OCULAR TRAUMA Spring 14 Epidemiology 2 4 million




- Slides: 41
OCULAR TRAUMA Spring 14
Epidemiology • 2. 4 million eye injuries from: – Pellet and air guns – Motor vehicle crashes – Violence – Falls – Sports injuries – Animal bites – Foreign bodies – Strikes to the eye
• • Mechanisms of Injury and Biomechanics Chemical, thermal, and UV radiation Foreign bodies Types of injuries Usual Concurrent Injuries – Head – Face
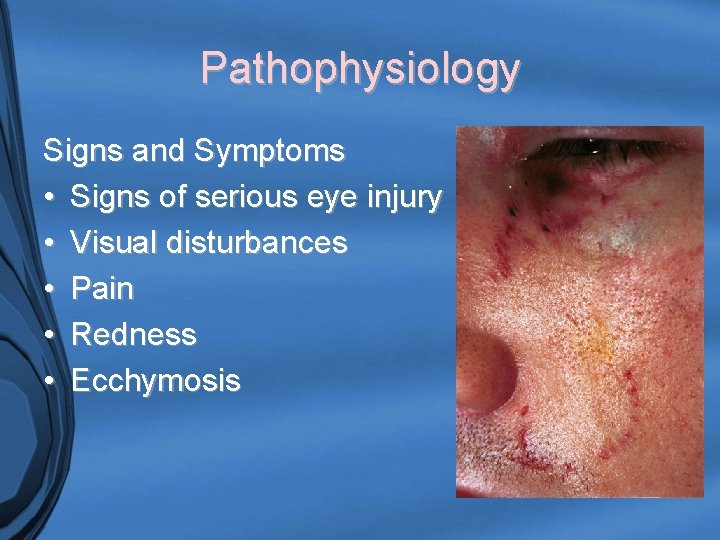
Pathophysiology Signs and Symptoms • Signs of serious eye injury • Visual disturbances • Pain • Redness • Ecchymosis
Nursing Care - Assessment History • Mechanism of injury? • Patient complaints? • History of eye problems? • Previous eye surgery? • Chronic conditions? • Glasses, contacts, or protective eye wear?
Nursing Care Physical Assessment Inspection • Inspect eye, tissues, and face • Observe for symmetry, edema, ecchymosis, ptosis, and lacerations • Inspect globe • Assess pupils • Assess for redness, tearing, and blinking
Nursing Care Physical Assessment Inspection (continued) • Foreign bodies • Impaled objects • Assess extraocular movements (unless globe injury) • Assess gaze defects • Assess for blurred or double vision • Perform visual acuity test
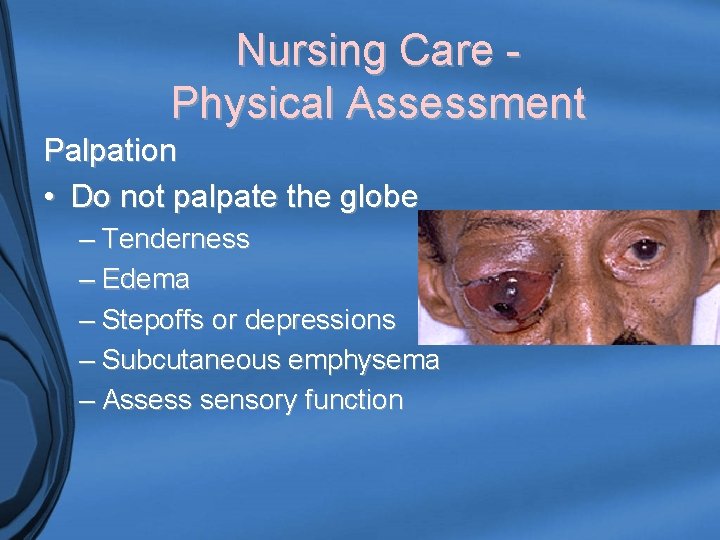
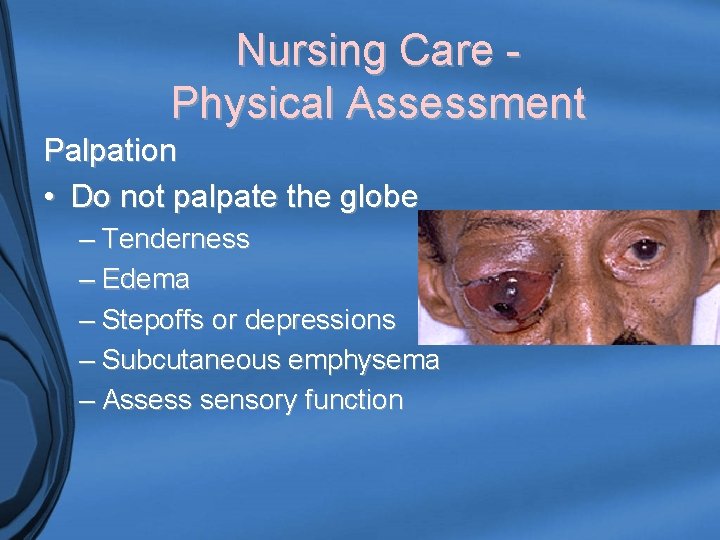
Nursing Care Physical Assessment Palpation • Do not palpate the globe – Tenderness – Edema – Stepoffs or depressions – Subcutaneous emphysema – Assess sensory function
