Operating Room Nurse to Post Anesthesia Care Unit
















- Slides: 19
Operating Room Nurse to Post Anesthesia Care Unit Nurse Handoff: Implementation of a Written SBAR Intervention Erin Long BSN, RN, DNP Student

Acknowledgements v Dr. Kessler v Perioperative Nurses v Family v Classmates

PICOT Question v In perioperative nurses, how will the implementation of a written SBAR Handoff Form affect the content of handoffs between OR and PACU nurses and impact the perceptions of teamwork and patient safety of perioperative nurses over the course of three months when compared to current oral report practice?

Significance of the Background 1. A unique setting subject to particular barriers to communication: v Noise v Interruptions v High rate of patient arrival & discharge 2. A lack of structure during handoff between OR and PACU nurses places surgical patients’ safety at risk as miscommunication is more common when handoff protocol is not standardized (Abraham, Kannampallil & Patel, 2014; Kalkman, 2010; Petrovic, Aboumatar & Scholl et al. , 2014; Petrovic, Martinez & Aboumatar, 2012; Riesenberg, Leitzsch & Cunningham, 2010; Riesenberg, Leitzsch & Little, 2009; The Joint Commission, 2015)

Review of Literature v. Databases: CINAHL, Pro. Quest, Medline (Pub. Med), Medline (Ebsco. HOST), Cochrane Library, & Joanna Briggs Institute v. Keywords: periop*, intraop*, handoff*, handover* v. Inclusion Criteria: v. Peer reviewed v. Scholarly journals v. Articles v. English language v. Published after 2005

Review of Literature v. Appraisal: Critical Appraisal Skills Programme (CASP) & Checklist for Evidence-Based Clinical Practice Guidelines Type Source Systematic Reviews Qualitative Appraisal Score Quantitative Expert Opinions Good Fair X I X X V X V X X VI X X VII X X Single Studies Level (CASP, 2013; Melnyk & Fineout-Overholt, 2011)

Decision to Change Practice 1. Mnemonic Phrase v. Aids nurse memory v. Associated with a handoff checklist 2. Standardized Protocol v. Decreases handoff variability v. Reduces communication errors risking patient safety (Abraham, Kannampallil, & Patel, 2012; Greenberg et al. , 2007; Holly & Poletick, 2013; Kalkman, 2010; Ong & Coiera, 2014; Riesenberg, Leitzsch, & Cunningham, 2010; Riesenberg, Leitzsch & Little, 2009; Petrovic, Aboumatar, & Scholl, 2015)

