Omega3 PUFA and Cardiac Arrhythmias Dalit Weisman R





















- Slides: 55
Omega-3 PUFA and Cardiac Arrhythmias Dalit Weisman R. D, Msc, Ph. D student Electrophysiology Unit Heart Institute Sheba Medical Center

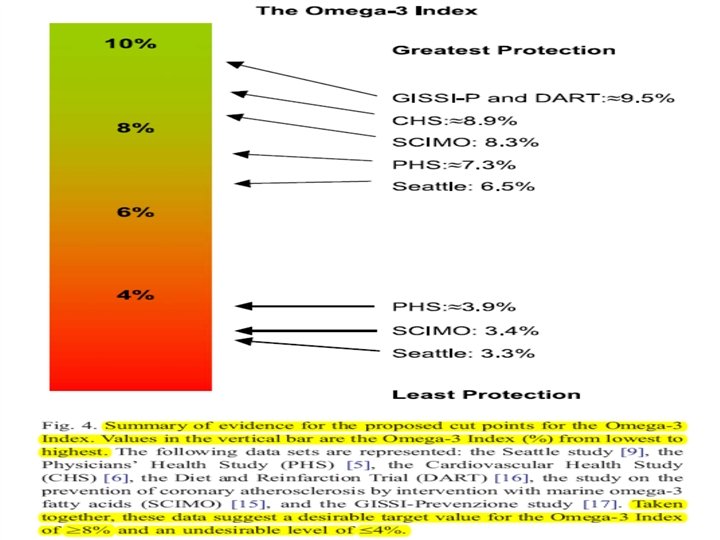
WILLIAM S. HARRIS, Ph. D. CLEVELAND CLINIC JOURNAL OF MEDICINE VOLUME 71 • NUMBER 3 MARCH 2004

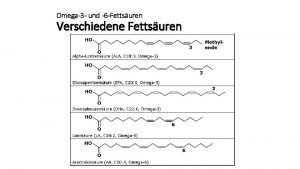
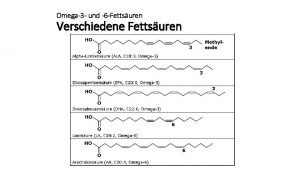
Breaking News on Food & Beverage Development - Europe 27/11/2007 - Dr. Jörn Dyerberg The inventor of omega-3 It all started with a trip to Greenland in 1970. Three Danes, a couple of dogsleds, and several years of study later and the omega-3 was born. Since then, awareness and understanding of marine omega-3 has sky-rocketed. science explosion has been followed by consumer and product blast-off. Different ratios for EPA (C 20: 5 n-3) to DHA (C 22: 6 n-3) are being marketed, or DHA alone, or products containing alpha-linolenic acid (ALA, C 18: 3 n-3), a shorter long-chain omega-3 from plants. The It's all a bit confusing… If we want the benefits of omega-3, we have to eat them as long chain, " he said, referring to EPA and DHA. "The ratios of EPA and DHA are not important, " said Dr. Dyerberg, "as they can be interconverted. " "But consumption should include both, and a decent combination is 3: 2 EPA: DHA. " So what about docosapentaenoic acid (DPA), labelled by some as "underrated" amongst the omega-3 fatty acids? "I don't know any specific effects of DPA, " he said. "But it is an intermediate in the conversion of EPA to DHA, so it will be present in the body all the time. " As for ALA, an omega-3 from plants that is converted in the body to EPA and subsequently DHA, he was unconvinced. In terms of biological effects of DHA and EPA, Dr. Dyerberg said there are many. "We don't know of any specific biological effects of ALA, " he said.

Mozaffariam D et al. JAMA. 2006; 296: 1885 -99.

Circulation. 2007: 116: e 320 -e 335.
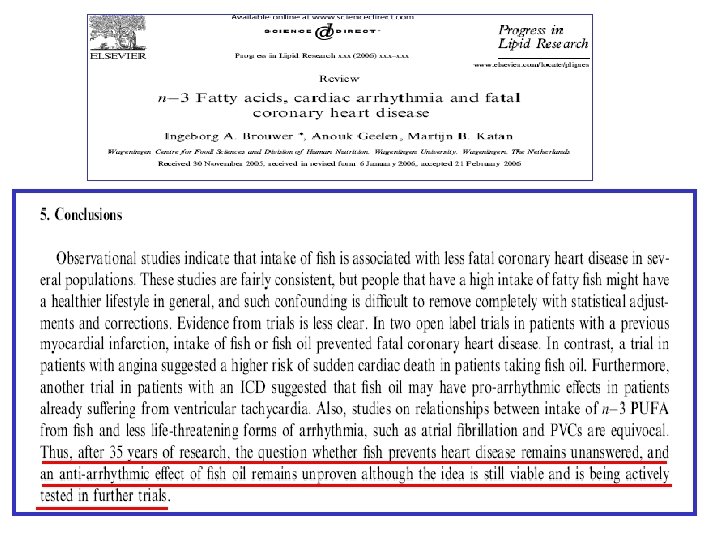
• Efforts to better understand the links between diet and cardiac rhythm have the potential to improve public health and welfare and to reduce the ballooning costs associated with treating cardiovascular disease. • That omega-3 fatty acids have an impact on the fundamental elements (ion channels, exchangers, and modulators) of cardiac electric activity is now indisputable. However, the translation of this understanding into evidence-based public policy guidelines that can decrease the incidence of arrhythmias and SCD still requires significant additional efforts. Circulation. 2007: 116: e 320 -e 335.


• 6 medical USA centers. • N= 200 (parallel group design). – 100 fish-oil. – 100 placebo. • 2 year follow-up. • Intervention dose: – 1. 8 g fish-oil = 1. 3 g EPA+DHA.
Results • At 6, 12, and 24 months after randomization, respectively, 46% 51% and 65% of pts assigned to fish-oil had ICD therapy for VT/VF compared with 36% 41% and 59% of pts assigned to placebo (p=. 19).
Comment • In the subset of 133 pts whose qualifying arrhythmia at the time of study entry was VT, pts assigned to fish-oil had a 61% 66% and 79% incidence of VT/VF treated by the ICD at 6, 12, and 24 months, respectively compared with 37%, 43%, and 65% among those

At 6, 12, and 24 months, 46%, 51%, and 65% of patients assigned to receive fish oil had ICD therapy for VT/VF, compared with 36%, 41%, and 59% for patients assigned to receive placebo (p = 0. 19). In the subset of 133 patients whose qualifying arrhythmia was VT, 61%, 66%, and 79% of patients in the fish oil group had VT/VF at 6, 12, and 24 months, respectively, compared with 37%, 43%, and 65% of patients in the placebo group (p = 0. 007). In addition, the number of days with episodes of. JAMA. ICD therapy for VT/VF was significantly greater in the fish oil group than in Raitt et al. 2005; 293: 2884 -2891.
Conclusions • Among patients with a recent episodes of sustained ventricular arrhythmia and an ICD, fish oil supplement does not reduce the risk of VT/VF and may be proarrhythmic in some patients.