Diagnostic Procedures • Radiographic Studies – Eye radiographs – Computerized tomography scan – Magnetic Resonance Imaging • Other – Fluorescein staining – Slit lamp exam – Tonometry

Nursing Diagnoses • Altered visual (sensory/perception) • Pain • Infection risk • Injury risk • Fear • Altered health maintenance risk
Planning and Implementation • • • Assess visual acuity test Elevate the head of the bed Instruct the patient not to bend or cough Assist with removal of foreign bodies Stabilize impaled objects Apply cool packs
Planning and Implementation • • • Use a new bottle of medication Instill topical anesthetic drops for pain Instill normal saline drops or artificial tears for moisture • Drops for ciliary spasm or dilation • Topical NSAIDS can also be used
Planning and Implementation • • • Topical steroids (ophthalmologist orders) Topical antibiotics Systemic antibiotics used for penetrating eye trauma (preoperatively) • Tetanus prophylaxis
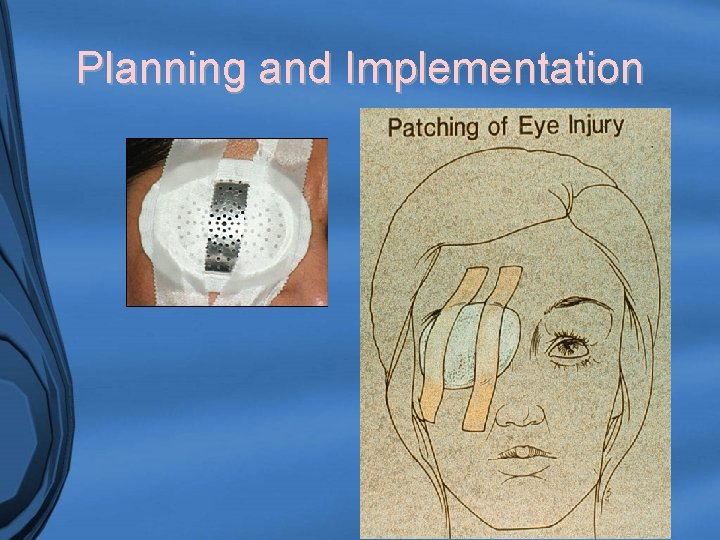
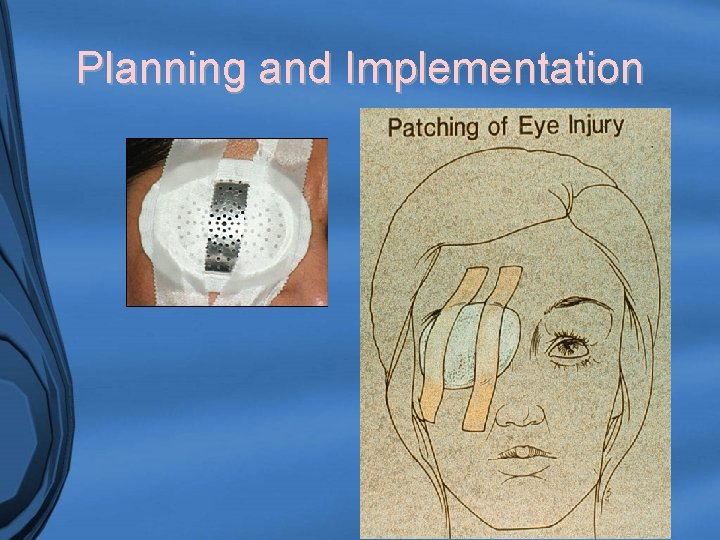
Planning and Implementation
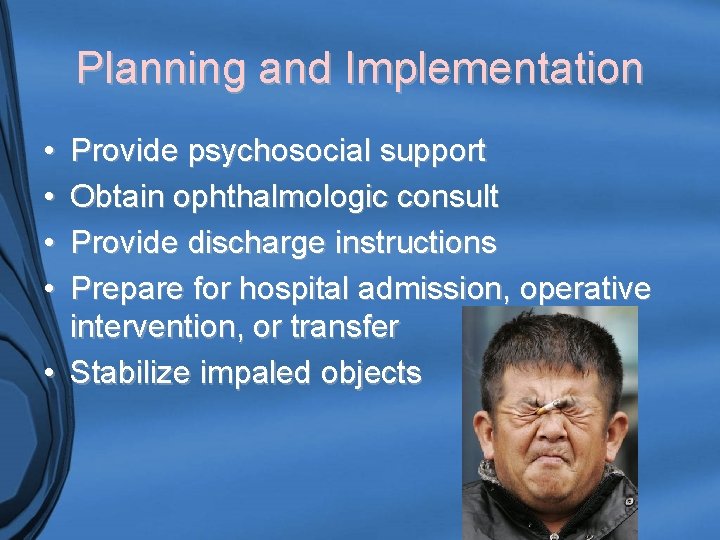
Planning and Implementation • • Provide psychosocial support Obtain ophthalmologic consult Provide discharge instructions Prepare for hospital admission, operative intervention, or transfer • Stabilize impaled objects
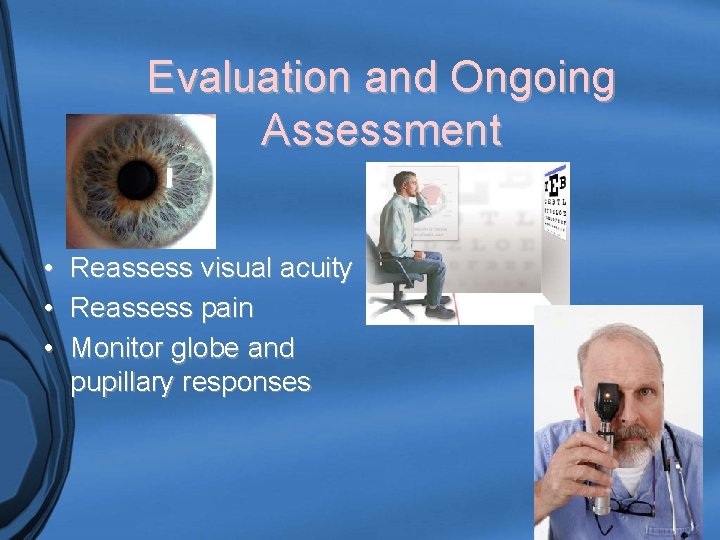
