Open Circuit Mouth Piece Ventilation BY AHMAD YOUNES
Open Circuit Mouth Piece Ventilation BY AHMAD YOUNES PROFESSOR OF THORACIC MEDICINE Mansoura faculty of medicine
QUICK LOOK Current knowledge • In 1980’s the introduction of masks and pressure ventilators which allowed for compensation of leaks resulted in a shift in methods. (Ease of use etc. ) • Noninvasive ventilation is an effective therapy to relieve dyspnea, decrease the work of breathing, and improve gas exchange in patients with acute respiratory failure and COPD. • Oro-nasal and nasal masks are most commonly used, although a wide variety of appliances are currently available. • The use of mouthpiece ventilation may be attractive for improving patient comfort and reducing skin breakdown.

Mouthpiece Ventilation (MPV) • MPV is a mode of ventilation that uses a mouthpiece interface which the patient holds with the lips when he wants to be supported during inspiration. • There exists a poor understanding of this method’s benefits compared to other modalities. • NIV is sometimes reported as suboptimal in neuromuscular disease patients due to excessive secretions in the airways , hypercapnia due to inadequate ventilator settings , or because of a lack of tolerance of the interface. • Interfaces that cover the nose and / or mouth and nose are the most commonly used, but may cause skin lesions and claustrophobia. Many of these drawbacks can be avoided by using a mouthpiece to administer the NIV.
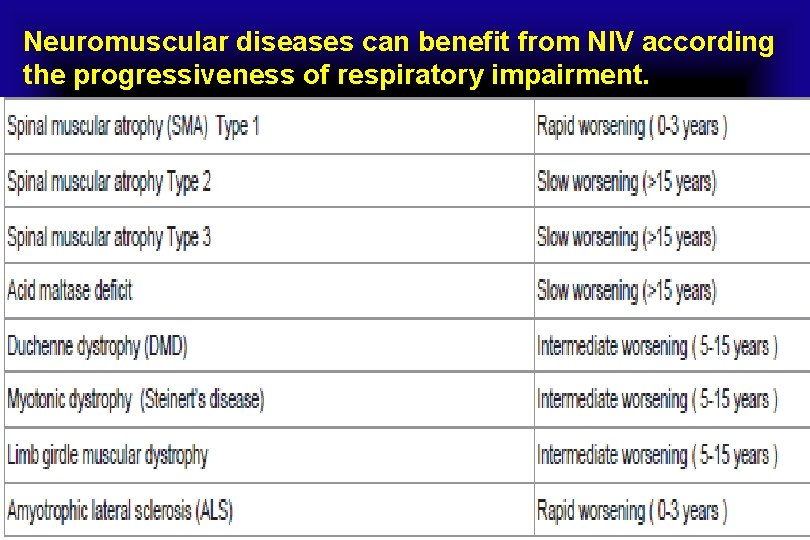
Neuromuscular diseases can benefit from NIV according the progressiveness of respiratory impairment.
Mouthpiece Ventilation (MPV) • Typical pathway of these patients today is Diagnosis then NIV at night then eventually tracheostomy. • Alternative pathway is that the patient can delay or sometimes go for years without tracheostomy. • When they can no longer tolerate MPV, then they are tracheostomized. • If given a choice to try a mouthpiece or a tracheostomy, which can include side effects, patients most likely would choose mouthpiece. • The only risk with mouthpiece is, if you fail mouthpiece, then you need a tracheostomy. • Traditionally performed on volume ventilators that were adapted and modified to allow for “sip breathing”.
Mouthpiece Ventilation (MPV) • The MPV is used by many patients as daytime ventilatory support in combination with other modes of ventilation interface effective for night ventilation. • There are two models mouthpiece of different sizes 15 and 22 mm. • NIV has been used for years in patients with neuromuscular disorders as a viable alternative to continuous ventilatory support via tracheotomy tube. • NIV is associated with a reduced risk of pneumonia and other respiratory complications. • Its use in the volumetric mode allows air-stacking to improve cough. The mouthpiece interface facilitates speech and swallowing, factors that lead to a better quality of life for patients.
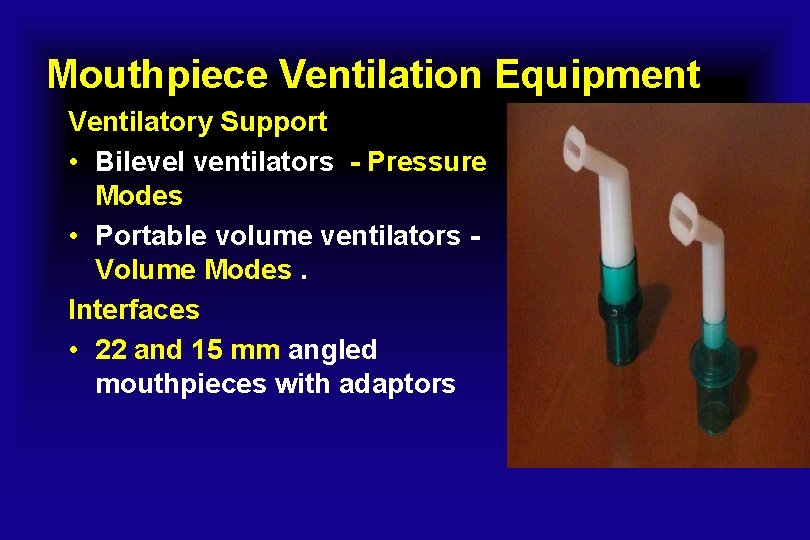
Mouthpiece Ventilation Equipment Ventilatory Support • Bilevel ventilators - Pressure Modes • Portable volume ventilators Volume Modes. Interfaces • 22 and 15 mm angled mouthpieces with adaptors
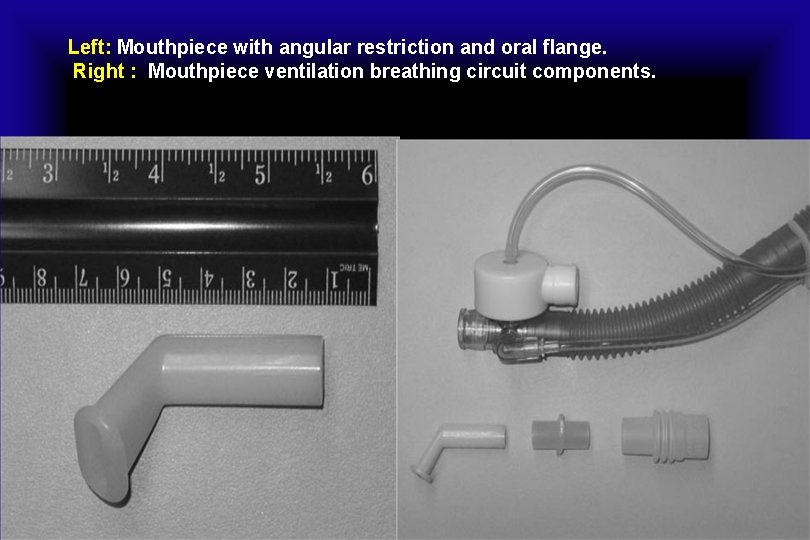
Left: Mouthpiece with angular restriction and oral flange. Right : Mouthpiece ventilation breathing circuit components.