• 8 European countries • N= 546 (parallel group design) – 273 fish-oil. – 273 placebo. • 1 year follow up. • Intervention dose: – 2 g fish-oil = 961 mg EPA+DHA.
Results • Event-free survival did not substantially improved in the fish-oil group (sustained ICD intervention or death from any cause accure 30% in the fish-oil group and 33% in the placebo (p=0. 33). • In total 75 pts (27%) in the fish oil group and 81 pts (30%) in the placebo received appropriate ICD intervention for VT or VF (p=0. 46).
Comments • In 342 patients with prior MI there was a nonsignificant tendency for a beneficial effect of fish oil on event free survival. • In this study patients had experienced MI between 2 weeks and 25 years before
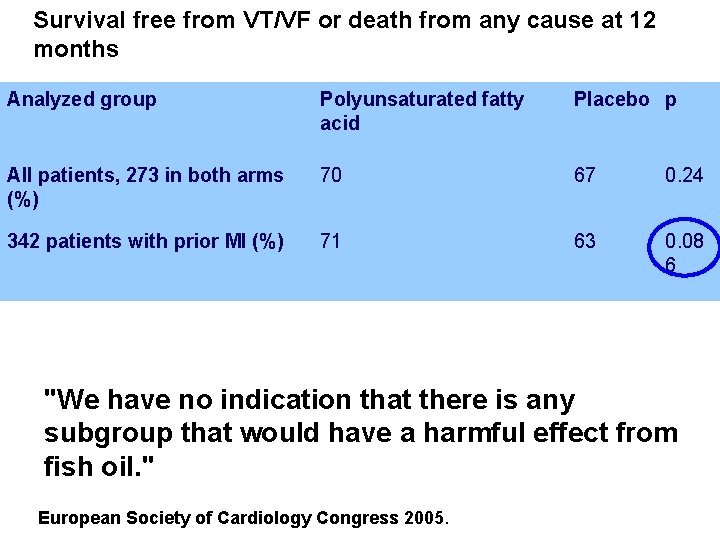
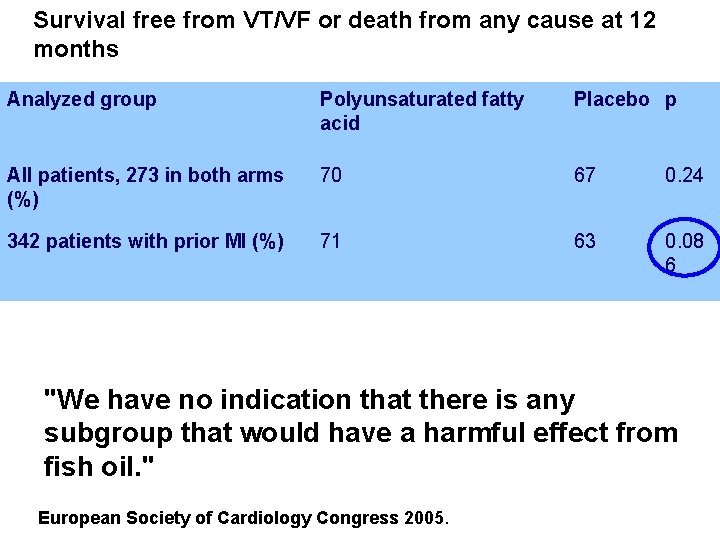
Survival free from VT/VF or death from any cause at 12 months Analyzed group Polyunsaturated fatty acid Placebo p All patients, 273 in both arms (%) 70 67 0. 24 342 patients with prior MI (%) 71 63 0. 08 6 "We have no indication that there is any subgroup that would have a harmful effect from fish oil. " European Society of Cardiology Congress 2005.
Conclusions • No evidence of a strong protective effect of intake of omega-3 PUFA from Fish oil against ventricular arrhythmias in patients with ICDs has been found. • In contrast to others, this study did not find that fish-oil may have proarrhythmic properties.
Circulation. 2005; 112: 2762 -2768
• USA. • N= 400 (parallel design). – 200 – fish-oil – 202 placebo. • 1 year follow up. • Intervention dose: – 4 g fish oil = 2. 6 g EPA+DHA
Results • In the primary analysis, according to the intention- to- treat principle, there was a trend toward a longer time to first ICD event for VT/VF confirmed by electrograms or death from any cause among patients randomized to fish oil compared with those of placebo (p=0. 057).
Results • In the second on-treatment analysis limited only to subjects who were compliant for at least 11 months, the relative risk was 0. 62 (P=0. 034). • 142 subjects (35%!!) discontinued their supplement before completing their year in the trial. )
Conclusions • Although significant was not achieved for the primary end point, this study provides evidence that for individuals at high risk of fatal ventricular arrhythmias, regular daily ingestion of fish oil fatty acids may significantly reduce potentially fatal ventricular arrhythmias.
Experts comments • “fish oil supplementation in ICD patients continues to be an ‘evolving area’…. ” • “there are no definitive data at this point”…. . • ”there are supporting data for both positions”. Dr. Douglas Zipes – Indiana University School of Medicine, Indianapolis. Heart wire Nov. 4, 2005.
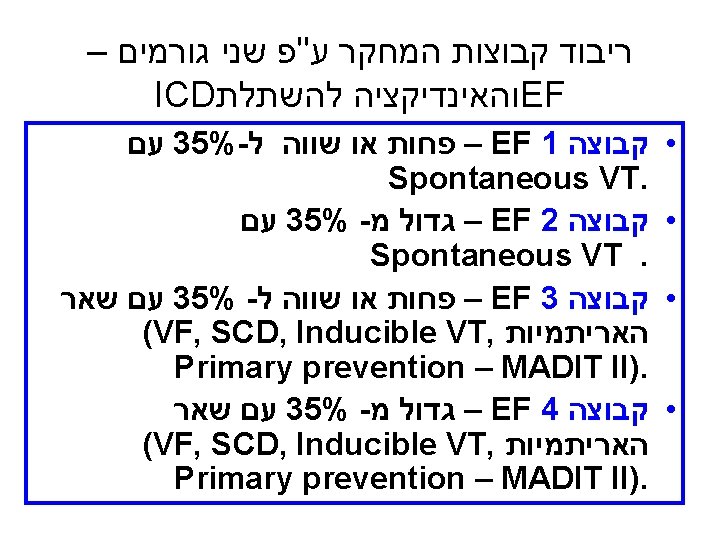
Effect of Supplemental intake of Omega-3 Polyunsaturated Fatty-Acids on the rate and complexity of spontaneously occurring ventricular and supraventricular arrhythmia in patients with Implantable Cardioverter Defibrillator. Prof. Uri Goldburt Prof. Michael Glikson Prof. Ehud Schwamental Dr. David Luria Prof. Sami Viskin Dalit Weisman R. D, Msc, Ph. D

