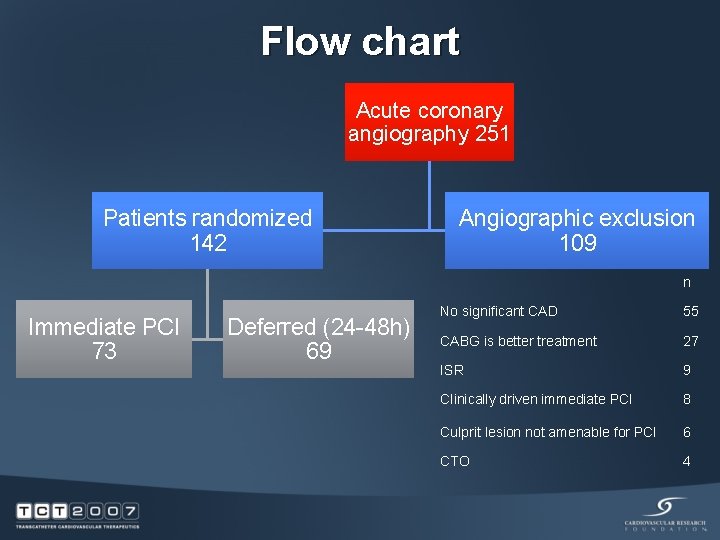
Flow chart Acute coronary angiography 251 Patients randomized 142 Angiographic exclusion 109 n Immediate PCI 73 Deferred (24 -48 h) 69 No significant CAD 55 CABG is better treatment 27 ISR 9 Clinically driven immediate PCI 8 Culprit lesion not amenable for PCI 6 CTO 4

Time from randomization to PCI
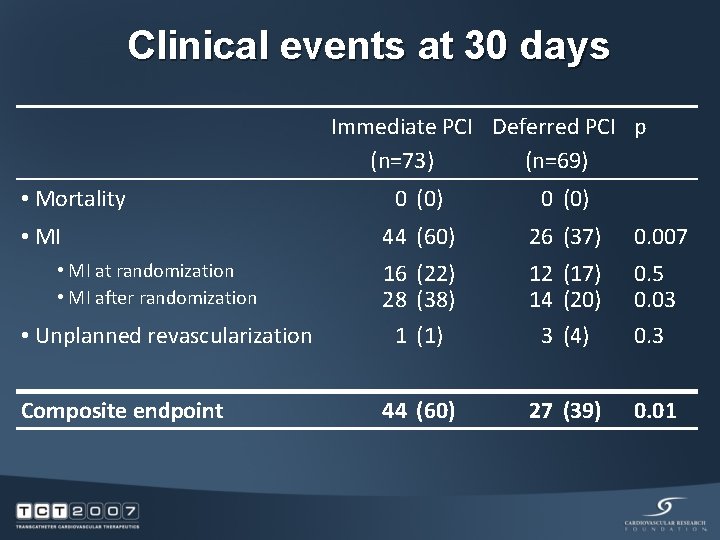
Clinical events at 30 days Immediate PCI Deferred PCI p (n=73) (n=69) • Mortality • MI at randomization • MI after randomization • Unplanned revascularization Composite endpoint 0 (0) 44 (60) 26 (37) 0. 007 16 (22) 28 (38) 12 (17) 14 (20) 0. 5 0. 03 1 (1) 3 (4) 0. 3 44 (60) 27 (39) 0. 01
