One Lung Ventilation Llalando L Austin II MHSc


- Slides: 47
One Lung Ventilation Llalando L. Austin II, MHSc, AA-C, RRT Nova Southeastern University
Objectives • Describe One Lung Ventilation • Understand the methods for securing one lung ventilation • Learn the indications and contraindications for each procedure • Understand hypoxic pulmonary vasoconstriction (HPV) • Understand commonly associated surgical procedures that require one lung ventilation • Common techniques and supplies for one lung ventilation • Understand the case setup and patient preparation for the procedure

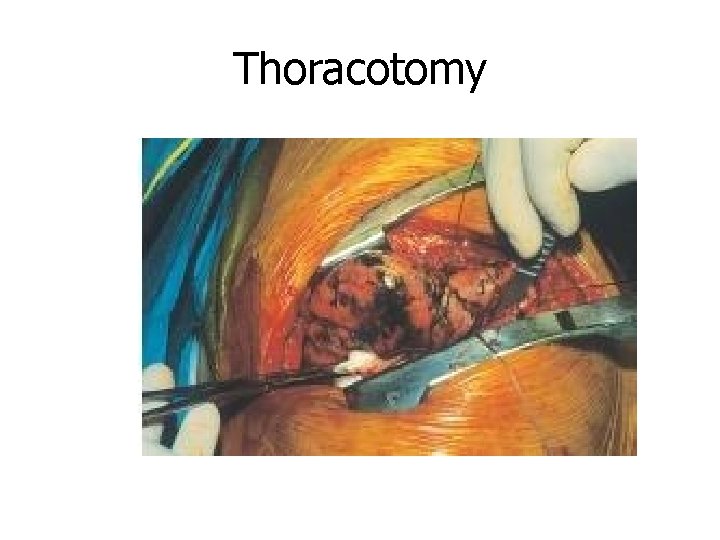
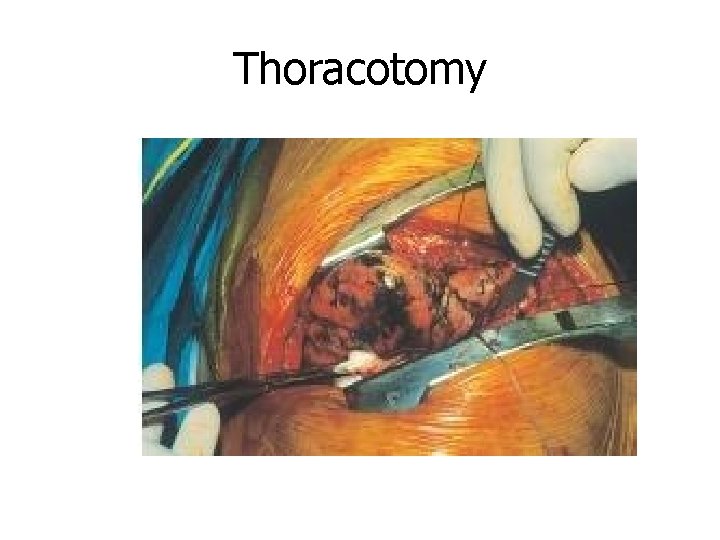
Thoracotomy
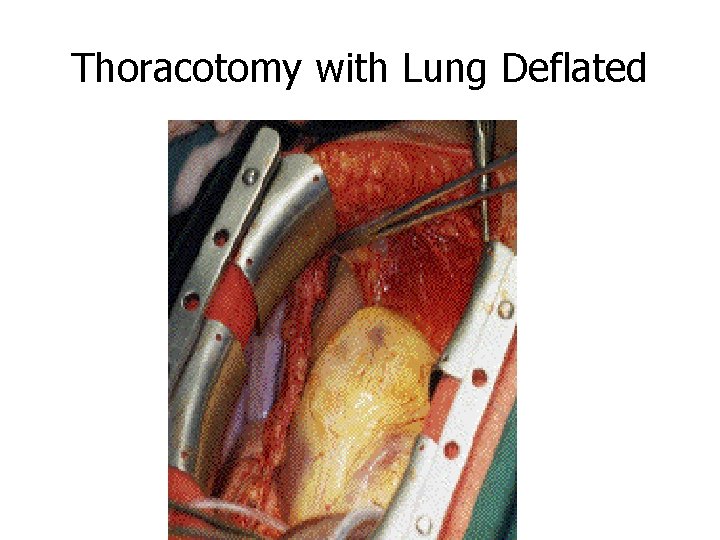
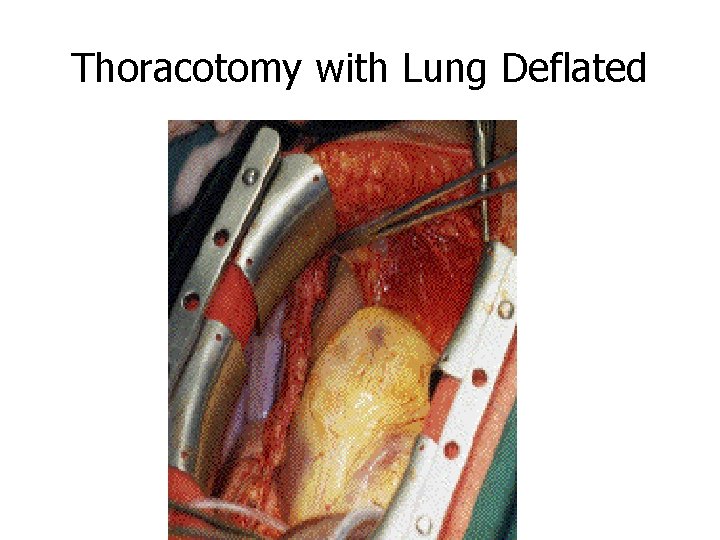
Thoracotomy with Lung Deflated
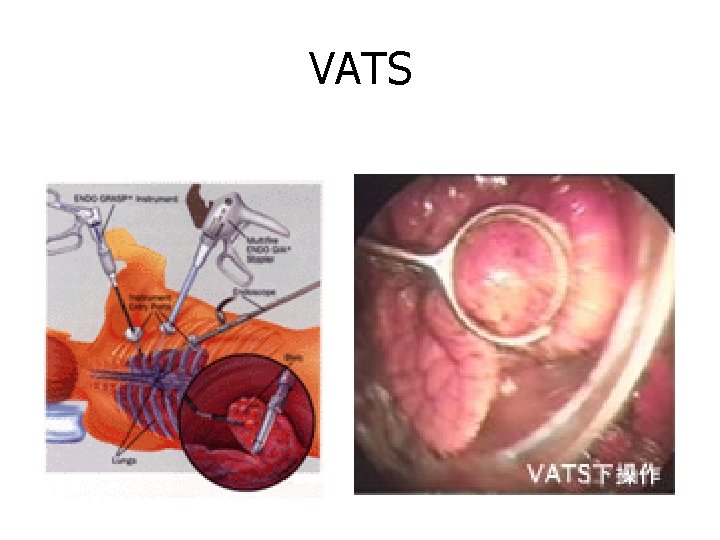
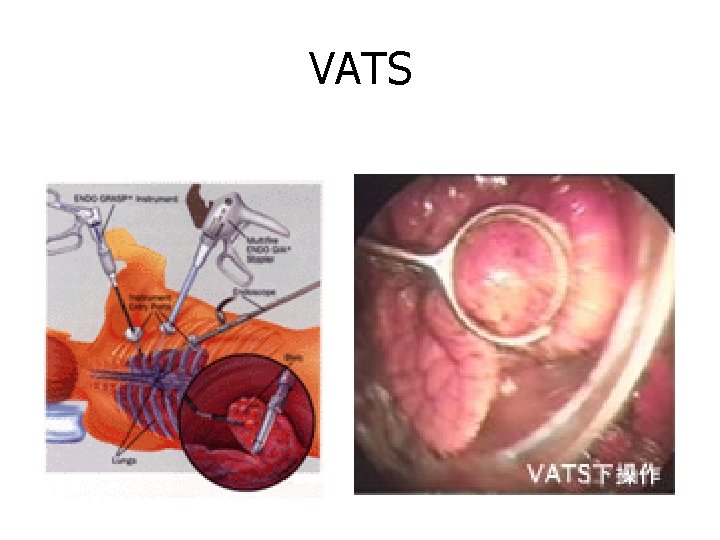
VATS
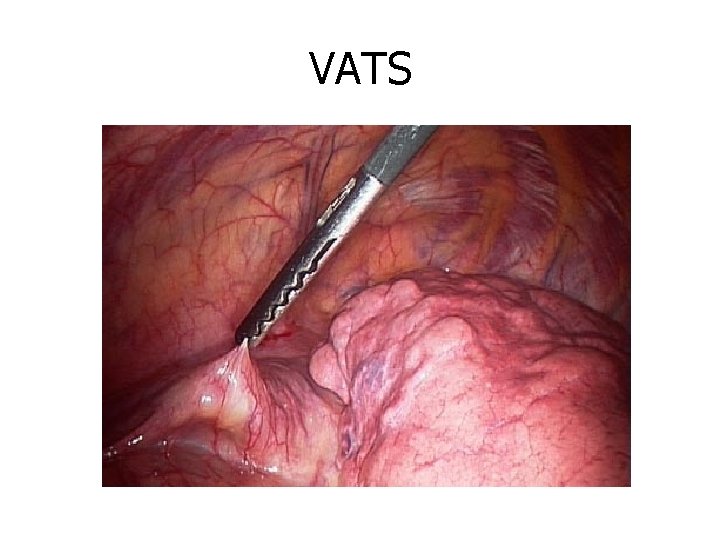
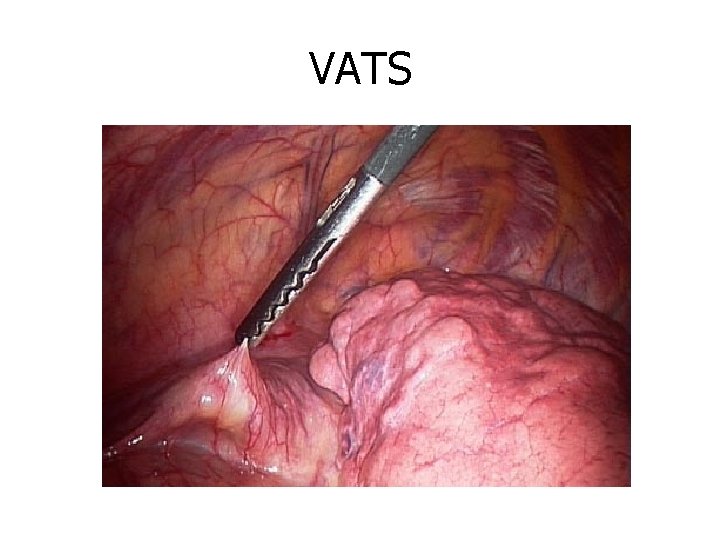
VATS
VATS
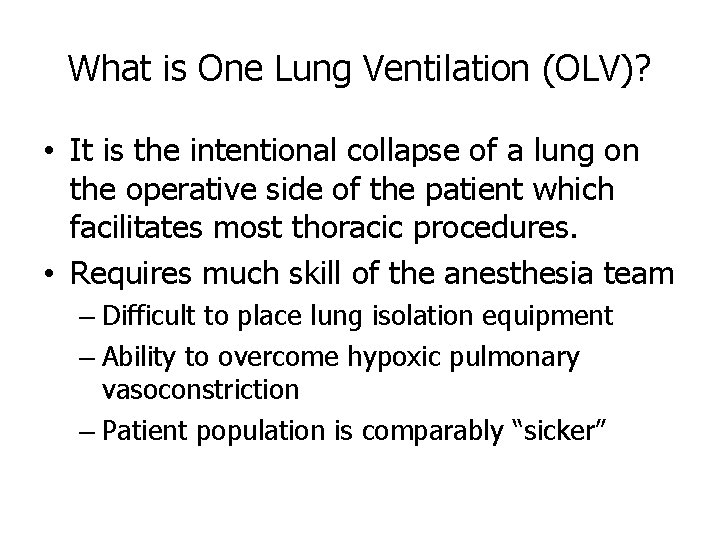
What is One Lung Ventilation (OLV)? • It is the intentional collapse of a lung on the operative side of the patient which facilitates most thoracic procedures. • Requires much skill of the anesthesia team – Difficult to place lung isolation equipment – Ability to overcome hypoxic pulmonary vasoconstriction – Patient population is comparably “sicker”
Definition of Terms • Dependent Lung or Down Lung – The lung that is ventilated • Non-dependent Lung or Up Lung – The lung that is collapsed to facilitate the surgery
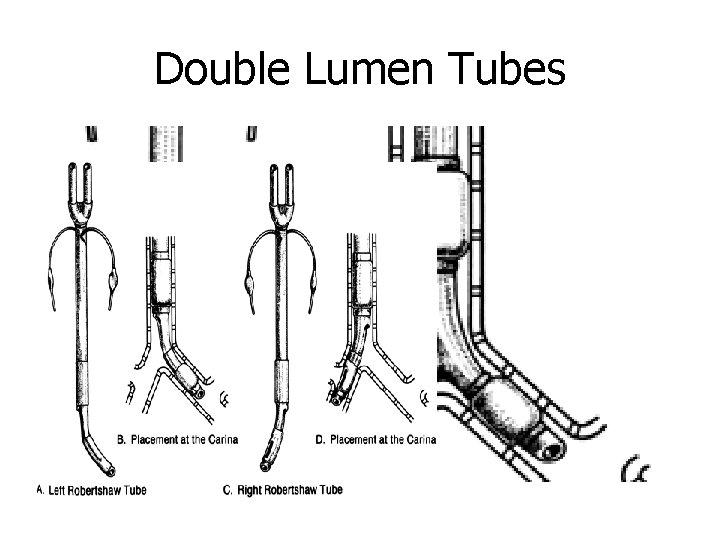
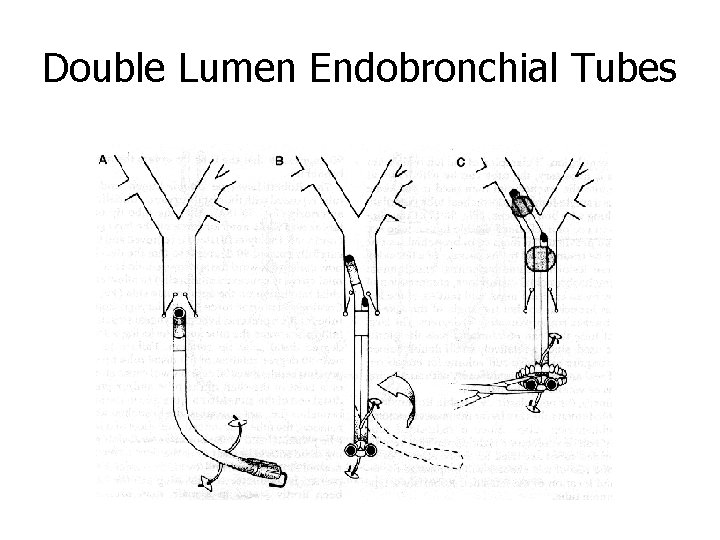
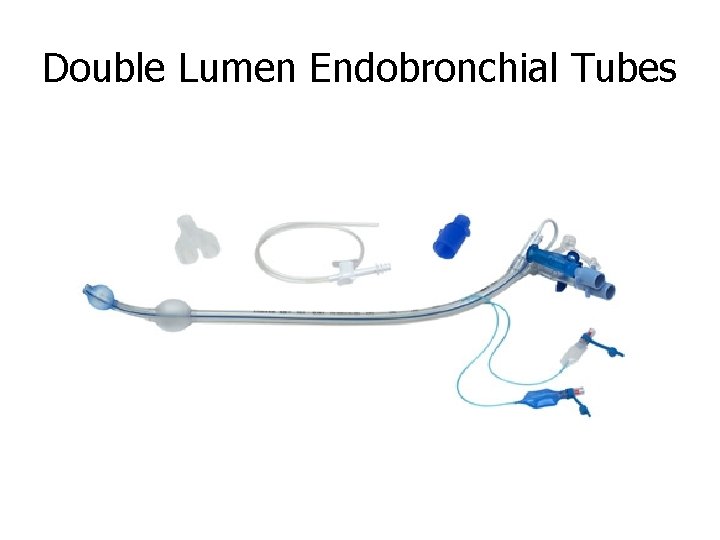
