OPEN compound FRACTURES Prof M Ngcelwane 1 2013


- Slides: 26
OPEN (compound) FRACTURES Prof. M. Ngcelwane 1 2013
OBJECTIVES • MUST BE ABLE TO DIAGNOSE OPEN FRACTURES • RECOGNIZE THAT THERE MAY BE ASSOCIATED INJURIES • BE ABLE TO CLASSIFY OPEN FRACTURE • PRINCIPLES OF EARLY MANAGEMENT • DEFINITIVE MANAGEMENT • COMPLICATIONS 2
WHAT IS A FRACTURE 3
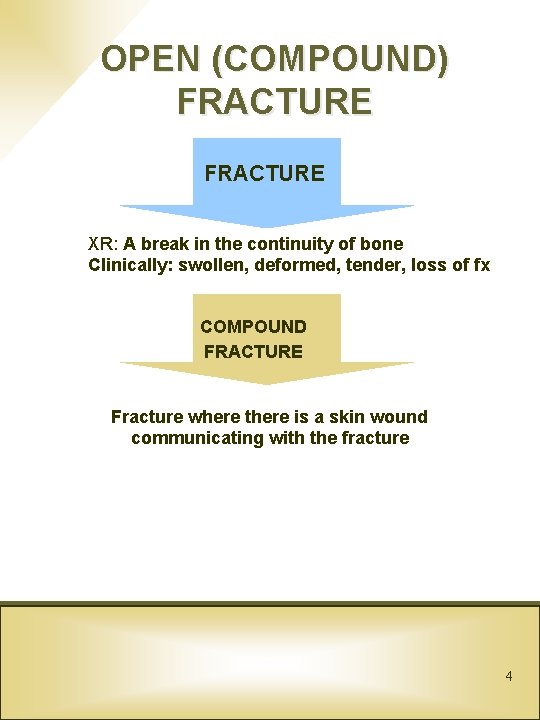
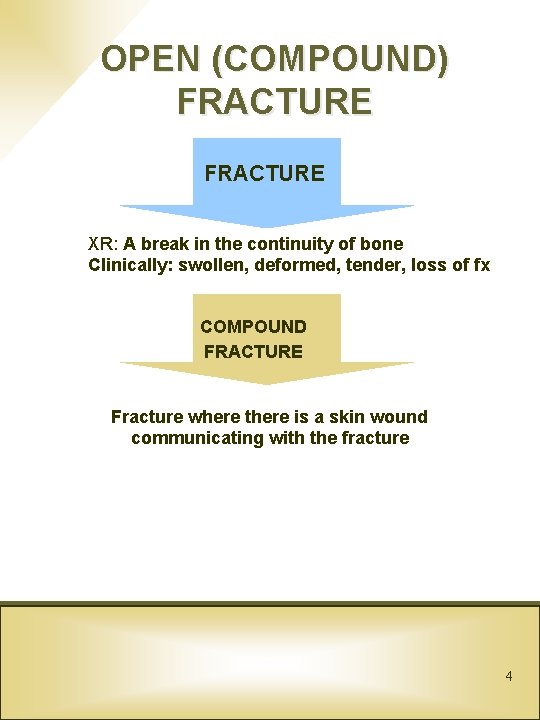
OPEN (COMPOUND) FRACTURE XR: A break in the continuity of bone Clinically: swollen, deformed, tender, loss of fx COMPOUND FRACTURE Fracture where there is a skin wound communicating with the fracture 4

Examples of open fractures 5
IMPORTANCE OF SOFT TISSUES • An open fracture is a severe soft tissue injury in which bone is also broken. • Extent of damage to soft tissue determine the prognosis 6
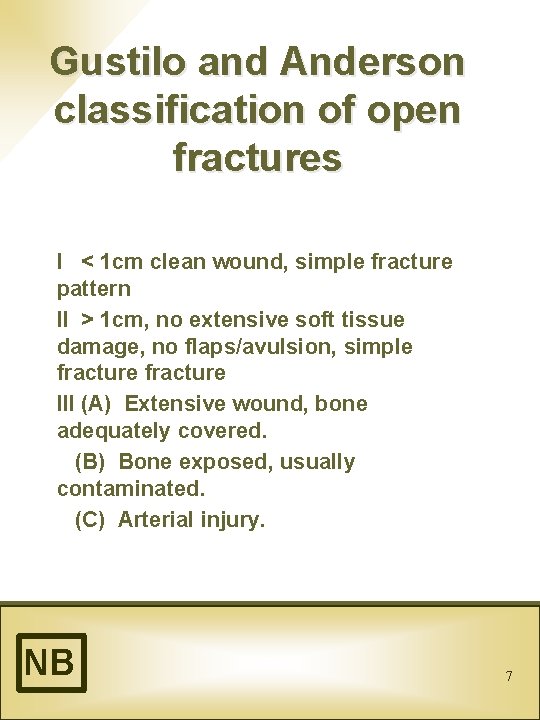
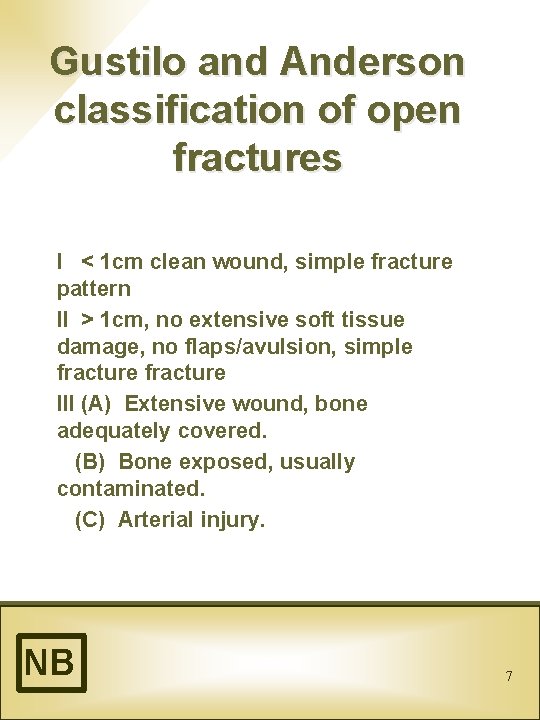
Gustilo and Anderson classification of open fractures I < 1 cm clean wound, simple fracture pattern II > 1 cm, no extensive soft tissue damage, no flaps/avulsion, simple fracture III (A) Extensive wound, bone adequately covered. (B) Bone exposed, usually contaminated. (C) Arterial injury. NB 7