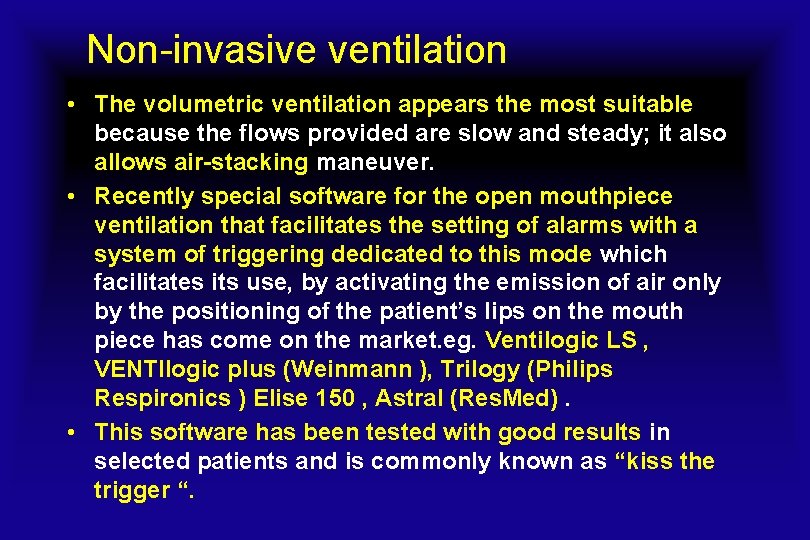
Non-invasive ventilation • The volumetric ventilation appears the most suitable because the flows provided are slow and steady; it also allows air-stacking maneuver. • Recently special software for the open mouthpiece ventilation that facilitates the setting of alarms with a system of triggering dedicated to this mode which facilitates its use, by activating the emission of air only by the positioning of the patient’s lips on the mouth piece has come on the market. eg. Ventilogic LS , VENTIlogic plus (Weinmann ), Trilogy (Philips Respironics ) Elise 150 , Astral (Res. Med). • This software has been tested with good results in selected patients and is commonly known as “kiss the trigger “.
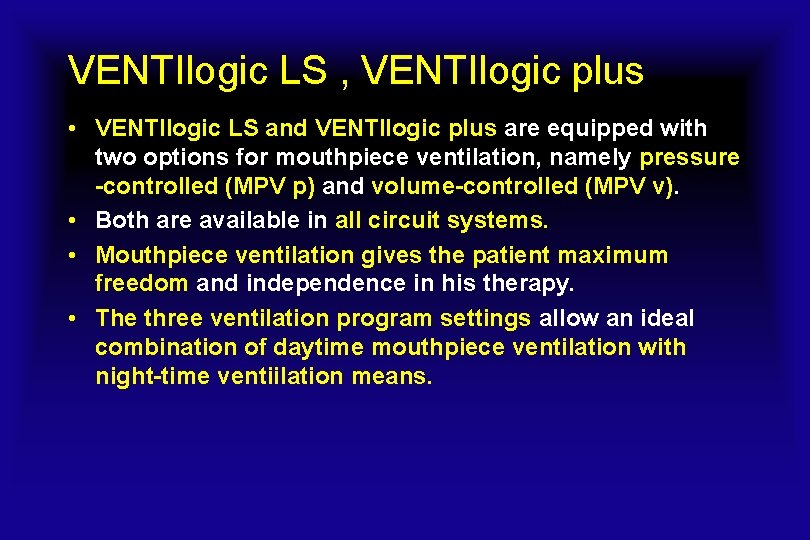
VENTIlogic LS , VENTIlogic plus • VENTIlogic LS and VENTIlogic plus are equipped with two options for mouthpiece ventilation, namely pressure -controlled (MPV p) and volume-controlled (MPV v). • Both are available in all circuit systems. • Mouthpiece ventilation gives the patient maximum freedom and independence in his therapy. • The three ventilation program settings allow an ideal combination of daytime mouthpiece ventilation with night-time ventiilation means.

VENTIlogic LS , VENTIlogic plus • Mobile use for intra-hospital transfers: With 9 hours of battery power (internal rechargeable battery and optional replaceable battery* have a capacity of 4. 5 hours each), the devices can adapt to any change of location. • Mobile use at home: VENTIlogic LS and VENTIlogic plus give your patients freedom of movement. • Sure in an unsure situation: Leakage is reliably compensated for in volume and pressure controlled modes. • The high-performance blower ensures continuous patient care in mobile use and difficult ventilation situations, even with imprecise fit of patient interface.
