Opioidfree Perioperative Pain Management D John Doyle MD









- Slides: 34
Opioid-free Perioperative Pain Management D. John Doyle MD Ph. D Chief, Department of General Anesthesia Cleveland Clinic Abu Dhabi Professor of Anesthesiology Cleveland Clinic

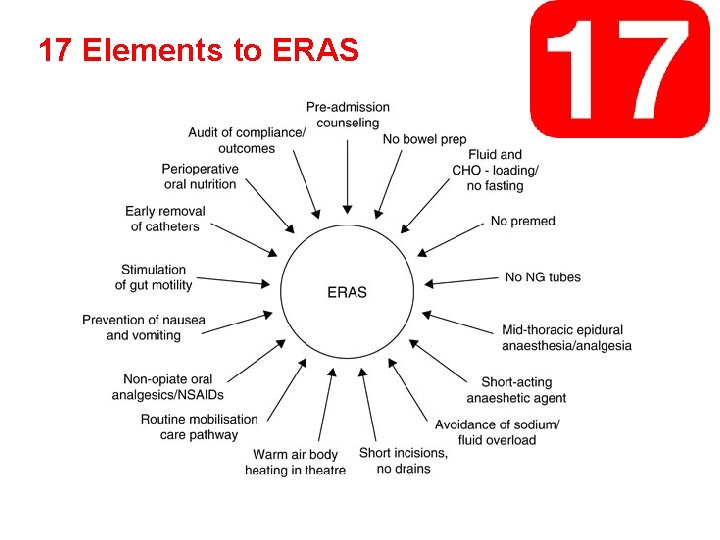
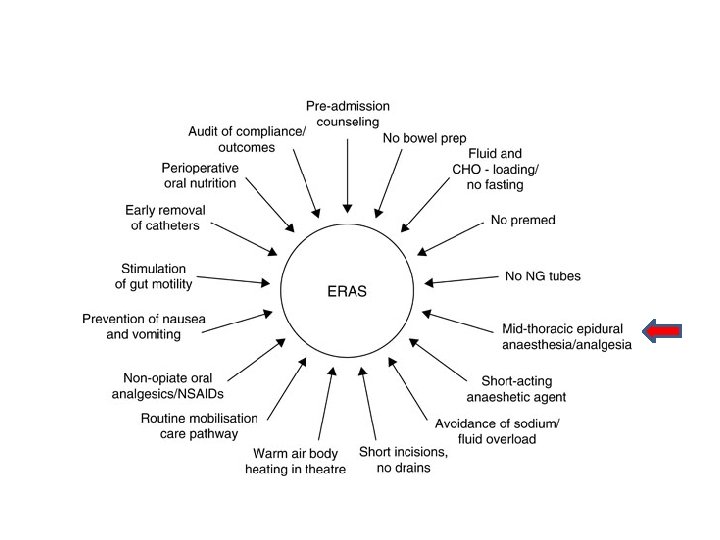
Much of what is known about opioid-free perioperative pain management comes to us from the Enhanced Recovery literature.
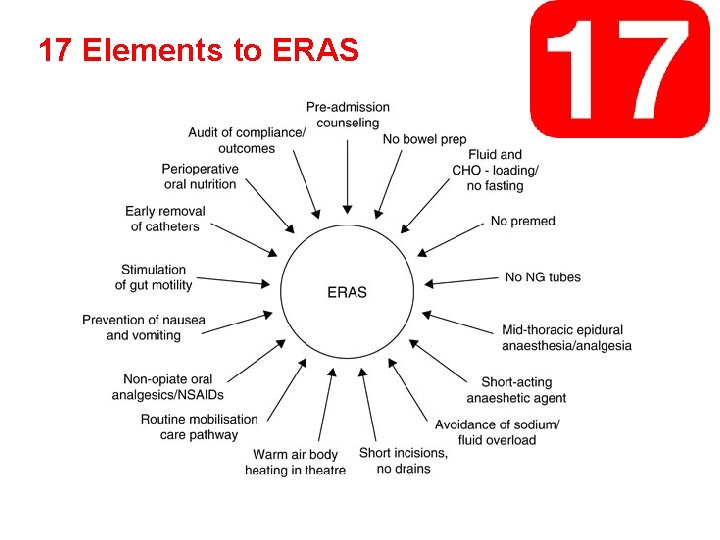
17 Elements to ERAS
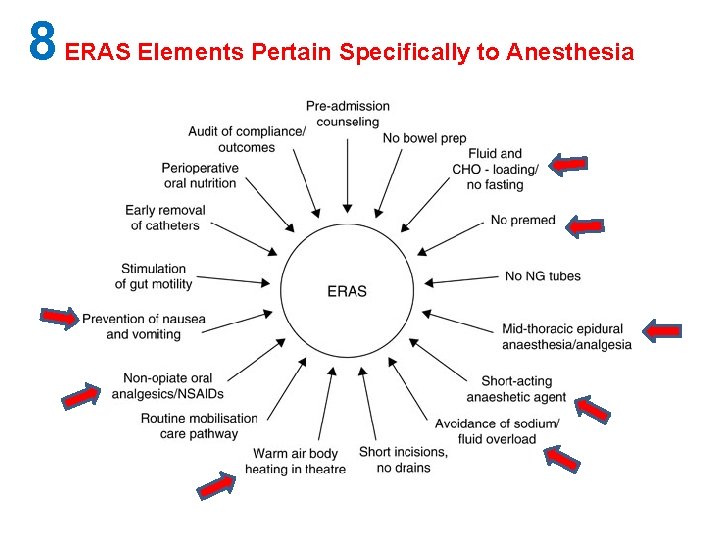
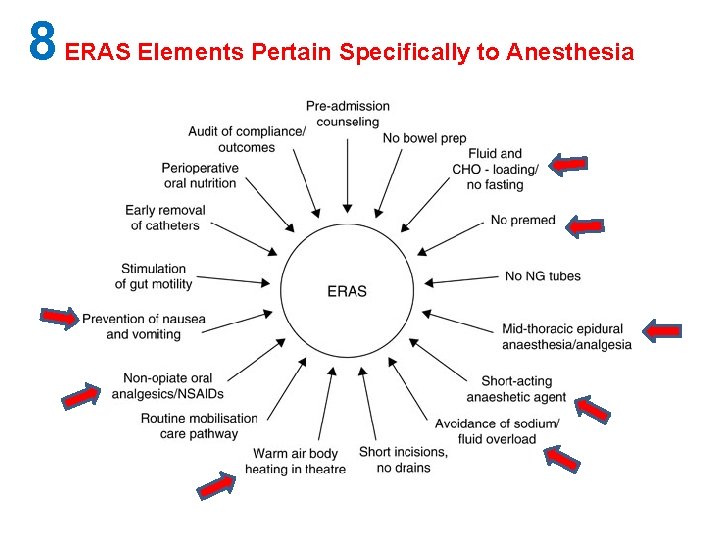
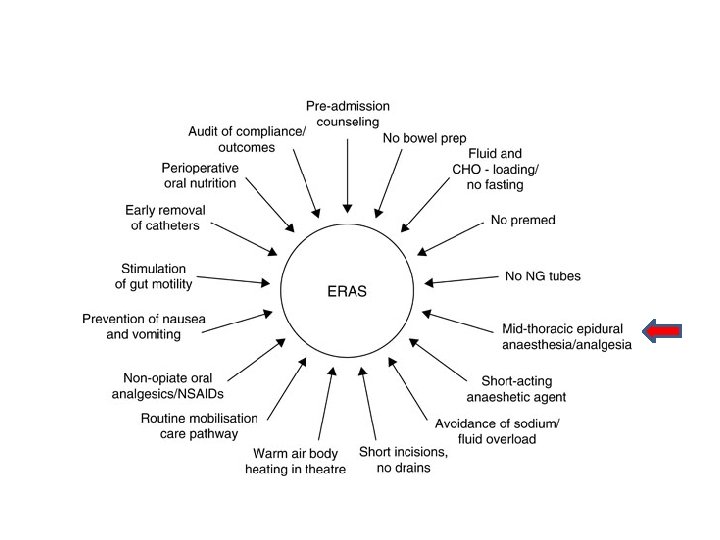
8 ERAS Elements Pertain Specifically to Anesthesia

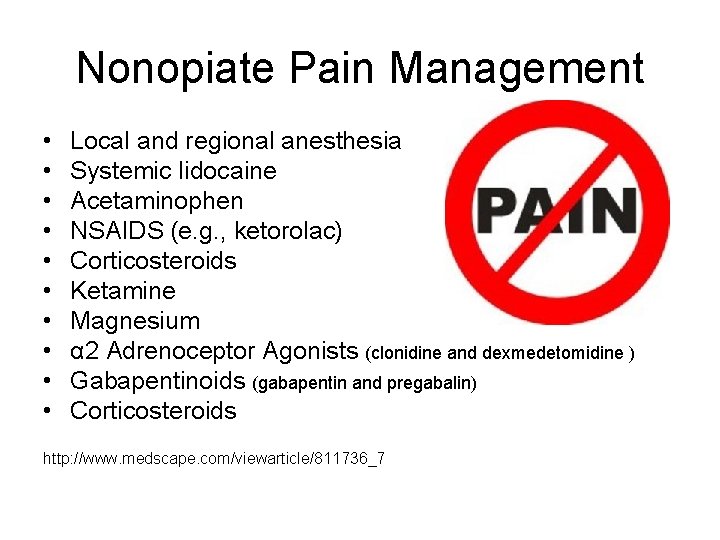
Nonopiate Pain Management • • • Local and regional anesthesia Systemic lidocaine Acetaminophen NSAIDS (e. g. , ketorolac) Corticosteroids Ketamine Magnesium α 2 Adrenoceptor Agonists (clonidine and dexmedetomidine ) Gabapentinoids (gabapentin and pregabalin) Corticosteroids http: //www. medscape. com/viewarticle/811736_7

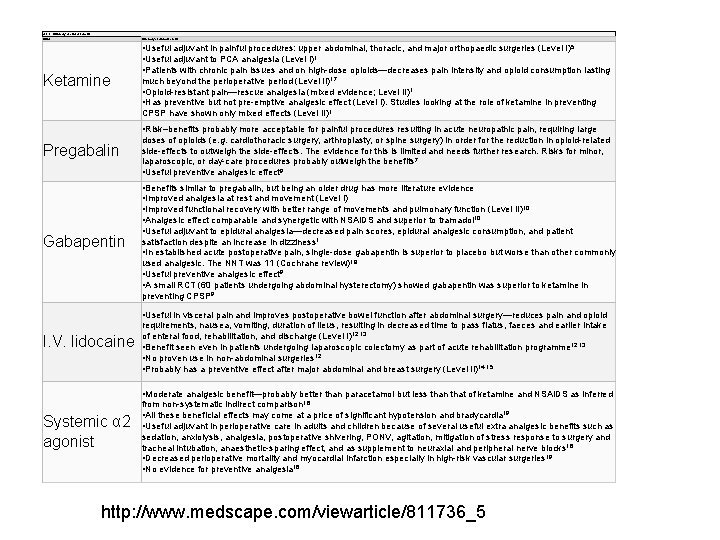
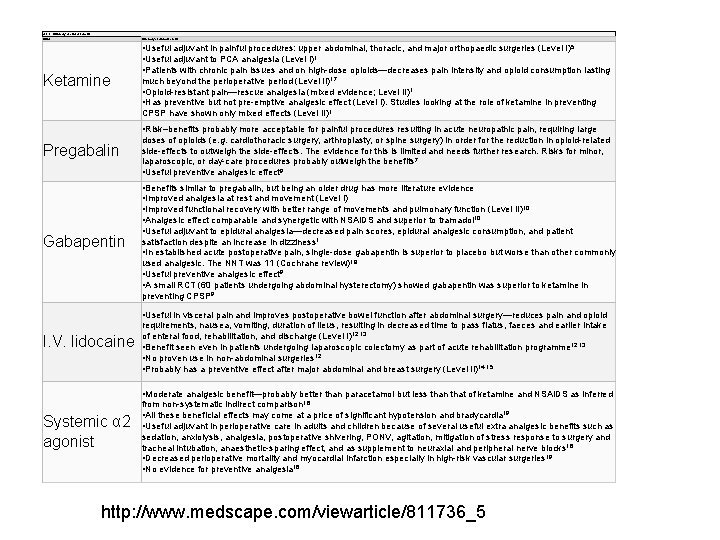