Methods of Lung Separation • Bronchial blockers – Single-lumen tracheal tubes w/ a bronchial blocker (Univent) – Arterial embolectomy catheter (ie Fogarty) • Single-lumen endobronchial tubes – Gordon-Green tube (carinal hook) • Double-lumen endobronchial tubes – – Robert-Shaw (R or L), Carlens (R), White (L) Carlens and White both have carinal hooks From 35 Fr to 41 Fr (35, 37, 39, 41) 26 Fr smallest size • Used for children as young as 8 years – 28 Fr and 32 Fr used for pediatric patients 10 and older
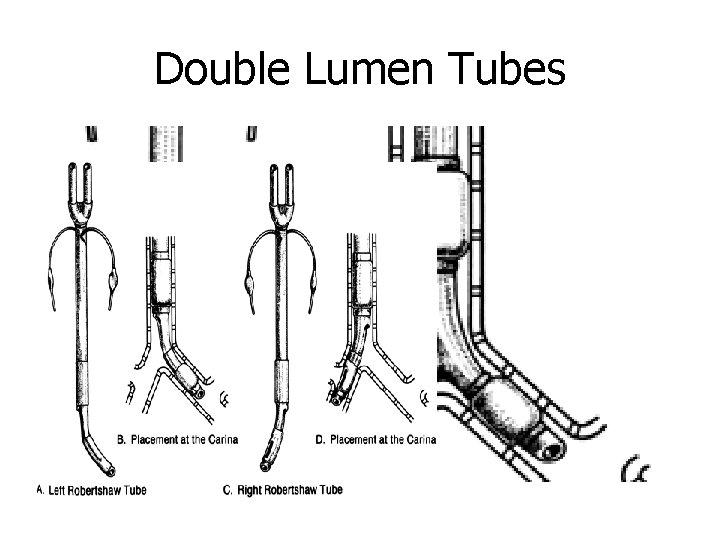
Double Lumen Tubes
Patient Monitoring Considerations • Direct arterial catheterization (a-line) – essential for nearly all thoracic cases – Allows for beat-to-beat blood pressure analysis – Sampling for determination of ABG • Central venous pressure monitoring (central line) – essential for measuring right atrial and right ventricular pressures – Useful in monitoring: • large volume shifts • hypovolemia • need for vasoactive drugs • Pulmonary artery catheterization – left sided filling pressures, cardiac output – Calculation of derived hemodynamic and respiratory parameters and clinical use of Starling curve – Most PA catheters (more than 90%) float to and locate in the right lung due to increased pulmonary blood flow • Create inaccurate reading for R thoracotomies
Patient Monitoring Considerations n Oxygenation and Ventilation n Monitoring inspired oxygen n Sampling of arterial blood for ABGs n Pulse oximetry n Transcutaneous oxygen tension n for neonates n Qualitative signs n chest expansion n observation of reservoir bag n auscultation of breath sounds n Et. CO 2 measurement, capnograph
