Oct 2018 The Surprise Question and Five Wishes



- Slides: 27
Oct, 2018 The Surprise Question and Five Wishes: Update October 2018 Laurie Jackson Masters of Divinity Masters Certificate in Clinical Ethics SENIOR DIRECTOR Virginia Mason Memorial’s Care Line for Advancing Illness Home Health & Hospice | Palliative Care | Bereavement | Ethics Advance Care Planning | Spiritual Care

THE SURPRISE QUESTION What’s Our Goal? BEST CARE POSSIBLE What hinders us? § Uncertain What “Best Care” Looks Like § Cure Versus Care, “Treatment” § Assumptions § Time § Uncomfortable conversations § Rarely is it bad intent
THE SURPRISE QUESTION IN YAKIMA 2015: Dr. Mimi Pattison in Yakima at Circle of Life Symposium 2016 10 -month adventure to add to hospital electronic admission set § Created Inpatient Navigation Team § Leader/Administration Buy-In § Physician Education § In Midst of Virginia Mason/Memorial Affiliation 2017: Haiti Road to New Jersey Road § Clinical Trial Began § Physician Education/Behavior Modification § New Angle to Education: Teamwork 2018: Beginning Work in Clinics
THE SURPRISE QUESTION December 21, 2016: Surprise Question Initiated First Hospital to Standardize Every Patient Admission Every Floor Every Physician Electronically Asked and Answered