able 2. Summary of clinical benefits Drug Summary of clinical benefits Ketamine • Useful adjuvant in painful procedures: upper abdominal, thoracic, and major orthopaedic surgeries (Level I)5 • Useful adjuvant to PCA analgesia (Level I)1 • Patients with chronic pain issues and on high-dose opioids—decreases pain intensity and opioid consumption lasting much beyond the perioperative period (Level II)17 • Opioid-resistant pain—rescue analgesia (mixed evidence; Level II)1 • Has preventive but not pre-emptive analgesic effect (Level I). Studies looking at the role of ketamine in preventing CPSP have shown only mixed effects (Level II)1 • Risk–benefits probably more acceptable for painful procedures resulting in acute neuropathic pain, requiring large Pregabalin Gabapentin doses of opioids (e. g. cardiothoracic surgery, arthroplasty, or spine surgery) in order for the reduction in opioid-related side-effects to outweigh the side-effects. The evidence for this is limited and needs further research. Risks for minor, laparoscopic, or day-care procedures probably outweigh the benefits 7 • Useful preventive analgesic effect 9 • Benefits similar to pregabalin, but being an older drug has more literature evidence • Improved analgesia at rest and movement (Level I) • Improved functional recovery with better range of movements and pulmonary function (Level II)10 • Analgesic effect comparable and synergetic with NSAIDS and superior to tramadol 10 • Useful adjuvant to epidural analgesia—decreased pain scores, epidural analgesic consumption, and patient satisfaction despite an increase in dizziness 1 • In established acute postoperative pain, single-dose gabapentin is superior to placebo but worse than other commonly used analgesic. The NNT was 11 (Cochrane review)18 • Useful preventive analgesic effect 9 • A small RCT (60 patients undergoing abdominal hysterectomy) showed gabapentin was superior to ketamine in preventing CPSP 9 • Useful in visceral pain and improves postoperative bowel function after abdominal surgery—reduces pain and opioid I. V. lidocaine requirements, nausea, vomiting, duration of ileus, resulting in decreased time to pass flatus, faeces and earlier intake of enteral food, rehabilitation, and discharge (Level I)12, 13 • Benefit seen even in patients undergoing laparoscopic colectomy as part of acute rehabilitation programme 12, 13 • No proven use in non-abdominal surgeries 12 • Probably has a preventive effect after major abdominal and breast surgery (Level II)14, 15 • Moderate analgesic benefit—probably better than paracetamol but less than