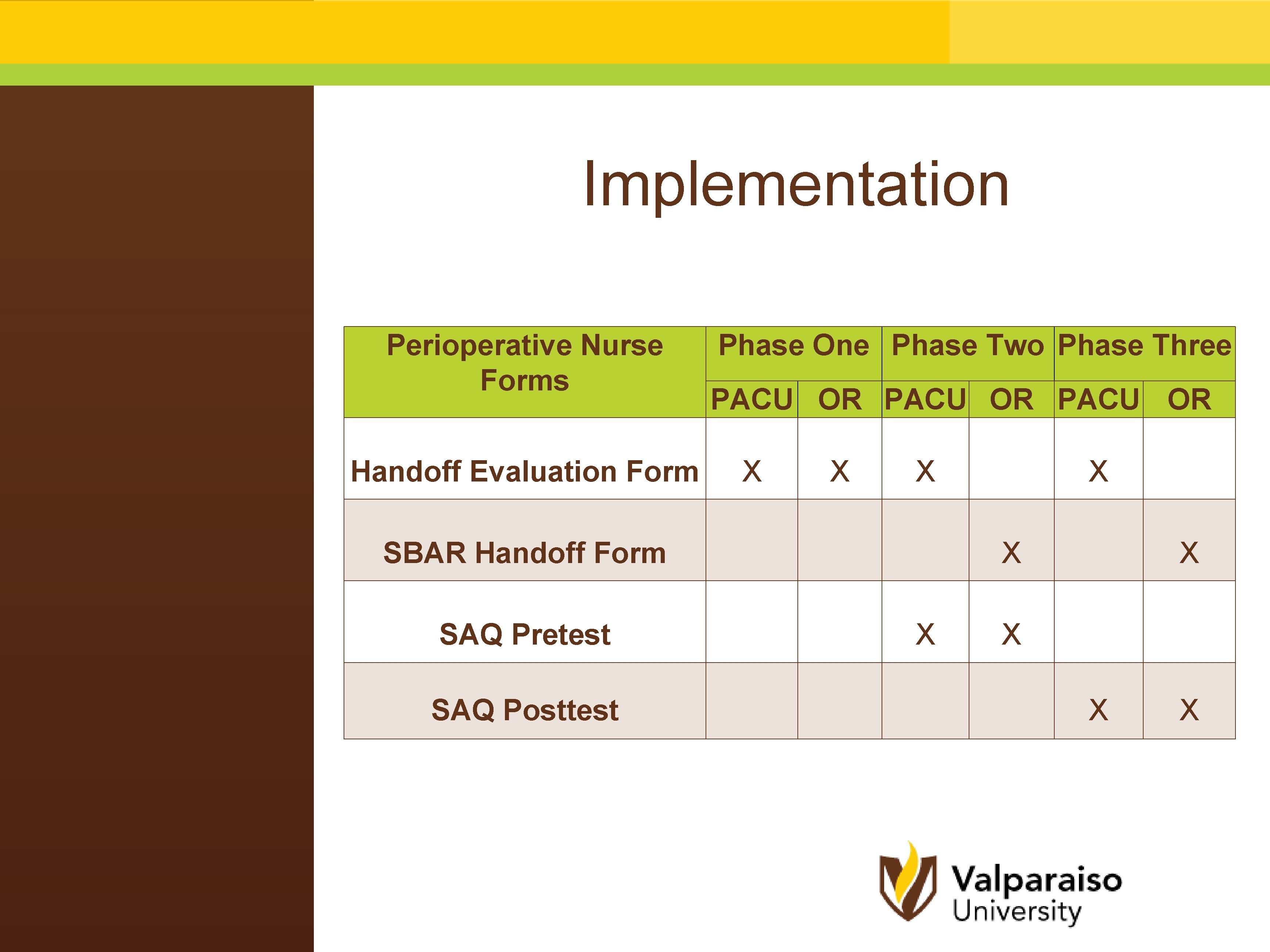
Implementation v. Project Design: Three, two week phases for a project duration of six weeks v. Phase One: v. Handoff Evaluation Form: 1 -page form, measuring 24 items, PACU & OR v Phase Two: v Education Session: Handoff Power. Point ® during staff meeting v Safety Attitudes Questionnaire (SAQ) Pretest: 36 safety items v Demographic Data v Handoff Evaluation Form: 1 -page form, measuring 24 items, PACU v. SBAR Handoff form: 1 -page form, measuring 24 items, OR v Phase Three: v Handoff Evaluation Form: 1 -page form, measuring 24 items, PACU v. SBAR Handoff form: 1 -page form, measuring 24 items, OR v Safety Attitudes Questionnaire (SAQ) Posttest v MIDAS Report Audit: risk report audit to measure change to patient safety
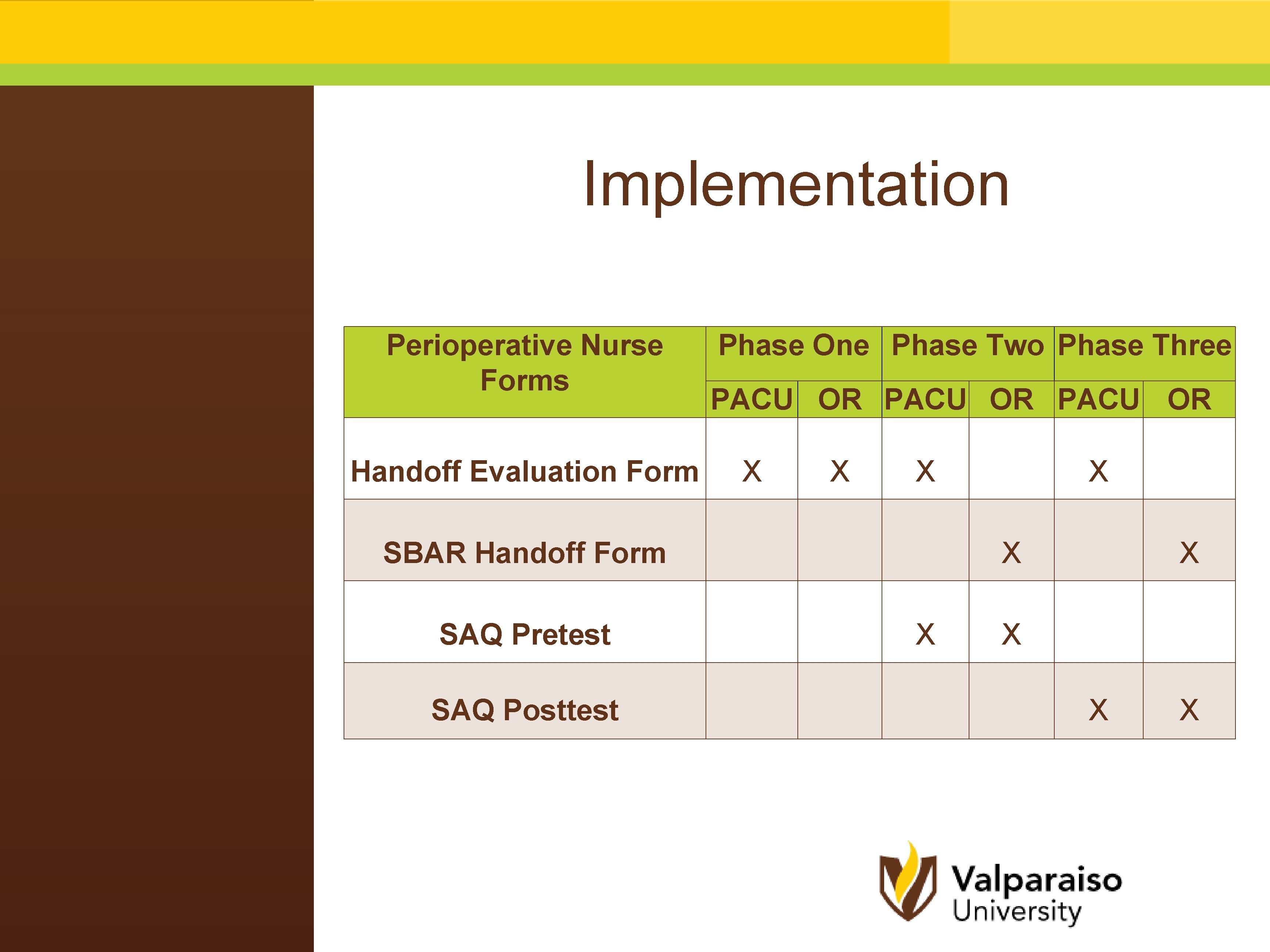
Implementation Perioperative Nurse Forms Phase One Phase Two Phase Three PACU OR Handoff Evaluation Form X X SBAR Handoff Form SAQ Pretest SAQ Posttest X X X

