Oncology 17102019 MLT 2 Rosalind Simpson Plan Pathology
![Nottingham Prognostic Index • tumour grade [1 – 3] + lymph node status [1 Nottingham Prognostic Index • tumour grade [1 – 3] + lymph node status [1](https://slidetodoc.com/presentation_image_h2/1a603cd3929c2076e8754fd575545c0f/image-11.jpg)

- Slides: 44
Oncology 17/10/2019 MLT 2 Rosalind Simpson
Plan • • Pathology + staging of common malignancies Oncological emergencies Screening theory and screening programmes Pain management and palliative care in terminal disease
Breast
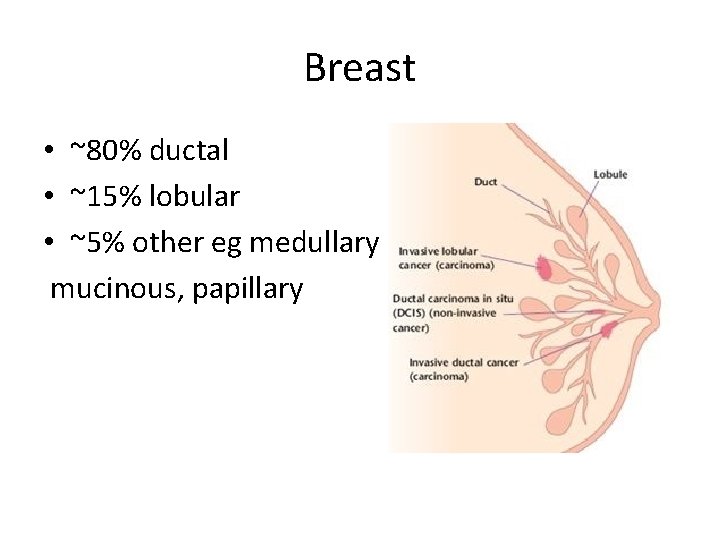
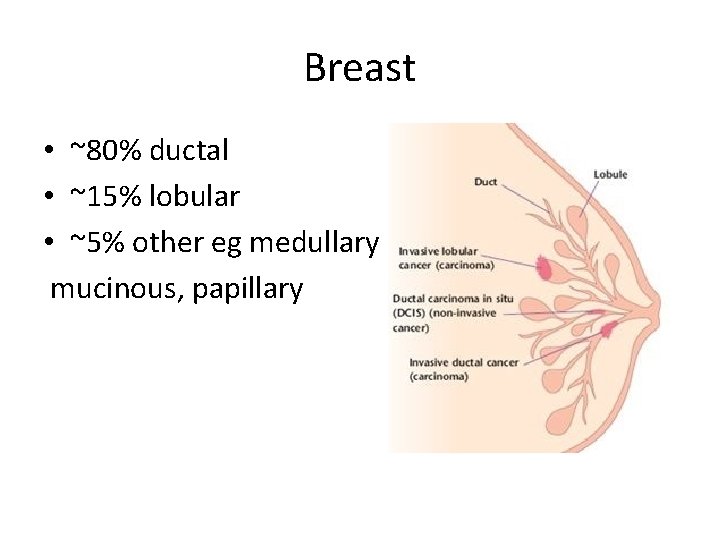
Breast • ~80% ductal • ~15% lobular • ~5% other eg medullary mucinous, papillary
Classification by histology • Oestrogen + progesterone • HER 2 (human epidermal growth factor receptor 2) • Triple negative • Proliferative markers eg ki 67
Oestrogen receptor Premenopausal = Tamoxifen SERM = antagonist at breast, agonist at bone Postmenopausal = aromatase inhibitors Block conversion of adrenal androgens to oestrogens in fatty tissues • Anastrozole • •