Indications for One-Lung Ventilation • Absolute – Isolation of one lung from another to prevent spillage or contamination (infection, massive hemorrhage) – Control of distribution of ventilation • Bronchopleural fistula • Surgical opening of major conducting airway – Unilateral bronchopulmonary lavage • Ex: pulmonary alveolar proteinosis

Indications for One-Lung Ventilation n Relative n Surgical exposure- high priority n Thoracic aortic aneurysm n Pneumonectomy n Upper lobectomy n Surgical exposure- lower priority n Middle lobectomies n Esophageal resection n Thoracoscopy n Thoracic spine procedures n Post-removal of totally-occluding chronic unilateral pulmonary emboli
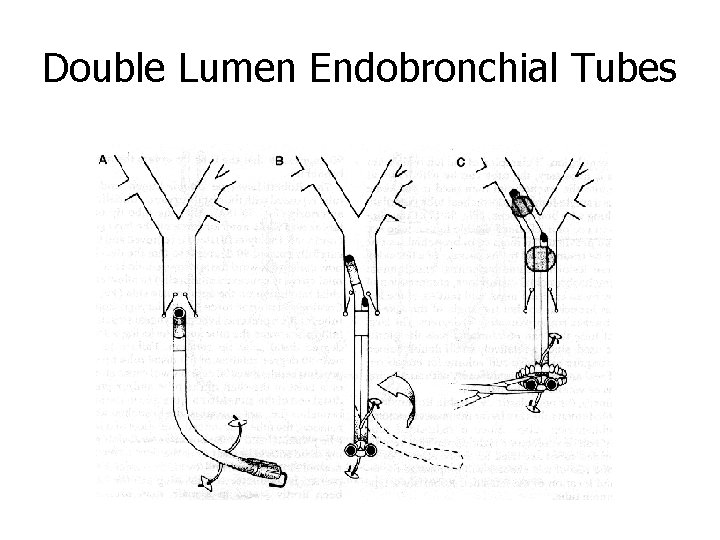
Double Lumen Endobronchial Tubes
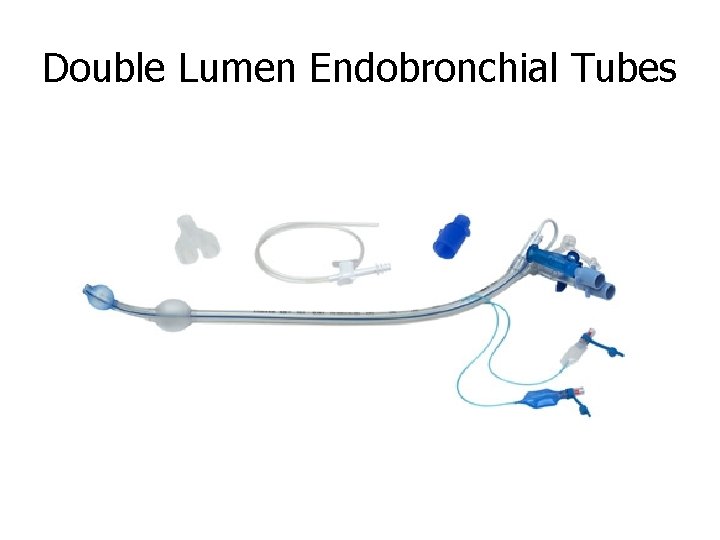
Double Lumen Endobronchial Tubes
Advantages n Relatively easy to place n Allow conversion back and forth from OLV to twolung ventilation n Allow suctioning of both lungs individually n Allow CPAP to be applied to the non-dependent lung n Allow PEEP to be applied to the dependent lung n Ability to ventilate around scope in the tube
Disadvantages • Cannot take patient to PACU or the Unit • Must be changed out for a regular ETT if post-op ventilation • Correct positioning is dependent on appropriate size for height of patient – Length of trachea
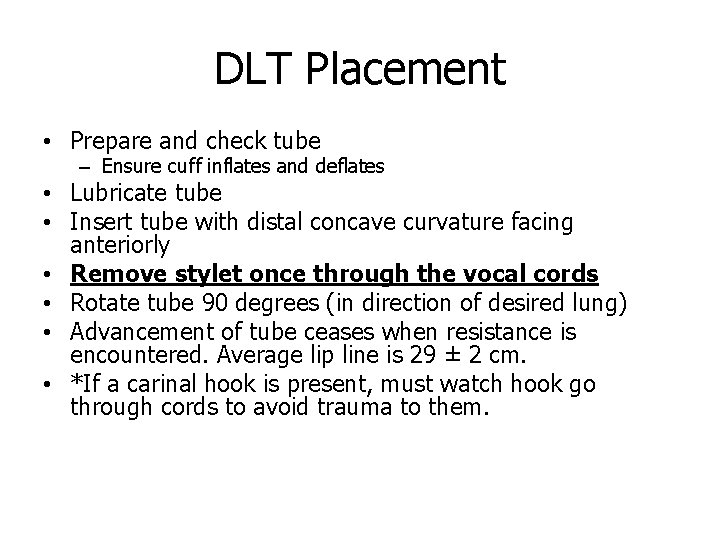
DLT Placement • Prepare and check tube – Ensure cuff inflates and deflates • Lubricate tube • Insert tube with distal concave curvature facing anteriorly • Remove stylet once through the vocal cords • Rotate tube 90 degrees (in direction of desired lung) • Advancement of tube ceases when resistance is encountered. Average lip line is 29 ± 2 cm. • *If a carinal hook is present, must watch hook go through cords to avoid trauma to them.
