Oligohydramnios and Polyhydramnios Hesham Adel MD IMPORTANT TOPICS







- Slides: 45
Oligohydramnios and Polyhydramnios Hesham Adel MD
IMPORTANT TOPICS Amniotic fluid function Clinical importance of AF Volume and composition Amniotic fluid abnormalities
Amniotic fluid function: Allows room for fetal growth, movement and development. Ingestion into GIT→ growth and maturation. Fetal pulmonary development (20 weeks). Protects the fetus from trauma. Maintains temperature. Contains antibacterial activity. Aids dilatation of the cervix during labor. Protects cord and placenta from compression in labor
Clinical importance of AF: Screening for fetal malformation (amniotc fluid αfetoprotein). Assessment of fetal well-being (amniotic fluid index). Assessment of fetal lung maturity (L/S ratio). Diagnosis and follow up of labour. Diagnosis of PROM (ferning test).
Amniotic fluid formation and composition: First & early second trimester : Amount is 5 -50 ml & arises from: - ultrafiltrate of Maternal plasma through the vascularized uterine decidua (in early pregnancy). - Transudation of fetal plasma through the fetal skin & umbilical cord (up to 20 weeks' gestation).
Volume and composition From 20 weeks up to term (mainly fetal urine): - At 18 th week, the fetus voids 7 -14 ml/day; at term fetal kidneys secrete 600 -700 ml of urine/day into AF. - Fetal respiratory tract secretes 250 ml/day into AF. - Fluid transfer across the placenta. - Fetal oro-nasal secretions. Secretion is controlled by: - Fetal swallowing at term removes 500 ml/day. - Resorption into maternal plasma AF constituents: - urea, creatinine & uric acid + desquamated fetal cells, vernix, lanugo hair