Her 2 receptor • Trastuzumab (aka Herceptin) • Humanized monoclonal antibody
Nomenclature of monoclonal antibodies • • • -umab = h. UMAn -zumab = h. UMAni. Zed -ximab = x = chimeric -imab = primate -omab = mouse • MAB Monoclonal Anti Body
Ki 67 + triple negative • Aggressive. Adjuvant chemo indicated • Ki 67 positive tumours are chemosensitive
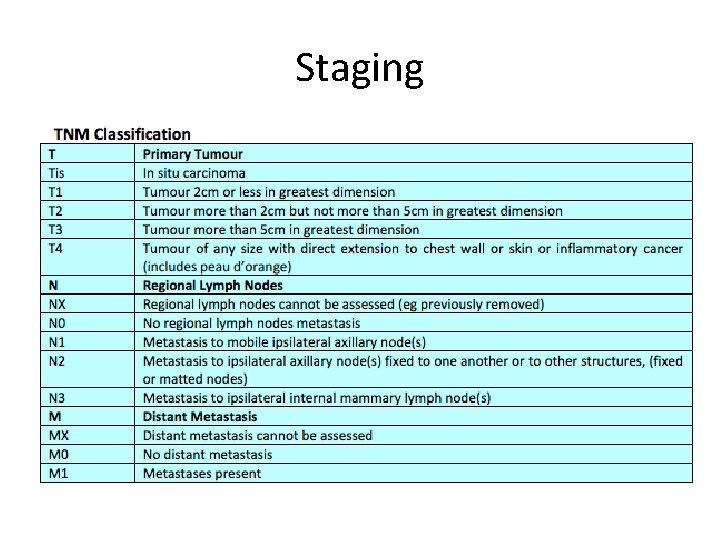
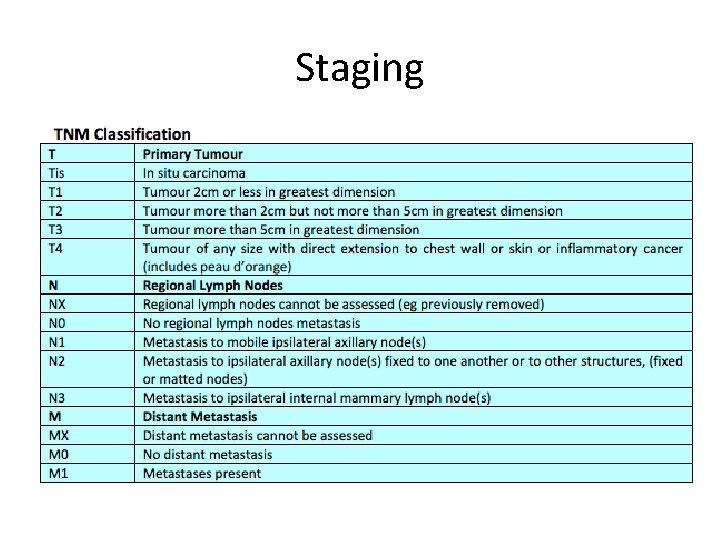
Staging
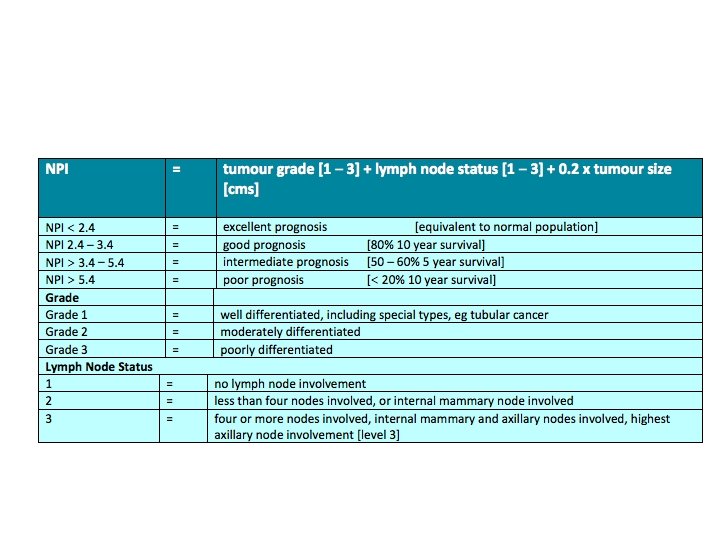
![Nottingham Prognostic Index tumour grade 1 3 lymph node status 1 Nottingham Prognostic Index • tumour grade [1 – 3] + lymph node status [1](https://slidetodoc.com/presentation_image_h2/1a603cd3929c2076e8754fd575545c0f/image-11.jpg)
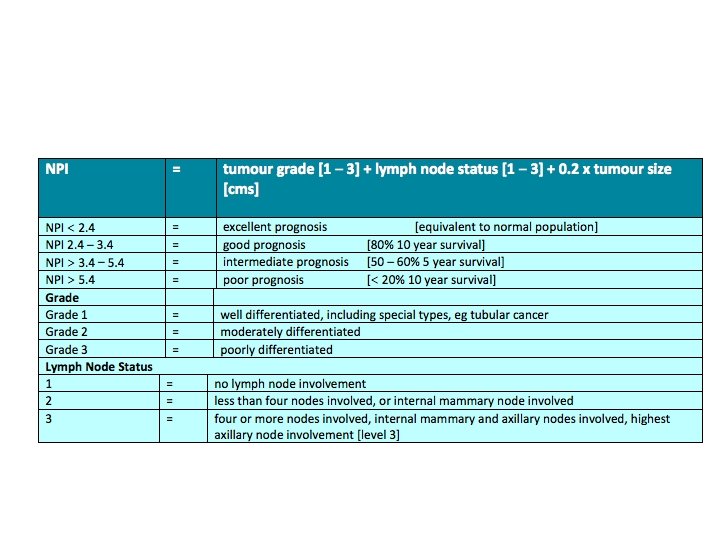
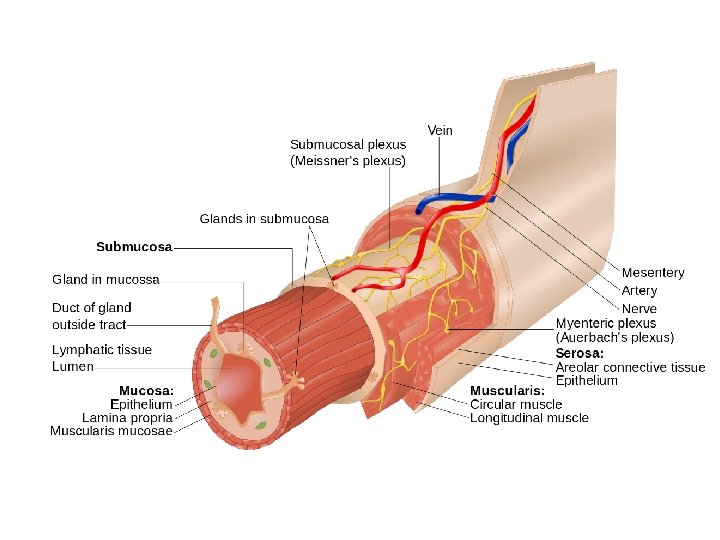
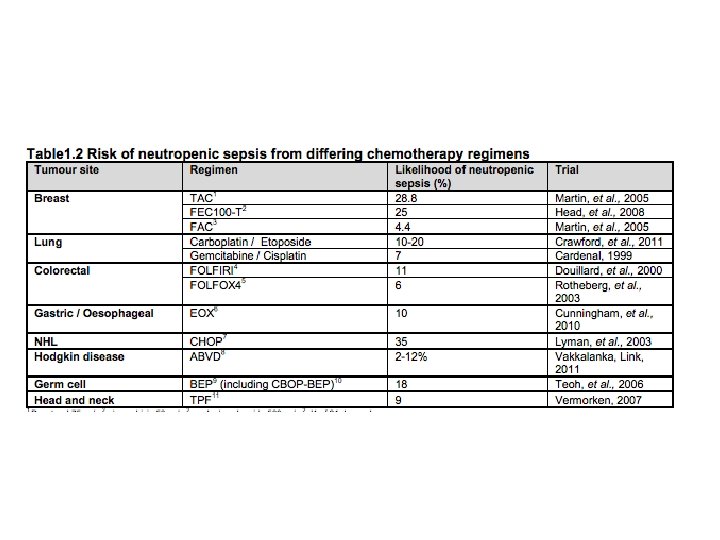
Nottingham Prognostic Index • tumour grade [1 – 3] + lymph node status [1 – 3] + 0. 2 x tumour size [cms] • Result between 0 and 7 • Less than 2. 4 = same survival • >5. 4 less than 20% 5 year survival