that of ketamine and NSAIDS as inferred Systemic α 2 agonist from non-systematic indirect comparison 16 • All these beneficial effects may come at a price of significant hypotension and bradycardia 19 • Useful adjuvant in perioperative care in adults and children because of several useful extra analgesic benefits such as sedation, anxiolysis, analgesia, postoperative shivering, PONV, agitation, mitigation of stress response to surgery and tracheal intubation, anaesthetic-sparing effect, and as supplement to neuraxial and peripheral nerve blocks 16 • Decreased perioperative mortality and myocardial infarction especially in high-risk vascular surgeries 19 • No evidence for preventive analgesia 16 http: //www. medscape. com/viewarticle/811736_5
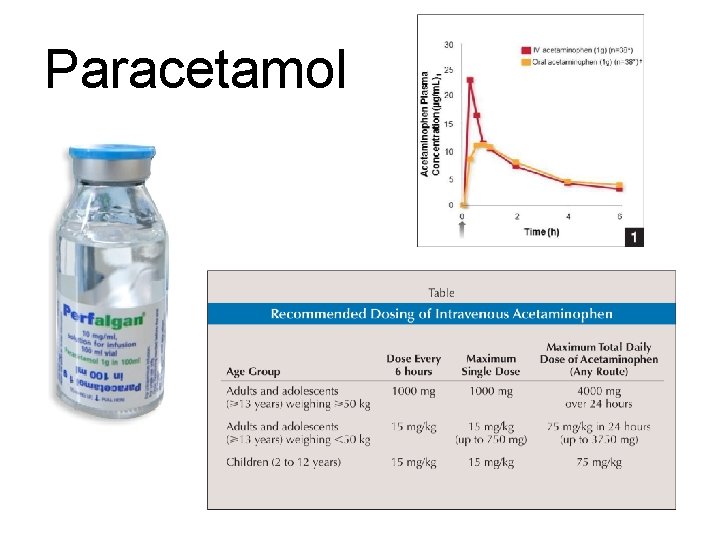
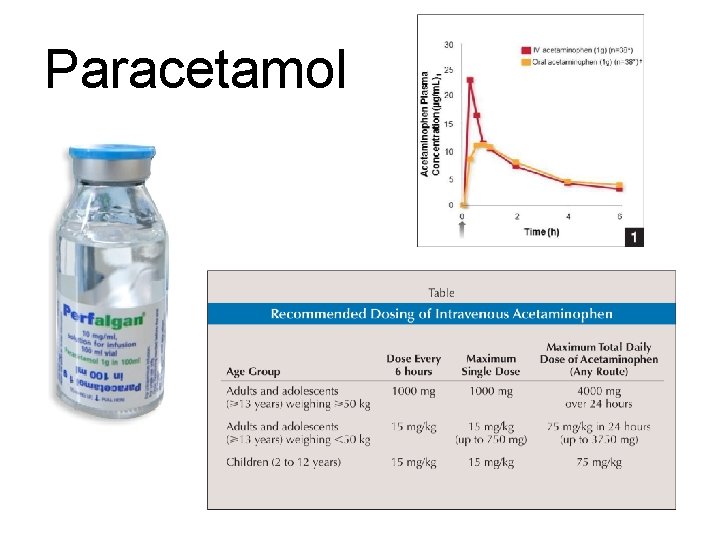
Paracetamol

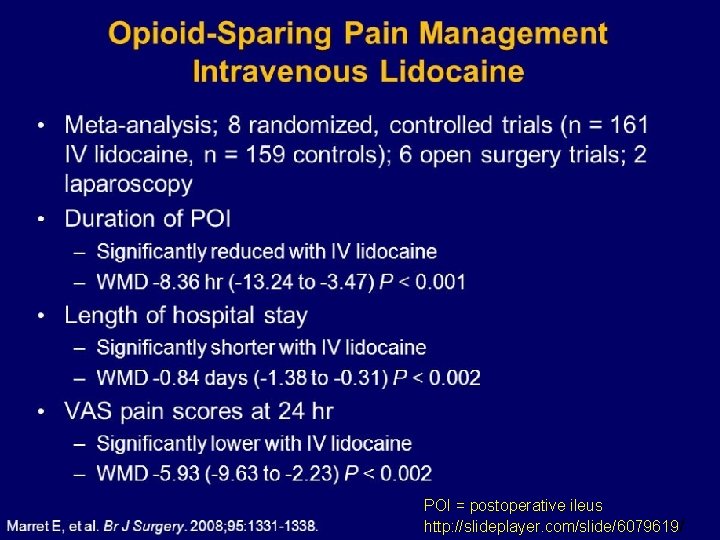
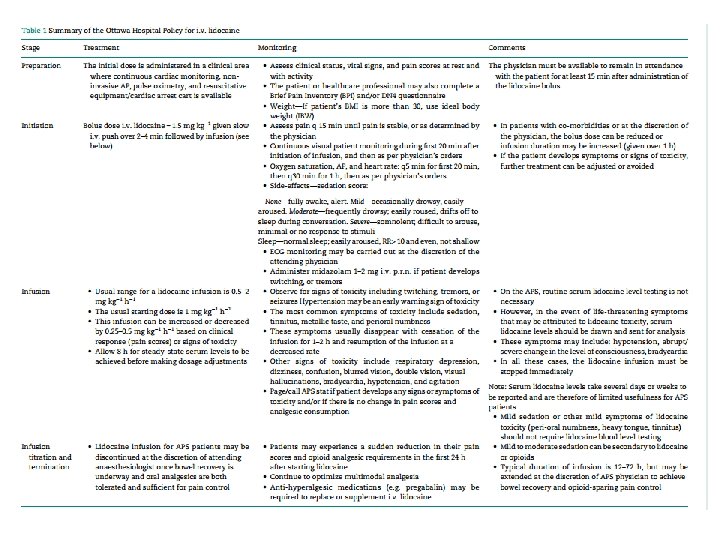
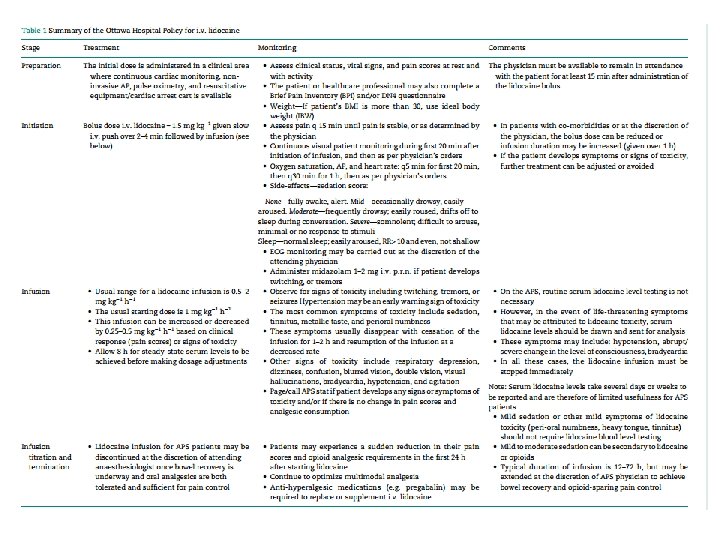
Lidocaine Recent literature suggests that an adjunctive intraoperative lidocaine infusion (100 mg intravenously prior to incision and then 1‐ 2 mg/kg/hour ) aids in patient recovery after surgery, presumably as a result of its newly discovered antiinflammatory properties.