Amniotic fluid volume : About 500 mls enter and leave the amniotic sac each hour. gradual ↑ up to 36 weeks to around 600 to 1000 ml then↓ after that. The normal range is wide but the approximate volumes are: - 500 ml at 18 weeks - 800 ml at 34 weeks. - 600 ml at term.
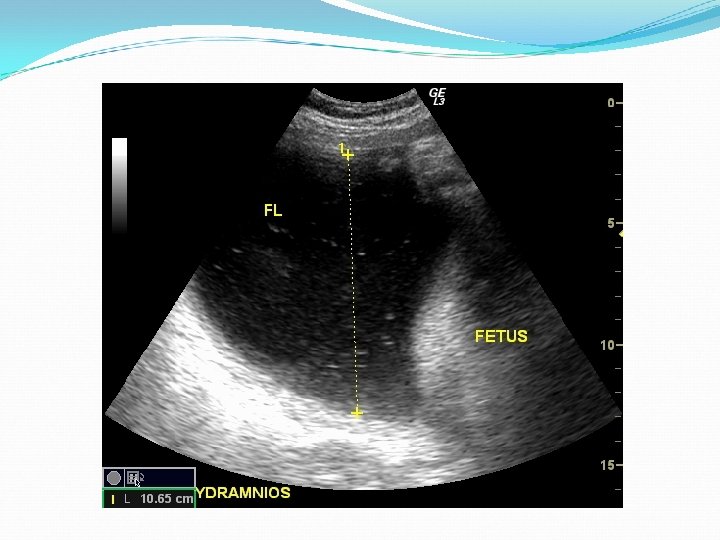
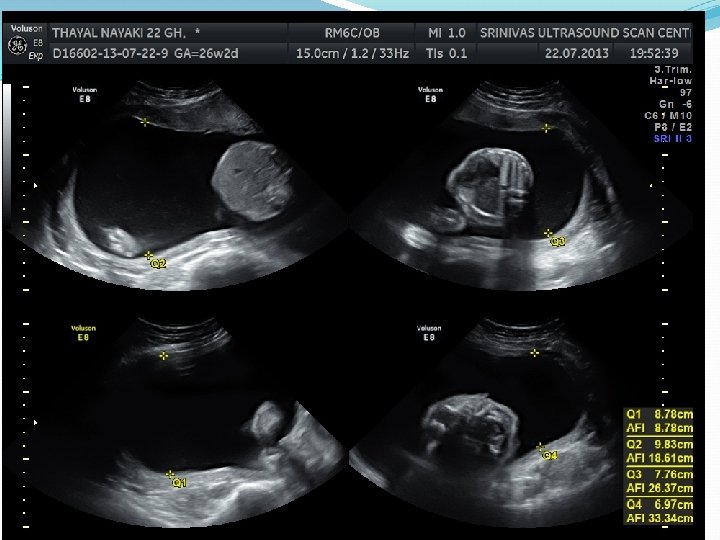
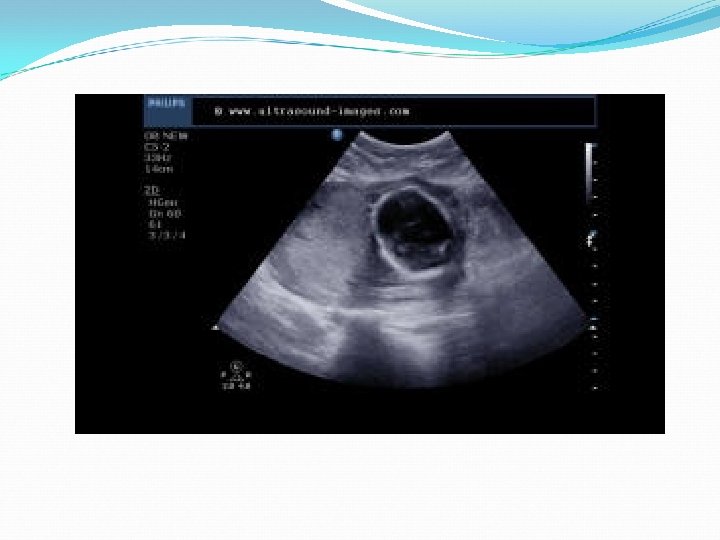
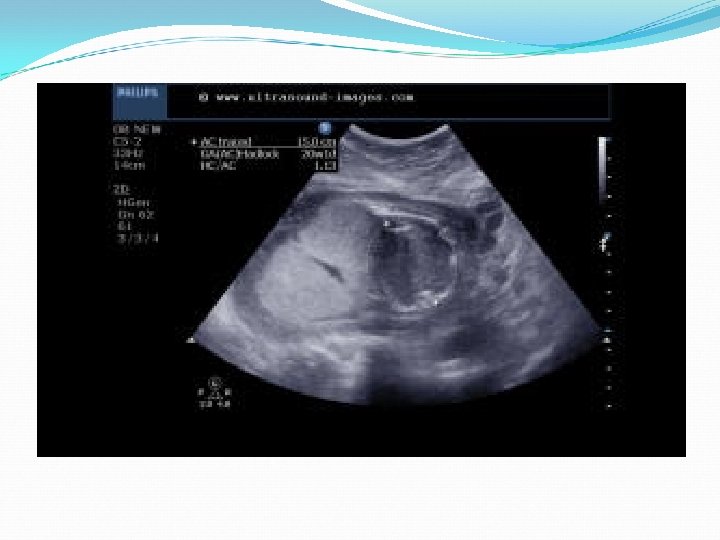
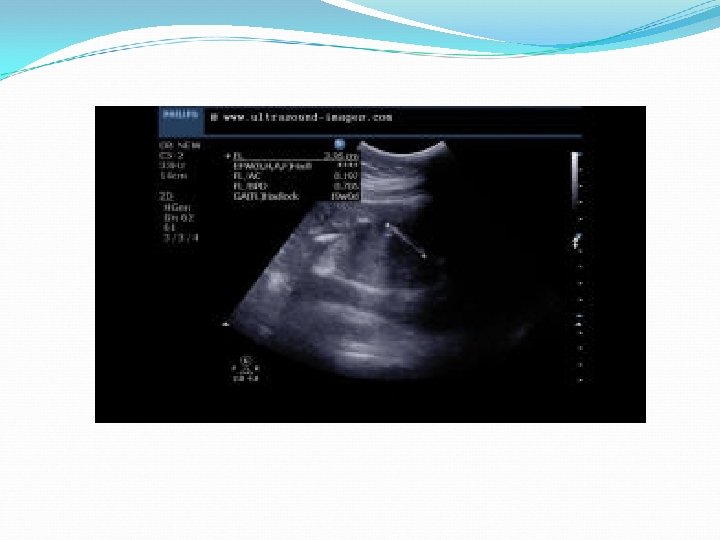
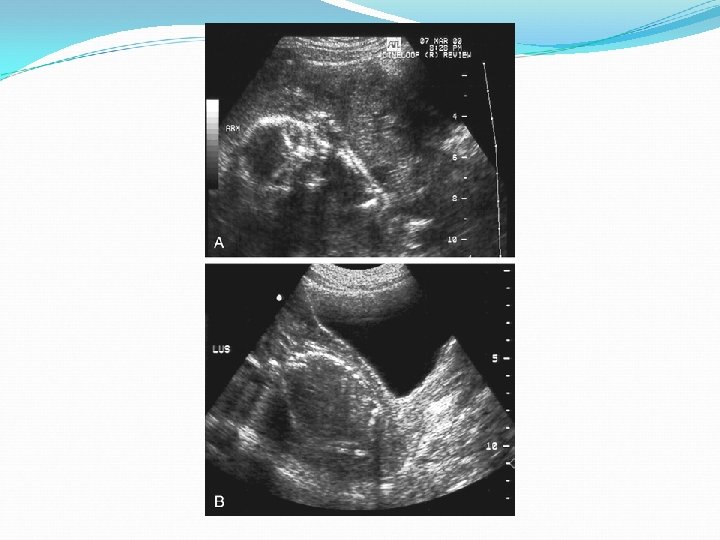
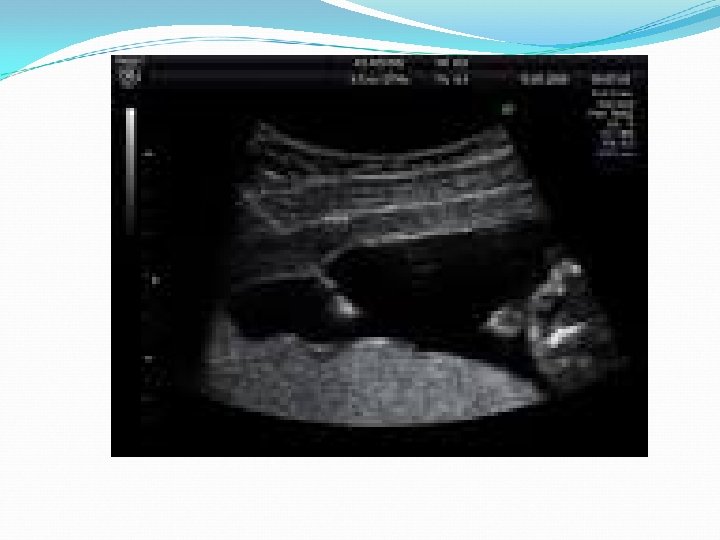
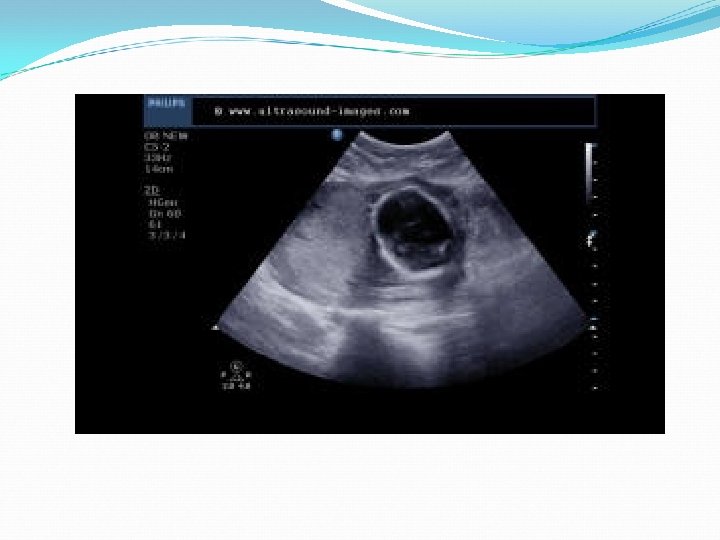
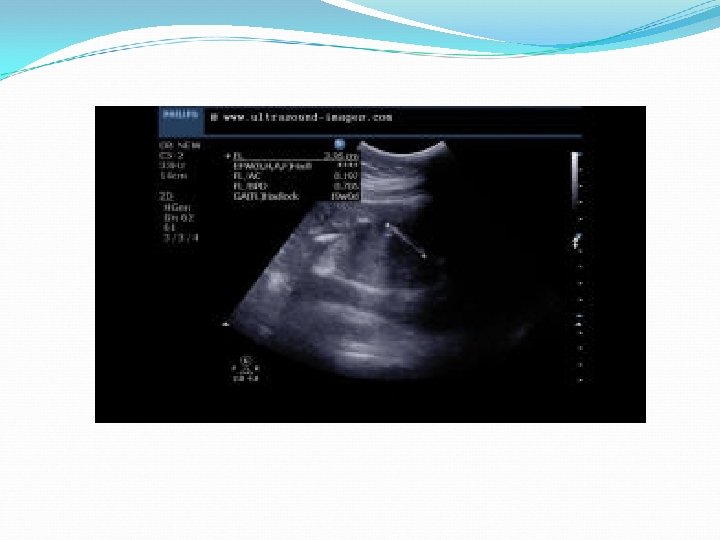
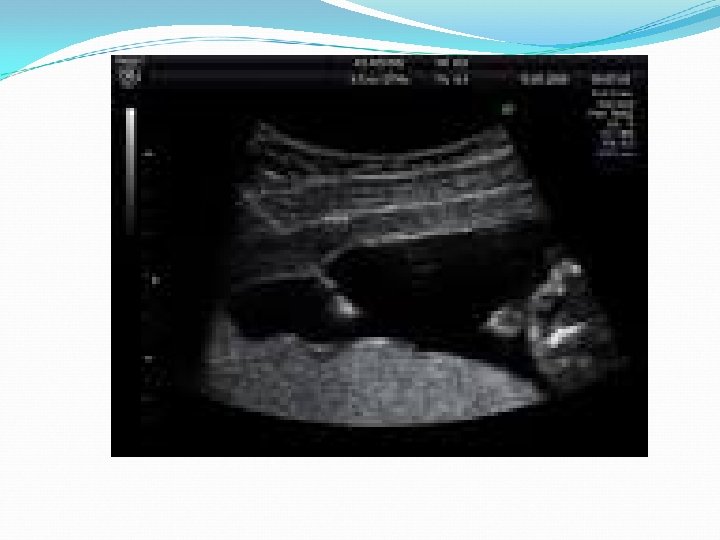
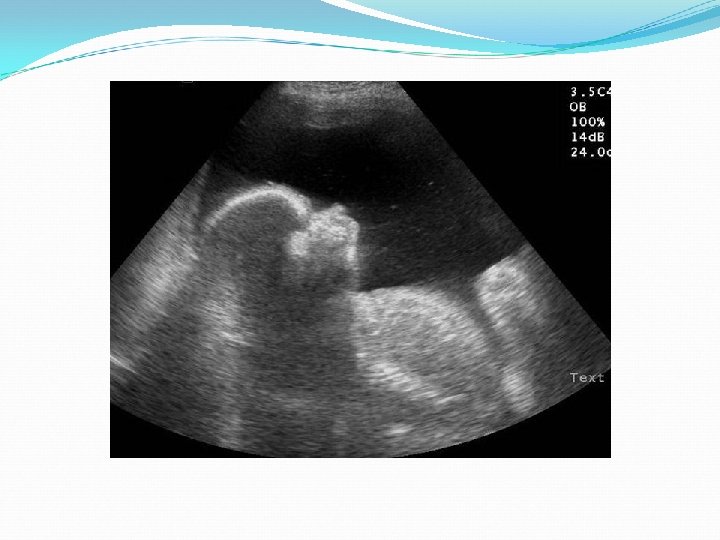
Amniotic fluid volume assessment Clinical assessment is unreliable. Objective assessment depends on U/S to measure: - deepest vertical pocket (DVP). - Amniotic fluid index (AFI): It is a total of the DVPs in each of the four quadrants of the uterus. it is a more sensitive indicator of AFV throughout pregnancy.