Evaluation and Ongoing Assessment • Reassess visual acuity • Reassess pain • Monitor globe and pupillary responses
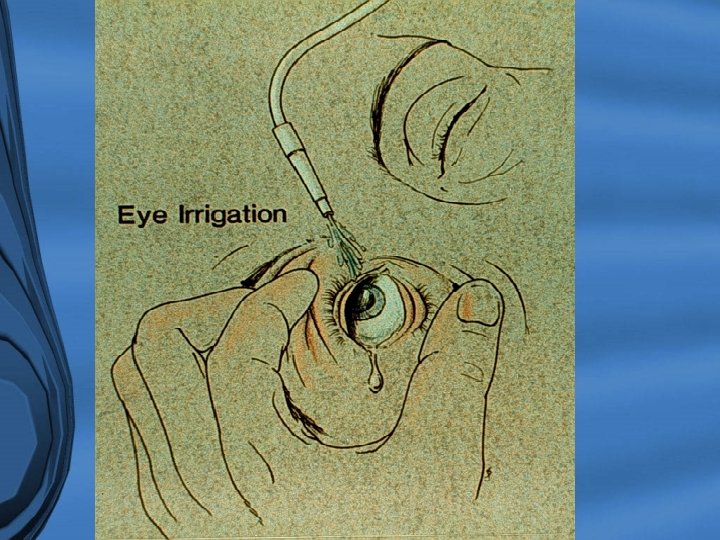

Morgan Lens

Selected Eye Emergencies
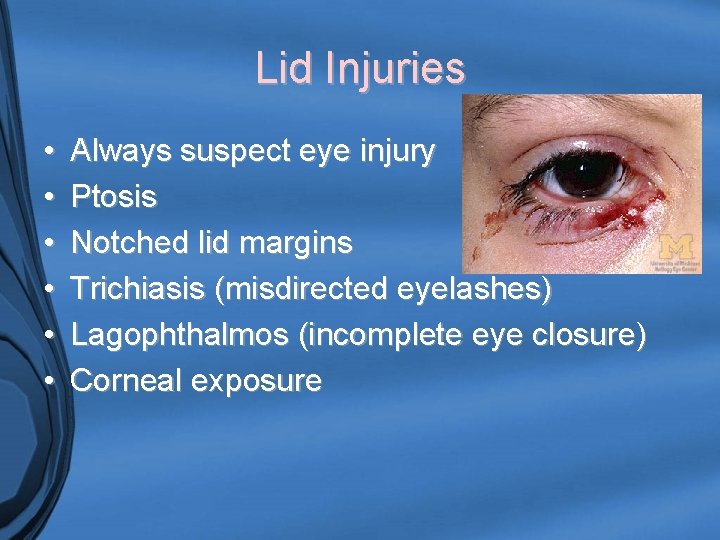
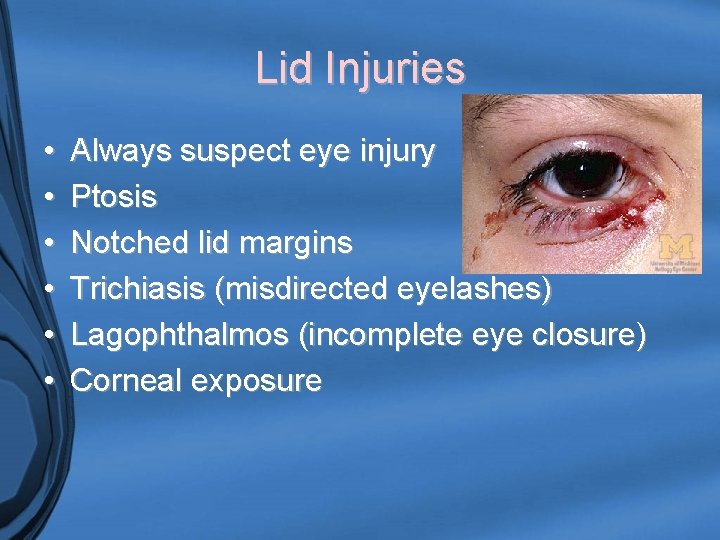
Lid Injuries • • • Always suspect eye injury Ptosis Notched lid margins Trichiasis (misdirected eyelashes) Lagophthalmos (incomplete eye closure) Corneal exposure
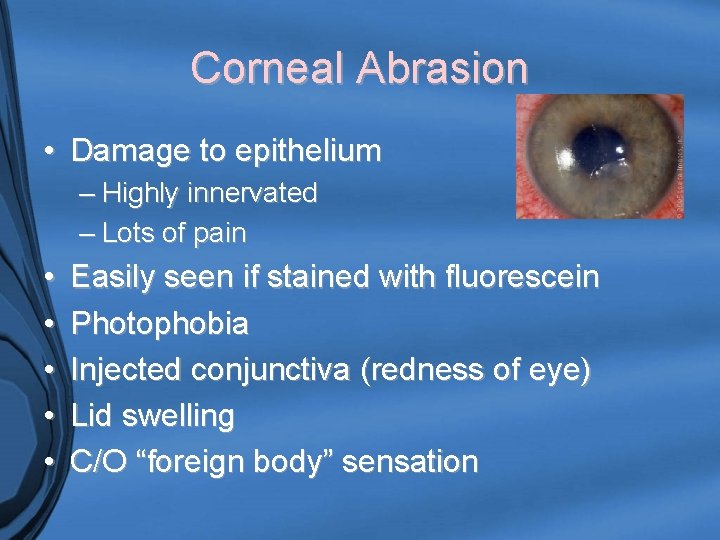
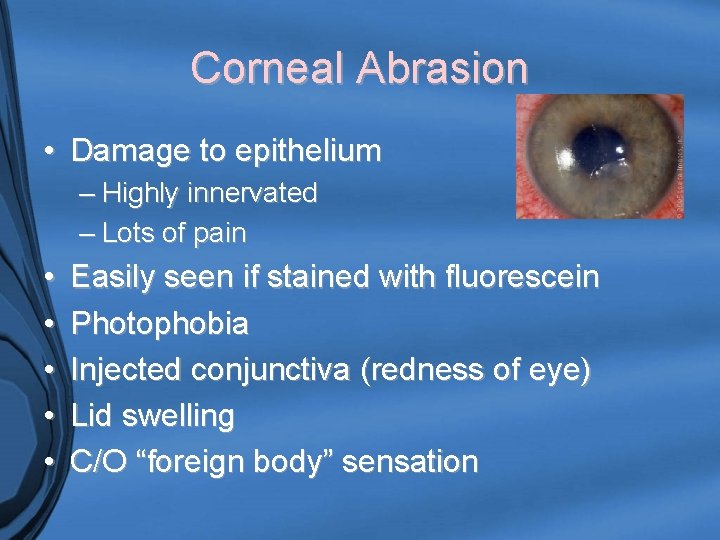
Corneal Abrasion • Damage to epithelium – Highly innervated – Lots of pain • • • Easily seen if stained with fluorescein Photophobia Injected conjunctiva (redness of eye) Lid swelling C/O “foreign body” sensation
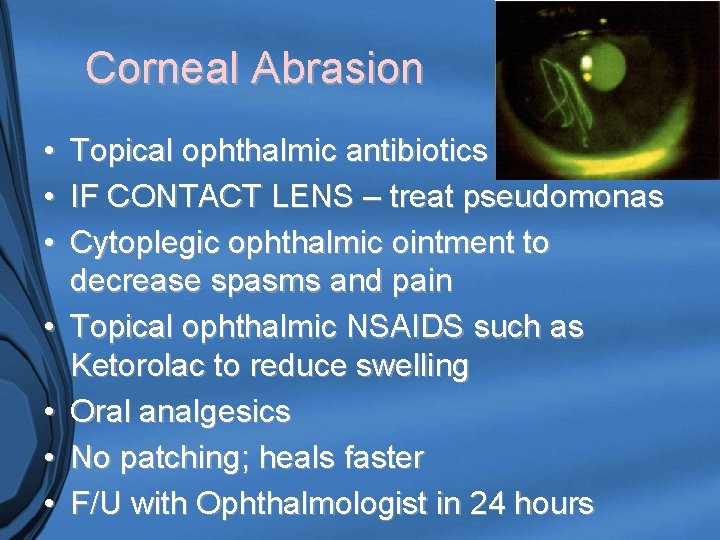
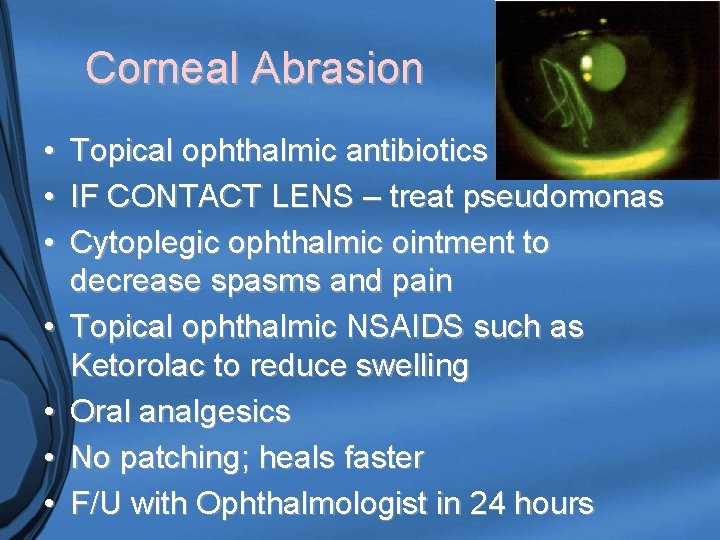
Corneal Abrasion • • Topical ophthalmic antibiotics IF CONTACT LENS – treat pseudomonas Cytoplegic ophthalmic ointment to decrease spasms and pain Topical ophthalmic NSAIDS such as Ketorolac to reduce swelling Oral analgesics No patching; heals faster F/U with Ophthalmologist in 24 hours
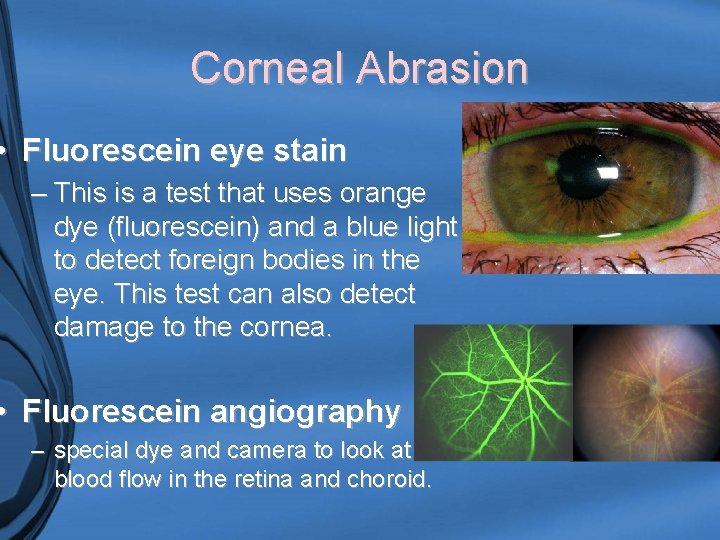
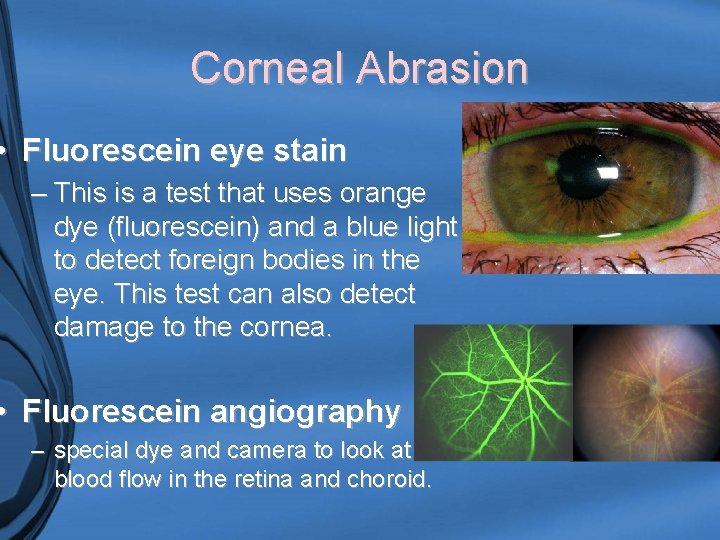
Corneal Abrasion • Fluorescein eye stain – This is a test that uses orange dye (fluorescein) and a blue light to detect foreign bodies in the eye. This test can also detect damage to the cornea. • Fluorescein angiography – special dye and camera to look at blood flow in the retina and choroid.
