OncologyHaematology 24 Hour Telephone Triage Rapid Assessment and

- Slides: 41
Oncology/Haematology 24 Hour Telephone Triage Rapid Assessment and Access Toolkit JOAN THOMAS 1
What we will discuss today • What is triage? • The development of the UKONS toolkit • UKONS/AUS version • Why we need triage training • What we need in place to be successful 2 2
3 What is triage? • Triage : a clinical assessment process that identifies and prioritises patients according to the current or potential severity of the presenting problem
4 What is triage? In modern healthcare systems triage is used at significant points in the patient pathway to determine level of urgency and intervention required: • Triage on arrival at ED or Medical Assessment Unit. • Pre hospital triage – 000 calls or in our case 24 hour advice lines. • On site triage by the first clinician attending the patient- para-medics In order to use triage effectively the infrastructure must be in place to manage the patient appropriately.
5 Why we need triage in Oncology / Haematology • We know that Systemic Anti Cancer Treatment (SACT) will produce unwanted side effects/toxicities some of which can be life threatening • We have to provide information and appropriate support for patients receiving Systemic Anti Cancer Treatment (SACT) • We know that we do not always identify those patients at risk from side effects/toxicities
6 Why we developed the UKONS toolkit 2 Driving Policies • • Audit carried out in response to concerns about quality and safety for patients receiving chemotherapy Ø National confidential enquiry into patient outcomes & death. For better or worse (NCEPOD, 2008) Ø National Chemotherapy Advisory Group in England: ensuring quality & safety (NCAG, 2009) Identified lack support/infrastructure for patients receiving chemotherapy and early detection and treatment of chemotherapy related toxicities/side effects
Why we developed the UKONS toolkit 7 • No agreed triage process or pathway – multitude of numbers- changing admission points – different level of service out of hours • No agreed training or competency assessment • No quality control or review • No data collection No recognition of need, value or importance 7