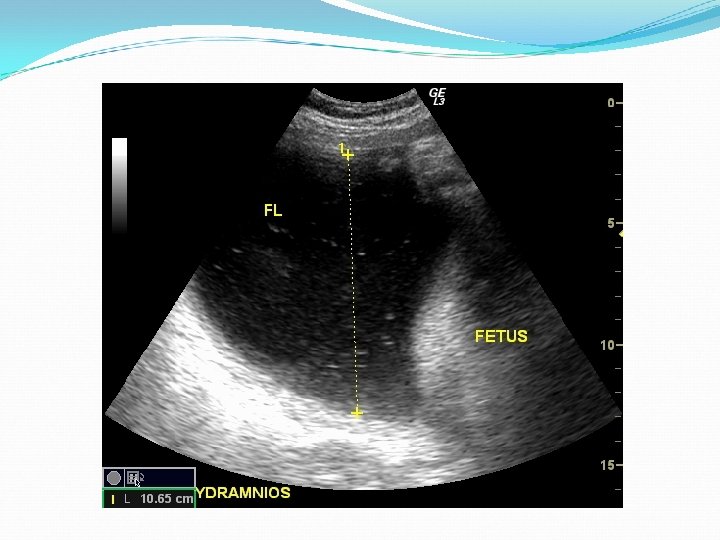
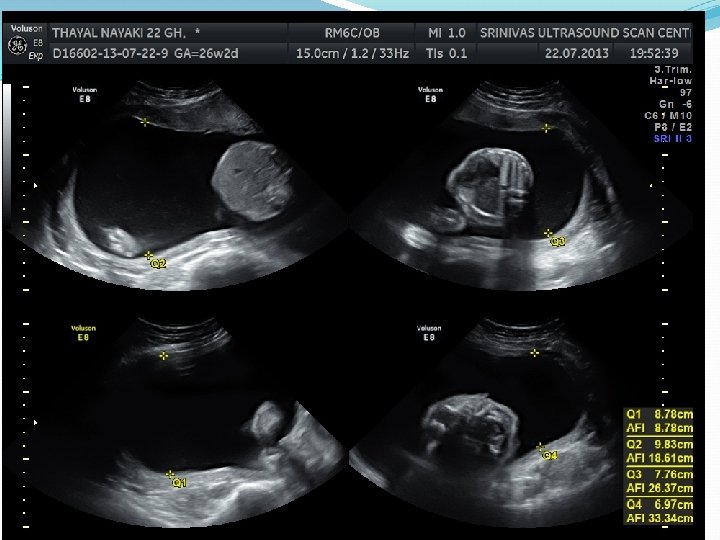
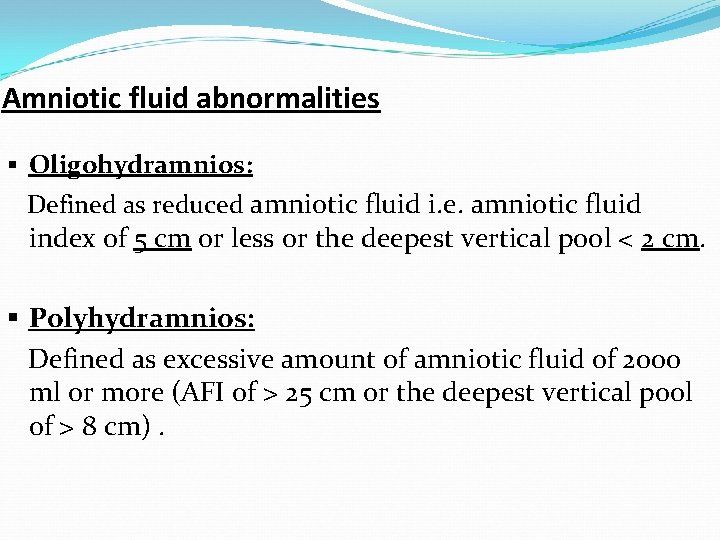
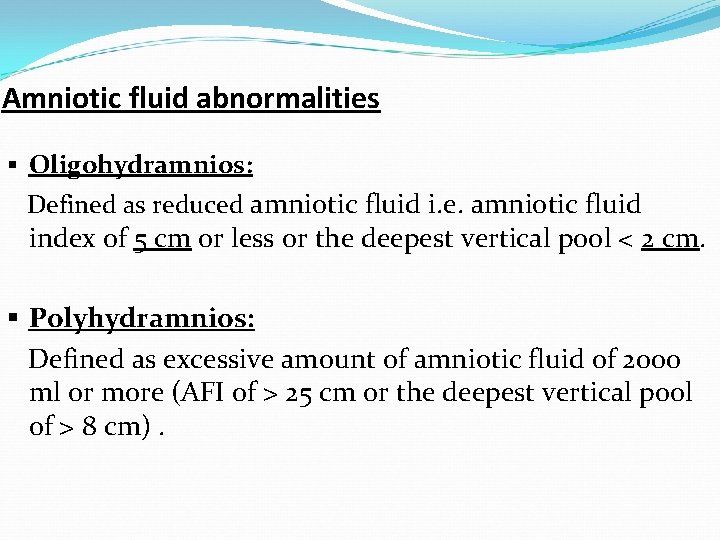
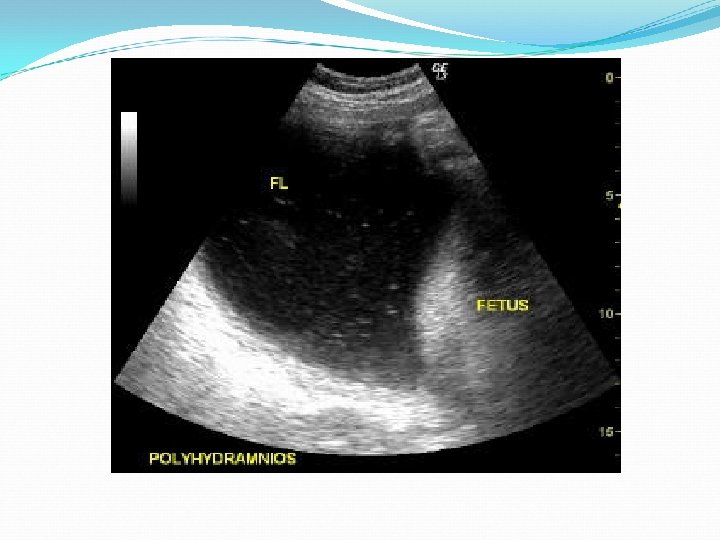
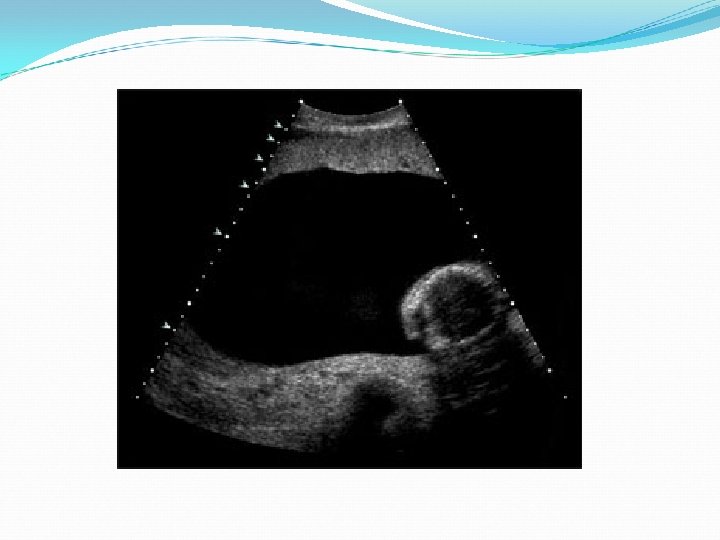
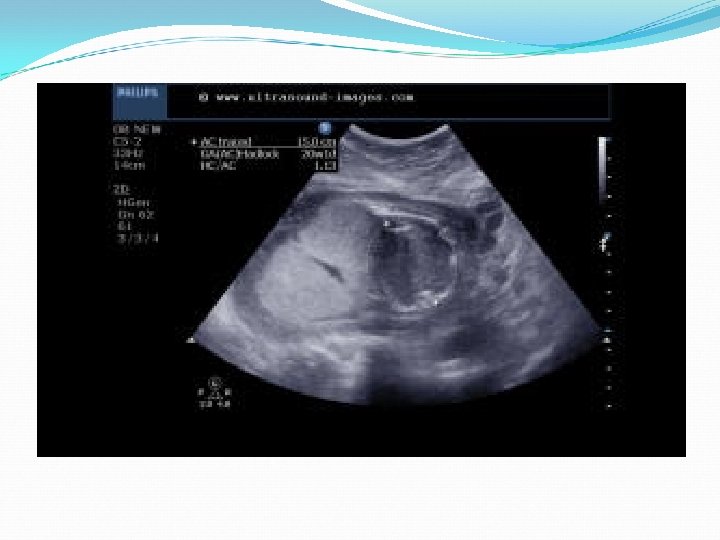
Amniotic fluid abnormalities § Oligohydramnios: Defined as reduced amniotic fluid i. e. amniotic fluid index of 5 cm or less or the deepest vertical pool < 2 cm. § Polyhydramnios: Defined as excessive amount of amniotic fluid of 2000 ml or more (AFI of > 25 cm or the deepest vertical pool of > 8 cm).
Causes of oligohydramnios: 1. Fetal causes: * Renal causes: - Renal agenesis (Potter’s syndrome). - polycystic kidney. - Urethral obstruction (atresia/posterior urethral valve). * Fetal growth restriction. * Fetal death. * Postterm pregnancy. * Preterm premature rupture membranes.