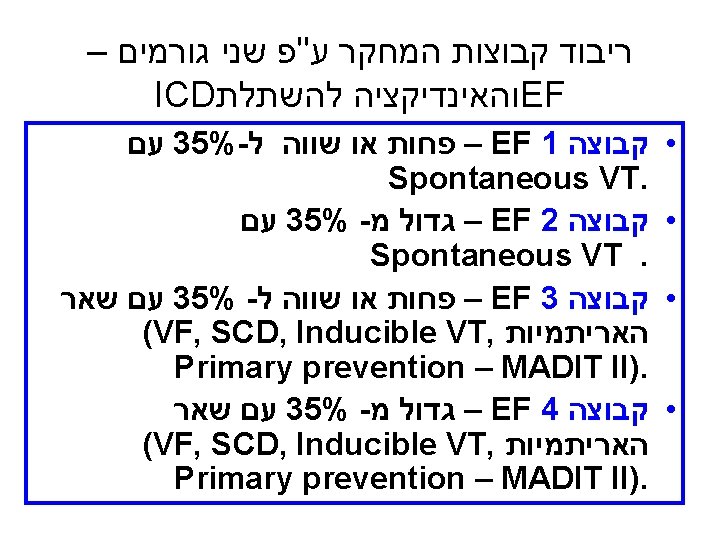
Study objectives • Primary Outcomes: – To investigate the effects of oral supplementation of omega-3 PUFA on the occurrence of life threatening ventricular arrhythmias in post-MI ICD recipients. • Secondary outcomes: – 1) All-cause mortality, cardiac mortality, recurrent and myocardial infarction. – 2) Atrial arrhythmia and non-sustained ventricular arrhythmia (non-sustained VT or ventricular premature complex (PVC)) as documented by ICD memory or 24 hour ECG (Holter) recording. – 3) Whether omega-3 PUFA supplementation exerts different effects according to ischemia severity assessed by stress perfusion nuclear imaging. – 4) The effect of omega-3 PUFA supplementation on C-reactive protein blood levels
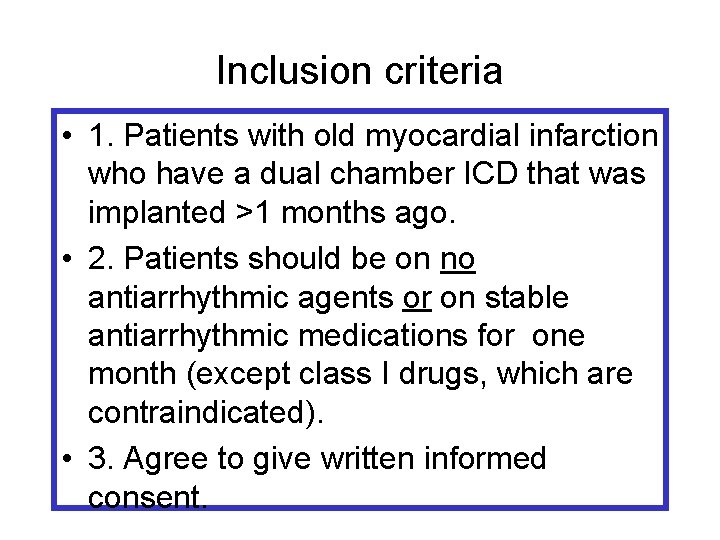
Inclusion criteria • 1. Patients with old myocardial infarction who have a dual chamber ICD that was implanted >1 months ago. • 2. Patients should be on no antiarrhythmic agents or on stable antiarrhythmic medications for one month (except class I drugs, which are contraindicated). • 3. Agree to give written informed consent.
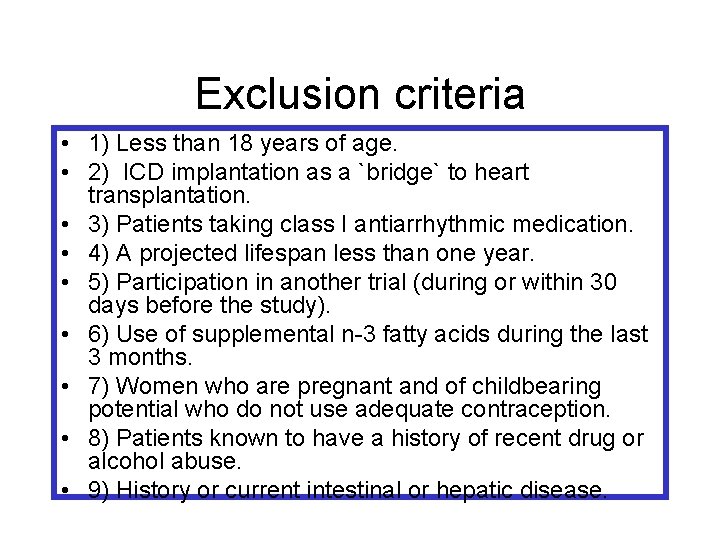
Exclusion criteria • 1) Less than 18 years of age. • 2) ICD implantation as a `bridge` to heart transplantation. • 3) Patients taking class I antiarrhythmic medication. • 4) A projected lifespan less than one year. • 5) Participation in another trial (during or within 30 days before the study). • 6) Use of supplemental n-3 fatty acids during the last 3 months. • 7) Women who are pregnant and of childbearing potential who do not use adequate contraception. • 8) Patients known to have a history of recent drug or alcohol abuse. • 9) History or current intestinal or hepatic disease.
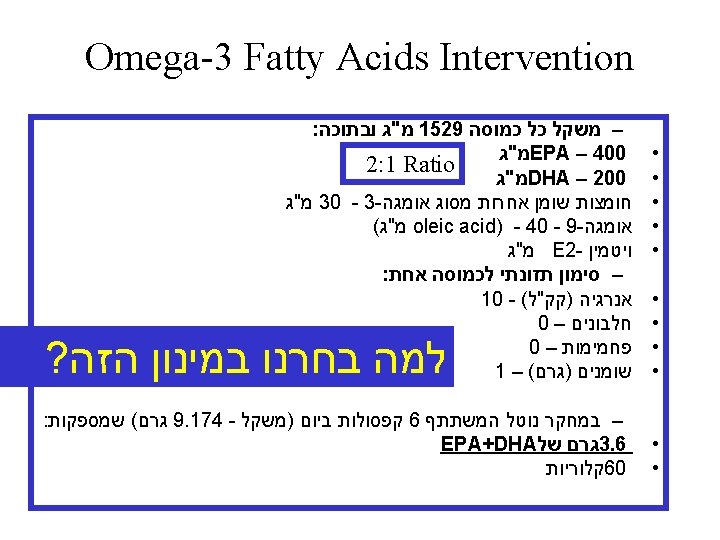
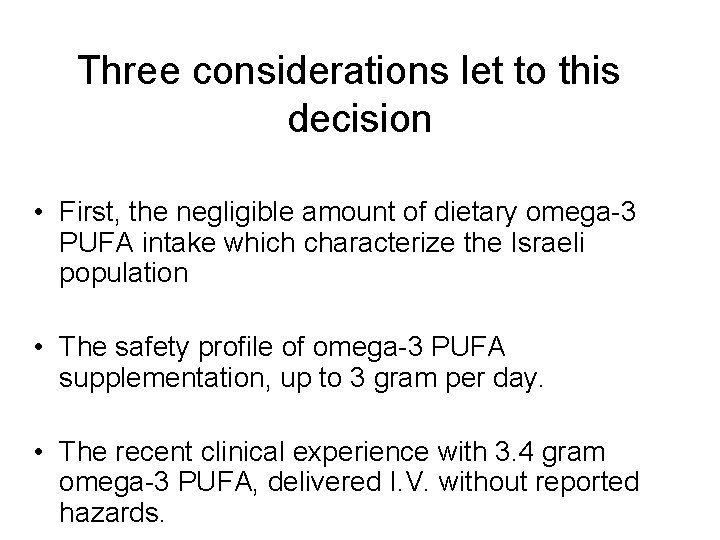
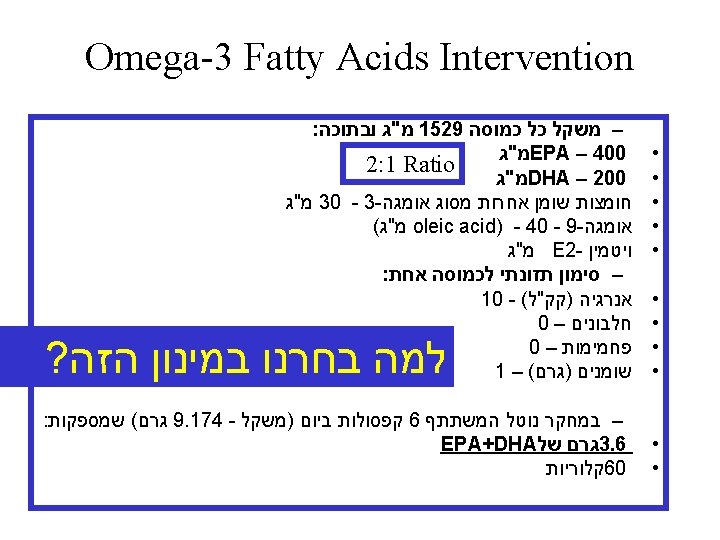
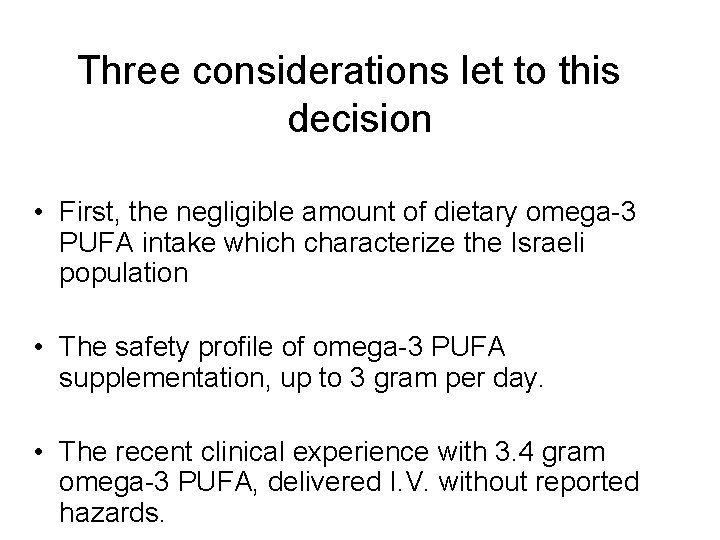
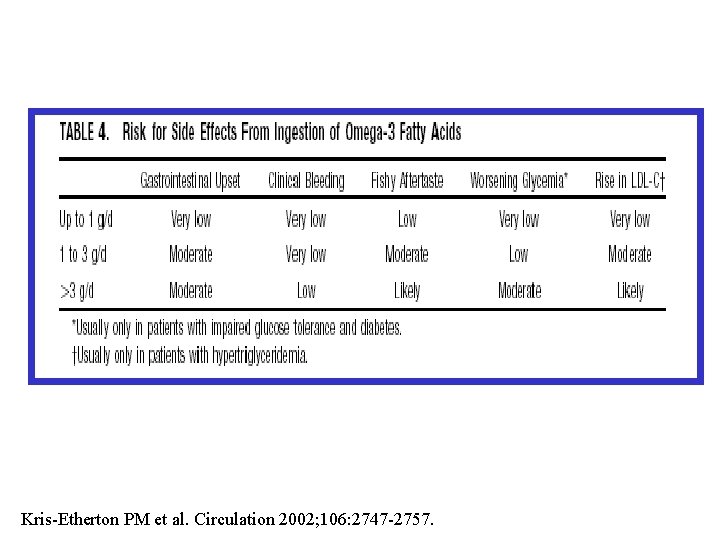
Three considerations let to this decision • First, the negligible amount of dietary omega-3 PUFA intake which characterize the Israeli population • The safety profile of omega-3 PUFA supplementation, up to 3 gram per day. • The recent clinical experience with 3. 4 gram omega-3 PUFA, delivered I. V. without reported hazards.