VENTIlogic LS , VENTIlogic plus • The comprehensive and clear monitoring concept provides the best support of your treatment. • Intuitive operation for fast check of ventilation settings. • Simple and direct monitoring of oxygen saturation and pulse with the Sp. O 2 module. • Unique alarm management (highly visible, large alarm window) for top safety: You can concentrate completely on therapy without any stress. • VENTI views: PC software for Weinmann ventilators reads out, displays, analyzes, archives and generates reports on patient and compliance data and their clinical application: Focus on ventilation requirements Process-oriented operation matches procedures in hospital
VENTIlogic LS , VENTIlogic plus Special shock resistance • Shock and vibration resistance were specially tested against recognized standards to ensure device‘s compliance with demands in mobile hospital and domestic surroundings. (Shock test as per IEC 60068 -2 -27 and Vibration test as per IEC 60068 -2 -64).
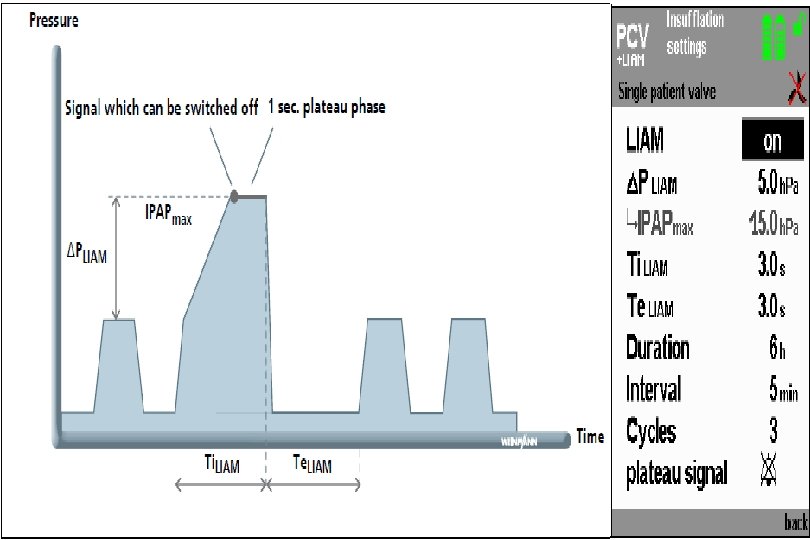
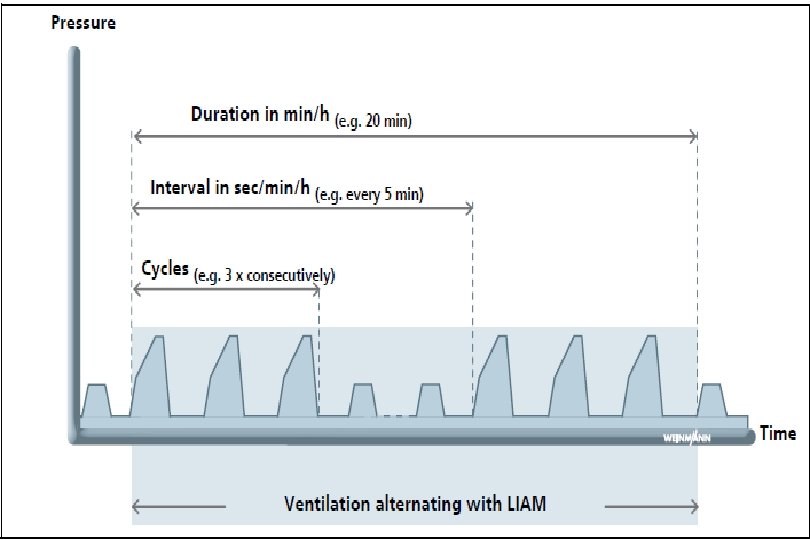
VENTIlogic LS , VENTIlogic plus • Doctors can configure three storable ventilation programs for patients who need varying degrees of ventilation support. • With the simple press of a key, the doctor, nurse or patient can select the individual programs to satisfy the patient‘s needs. • LIAM (Lung Insufflation Assist Maneuver): the integrated cough support is easy to use and requires no change of masks. The patient himself or a nurse can activate the function. • During mouthpiece ventilation the LIAM function is available as cough support or sigh function. • Volume compensation: Function to guarantee a pre-set target volume. The speed can be set in three levels.
VENTIlogic LS , VENTIlogic plus • Air Trap Control: Exhalation pressure relief to prevent dynamic hyperinflation. • Thanks to Air Trap Control, VENTIlogic LS and VENTIlogic plus automatically regulate pressure to a frequency and expiration time ideal for the patient. The titration process is thereby significantly simplified. • Trigger lockout: effective protection from false triggering and trigger artefacts at higher trigger sensitivity. The fast way to perfectly synchronized ventilation. • Expiratory pressure ramp: temporary pneumatic splint in airways at the start of expiration to counteract expiratory collapse of airways. The expiratory flow remains larger on average, the volume can be exhaled more easily and respiratory position can be lowered.
