Ontario Medical Association Dr Jim Wright Ontario Health





- Slides: 18

Ontario Medical Association • Dr. Jim Wright Ontario Health Teams Moving Forward with Integration in Ontario November 14, 2019 • Rena Menaker • Jennifer Gold • Dara Laxer Ministry of Health • Allison Costello • Neil Mc. Mullin
Tonight’s Agenda (not in order of presentation) MOH: • Current status of applications • Overview of attribution model OMA: • Communications among physicians/OHTs • Organization of community-based physicians • Governance overview of OHTs 2

Goals of Ontario Health Teams (OHTs) • Goal: fully integrate across the continuum of care at a lower cost • Quadruple aim (population health, patient experience, efficiency, provider experience) OMA’s Position: • Voluntary • Physician led • Primary care based 3

Ministry of Health Status Update & Review of Attribution Methodology 4

Recall: Ontario Health Teams Readiness Assessment • Ontario Health Teams will provide a full and coordinated continuum of care to a defined population of Ontario residents, and will be accountable for the health outcomes and health care costs of that population. • Groups of healthcare providers and organizations can become Ontario Health Teams through the Readiness Assessment process. The process is standardized and will be repeated until full provincial scale is achieved. • The Readiness Assessment process consists of several stages and is intended to evaluate readiness against the criteria set out in the Guidance Document. Self-Assessment • Full Application Community Visit Selection of Teams The process helps identify how ready a team is to implement the model. There are different stages of readiness, ranging from In Discovery In Development Ontario Health Team Candidate 5
Results of the First Readiness Assessment Process Through the April 2019 call for self assessments, over 150 groups put themselves forward to be OHTs in the initial waves of implementation. Results of the First Self-Assessment review: • 31 teams were invited to complete a Full Application ü 31 Full Applications were received on October 9, 2019 for evaluation • 41 teams are In Development and working towards Full Application • Remaining providers/teams are In Discovery Full Applicants and In Development teams were provided with: • A ministry point of contact – a ‘one-window’ liaison for access to supports, key communications, and questions • These points of contact have directed teams to available resources, helped find answers to technical questions, and have kept teams up-to-date on upcoming events and supports • Data on each team’s attributed population • Access to RISE suite of supports 6