Lung
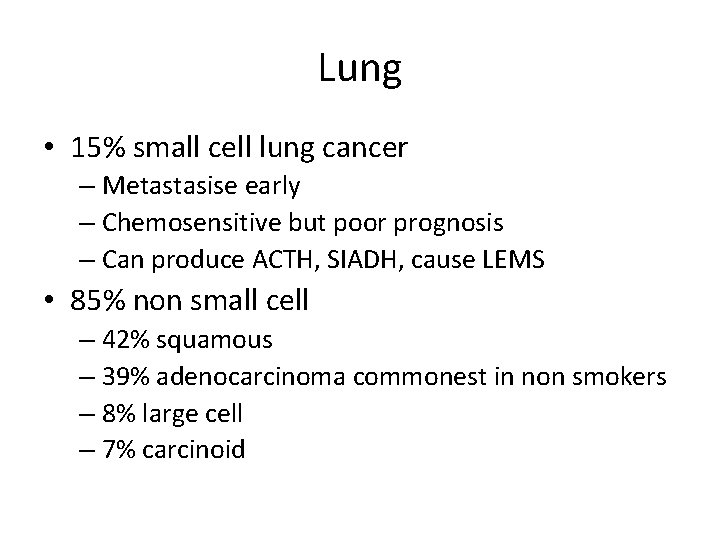
Lung • 15% small cell lung cancer – Metastasise early – Chemosensitive but poor prognosis – Can produce ACTH, SIADH, cause LEMS • 85% non small cell – 42% squamous – 39% adenocarcinoma commonest in non smokers – 8% large cell – 7% carcinoid
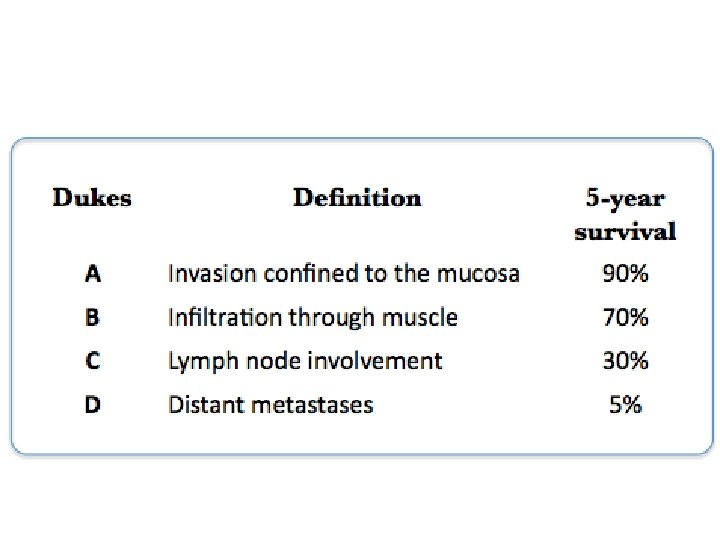
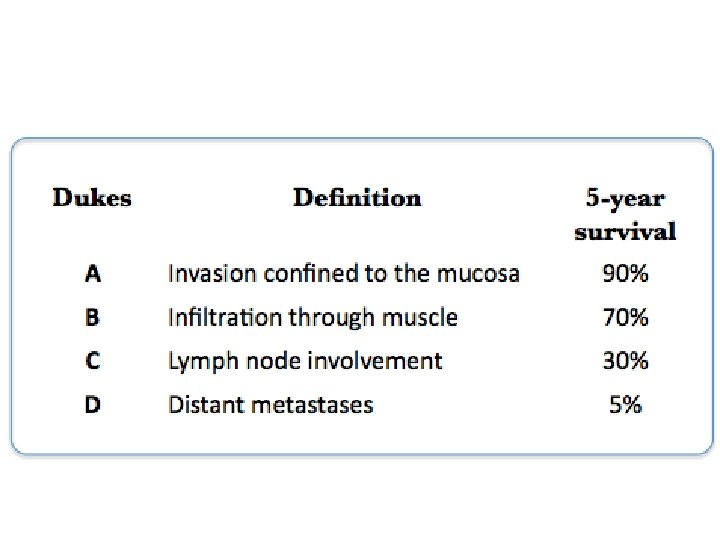
Colorectal
Colorectal • Two thirds colon one third rectum • Adenocarcinomas that arise from polyps
Prostate cancer • Adenocarcinoma • Multi-focal (different foci have different properties) • Mostly indolent but minority are aggressive • Metastasise to bone
Presents • Bone pain, erectile dysfunction, lower back pain, lethargy, anorexia, wt loss, haematuria • LUTS – less commonly • Raised or rising PSA – not particularly sensitive or specific • Hard and nodular prostate on DRE