Why we developed the UKONS toolkit • United Kingdom Oncology Nursing Society (UKONS) • The original version was developed in 2007/2009 positively evaluated and released in 2010 • Now used widely in all areas of the UK and internationally • No serious incidents or adverse events due to the correct use of tool kit reported during the pilot or since release • The tool has now been updated and version 2 was approved in November 2016 includes Immunotherapy 8
Development of the telephone triage toolkit • • 9 Developed over a 3 year period by a group of experienced senior nurses working within Chemotherapy Haematology and Oncology Supported by UK Oncology Nursing Society Multidisciplinary consultation. Supported by the U. K. National Patient Safety Agency Meets national recommendations, NCEPOD, NCAG and Acute Oncology measures Extensive pilot study in 26 cancer centres and units Positive evaluation and now widely adopted throughout the UK and internationally 9
10 Pilot study and evaluation The Tool Kit achieved its primary aims and objectives. • It was shown to be reliable, robust as a planned standardised approach to triage and assessment Ø An evidence-based assessment tool Ø A log sheet that acts as a checklist to prompt practitioners and a record of triage and assessment, supporting communication. • It sets a standard for best practice and is an excellent training and educational resource: Ø It can be used to provide evidence of quality and safety for both the organisation and the individual practitioner Ø It is useful in identifying risks and poor practice, helping to determine education and training needs Ø It can support consistency of advice, and consistency of service across Cancer Centers, Cancer Units and Primary Care. • Positively evaluated by those using it during the pilot. 10