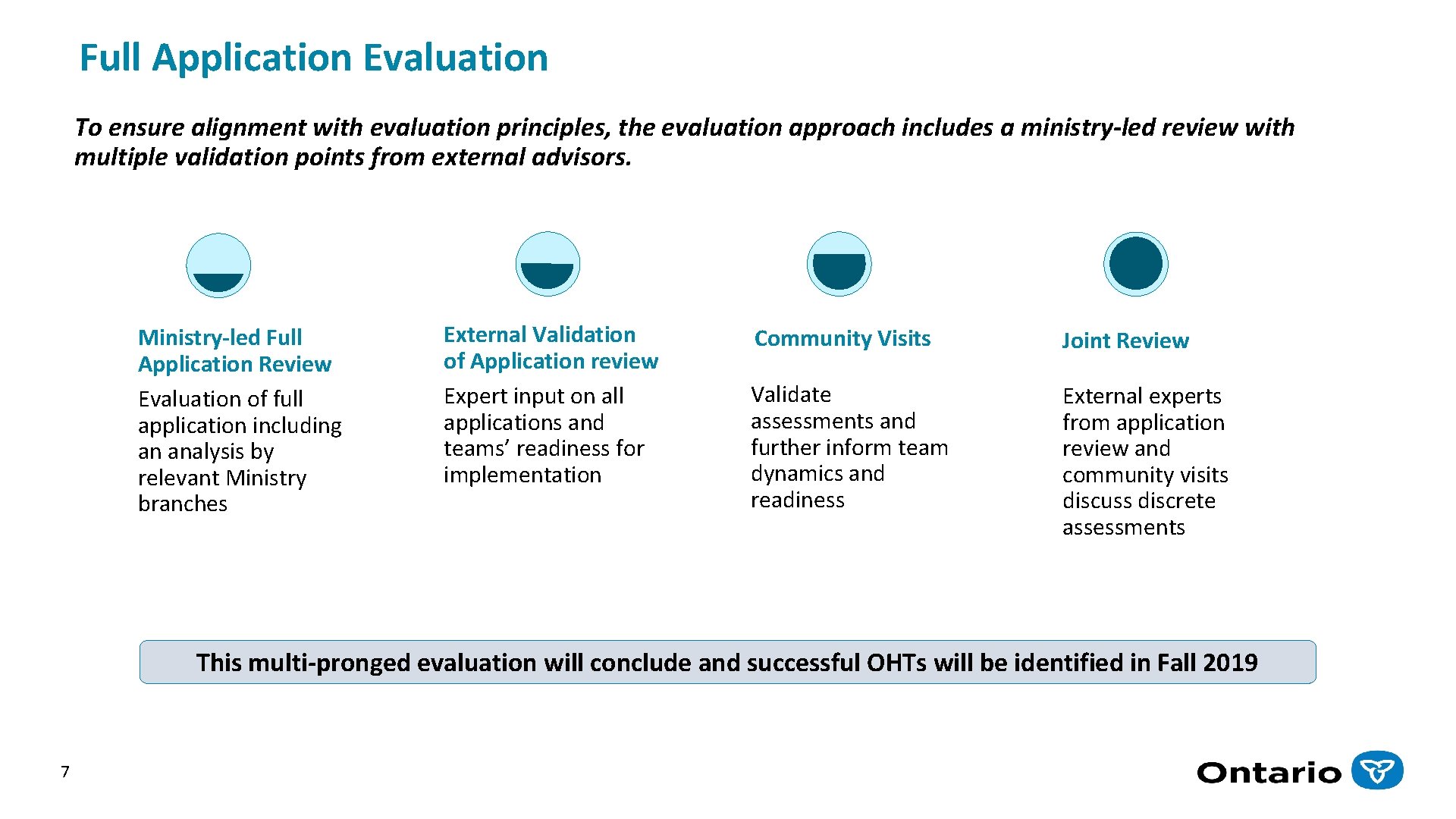
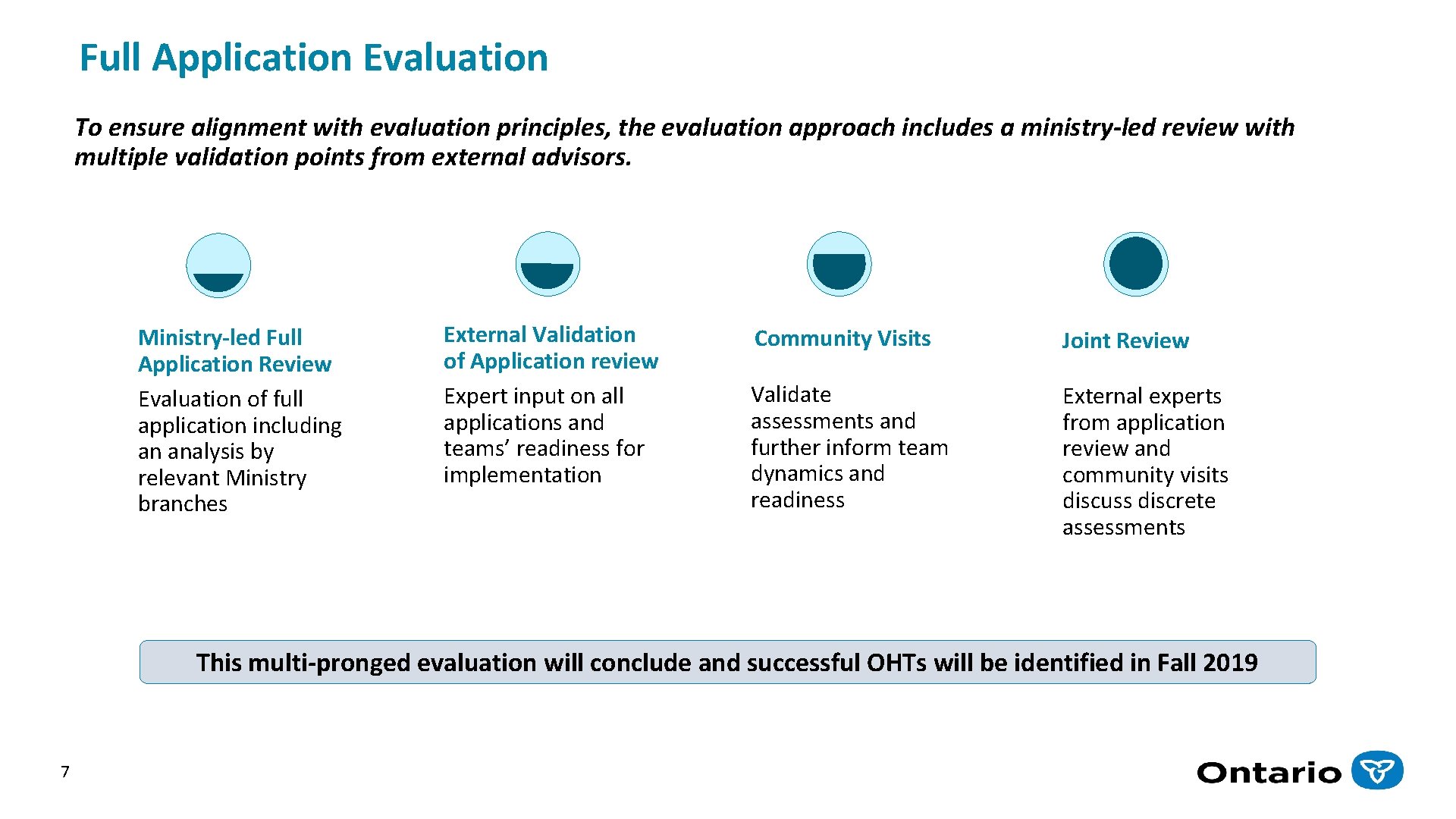
Full Application Evaluation To ensure alignment with evaluation principles, the evaluation approach includes a ministry-led review with multiple validation points from external advisors. Ministry-led Full Application Review Evaluation of full application including an analysis by relevant Ministry branches External Validation of Application review Expert input on all applications and teams’ readiness for implementation Community Visits Joint Review Validate assessments and further inform team dynamics and readiness External experts from application review and community visits discuss discrete assessments This multi-pronged evaluation will conclude and successful OHTs will be identified in Fall 2019 7
Patient Attribution & Population Health Ontario Health Teams are groups of providers and organizations that will be clinically and fiscally accountable for delivering a full and coordinated continuum of care to a defined population. • As a population health model, successful OHT implementation requires that both the Ministry and providers have the ability to track: § The health… § The health care experiences, and… § The health care utilization and spending. . . § For a population across the continuum of care and beyond traditional sector boundaries • The first step in this transformation is to identify the population for which an OHT will be held accountable 8
Linking Patients & Providers to Form Networks The Institute for Clinical Evaluative Sciences (ICES) has identified “multispecialty physician networks” in Ontario by using administrative data to reveal natural linkages among patients, physicians, and hospitals based on patient flow Methods: § Ontario residents are linked to a primary care physician based on their: § Enrollment with a primary care physician § Use of primary care services § Primary care physicians are linked to the hospital where most of his or her patients are admitted § Specialists are linked to the hospital where he or she provided the highest volume of inpatient services § All residents with health claims are linked § Small clusters are aggregated to form multispecialty physician networks 9