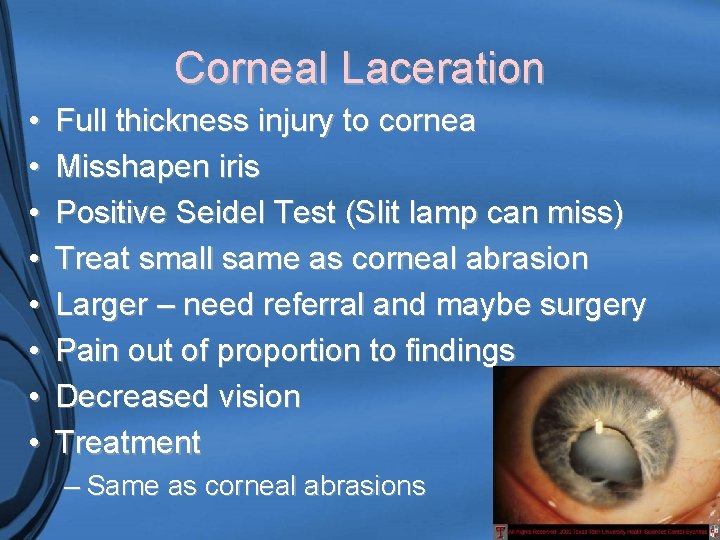
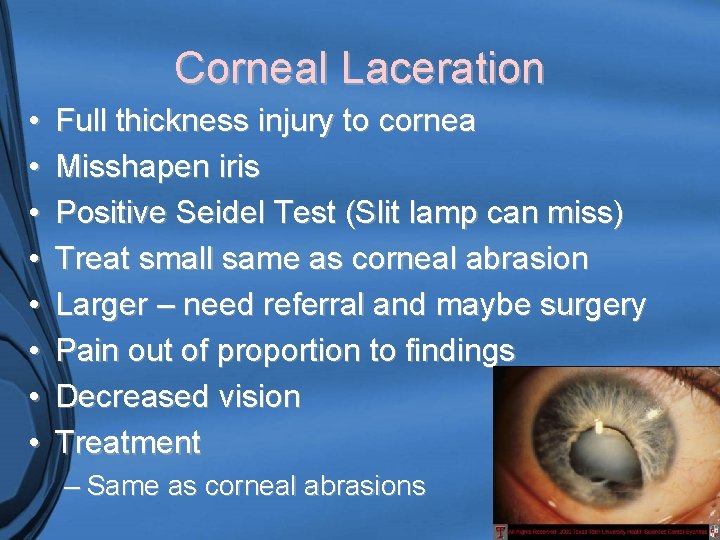
Corneal Laceration • • Full thickness injury to cornea Misshapen iris Positive Seidel Test (Slit lamp can miss) Treat small same as corneal abrasion Larger – need referral and maybe surgery Pain out of proportion to findings Decreased vision Treatment – Same as corneal abrasions

Corneal Foreign body • Potential of a high-speed penetration • Metal, plastic, wood – Photophobia – Tearing – Pain – Injected conjuctiva – Lid swelling • Treatment: topical anesthetic, removal of foreign body, discharged with topical opthalmic antibiotics, cytoplegics, oral analgesics
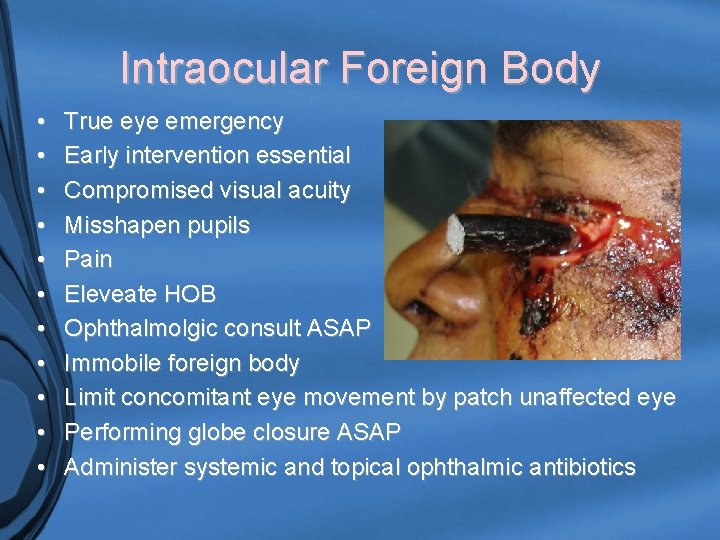
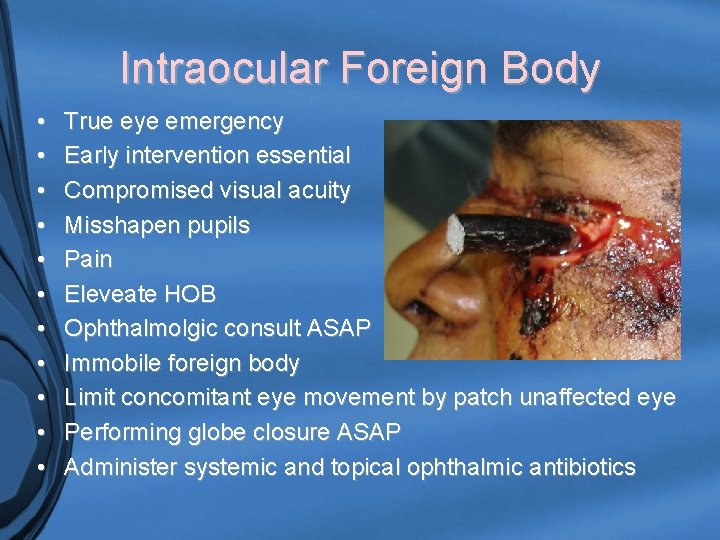
Intraocular Foreign Body • • • True eye emergency Early intervention essential Compromised visual acuity Misshapen pupils Pain Eleveate HOB Ophthalmolgic