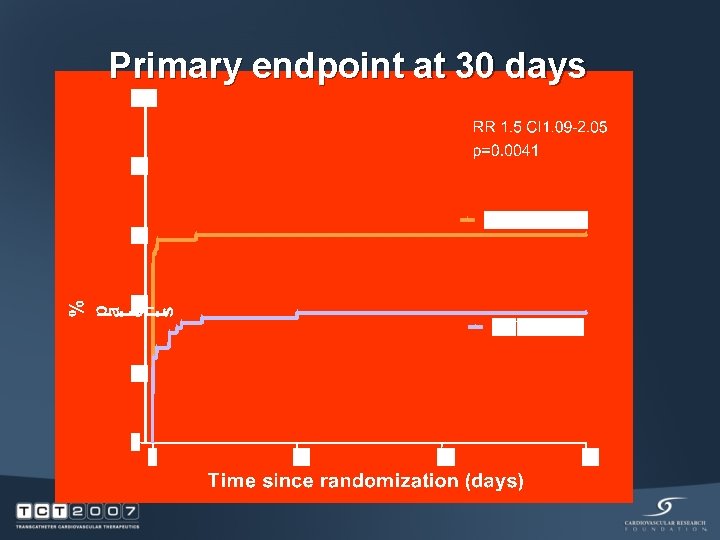
Primary endpoint at 30 days
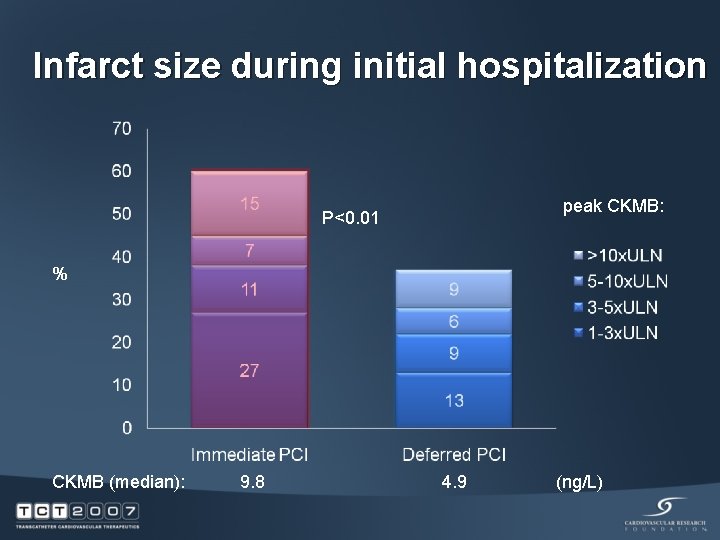
Infarct size during initial hospitalization peak CKMB: P<0. 01 % CKMB (median): 9. 8 4. 9 (ng/L)
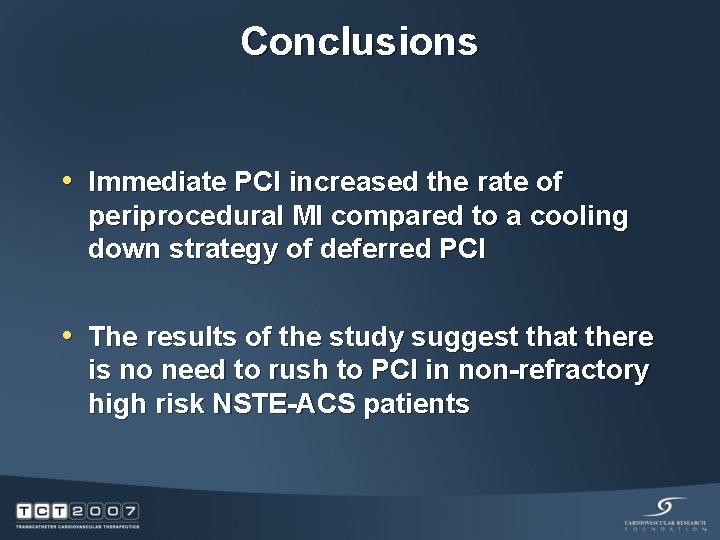
Conclusions • Immediate PCI increased the rate of periprocedural MI compared to a cooling down strategy of deferred PCI • The results of the study suggest that there is no need to rush to PCI in non-refractory high risk NSTE-ACS patients
- Slides: 11