Causes of oligohydramnios (cont’): 2. Maternal causes: • Uteroplacental insufficiency. • Preeclampsia. 3. Placental causes: • twin-twin transfusion. 4. Drug causes: Prostaglandin synthase inhibitors as NSAID. 5. Idiopathic
Complications of oligohydramnios: In early pregnancy: • Amniotic adhesions or bands→ amputation/death. • Pressure deformities (Flattened face). • Pulmonary hypoplasia: - Thoracic compression. - No breathing movement. - No amniotic fluid retained in the lungs. • Postural deformities (Talipes Equino Varus).
Complications of oligohydramnios: In late pregnancy: • Fetal growth restriction (association rather than a complication). • Preterm labor. • Fetal distress. • Fetal death. • Meconium aspiration. • Labor induction/CS.
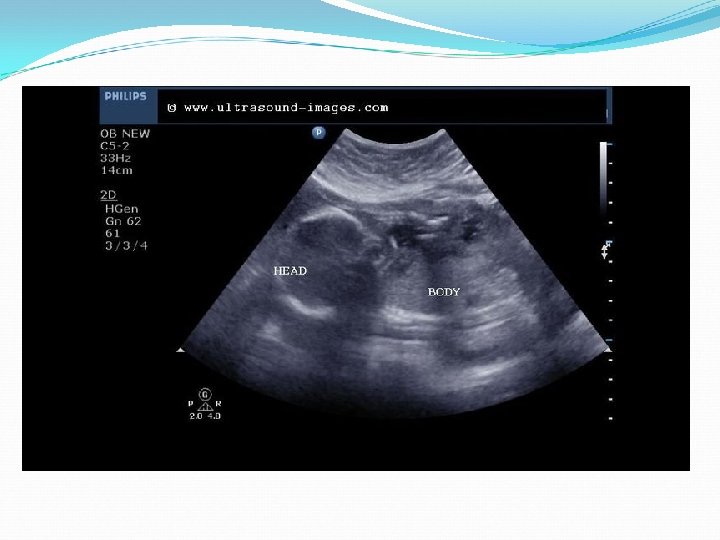
v. Diagnosis: - Fundal level < date. - AF I < 5 CM , DVP < 2. - IUGR: abdominal circumference < 10 th centile. - Doppler abnormalities - Congenital fetal anomalies.
