Ongoing High HIV Incidence among Women and Men

- Slides: 15
Ongoing High HIV Incidence among Women and Men in Chókwè, Southern Mozambique: A Call for Rapid Scale‐up of Combination HIV Prevention Robert Nelson 1, Ricardo Thompson 2, Isabelle Casavant 3, Sherri Pals 1, Juvencio Bonzela 2, Didier Mugabe 2, José Come 2, Dawud Ujamaa 1, Judite Cardoso 4, Andrew Auld 1, Bertur Maculuve 5, Stan Wei 3, Daniel Shodell 6, Duncan Mac. Kellar 1 1 Centers for Disease Control and Prevention, Atlanta, Georgia, USA 2 Chókwè Health Research and Training Center (CITSC), National Institute of Health, Mozambique 3 Centers for Disease Control and Prevention, Maputo, Mozambique 4 Jhpiego, Maputo, Mozambique 5 Public Health Department Gaza, Xaixai, Mozambique 6 Colorado Department of Public Health and Environment, Denver, Colorado, USA The findings and conclusions in this presentation are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention. #AIDS 2016 | @AIDS_conference
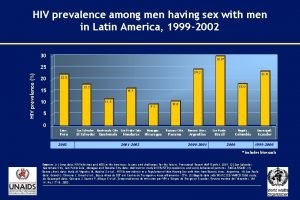
Background • UNAIDS estimates that over 1. 5 million Mozambicans are infected with HIV • Highest burden is in southern Mozambique, with community prevalence as high as 40% 1 • A 2012 cohort study of sexually active women 18‐ 35 years of age in Chokwe District found incidence of 4. 6 (95% CI: 2. 7‐ 7. 3) per 100 PY 2 • HIV incidence is high in regions of South Africa close to Mozambique, with location‐specific incidence as high as 14. 8 (95% CI: 9. 7‐ 19. 8) per 100 PY 3 • In 2014, the Chókwè Health Demographic Surveillance System (CHDSS) incorporated HIV testing and counseling (HTC) within annual rounds of demographic surveillance • In this presentation, we report HIV prevalence, prior diagnosis, ART coverage from the first round and incidence during the first two rounds 1 Gonzalez, et