DLT Placement • Check for placement by auscultation • Inflate tracheal cuff- expect equal lung ventilation • Clamp the white side (marked "tracheal" for left-sided tube) and remove cap from the connector – Expect some left sided ventilation through bronchial lumen, and some air leak past bronchial cuff, which is not yet inflated • Slowly inflate bronchial cuff until minimal or no leak is heard at uncapped right connector – Go slow- it only requires 1 -3 cc of gas and bronchial rupture is a risk • Remove the clamp and replace the cap on the tracheal side • Check that both lungs are ventilated • Selectively clamp each side, and expect visible chest movement and audible breath sounds only on the right when left is clamped, and vice versa
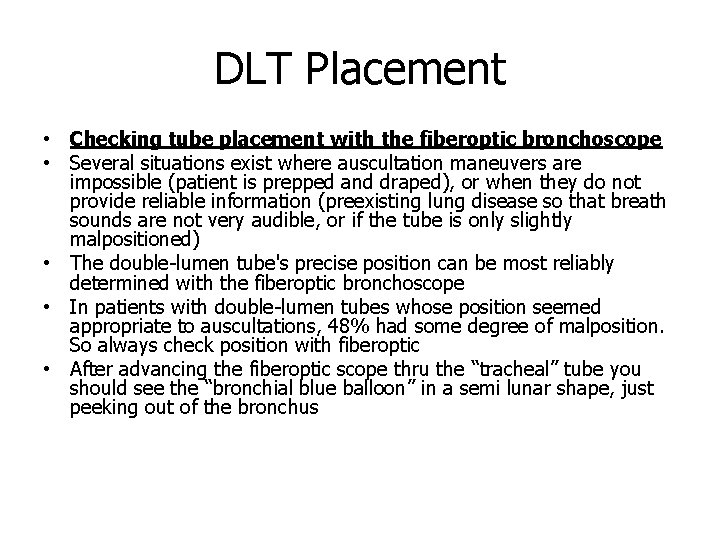
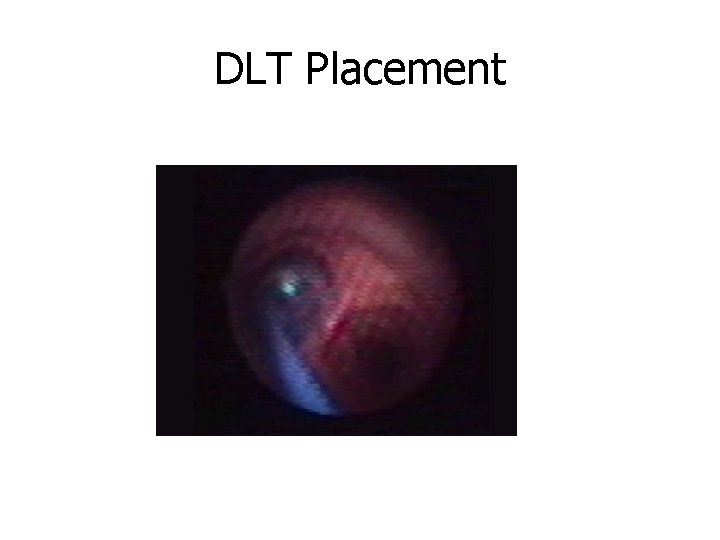
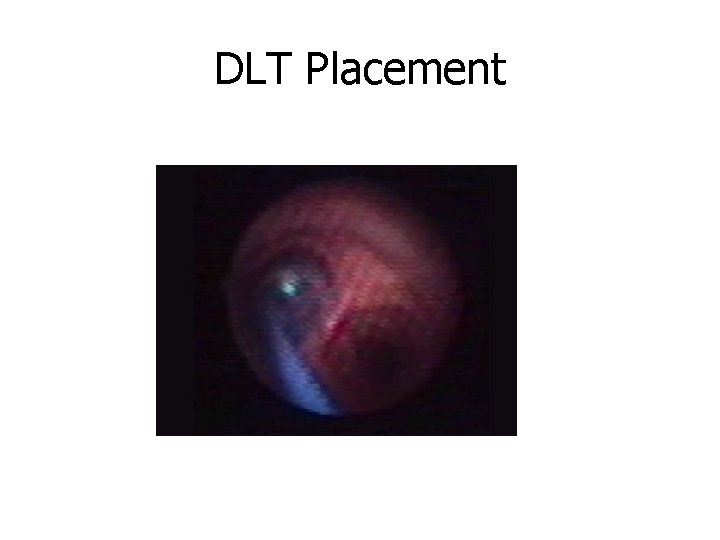
DLT Placement • Checking tube placement with the fiberoptic bronchoscope • Several situations exist where auscultation maneuvers are impossible (patient is prepped and draped), or when they do not provide reliable information (preexisting lung disease so that breath sounds are not very audible, or if the tube is only slightly malpositioned) • The double-lumen tube's precise position can be most reliably determined with the fiberoptic bronchoscope • In patients with double-lumen tubes whose position seemed appropriate to auscultations, 48% had some degree of malposition. So always check position with fiberoptic • After advancing the fiberoptic scope thru the “tracheal” tube you should see the “bronchial blue balloon” in a semi lunar shape, just peeking out of the bronchus
DLT Placement
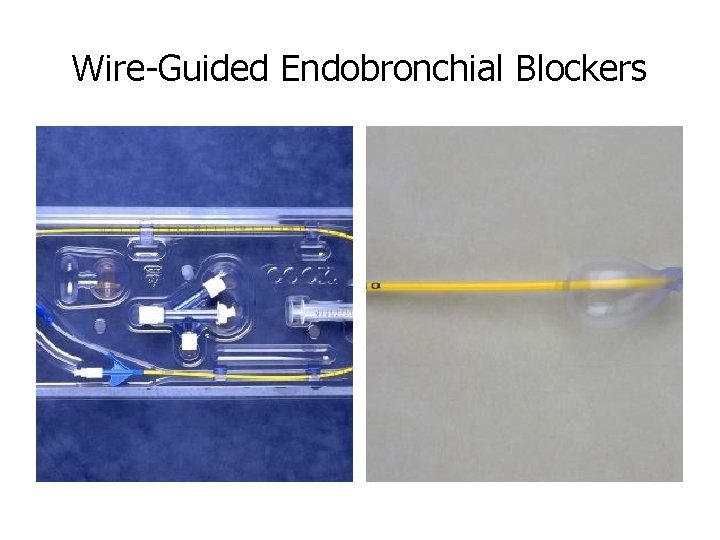
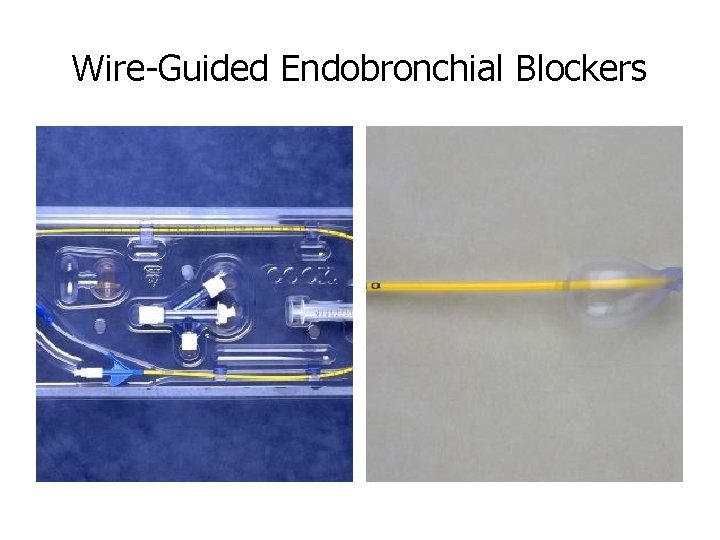
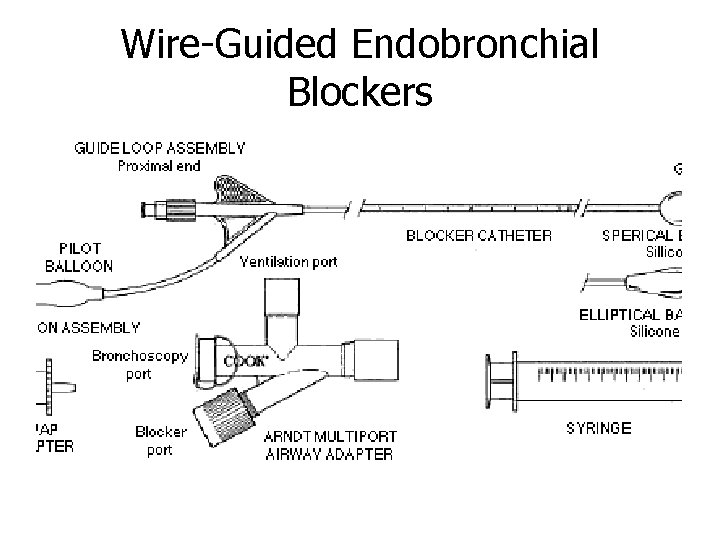
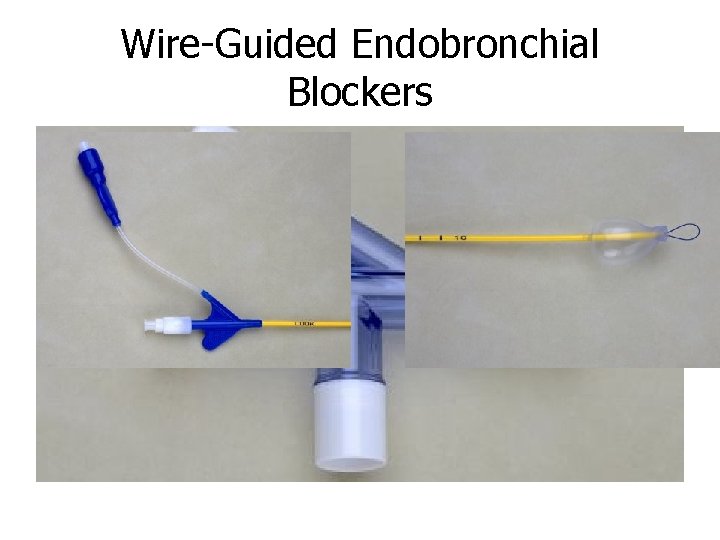
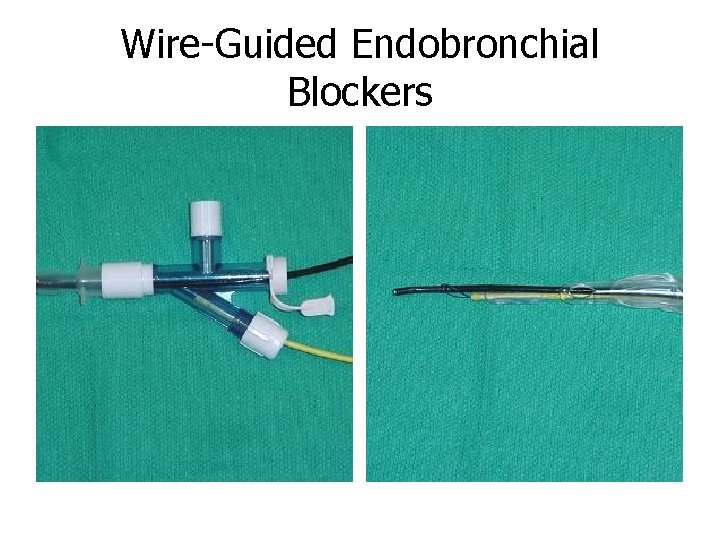
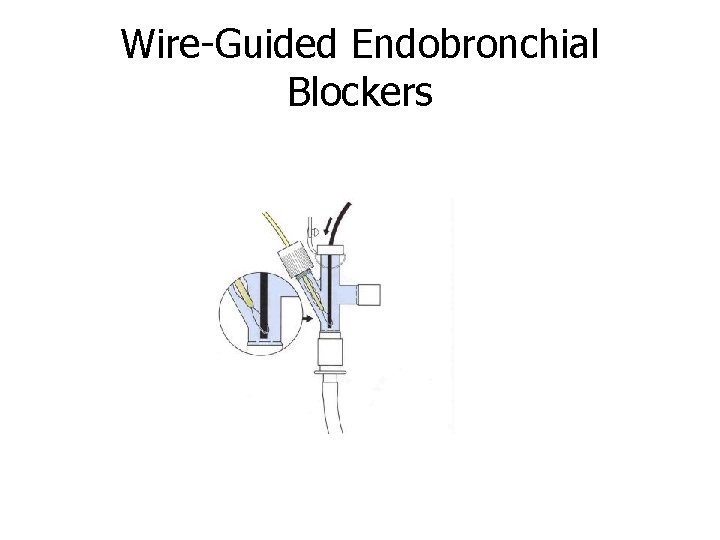
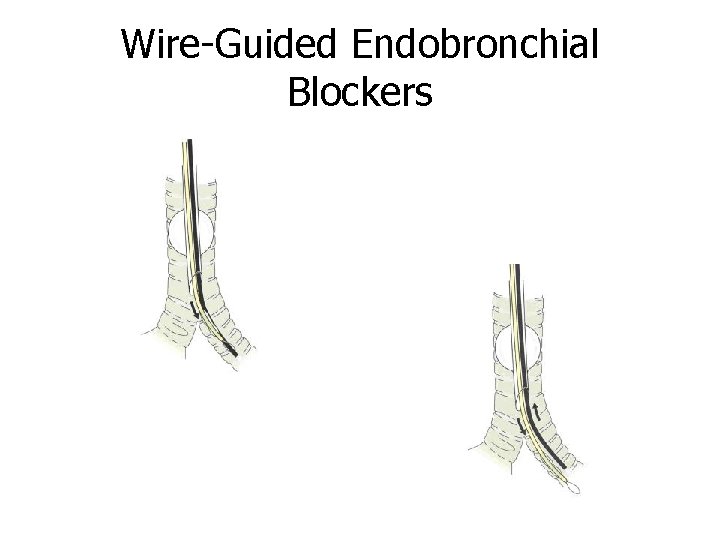
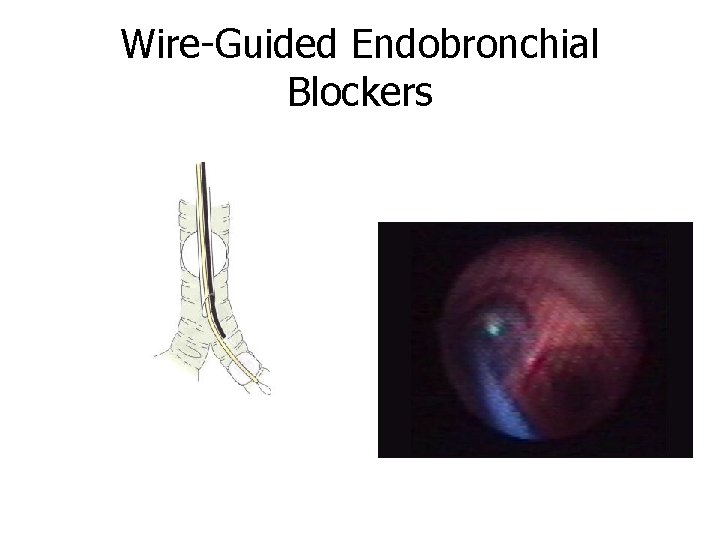
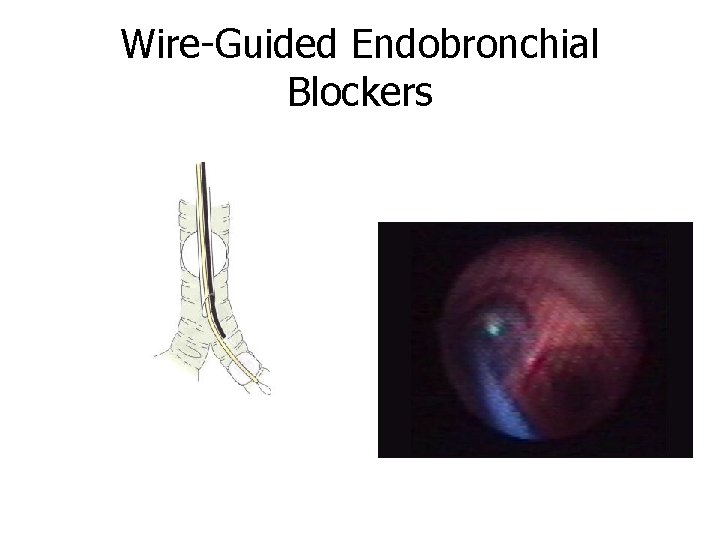
Wire-Guided Endobronchial Blockers
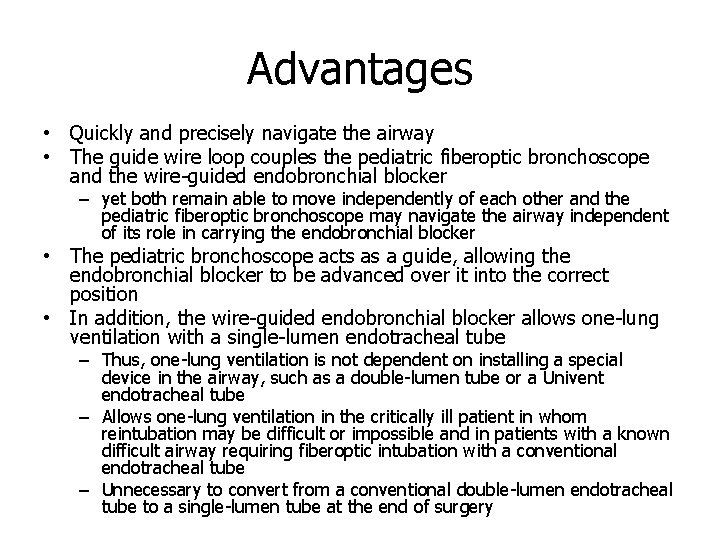