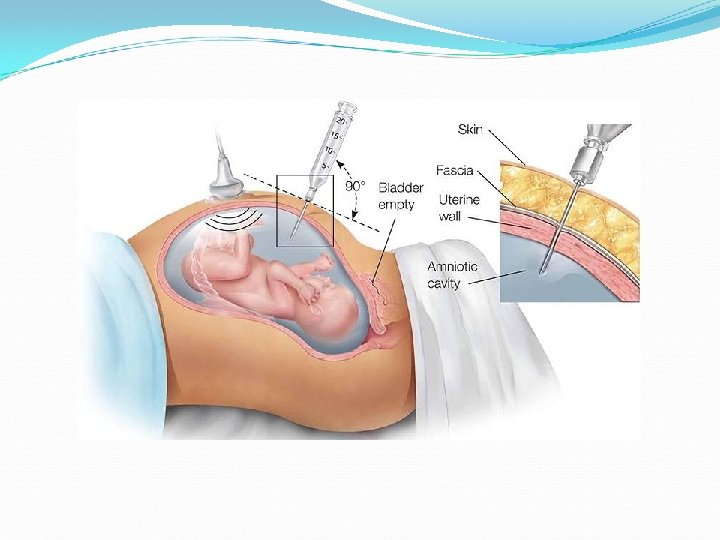
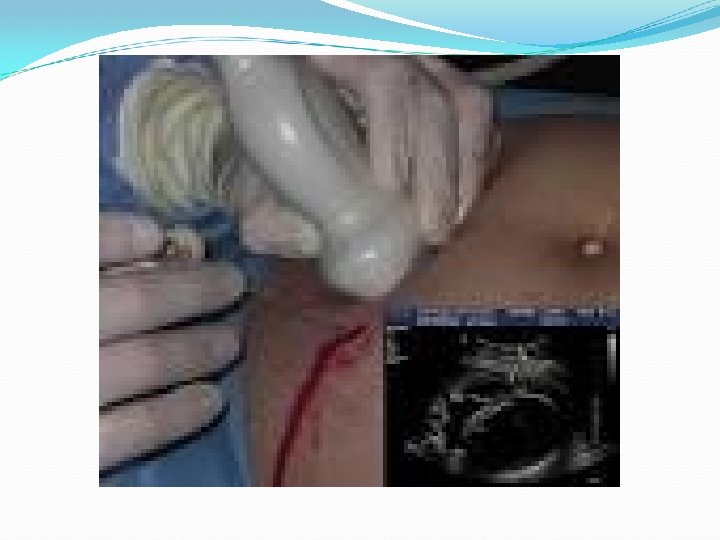
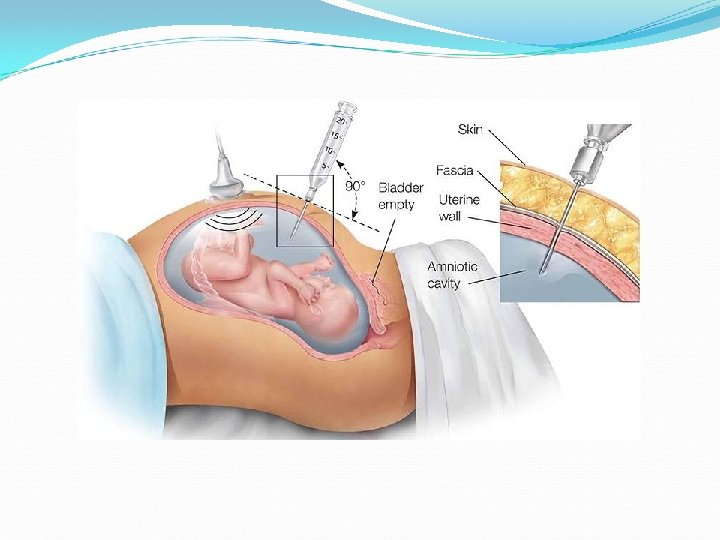
Management: -Treat the cause (pprom, preeclampsia). -Assess fatal wellbeing (U/S/CTG/Doppler/BPP). -Vesicoamniotic shunting (urethral obstruction). -Amnioinfusion: Indications of amnioinfusion: 1. Meconium stained amniotic fluid 2. Variable decelerations 3. Prophylactic for severe degrees
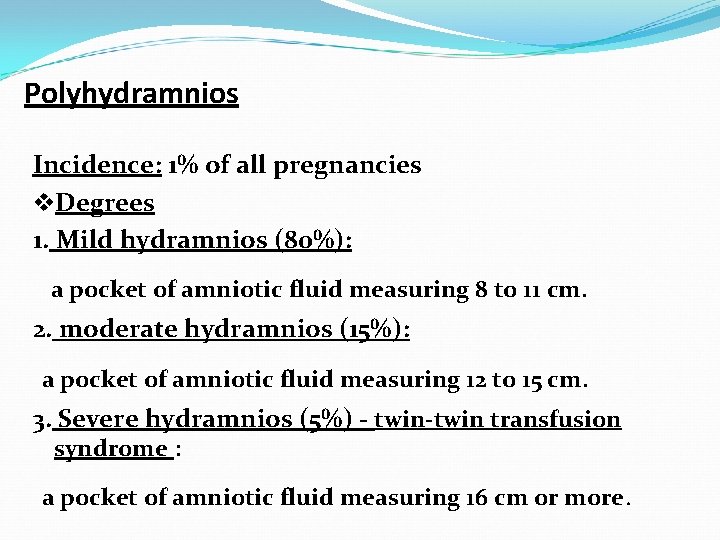
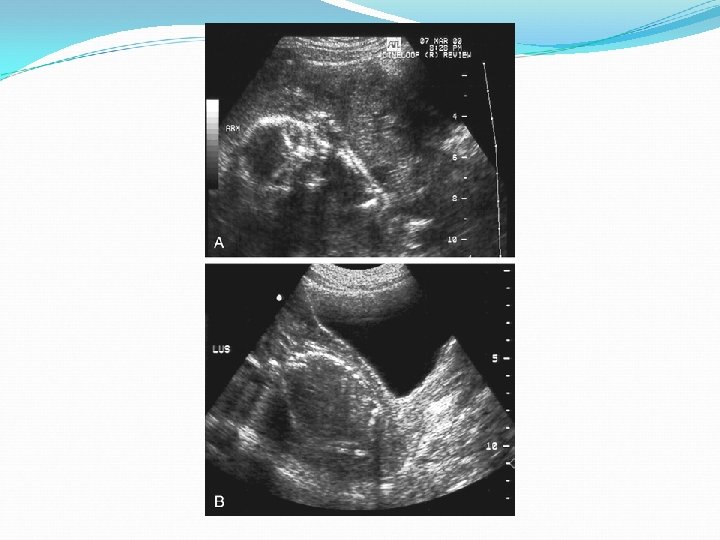
Polyhydramnios Incidence: 1% of all pregnancies v. Degrees 1. Mild hydramnios (80%): a pocket of amniotic fluid measuring 8 to 11 cm. 2. moderate hydramnios (15%): a pocket of amniotic fluid measuring 12 to 15 cm. 3. Severe hydramnios (5%) - twin-twin transfusion syndrome : a pocket of amniotic fluid measuring 16 cm or more.