al. (2012). High HIV prevalence in a southern semi‐rural area of Mozambique… HIV medicine. et al. (2014). HIV prevalence and incidence in a cohort of women… PLo. S One 3 Nel, et al. (2012). HIV incidence remains high in Kwa. Zulu‐Natal, South Africa. . . PLo. S One 4 Casavant et al. (2016). Home‐based HIV Testing and New HIV Diagnoses… CROI 2016. 2 Feldblum, #AIDS 2016 | @AIDS_conference
Overarching Project Objectives • Move toward 90‐ 90 by increasing HIV testing and ART coverage • Assess trends in the uptake of evidence‐based interventions, community viral load, and HIV prevalence and incidence • Assess individual factors associated with the uptake of evidence‐based interventions and HIV infection #AIDS 2016 | @AIDS_conference
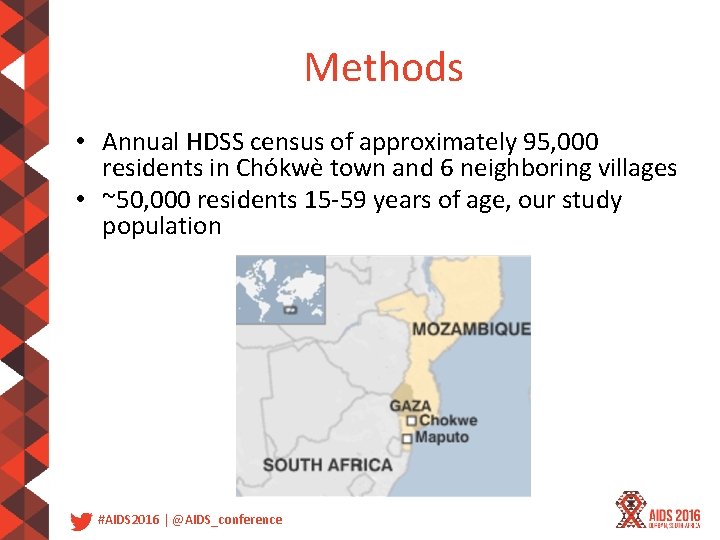
Methods • Annual HDSS census of approximately 95, 000 residents in Chókwè town and 6 neighboring villages • ~50, 000 residents 15‐ 59 years of age, our study population #AIDS 2016 | @AIDS_conference
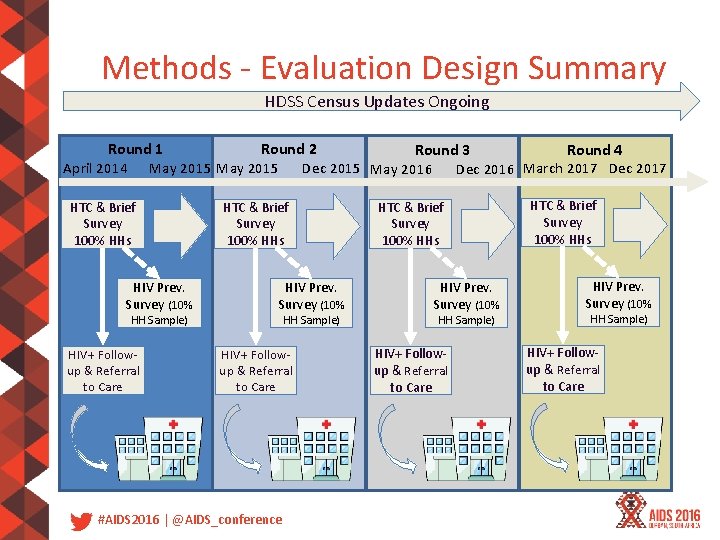
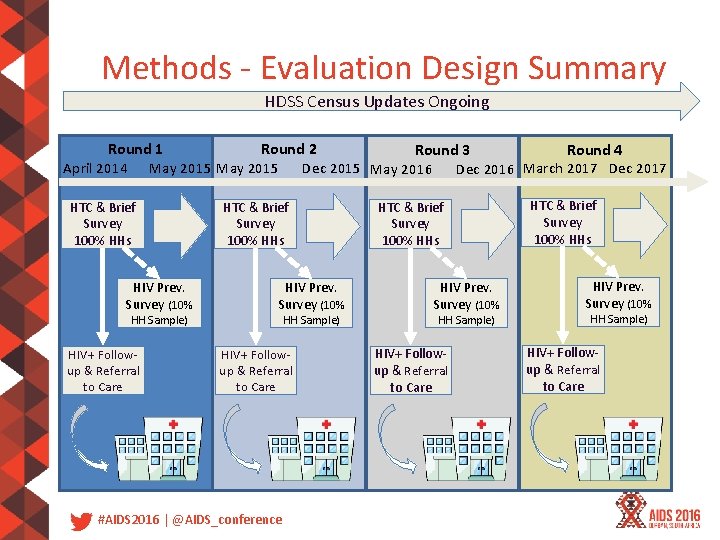
Methods ‐ Evaluation Design Summary HDSS Census Updates Ongoing Round 2 Round 1 Round 4 Round 3 Dec 2015 May 2016 April 2014 May 2015 Dec 2016 March 2017 Dec 2017 HTC & Brief Survey 100% HHs HIV Prev. Survey (10% HH Sample) HIV+ Follow‐ up & Referral to Care #AIDS 2016 | @AIDS_conference HTC & Brief Survey 100% HHs HIV Prev. Survey (10% HH Sample) HIV+ Follow‐ up & Referral to Care
Round 1 Testing and HIV Prevalence • 25, 435 residents 15‐ 59 years of age tested – – – 7959 (31%) men 17476 (69%) women 9942 (39%) 15‐ 24 years of age 10, 666 (42%) 25‐ 44 years of age 4789 (19%) 45‐ 59 years of age • 5, 170 (20%) Tested HIV+ – 994 (13%) of men tested HIV+ – 4176 (24%) of women tested HIV+ • 1947 (38%) newly diagnosed with HIV – 471 (47%) among men – 1476 (35%) among women #AIDS 2016 | @AIDS_conference