11 Pilot study and evaluation • Improve patient safety and care by ensuring that everyone receives a robust, reliable assessment every time the helpline is contacted for advice • Ensure assessments are of a consistent quality and use an evidence-based tool • Provide management and advice appropriate to the patient’s level of risk. Ensure that those patients who require urgent assessment in an acute area are identified and that appropriate action is taken. Also identify and reassure those patients who are at lower risk and may safely be managed by the primary care team or a planned clinical review and avoid unnecessary attendance • Form the basis of triage training and competency assessment for practitioners • Maintain accurate records of the assessment and decision-making process in order to monitor quality, safety and activity. assessment 11
Aim of the tool kit 12 To provide guidance and support to the practitioner at all stages of the triage process: • • • Contact and data collection Assessment/definition of problem Appropriate intervention/action To provide: • • • A simple reliable assessment process Safe understandable advice Communication and record keeping Competency based training An audit tool 12
It’s a risk assessment tool kit? 13 A risk assessment tool using a RAG (RED, AMBER, GREEN) scoring system. For telephone triage of patients who: • Have received or are receiving Systemic Anti Cancer Therapy (SACT) • Have received any other type of anticancer treatment, including Radiotherapy and bone marrow graft • May be suffering from disease/treatment related immunosuppression (i. e. acute leukaemia, corticosteroids) 13
It’s a risk assessment tool kit 14 • Action is based on the triage practitioner’s grading of symptoms/toxicity: • RED – priority and action should follow immediately. Patient should be advised to attend for urgent assessment as soon as possible • 2 or more AMBER = RED – two or more toxicities graded amber should be escalated to red action • AMBER – one toxicity should be followed up within 24 hours, call from practitioner or call back if they continue to have concerns, or their condition deteriorates • GREEN – callers instructed to call back if they continue to have concerns or their condition deteriorates. 14
The manual • Brief background and development history • Instructions for use • Training and competency requirements and assessment proforma • The Triage Pathway Algorithm and Clinical Governance recommendations • Examples of all component parts of the Tool Kit 15 15