Diagnosis + gleason grade • TRUS biopsy • 10 -12 cores taken • Commonest and second most common tumour patterns identified • Each graded from 1 (normal tissue) to 5 (completely undifferentiated • Sum them • Get a number between 2 and 10 • Low grade = 6 or less, intermediate = 7, high grade = 8+
Goals of treatment • Radical = with curative intent • Palliative = to reduce symptoms/prolong life – WITHOUT curative intent • Adjuvant = alongside/after definitive (normally surgical therapies) – implies curative intent • Neo-adjuvant = before definitive treatment to eliminate micrometastases

Goals of treatment • Watchful waiting = postponing palliative treatment • Active surveillance = postponing radical treatment and involves re-biopsy
Radical Therapy • External Beam Radiotherapy • Prostatectomy
Adjuvant therapies • Androgen withdrawal – surgery, LHRH agonist or LHRH antagonist • LHRH agonists eg gosrelin • Agonists can cause a flare which you can block with bicalutaide • LHRH antagonists eg cyproterone acetate
Also be ready for • • melanoma cervical endometrial bladder kidney liver pancreas
Oncological emergencies • • • Tumour lysis syndrome Spinal cord compression SVC obstruction Neutropenic sepsis Hypercalcaemia
Tumour Lysis Syndrome • The abrupt release of large quantities of cellular components into the blood following rapid lysis of malignant cells
Who gets it • Cancers with large tumour bulk (more tumour to lyse) • Cancers that are very chemosensitive (more of the tumour lyses at once) • Leukaemias and lymphomas especially aggressive lymphomas • Poor renal function (cannot clear the toxic cell contents)
What happens • Proteins are released -> hyperuricaemia • Electrolytes that are more concentrated in the cells are released -> hyperphosphataemia and hyperkalaemia • The phosphate complexes with calcium -> hypocalcaemia • The uric acid and calcium phosphate crystals deposit in the renal tubules -> acute renal failure
Presentation • Weakness • Paralytic ileus - Constipation, vomiting, abdo pain • Cardiac arhythmias - Palpitations, chest pain, collapse • Acute kidney injury - reduced UO, lethargy, nausea