THE SURPRISE QUESTION How It Works Physician Responds to Admission Queries Diagnosis, Code Status, etc. Then, HARD STOP: Would you be surprised if this patient died in the next six months?
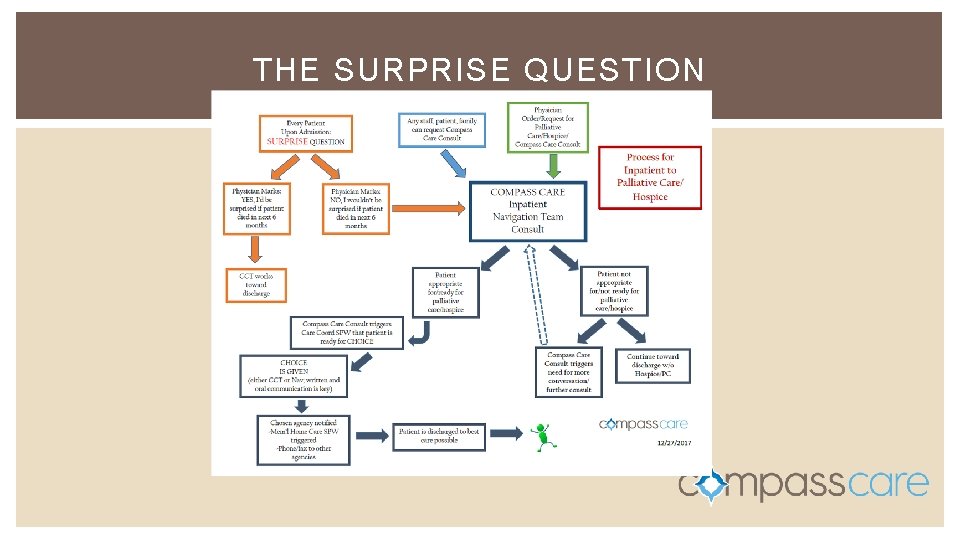
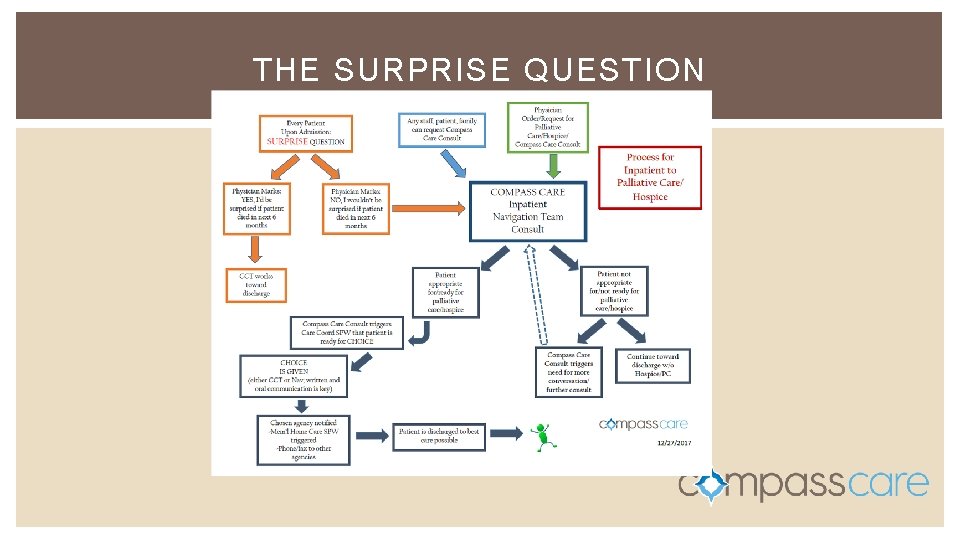
THE SURPRISE QUESTION
THE SURPRISE QUESTION How It Works Would you be surprised if this patient died in the next six months? If Physician Replies YES: Physician Able to Continue with Admission If Physician Replies NO: Electronic Order Sent to Navigation Team for Consult Physician asked if Palliative Care or Hospice has been ordered Physician Then Able to Continue with Admission
THE SURPRISE QUESTION First Physician That Answered NO Orthopedic Surgeon Who Replaced a Knee § Did we do the education incorrectly? What We Learned From This
THE SURPRISE QUESTION What We Learned in First Months 2/3 of physicians always answered YES Lessons Learned: (come to presentation) Time to Bust Some Myths
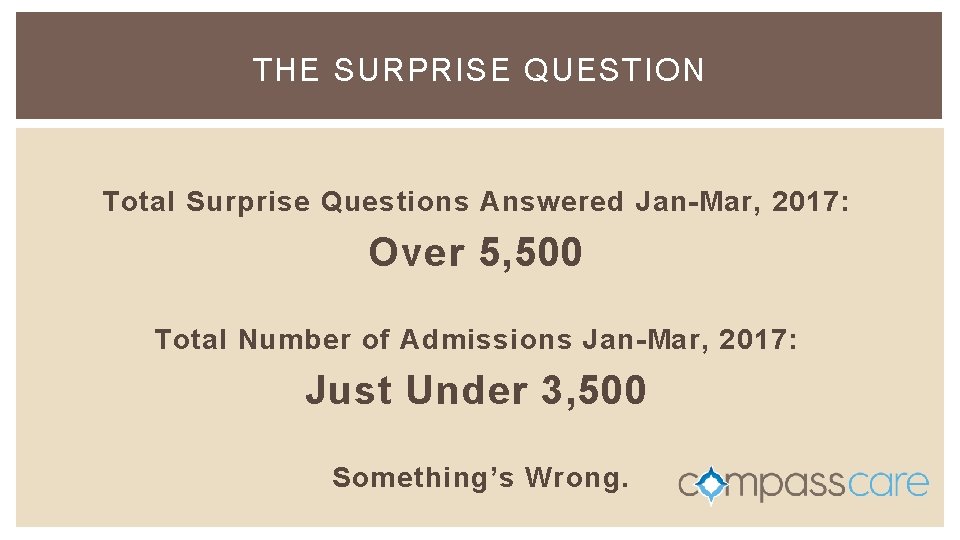
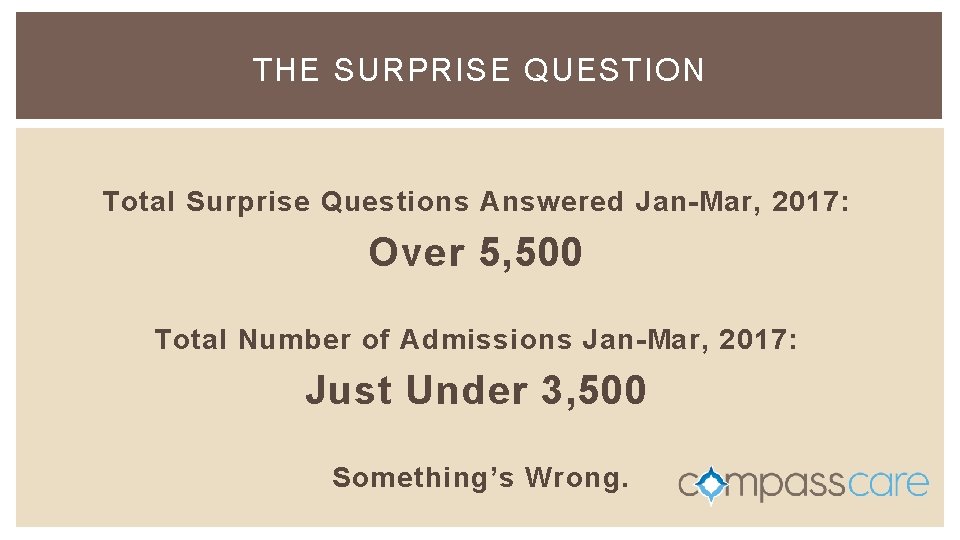
THE SURPRISE QUESTION Total Surprise Questions Answered Jan-Mar, 2017: Over 5, 500 Total Number of Admissions Jan-Mar, 2017: Just Under 3, 500 Something’s Wrong.
THE SURPRISE QUESTION Turns Out…Another lesson learned (you’ll have to attend the seminar to learn the lesson)
