Odontogenic cysts What is an odontogenic cyst A
- Slides: 15
Odontogenic cysts
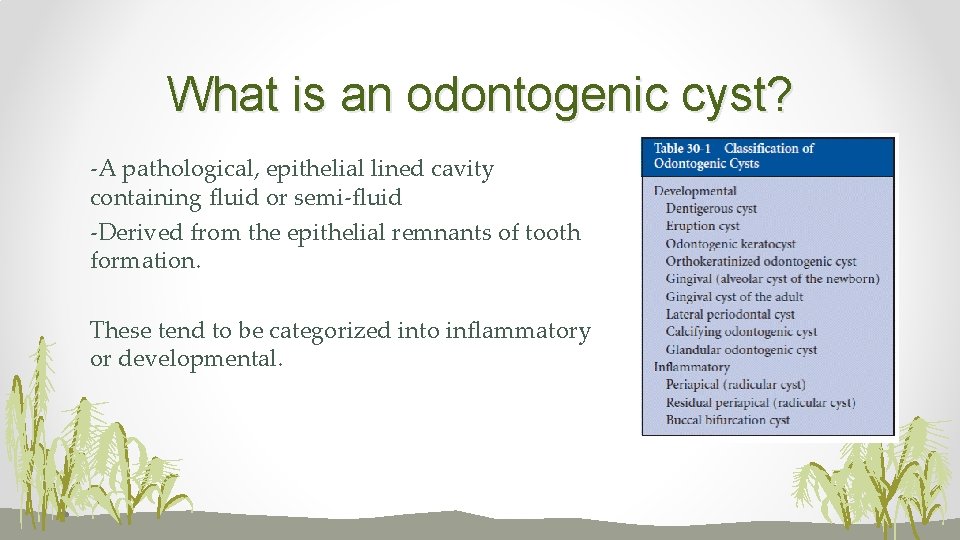
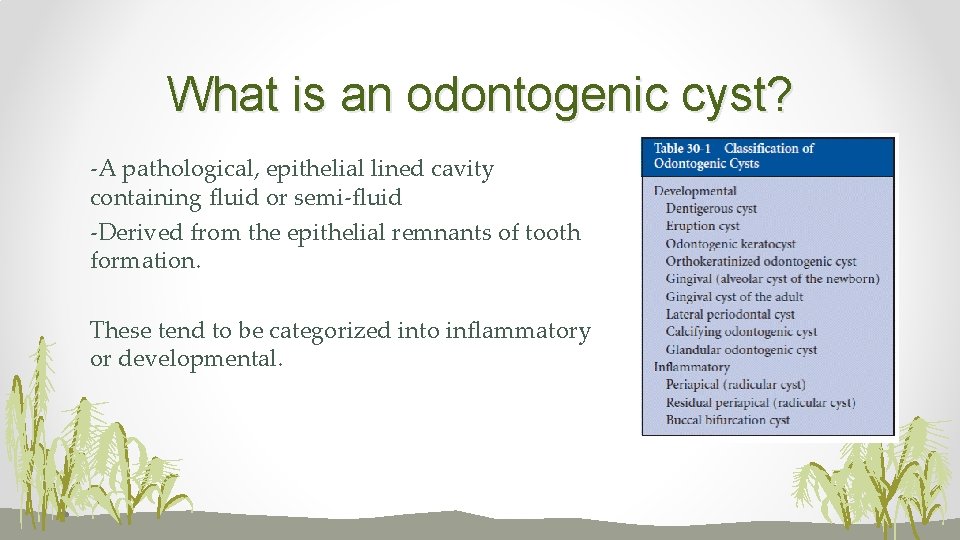
What is an odontogenic cyst? -A pathological, epithelial lined cavity containing fluid or semi-fluid -Derived from the epithelial remnants of tooth formation. These tend to be categorized into inflammatory or developmental.