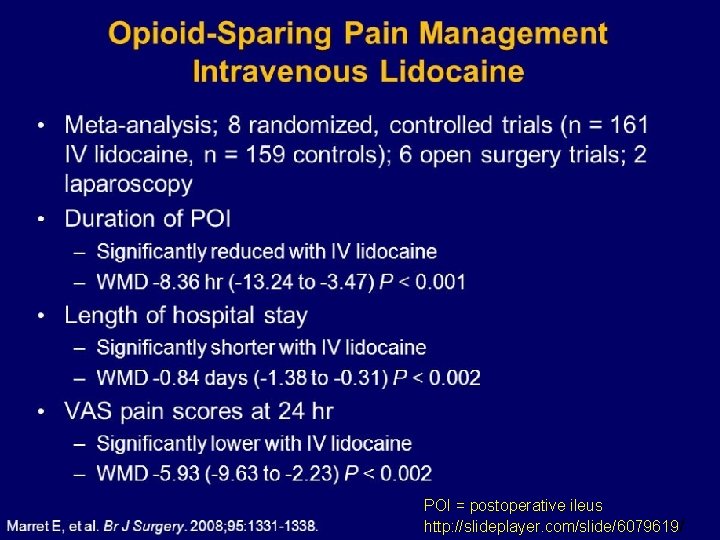
POI = postoperative ileus http: //slideplayer. com/slide/6079619/
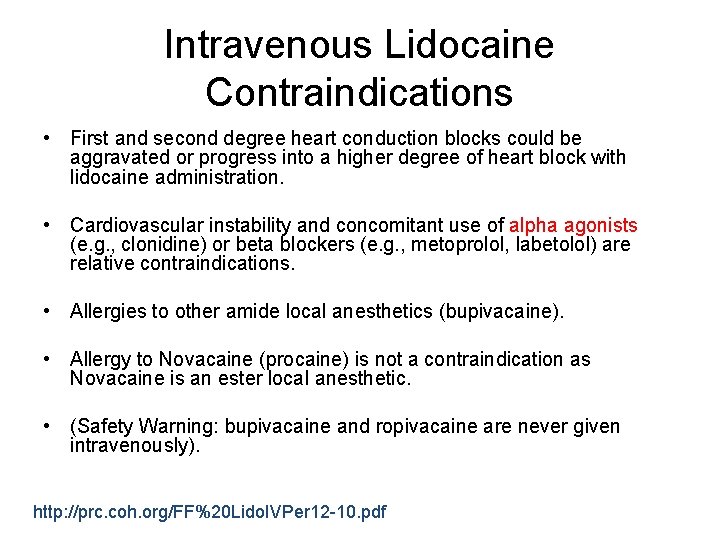
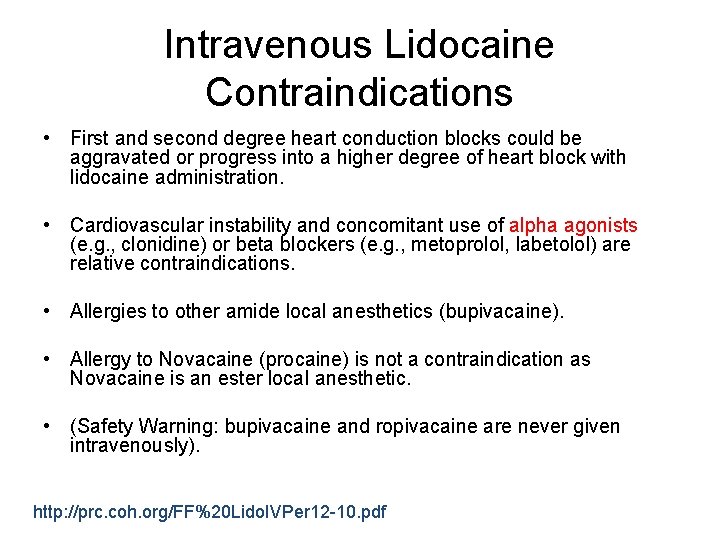
Intravenous Lidocaine Contraindications • First and second degree heart conduction blocks could be aggravated or progress into a higher degree of heart block with lidocaine administration. • Cardiovascular instability and concomitant use of alpha agonists (e. g. , clonidine) or beta blockers (e. g. , metoprolol, labetolol) are relative contraindications. • Allergies to other amide local anesthetics (bupivacaine). • Allergy to Novacaine (procaine) is not a contraindication as Novacaine is an ester local anesthetic. • (Safety Warning: bupivacaine and ropivacaine are never given intravenously). http: //prc. coh. org/FF%20 Lido. IVPer 12 -10. pdf

Intravenous Lidocaine Contraindications Unstable coronary disease Recent MI Heart failure Heart block Electrolyte disturbances Liver disease Cardiac arrhythmia disorders Seizure disorders https: //www. mc. vanderbilt. edu/documents/periopservices/files/ Lidocaine%20 Infusion%20 PP%20 for%20 HR-PACU. pdf
May One Give a Lidocaine Infusion on a General Care Floor? Must be approved by the Pharmacy and Therapeutics Committee (similar issue for ketamine). IV lipid emulsion (20%) therapy should be available (lipidrescue. org).