Causes • High energy trauma • Look for other injuries 8
Anatomic considerations • Commonest long bone open fracture is tibia • Most studied bone • Poor soft tissue cover • Cf. femur 9
CLINICAL APPROACH TO PATIENT WITH OPEN FRACTURE 1. 2. Assess life threatening injuries • ABC of resuscitation • Physical and neurologic exam • Emergency Surgery (decision) Assess limb (a) Vasculature pulse doppler angiogram (b) Soft tissues Skin - site - bruising contamination muscles periosteum (c) Neurology Plantar skin sensation 3. NB Fracture pattern XR 10
Neurovascular assessment (tibia) Vascular: - Dorsalis pedis - Posterior tibial Motor: - all compartments of the leg: toe flexures, toe dorsiflexors, ankle evertors, plantar flexors Sensory: - Tibial n: plantar surface of foot - Deep peroneal n: dorsal web space 1 st and 2 nd toe - Superficial peroneal n: dorsolateral - Saphenous n: medial REMEMBER - NOT POSSIBLE IN ALL PATIENTS NB 11

Treatment • MAIN COMPLICATION OF OPEN FRACTURES IS INFECTION 12
Open Tibial Fractures A Open Fractures: Challenges 1. Management of traumatic wound 2. Achieving bony stability 3. Decision making -limb salvage vs. amputation 4. Achieving soft tissue coverage 5. Achieving fracture union 13
PRINCIPLES OF TREATMENT B 1. 2. 3. 4. 5. NB Wound debridement Antibiotic therapy Bony stabilization Wound coverage Maintain vascularization 14
Emergency Room Treatment C 1. 2. 3. 4. 5. 6. 7. 8. 9. Reduce and splint the limb Document neurologic and vascular status (Lavage wound) Sterile compression dressing, do not open again (photograph) Start I/V antibiotics Tetanus prophylaxis X-ray evaluation To surgery as soon as possible < 6 hours 15
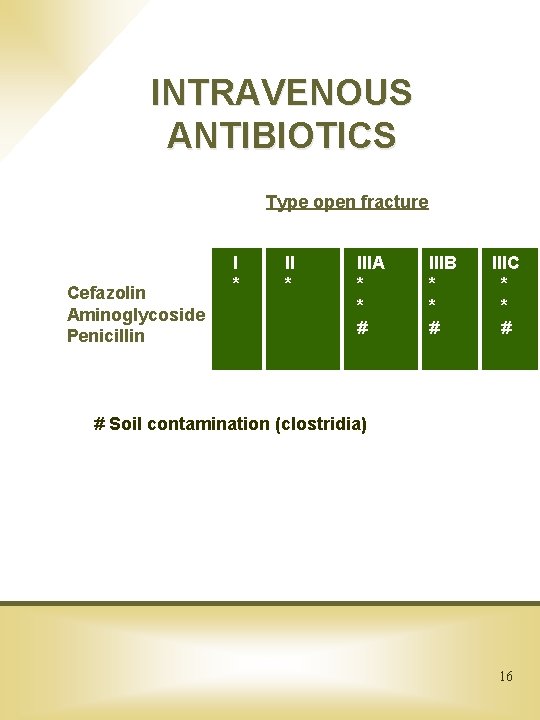
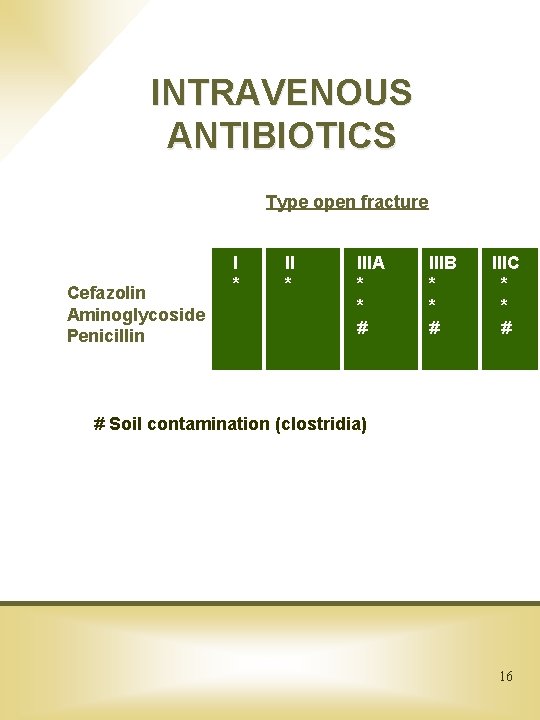
INTRAVENOUS ANTIBIOTICS Type open fracture Cefazolin Aminoglycoside Penicillin I * IIIA * * # IIIB * * # IIIC * * # # Soil contamination (clostridia) 16
MANAGEMENT Limb - specific treatment (a) debride/decontaminate • No tornique • Remove all dead tissue • Save bone (b) (c) (d) (e) Skeletal stabilization Soft tissue cover Bone reconstruction Rehabilitation 17
Sepsis cannot occur if good bleeding tissue is present “The solution to pollution is dilution” 18