Reference Sample Size (N) Fish consumption (grams/day) EPA + DHA consumption (grams/day) 78 – 102 (mean range) 0. 04 – 0. 1 3242 27. 04 0. 17 605 (fish eaters only) 1124 144. 9 0. 75 10 Data not available 158 (fish eaters only) 91 Data not available NHANES [48]. Israel Center for Disease Control [47]. Daniel Abraham Nutrition Center, Ben-Gurion University (personal communication).

Three considerations let to this decision • The safety profile of omega-3 PUFA supplementation, up to 3 gram per day. • The recent clinical experience with 3. 4 gram omega-3 PUFA, delivered I. V. without reported hazards.
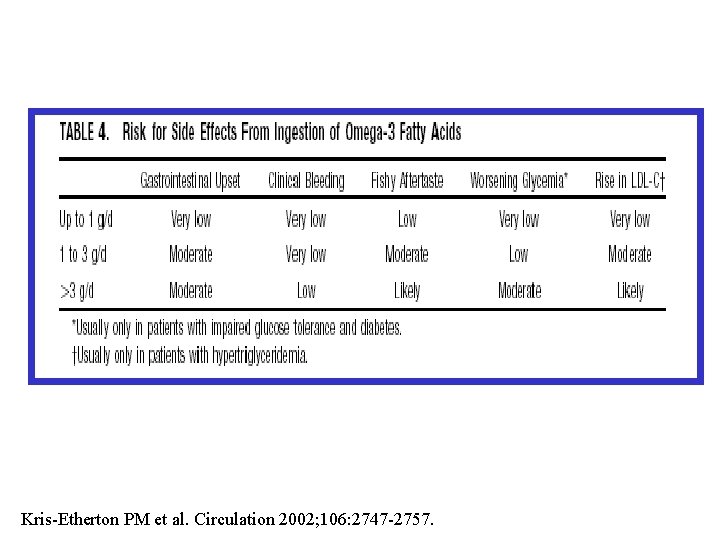
Kris-Etherton PM et al. Circulation 2002; 106: 2747 -2757.