Investigations • FBC • U+E - raised urea, raised creatinine (AKI(, hyperkalaemia • Serum LDH - high • Serum phosphate - high • Serum calcium - low • Serum urate - high
Management • • • Awareness, identification of high risk patients, implementation of prophylaxis, monitoring patient during chemotherapy Starting active treatment when necessary
Prevention for high risk patients • IV fluids, • Rasburicase: recombinant urate oxidase catalyses the oxidation of uric acid to more soluble allantoin, • Allopurinol: xanthine oxidase inhibitor - blocks conversion of xanthines to uric acid
Active treatment • Vigourous hydration • Correct hyperkalaemia – Protect the myocardium with 10 mls of 10% calcium gluconate – Drive potassium into cells with 10 units of rapid acting insulin and 50 mls of 50% glucose – Salbutamol neb – Remove the potassium with oral calcium resonium
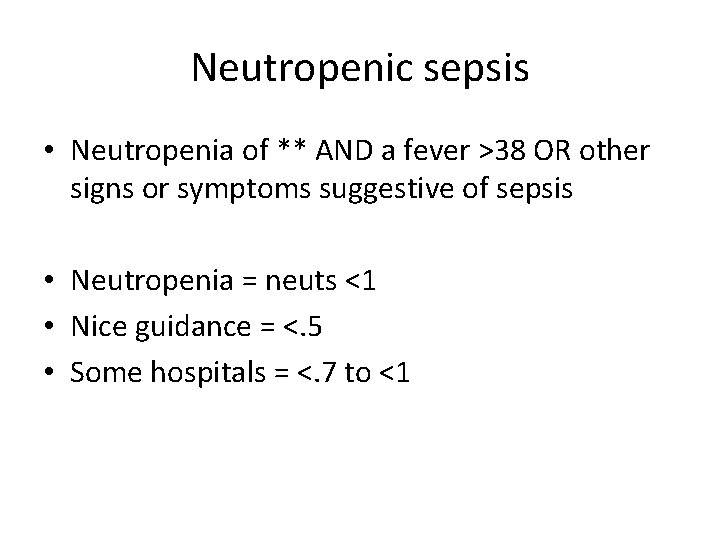
Active treatment • Rasburicase (stop allopurinol) • Acetazolomide = alkalinize urine make uric acid more soluble • Phosphate binders • If above fails dialyse