Odontogenic cysts • Presentation; • often asymptomatic, incidental findings on x-rays. This is due to the slow nature of growth of cysts, they tend to displace rather than affect surrounding structures such as the inferior alveolar nerve so altered/loss of sensation is unlikely. • Swelling- egg shell crackling of thin overlying bone • Discharge- if a communication exists with the oral cavity • Pain- if the jaw fractures due to weakness or if the cyst is pathological • Incidence- More common in males • Overall 3 times more likely to be present in the mandible- however this is dependant on the type of cyst
Diagnosis of cysts • Cysts are diagnosed by a variety of methods; • Radiographically (size, location, relationship with teeth/surrounding structures) • CBCT can be used to gain a more accurate picture of the size of a cyst and the relationship to surrounding structures • Biopsy of cyst lining; for a definitive diagnosis • Aspiration of cyst contents- the colour and consistency is very useful in diagnosis
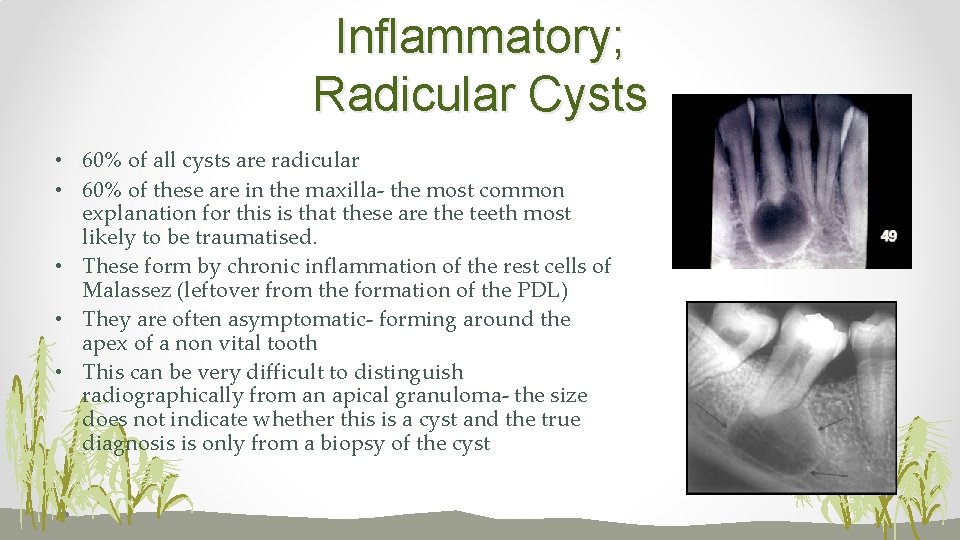
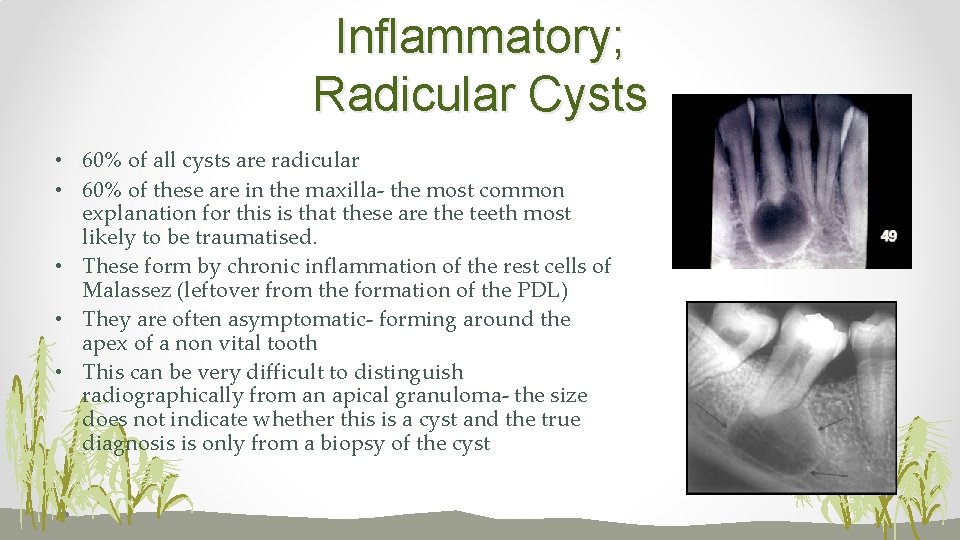