Advantages • Quickly and precisely navigate the airway • The guide wire loop couples the pediatric fiberoptic bronchoscope and the wire-guided endobronchial blocker – yet both remain able to move independently of each other and the pediatric fiberoptic bronchoscope may navigate the airway independent of its role in carrying the endobronchial blocker • The pediatric bronchoscope acts as a guide, allowing the endobronchial blocker to be advanced over it into the correct position • In addition, the wire-guided endobronchial blocker allows one-lung ventilation with a single-lumen endotracheal tube – Thus, one-lung ventilation is not dependent on installing a special device in the airway, such as a double-lumen tube or a Univent endotracheal tube – Allows one-lung ventilation in the critically ill patient in whom reintubation may be difficult or impossible and in patients with a known difficult airway requiring fiberoptic intubation with a conventional endotracheal tube – Unnecessary to convert from a conventional double-lumen endotracheal tube to a single-lumen tube at the end of surgery
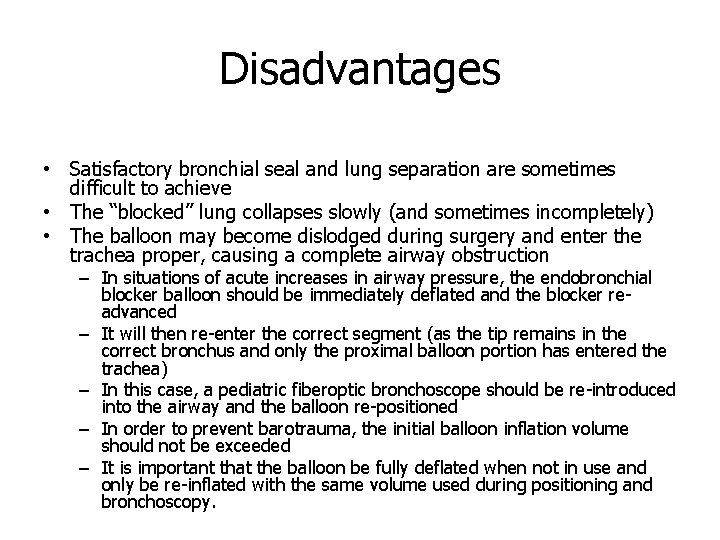
Disadvantages • Satisfactory bronchial seal and lung separation are sometimes difficult to achieve • The “blocked” lung collapses slowly (and sometimes incompletely) • The balloon may become dislodged during surgery and enter the trachea proper, causing a complete airway obstruction – In situations of acute increases in airway pressure, the endobronchial blocker balloon should be immediately deflated and the blocker readvanced – It will then re-enter the correct segment (as the tip remains in the correct bronchus and only the proximal balloon portion has entered the trachea) – In this case, a pediatric fiberoptic bronchoscope should be re-introduced into the airway and the balloon re-positioned – In order to prevent barotrauma, the initial balloon inflation volume should not be exceeded – It is important that the balloon be fully deflated when not in use and only be re-inflated with the same volume used during positioning and bronchoscopy.