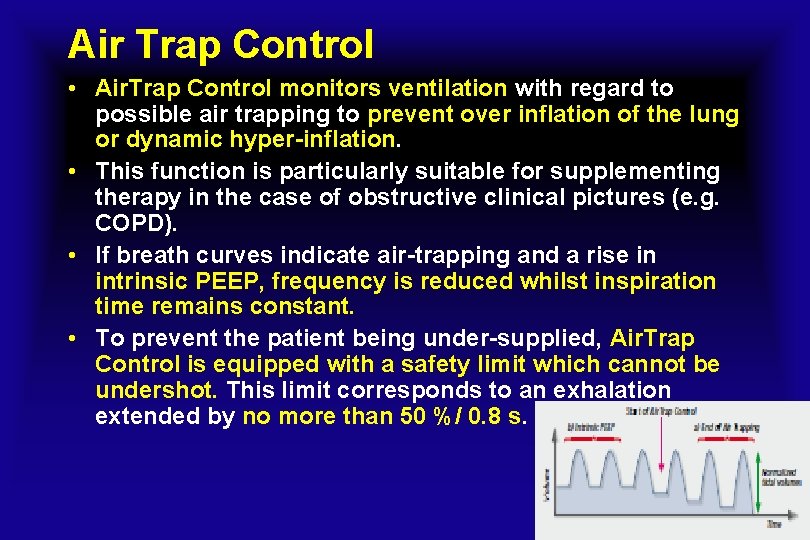
Air Trap Control • Air. Trap Control monitors ventilation with regard to possible air trapping to prevent over inflation of the lung or dynamic hyper-inflation. • This function is particularly suitable for supplementing therapy in the case of obstructive clinical pictures (e. g. COPD). • If breath curves indicate air-trapping and a rise in intrinsic PEEP, frequency is reduced whilst inspiration time remains constant. • To prevent the patient being under-supplied, Air. Trap Control is equipped with a safety limit which cannot be undershot. This limit corresponds to an exhalation extended by no more than 50 %/ 0. 8 s.
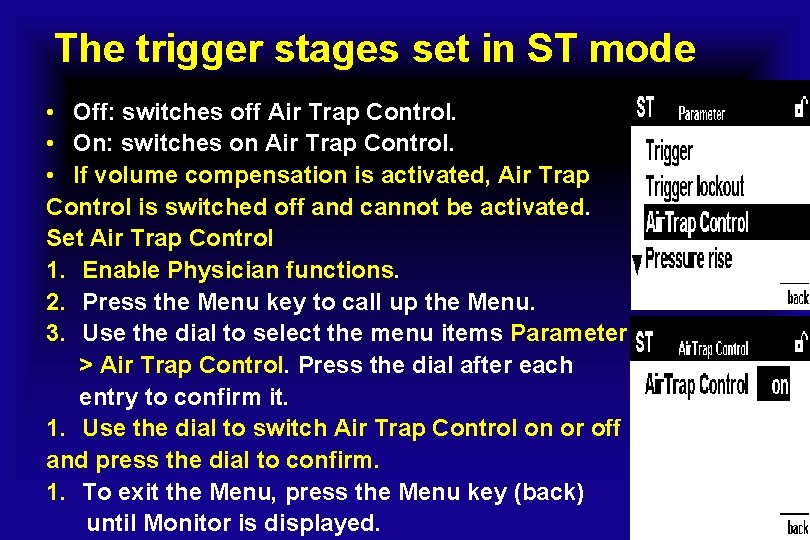
The trigger stages set in ST mode • Off: switches off Air Trap Control. • On: switches on Air Trap Control. • If volume compensation is activated, Air Trap Control is switched off and cannot be activated. Set Air Trap Control 1. Enable Physician functions. 2. Press the Menu key to call up the Menu. 3. Use the dial to select the menu items Parameter > Air Trap Control. Press the dial after each entry to confirm it. 1. Use the dial to switch Air Trap Control on or off and press the dial to confirm. 1. To exit the Menu, press the Menu key (back) until Monitor is displayed.
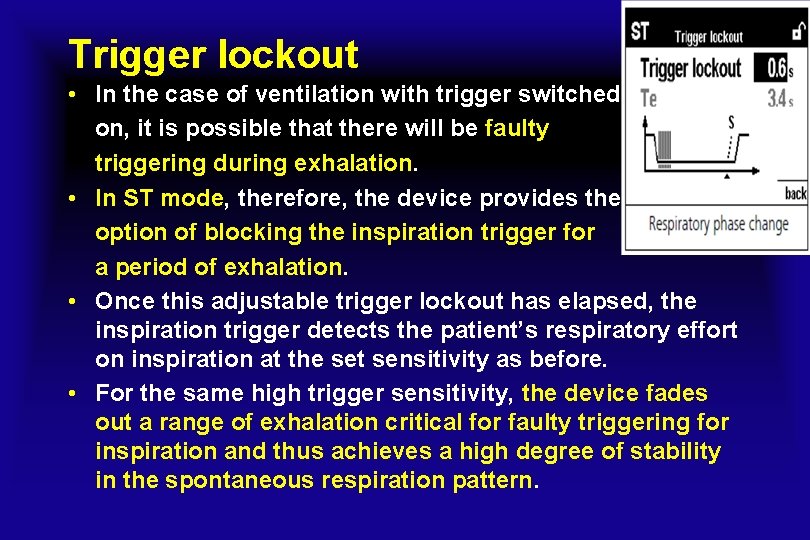
Trigger lockout • In the case of ventilation with trigger switched on, it is possible that there will be faulty triggering during exhalation. • In ST mode, therefore, the device provides the option of blocking the inspiration trigger for a period of exhalation. • Once this adjustable trigger lockout has elapsed, the inspiration trigger detects the patient’s respiratory effort on inspiration at the set sensitivity as before. • For the same high trigger sensitivity, the device fades out a range of exhalation critical for faulty triggering for inspiration and thus achieves a high degree of stability in the spontaneous respiration pattern.