Inflammatory; Radicular Cysts • 60% of all cysts are radicular • 60% of these are in the maxilla- the most common explanation for this is that these are the teeth most likely to be traumatised. • These form by chronic inflammation of the rest cells of Malassez (leftover from the formation of the PDL) • They are often asymptomatic- forming around the apex of a non vital tooth • This can be very difficult to distinguish radiographically from an apical granuloma- the size does not indicate whether this is a cyst and the true diagnosis is only from a biopsy of the cyst
Radicular cysts contd • Treatment; root treatment of the affected tooth/ re-root treatment/ periradicular surgery/ extraction. Small cysts can regress but larger cysts require enucleation by peri-radicular surgery or extraction • Histologically- stratified squamous epithelium • Aspiration of a radicular cyst reveals straw like contents which is useful in diagnosis- particularly if the nature of the cyst is unclear
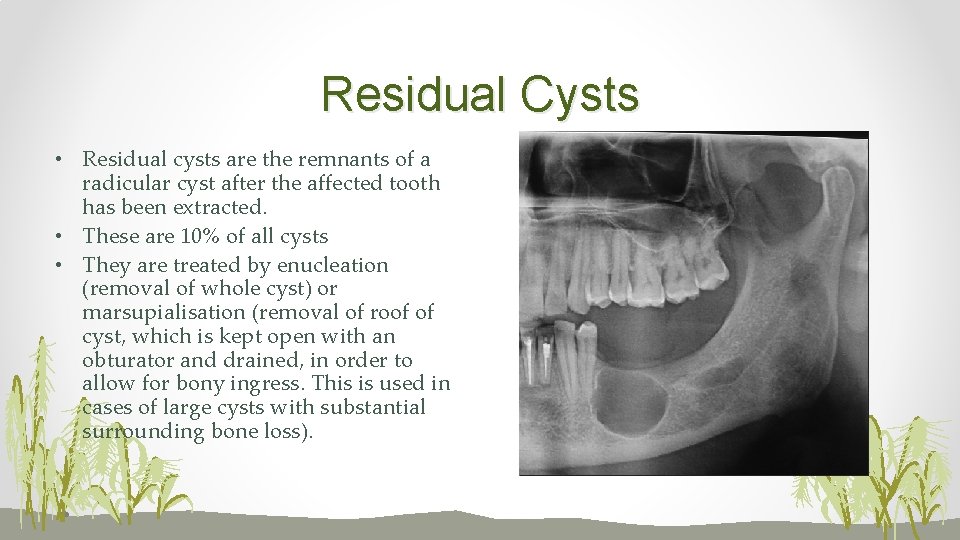
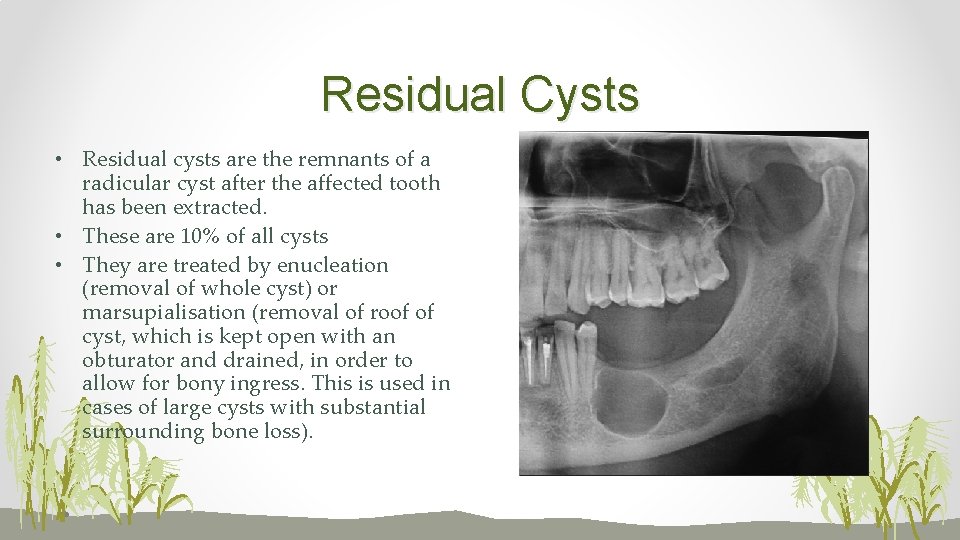
Residual Cysts • Residual cysts are the remnants of a radicular cyst after the affected tooth has been extracted. • These are 10% of all cysts • They are treated by enucleation (removal of whole cyst) or marsupialisation (removal of roof of cyst, which is kept open with an obturator and drained, in order to allow for bony ingress. This is used in cases of large cysts with substantial surrounding bone loss).