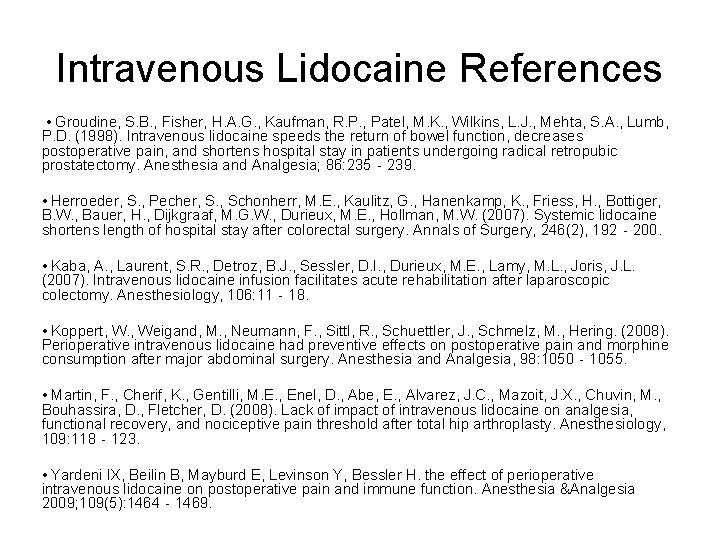
Intravenous Lidocaine References • Groudine, S. B. , Fisher, H. A. G. , Kaufman, R. P. , Patel, M. K. , Wilkins, L. J. , Mehta, S. A. , Lumb, P. D. (1998). Intravenous lidocaine speeds the return of bowel function, decreases postoperative pain, and shortens hospital stay in patients undergoing radical retropubic prostatectomy. Anesthesia and Analgesia; 86: 235‐ 239. • Herroeder, S. , Pecher, S. , Schonherr, M. E. , Kaulitz, G. , Hanenkamp, K. , Friess, H. , Bottiger, B. W. , Bauer, H. , Dijkgraaf, M. G. W. , Durieux, M. E. , Hollman, M. W. (2007). Systemic lidocaine shortens length of hospital stay after colorectal surgery. Annals of Surgery, 246(2), 192‐ 200. • Kaba, A. , Laurent, S. R. , Detroz, B. J. , Sessler, D. I. , Durieux, M. E. , Lamy, M. L. , Joris, J. L. (2007). Intravenous lidocaine infusion facilitates acute rehabilitation after laparoscopic colectomy. Anesthesiology, 106: 11‐ 18. • Koppert, W. , Weigand, M. , Neumann, F. , Sittl, R. , Schuettler, J. , Schmelz, M. , Hering. (2008). Perioperative intravenous lidocaine had preventive effects on postoperative pain and morphine consumption after major abdominal surgery. Anesthesia and Analgesia, 98: 1050‐ 1055. • Martin, F. , Cherif, K. , Gentilli, M. E. , Enel, D. , Abe, E. , Alvarez, J. C. , Mazoit, J. X. , Chuvin, M. , Bouhassira, D. , Fletcher, D. (2008). Lack of impact of intravenous lidocaine on analgesia, functional recovery, and nociceptive pain threshold after total hip arthroplasty. Anesthesiology, 109: 118‐ 123. • Yardeni IX, Beilin B, Mayburd E, Levinson Y, Bessler H. the effect of perioperative intravenous lidocaine on postoperative pain and immune function. Anesthesia &Analgesia 2009; 109(5): 1464‐ 1469.
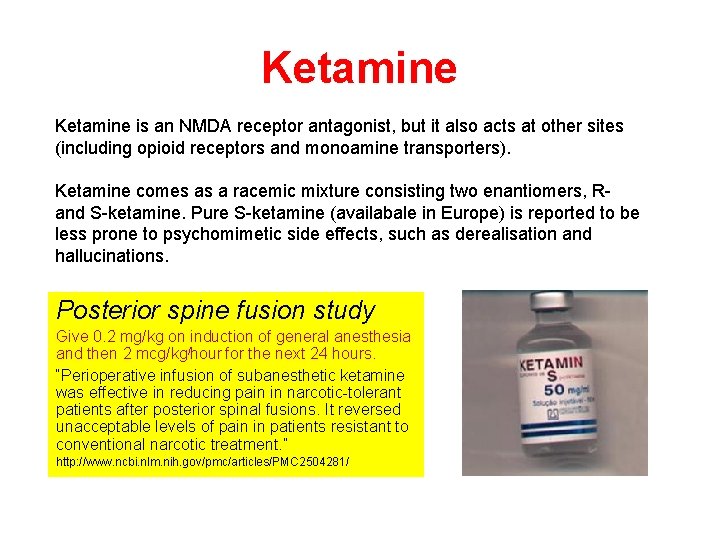
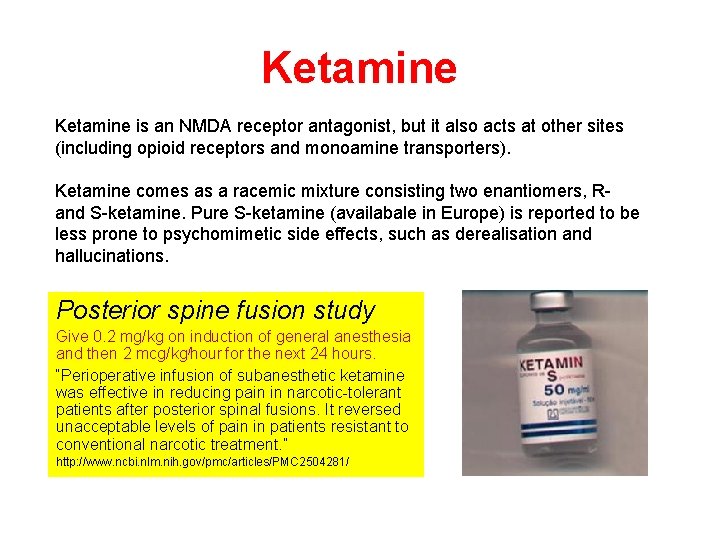