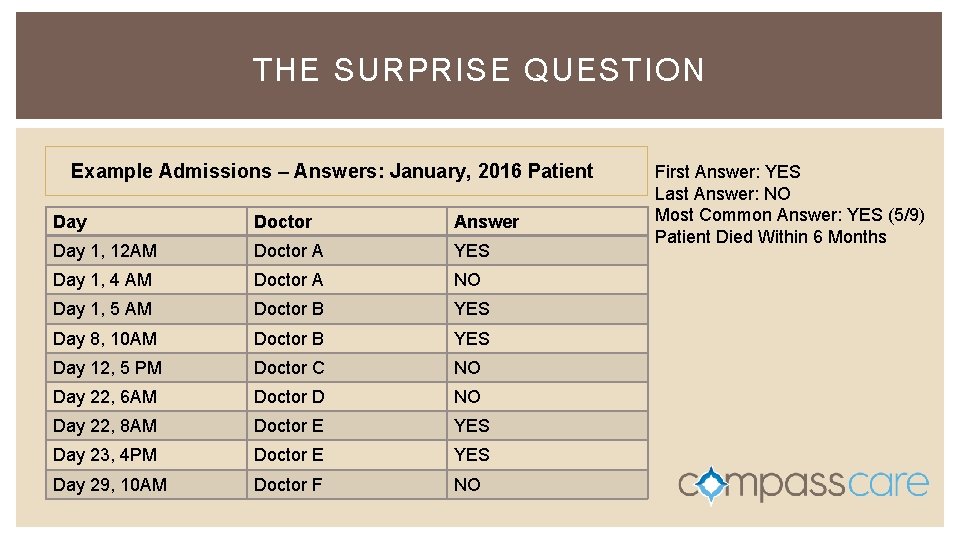
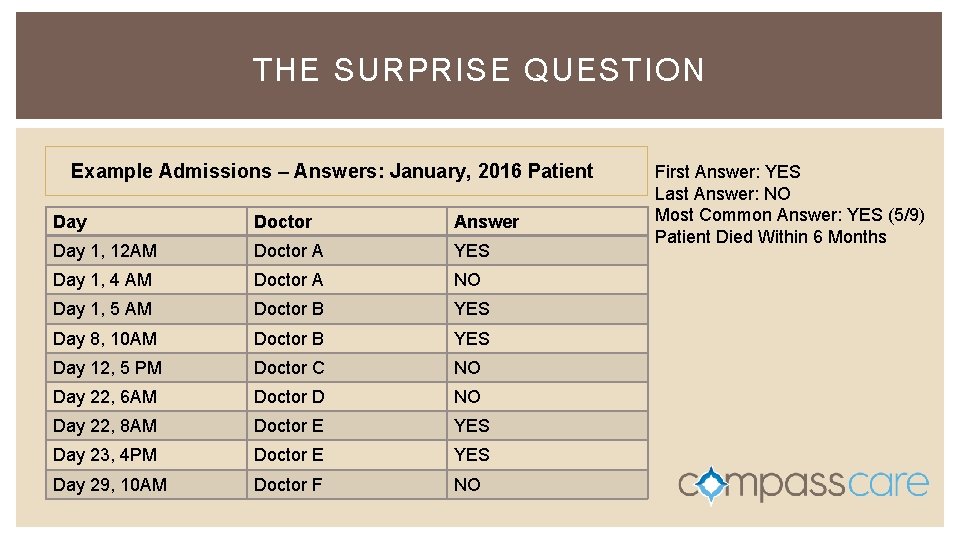
THE SURPRISE QUESTION Example Admissions – Answers: January, 2016 Patient Day Doctor Answer Day 1, 12 AM Doctor A YES Day 1, 4 AM Doctor A NO Day 1, 5 AM Doctor B YES Day 8, 10 AM Doctor B YES Day 12, 5 PM Doctor C NO Day 22, 6 AM Doctor D NO Day 22, 8 AM Doctor E YES Day 23, 4 PM Doctor E YES Day 29, 10 AM Doctor F NO First Answer: YES Last Answer: NO Most Common Answer: YES (5/9) Patient Died Within 6 Months
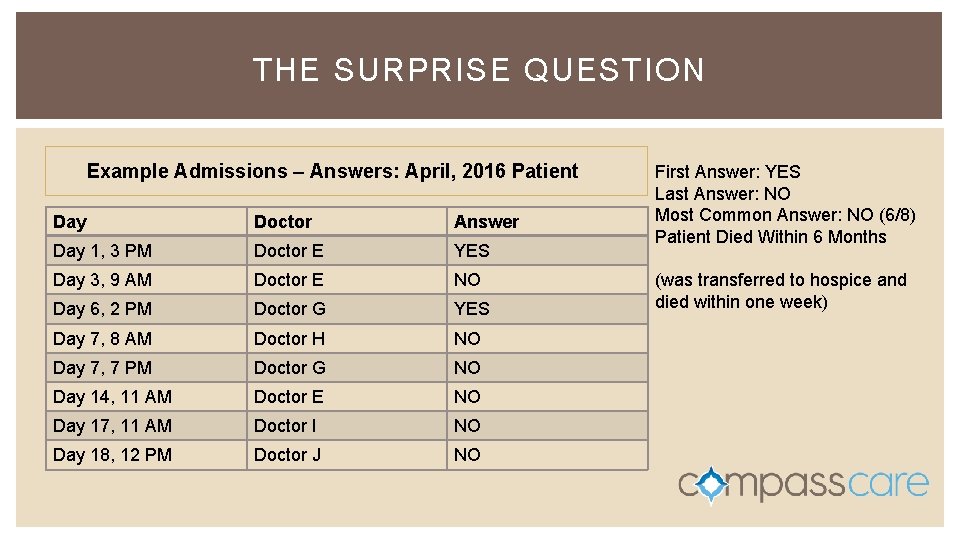
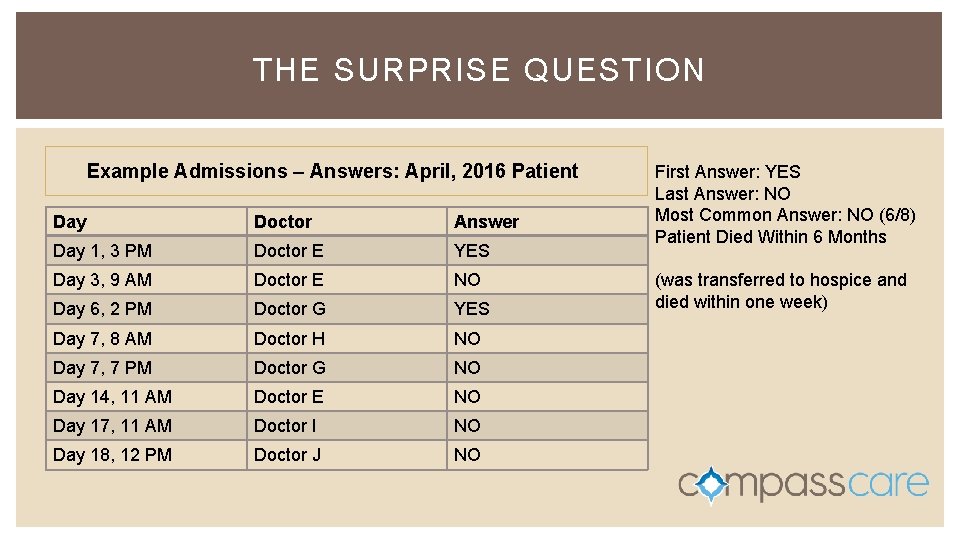
THE SURPRISE QUESTION Example Admissions – Answers: April, 2016 Patient Day Doctor Answer Day 1, 3 PM Doctor E YES Day 3, 9 AM Doctor E NO Day 6, 2 PM Doctor G YES Day 7, 8 AM Doctor H NO Day 7, 7 PM Doctor G NO Day 14, 11 AM Doctor E NO Day 17, 11 AM Doctor I NO Day 18, 12 PM Doctor J NO First Answer: YES Last Answer: NO Most Common Answer: NO (6/8) Patient Died Within 6 Months (was transferred to hospice and died within one week)
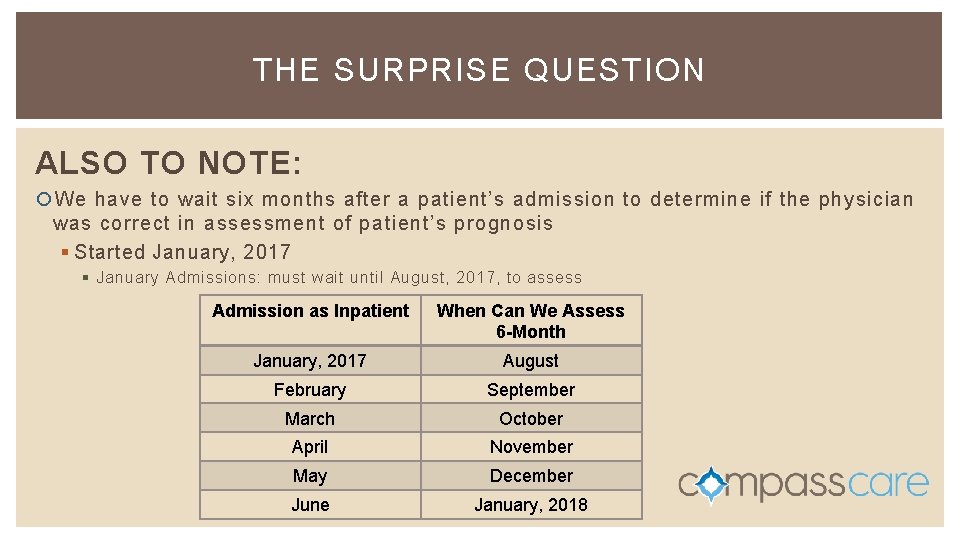
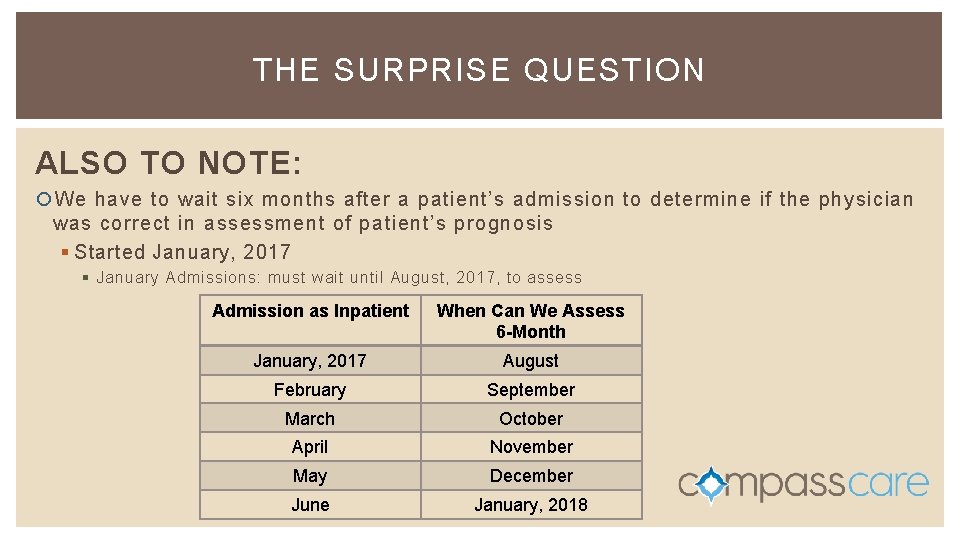