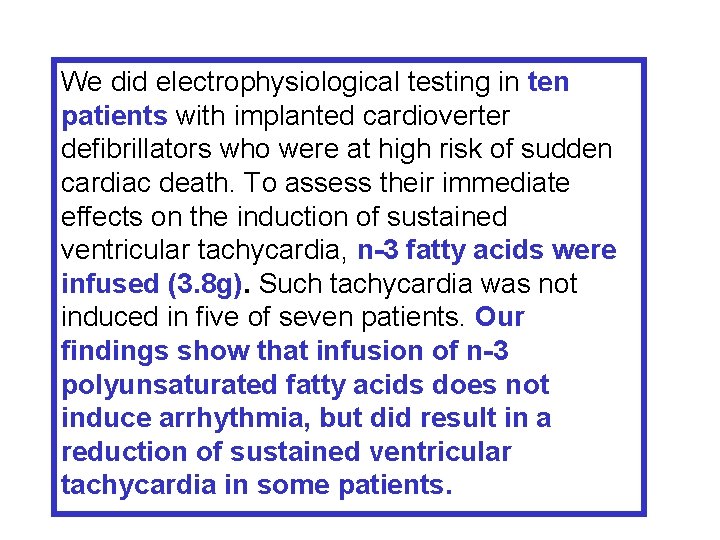
Three considerations let to this decision • The recent clinical experience with 3. 4 gram omega-3 PUFA, delivered I. V. without reported hazards.
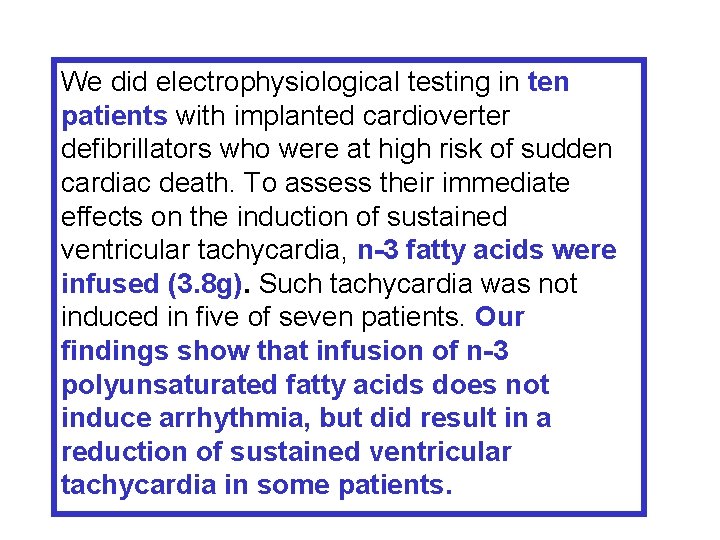
We did electrophysiological testing in ten patients with implanted cardioverter defibrillators who were at high risk of sudden cardiac death. To assess their immediate effects on the induction of sustained ventricular tachycardia, n-3 fatty acids were infused (3. 8 g). Such tachycardia was not induced in five of seven patients. Our findings show that infusion of n-3 polyunsaturated fatty acids does not induce arrhythmia, but did result in a reduction of sustained ventricular tachycardia in some patients.
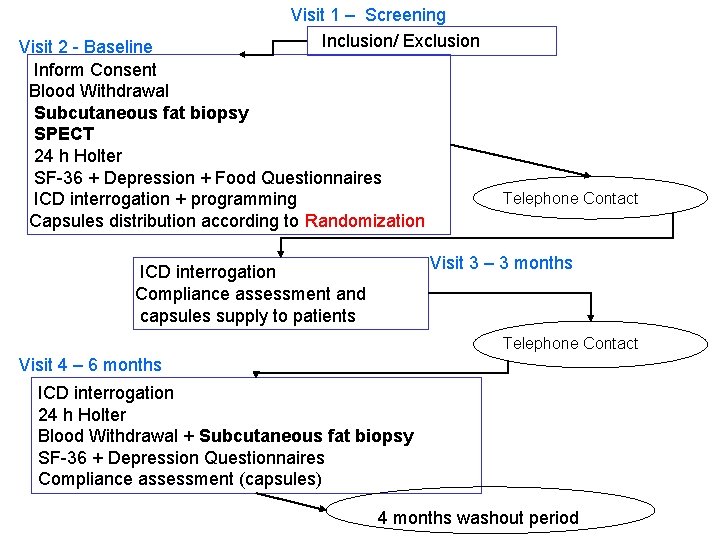
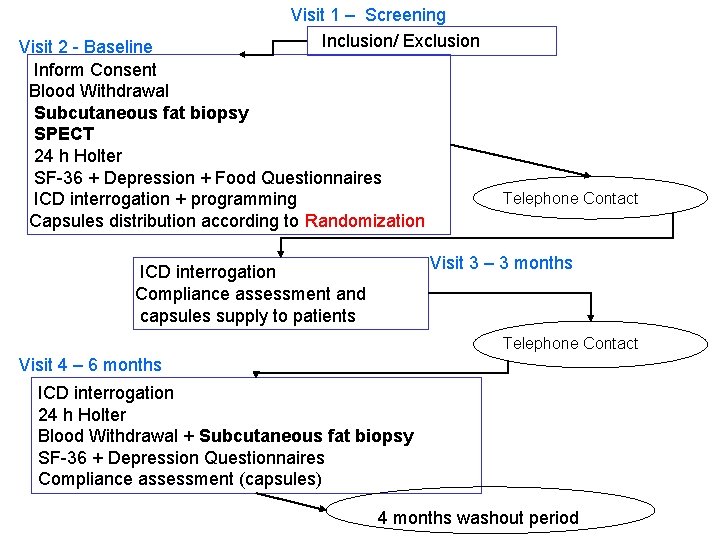
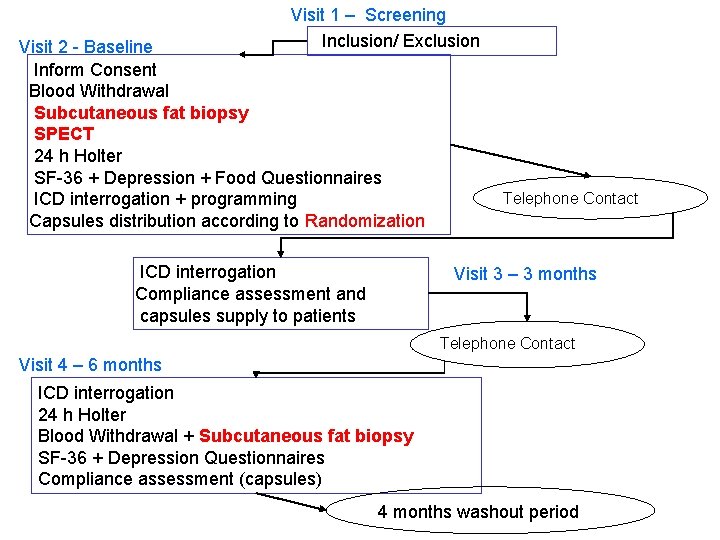
Visit 1 – Screening Inclusion/ Exclusion Visit 2 - Baseline Inform Consent Blood Withdrawal Subcutaneous fat biopsy SPECT 24 h Holter SF-36 + Depression + Food Questionnaires ICD interrogation + programming Capsules distribution according to Randomization Telephone Contact Visit 3 – 3 months ICD interrogation Compliance assessment and capsules supply to patients Telephone Contact Visit 4 – 6 months ICD interrogation 24 h Holter Blood Withdrawal + Subcutaneous fat biopsy SF-36 + Depression Questionnaires Compliance assessment (capsules) 4 months washout period


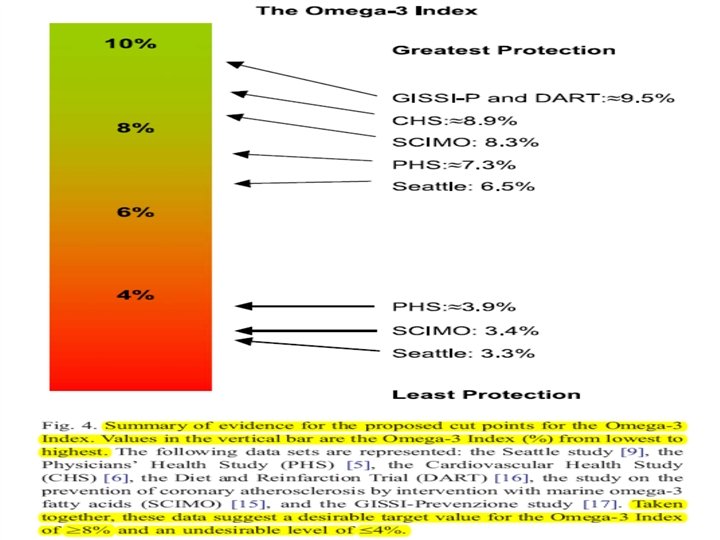
A case for the use of the Omega-3 Index as a risk stratification tool for CHD death. Harris et al. suggested that an Omega-3 Index level of ≥ 8% is a reasonable preliminary target value for reducing risk. The Omega-3 Index may represent a novel, physiologically relevant, modifiable, and independent marker of risk for death from CHD.