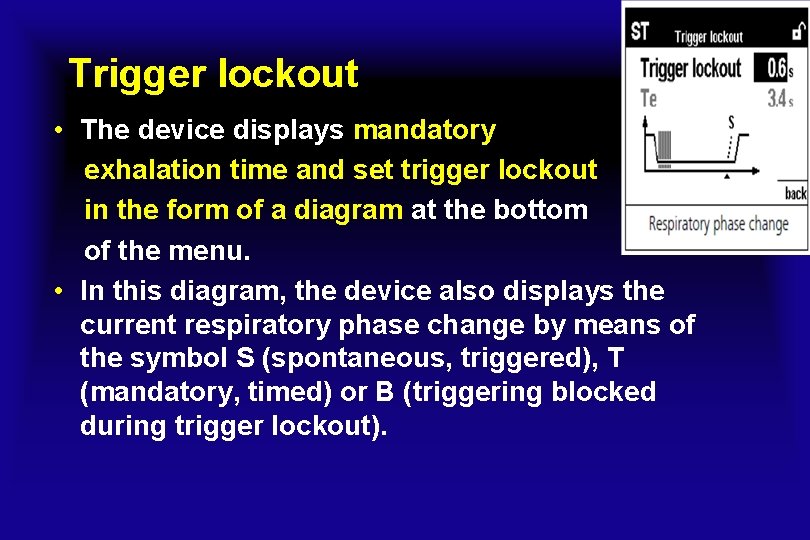
Trigger lockout • The device displays mandatory exhalation time and set trigger lockout in the form of a diagram at the bottom of the menu. • In this diagram, the device also displays the current respiratory phase change by means of the symbol S (spontaneous, triggered), T (mandatory, timed) or B (triggering blocked during trigger lockout).
VENTIlogic LS and VENTIlogic plus • While being ventilated, the patient can eat and speak without any trouble. • Greater flexibility and mobility also greatly improve the quality of life. • To satisfy patient needs completely, we have integrated two different types of mouthpiece ventilation 1 - MPVp pressure-controlled mouthpiece ventilation 2 - MPVv volume-controlled mouthpiece ventilation • Both modes can be used during leakage ventilation and during valve ventilation.
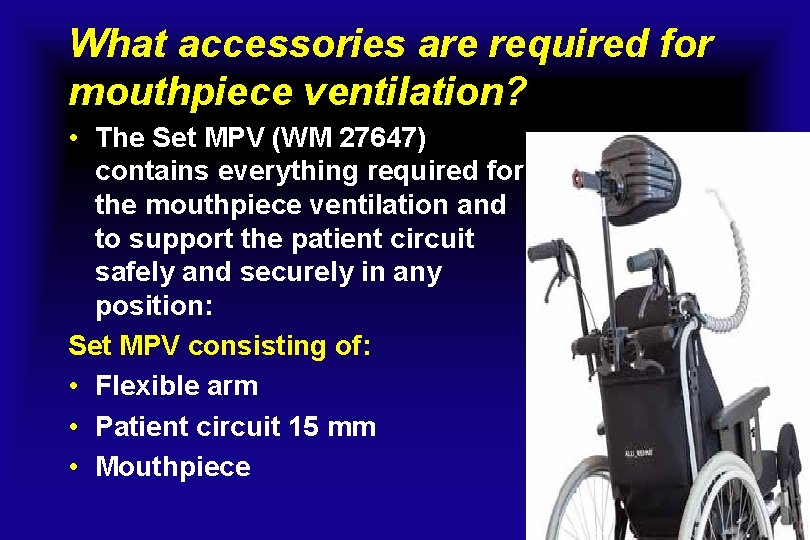
What accessories are required for mouthpiece ventilation? • The Set MPV (WM 27647) contains everything required for the mouthpiece ventilation and to support the patient circuit safely and securely in any position: Set MPV consisting of: • Flexible arm • Patient circuit 15 mm • Mouthpiece
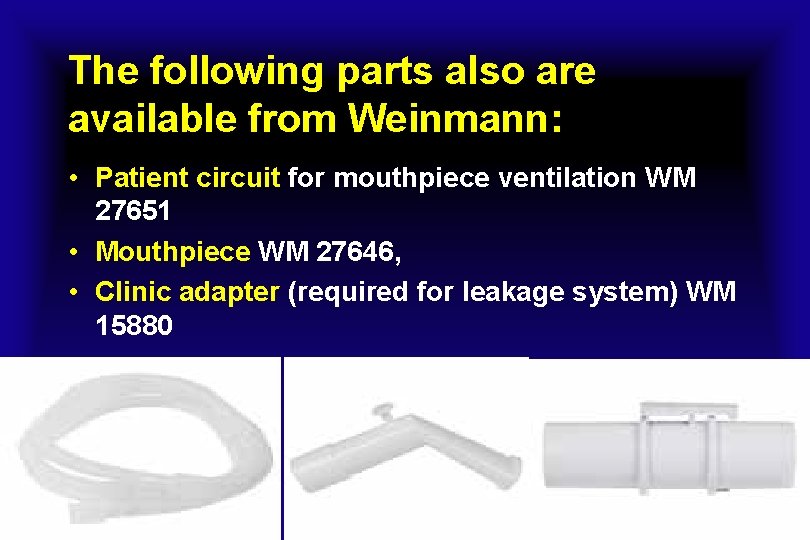
The following parts also are available from Weinmann: • Patient circuit for mouthpiece ventilation WM 27651 • Mouthpiece WM 27646, • Clinic adapter (required for leakage system) WM 15880
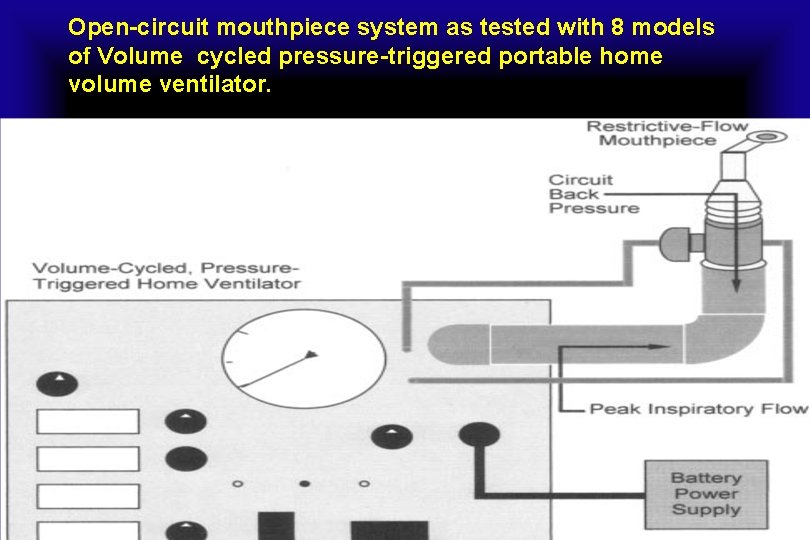
Open-circuit mouthpiece system as tested with 8 models of Volume cycled pressure-triggered portable home volume ventilator.