Indications for Wire-Guided Endobronchial Blockers vs. DLT • • • Critically ill patients Rapid sequence induction Known and unknown difficult airway Postoperative intubation Small adult and pediatric patients Obese adults
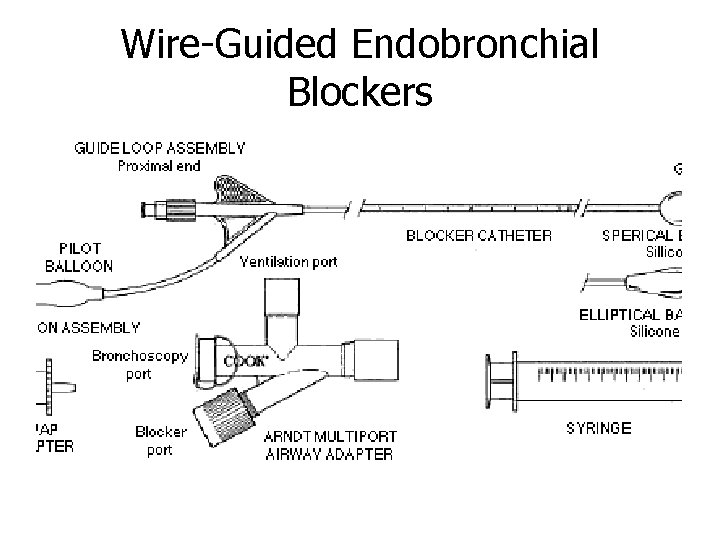
Wire-Guided Endobronchial Blockers
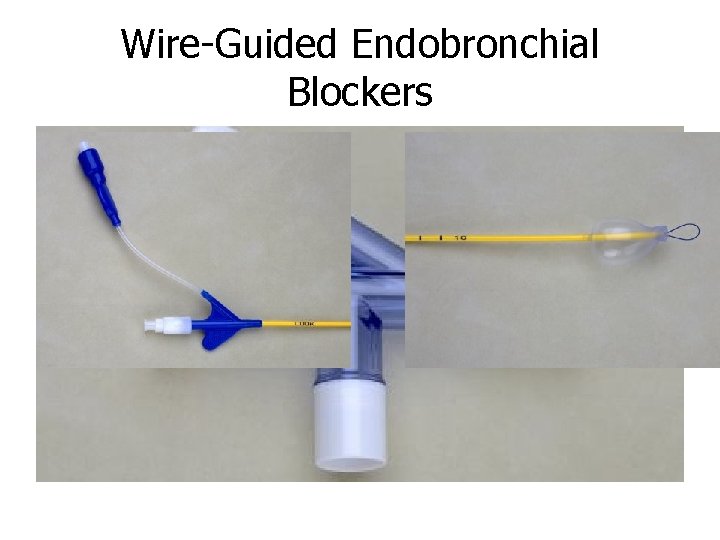
Wire-Guided Endobronchial Blockers
Wire-Guided Endobronchial Blockers • Available sizes – Adult 9 Fr – Pediatric 5 Fr
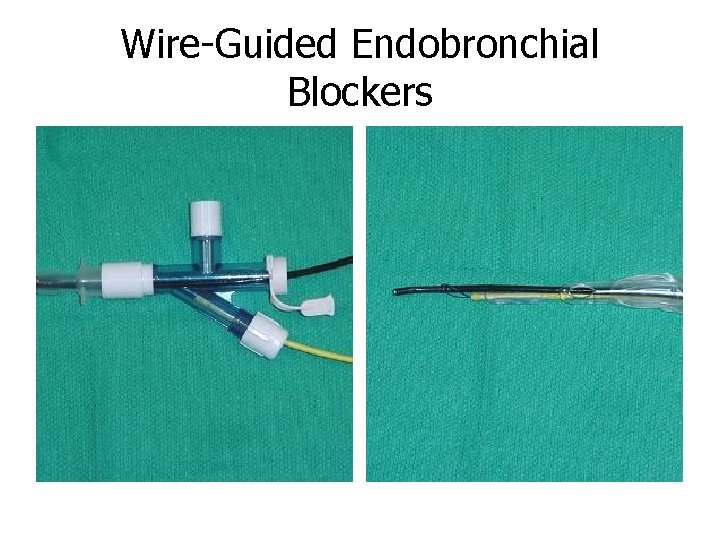
Wire-Guided Endobronchial Blockers
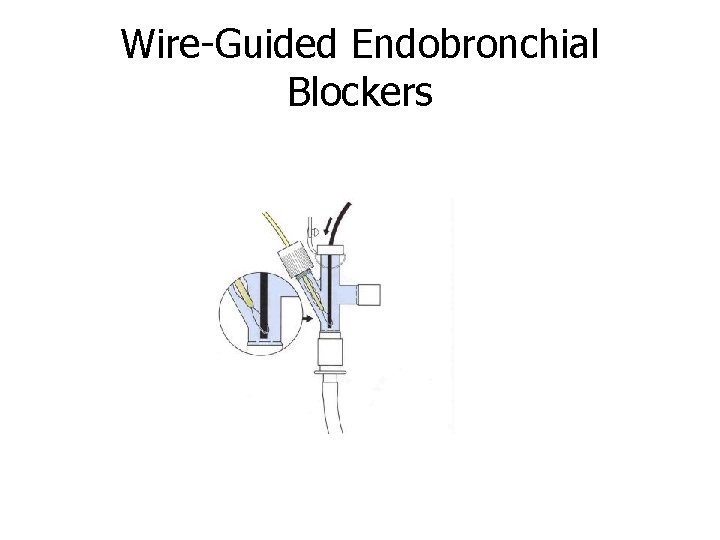
Wire-Guided Endobronchial Blockers
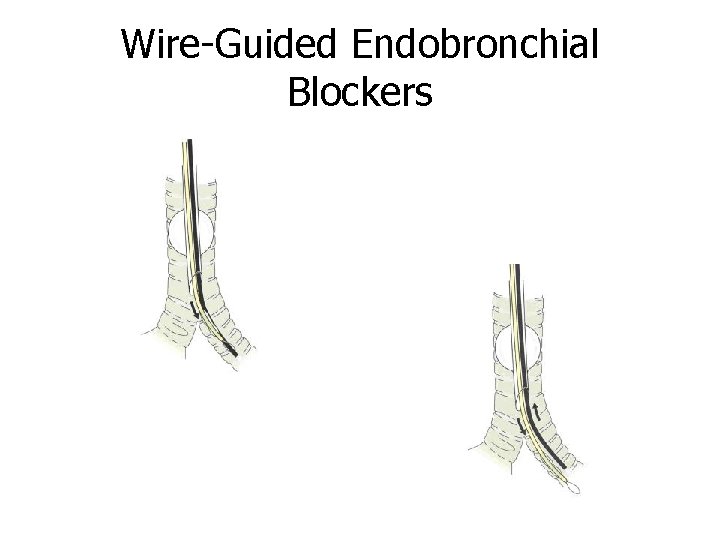
Wire-Guided Endobronchial Blockers
Wire-Guided Endobronchial Blockers
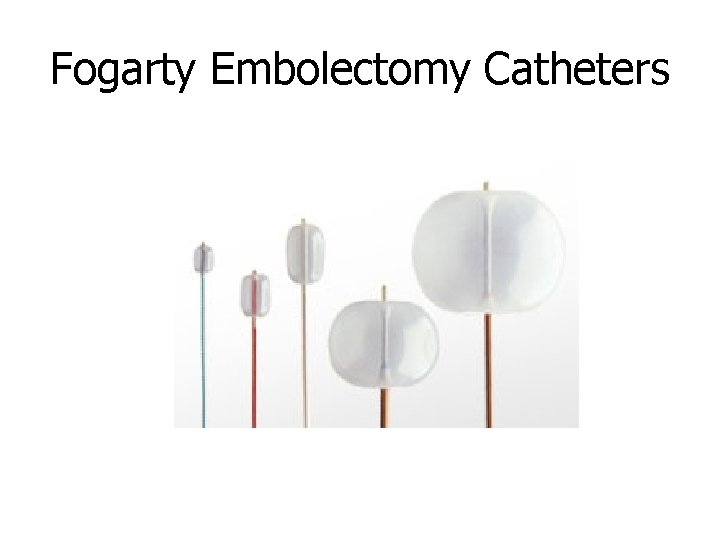
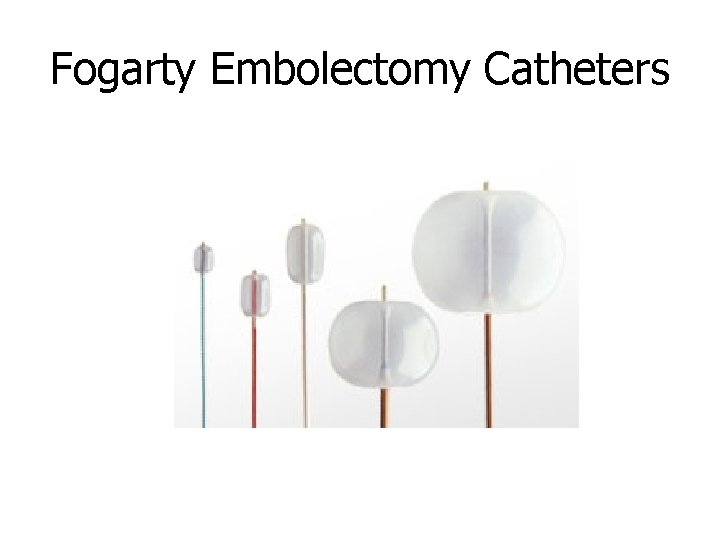
Fogarty Embolectomy Catheters
Fogarty Embolectomy Catheter • Single-lumen balloon tipped catheter with a removable stylet • In the parallel fashion, the Fogarty catheter is inserted prior to intubation • In the co-axial fashion, the Fogarty catheter is placed through the endotracheal tube • Both techniques require fiberoptic bronchoscopy to direct the Fogarty catheter into the correct pulmonary segment • Once the catheter is in place, the balloon is inflated, sealing the airway • Clinical limitations to the Fogarty technique – Difficult to direct and cannot be coupled to a fiberoptic bronchoscope – No accessory lumen for either removal of gas from the blocked segment or insufflation of oxygen to reverse hypoxemia – Ventilate w/ 100% O 2 prior to balloon inflation to aid in gas removal
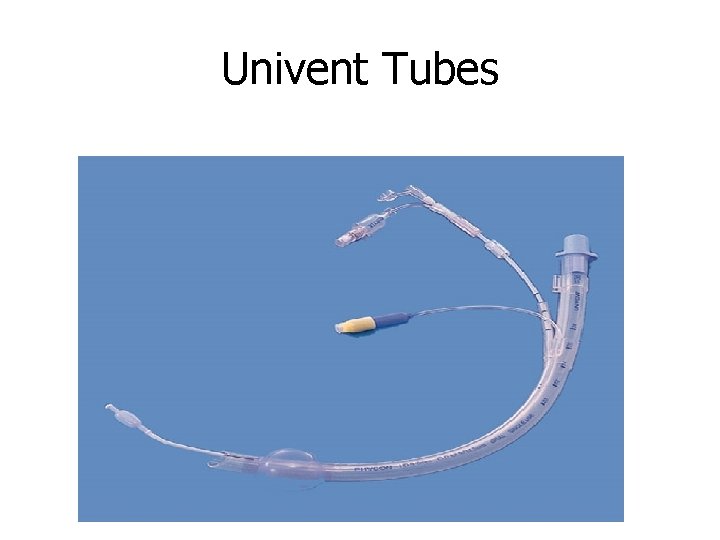
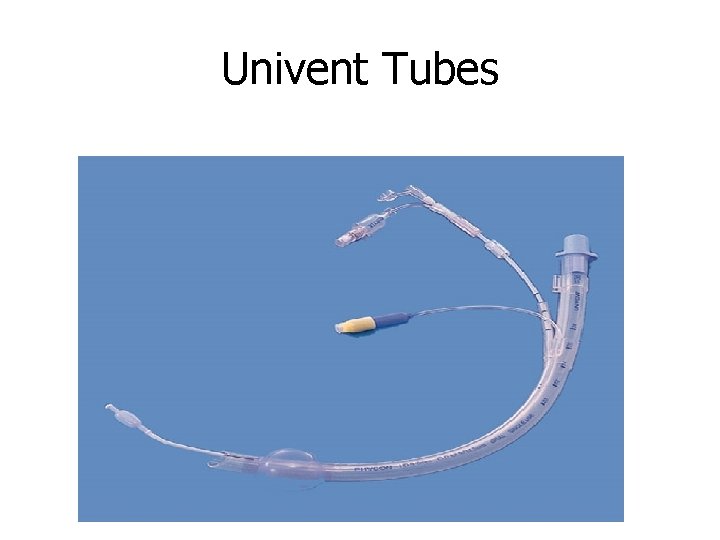
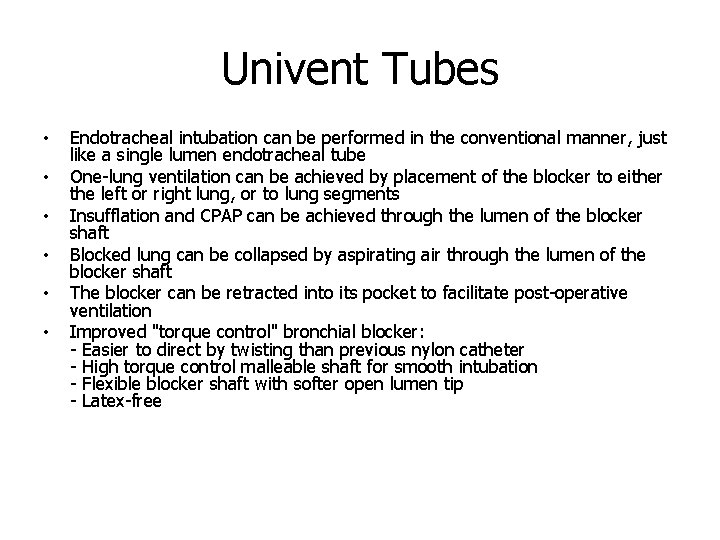
Univent Tubes
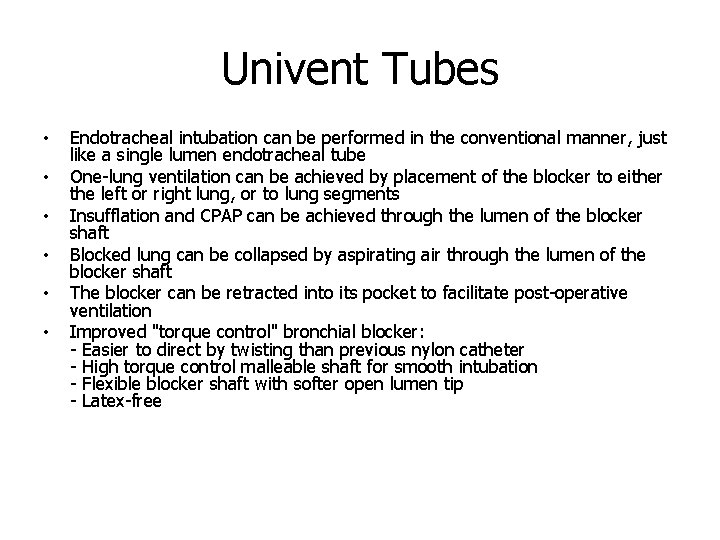
Univent Tubes • • • Endotracheal intubation can be performed in the conventional manner, just like a single lumen endotracheal tube One-lung ventilation can be achieved by placement of the blocker to either the left or right lung, or to lung segments Insufflation and CPAP can be achieved through the lumen of the blocker shaft Blocked lung can be collapsed by aspirating air through the lumen of the blocker shaft The blocker can be retracted into its pocket to facilitate post-operative ventilation Improved "torque control" bronchial blocker: - Easier to direct by twisting than previous nylon catheter - High torque control malleable shaft for smooth intubation - Flexible blocker shaft with softer open lumen tip - Latex-free