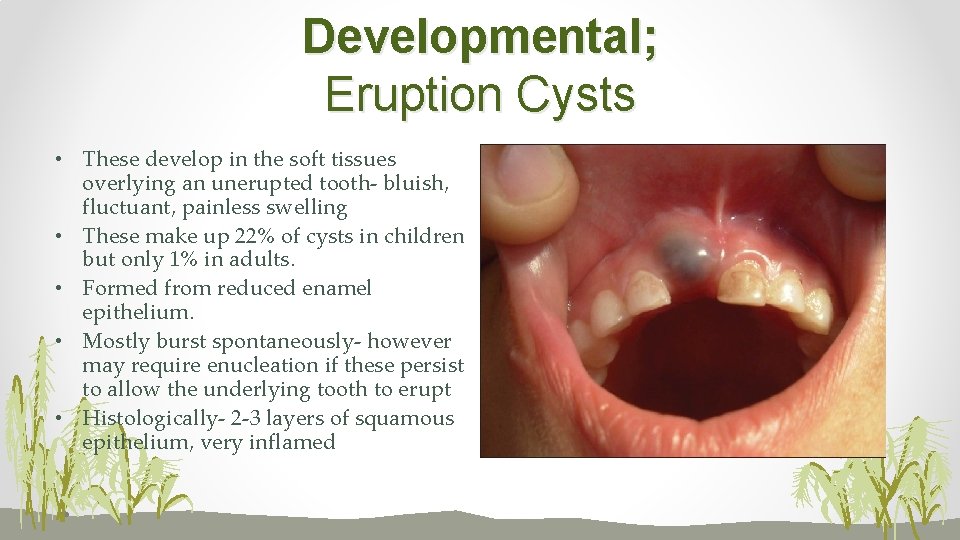
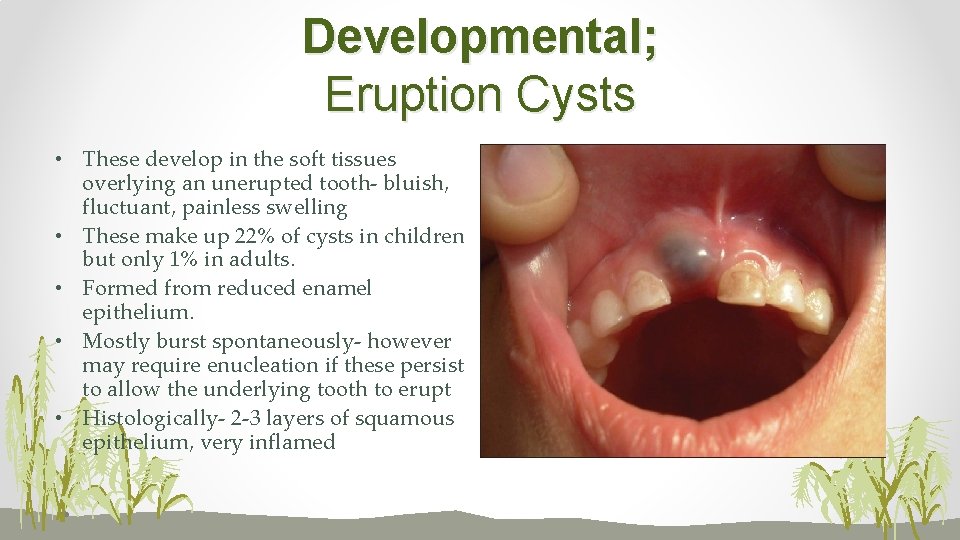
Developmental; Eruption Cysts • These develop in the soft tissues overlying an unerupted tooth- bluish, fluctuant, painless swelling • These make up 22% of cysts in children but only 1% in adults. • Formed from reduced enamel epithelium. • Mostly burst spontaneously- however may require enucleation if these persist to allow the underlying tooth to erupt • Histologically- 2 -3 layers of squamous epithelium, very inflamed
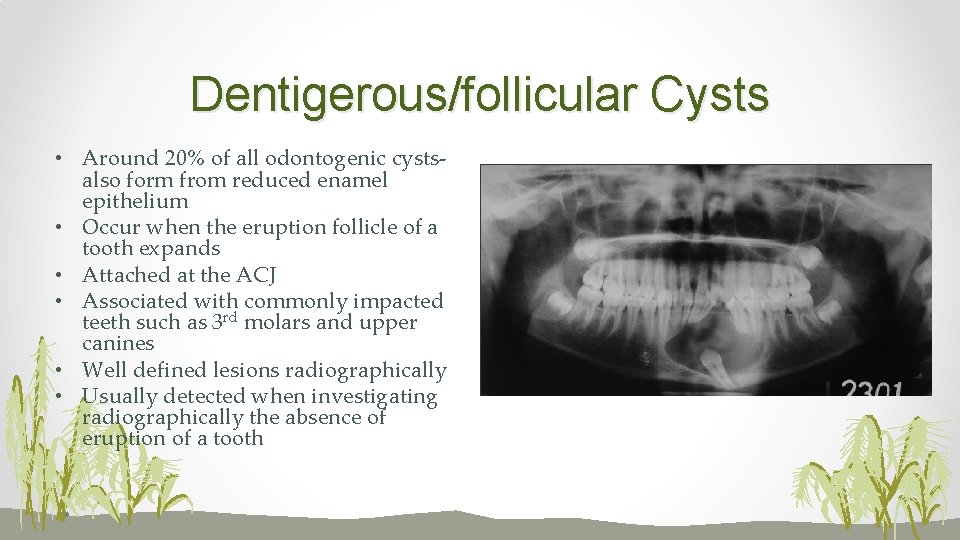
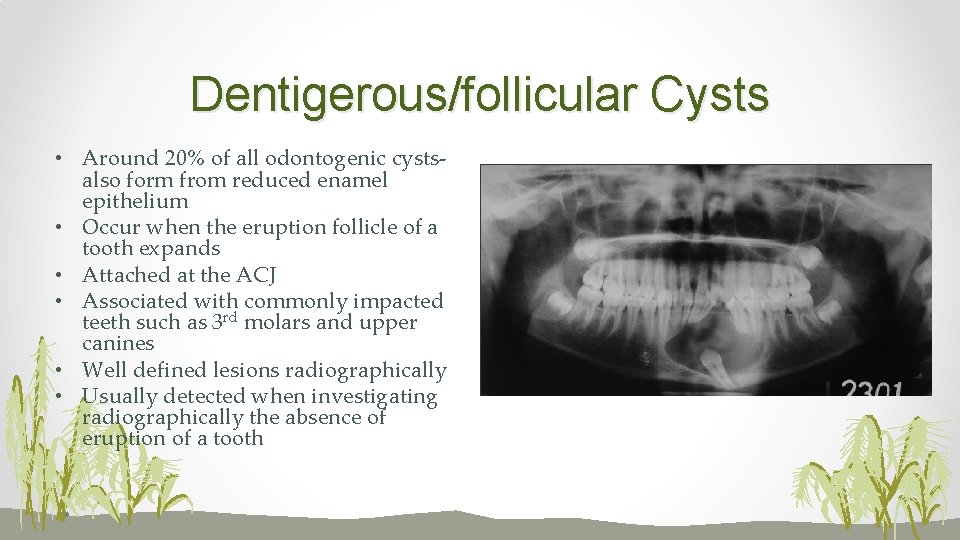
Dentigerous/follicular Cysts • Around 20% of all odontogenic cystsalso form from reduced enamel epithelium • Occur when the eruption follicle of a tooth expands • Attached at the ACJ • Associated with commonly impacted teeth such as 3 rd molars and upper canines • Well defined lesions radiographically • Usually detected when investigating radiographically the absence of eruption of a tooth