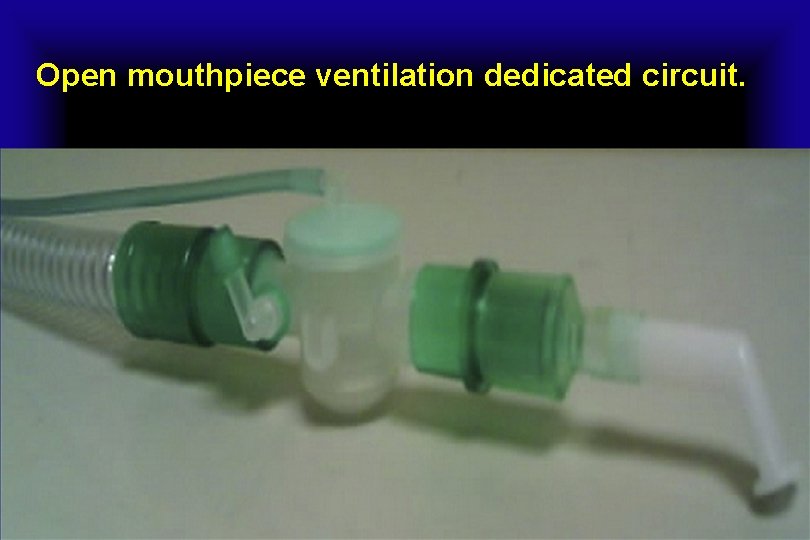
Open mouthpiece ventilation dedicated circuit.
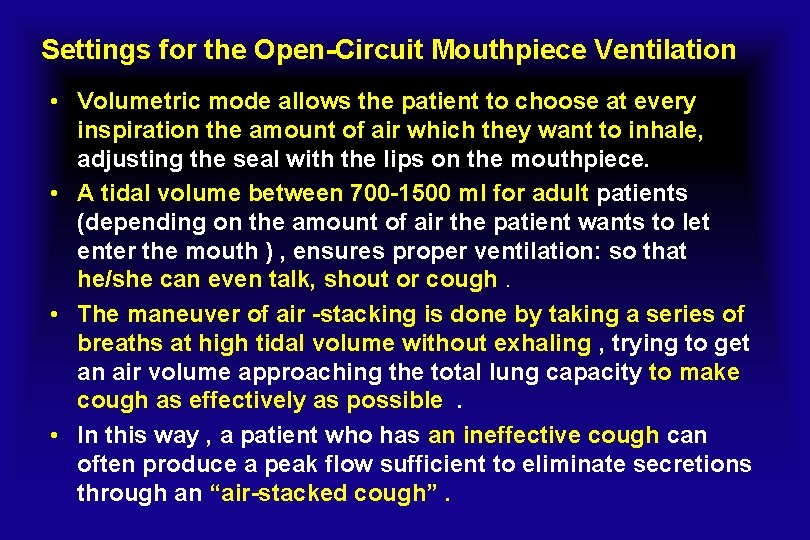
Settings for the Open-Circuit Mouthpiece Ventilation • Volumetric mode allows the patient to choose at every inspiration the amount of air which they want to inhale, adjusting the seal with the lips on the mouthpiece. • A tidal volume between 700 -1500 ml for adult patients (depending on the amount of air the patient wants to let enter the mouth ) , ensures proper ventilation: so that he/she can even talk, shout or cough. • The maneuver of air -stacking is done by taking a series of breaths at high tidal volume without exhaling , trying to get an air volume approaching the total lung capacity to make cough as effectively as possible. • In this way , a patient who has an ineffective cough can often produce a peak flow sufficient to eliminate secretions through an “air-stacked cough”.
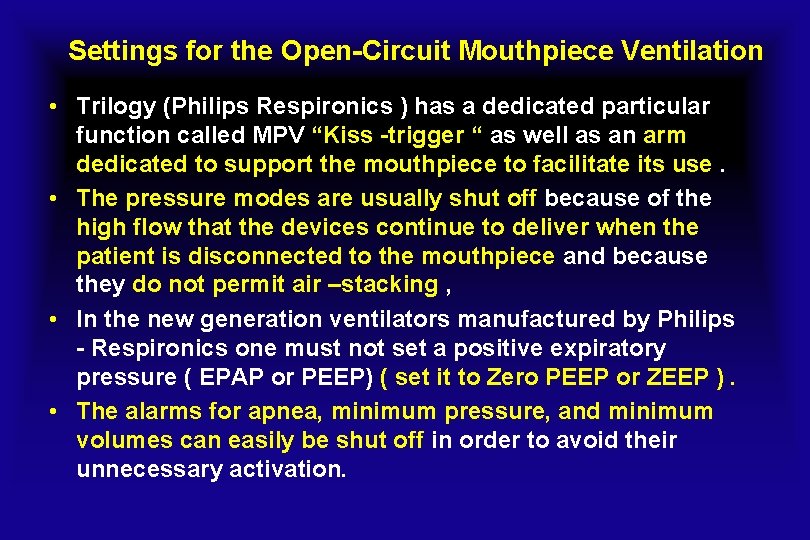
Settings for the Open-Circuit Mouthpiece Ventilation • Trilogy (Philips Respironics ) has a dedicated particular function called MPV “Kiss -trigger “ as well as an arm dedicated to support the mouthpiece to facilitate its use. • The pressure modes are usually shut off because of the high flow that the devices continue to deliver when the patient is disconnected to the mouthpiece and because they do not permit air –stacking , • In the new generation ventilators manufactured by Philips - Respironics one must not set a positive expiratory pressure ( EPAP or PEEP) ( set it to Zero PEEP or ZEEP ). • The alarms for apnea, minimum pressure, and minimum volumes can easily be shut off in order to avoid their unnecessary activation.