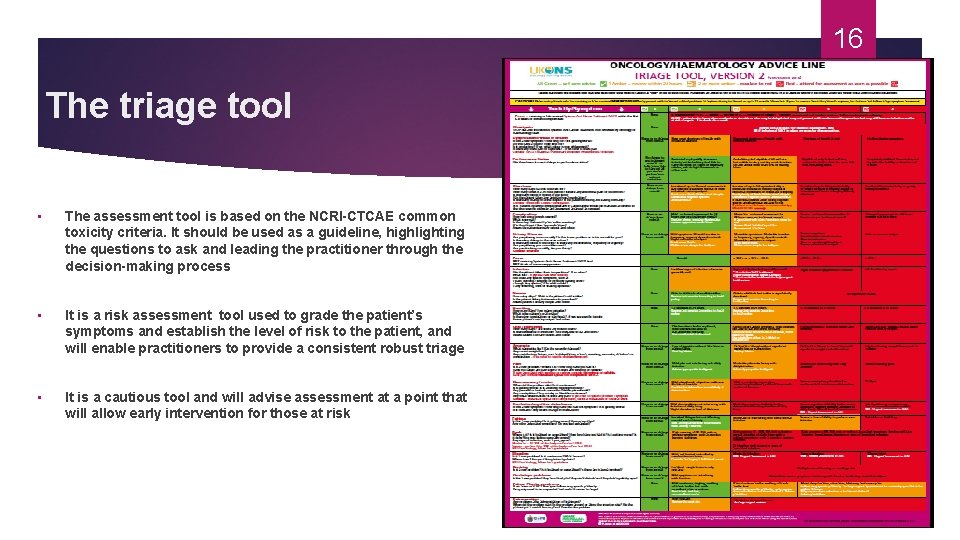
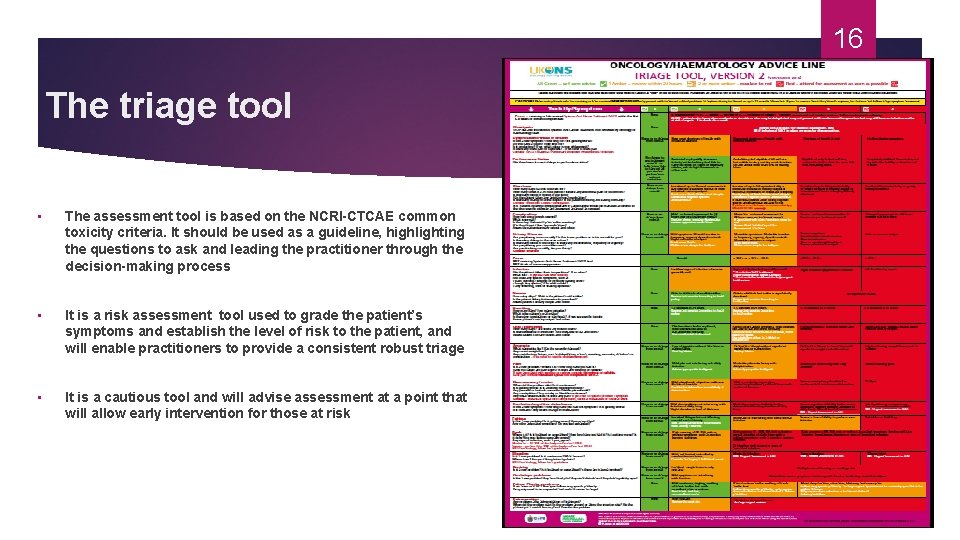
16 The triage tool • The assessment tool is based on the NCRI-CTCAE common toxicity criteria. It should be used as a guideline, highlighting the questions to ask and leading the practitioner through the decision-making process • It is a risk assessment tool used to grade the patient’s symptoms and establish the level of risk to the patient, and will enable practitioners to provide a consistent robust triage • It is a cautious tool and will advise assessment at a point that will allow early intervention for those at risk
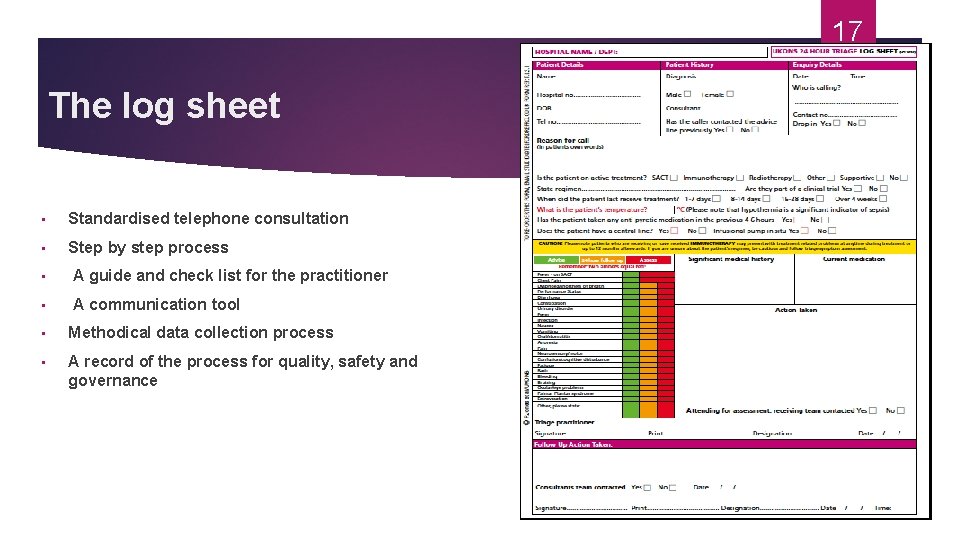
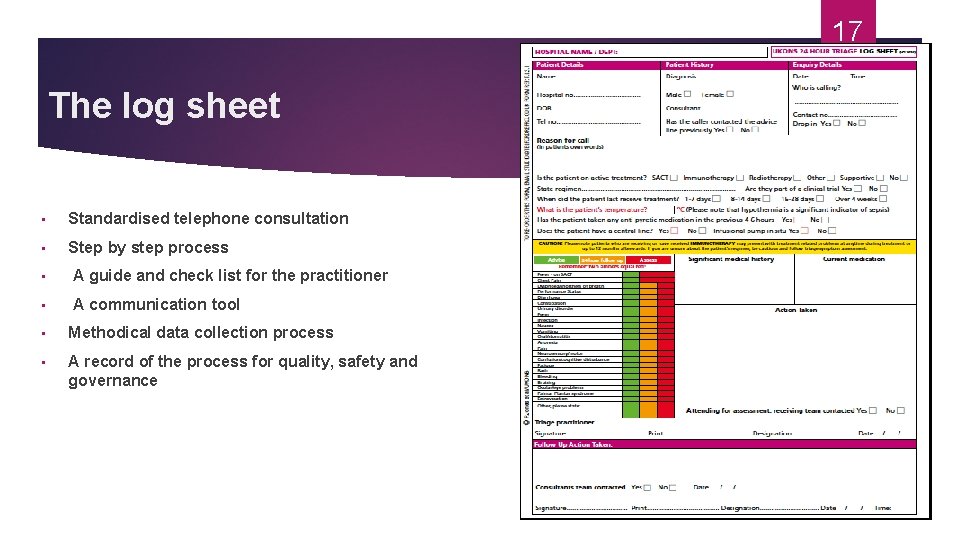
17 The log sheet • Standardised telephone consultation • Step by step process • A guide and check list for the practitioner • A communication tool • Methodical data collection process • A record of the process for quality, safety and governance
Why An Australian Tool • Nurses recognised the need to triage our patients to manage them safely, appropriate care at the right time and the right place by the right person • Evidence based practice - opportunity to bench mark our practice • UKONS received Aus requests to use the tool 18
AUSTRALIAN Working Group • 4 States & ACT • 23 Hospitals • Expert Panel • 6 Months review of toolkit & recent changes (2 years in total) • National Platform to host Toolkit - evi. Q 19
20 Changes : UK - AUS • Terminology & Grammar • Temperature – Febrile Alert : 37. 5* • What does this mean -New ways of thinking • Opportunity to prevent serious adverse events • early identification of symptoms and early management • its not always about the temperature … • its about the alert 20

21 Why do we need training for telephone assessment All staff using the toolkit must receive training and assessment of competency. • Training should include: Ø Formal education session Ø Discussion Ø Scenario and role play Ø Observation • A competency framework is supplied to be completed prior to using the toolkit • Example scenarios have been provided to assist with training Staff who are not trained to use the toolkit should not provide telephone advice