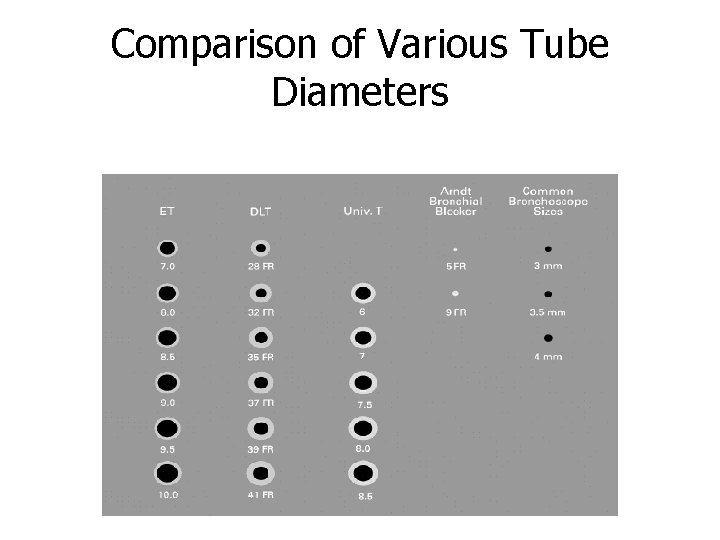
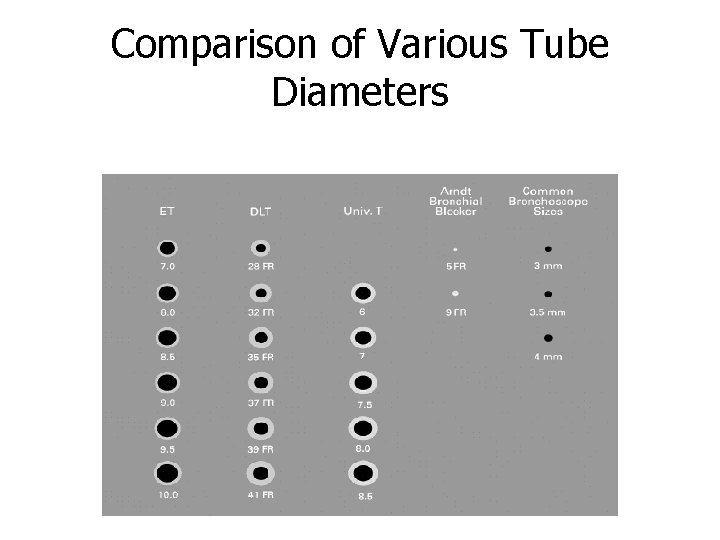
Comparison of Various Tube Diameters
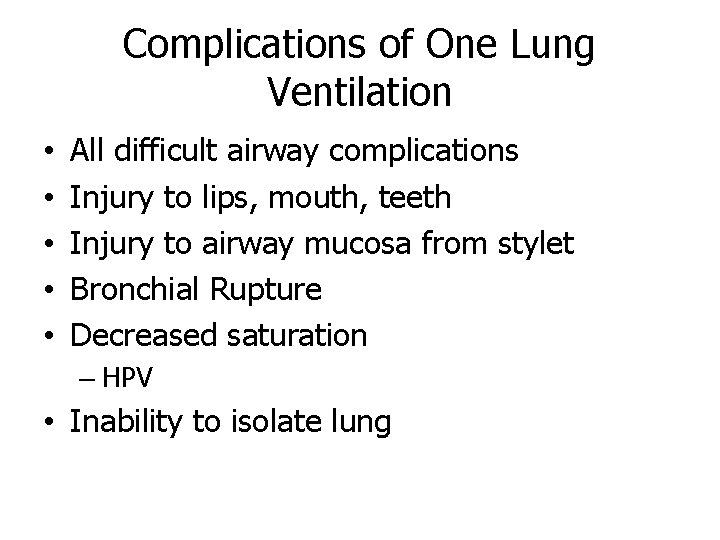
Complications of One Lung Ventilation • • • All difficult airway complications Injury to lips, mouth, teeth Injury to airway mucosa from stylet Bronchial Rupture Decreased saturation – HPV • Inability to isolate lung
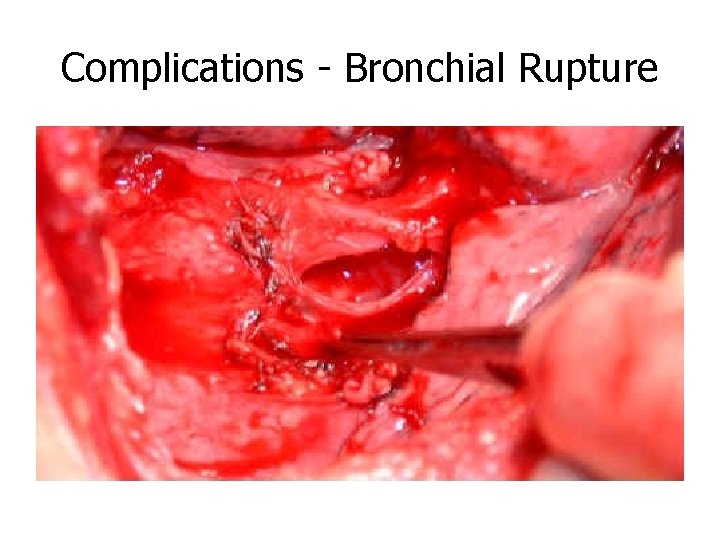
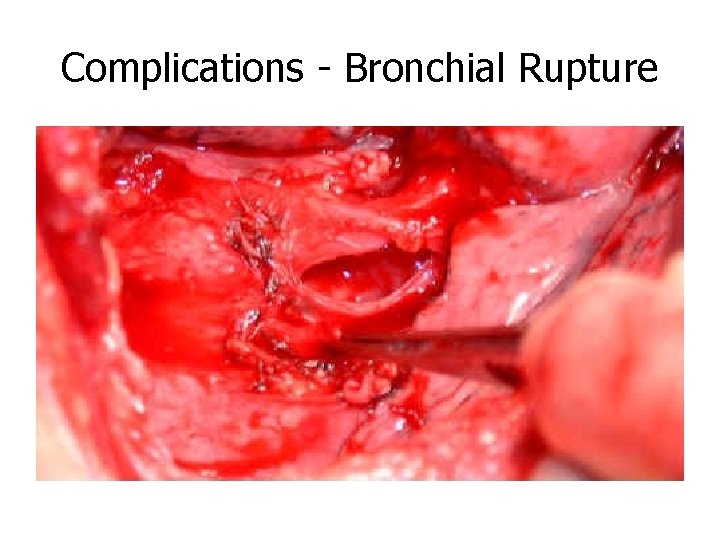
Complications - Bronchial Rupture
Hypoxic Pulmonary Vasoconstriction • Hypoxia is a powerful stimulus for pulmonary vascular constriction • Body’s mechanism to divert blood flow away from areas of no ventilation to areas of ventilation • Vasoconstriction that decreases blood flow from alveoli that are not ventilated to alveoli that are ventilated • Body’s way to decrease the shunt that was created by change – Position – V/Q mismatch
HPV • Body’s compensatory mechanism for hypoxia • Clinical Notes: – Direct acting vasodilators inhibit HPV response – Volatile agents at higher concentrations inhibit HPV response • No HPV = – Increases shunt – Decreases Pa. O 2
Management of Hypoxia in One Lung Ventilation • 100% FIO 2 • 10 m. L/kg tidal volume – Do not change the tidal volume from 2 lung ventilation • • Maintain normocapnia Maintain correct tube position Suction both lungs Apply PEEP to dependant lung Apply CPAP to non-dependant lung Re-inflate collapsed lung at various intervals Extreme cases – Clamp the pulmonary artery to collapsed lung
Case Setup for DLT & OLV • MSMAID • Preferred blade and handle • Airway – Have standard supplies & assortment of sizes for DLT or other OLV choice equipment • Fiberoptic cart • Hemostats or clamps to clamp off lumens of the tube • Suction!!
References n http: //ourworld. cs. com/_ht_a/doschk/onelung. htm n Finucane and Santora n Morgan and Mikhail n Barash, Cullen, Stoelting
 Modes of mechanical ventilation
Modes of mechanical ventilation One god one empire one emperor
One god one empire one emperor Little dog run
Little dog run One king one law one faith
One king one law one faith One empire one god one emperor