Settings for the Open-Circuit Mouthpiece Ventilation • In most home volumetric ventilators the minimum pressure alarm cannot be excluded; therefore it is necessary to set up a PEEP (often 2 cm H 2 O ) , which, thanks to the resistance to the flow of air created from the angle of the mouthpiece creates a pressure that prevents the continuous activation of the alarms. • The most common mode of ventilation is ACV with a tidal volume between 0. 7 and 1. 5 L without PEEP ( EPAP ) , alarm with low set pressure to minimum possible or excluded , and the maximum apnea time.
Settings for the Open-Circuit Mouthpiece Ventilation • The patient activates the breath by putting the mouth on the mouthpiece and creating a small negative pressure in the circuit as drinking or inhaling from the mouthpiece. • With the “Kiss trigger”, ventilation is activated when the patient simply leans the mouth on the mouthpiece; no other effort is required for the patient. • Sometimes volume cycling ventilation produces gastric distention; in these cases, one switches to pressure cycling ventilation.
Recommended Trilogy 100 Setup with dedicated MPV mode • Available in AC and PC mode • New Kiss Trigger with Signal Flow Technology • Passive circuit type • Spontaneous mode, S/T or PC mode • Respiratory rate = 2 – 4 • IPAP = enough to give Vt that is required • EPAP = 4 • Alarms = off
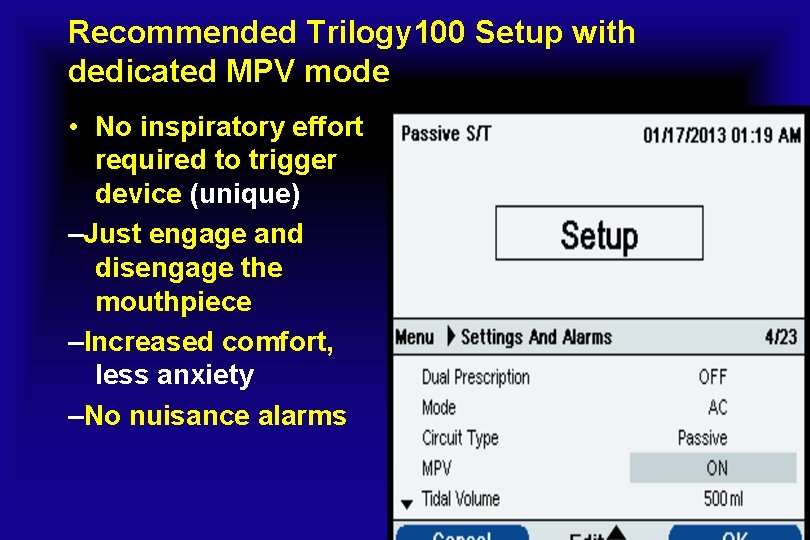
Recommended Trilogy 100 Setup with dedicated MPV mode • No inspiratory effort required to trigger device (unique) –Just engage and disengage the mouthpiece –Increased comfort, less anxiety –No nuisance alarms
MPV mode Assist Control (AC) vs. Pressure Control (PC) AC volume: - e. g. 1200 mls • Breathing techniques such as Air Stacking and Glossopharyngeal breathing (Frog) easier to perform. (Increase VC/Muscle strength ) • Flow patterns square vs ramp • Traditional and referenced PC pressure: - e. g. 18 cm. H 2 O • Feels like usual nocturnal ventilation • Easier to assess for prescription and setting • Rise time
Trilogy and MPV: dual prescription • Night time ventilation: Primary prescription • Daytime ventilation: Secondary settings – PC MPV • Pt only has to swap the circuit and press 2 buttons • No calibration between circuits
Advantages of mouthpiece ventilation • Less interference with speech, very little dead space, better appearance, and no need for headgear, thereby eliminating any possibility of claustrophobia. • Its limitation to being useful predominantly for waking hours except when retained by a lip covering interface like the Lip seal or Oracle. • Nasal leaks, but mouth air leaks can be controlled with a tight -fitting lip seal and nasal pledges or nose clips can be used to avoid air leak via the nares. • EPAP or PEEP cannot be maintained for patients using open systems of NIV and, indeed, are rarely if ever needed for these patients. • Apnea alarms, when preset, should be set at the highest threshold to avoid unnecessary activation and nuisance.
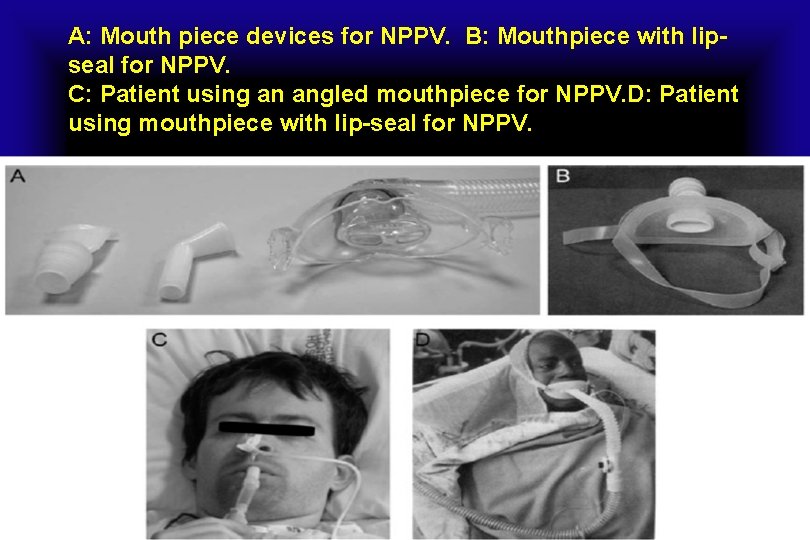
A: Mouth piece devices for NPPV. B: Mouthpiece with lipseal for NPPV. C: Patient using an angled mouthpiece for NPPV. D: Patient using mouthpiece with lip-seal for NPPV.