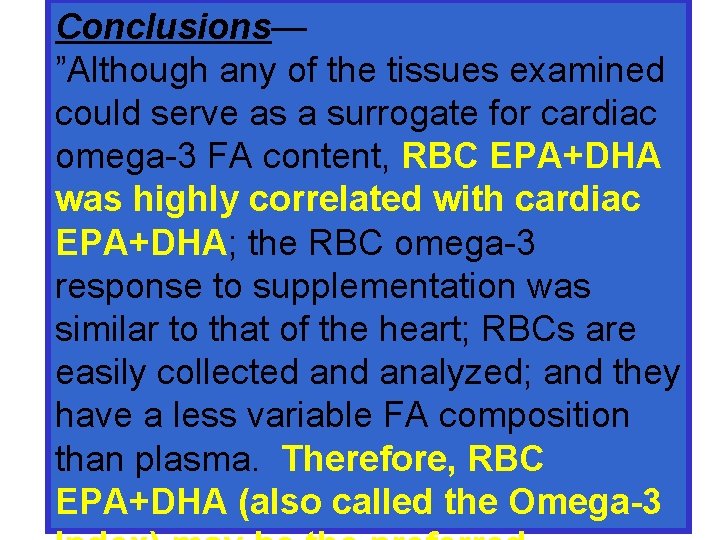
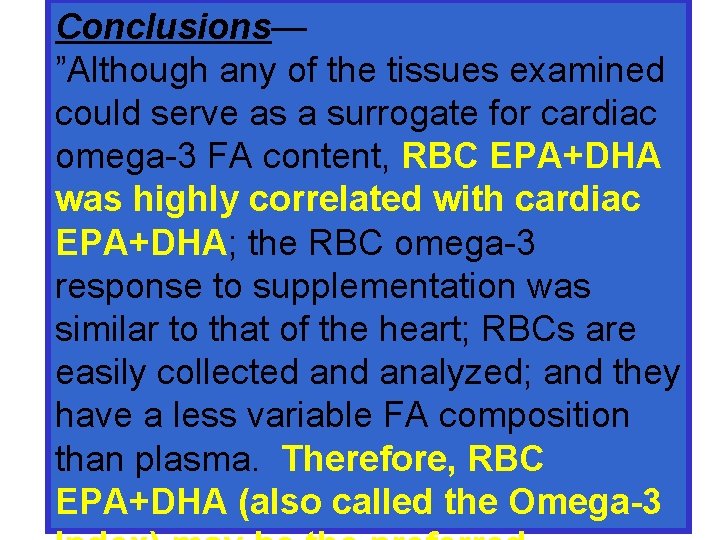
Conclusions— ”Although any of the tissues examined could serve as a surrogate for cardiac omega-3 FA content, RBC EPA+DHA was highly correlated with cardiac EPA+DHA; the RBC omega-3 response to supplementation was similar to that of the heart; RBCs are easily collected analyzed; and they have a less variable FA composition than plasma. Therefore, RBC EPA+DHA (also called the Omega-3

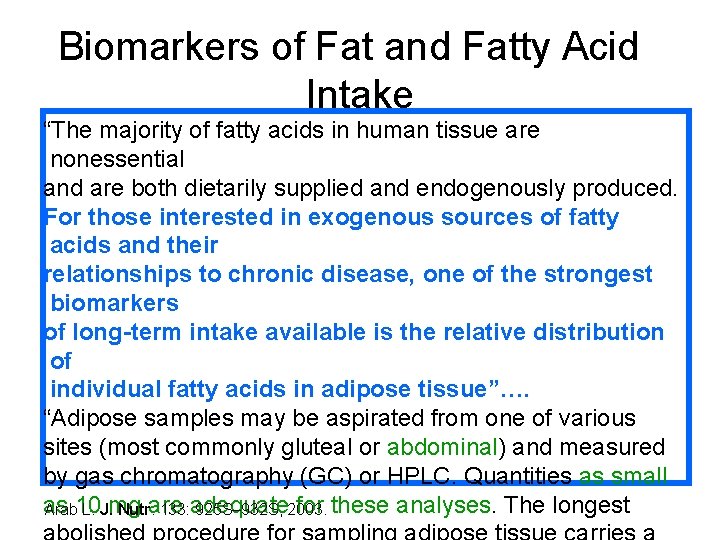
We also chose to obtain subcutaneous adipose-tissue biopsies, a biomarker considered the gold-standard for the objective assessment of long-term habitual dietary intake of fish and marine omega-3 PUFA (EPA and DHA). It can be considered a helpful tool in interpreting results.
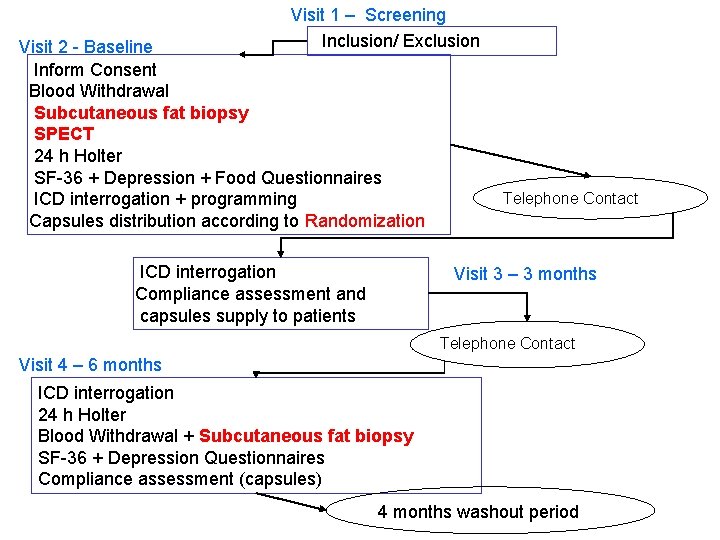
Visit 1 – Screening Inclusion/ Exclusion Visit 2 - Baseline Inform Consent Blood Withdrawal Subcutaneous fat biopsy SPECT 24 h Holter SF-36 + Depression + Food Questionnaires ICD interrogation + programming Capsules distribution according to Randomization ICD interrogation Compliance assessment and capsules supply to patients Telephone Contact Visit 3 – 3 months Telephone Contact Visit 4 – 6 months ICD interrogation 24 h Holter Blood Withdrawal + Subcutaneous fat biopsy SF-36 + Depression Questionnaires Compliance assessment (capsules) 4 months washout period