22 Why do we need training for telephone assessment • How many calls do you anticipate • During Hours • Out of Hours • Who will take the calls: in the uk evaluation 85% of staff had 3 years Chemotherapy experience and were senior grades • High volume of calls 8 pm – midnight • What happens overnight • What happens at weekend and public holidays
23 Limitations of telephone triage • Barriers : only verbal and emotional cues • No visual information : what do we look for: colour, general appearance, body language, signs in behavior, smell ! • Symptoms have a wide ranging differential : lack of visual cues, lack of ability to capture overall facial expressions, face to face assessment • Poor language • Cognitive impairment • Elderly
24 Common errors in telephone assessment • Inadequate talk time • Insufficient history taking and documentation • Absence of key questions • Lack of structure • Improper use of or failure to use protocols • Premature diagnosis, without detailed assessment • Risk of stereotyping of clients and problems • Second guessing or over reliance on callers • “ my new meds are making me dizzy” “ I have the flu” • Patient may seriously misrepresent the symptom
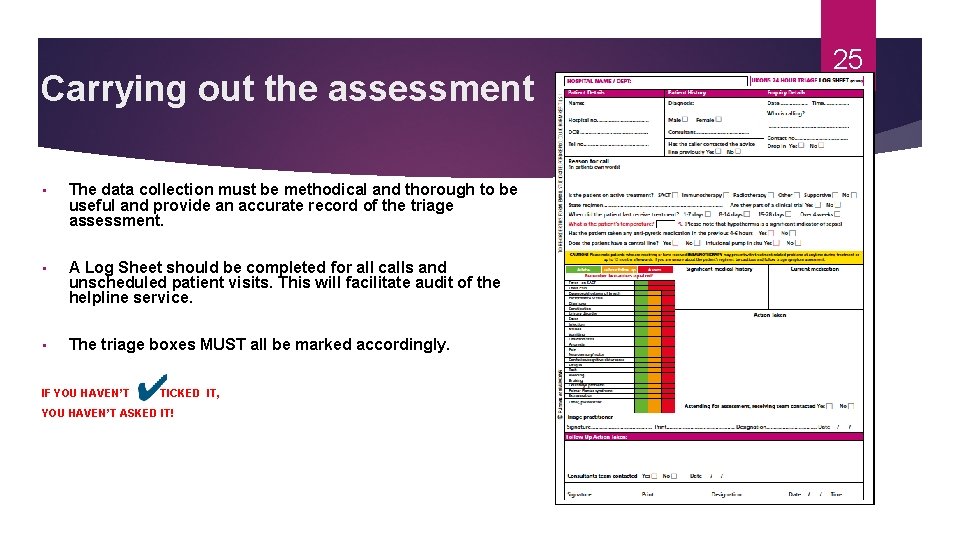
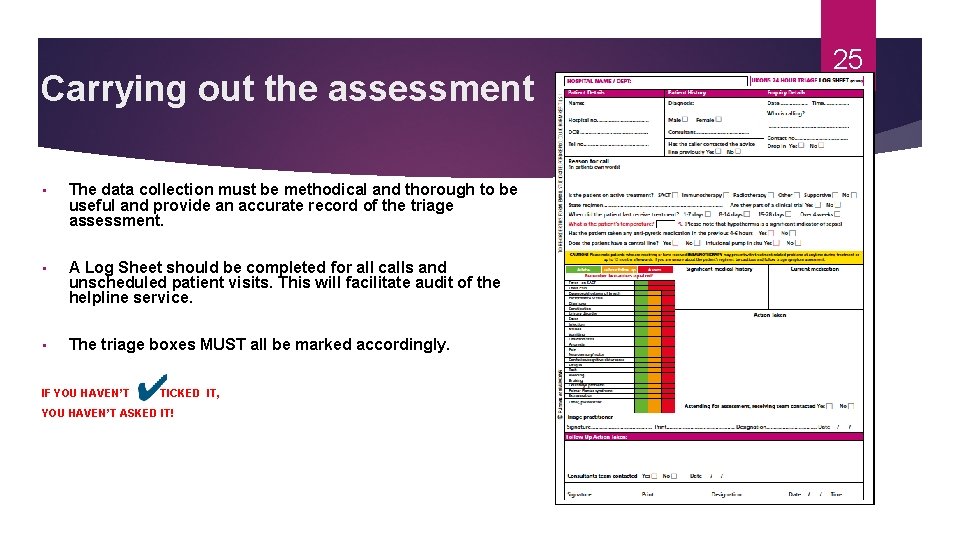
Carrying out the assessment • The data collection must be methodical and thorough to be useful and provide an accurate record of the triage assessment. • A Log Sheet should be completed for all calls and unscheduled patient visits. This will facilitate audit of the helpline service. • The triage boxes MUST all be marked accordingly. IF YOU HAVEN’T TICKED IT, YOU HAVEN’T ASKED IT! 25
26 Assessment • Assessment tool acts as Prompt for Triage Practitioner • RED- Priority & Action • Reliable guide to toxicity grading based on NCI Common Terminology Criteria for Adverse Events • AMBER- One Amber may require advice & follow-up. More than two Ambers may indicate assessment & follow-up. • GREEN- Patients should be encouraged to monitor symptoms & recontact if issues arise. • Practitioner judgement & experience plays a vital part in assessment.