Leveraging the Multispecialty Physician Networks Applicability to the OHT Model Key Benefits: • Current patient-provider relationships are respected • Approach does not lock patients to particular care providers (patient choice is not limited) • Networks are sufficiently sized that they can be held accountable for quality and spending (i. e. , networks have sufficient patients to measure performance and outcomes) • Patient care is tightly concentrated within local providers • Specialists are tightly affiliated with hospitals Please note that while the data identifies historical patient access and referral patterns, physicians and organizations will have a significantly greater understanding of patient needs and are free to choose the OHT or organization(s) they partner with, based on the needs and health utilization of their patients. 10
Networks & OHTs: How the Approach will be Used • Inform partnerships and collaboration among providers based on current health care utilization patterns § Teams may find their data either confirms their partnerships or it may help them find new or different provider partners. (e. g. , teams that submitted separate self-assessments may decide to submit a Full Application as one team) • Attribute (assign) patients to OHTs to monitor indicators and health care spending § Data may not align with historical calculations of performance indicators. Indicators have been calculated to reflect the health utilization of the patients that have been attributed to OHTs • Identify linkages and partnerships with non-physician health service providers § Although networks are not geographically based, maps that illustrate natural linkages between providers will help inform potential provider partnerships The attribution methodology does not dictate partnerships, nor should teams regard the data as prescriptive. Providers are encouraged to partner with the individuals and organizations they deem to be the “best fit”. 11

Communication • • • 12 OMA sent letters to members assigned to the 31 groups in full application. OHT meetings as part of OMA President’s Tour. Leading and/or attending local meetings to address questions. Planning communications for those in development. Ongoing discussions with Government and system stakeholders.