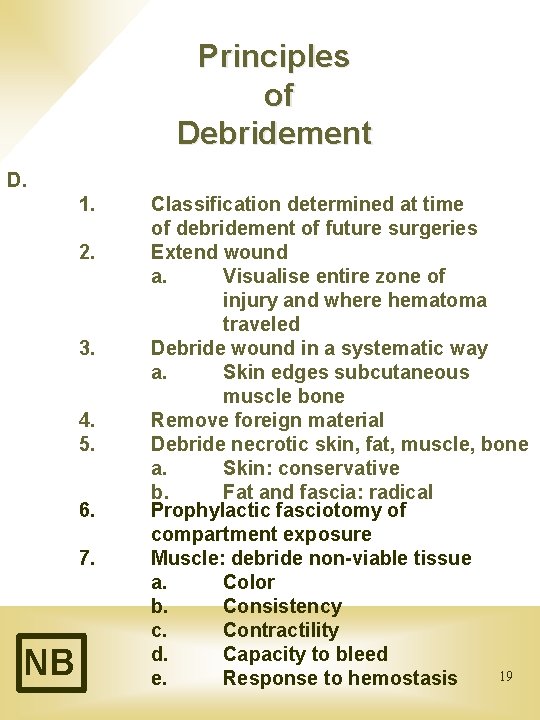
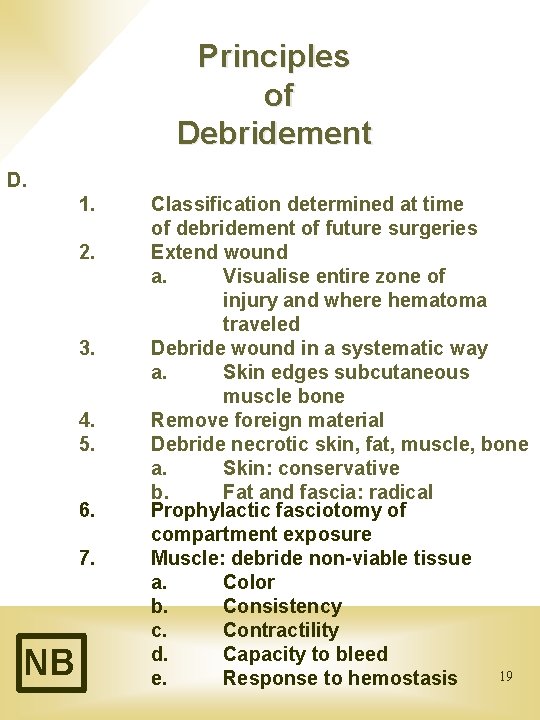
Principles of Debridement D. 1. 2. 3. 4. 5. 6. 7. NB Classification determined at time of debridement of future surgeries Extend wound a. Visualise entire zone of injury and where hematoma traveled Debride wound in a systematic way a. Skin edges subcutaneous muscle bone Remove foreign material Debride necrotic skin, fat, muscle, bone a. Skin: conservative b. Fat and fascia: radical Prophylactic fasciotomy of compartment exposure Muscle: debride non-viable tissue a. Color b. Consistency c. Contractility d. Capacity to bleed 19 e. Response to hemostasis
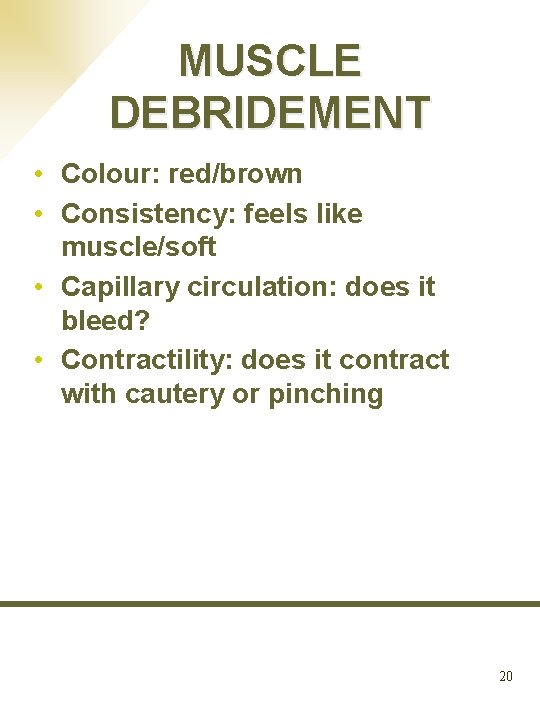
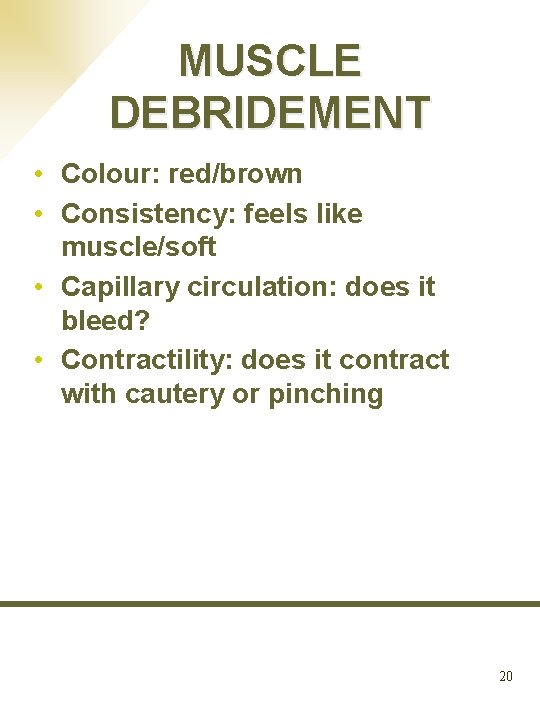
MUSCLE DEBRIDEMENT • Colour: red/brown • Consistency: feels like muscle/soft • Capillary circulation: does it bleed? • Contractility: does it contract with cautery or pinching 20
COVER EXPOSED 9 a b c d Neurovascular structures Tendon Bone Articular surface 21
BONE STABILIZATION • EXTERNAL FIXATOR • Reason: be able to clean/dress wound; difficult to eradicate infection with internal fixation/plate NB 22