consult ASAP Immobile foreign body Limit concomitant eye movement by patch unaffected eye Performing globe closure ASAP Administer systemic and topical ophthalmic antibiotics
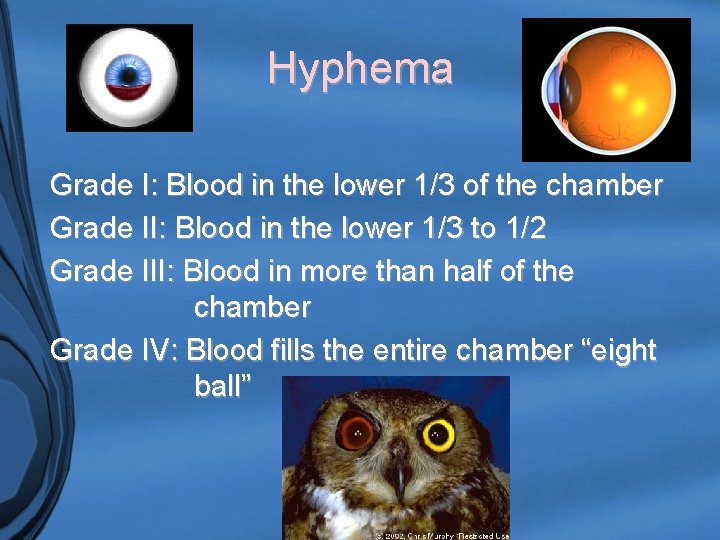
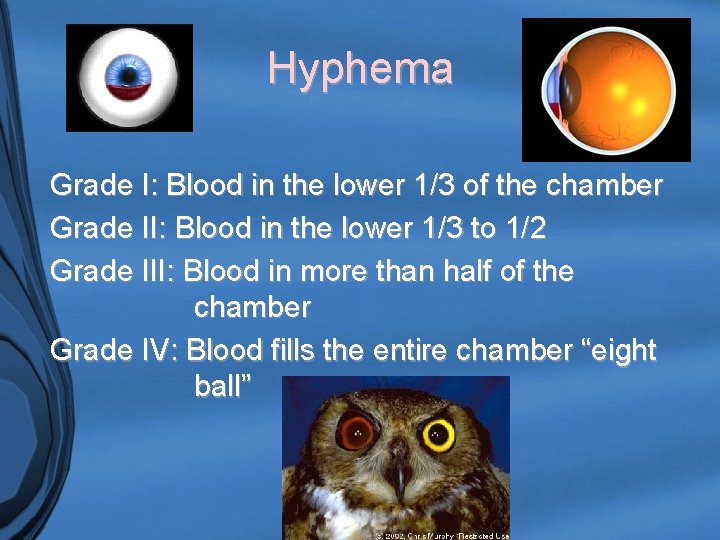
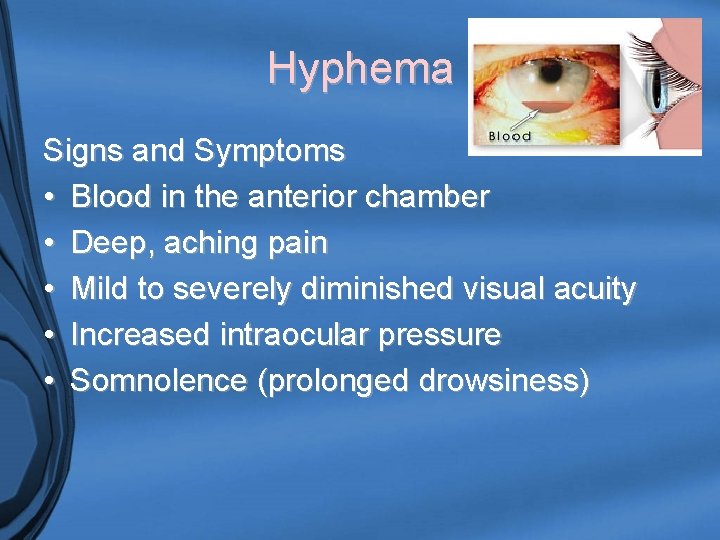
Hyphema Grade I: Blood in the lower 1/3 of the chamber Grade II: Blood in the lower 1/3 to 1/2 Grade III: Blood in more than half of the chamber Grade IV: Blood fills the entire chamber “eight ball”
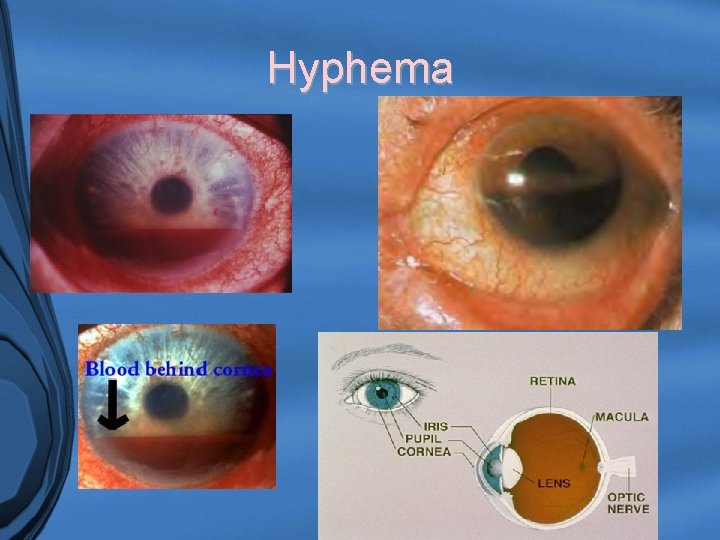
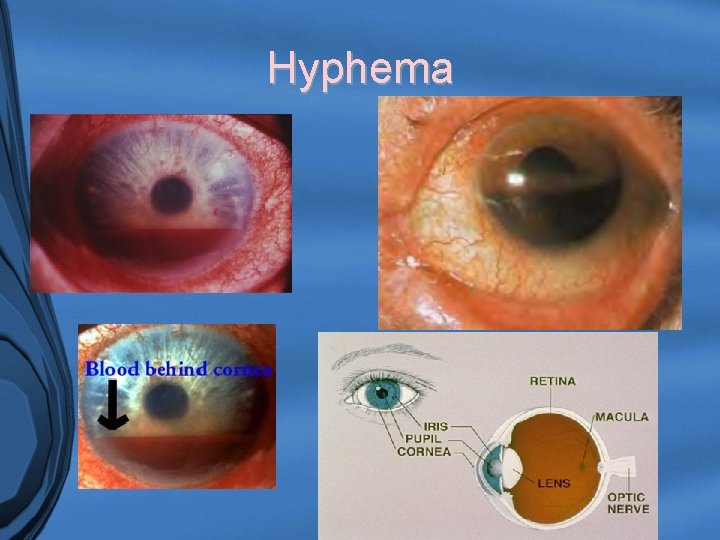
Hyphema
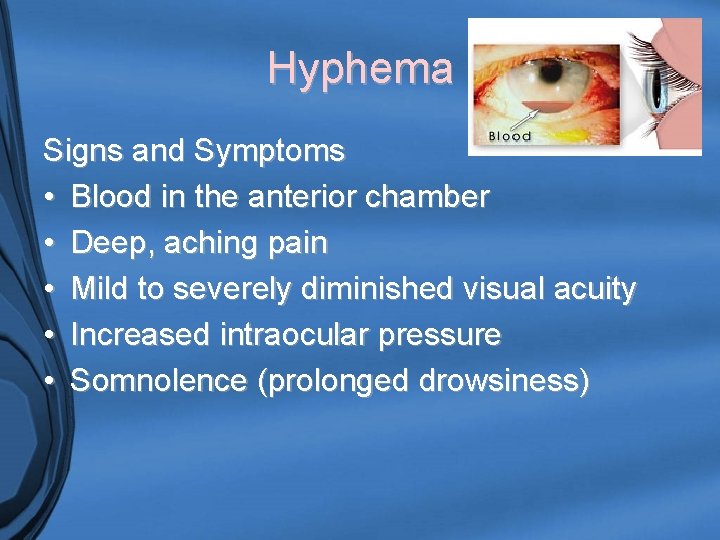
Hyphema Signs and Symptoms • Blood in the anterior chamber • Deep, aching pain • Mild to severely diminished visual acuity • Increased intraocular pressure • Somnolence (prolonged drowsiness)
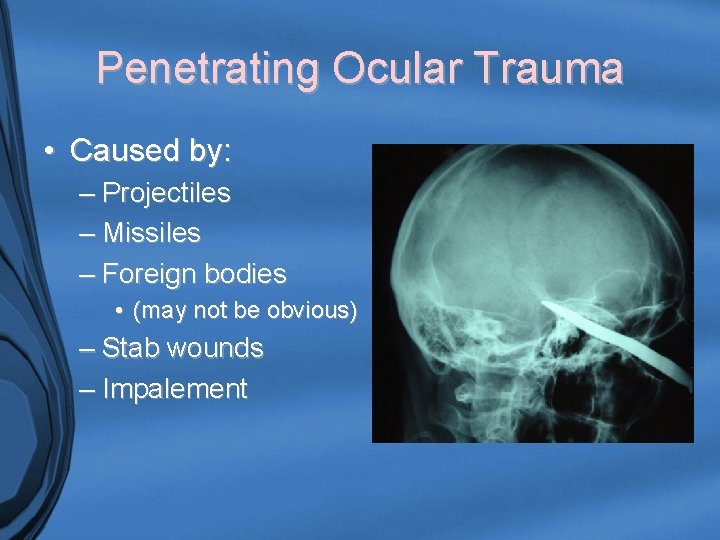