THE SURPRISE QUESTION ALSO TO NOTE: We have to wait six months after a patient’s admission to determine if the physician was correct in assessment of patient’s prognosis § Started January, 2017 § January Admissions: must wait until August, 2017, to assess Admission as Inpatient When Can We Assess 6 -Month January, 2017 August February September March October April November May December June January, 2018
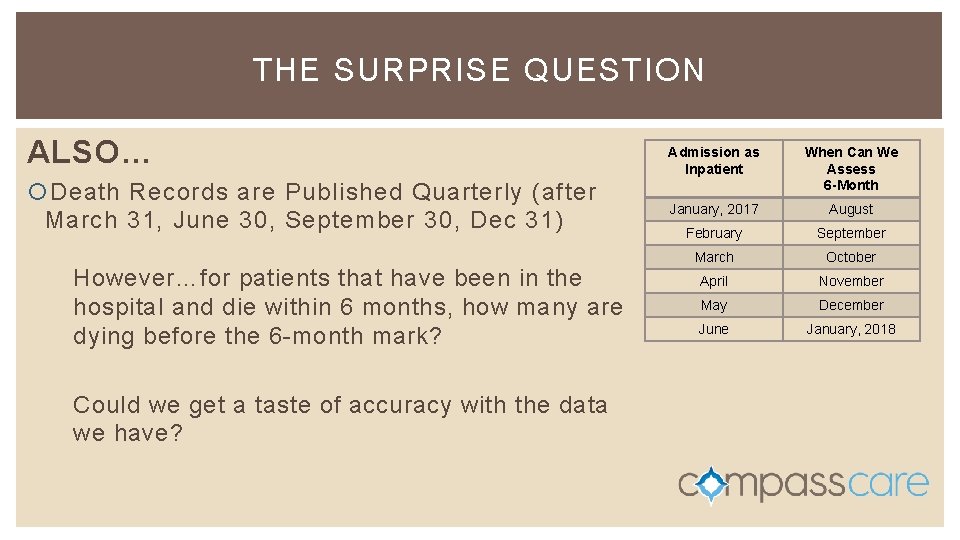
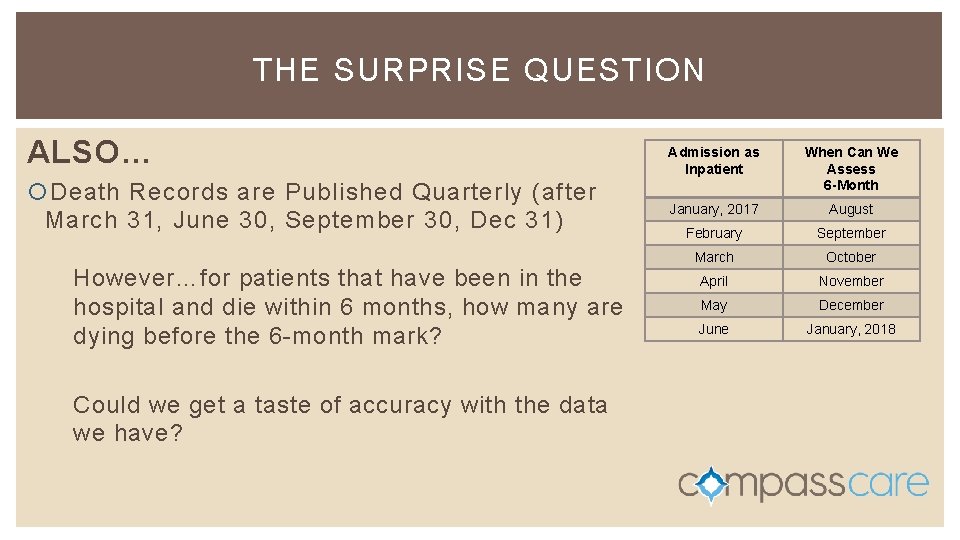
THE SURPRISE QUESTION ALSO… Death Records are Published Quarterly (after March 31, June 30, September 30, Dec 31) However…for patients that have been in the hospital and die within 6 months, how many are dying before the 6 -month mark? Could we get a taste of accuracy with the data we have? Admission as Inpatient When Can We Assess 6 -Month January, 2017 August February September March October April November May December June January, 2018
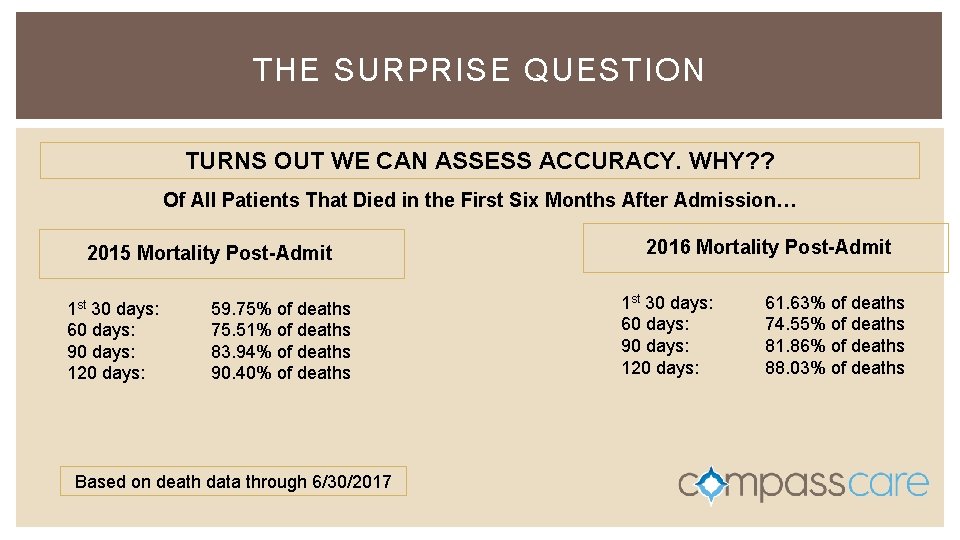
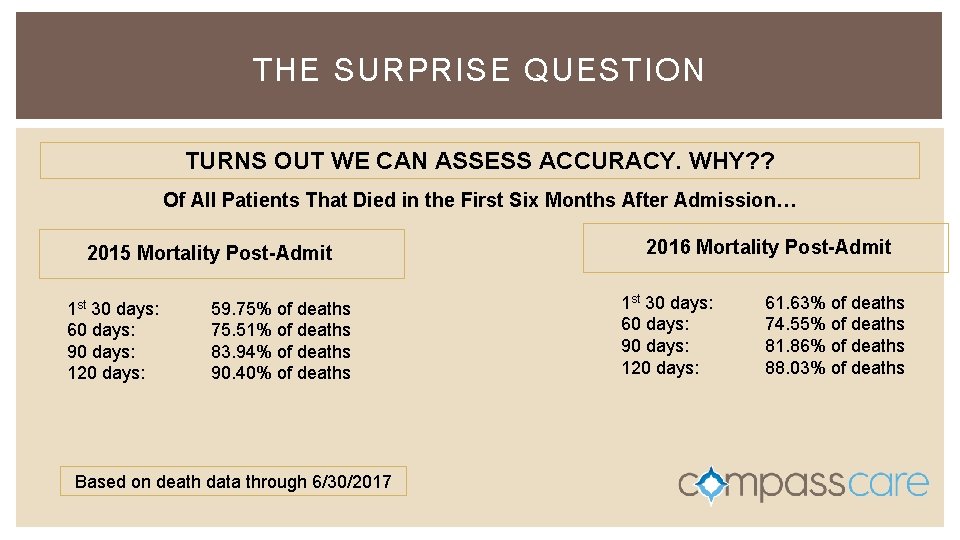
THE SURPRISE QUESTION TURNS OUT WE CAN ASSESS ACCURACY. WHY? ? Of All Patients That Died in the First Six Months After Admission… 2015 Mortality Post-Admit 1 st 30 days: 60 days: 90 days: 120 days: 59. 75% of deaths 75. 51% of deaths 83. 94% of deaths 90. 40% of deaths Based on death data through 6/30/2017 2016 Mortality Post-Admit 1 st 30 days: 60 days: 90 days: 120 days: 61. 63% of deaths 74. 55% of deaths 81. 86% of deaths 88. 03% of deaths