Data Analysis SBAR Handoff Form Outcomes: Inclusion of 24 handoff items Measure: Individual items & total score Statistical Tests: Frequencies, Mean Scores, & Independent-Samples t Test Significance: v Frequencies: no significant changes in the reporting of individual items v Mean Scores: decreased from phase two to phase three v Independent-Samples t Test: 1 statistically significant item (Implants)

Data Evaluation SBAR Handoff Form Phase Three Phase Two Statistical Significance Frequencies No Significant items across Phases Two-Three Mean Scores (M = 12. 38, SD = 3. 69) (M = 11. 5, SD = 3. 48) (t(82) = 1. 81, p = 0. 241) Independent-Samples t Test Items Implants Result (M = 0. 92, SD = 0. 28) (M = 0. 57, SD = 0. 51) (t(25) = 2. 19, p < 0. 038)

Data Analysis Handoff Evaluation Form Outcomes: Inclusion of 24 handoff items Measure: Individual items & total score Statistical Tests: Frequencies, Mean Scores, Independent-Samples t Test, Paired-Samples t Test & ANOVA Significance: v Frequencies: no significant changes in the reporting of individual items v Mean Scores: PACU > OR (phase one), PACU scores decreased from phase two-three v Independent-Samples t Test: 3 statistically significant items (NPO, Skin, Shift) v Paired-Samples t Test: 3 statistically significant items (NPO, Skin, Shift) v ANOVA: not significant for PACU mean scores or for PACU Handoff Evaluation forms from all three phases