Round 1 prevalence of HIV infection and percentage of new HIV diagnoses, by age‐group and sex #AIDS 2016 | @AIDS_conference
ART Coverage Abstract WEPEC 173 addresses ART coverage • Patient‐reported ART uptake was confirmed in ≥ 95% of cases by observing ART pill bottles • Among HIV positive participants, 3, 179 (62%) had been previously diagnosed, 3, 092 (60%) were ever in HIV care, 2, 946 (58%) received HIV care within 90 days, and 2, 587 (51%) were on ART eligibility at the time of the study was CD 4 ≤ 350 or WHO stage III/IV #AIDS 2016 | @AIDS_conference
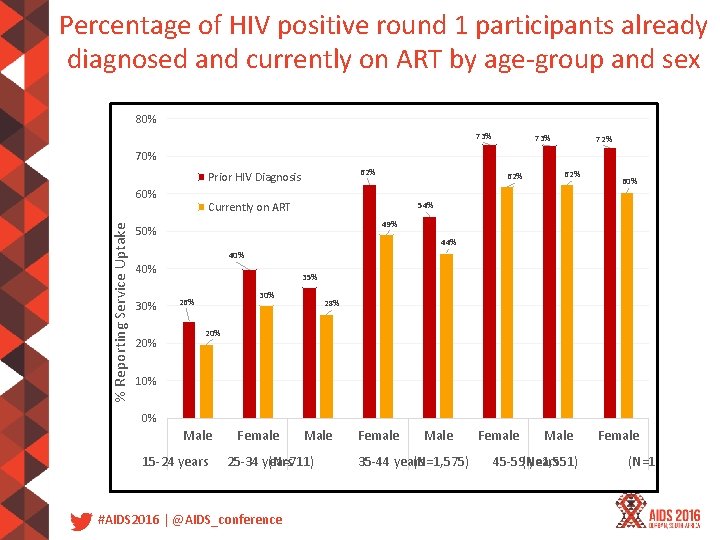
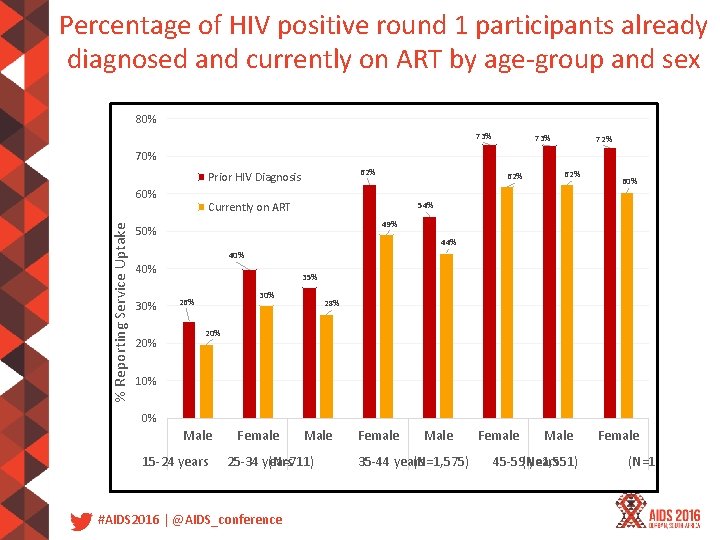
Percentage of HIV positive round 1 participants already diagnosed and currently on ART by age‐group and sex 80% 73% 72% 70% 62% Prior HIV Diagnosis % Reporting Service Uptake 60% 62% 60% 54% Currently on ART 49% 50% 44% 40% 30% 20% 35% 30% 26% 28% 20% 10% 0% Male 15‐ 24 years Female Male 25‐ 34 years (N=711) #AIDS 2016 | @AIDS_conference Female Male 35‐ 44 years (N=1, 575) Female Male 45‐ 59(N=1, 551) years Female (N=1, 282)
Incidence • 15, 933 round 1 participants enrolled in round 2 • 11, 822 were HIV negative in round 1 and tested again (58% of round 1 HIV negative) • 550 tested HIV positive in round 2 • Incidence analysis is restricted to residents who tested HIV‐negative in round 1 and retested in round 2 • Adjusted incidence rates (IR) per 100 person‐years were estimated with a generalized linear model using SAS 9. 4 #AIDS 2016 | @AIDS_conference
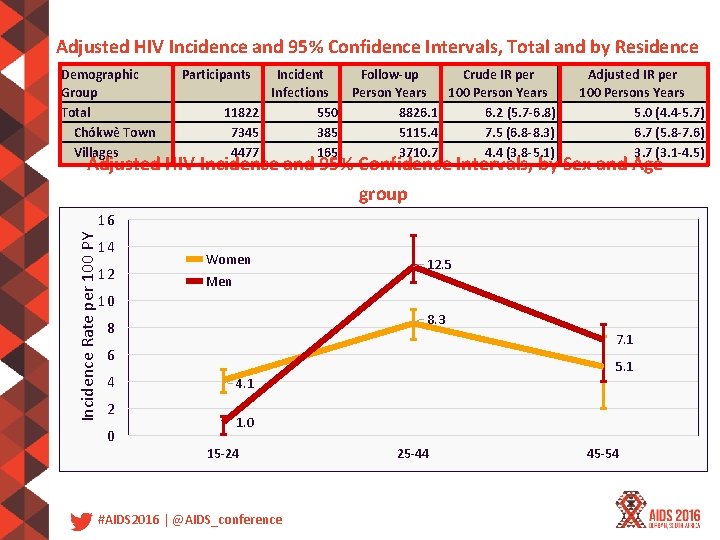
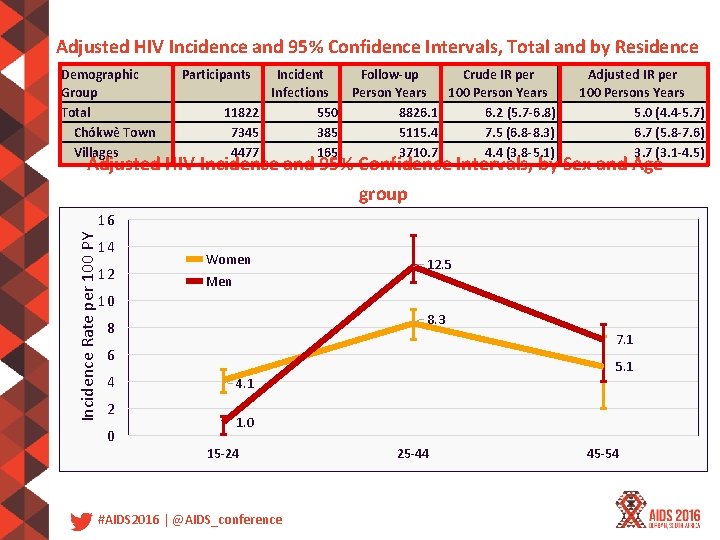