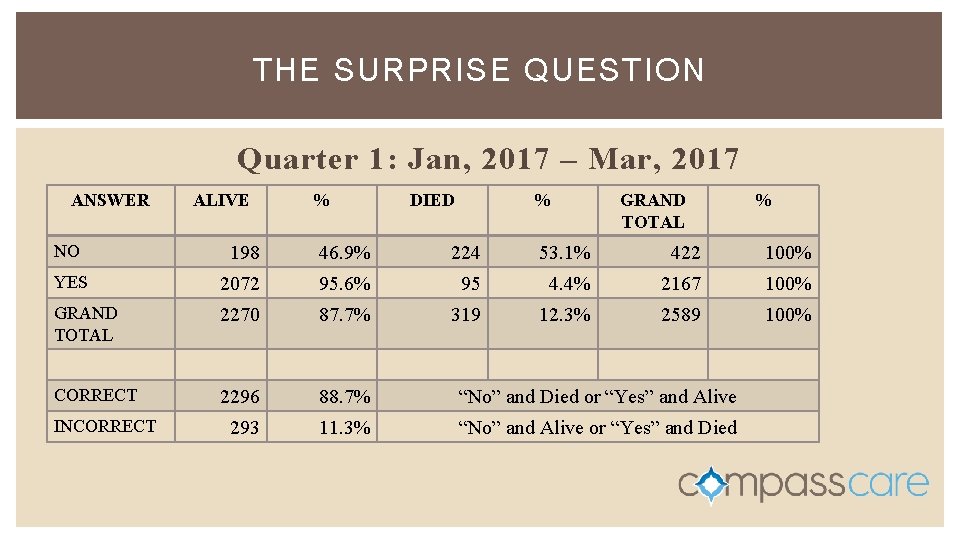
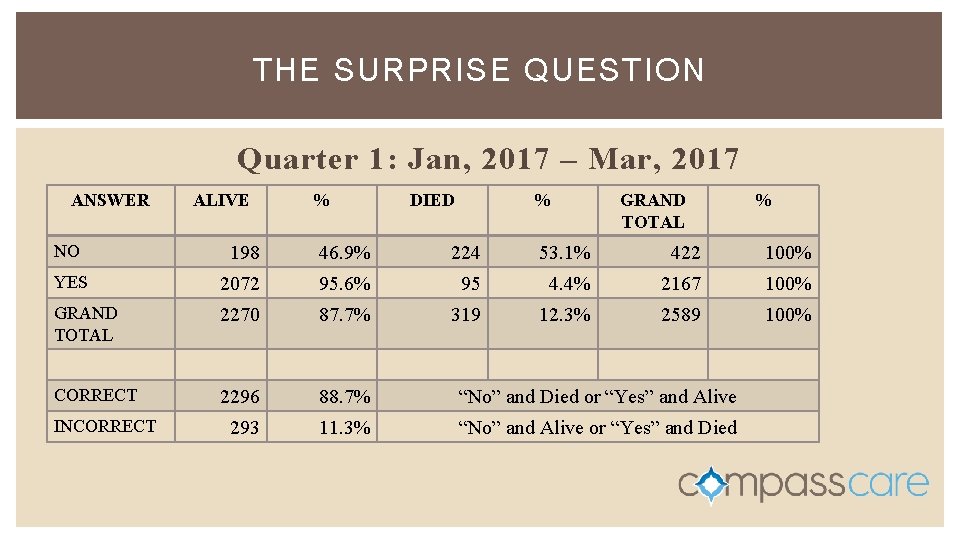
THE SURPRISE QUESTION Quarter 1: Jan, 2017 – Mar, 2017 ANSWER ALIVE % DIED % GRAND TOTAL % NO 198 46. 9% 224 53. 1% 422 100% YES 2072 95. 6% 95 4. 4% 2167 100% GRAND TOTAL 2270 87. 7% 319 12. 3% 2589 100% CORRECT 2296 88. 7% “No” and Died or “Yes” and Alive 293 11. 3% “No” and Alive or “Yes” and Died INCORRECT
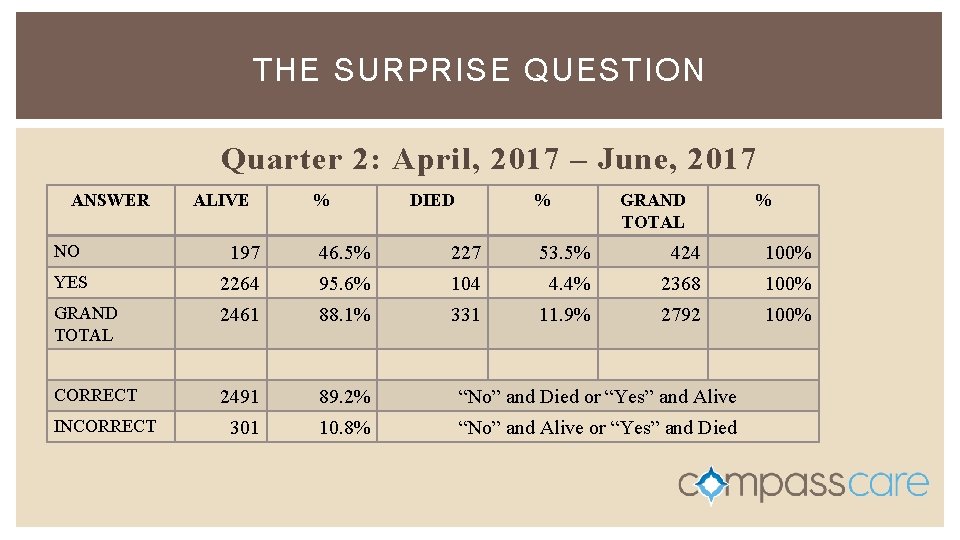
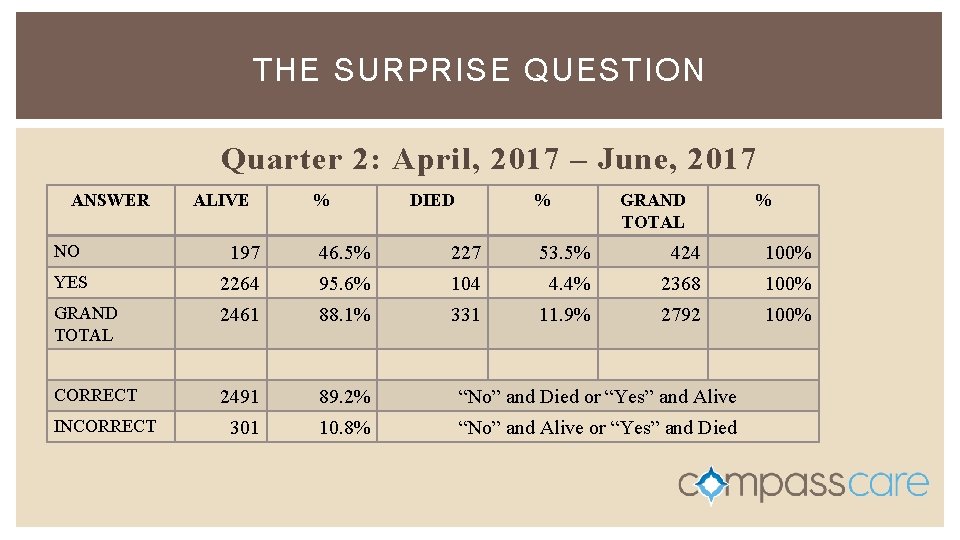
THE SURPRISE QUESTION Quarter 2: April, 2017 – June, 2017 ANSWER ALIVE % DIED % GRAND TOTAL % NO 197 46. 5% 227 53. 5% 424 100% YES 2264 95. 6% 104 4. 4% 2368 100% GRAND TOTAL 2461 88. 1% 331 11. 9% 2792 100% CORRECT 2491 89. 2% “No” and Died or “Yes” and Alive 301 10. 8% “No” and Alive or “Yes” and Died INCORRECT
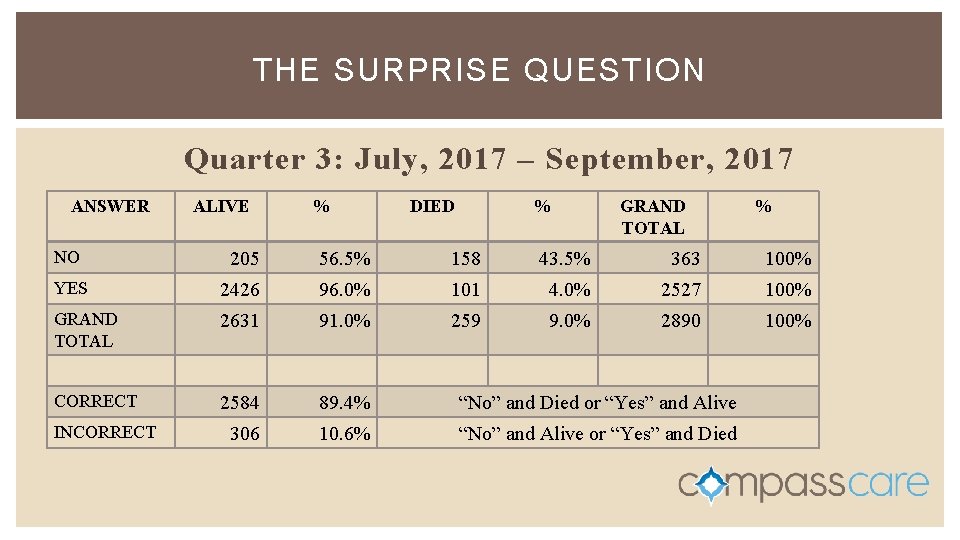
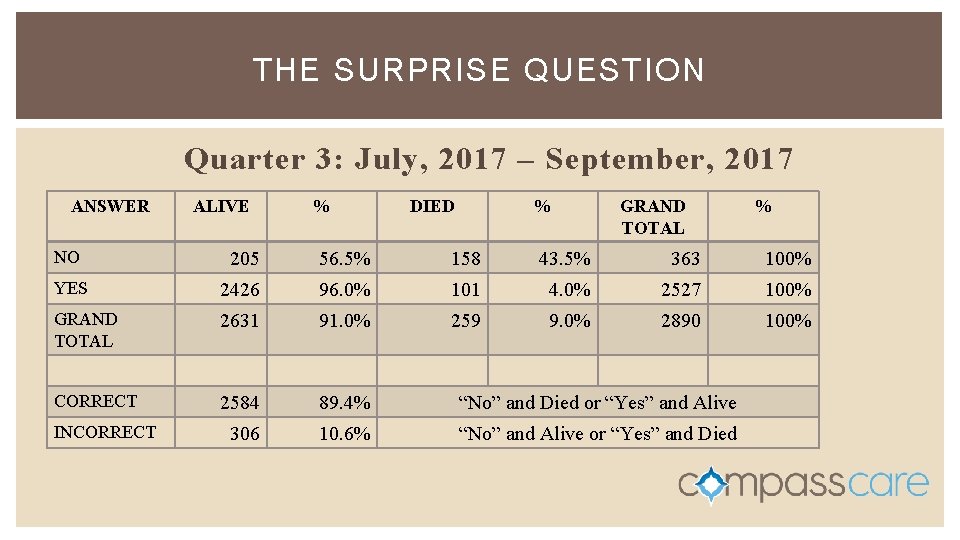
THE SURPRISE QUESTION Quarter 3: July, 2017 – September, 2017 ANSWER ALIVE % DIED % GRAND TOTAL % NO 205 56. 5% 158 43. 5% 363 100% YES 2426 96. 0% 101 4. 0% 2527 100% GRAND TOTAL 2631 91. 0% 259 9. 0% 2890 100% CORRECT 2584 89. 4% “No” and Died or “Yes” and Alive 306 10. 6% “No” and Alive or “Yes” and Died INCORRECT