One empire one god one emperor Ford one plan
Ford one plan See one do one teach one
See one do one teach one See one, do one, teach one
See one, do one, teach one Twelfth night speeches
Twelfth night speeches Studiendekanat uni bonn
Studiendekanat uni bonn One vision one identity one community
One vision one identity one community One vision one identity one community
One vision one identity one community Lev hood
Lev hood Contoh ventilasi buatan
Contoh ventilasi buatan Gun range ventilation
Gun range ventilation Mode of ventilation
Mode of ventilation Jay taneja
Jay taneja Minute ventilation normal
Minute ventilation normal Respiration vs ventilation
Respiration vs ventilation Dynamic compliance
Dynamic compliance Vertical ventilation cut sequence
Vertical ventilation cut sequence Ashrae standard 15 refrigerant monitor
Ashrae standard 15 refrigerant monitor Bag mask ventilation
Bag mask ventilation Pediatric life support algorithm
Pediatric life support algorithm How is respiration controlled
How is respiration controlled Bag mask ventilation
Bag mask ventilation Ventilation formula
Ventilation formula Architectural ventilation
Architectural ventilation 5 myths about attic ventilation
5 myths about attic ventilation T-piece ventilation images
T-piece ventilation images Mechanical ventilation indications
Mechanical ventilation indications Mechanical ventilation 101
Mechanical ventilation 101 Dyspnea index formula
Dyspnea index formula Normal minute ventilation
Normal minute ventilation Greenhouse ventilation calculator
Greenhouse ventilation calculator General shop safety rules
General shop safety rules General dilution ventilation
General dilution ventilation Iso 21789 pdf
Iso 21789 pdf 798 ventilation cut
798 ventilation cut Ss-en 12097
Ss-en 12097 Types of ventilation fire fighting
Types of ventilation fire fighting Virus that causes croup
Virus that causes croup Residential ventilation fans market
Residential ventilation fans market Ventilation
Ventilation Atkinson formula ventilation
Atkinson formula ventilation Factors affecting oxygenation in nursing foundation
Factors affecting oxygenation in nursing foundation Pulse check in unresponsive victim
Pulse check in unresponsive victim Positive end expiratory pressure
Positive end expiratory pressure