Member Supports • Teletown halls. • OMA Regional Managers supporting physician engagement and physician-led OHT meetings (e. g. organizing / funding). • Identifying community leaders • Dedicated OHT: o FAQs, educational tools and resources; o Advice on appropriate governance models; o Interactive map identifying where OHTs are located and supporting linkages; o Legal support with contract, agreement templates and advice; o Digital health service advice through Ontario. MD. 13
Helping Physicians Organize • There are TWO levels of governance for physicians: o OHT governance; and o Physician governance within the OHT • The OMA draft governance structure includes: o A physician association agreement; o A dispute resolution mechanism and terms of reference; o Data governance model. 14
Helping Physicians Organize • Physicians are beginning to organize in many ways • Purpose: creates grass roots input and legitimacy for physician leaders to speak on behalf of physicians • Examples: o East Toronto Physician Family Practice Network (corporation) o Guelph: Physician Association (includes all physicians) o Southlake OHT: Primary Care Association / Primary Care Council o North York physician engagement: Physician allocated to do physician engagement 15
Helping Physicians Organize Lessons from other jurisdictions with successful integrated care systems recommend: • Must be physician led • Involve ALL physicians (e. g. primary care, specialists, community and hospitalbased): o Physician voice will be stronger if united. o Excluding groups of physicians creates artificial silos. o Harder to bring specialists on board, if not engaged from the outset. • Please send information regarding how your OHT is organizing physician groups to oma_oht@OMA. ORG or contact your Regional Manager. 16
Questions? 17
OMA OHT Email & Webpage Email: OMA_OHT@oma. org OHT resources webpage: www. oma. org and search “OHT” https: //www. oma. org/section/search/about-ontario-health-teams? type=topics 18
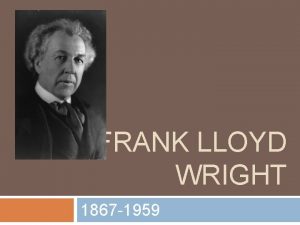
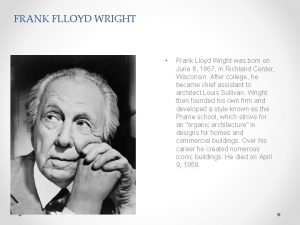
 Rti writing interventions
Rti writing interventions Dr. jim wright
Dr. jim wright Jim wright intervention central
Jim wright intervention central Rti behavior checklist
Rti behavior checklist Jim wright rti
Jim wright rti Construction safety association of ontario
Construction safety association of ontario Dr. marina spudic
Dr. marina spudic California central service association
California central service association Ontario search and rescue volunteer association
Ontario search and rescue volunteer association Physiotherapy ontario association
Physiotherapy ontario association Ontario public buyers association
Ontario public buyers association Ontario disc sports association
Ontario disc sports association Regulation 851 ontario
Regulation 851 ontario Hfo ontario
Hfo ontario 4 moments of hand hygiene
4 moments of hand hygiene Natural health product regulations canada
Natural health product regulations canada Occupational health clinics for ontario workers purpose
Occupational health clinics for ontario workers purpose Kuwait medical association training center
Kuwait medical association training center Association of medical engineering of kenya nairobi
Association of medical engineering of kenya nairobi