Subcutaneous Fat Biopsy


ADIPOSE TISSUE AS A MEDIUM FOR EPIDEMIOLOGIC EXPOSURE ASSESSMENT • “Experience in the use of adipose tissue sampling in epidemiologic studies in various countries has shown that it is simple to conduct, requires little training, carries little risk, and does not result in excessive participant refusal”. • In contrast to more traditional methods of assessment of long term dietary intakes it holds the promise of being able to sample past dietary habits Kohlmeier, Lenore, Kohlmeier, Martin, Environmental Health Perspectives Supplements, 10780475, Apr 95, Vol. 103, Issue Suppl. 3 without bias.
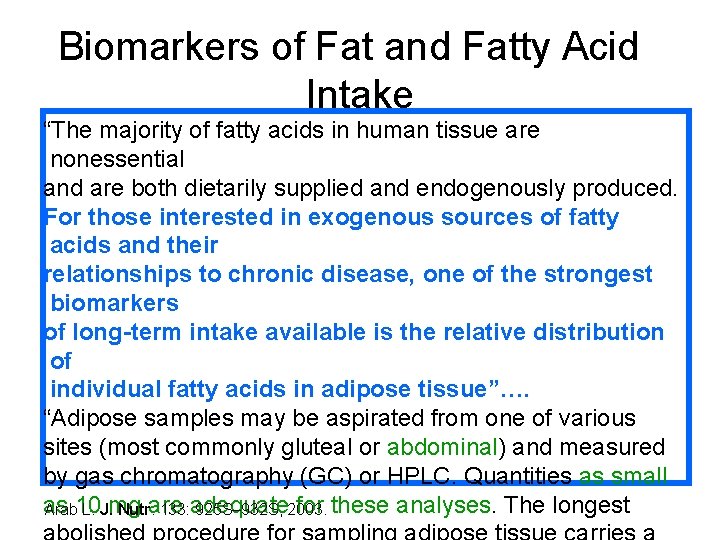
Biomarkers of Fat and Fatty Acid Intake “The majority of fatty acids in human tissue are nonessential and are both dietarily supplied and endogenously produced. For those interested in exogenous sources of fatty acids and their relationships to chronic disease, one of the strongest biomarkers of long-term intake available is the relative distribution of individual fatty acids in adipose tissue”…. “Adipose samples may be aspirated from one of various sites (most commonly gluteal or abdominal) and measured by gas chromatography (GC) or HPLC. Quantities as small as for these analyses. The longest Arab 10 L. J. mg Nutr. are 133: adequate 925 S– 932 S, 2003.

Visit 2 - Baseline Visit 1 – Screening Inclusion/ Exclusion Inform Consent Blood Withdrawal+ Subcutaneous fat biopsy SPECT 24 h Holter SF-36 + Depression + Food Questionnaires ICD interrogation + programming Capsules distribution according to Randomization Telephone Contact Visit 3 – 3 months ICD interrogation 24 h Holter Compliance assessment and capsules supply to patients Telephone Contact Visit 4 – 6 months ICD interrogation 24 h Holter Blood Withdrawal + Subcutaneous fat biopsy SF-36 + Depression Questionnaires Compliance assessment (capsules) 3 months washout period
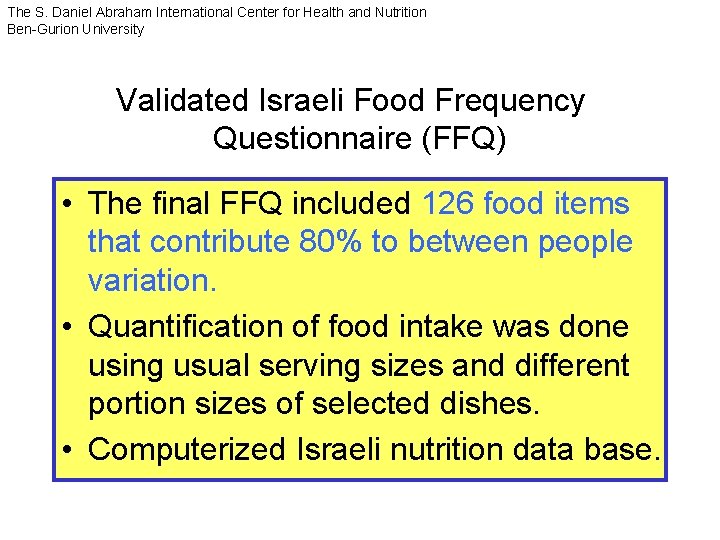
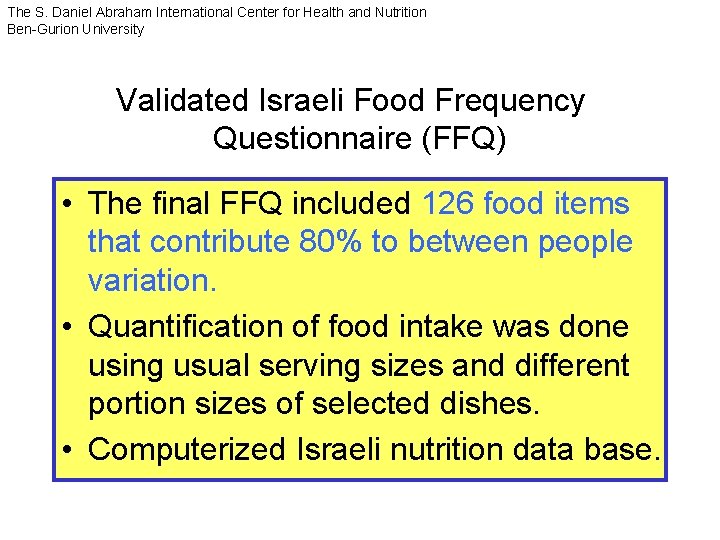
The S. Daniel Abraham International Center for Health and Nutrition Ben-Gurion University Validated Israeli Food Frequency Questionnaire (FFQ) • The final FFQ included 126 food items that contribute 80% to between people variation. • Quantification of food intake was done using usual serving sizes and different portion sizes of selected dishes. • Computerized Israeli nutrition data base.
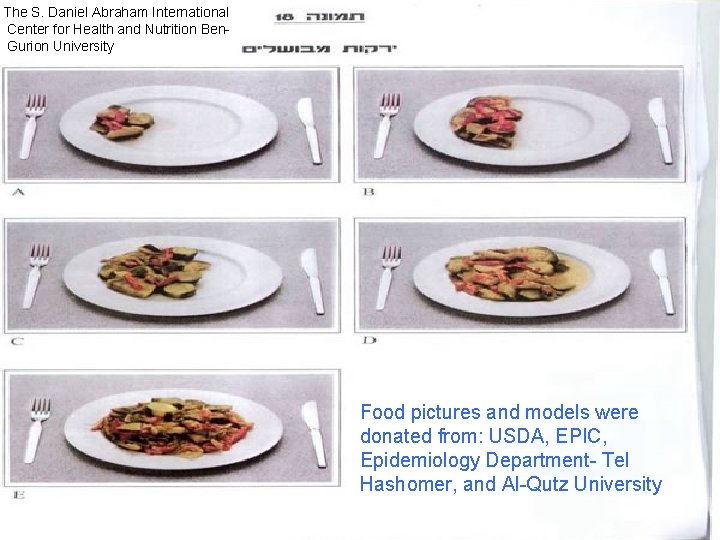
The S. Daniel Abraham International Center for Health and Nutrition Ben. Gurion University Food pictures and models were donated from: USDA, EPIC, Epidemiology Department- Tel Hashomer, and Al-Qutz University
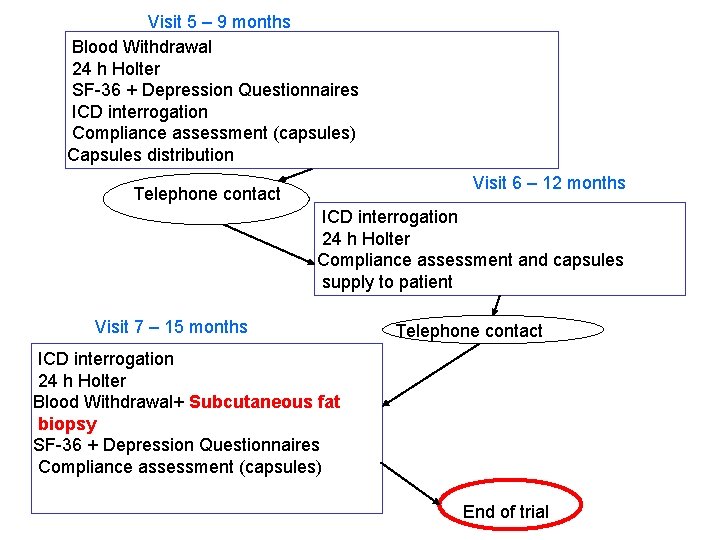
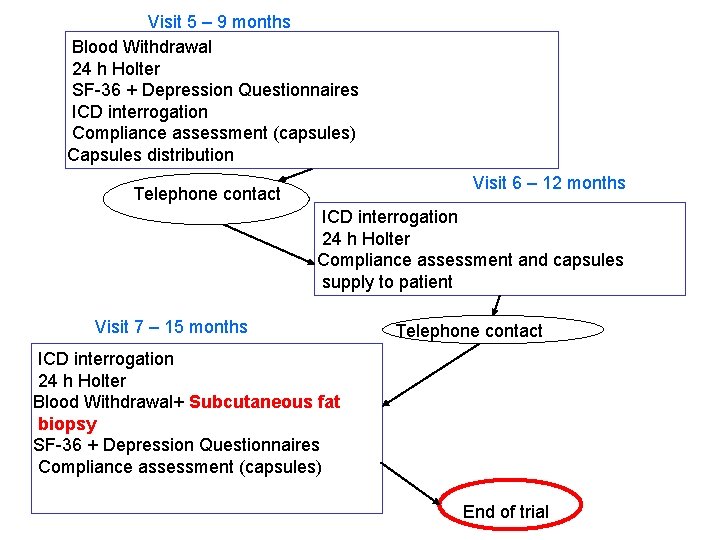
Visit 5 – 9 months Blood Withdrawal 24 h Holter SF-36 + Depression Questionnaires ICD interrogation Compliance assessment (capsules) Capsules distribution Visit 6 – 12 months Telephone contact ICD interrogation 24 h Holter Compliance assessment and capsules supply to patient Visit 7 – 15 months Telephone contact ICD interrogation 24 h Holter Blood Withdrawal+ Subcutaneous fat biopsy SF-36 + Depression Questionnaires Compliance assessment (capsules) End of trial