Neutropenic sepsis • Neutropenia of ** AND a fever >38 OR other signs or symptoms suggestive of sepsis • Neutropenia = neuts <1 • Nice guidance = <. 5 • Some hospitals = <. 7 to <1
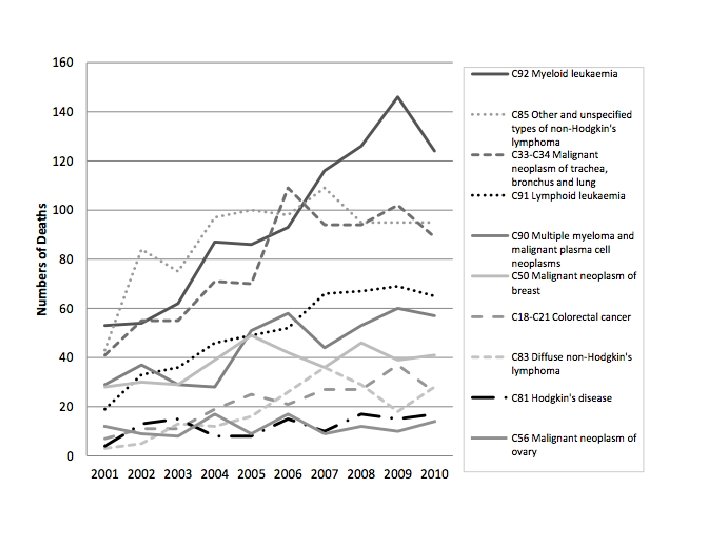
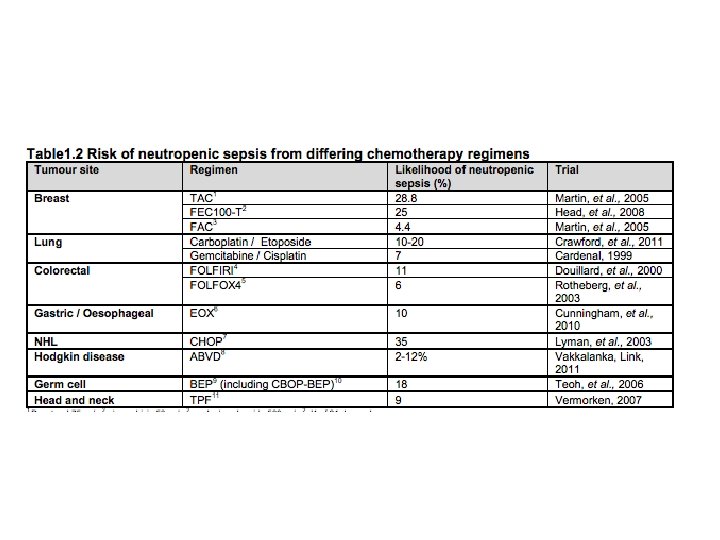
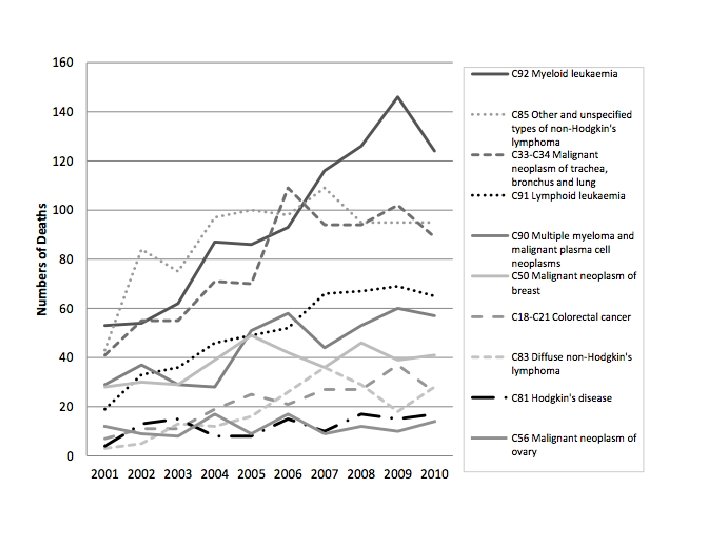
At risk of neutropenic sepsis • Current or recent anticancer treatment • Most commonly chemo for blood cancers • But also lung, breast, ovarian, colorectal
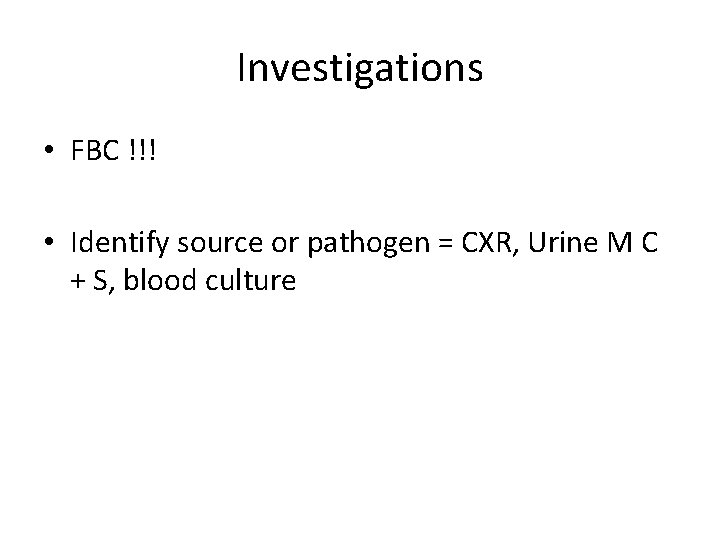
Investigations • FBC !!! • Identify source or pathogen = CXR, Urine M C + S, blood culture
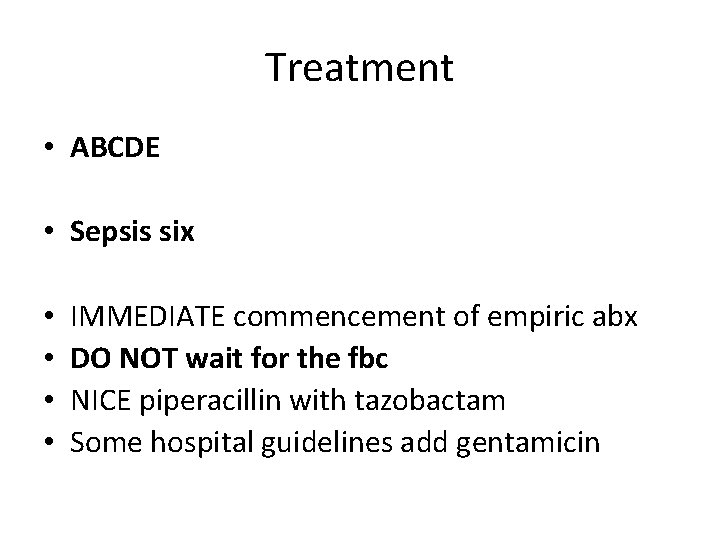
Treatment • ABCDE • Sepsis six • • IMMEDIATE commencement of empiric abx DO NOT wait for the fbc NICE piperacillin with tazobactam Some hospital guidelines add gentamicin
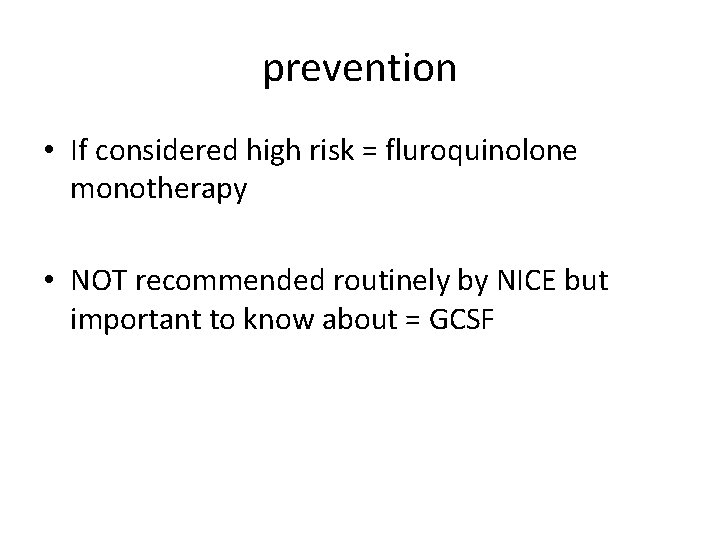
prevention • If considered high risk = fluroquinolone monotherapy • NOT recommended routinely by NICE but important to know about = GCSF