Dentigerous cysts contd. • Can cause resorption of roots of surrounding teeth • Treatment is usually by extraction of the affected tooth and enucleation of the cyst • However, if detected prior to the complete formation of the apex of the tooth the cyst can be marsupialised and the tooth allowed to erupt naturally • Histologically- non-keratinised stratified squamous, resembles the reduced enamel epithelium • Aspiration reveals a clear, protein-rich yellowish fluid
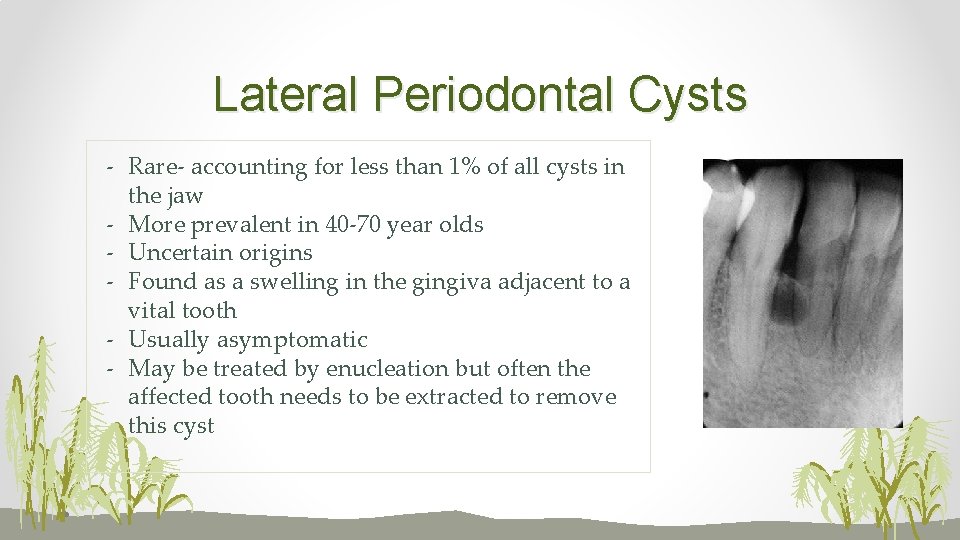
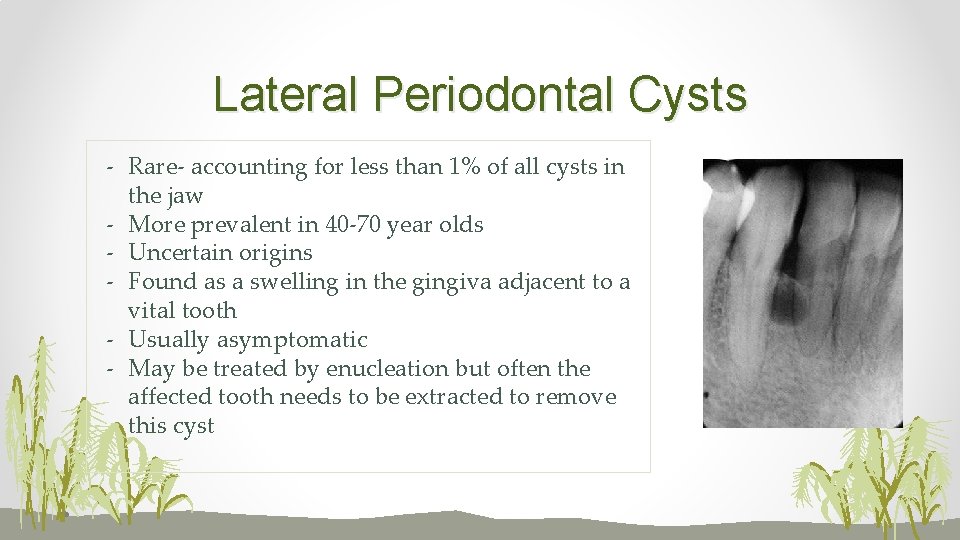
Lateral Periodontal Cysts - Rare- accounting for less than 1% of all cysts in the jaw - More prevalent in 40 -70 year olds - Uncertain origins - Found as a swelling in the gingiva adjacent to a vital tooth - Usually asymptomatic - May be treated by enucleation but often the affected tooth needs to be extracted to remove this cyst