 Omega3
Omega3 Jerry weisman
Jerry weisman Kilalanin ang karaniwang layunin ng mga akdang patula
Kilalanin ang karaniwang layunin ng mga akdang patula Tanaga halimbawa 7-7-7-7
Tanaga halimbawa 7-7-7-7 Dalit moksha
Dalit moksha Cinquain tula halimbawa
Cinquain tula halimbawa Ang tawag sa dula na namalasak sa panahon ng amerikano.
Ang tawag sa dula na namalasak sa panahon ng amerikano. Pediatric assesment triangle
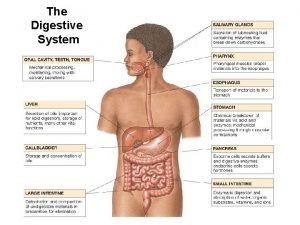
Pediatric assesment triangle Comparison of skeletal cardiac and smooth muscle
Comparison of skeletal cardiac and smooth muscle Characteristics of skeletal smooth and cardiac muscle
Characteristics of skeletal smooth and cardiac muscle Com
Com Lesson 6: cardiac emergencies and using an aed
Lesson 6: cardiac emergencies and using an aed Cardiac rhythms and interventions
Cardiac rhythms and interventions Slide
Slide Comparison of skeletal cardiac and smooth muscle
Comparison of skeletal cardiac and smooth muscle Refractory period cardiac
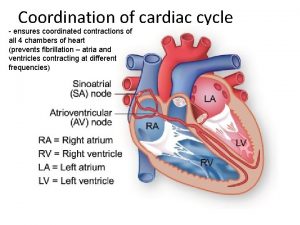
Refractory period cardiac Cardiac cycle
Cardiac cycle Characteristics of skeletal smooth and cardiac muscle
Characteristics of skeletal smooth and cardiac muscle Characteristics of skeletal smooth and cardiac muscle
Characteristics of skeletal smooth and cardiac muscle Cardiac stimulants and depressants
Cardiac stimulants and depressants Cardiac output and stroke volume
Cardiac output and stroke volume Co = hr x sv
Co = hr x sv Cardiac output and heart rate
Cardiac output and heart rate Gross features
Gross features Homometric regulation of cardiac output
Homometric regulation of cardiac output Cardiac distension
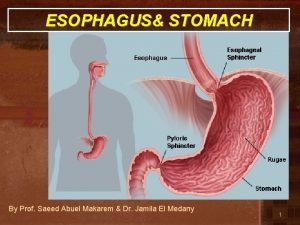
Cardiac distension Cardiac sphincter
Cardiac sphincter Cardiac cycle steps
Cardiac cycle steps Cardiac fundic pyloric
Cardiac fundic pyloric Cardiac portion of stomach
Cardiac portion of stomach Cardiac orifice
Cardiac orifice Smooth muslce
Smooth muslce Mets score cardiac
Mets score cardiac Lidocaine in cardiac arrest
Lidocaine in cardiac arrest Aschoff bodies diagram
Aschoff bodies diagram Renal denervation
Renal denervation Amputation bed introduction
Amputation bed introduction Fick cardiac output
Fick cardiac output Dullness of heart
Dullness of heart Bed cradle comfort device
Bed cradle comfort device Gastroesophageal junction histology labeled
Gastroesophageal junction histology labeled Svv cardiac
Svv cardiac Map tpr x co
Map tpr x co Cardiac orifice of stomach
Cardiac orifice of stomach Medany makarem
Medany makarem Stomach location
Stomach location Nyha classification
Nyha classification Wandering atrial pacemaker ecg
Wandering atrial pacemaker ecg Nesiritide mechanism of action
Nesiritide mechanism of action Coordination of the cardiac cycle
Coordination of the cardiac cycle Cardiac clearance meaning
Cardiac clearance meaning Acute responses to training definition
Acute responses to training definition Cardiac output trained vs untrained
Cardiac output trained vs untrained Cardiac output trained vs untrained
Cardiac output trained vs untrained Cardiac output trained vs untrained
Cardiac output trained vs untrained William harwey
William harwey