Ketamine is an NMDA receptor antagonist, but it also acts at other sites (including opioid receptors and monoamine transporters). Ketamine comes as a racemic mixture consisting two enantiomers, R- and S-ketamine. Pure S-ketamine (availabale in Europe) is reported to be less prone to psychomimetic side effects, such as derealisation and hallucinations. Posterior spine fusion study Give 0. 2 mg/kg on induction of general anesthesia and then 2 mcg/kg/hour for the next 24 hours. “Perioperative infusion of subanesthetic ketamine was effective in reducing pain in narcotic-tolerant patients after posterior spinal fusions. It reversed unacceptable levels of pain in patients resistant to conventional narcotic treatment. ” http: //www. ncbi. nlm. nih. gov/pmc/articles/PMC 2504281/
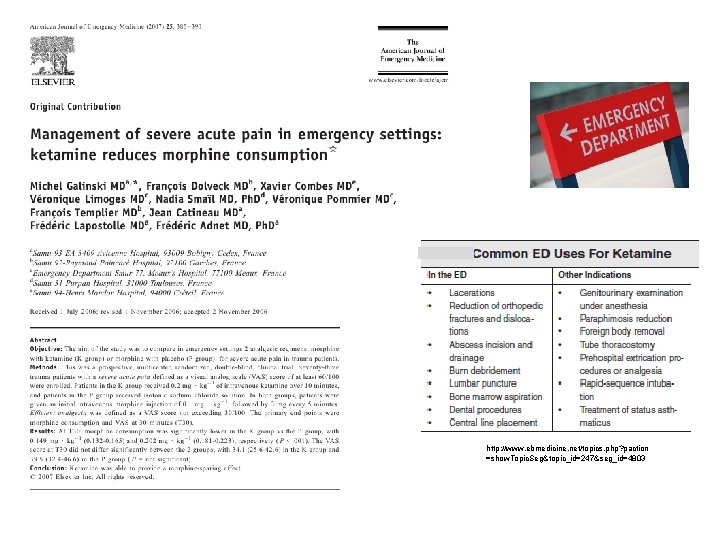
http: //www. ebmedicine. net/topics. php? paction =show. Topic. Seg&topic_id=247&seg_id=4803


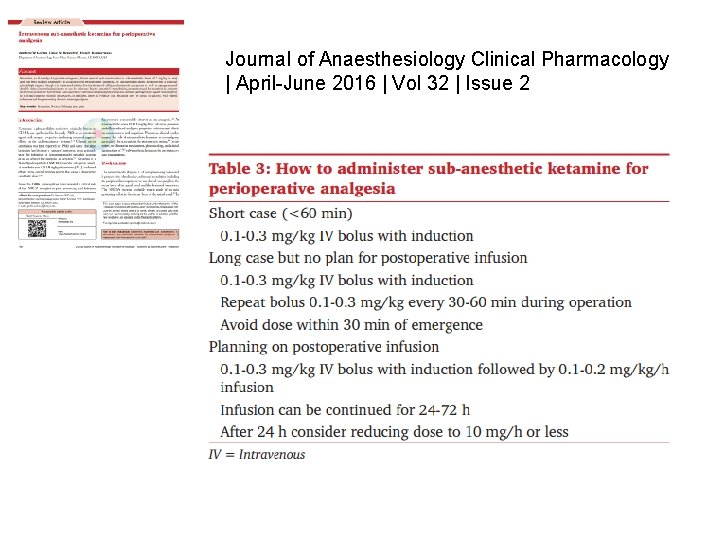
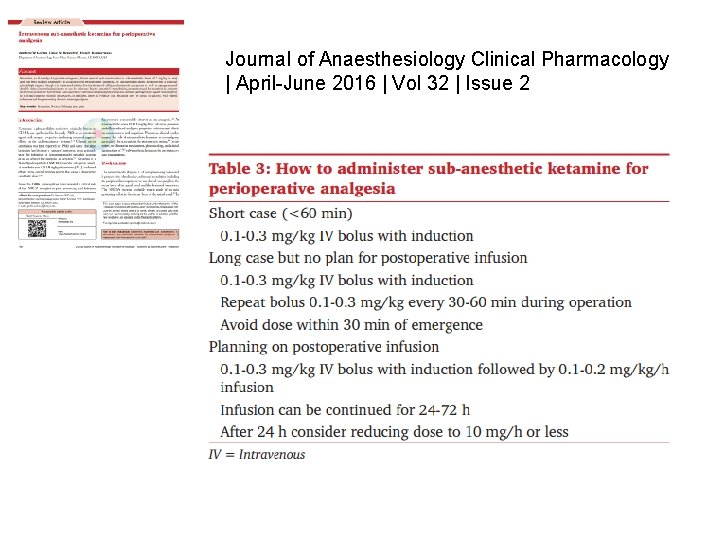
Journal of Anaesthesiology Clinical Pharmacology | April-June 2016 | Vol 32 | Issue 2
Therapy For Depression And Chronic Pain
3 -Day Ketamine Treatment for Complex Regional Pain Syndrome https: //www. youtube. com/watch? v=IGqo 5 NBr_xw https: //www. youtube. com/watch? v=pii. Bg 1 K-bm 0 Rapid Relief from Treatment Resistant Depression with Oral Ketamine https: //www. youtube. com/watch? v=7 A 26 mi. Rl. YBc
Gabapentin and Pregabalin “Gabapentinoids mainly act on the α-2 -δ-1 subunit of pre-synpatic calcium channels and inhibit neuronal calcium influx. This results in a reduction in the release of excitatory neurotransmitters such as glutamate, substance P, and calcitonin gene -related peptide from primary afferent nerve fibres thus suppressing neuronal excitability after nerve or tissue injury. ” http: //www. medscape. com/viewarticle/811736_3
Magnesium Systemic administration of perioperative magnesium reduces postoperative pain and opioid consumption. De Oliveira GS Jr, Castro-Alves LJ, Khan JH, Mc. Carthy RJ. Perioperative systemic magnesium to minimize postoperative pain: a meta-analysis of randomized controlled trials. Anesthesiology. 2013 Jul; 119(1): 17890.