COMPLICATIONS • • Neurovascular Compartment syndrome INFECTION (prophylaxis NB!!) Loss of limb NB 23
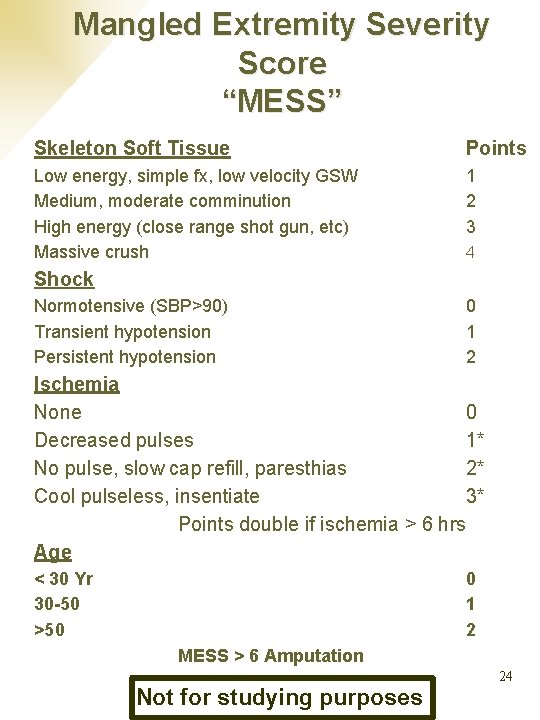
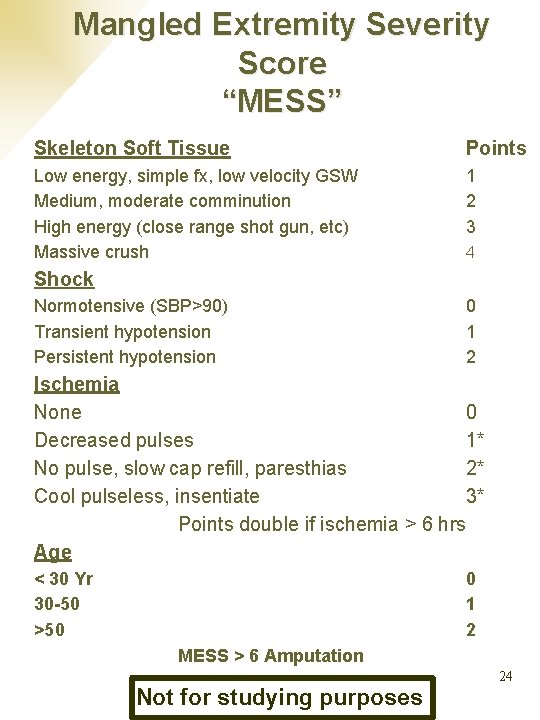
Mangled Extremity Severity Score “MESS” Skeleton Soft Tissue Points Low energy, simple fx, low velocity GSW Medium, moderate comminution High energy (close range shot gun, etc) Massive crush 1 2 3 4 Shock Normotensive (SBP>90) Transient hypotension Persistent hypotension 0 1 2 Ischemia None 0 Decreased pulses 1* No pulse, slow cap refill, paresthias 2* Cool pulseless, insentiate 3* Points double if ischemia > 6 hrs Age < 30 Yr 30 -50 >50 0 1 2 MESS > 6 Amputation 24 Not for studying purposes
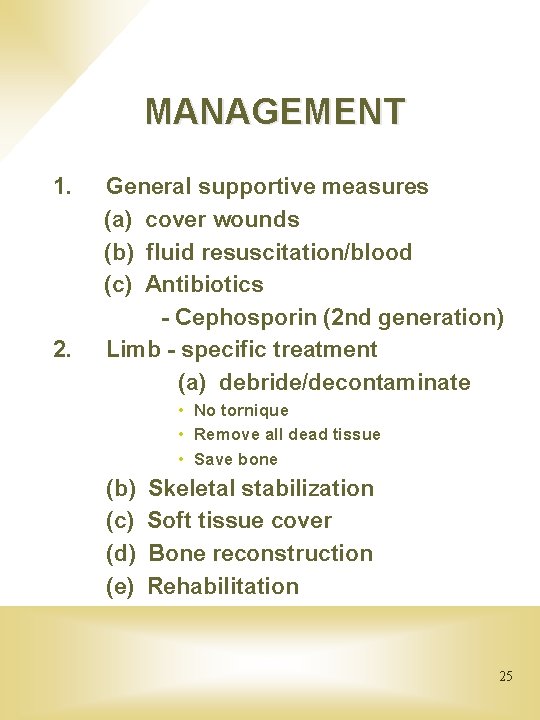
MANAGEMENT 1. 2. General supportive measures (a) cover wounds (b) fluid resuscitation/blood (c) Antibiotics - Cephosporin (2 nd generation) Limb - specific treatment (a) debride/decontaminate • No tornique • Remove all dead tissue • Save bone (b) (c) (d) (e) Skeletal stabilization Soft tissue cover Bone reconstruction Rehabilitation 25
End Thank you 26