Good technique-structure • State your name and position • Obtain caller's name and telephone number • Record date and time of call. • Record person's name, gender and age • Speak directly with the person who has a problem. • Take a detailed and structured history. • Triage protocols or checklists : UKONS tool 27
Good technique-advice giving • Provide advice on treatment/disposition • Give specific advice regarding follow-up and when to contact • Summarise and record the main points covered • Request caller to repeat advice given. • Ask if the person has any outstanding questions or concerns. 28
Questioning techniques • Open questions: Ø Elicit more information, Ø Encourages clients to describe symptoms • Exceptions to open questioning: Ø Crisis-level calls and poor historians Ø Use facilitative questions instead: “Is your pain severe, moderate or mild” • Symptoms • Reflecting and paraphrasing • Clarifying and asking for detail • Attentiveness to verbal and emotional cues Ø Ø UKONS tool, NCI Toxicity Grading Symptom acronyms –SCHOLAR, OLDCART 29
Step By Step 1 • Perform a rapid initial assessment of the situation: “Is this an emergency? ” Ambulance or Attend • Ask questions in a logical sequence. Follow log sheet and triage tool • Provide information slowly, assessing the patient’s comprehension, anxiety and distress throughout the process • Do you have any doubt about the patient/carers ability to provide information accurately or understand questions or instructions provided? If so then a face-toface consultation must be arranged • Record caller’s name and current contact details in case the call is interrupted and you need to get back to the caller. 30
Step By Step 2 • What is the patient/carer’s initial concern, why are they calling? • You should assess and grade this problem first, ensuring that you record this on the Log Sheet. If this score is RED then you may decide to stop at this point and proceed to organising urgent face-to-face assessment • If the patient is stable you may decide to complete the assessment process in order to gather further information for the face-to-face assessment. 31
Step By Step 3 32 • If the patient/carer’s initial concern scores AMBER, record this on the Log Sheet and proceed with further assessment • Move methodically down the triage assessment tool, asking appropriate questions. e. g. Do you have any nausea? If NO tick the green box on the Log Sheet and move on • If YES use the questions provided to help you grade the problem and note either amber or red and initiate action (tick the Log Sheet) • If the patients symptoms score RED or another AMBER at any time they should be asked to attend for assessment
Step By Step 4 33 Look back at your Log Sheet • Have you arranged assessment for patients who have scored RED? • Have you arranged assessment for patients who have scored more than one AMBER? • Have you fully assessed all the patients who have scored one AMBER, is there a tick in all the other green boxes of the Log Sheet? • Have you fully assessed all the patients who have scored GREEN, is there a tick in all the other green boxes of the Log Sheet? • Have you recorded the action taken and advice given? • Have you documented any decision you have taken or advice you have given that falls outside this guideline, and recorded the rationale for your actions? • Have you fully completed the triage process?