Dexamethasone Single dose IV dexamethasone at doses over 0. 1 mg/kg is an effective adjunct to reduce postoperative pain and opioid consumption after surgery. De Oliveira GS Jr, Almeida MD, Benzon HT, Mc. Carthy RJ. Perioperative single dose systemic dexamethasone for postoperative pain: a meta-analysis of randomized controlled trials. Anesthesiology. 2011 Sep; 115(3): 575 -88.
“In summary, we found that perioperative singledose dexamethasone was associated with small but statistically significant reductions in postoperative pain, postoperative opioid consumption, need for rescue analgesia, PACU stays, and a longer time to first analgesic dose. The effect on postoperative opioid consumption was not dose-dependent. In addition, we found no increased risk of infection or delayed wound healing, although dexamethasone was associated with slight hyperglycaemia on the first postoperative day. ”
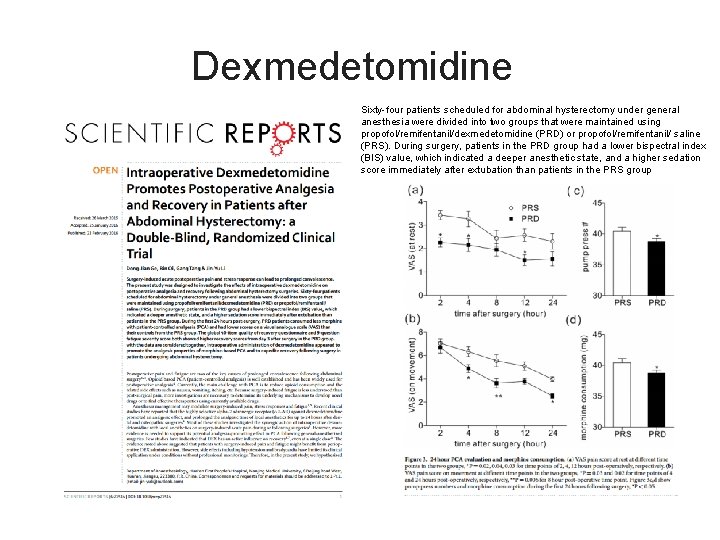
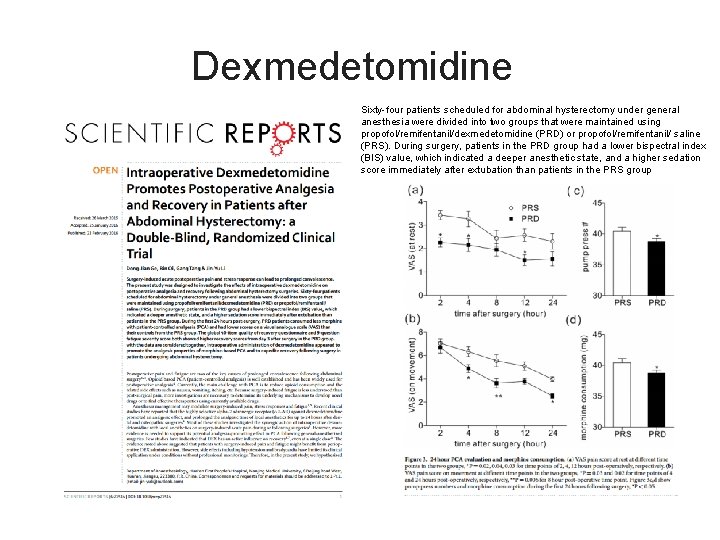
Dexmedetomidine Sixty-four patients scheduled for abdominal hysterectomy under general anesthesia were divided into two groups that were maintained using propofol/remifentanil/dexmedetomidine (PRD) or propofol/remifentanil/ saline (PRS). During surgery, patients in the PRD group had a lower bispectral index (BIS) value, which indicated a deeper anesthetic state, and a higher sedation score immediately after extubation than patients in the PRS group

 Madpain
Madpain Symptoms before period
Symptoms before period Period cramps vs early pregnancy cramps
Period cramps vs early pregnancy cramps Evelyn doyle ucd
Evelyn doyle ucd Short doyle
Short doyle Short doyle
Short doyle Paul rayley
Paul rayley Sir arthur conan doyle biography
Sir arthur conan doyle biography Wendy doyle
Wendy doyle Adam doyle nhs
Adam doyle nhs Mariane asad doyle
Mariane asad doyle Sherlock holmes is a fictional detective created by
Sherlock holmes is a fictional detective created by Jeremiah doyle
Jeremiah doyle Doyle v white city stadium
Doyle v white city stadium Dissociated meaning
Dissociated meaning Father of forensic serology
Father of forensic serology Doyle mcmanus political affiliation
Doyle mcmanus political affiliation Doyle
Doyle Red headed league setting
Red headed league setting 2016679
2016679 Sir arthur conan doyle cae answers
Sir arthur conan doyle cae answers Celia doyle
Celia doyle Retirement agenda
Retirement agenda 3 phases of perioperative nursing
3 phases of perioperative nursing Definition of perioperative nursing
Definition of perioperative nursing Perioperative case study nursing
Perioperative case study nursing Ccs perioperative guidelines
Ccs perioperative guidelines Site:slidetodoc.com
Site:slidetodoc.com Pain management okc soonercare
Pain management okc soonercare Pico question example
Pico question example Pain management stony brook
Pain management stony brook Iu health pain management
Iu health pain management Chapter 7 nursing management of pain during labor and birth
Chapter 7 nursing management of pain during labor and birth Dr ruben gonzalez-vallina
Dr ruben gonzalez-vallina Fetal descent stations
Fetal descent stations