Penetrating Ocular Trauma • Caused by: – Projectiles – Missiles – Foreign bodies • (may not be obvious) – Stab wounds – Impalement
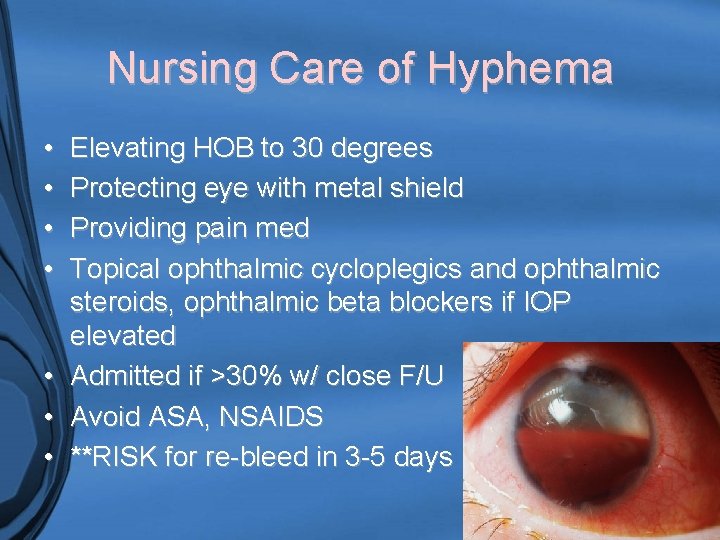
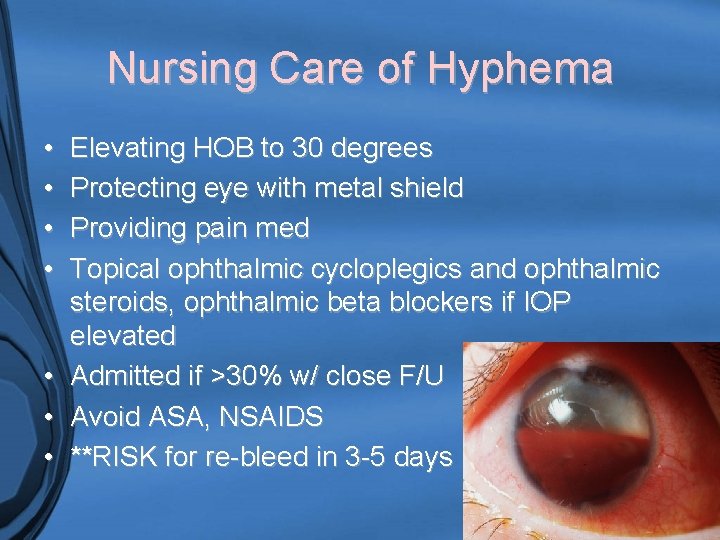
Nursing Care of Hyphema • • Elevating HOB to 30 degrees Protecting eye with metal shield Providing pain med Topical ophthalmic cycloplegics and ophthalmic steroids, ophthalmic beta blockers if IOP elevated • Admitted if >30% w/ close F/U • Avoid ASA, NSAIDS • **RISK for re-bleed in 3 -5 days
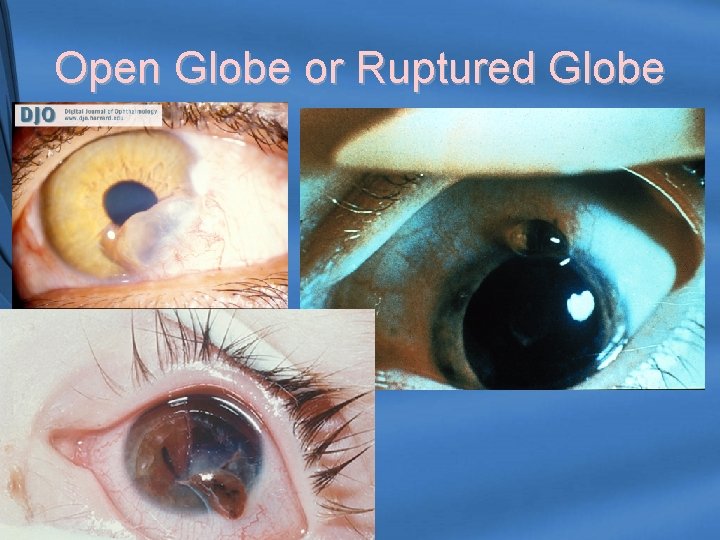
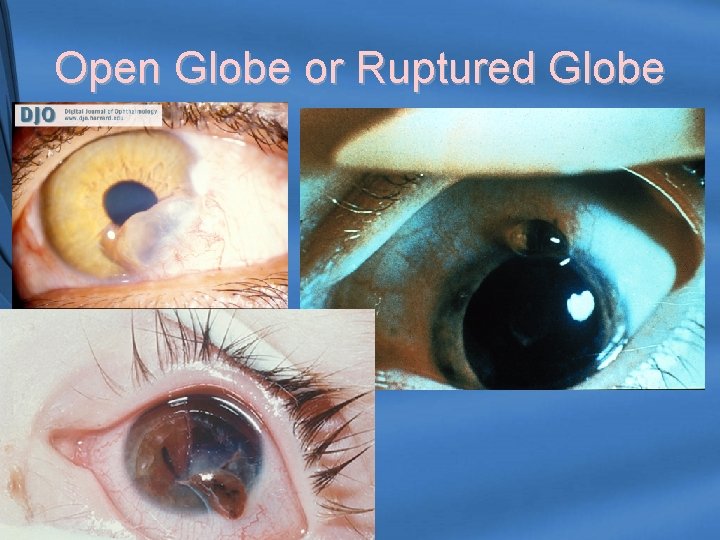
Open Globe or Ruptured Globe
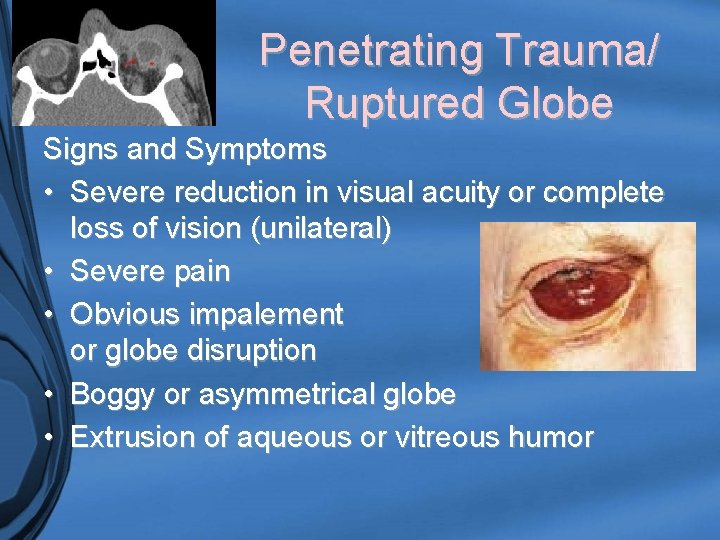
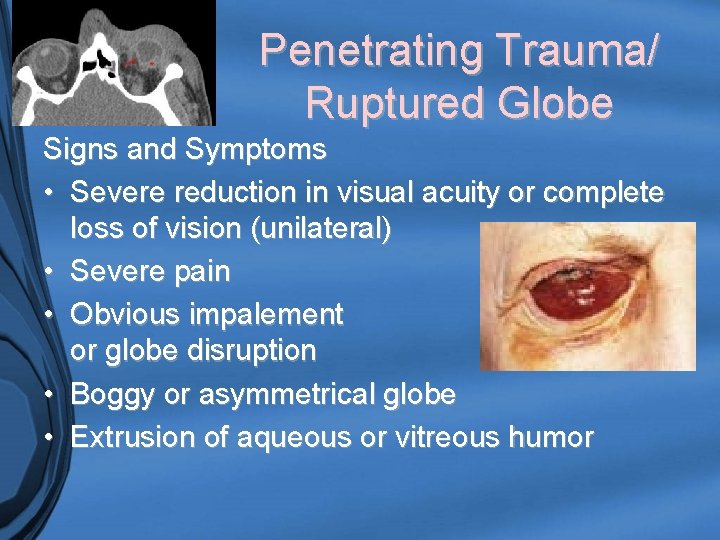
Penetrating Trauma/ Ruptured Globe Signs and Symptoms • Severe reduction in visual acuity or complete loss of vision (unilateral) • Severe pain • Obvious impalement or globe disruption • Boggy or asymmetrical globe • Extrusion of aqueous or vitreous humor