Data Evaluation Handoff Evaluation Form Phase One Phase Two Phase Three Frequencies No Significant items across Phases One-Three Mean Scores PACU (M = 8. 14, SD = 3. 2) PACU (M = 8. 31, SD = 3. 4) PACU (M = 7. 57, SD = 3. 25) OR (M = 8. 87, SD = 4. 15) Phase One Paired-Samples t Test OR SBAR Handoff & PACU Handoff Evaluation Independent-Samples t Test Result Item Result NPO Skin Shift PACU (M = 2. 71, SD = 0. 46) NPO PACU (M = 2. 71, SD =. 46) OR (M = 1. 5, SD = 0. 86) OR (M = 1. 50, SD = 0. 86) (t(41) =7. 51, p < 0. 00) (t(82) = 8. 061, p = 0. 00) PACU (M = 2. 98, SD =. 15) OR (M = 2. 62, SD = 0. 76) (t(82) = -2. 97, p = 0. 004) PACU (M = 1. 24, SD =. 62) OR (M = 1. 02, SD = 0. 15) (t(82) = 2. 18, p = 0. 032) PACU (M = 2. 98, SD = 0. 15) OR (M = 2. 62, SD = 0. 77) (t(41) = 2. 93, p < 0. 006) PACU (M = 1. 24, SD = 0. 62) OR (M =1. 02, SD = 0. 15) (t(41) = 0. 04, p < 0. 037) PACU Handoff Evaluation Form PACU Mean Scores Skin Shift ANOVA No Significant Results (No Post Hoc Testing) No Significant Results (F(66, 68) =. 21, p =. 81)

Data Analysis Safety Assessment Questionnaire (SAQ) Outcomes: 36 items scoring perioperative nurse perceptions of teamwork, safety, job satisfaction, stress recognition, perception of management, and working conditions Measure: Likert Scale & 6 Subsections Total Score (%) Statistical Testing: Independent & Paired-Samples t Tests Significance: Independent-Samples t Test showed 4 significant items (Ask Questions, Good Job B, Problem Personnel B, & Timely Info B) & Paired-Samples t Test showed eight significant items (Family, Daily Efforts B, Compromise Patient Safety B, Good Job B, Problem Personnel B, Timely Info B, Level of Staffing, and Communication Breakdowns) v Teamwork & Patient Safety Scores: not significantly different

Data Evaluation SAQ Pretest Independent-Samples t Test Results Item OR (M = 2. 70, SD = 1. 16) Ask Questions PACU (M = 3. 86, SD = 1. 07) (t(15) = -2. 14, p = 0. 050) OR (M = 2. 20, SD = 1. 87) Good Job B PACU (M = 4. 29, SD = 0. 95) (t(15) = -2. 69, p = 0. 017) OR (M = 1. 20, SD = 1. 03) Problem PACU (M = 3. 57, SD = 0. 79) Personnel B (t(15) = -5. 11, p = 0. 000) OR (M = 2. 0, SD = 1. 69) Timely Info B PACU (M = 4. 0, SD = 0. 82) (t(15) = -2. 87, p = 0. 012) Posttest Independent-Samples t Test Results Item OR (M = 4. 43, SD = 0. 79) Family PACU (M = 3. 00, SD =. 71) (t(10) = 3. 227, p = 0. 009) OR (M = 2. 86, SD = 1. 46) Daily Efforts B PACU (M =. 00, SD =. 00) (t(10) = 4. 03, p = 0. 002) OR (M = 3. 57, SD = 1. 81) Compromise PACU (M =. 00, SD =. 00) Patient Safety B (t(10) = 4. 34, p = 0. 001) OR (M = 3. 29, SD = 1. 70) Good Job B PACU (M =. 00, SD =. 00) (t(10) = 4. 25, p = 0. 002) OR (M = 2. 00, SD = 1. 63) Problem PACU (M =. 00, SD =. 00) Personnel B (t(10) = 2. 70, p = 0. 022) OR (M = 3. 00, SD = 1. 53) Timely Info B PACU (M =. 00, SD =. 00) (t(10) = 4. 33, p = 0. 001) OR (M = 3. 14, SD = 1. 07) Level of Staffing PACU (M = 1. 60, SD =. 89) (t(10) = 2. 63, p = 0. 025) OR (M = 2. 71, SD = 0. 76) Communication PACU (M = 1. 40, SD = 1. 14) Breakdowns (t(10) = 2. 42, p = 0. 036) Pretest & Posttest Paired-Samples t Test Item Results pretest (M = 4. 58, SD = 0. 67) Support posttest (M = 3. 92, SD = 0. 90) (t(11) = 2. 60, p = 0. 025)