Disadvantages of mouthpiece ventilation • Mouthpiece NIV is not successful when patients are uncooperative, cannot access the interface, or when a severe bulbar dysfunction causes aspiration of saliva such that the O 2 saturation baseline remains below 95%. • It can cause or exacerbate dry mouth. Such patients may benefit from heated humidification or switching to oro-nasal interfaces.
MPV in neuromuscular disease • MPV, combined with aggressive mechanically assisted cough, has also been proposed as part of a protocol designed to wean patients from invasive mechanical ventilation after an episode of acute respiratory failure because of a congenital or acquired neuromuscular disease. • Mouthpiece ventilation is used with single-limb non-vented circuit ventilators in pressurecontrolled or, more frequently, in volumecontrolled mode for allowing air stacking.
MPV in neuromuscular disease • The patient can get mouthpiece ventilation breaths passively, using the set backup frequency on the ventilator, or he/she can actively trigger the breath, retaining a part or all of the delivered volume. • As a matter of fact, depending on the ability to move the neck, the patient can continuously keep the mouthpiece between his/her lips or leave it for a variable time.
MPV in neuromuscular disease • Despite these attractive features, the practical application of mouthpiece ventilation and the possibility of adapting a ventilator conceived for invasive or noninvasive ventilation to completely open mouthpiece ventilation may pose some technical problems. • Some drawbacks like alarm activation and/or the presence of a noisy bias flow during disconnection from the mouthpiece may make it unacceptable for the patient.
MPV in neuromuscular disease • A recent study found that alarms (mainly disconnection and low-pressure alarms) were frequently activated during mouthpiece ventilation, becoming a source of nuisance for the user. This can lead to unsuccessful application of mouthpiece ventilation. • The main alarms to consider during mouthpiece ventilation in volume-target mode are apnea, lowpressure, and disconnection alarms. • An apnea alarm indicates the absence of a breath activated by the patient. When it cannot be switched off (Astral 150), it is activated if the mouthpiece ventilation user does not breathe for a time longer than the set apnea alarm (60 or 120 s)
MPV in neuromuscular disease • A disconnection alarm works in the same way as the low-pressure alarm, and both are activated when the pressure in the circuit does not reach the set low-pressure alarm. • This is likely to happen when the mouthpiece ventilation user can remain disconnected from the ventilator for several minutes, and the backup rate cannot be set to zero, delivering mandatory breaths, or when auto-triggering occurs.
MPV in neuromuscular disease • An accurate combination of VT and TI is the key factor in avoiding alarm activation. • We agree that the backup rate should be set at the minimum available value to significantly reduce the discomfort due to continuous flow on the user’s face during mouthpiece disconnection. • A decrease in the TI can be obtained only by increasing the backup rate in some devices. This is due to an internal algorithm that links the TI, VT, and backup rate to ensure that the inspiratory-expiratory ratio and, consequently , the peak inspiratory flow is maintained in a predefined range. • As a consequence, the possible relationship between the backup rate and the maximum TI value should be taken into account when setting mouthpiece ventilation with this ventilator.
MPV in neuromuscular disease • Auto-triggering was seldom found and easily fixed except in the Astral 150. A speculation from some researchers is that ventilators should have a pressure trigger to avoid auto-triggering. • Nowadays, the majority of home ventilators available in Europe have only a flow trigger option when the noninvasive ventilation mode is chosen. • Because new algorithms for leak compensation have been developed , only minimal problems of auto-triggering have been found in our study.
MPV in neuromuscular disease • Even when the end-expiratory pressure was set to zero, some ventilators have a bias flow exiting the circuit. This variable must be taken into consideration when choosing a ventilator for mouthpiece ventilation because it could be a source of discomfort in users who cannot move their head. • More than 70% of subjects treated with mouthpiece ventilation used it in volume controlled mode. The majority used the same ventilator during night and day but with different settings. This result underlines the usefulness of having more than one simultaneous setting, called ventilator prescription, in a single ventilator unit. (eg, one for mask ventilation and the other for mouthpiece ventilation).
MPV in neuromuscular disease • The majority of available home ventilators may be used for mouthpiece ventilation even in the absence of a specific mode. • An appropriate combination of tidal volume and inspiratory time and an appropriate setting of alarms may avoid nuisance alarm activation.
Open-Mouthpiece Ventilation Versus Nasal Mask Ventilation in COPD Exacerbation • Open-Mouthpiece Ventilation is used in patients with exacerbations of COPD with mild to moderate acidosis. • The study was performed in fifty subjects with exacerbations of COPD, breathing frequency > 25, Pa. CO 2 > 45, and p. H between 7. 25 and 7. 30. • Subjects were randomly assigned to receive NIV via nasal mask or mouthpiece ventilation. • No subjects had deterioration of gas exchange. The 2 groups had similar trends in arterial blood gases and breathing frequency. No differences in duration of NIV or hospital stay were noted.
Open-Mouthpiece Ventilation Versus Nasal Mask Ventilation in COPD Exacerbation • Subjects preferred mouthpiece ventilation. • CONCLUSIONS: Open mouthpiece ventilation is a useful technique and may prevent further deterioration of gas exchange in COPD patients with mild to moderate acidosis (similar to traditional NIV delivered by a nasal mask). • [Respir Care 2014; 59(12): 1– • . © 2014 Daedalus Enterprises]

- Slides: 51