Special Considerations • If, in the triage practitioner’s clinical judgement, the guideline is not appropriate to that individual situation, the rationale for that decision should be clearly documented • If the triage practitioner’s assessment is borderline select the higher risk category; BE CAUTIOUS • The organisation must agree the triage pathway and populate it with local detail and responsibilities. 34
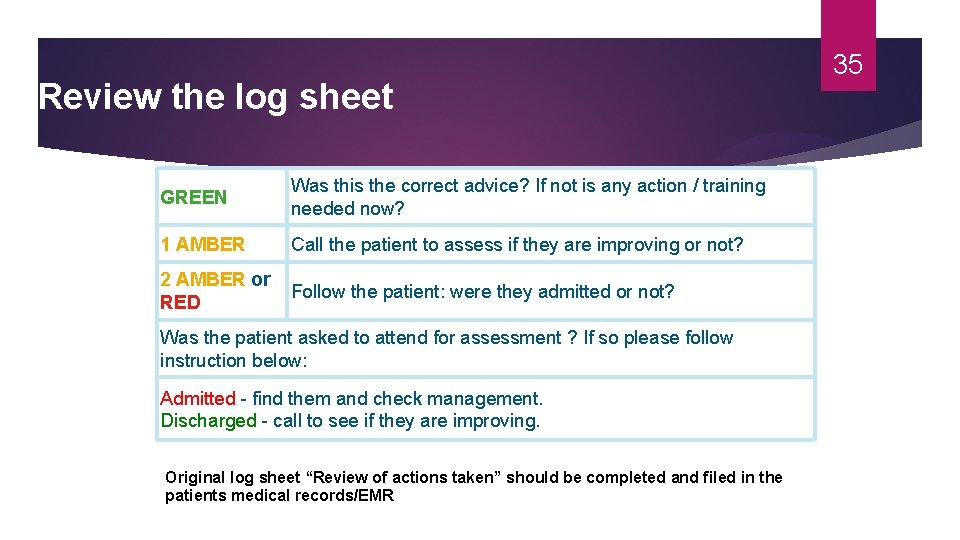
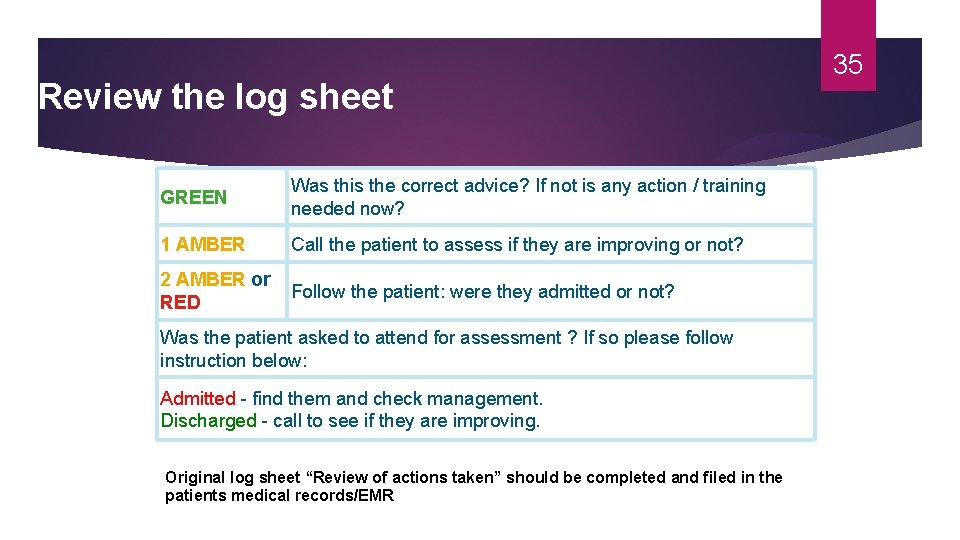
Review the log sheet GREEN Was this the correct advice? If not is any action / training needed now? Hospital Designated Responsible must review 1 The AMBER Call the patient to. Practitioner assess if they are improving or not? all Log Sheets within 24 hours of the call as follows: 2 AMBER or RED Follow the patient: were they admitted or not? Was the patient asked to attend for assessment ? If so please follow instruction below: Admitted - find them and check management. Discharged - call to see if they are improving. Original log sheet “Review of actions taken” should be completed and filed in the patients medical records/EMR 35
Additional information • The tool has been piloted in its present format and should not be amended or adapted without the express permission of the UKONS board. • There are new and novel drugs on the market that have a protracted side effect profile, please be careful when providing advice for this group of patients. 36
Governance and responsibility 37 • The 24 Hour Triage tool is a guideline and should be approved for use according to the user organisations governance and approval process • The tool is a guideline which makes recommendations for best practice, these are not binding and should be seen as suggestions and or advice, they do not replace clinical judgment or remove autonomy • Neither UKONS nor authors bear any responsibility for the use of the tool RCP developing concise guidelineshttps: //www. rcplondon. ac. uk/resources/developing-concise-guideline.
38 Competency Framework • The manual contains a competency assessment document linked to the national key skills framework that should be completed for all those who undertake UKONS triage and assessment. • It is recommended that this assessment be repeated annually to ensure that competency is maintained.
39 Audit • Please ensure that all copies of Log sheets are retained safely for audit and clinical governance purposes. • Information may be entered onto a data base.
Factors to consider when implementing the Toolkit in your health service 40 • Organisational approval and agreement should be sought as the governance responsibility sits with the user/organisation • Clear decisions should be made about the triage pathway, identifying admission/assessment areas and triage practitioners who will provide review and follow-up calls • A plan for education, training and competency assessment. This is a vital step in the process; users need to have a clear understanding of the value of the Tool Kit and the risk to the patient and themselves if it is not used properly • Regular audit and quality review of all data collected – consider electronic data collection • Governance process – as with any service, the advice line will need to be monitored and reported. 40
41 Thank You For Listening 41