Data Analysis & Evaluation MIDAS Risk Report Audit Outcomes: process used by perioperative nurses to file risk reports Measure: the number of reports filed 4 weeks prior to intervention were compared to the number of reports filed 4 weeks after the education session Statistical Tests: No testing required Significance: No change in reported events pertaining to perioperative patient safety MIDAS Report Audit Before Education Session After Education Session 0 0
Recommendations v. Literature supports the use of a mnemonic phrase and standardized handoff protocol during nurse handoff to reduce risks to patient safety v. Repeat the project during a time when fewer changes are happening simultaneously v. Repeat project over a longer period of time

Conclusions v. Implementation of a written SBAR Handoff form was not successful in standardizing perioperative nurse Handoff from the OR to the PACU v. SBAR Handoff Forms: Mean scores decreased from Phase Two. Three and the Implants item decreased in handoff inclusion v. Handoff Evaluation Forms: Phases One-Two revealed promising trends in mean scores, but overall project statistical testing showed only 3/24 items improved with the intervention v. SAQ: Perioperative nurse perceptions of Teamwork and Patient Safety showed variations in individual items v. MIDAS Audit: No change in nurse reported patient safety events

References Abraham, J. , Kannampallil, T. , & Patel, V. (2014). A systematic review of the literature on the evaluation of handoff tools: Implications for research and practice. Journal of the American Medical Informatics Association, 21, 154 - 162. doi: 10. 1136/amiajnl-2012 -001351 Critical Appraisal Skills Programme (CASP). (2013). Making Sense of the Evidence. Retrieved from http: //www. caspuk. net/ Holly, C. , & Poletick, E. (2013). A systematic review on the transfer of information during nurse transitions in care. Journal of Clinical Nursing, 2387 -2396. doi: 10. 1111/jocn. 12365 Greenberg, C. , Regenbogen, S. , Studdert, D. , Lipsitz, S. , Rogers, S. , Zinner, M. , & Gawande, A. (2007). Patterns of communication breakdowns resulting in injury to surgical patients. The American College of Surgeons, 204(4), 533 -540. doi 10. 1016/j. jamcollsurg. 2007. 010 Kalkman, C. (2010). Handover in the perioperative care process. Current Opinion in Anesthesiology, 23, 749 -753. doi: 10. 1097/ACO. 0 b 013 e 32834 ac. B Melnyk, B. & Fineout-Overholt, E. (2011). Evidence-based practice in nursing and healthcare. Philadelphia, PA: LWW. Ong, M. & Coiera, E. (2011). A systematic review of failures in handoff communication during intrahospital transfers. The Joint Commission Journal of Quality and Patient Safety, 37(6) 274 -284. Petrovic, M. , Aboumatar, H. , Scholl, A. , Krenzischek, D. , Camp, M. , Senger, C. , Chang, T. , Jurdi A. , & Martinez, E. (2014). The perioperative handoff protocol: evaluating impacts on handoff defects and provider satisfaction in adult perianesthesia care units. Journal of Clinical Anesthesia, 27, 111 -119. Petrovic, M. , Martinez E. , & Aboumatar, H. (2012). Implementing a perioperative handoff tool to improve postprocedural patient transfers. The Joint Commission Journal on Quality and Patient Safety, 38(3) 135 -142. Riesenberg, L. , Leitzsch, J. , & Cunningham, J. (2010). Nursing handoffs: A systematic review of the literature. American Journal of Nursing, 110(4), 24 -34. Riesenberg, L. , Leitzsch, J. , & Little, B. (2009). Systematic review of handoff mnemonics literature. American Journal of Medical Quality, 24(3), 196 -202. doi: 10. 1177/1062860609332512 The Joint Commission. (2015). National Patient Safety Goal 2015. Retrieved from http: //www. jointcommission. org/standards_information/npsgs. aspx