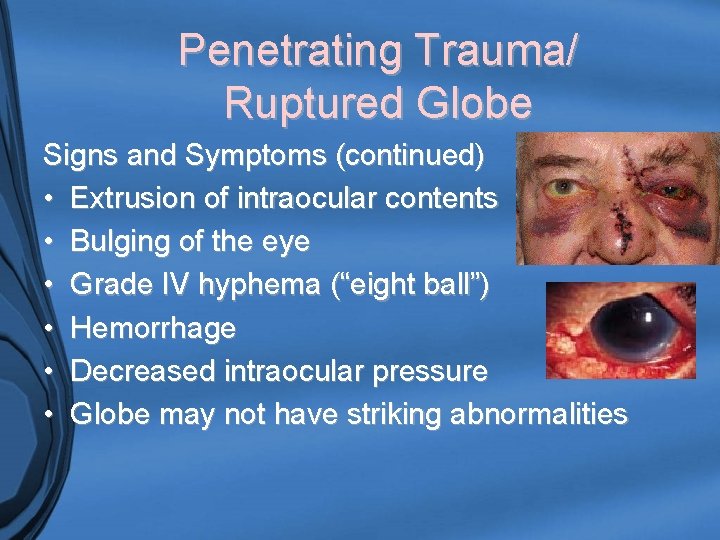
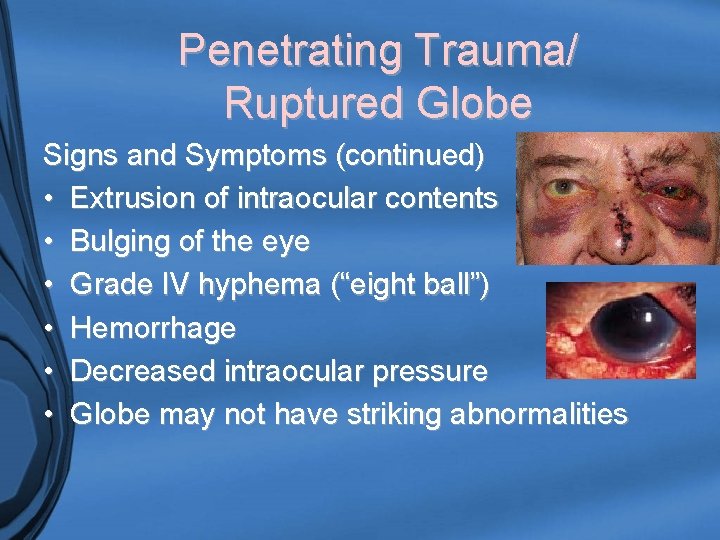
Penetrating Trauma/ Ruptured Globe Signs and Symptoms (continued) • Extrusion of intraocular contents • Bulging of the eye • Grade IV hyphema (“eight ball”) • Hemorrhage • Decreased intraocular pressure • Globe may not have striking abnormalities
Penetrating Trauma/ Ruptured Globe • Treatment – Avoidance of any type of pressure on the globe – do NOT perform TONOMETRY!! – Apply rigid shield – Administer antiemetics to decrease risk of vomiting (increasing IOP) – Avoid ophthalmic drops or meds – Consult with OPHTHALMOLOGY
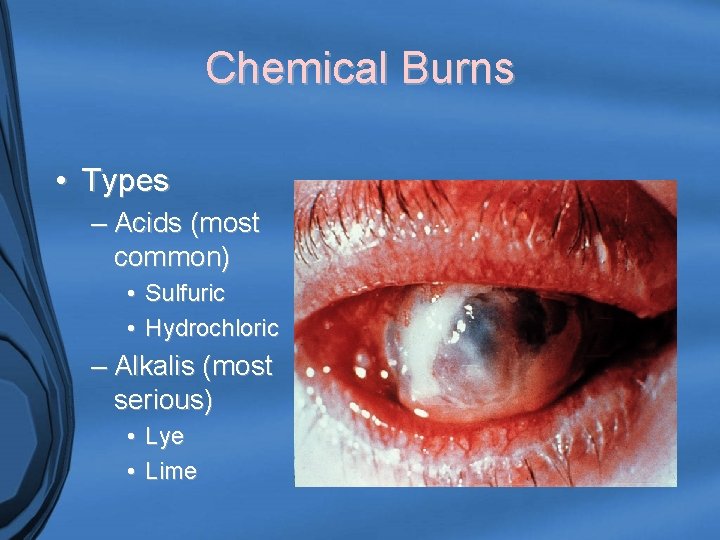
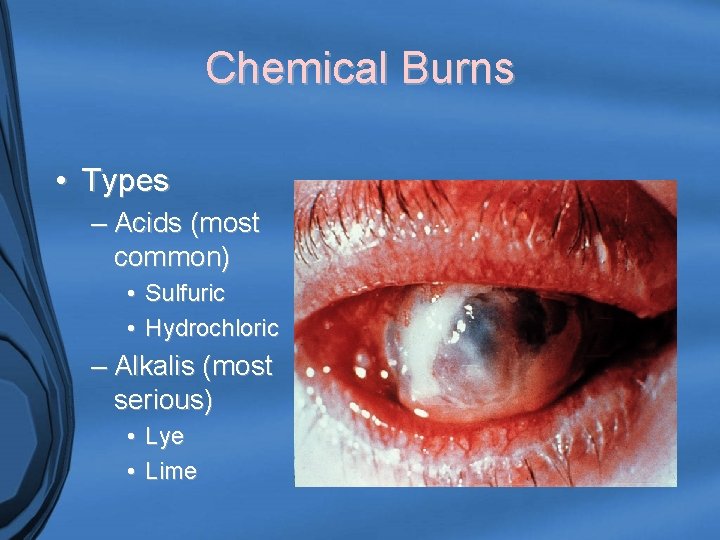
Chemical Burns • Types – Acids (most common) • Sulfuric • Hydrochloric – Alkalis (most serious) • Lye • Lime