Adjusted HIV Incidence and 95% Confidence Intervals, Total and by Residence Demographic Group Total Chókwè Town Villages Participants Incident Follow-up Crude IR per Infections Person Years 100 Person Years 11822 550 8826. 1 6. 2 (5. 7 -6. 8) 7345 385 5115. 4 7. 5 (6. 8 -8. 3) 4477 165 3710. 7 4. 4 (3. 8 -5. 1) Adjusted IR per 100 Persons Years 5. 0 (4. 4 -5. 7) 6. 7 (5. 8 -7. 6) 3. 7 (3. 1 -4. 5) Adjusted HIV Incidence and 95% Confidence Intervals, by Sex and Agegroup Incidence Rate per 100 PY 16 14 12 Women Men 12. 5 10 8. 3 8 7. 1 6 4 2 0 5. 1 4. 1 1. 0 15 -24 #AIDS 2016 | @AIDS_conference 25 -44 45 -54
Limitations • Findings are preliminary. Round 2 data are still being validated and cleaned • Results were not weighted to account for underlying HDSS demographic distribution • Findings may be subject to bias of unknown magnitude and direction – Approximately half of HDSS residents tested in round 1 – Only 60% of HIV‐negative participants re‐tested in round 2 – Men were under‐represented in both rounds #AIDS 2016 | @AIDS_conference
Conclusion • HIV incidence is exceptionally high among residents aged 25‐ 44 years in Chókwè District. Among persons under 25 years, HIV incidence is higher in women than men; among persons older than 25, incidence is higher in men • ART coverage in round 1 was low, at 51%. Coverage by age‐group and sex was lowest at 20% among men ages 15‐ 24 • To reduce HIV incidence, combined evidence‐based HIV prevention interventions such as HIV testing and linkage to care, antiretroviral treatment as prevention, and male circumcision should be scaled up in Chókwè District • The district has been selected by the Ministry of Health to pilot test‐and‐start beginning in 2016 • The Chokwe HDSS is well positioned to measure the impact of these interventions #AIDS 2016 | @AIDS_conference