THE SURPRISE QUESTION Quarter 4: October, 2017 – December, 2017 ANSWER NO YES GRAND TOTAL ALIVE % DIED % % GRAND TOTAL s h t n 6 mo % d e e n % % — d e a m t r i a f d n % th co % a t e o d n e t a t Data s death CORRECT % “No” and Died or “Yes” and Alive INCORRECT % “No” and Alive or “Yes” and Died % 100%
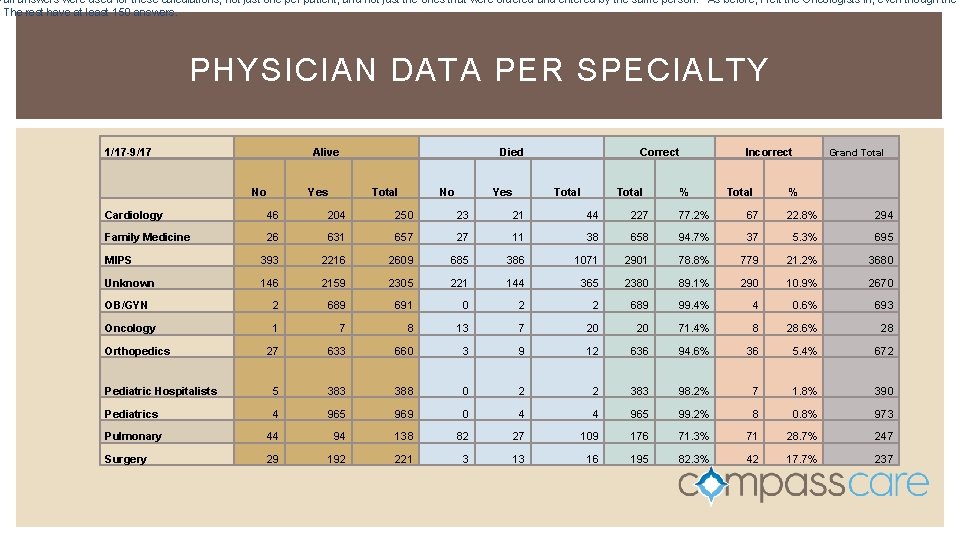
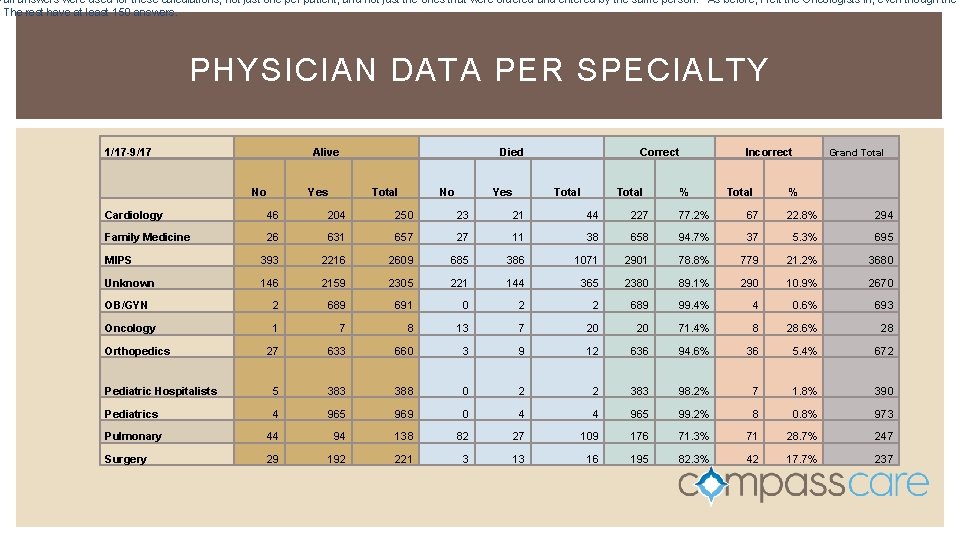
– all answers were used for these calculations, not just one per patient, and not just the ones that were ordered and entered by the same person. As before, I left the Oncologists in, even though the The rest have at least 150 answers. PHYSICIAN DATA PER SPECIALTY 1/17 -9/17 Alive No Died Yes Total No Yes Correct Total Incorrect % Total Grand Total % Cardiology 46 204 250 23 21 44 227 77. 2% 67 22. 8% 294 Family Medicine 26 631 657 27 11 38 658 94. 7% 37 5. 3% 695 MIPS 393 2216 2609 685 386 1071 2901 78. 8% 779 21. 2% 3680 Unknown 146 2159 2305 221 144 365 2380 89. 1% 290 10. 9% 2670 OB/GYN 2 689 691 0 2 2 689 99. 4% 4 0. 6% 693 Oncology 1 7 8 13 7 20 20 71. 4% 8 28. 6% 28 27 633 660 3 9 12 636 94. 6% 36 5. 4% 672 Pediatric Hospitalists 5 383 388 0 2 2 383 98. 2% 7 1. 8% 390 Pediatrics 4 965 969 0 4 4 965 99. 2% 8 0. 8% 973 Pulmonary 44 94 138 82 27 109 176 71. 3% 71 28. 7% 247 Surgery 29 192 221 3 13 16 195 82. 3% 42 17. 7% 237 Orthopedics