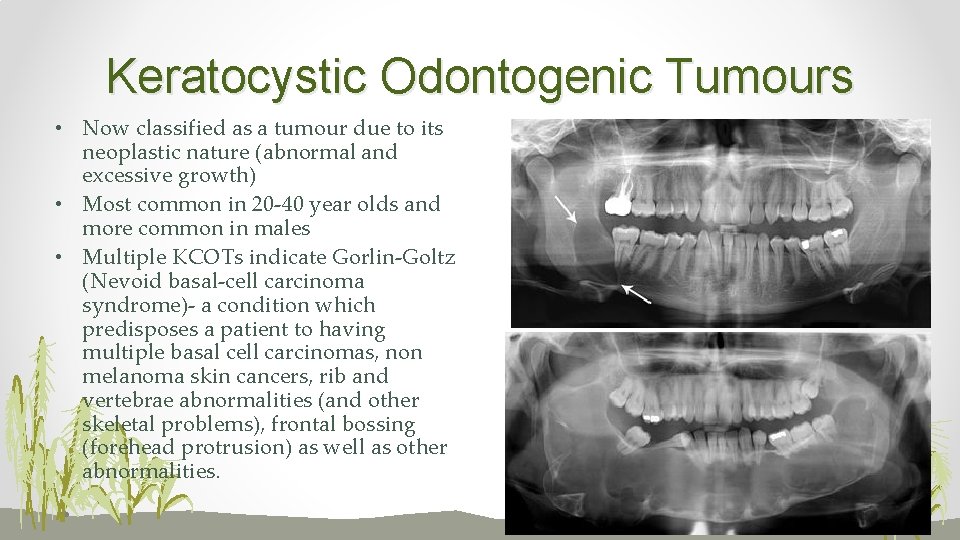
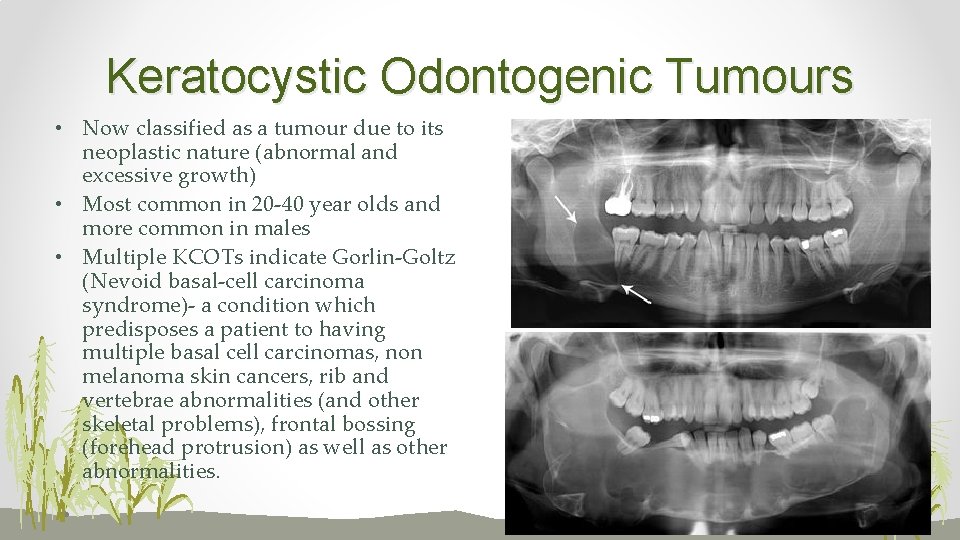
Keratocystic Odontogenic Tumours • Now classified as a tumour due to its neoplastic nature (abnormal and excessive growth) • Most common in 20 -40 year olds and more common in males • Multiple KCOTs indicate Gorlin-Goltz (Nevoid basal-cell carcinoma syndrome)- a condition which predisposes a patient to having multiple basal cell carcinomas, non melanoma skin cancers, rib and vertebrae abnormalities (and other skeletal problems), frontal bossing (forehead protrusion) as well as other abnormalities.
KCOTs contd. • Form from dental lamina and basal cells from overlying epithelium • Most (65 -83%) occur in the mandible and 50% occur at the angle of the mandible • Have been associated with a tumour suppressant gene • This cyst is destructive- causes resorption/ displacement of surrounding teeth and affects structures such as the ID nerve. The patient may present with paraesthesia • Well demarcated lesions, uni/multilocular
KCOTs • Often have satellite cysts so recurrence rates are high (50 -60%) as it is difficult to remove all remnants of cyst lining • May be treated by enucleation/ marsupialisation but more commonly now treated by jaw resection and reconstruction/grafting due to the high recurrence rates • Aspiration of a KCOT gives a creamy, thick, cheesy textured aspirate which is very useful in diagnosis • Histologically- keratinised stratified squamous epithelium, well defined basal layertakes up staining very readily (defining feature). Some KCOTs show evidence of dysplasia
Sources • Dental Update 2015; 42: 548– 555 • Dental Update 2014; 41: 182 -184