Acknowledgements CITSC Ricardo Thompson Juvencio Bonzela Didier Mugabe Jose Come Salvador Machava Jhpiego/Anglican Church Judite Cardoso Argentina Balate Alegria Bendzane CDC-Mozambique Provincial Public Health Alfredo Vergara Directorate Edgar Monterroso Isaias Ramiro Stan Wei Bertur Alface Isabelle Casavant Braiton Maculuve Daniel Shodell Nick Schaad Peter Young CDC-Atlanta Duncan Mac. Kellar Irene Benech Jan Moore Robert Nelson Andrew Auld Ishani Pathmanathan Laura Broyles Sherri Pals Bharat Parekh Chunfu Yang Susan Nkengasong Eduardo Valverde This research has been supported by the President’s Emergency Plan for AIDS Relief (PEPFAR) through the Centers for Disease Control and Prevention under the terms of GH 11‐ 1158 and PS 09‐ 905. #AIDS 2016 | @AIDS_conference
Contact rnelson 1@cdc. gov #AIDS 2016 | @AIDS_conference
 Attack rate epidemiology formula
Attack rate epidemiology formula Incidence vs incidence rate
Incidence vs incidence rate White men are saving brown women from brown men
White men are saving brown women from brown men Of mice and men chapter 1
Of mice and men chapter 1 Box plots gcse questions
Box plots gcse questions Difference between mens and womens soccer
Difference between mens and womens soccer Economic activities by men and women
Economic activities by men and women Wake up my brain
Wake up my brain Pornography: men possessing women
Pornography: men possessing women Woman feet
Woman feet Phil 4 3
Phil 4 3 What men wish women knew
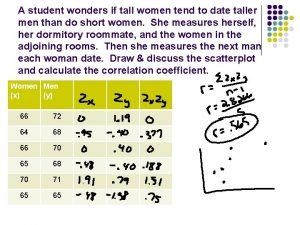
What men wish women knew A student wonders if tall women tend to date taller men
A student wonders if tall women tend to date taller men Women give men chocolate on valentines day
Women give men chocolate on valentines day Understanding the management process
Understanding the management process Ongoing professional practice evaluation template
Ongoing professional practice evaluation template