ANOTHER INITIATIVE: ADVANCE CARE PLANNING Changing the Game
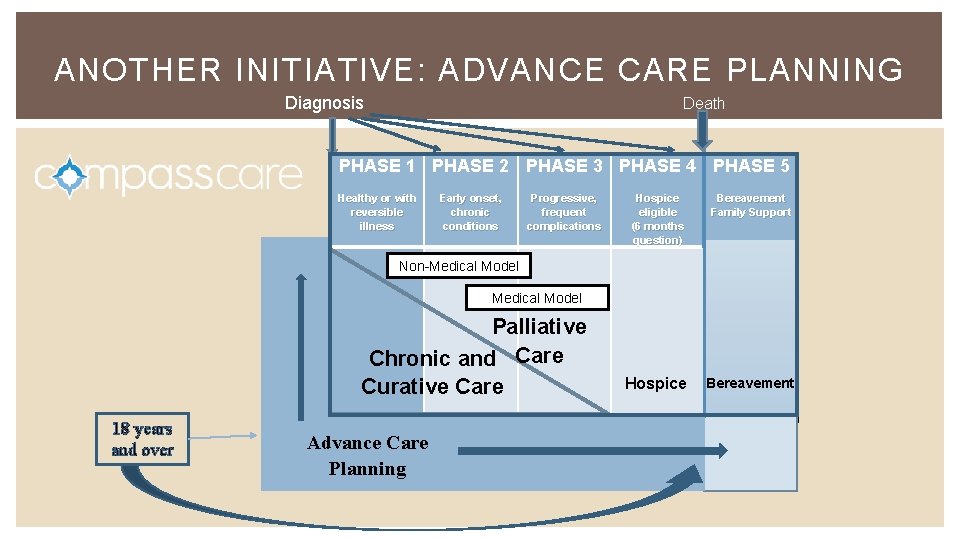
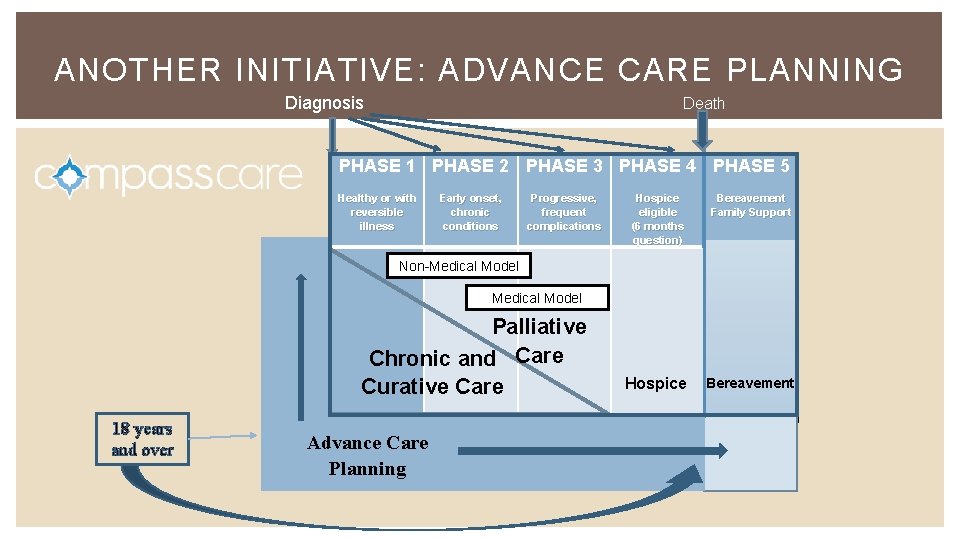
ANOTHER INITIATIVE: ADVANCE CARE PLANNING Diagnosis Death PHASE 1 PHASE 2 PHASE 3 PHASE 4 PHASE 5 Healthy or with reversible illness Early onset, chronic conditions Progressive, frequent complications Hospice eligible (6 months question) Bereavement Family Support Hospice Bereavement Non-Medical Model Palliative Chronic and Care Curative Care 18 years and over Advance Care Planning
FIVE WISHES IN YAKIMA: SOME STATISTICS • 70% of individuals would wish to die at home • 82% say it is important to have EOL wishes in writing • 80% say that if seriously ill they would want to talk with their doctor about EOL care • 70% of people die in a SNF, hospital, or LTC facility • 23% have ever written their EOL wishes • 7% report having an end of life conversation with their doctor • 8. 8 x increased likelihood of prolonged grief if loved one dies in ICU vs hospice • 5 x increased likelihood of PTSD if loved one dies in ICU vs. hospice • 10 more days spent in the hospital in the last 2 years of life when the patient does not participate in advance care planning Stats thanks to Honoring Choices PNW and Californian Healthcare Foundation
FIVE WISHES IN YAKIMA: SOME STATISTICS Why are we using FIVE WISHES? Valid in 42 States Customizable Addresses Biggest Fears Cost-Effective User-Friendly Not a Do Not Attempt Resuscitation Order in the Home We Have Trained Facilitators To Go To Community Groups, Homes, Churches, Hospital, Clinics for Five Wishes Parties We Have Distributed Over 70, 000 Five Wishes In Our Community Memorial Foundation Pays for Five Wishes for Yakima Stats thanks to Honoring Choices PNW and Californian Healthcare Foundation
NEARLY 2 YEARS INTO SURPRISE QUESTION, WHAT WE ARE LEARNING: Not all physicians understanding difference between advance directives and POLST Hospital/Clinic Physicians benefit from team members knowing § Decision-making order § How to provide difficult conversations § Objective methods for providing best care possible for patients with advancing illness and end-of-life concerns We still have work to do Surprise Question is a key element to providing great medical care and getting patients onto extra levels of care Stats thanks to Honoring Choices PNW and Californian Healthcare Foundation

QUESTIONS? Thank you!! Stats thanks to Honoring Choices PNW and Californian Healthcare Foundation