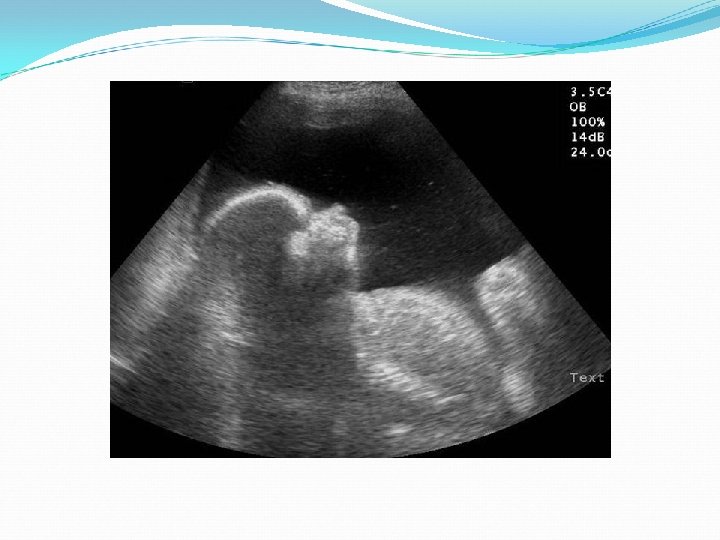
Causes of polyhydramnios Fetal malformation: - GIT: esophageal/duodenal atresia, tracheoesophageal fistula. - CNS: anencephaly (↓swallowing, exposed meninges, no antidiuretic hormone). Twin-twin transfusion → fetal polyuria.
Causes of polyhydramnios (cont’) Hydrops fetalis: congestive heart failure, severe anaemia or hypoproteinemia → placental transudation n Placental tumors e. g. chorioangioma n diabetes mellitus (osmotic diuresis). n Idiopathic 60%. n
Types: Acute: usually develops in the first half of pregnancy with rapid expansion to huge dimensions. Usually ends in abortion, or termination becomes mandatory Chronic: develops gradually so a much larger size can be tolerated.

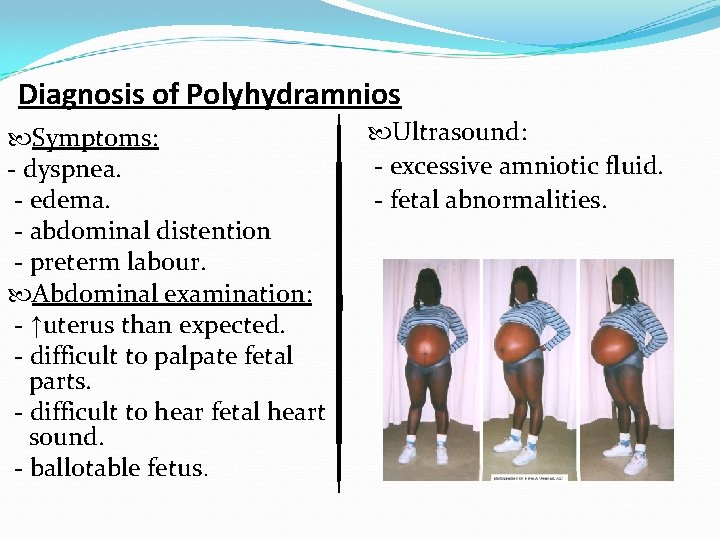
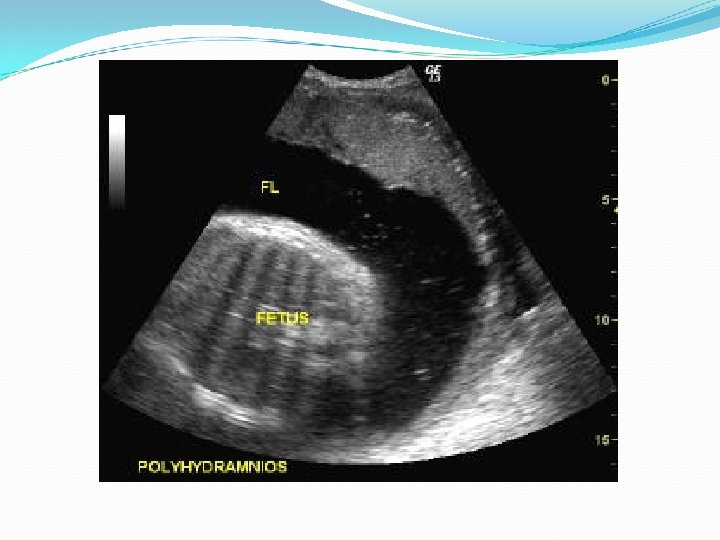
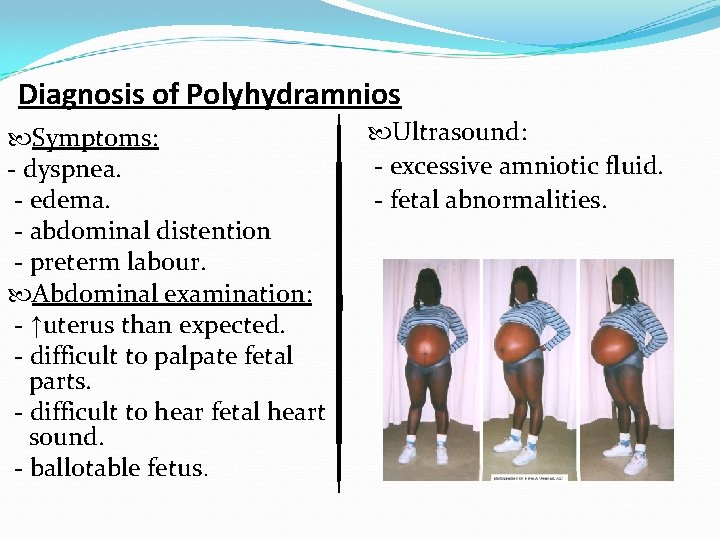
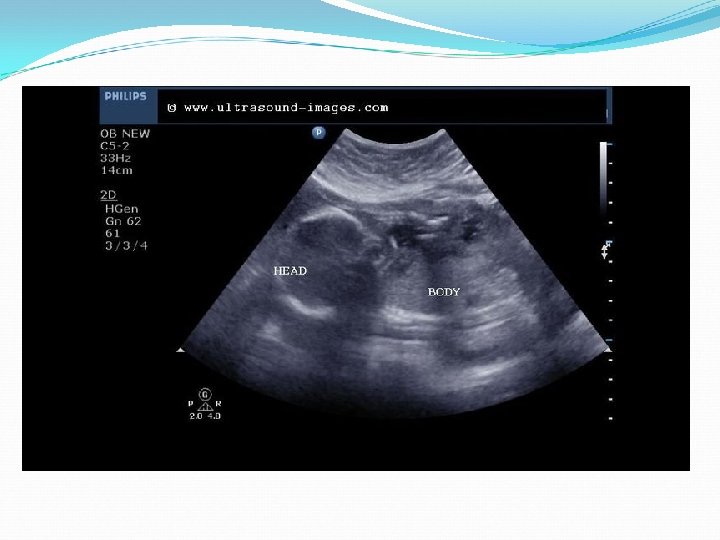
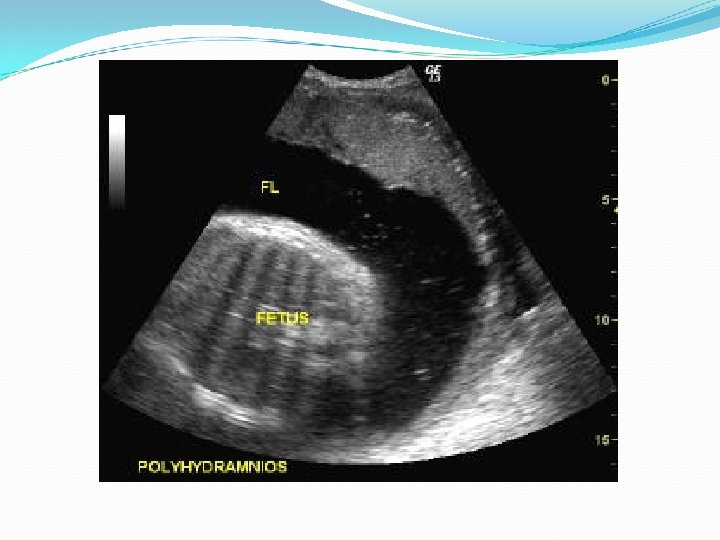
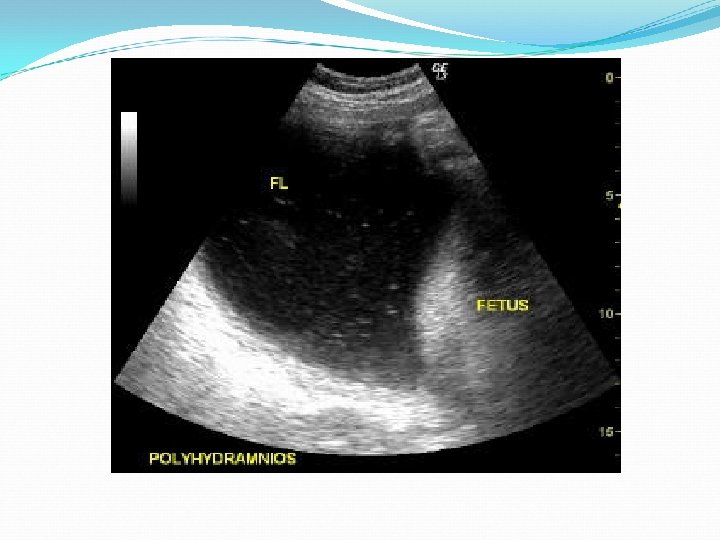
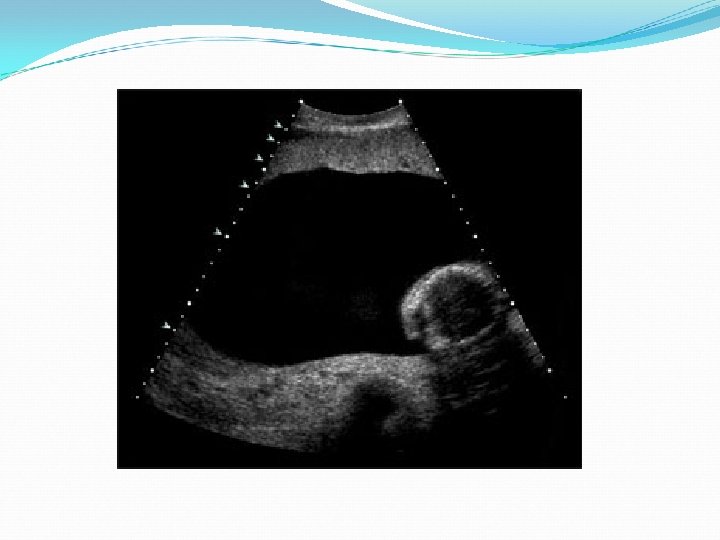
Diagnosis of Polyhydramnios Symptoms: - dyspnea. - edema. - abdominal distention - preterm labour. Abdominal examination: - ↑uterus than expected. - difficult to palpate fetal parts. - difficult to hear fetal heart sound. - ballotable fetus. Ultrasound: - excessive amniotic fluid. - fetal abnormalities.
Complications of Polyhydramnios Preeclampsia UTI Preterm labor PROM Accidental hemorrhage Cord prolapse Abnormal presentations Increased risk for C. S. Post-partum hemorrhage
Management Minor degrees: no treatment. Bed rest, diuretics, water and salt restriction: ineffective. Hospitalization: dyspnea, abdominal pain or difficult ambulation. Endomethacin therapy: - Decreases urine production - impairs lung liquid production/enhances absorption. - ↑fluid movement across fetal membranes. * complications: premature closure of ductus arteriosus, impairment of renal function, and cerebral vasoconstriction. So not used after 35 weeks
Management Amniocentesis: to relieve maternal distress and to test for fetal lung maturity. Complications: ruptured membrane, chorioamnionitis, placental abruption, preterm labour. Amniocentesis may be done repeatedly.