Chemical Burns • Prognosis depends on: – Agent – Concentration – Length of exposure – Adequacy of decontamination – Degree of corneal involvement – Presence of ischemia
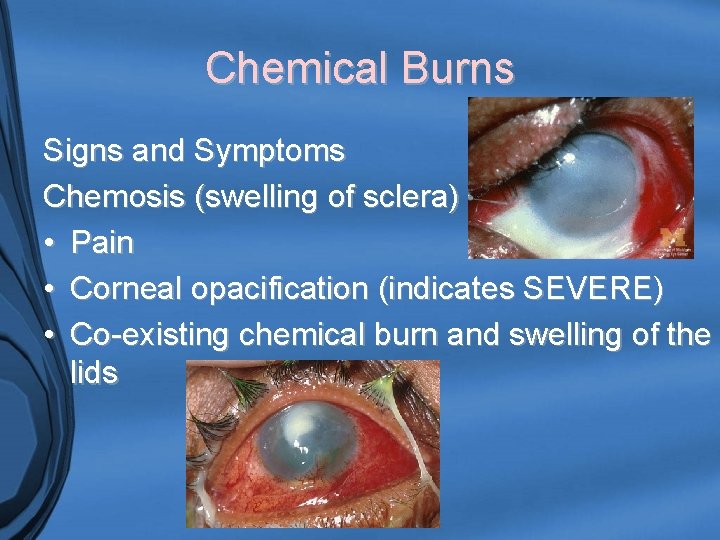
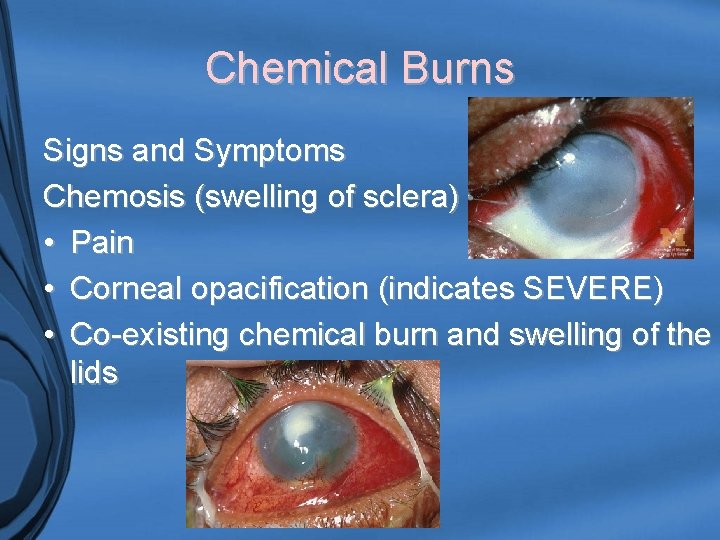
Chemical Burns Signs and Symptoms Chemosis (swelling of sclera) • Pain • Corneal opacification (indicates SEVERE) • Co-existing chemical burn and swelling of the lids
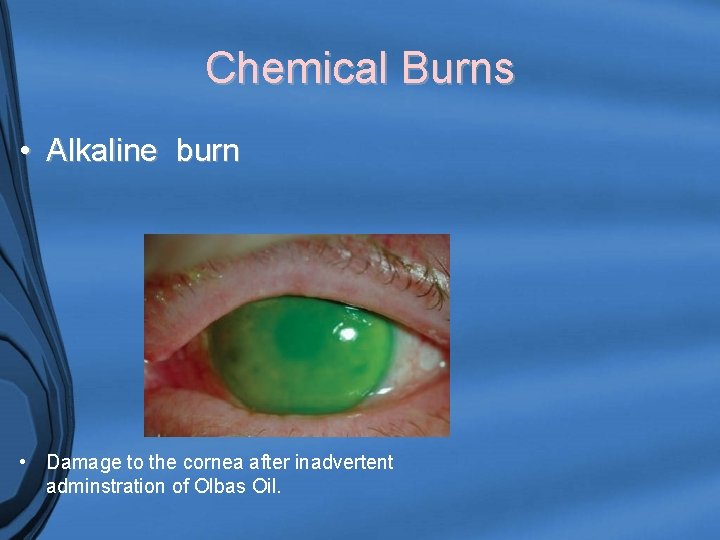
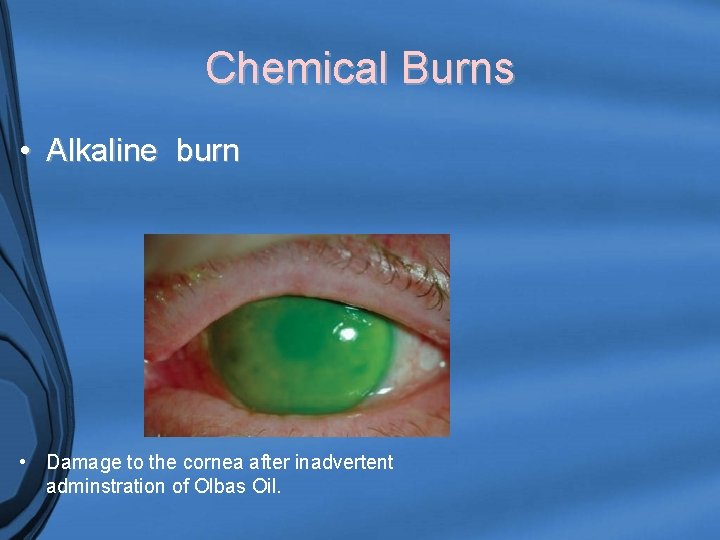
Chemical Burns • Alkaline burn • Damage to the cornea after inadvertent adminstration of Olbas Oil.
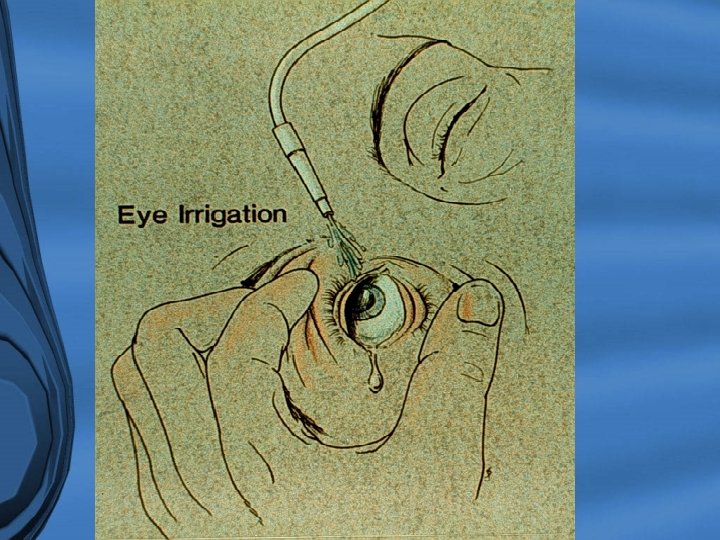
Treatment of Burns • Irrigate, irrigate until p. H returns to normal range • NORMAL RANGE IS 7. 0 -7. 3 • Administer topical ophthalmic antibiotics and cytoplegics • Administer tetracaine drops for pain • Visual Acuity test as assessment guide
The End